Abstract
Purpose
In critically ill patients treated with meropenem, the proposed pharmacokinetics/pharmacodynamics (PK/PD) efficacy index is to keep the free drug concentration 4–5 times above the minimum inhibitory concentration (MIC) of the germ isolated, for 100% of the interval regimen. The objectives were to design a population pharmacokinetics model for meropenem in critically ill patients and to evaluate different dosage schemes that achieve the optimal PK/PD objectives.
Methods
This retrospective, observational, single-centre study included 80 critically ill patients (154 samples) treated with meropenem between May 2011 and December 2017. Patient data, concentrations, treatment and bacteriological variables were collected from electronic medical records. Total and free concentrations of meropenem were modelled in Pmetrics. Monte Carlo simulations were performed to assess the probability of achieving the PK/PD target for different dosage regimens. For patients with available data, the number of patients with a free concentration 4 times higher or lower than the observed MIC for the P. aeruginosa and E. coli was investigated.
Results
A one-compartment model with first-order elimination adequately described serum total and free meropenem concentrations. The only variable that significantly influenced the elimination constant of meropenem was the creatinine clearance (CLcr) calculated using the CKD-EPI formula. The highest probability of achieving the pharmacodynamic objective was with 3-h infusion dosage regimens. Sixty percent and 89% of patients attained a free drug concentration 4 times above the MIC for P. aeruginosa and E. coli respectively.
Conclusions
This study proposed different dosing regimens depending on renal clearance strata and the MIC of the germ targeted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inadequate use of antimicrobials is associated with a higher rate of therapeutic failure, increased toxicity and mortality, incremented costs and development of resistance [1]. Dosage in critically ill patients is complicated due to pathophysiologic changes that may alter the pharmacokinetics (PK) of antibiotics and therefore their efficacy [2]. Indeed, sepsis, polytrauma, acute renal failure, ascites and fluid drainage from the site of the infection are some of the factors that may explain fluctuations in meropenem serum concentrations in these patients [2]. Additionally, these physiological alterations cause complications when adjusting meropenem dosage based only on the patient’s creatinine levels.
Moreover, it is known that dosage regimens that have been applied to healthy volunteers or in vitro studies are not appropriate for critically ill patients [2].
Meropenem is a time-dependent antibiotic [3] and in many studies, its bactericidal activity has been associated with a free drug time more than 40% above the MIC (fT > MIC) [3, 4]. Other authors consider that, for specific diseases such as community-acquired pneumonia or respiratory tract infections, dosage regimens with fT > MIC around 100% are necessary [2, 4, 5]. Recently, it has been shown that in critically ill patients, the maximum efficacy criterion was associated with 100% fT > 4–5 MIC [6], meaning that free drug concentrations of 4 to 5 times more than the isolated organism’s MIC should be achieved.
Another factor that significantly influences the achievement of the PK/PD target is the duration of meropenem infusion. The principal advantage of a bolus dose or a short infusion is that an infusion pump is not necessary and that the stability of the carbapenem does not need to be taken into account, unlike with continuous infusions. Studies have compared the probability of obtaining the PK/PD target if the drug is administered by infusion over half an hour or over 3 h [6, 7].
The purpose of this study was to develop a non-parametric population pharmacokinetics model for free and total meropenem concentrations in critically ill patients and to compare different dosage regimens by simulation to attain the PK/PD target.
