Abstract
Introduction
Our aim was to assess the feasibility of using time-resolved 3D phase-contrast (4D flow) MRI to characterize extracranial-intracranial (EC-IC) bypass.
Methods
We enrolled 32 patients who underwent EC-IC bypass (15 men, 17 women; mean age 66.4 years). In all, 16 underwent radial artery graft (RAG) bypass and 16 underwent superficial temporal artery (STA) bypass. 4D flow MRI, time-of-flight (TOF) magnetic resonance angiography (MRA), and computed tomography angiography (CTA) were performed. Bypass patency, flow direction, and blood flow volume (BFV) of each artery were determined by 4D flow MRI. Arterial diameters were measured by TOF-MRA and CTA. We compared RAG and STA bypasses by evaluating the flow direction and BFV of each artery. We evaluated the correlation between arterial diameters (measured by CTA or MRA) and the BFV and the detectability of flow direction (measured by 4D flow MRI) of each artery.
Results
4D flow MRI confirmed the patency of each bypass artery. Flow direction of the M1 segment of the middle cerebral artery and BFV in the bypass artery differed between RAG and STA groups (p < 0.01). BFV in the bypass slightly correlated with the diameters on CTA (p < 0.05, R 2 = 0.287). Of the 29 arteries in the circle of Willis, nine were not depicted on 4D flow MRI. Cutoff values for arterial diameters on CTA and TOF-MRA for detecting the artery on 4D flow MRI were 2.4 and 1.8 mm, respectively.
Conclusion
4D flow MRI provided unique information for characterizing EC-IC bypasses, although this detectability is limited when addressing small arteries with slow flow.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Extracranial-intracranial (EC-IC) bypass is an option in carefully selected patients with ischemic cerebrovascular disease and a complex intracranial aneurysm, although its use remains controversial [1–5]. Cerebral catheter angiography has been considered a gold standard for assessing the patency of the EC-IC bypass, collateral vessel formation, and individual vessel contributions to cerebral blood flow. However, the complications associated with diagnostic cerebral catheter angiography are not rare [6]. This invasive follow-up procedure should be replaced by some noninvasive imaging modality, because the long-term patency of EC-IC bypass grafts has been reported to be high, so that the patients need repeated follow-up studies [7]. During the last three decades, alternative imaging procedures have been developed. The representative modalities are computed tomography angiography (CTA) and time-of-flight magnetic resonance angiography (TOF-MRA) [8, 9]. Both are widely performed. Although CTA provides vascular images with high spatial resolution, it can lead to side effects from the contrast injection and radiation exposure, making it less suitable for repeated follow-up evaluations. Compared to cerebral catheter angiography, a drawback of both CTA and MRA is the lack of hemodynamic information, flow direction, flow speed, and the contributions of individual vessels to cerebral blood flow.
The bypass arteries and native arteries work in a complementary fashion, with the pattern of flow dynamics varying depending on pretreatment and posttreatment conditions. Some state-of-the-art MRI sequences to assess for these flow dynamics in detail have been evaluated. They have been found to determine qualitative flow dynamics or quantitative information [10–16]. Most of them, however, lack initiative output, do not provide information on each vessel’s contribution, or do not have an acceptable scan duration for combination with other conventional clinical imaging workups. Among them are diffusion-weighted image (DWI), fluid-attenuated inversion recovery (FLAIR), and TOF-MRA.
Ideal imaging modalities for assessing the EC-IC bypass must meet a number of requirements: (1) imaging without being invasive; (2) no extra radiation dose; (3) require no additional contrast media; (4) output includes flow-functional information; (5) separate information from each artery; (6) initiative output; and (7) imaging easy to combine with other clinical examinations. Time-resolved three-dimensional phase-contrast (4D flow) MRI is one of the promising methods that meets all of these requirements. It acquires the quantitative flow information in each voxel, which can generate qualitative and quantitative flow images [17, 18]. No studies, however, have evaluated flow dynamics in an EC-IC bypass using 4D flow MRI.