Methods
This retrospective, observational, single-centre study was conducted in the intensive care unit (ICU) between May 2011 and December 2017. Data used were anonymized at the time of collection, so no written consent of the patients collected, as authorized by French laws. Ethical approval for the study was obtained from the hospital’s research ethics committee. This study was accepted and approved by AEMPS as a post-authorization study (EPAOD). This study was conducted in accordance with the WMO declaration of Helsinki, ICH and GCP guidelines. The patients included in this study were aged over 18 years, admitted to ICU, treated with empirical or targeted therapy with meropenem, and had received at least 3 doses of meropenem prior to monitoring. All critically ill patients who had received renal replacement therapy were excluded. Meropenem dosage regimens prior to analysis were highly variable (1 g/6 h, 1 g/8 h, 1 g/12 h, 1 g/24 h) and were prescribed according to the literature, taking into account the site of infection and the patient’s renal function on the first days of meropenem treatment. All meropenem solutions were prepared in the hospital pharmacy using aseptic techniques in a horizontal laminar flow cabinet. Each IV mixture was prepared by diluting the corresponding quantity of meropenem in 0.9% NaCl to a volume of 50 ml per mixture.
Sample collection and storage
For the pharmacokinetic analysis, two serum samples were drawn from most of the patients (a peak sampled at the end of the infusion and a sample in the elimination phase) for quantification of the total and free meropenem concentrations. Free concentrations were available for some patients only after 2015 (when the free drug concentration measurement began) and analysed together with the total concentrations in the elimination phase to better adjust the meropenem dose. Samples were drawn between days 1 and 10 of treatment. Blood samples were collected in 5-mL glass test tubes without gel and centrifuged for 6 min at 6,000 RPM and a temperature of 18 °C to separate the serum as quickly as possible. Free concentrations were obtained from 1 mL of serum using Centrifree® ultrafiltration devices at a temperature of 37 °C. The total and free serum samples obtained were stored at a temperature between 2 and 8 °C if analysis was performed within 24 h, or an aliquot (1.5 mL Eppendorf) was frozen at − 30 °C until analysis in the case of delayed drug measurement.
HPLC technique
Serum meropenem concentrations were quantified by high-performance liquid chromatography (HPLC) using an Xbridge Shield® RP18 2.5 μm 4.6 × 75 mm column, an Xbridge Shield® RP18 2.5 μm precolumn and an Ostro 96-Well Plate® 25 mg 1/Pkg solid-phase extraction plate. The mobile phase was prepared with 6.8 g of potassium dihydrogen phosphate dissolved in 1 l of water and adjusted to a pH of 3.1 using phosphoric acid. The quantification range for the technique varies between 0.5 and 100 μg/mL of meropenem and the detection limit is 0.05 μg/mL. The specificity was 100% and there was a perfect linearity (r = 0.9995). Accuracy was 4.25%, 3.87% and 0.51% on the same day and 4.28%, 4.28% and 3.37% on different days, for control levels of 2.5, 25 and 75 mg/L respectively. Precision was 2.67%, 2.86% and 3.04% on the same day and 3.37%, 3.17% and 3.33% on different days, for the same control levels.
Data collection
The study variables obtained from the electronic medical records and pharmacokinetics sheets were anthropometric data (age, sex, height, real weight, BMI, ideal weight, body surface area), infectious diagnosis, acute and chronic kidney disease and hepatic failure or others comorbidities, clinical prediction tools such as the SOFA score (Sequential Organ Failure Assessment) and the SAPS 3 (Simplified Acute Physiology Score) on the first day of ICU, the worst SOFA score on admission, need for mechanical ventilation and intubation, use of vasopressors on the first day of ICU and evolution of clinical markers (procalcitonin, CRP, leucocytosis, analytical data (plasma creatinine, etc.), meropenem start date and dosage regimen, administration times, drawn serum samples times, days in ICU, intra-hospital mortality, mortality at 14 days after finishing treatment with meropenem and 30-day readmission. The main isolated germs were collected in blood, lung, abdominal and urinary tract cultures, and the MIC values were recorded in these samples. The E-test was the method used to determine the value of MIC.
Population pharmacokinetics model
A meropenem population pharmacokinetics analysis was performed using a non-parametric method in Pmetrics [8] software. The assay error polynomial equation was defined as SD = 0.25 + 0.05C for each output equation with a multiplicative coefficient for residual errors (gamma).
An initial analysis was conducted to estimate the parameters of the structural model: mono- and two-compartment models with first-order elimination were explored.
The selection of the best structural model was based on the Akaike information criterion (AIC) and Bayesian information criterion (BIC) (lowest values) and visual examination of the diagnostic plots (observed concentration vs. individual predicted concentrations, weighted residuals vs. time or individual predicted concentrations).
Demographic and clinical characteristics were used as covariates to assess their effect on the pharmacokinetic parameters of meropenem. Linear and power relationships were evaluated graphically (using a scatterplot) and covariates were retained if they decreased the AIC and BIC, the bias and RMSE (Root Mean Squared Error). The final model was evaluated using a visual predictive check. A total of 1,000 replicates of the original dataset were simulated using the final model to generate expected concentrations and the 90% prediction intervals. The observed data were overlaid on the prediction intervals and compared visually.
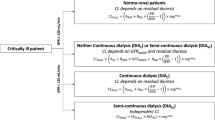
Monte Carlo simulation and probability of target attainment
The final pharmacokinetics model was used to perform semi-parametric Monte Carlo [9] simulations (n = 1000) in Pmetrics in order to determine the probability of PK/PD target attainment (PTA) 3 days after the start of treatment. Steady-state conditions were assumed whatever the dosage regimen was, given the short half-life of meropenem. The pharmacodynamic goal to achieve was 100% fT > 4MIC. The administration of 1 g/6 h, 1 g/8 h, 1 g/12 h, 1 g/16 h, 1 g/24 h and 500 mg/8 h with a 3-h infusion rate and 1 g/8 h and 1 g/12 h with a 30-min infusion rate was simulated. The probability was evaluated for 12 different MIC values (0.016, 0.032, 0.038, 0.094, 0.125, 0.25, 0.5, 0.75, 1, 2, 4, 8 μg/mL) isolated in clinical practice in ICU patients. Simulations were performed for different possible ranges of creatinine clearance: 8.3–29.9 mL/min, 30–59.5 mL/min, 59.6–89 mL/min, 89.5–140 mL/min. The dosage scheme simulated was considered as optimal if it achieved the objective for ≥ 85% of the simulated profiles.
Estimation of the fC0/4MIC value for observed MIC
The fC0/4*MIC was estimated for the 2 more prevalent germs isolated (Pseudomonas aeruginosa and Escherichia coli), according to the MIC values measured. A ratio lower than 1 is associated with a fC0 value < 4MIC (underdose) while a ratio > 1 is associated with a correct or overdose.
Results
One hundred and fifty-four total concentrations and 29 free concentrations sampled in 80 patients were used to build the model. The characteristics of these patients are described in Table 1. Samples were collected at approximately the peak time Tmax (mean[min-max] = 186[140–240] minutes after the beginning of the infusion) and in the elimination phase (217 [97–435] minutes after the first sample). A one-compartment model best describes the serum meropenem free and total concentrations in our population using 66 support points (supplemental Fig. 1; one-compartment model: BIC = 248.6, two-compartment model: BIC = 315.9). Two different values of gamma (1, 1.3) were investigated as a residual error and gamma = 1 was retained (BIC = 248.6 for gamma = 1 and 339.7 for gamma = 1.3).
The best relationship between unbound and total concentrations was described using a proportional relationship as follows:
CF = prop × CT; where CF is the free meropenem concentration, prop is a proportional term estimated individually and CT is the total meropenem concentration. The creatinine clearance (CLcr) estimated using the CKD-EPI formula [10] was the only covariate that significantly affected meropenem pharmacokinetics (BIC = 224.9). This covariate was integrated into the elimination constant (Ke), using a power association, where CLcr is weighted by the population median (4.975 L/h per 1.73 m2) as follows:
where Ke1 is the value for a patient having the median value of CLcr and Ke2 is the power term associated with CLcr.