The purposes of this study were threefold: (1) to present our initial experience with 4D flow MRI evaluation of two types of EC-IC bypass; (2) to assess the feasibility of 4D flow MRI (we focused on quantitative aspects by comparing the blood flow volume measured by 4D flow MRI to the arterial diameter measured by CTA and MRA); and (3) to clarify the limits of 4D flow MRI capability (we assessed the detectability of flow direction in small vessels).
Materials and methods
This study followed the institutional ethics guideline approved by the institutional review board. We enrolled 32 patients (15 men, 17 women; mean age, 66.4 years, range 41–87 years) with no symptoms related to neurovascular disease and who underwent EC-IC bypass. The 16 patients who also underwent ligation of the internal carotid artery (ICA) for treatment of a complex aneurysm had radial artery graft (RAG) bypass surgery. The remaining 16 patients with ICA occlusion (ICO) underwent superficial temporal artery (STA) bypass. In all, 15 of the 32 patients underwent CTA within 90 days. The average interval from CTA to 4D flow MRI was 13 days (range 33 days before to 85 days after). Among these 15 patients, 9 had a RAG bypass and 6 underwent STA bypass.
Imaging techniques
In addition to clinical MRI sequences, DWI, FLAIR, and TOF-MRA, 4D flow MRI was performed using a Achieva 3.0-T MRI unit with eight-channel head coil (Philips Medical Systems, Best, The Netherlands). 4D flow MRI and TOF-MRA were used for further analyses. The 4D flow MRI parameters were as follows: repetition time/echo time (TR/TE) 8.4/5.4 ms; TFE factor 2; temporal resolution 67.2 ms; flip angle (FA) 13°; bandwidth 228.6 Hz, velocity encoding (VENC) 70 cm/s, FOV 210 × 210 × 44.8 mm3, 1 slab acquisition, actual voxel size 1.19 × 1.36 × 2.80 mm3, reconstruction voxel size 0.82 × 0.82 × 1.40 mm3; 15 cardiac phases; sensitivity encoding (SENSE) factor 2; k-space shutter on (partial k-space coverage in phase- and slice-encoding direction; 87.9 %); nominal acquisition time 6 min; background phase correction was performed on the scanner by using the method provided by the vendor [19].
The parameters of TOF-MRA were as follows: TR/TE 25/3.45 ms; FA 18°; bandwidth 73.8 Hz, FOV 210 × 210 × 96 mm3, 5 slab acquisition, slab thickness 36 mm, actual voxel size 0.39 × 0.77 × 1.20 mm3, reconstruction voxel size 0.39 × 0.39 × 0.60 mm3; 15 cardiac phases; SENSE factor 2.2.
CTA with contrast injection was performed using 64-slice multidetector CT (VCT; GE Healthcare, Waukesha, WI, USA) with the following parameters: tube voltage 120 kV; tube current 300 mA; collimation 64 DAS; pitch 0.531.1 (10.62 mm/rotation); rotation time 0.4 s; coverage speed 10.62 mm (26.56 mm/s); FOV 22 cm; voxel size 0.43 × 0.43 × 0.625 mm3; injection rate 4 ml/s with contrast medium using bolus tracking in the common carotid artery.
Reconstruction of 4D flow MRI
The velocity data were generated from a 4D flow MRI data set using GT Flow software (GyroTools, Zurich, Switzerland). We also imported the TOF-MRA data set, which was resliced on the MRI scanner (View Forum; Philips Medical Systems, Best, The Netherlands) to the same slice thickness and orientation as those of the 4D flow MRI dataset. Intensity thresholds were applied using MRA images. Flow volumes were measured by manual region-growing on the three sequential planes, which were resliced as perpendicular to the target artery points and averaged from these three values. Manual velocity unwrapping was performed in four patients. 3D pathline imaging and 2D in-plane vector map imaging were generated for further study (Figs. 1 and 2). These procedures were completed within ≤30 min [19].