The estimations of the population pharmacokinetics parameters are presented in Table 2. The observed concentration vs. individual-predicted concentrations and population-predicted concentrations of the final model for total and free meropenem concentrations are presented in Fig. 1. The weighted residuals vs. time or individual-predicted concentrations for total and free meropenem concentrations are presented in Fig. 2. The visual predictive check for the total and free concentrations are presented in Fig. 3 showing that the average prediction of the simulated data matched the observed concentration–time profiles and that the variability was reasonably accurately estimated. The probability of target attainment, 100% fT > 4 MIC for various meropenem dose regimens simulated for different ranges of creatinine clearance (Clcr): (A) 140–89.5 mL/min, (B) 89.4–59.6 mL/min, (C) 59.5–30 mL/min, (D) 29.9–8 mL/min, is represented in Fig. 4.
a Weighted residuals for free concentrations as a function of individual predicted free concentrations (mg/l). b Weighted residuals for total free concentration as a function of post-administration times (h). c Weighted residuals for total concentrations as a function of individual predicted total concentrations (mg/l). d Weighted residuals for total concentrations as a function of post-administration times (h)
Visual predictive checks obtained for 1,000 simulated patients from the final model for total (a) and free (b) meropenem concentrations. The lower line represents the 0.05 quantile, the intermediate line the median and the upper quartile line is the 0.95 quantile. Proportion of total and free concentrations between the 0.05 and the 0.95 quantiles were 0.916 (p = 0.102) and 0.893 (p = 0.756) respectively
Among the 80 patients, the lungs (33.60%), abdomen (21.31%) and blood (14.75%) were the main sites of infection. Forty-five percent (n = 36) of patients had a measured MIC value (median = 0.25 μg/mL [0.006–2]) and 72.2% (n = 26) of them attained the PK/PD target after 48 h of the initial infusion, considering that the steady state has been reached.
The most frequently isolated germs in our study were Pseudomonas aeruginosa (n = 15) with a median MIC of 1 (0.13–2) and Escherichia coli (n = 9) with a median MIC of 0.25 (0.06–2).
Sixty percent of patients (n = 9) with Pseudomonas aeruginosa infection attained the PK/PD target (free drug 4 times above the MIC) but with a median of 5.24 (range 1.31–39.81) times higher than the marked point, taking into account the isolated MIC values that we measured. For Escherichia coli, 92.86% of patients (n = 13) attained the PK/PD target with a mean 13.07 (1.95–30.25) times higher than the marked target (Fig. 5).
Discussion
The primary goal of this study was to develop a non-parametric pharmacokinetic model for meropenem, allowing us to describe the existing heterogeneity in the critically ill population. The secondary goal was to evaluate the ability of the intravenous meropenem dosage regimen adjusted for renal function to achieve free concentrations more than 4 times above the MIC of the organisms routinely present in the intensive care unit.