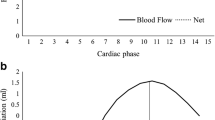
Analysis was performed using GT Flow software. Magnitude image (top left), in-plane vector overlay image (top right), continuous graph of velocity on the voxel (bottom left), and quantitative values (bottom right). We set the voxel contour at the right postcommunicating artery (red dot, arrowheads on the magnitude image) after masking the nonvascular lesion with the dedicated threshold. The in-plane vector overlying the image provides the color-coded flow direction and flow velocity at each voxel (red is fast and blue is slow). The continuous graph can provide the velocity along the cursor in each direction—right to left (RL), anteroposterior (AP), foot to head FH)—during the cardiac cycle. We could then easily detect the flow direction from this information
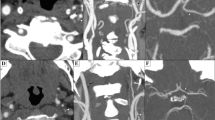
A 75-year-old woman underwent left internal carotid artery ligation and placement of a radial arterial graft. a–e Three-dimensional surface-rendered arterial images of time-resolved 3D phase contrast (4D flow) MRI generated by GT Flow software. Each of the five images provides the flow at each time point. The two regions of interest (ROIs) for flow analysis were in a grafted artery (arrows, a) and at the right internal carotid artery (ICA) (arrowheads, a). The red pathline, which simulates blood flow from the ROI of the bypass artery, runs through the bypass artery (arrows, b), the left M1 (arrows, c), and the left A1 (arrows, d). Part of this flow runs through the right A1 together with the blue pathline (arrows, e), which simulates blood flow from the right ICA. The images clearly depict patency of the bypass, retrograde flow of the ipsilateral M1, and antegrade flow of the ipsilateral A1. The ipsilateral postcommunicating artery is unclear. Graft flow was 3.97 ml/s, right ICA flow 9.69 ml/s, and basilar artery flow 4.14 ml/s. For a more detailed description, the reader is referred to Supplementary Movie 1
Imaging evaluation
One neuroradiologist with 10 years of experience and who had interpreted >100 cases of cerebral 4D flow MRI was enlisted to evaluate 4D flow MRI, TOF-MRA, and CTA results in random order. For 4D flow analysis, we first assessed the patency of the graft by 3D pathline imaging. Second, we visually assessed the flow direction in the ipsilateral M1 segment of the middle cerebral artery (MCA) and circle of Willis, the ipsilateral A1 segment of the anterior cerebral artery (ACA), and the posterior communicating artery (Pcom). The flow direction was classified as being in the antegrade and retrograde directions compared to the flow direction of the native flow. This flow direction was determined by 2D in-plane vector map imaging and 3D pathline imaging. When the flow direction was not determined by 3D pathline imaging, we investigated the vector data in each voxel, which corresponds to the vessel seen on TOF-MRA. For each direction—right-to-left (RL), anteroposterior (AP), foot-to-head (FH)—the flow speeds at the target voxels during the cardiac cycle were easily calculated as continuous graphs on GT Flow software (Fig. 1). We chose at least three voxels from the target artery. If all of them had the same flow direction during the cardiac cycle, the flow direction was determined according to these results. If there was a difference between flow results on the voxels, we defined the flow direction in the vessel as “unclear.” As a result, to-and-fro flow was classified as unclear. Third, we quantified the blood flow volume (BFV) of the bypass artery, ICA, and basilar artery (BA). In the 15 patients who underwent both CTA and 4D flow MRI combined with TOF-MRA within 3 months, we measured the diameter of the bypass artery, ipsilateral A1 segment of the ACA, and the Pcom on three slices for each artery and obtained their averages. These slices were identical to that on the 4D flow MRI. We used a dedicated workstation for the analysis (AZE Virtual Place; AZE, Tokyo, Japan).
Statistics
We evaluated correlations between the bypass pattern (RAG or STA) and flow information, with the following results:
-
1.
regarding the flow pattern on each ipsilateral M1, A1, and Pcom, the flow patterns were assigned to one of two groups. One group had a native flow pattern (antegrade or unclear), and the other had a nonnative pattern (retrograde). Fisher’s exact test was performed for each artery.
-
2.
Regarding the BFV of the bypass artery, ICO, and BA, an unpaired t test with Bonferroni correction was performed for each artery.
We also evaluated the correlation between arterial diameter for each static imaging (CTA and MRA), with the findings obtained with 4D flow MRI: (1) Pearson’s product-moment correlation coefficient test was performed on the flow volume of the bypass artery; (2) to test the detectability of flow direction in ipsilateral A1 and Pcom, an unpaired t test was performed for each artery. For all analyses, a value of p < 0.05 was deemed to indicate statistical significance. All statistical analyses were carried out with IBM SPSS Statistics19.0.0 (IBM, Armonk, NY, USA).