Eighty critically ill patients with one or 2 samples were included to develop our model, while the other published studies included only 12 [10], 34 [11] and 15 [12] patients, but with more than 5 samples each which is more accurate to describe the pharmacokinetics of a drug. These studies evaluated the suitability of the initial standard dosage regimen (1 g/8 h) in a critically ill population. However, in our study, the initial regimen was highly heterogeneous; the meropenem dosage was adjusted based on renal function at the beginning of treatment, a situation that is more representative of routine clinical practice. The median SOFA score in the study by Roberts et al. [13] is 3 in the intermittent infusion group and 5 in the continuous infusion group, which is very similar to our study, in which a median of 4 was observed in the patients. Seven patients included in the study had leukaemia as a comorbidity, a condition that affects creatinine clearance, which is generally higher than in the healthy population and can therefore affect the dosage of drugs excreted by the kidney. In these situations, the recommendation is to use extended infusion regimens. A dosage regimen of 0.5 g/4 h (3-h infusion) offers the best results as this allows the target to be achieved in 61.1% of subjects with an MIC of 1 and in 30.8% of those with an MIC of 2. In the latter case, it is recommended that doctors combine several antibiotics to increase the percentage of therapeutic success. Other PK-PD analyses for meropenem have been previously reported: for example, Kim et al. developed a popPK analysis in only 37 Korean patients with acute infections, and the patient demographic and genetic characteristics differ from those of European patients. On the opposite, our study includes patients with a larger panel of indications, some having acute infection and others being empirically treated with meropenem [14]. Usman et al. performed their study in elderly patients, while we have a mix between elderly and young patients (mean ± D age in our study was 63.26 ± 15.07 years) [15]. Finally, Minichmayr et al. developed a nomogram from a validated PKPOP model. In their study and similarly to our findings, the creatinine clearance was the only covariate that significantly affected the CL of meropenem. The difference was that their investigated theoretical PK/PD target was based on the EUCAST standard cut-off point. Therefore, their recommendations may tend to overdose patients, especially in case of low MIC [16]. Overall, the novelty of the current work is the measurement of free concentrations (PK/PD criteria are based on free concentrations) and real MIC in critically ill patients in routine practice in our hospital (as opposed to the EUCAST breakpoint) which allowed us to draw curves presenting the number of patients with 100 times > 4 times observed MIC.
There was huge variability in the estimated pharmacokinetic parameters. One possible explanation for this is the large number of physiological changes in critically ill patients due to diseases, mainly affecting the renal function. Pharmacokinetic studies of meropenem in critically ill patients showed elevated V and Cl values, with large inter-individual variability [13, 17, 18]. This high variability was also observed in our study, in which the mean V was 32.77 L with a 71.15% coefficient of variation for estimations using a non-parametric method needing reservation to interpret the mean and SD values. The variability in volume may be the result of changes in fluids and decreased fluid volume in the interstitial space [19]. This implies a limitation in our model, in which we observed a single compartment by having only 2 samples per patient and, therefore, we could consider the patient’s situation at any given moment. The ideal approach would be to have more repeated samples per patient at different times of the treatment and to observe the variation of distribution volume according to the clinical changes. Conversely, the Ke values obtained in the present study are similar to the findings of other clinical studies [11] that include two-compartment models. This large variability highlights the need to monitor meropenem levels in critically ill patients.
In terms of covariates, only creatinine clearance calculated by CKD-EPI formula exhibited an effect on Ke. This effect makes sense if we consider that for meropenem, approximately 70% (50–75%) of the dose is excreted unaltered in 12 h via the kidneys. No covariable significantly affecting the V was found. As expected, weight did not affect the V, as meropenem, like all beta-lactams, is primarily a hydrophilic compound. Approximately 30% of adipose tissues contain water, so the V of meropenem is not heavily affected by the amount of adipose tissue, as observed by Wittau et al. [20]. Finally, it is obvious that creatinine clearance is a composite covariate that includes the patient’s anthropometric data (weight, sex, creatinine), which when taken one by one may be non-significant.
The present article shows that 3-h infusion regimens are superior in their attainment of PK/PD objectives to 0.5-h infusions in the critically ill patients. In these cases, it would be necessary to rigorously monitor the ambient temperature. Indeed, it has been shown that the chemical and physical stability of a meropenem solution for intravenous injection is 3 h at 25 °C or 12 h at 2–8 °C. In our centre, meropenem preparations are dispensed to the ICU twice daily. They are stored in refrigerators (2–8 °C) and the administration is completed within the mixture’s stability interval. The stability of meropenem must be taken into account before incorporating these dosage regimens in practice.