Results
The flow volume in the BA was not calculated in two patients because it was out of the FOV. There were no apparent artifacts (e.g., motion artifact, susceptibility artifact by implant) that caused MRI deterioration. Representative cases are given in Fig. 2 and Supplementary Movie 1. EC-IC bypass flow was successfully generated in all patients. Nonnative, retrograde flow was observed at the M1 segment of the MCA in 10 of the 19 patients. Retrograde flow at M1 was observed more frequently in patients with a RAG bypass than in those with an STA bypass (p < 0.01) (Table 1). The BFVs of the bypass arteries were significantly higher in patients with a RAG bypass than in those with an STA bypass (3.19 ± 1.13 vs. 1.68 ± 0.97 ml, p < 0.01). In contrast, there was no correlation of the BFV of the contralateral ICA or BA with the type of bypass artery (Table 2). The BFV in the bypass artery significantly (but only slightly) correlated with the arterial diameter of the CTA (p < 0.05, R 2 0.287) and not with that of the TOF-MRA (Fig. 3). One Pcom was hypoplastic on CTA and TOF-MRA. Other arteries were detectable on both CTA and TOF-MRA. In these 29 arteries, the detectability of flow direction in the ipsilateral A1 segment and the Pcom artery were significantly correlated with the arterial diameter seen on TOF-MRA (p < 0.01) but not with that of the CTA (Fig. 4). The cutoff values for the CTA and the TOF-MRA arterial diameters to detect the artery on 4D flow MRI were 2.4 and 1.8 mm, respectively.
Scatterplot of the correlation between the arterial diameter on CTA (a) and time-of-flight (TOF) MRA (b) and the flow volume of the bypass artery. A total of 15 bypass arteries were assessed. Blood flow volume (BFV) in the bypass artery significantly but slightly correlated with the arterial diameter measured on CTA (p < 0.05, R 2 = 0.287) and was not correlated with that measured on MRA
Dot plot of the correlation between each arterial diameter measured on CTA (a) and TOF-MRA (b), and the detectability of flow direction in arteries in the circle of Willis. Merged figure is shown as another scatter plot (c). In 15 patients (29 arteries), the ipsilateral A1 and postcommunicating artery were assessed. The detectability of flow direction on 4D flow MRI statistically correlated with the arterial diameter measured on MRA (p < 0.01) but did not correlate with that measured on CTA. The cutoff values of the diameter measured on CTA and on TOF-MRA to detect the artery on 4D flow MRI were 2.4 and 1.8 mm, respectively
Discussion
There were four major findings in this study: (1) the patency of the bypass and the flow direction in the M1 segment of the MCA in patients with EC-IC bypass were successfully generated by 4D flow MRI; (2) the flow characteristics after bypass surgery differed depending on the presurgerical condition and the choice of bypass artery; (3) the flow volume of the bypass artery had a weak correlation with the arterial diameter on CTA and no correlation on MRA; and (4) the detectability of flow directions in small arteries on 4D flow MRI had a significant but slight correlation with the arterial diameter on MRA, and detectability was not correlated with arterial diameters on CTA.
This study revealed that flow patterns and BFVs differed between the RAG and STA groups because of differences in the diameters and the role of the bypass. The RAG bypass vessel has a wider diameter and plays a role in flow replacement, whereas the STA bypass has a narrow diameter, which plays a role in flow augmentation [3]. In this study, 4D flow MRI provided comprehensive and objective evaluation of this difference. Bypass function has traditionally been assessed by a grading system using angiographic images [14], with the vascular tree filled with contrast material injected from the bypass artery. However, such a grading system is difficult to quantify and less easy to reproduce. Also, manual injection of a contrast medium causes nonphysiologic hemodynamics. Although this effect may be small, 4D flow MRI offers more accurate imaging. Some state-of-art MRI techniques have been performed to assess hemodynamics in patients with EC-IC bypass [10, 12, 16]. However, it is difficult to provide initiative results or information on each vessel (i.e., which vessels are perfused by blood flowing through from the bypass).