In intensive care units, the isolation of the same germ repeatedly over a short period of time may contribute to inadequate empirical treatment of patients, thus leading to the development of resistance. In both EPIC studies and prevention programmes in intensive care areas, there is a predominance of Gram-negative organisms (55–65%), followed by Gram-positive organisms (25–35%) and yeasts (10–20%) [21,22,23]. The literature therefore reveals isolated organisms similar to those found in our study, in which we observed a prevalence of P. aeruginosa with a median MIC of 1 (0.13–2) and E. coli with a median MIC of 0.25 (0.06–2). These low MIC values are more susceptible to meropenem overdosing (up to 5.24 times for P. aeruginosa and 13.07 times for E. coli) as our study shows, probably without providing any extra benefit. This might lead to an increase in the occurrence of adverse effect and obviously to an increase in the cost of care, showing the importance of identifying the germ and performing therapeutic drug monitoring.
There is currently a tendency for studies to focus on the dosage of antibiotics in patients with very elevated MICs that approach the breaking point. However, the clinical reality is that most patients are on the other side. More studies are needed in these patients in order to decrease meropenem overdose and fight against resistance. In our hospital, up to 80% of isolated organisms have MICs of less than 0.5, which means that the 1 g/8 h regimen is not always appropriate.
In conclusion, for MIC = 2 mg/L (EUCAST breakpoint for P. aeruginosa or E. coli), no dosing scheme allows attaining the PK/PD objective for at least 85% of the simulations, even in patients with low renal function. However, in our population, 80% of isolated organisms have MICs of less than 0.5 which means that for patients with augmented or normal renal clearance (CLCR of 89.5 to 140 mL/min or 59.6 to 89.4 mL/min respectively), a dose of 1000 mg/6 h by IV infusion over 3 h is the best dosage regimen. However, even this regimen does not allow attaining the PK/PD objective in case of augmented renal clearance, and an association of synergistic antibiotics can be proposed. In patients with low renal function (CLCR < 59.5 mL/min), a dose of 1000 mg/8 h or 500 mg/8 h (< 30 mL/min) over 3 h allows attaining the PK/PD objectives.
References
Friedman ND, Temkin E, Carmeli Y (2016) The negative impact of antibiotic resistance. Clin Microbiol Infect 22:416–422
Roberts JA, Lipman J (2009) Pharmacokinetic issues for antibiotics in the critically ill patient. Crit Care Med 37:840–851 quiz 859
Nicolau DP (2008) Pharmacokinetic and pharmacodynamic properties of meropenem. Clin Infect Dis 47(Suppl 1):S32–S40
Perrott J, Mabasa VH, Ensom MHH (2010) Comparing outcomes of meropenem administration strategies based on pharmacokinetic and pharmacodynamic principles: a qualitative systematic review. Ann Pharmacother 44:557–564
Pea F, Viale P (2009) Bench-to-bedside review: appropriate antibiotic therapy in severe sepsis and septic shock--does the dose matter? Crit Care 13:214
Capitano B, Nicolau DP, Potoski BA, Byers KE, Horowitz M, Venkataramanan R, Paterson DL (2004) Meropenem administered as a prolonged infusion to treat serious gram-negative central nervous system infections. Pharmacotherapy 24:803–807
Roberts JA, Webb S, Paterson D, Ho KM, Lipman J (2009) A systematic review on clinical benefits of continuous administration of beta-lactam antibiotics. Crit Care Med 37:2071–2078
Neely MN, van Guilder MG, Yamada WM, Schumitzky A, Jelliffe RW (2012) Accurate detection of outliers and subpopulations with Pmetrics, a nonparametric and parametric pharmacometric modeling and simulation package for R. Ther Drug Monit 34:467–476
Goutelle S, Bourguignon L, Maire PH, Van Guilder M, Conte JE, Jelliffe RW (2009) Population modeling and Monte Carlo simulation study of the pharmacokinetics and antituberculosis pharmacodynamics of rifampin in lungs. Antimicrob Agents Chemother 53:2974–2981