In regard to qualitative assessment using 4D flow MRI, interobserver variability is one of the issues about which care should be taken. Although there are no large cohort studies of cerebral vascular lesions, Stankovic et al. assessed the interobserver variability on 4D flow MRI visualization of the vascular system in regard to abdominal lesions [20]. They showed high interobserver agreement (Cohen’s kappa value was 0.93) for assessing the vascular tree, including small-diameter vessels, hepatic artery, and slow-flow vessels, the portal branches on 4D flow MRI. In contrast, quantitative analysis by 4D flow MRI—based on almost the same quantification theory as is used for 2D phase-contrast MRI—has been evaluated in many studies and is an established technique [21].
Several studies used 2D phase-contrast imaging to evaluate patients with an EC-IC bypass. Horn et al. performed 2D phase-contrast MRI in 41 patients with EC-IC bypass for ICO [15]. They concluded that BFV on 2D phase-contrast MRI correlated with the grading system by catheter angiography and that it provides more exact and investigator-independent information. Amin et al. performed a similar study in 59 patients with an EC-IC bypass using STA or long vein grafts for cerebral flow augmentation and flow replacement [14]. They also mentioned that the correlation between 2D phase-contrast MRI and catheter angiography was excellent. The BFV of the bypass artery was assessed in these two studies. The BFV of the STA bypass was 0.81–2.96 ml/s in the former study and 1.75 ± 0.12 ml in the latter study. Brockmann et al. performed a similar study in patients with a high-flow bypass using the saphenous vein, whose diameter is similar to that of the radial artery. They estimated that the BFV of the bypass was 3.20 ± 1.22 ml/s [22]. Although care should be taken when comparing these results because patients’ backgrounds and surgical procedures vary, our results (1.68 ± 0.97 ml/s in the STA bypass and 3.19 ± 1.13 ml/s in the RAG bypass) were consistent with these results. Compared to 2D phase-contrast imaging, one of the advantages of 4D flow is that it can acquire comprehensive flow information in a large FOV. This encourages us to save the procedure for choosing the imaging slice perpendicular to the target vessel. If the target vessel is small or complicated, the examination requires a highly skilled operator during the MRI scan, which is difficult in clinical setting. The arterial diameter on CTA was not strongly correlated with the flow volume, suggesting that the static image did not reflect the functional information, BFV well. To obtain information on flow dynamics, 4D flow MRI is mandatory.
The parameters of our protocol were an approximately 1-cm voxel size, 67.2-ms temporal resolution, and VENC at 70 cm/s. For covering both the bypass artery and the circle of Willis, we determined that these parameters are suitable for clinical use (6-min scan duration) and could be added to other sequences for routine clinical MRI examinations (e.g., TOF-MRA, FLAIR, DWI). If the scan duration is prolonged, patient motion is inevitable even in the case of volunteers [23]. The cerebral artery is very small, so any motion artifact could be critical. In this setting, 9 of 29 small arteries were not depicted by 4D flow MRI because of the limited spatial resolution and/or velocity resolution. TOF-MRA was more significantly correlated with detectability on 4D flow MRI scans than on CTA. The reason might be that some part of the signal intensity on TOF-MRA is derived from the flow velocity, which is linked to the velocity noise ratio (VNR) on 4D flow MRI. The VNR of 4D flow MRI is based on two factors. One is velocity itself, and the other is the signal noise ratio of vascular on magnitude image of 4D flow MRI. The latter also depends on the flow velocity because in-flow phenomenon contributes to the signal of the vascular on magnitude image [24]. Our result may indicate that even if the vascular has some extent of lumen’s diameter, the flow direction could not be detected on 4D flow MRI unless it has sufficient flow velocity.
There are several solutions that could avoid prolonged scanning times and thus improve the resolution. One is to use a stronger magnetic field. Seven-tesla MRI improves the spatial resolution on 4D flow MRI at the same scan time [25]. Second is to add an acceleration technique, such as recently proposed acceleration schemes which use correlations in space and time [26]. We can use the excess scan time to improve the resolution. Third is to use blood-pool contrast medium. An improved signal to noise ratio on magnitude images also affects velocity resolution [27]. Fourth, for improving velocity resolution, the multi-VENC sequence is useful [28]. By using this technique, we are able to acquire information continuously from slow- to high-velocity flow. 4D flow MRI combined with these methods can provide more-detailed flow information.
The major limitation in our study is that the clinical impact of flow information on 4D flow MRI is not clear in this preliminary study. This situation is present partially because no previous studies have provided sufficient evidence to assess prognosis in patients with EC-IC bypass. This is an intrinsic limitation when a new imaging technique is introduced. The second limitation is that both quantitative and qualitative assessments were performed by only one radiologist. However, high interobserver agreement was proved in a previous study [20]. Third, we did not compare 4D flow result with other “gold standard” modalities, catheter angiography, or Doppler echo. To replace these established examinations to 4D flow MRI, it may be needed to perform further study. However, previous studies proved that the qualitative and quantitative information derived from phase-contrast MRI had good correlation with other gold standard modalities [21]. Fourth, the VENC was uniform in this study. The VNR is definitely improved by setting an appropriate VENC for each patient and each artery. When we choose other targets (i.e., detailed assessment of the circle of Willis), we have to change the parameters and perform another study.
In conclusion, this preliminary study revealed that 4D flow MRI could provide unique information for assessing flow dynamics in patients with EC-IC bypass, both qualitatively and quantitatively. Its detectability of flow direction, however, is limited when addressing small arteries with slow flow.
References
Hanggi D, Steiger HJ, Vajkoczy P (2014) The role of MCA-STA bypass surgery after COSS and JET: the European point of view. Acta Neurochir Suppl 119:77–78
Vilela MD, Newell DW (2008) Superficial temporal artery to middle cerebral artery bypass: past, present, and future. Neurosurg Focus 24:2
Sia SF, Morgan MK (2013) High flow extracranial-to-intracranial brain bypass surgery. J Clin Neurosci 20:1–5
Murai Y, Mizunari T, Umeoka K, Tateyama K, Kobayashi S, Teramoto A (2011) Radial artery grafts for symptomatic cavernous carotid aneurysms in elderly patients. Neurol India 59:537–541
Kataoka H, Miyamoto S, Ogasawara K et al (2015) Results of prospective cohort study on symptomatic cerebrovascular occlusive disease showing mild hemodynamic compromise [Japanese extracranial-intracranial bypass trial (JET)-2 study]. Neurol Med Chir (Tokyo) 55:460–468
Kaufmann TJ, Huston J 3rd, Mandrekar JN, Schleck CD, Thielen KR, Kallmes DF (2007) Complications of diagnostic cerebral angiography: evaluation of 19,826 consecutive patients. Radiology 243:812–819
Schaller B (2008) Extracranial-intracranial bypass to reduce the risk of ischemic stroke in intracranial aneurysms of the anterior cerebral circulation: a systematic review. J Stroke Cerebrovasc Dis 17:287–298
Thines L, Agid R, Dehdashti AR et al (2009) Assessment of extracranial-intracranial bypass patency with 64-slice multidetector computerized tomography angiography. Neuroradiology 51:505–515
Praharaj SS, Coulthard A, Gholkar A, English P, Mendelow AD (1996) Magnetic resonance angiographic assessment after extracranial-intracranial bypass surgery. J Neurol Neurosurg Psychiatry 60:439–441
Tsuchiya K, Imai M, Nitatori T, Kimura T (2013) Postoperative evaluation of superficial temporal artery-middle cerebral artery bypass using an MR angiography technique with combined white-blood and black-blood sequences. J Magn Reson Imaging 38:671–676
Tsuchiya K, Honya K, Fujikawa A, Tateishi H, Shiokawa Y (2005) Postoperative assessment of extracranial–intracranial bypass by time-resolved 3D contrast-enhanced MR angiography using parallel imaging. Am J Neuroradiol 26:2243–2247
Akashi T, Taoka T, Miyasaka T et al (2010) Magnetic resonance angiography with midsagittal saturation for the assessment of blood flow from superficial temporal artery-to-middle cerebral artery bypass. J Comput Assist Tomogr 34:89–92
Neff KW, Horn P, Dinter D, Vajkoczy P, Schmiedek P, Duber C (2004) Extracranial-intracranial arterial bypass surgery improves total brain blood supply in selected symptomatic patients with unilateral internal carotid artery occlusion and insufficient collateralization. Neuroradiology 46:730–737
Amin-Hanjani S, Shin JH, Zhao M, Du X, Charbel FT (2007) Evaluation of extracranial-intracranial bypass using quantitative magnetic resonance angiography. J Neurosurg 106:291–298
Horn P, Vajkoczy P, Schmiedek P, Neff W (2004) Evaluation of extracranial-intracranial arterial bypass function with magnetic resonance angiography. Neuroradiology 46:723–729
Lanzman R, Kröpil P, Schmitt P et al (2011) Nonenhanced ECG-gated time-resolved 4D Steady-state free precession (SSFP) MR angiography (MRA) for assessment of cerebral collateral flow: comparison with digital subtraction angiography (DSA). Eur Radiol 21:1329–1338
Markl M, Frydrychowicz A, Kozerke S, Hope M, Wieben O (2012) 4D flow MRI. J Magn Reson Imaging 36:1015–1036
Meckel S, Leitner L, Bonati LH et al (2013) Intracranial artery velocity measurement using 4D PC MRI at 3 T: comparison with transcranial ultrasound techniques and 2D PC MRI. Neuroradiology 55:389–398
Sekine T, Amano Y, Takagi R, Matsumura Y, Murai Y, Kumita S (2014) Feasibility of 4D flow MR imaging of the brain with either Cartesian y-z radial sampling or k-t SENSE: comparison with 4D flow MR imaging using SENSE. Magn Reson Med Sci 13:15–24
Stankovic Z, Jung B, Collins J et al (2014) Reproducibility study of four-dimensional flow MRI of arterial and portal venous liver hemodynamics: influence of spatio-temporal resolution. Magn Reson Med 72:477–484
Lotz J, Meier C, Leppert A, Galanski M (2002) Cardiovascular flow measurement with phase-contrast MR imaging: basic facts and implementation. Radiographics 22:651–671
Brockmann C, Gerigk L, Vajkoczy P, Groden C, Neumaier-Probst E (2012) Magnetic resonance imaging flow quantification of non-occlusive excimer laser-assisted EC-IC high-flow bypass in the treatment of complex intracranial aneurysms. Clin Neuroradiol 22:39–45
Ikari Y, Nishio T, Makishi Y et al (2012) Head motion evaluation and correction for PET scans with 18F-FDG in the Japanese Alzheimer’s disease neuroimaging initiative (J-ADNI) multi-center study. Ann Nucl Med 26:535–544
Dyverfeldt P, Bissell M, Barker AJ et al (2015) 4D flow cardiovascular magnetic resonance consensus statement. J Cardiovasc Magn Reson 17:72
van Ooij P, Zwanenburg JJ, Visser F et al (2013) Quantification and visualization of flow in the circle of willis: time-resolved three-dimensional phase contrast MRI at 7 T compared with 3 T. Magn Reson Med 69:868–876
Pedersen H, Kozerke S, Ringgaard S, Nehrke K, Kim WY (2009) k-t PCA: temporally constrained k-t BLAST reconstruction using principal component analysis. Magn Reson Med 62:706–716
Bock J, Frydrychowicz A, Stalder AF et al (2010) 4D phase contrast MRI at 3 T: effect of standard and blood-pool contrast agents on SNR, PC-MRA, and blood flow visualization. Magn Reson Med 63:330–338
Ha H, Kim GB, Kweon J et al (2015) Multi-VENC acquisition of four-dimensional phase-contrast MRI to improve precision of velocity field measurement. Magn Reson Med. doi:10.1002/mrm.25715
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
We declare that all human studies have been approved by the Institutional Review Board and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. We declare that all patients gave informed consent prior to inclusion in this study.
Conflict of interest
We declare that we have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Movie 1
(MPG 4582 kb)
Rights and permissions
About this article
Cite this article
Sekine, T., Takagi, R., Amano, Y. et al. 4D flow MRI assessment of extracranial-intracranial bypass: qualitative and quantitative evaluation of the hemodynamics. Neuroradiology 58, 237–244 (2016). https://doi.org/10.1007/s00234-015-1626-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-015-1626-1