Ramon-Lopez A, Allen JM, Thomson AH, Dheansa BS, James SE, Hanlon GW, Stewart B, Davies JG (2015) Dosing regimen of meropenem for adults with severe burns: a population pharmacokinetic study with Monte Carlo simulations. J Antimicrob Chemother 70:882–890
Mathew SK, Mathew BS, Neely MN, Naik GS, Prabha R, Jacob GG, K S, Fleming DH (2016) A nonparametric pharmacokinetic approach to determine the optimal dosing regimen for 30-minute and 3-hour meropenem infusions in critically ill patients. Ther Drug Monit 38:593–599
Goncalves-Pereira J, Silva NE, Mateus A, Pinho C, Povoa P (2014) Assessment of pharmacokinetic changes of meropenem during therapy in septic critically ill patients. BMC Pharmacol Toxicol 15:21
Roberts JA, Kirkpatrick CMJ, Roberts MS, Robertson TA, Dalley AJ, Lipman J (2009) Meropenem dosing in critically ill patients with sepsis and without renal dysfunction: intermittent bolus versus continuous administration? Monte Carlo dosing simulations and subcutaneous tissue distribution. J Antimicrob Chemother 64:142–150
Kim YK, Lee D-H, Jeon J, Jang H-J, Kim H-K, Jin K, Lim SN, Lee SS, Park BS, Kim YW, Shin JG, Kiem S (2018) Population pharmacokinetic analysis of meropenem after intravenous infusion in Korean patients with acute infections. Clin Ther 40:1384–1395
Usman M, Frey OR, Hempel G (2017) Population pharmacokinetics of meropenem in elderly patients: dosing simulations based on renal function. Eur J Clin Pharmacol 73:333–342
Minichmayr IK, Roberts JA, Frey OR, Roehr AC, Kloft C, Brinkmann A (2018) Development of a dosing nomogram for continuous-infusion meropenem in critically ill patients based on a validated population pharmacokinetic model. J Antimicrob Chemother 73:1330–1339
Jaruratanasirikul S, Sriwiriyajan S, Punyo J (2005) Comparison of the pharmacodynamics of meropenem in patients with ventilator-associated pneumonia following administration by 3-hour infusion or bolus injection. Antimicrob Agents Chemother 49:1337–1339
de Stoppelaar F, Stolk L, van Tiel F, Beysens A, van der Geest S, de Leeuw P (2000) Meropenem pharmacokinetics and pharmacodynamics in patients with ventilator-associated pneumonia. J Antimicrob Chemother 46:150–151
Nduka OO, Parrillo JE (2009) The pathophysiology of septic shock. Crit Care Clin 25:677–702 vii
Wittau M, Scheele J, Kurlbaum M, Brockschmidt C, Wolf AM, Hemper E, Henne-Bruns D, Bulitta JB (2015) Population pharmacokinetics and target attainment of meropenem in plasma and tissue of morbidly obese patients after laparoscopic intraperitoneal surgery. Antimicrob Agents Chemother 59:6241–6247
Olaechea PM, Insausti J, Blanco A, Luque P (2010) Epidemiology and impact of nosocomial infections. Med Int 34:256–267
Vincent JL, Bihari DJ, Suter PM, Bruining HA, White J, Nicolas-Chanoin MH et al (1995) The prevalence of nosocomial infection in intensive care units in Europe. Results of the European prevalence of infection in intensive care (EPIC) study. EPIC international advisory committee. JAMA 274:639–644
Mertens K, Morales I, Catry B (2013) Infections acquired in intensive care units: results of national surveillance in Belgium, 1997-2010. J Hosp Infect 84:120–125
Acknowledgements
We are grateful to K. Poole for manuscript editing.
Funding
The project was supported by FBCN (Fundación Bancaria Caja Navarra) through a “mobility grant for Ph.D. research studies” for Ana Isabel Idoate Grijalba.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
What is already known about this subject (up to three bullet points)
• Meropenem is a time-dependent antibiotic and its bactericidal activity is associated with free concentration (%T > 4 MIC).
• Dosage regimens that have been applied to healthy volunteers or in vitro studies are not appropriate for critically ill patients due to their pathophysiologic changes.
What this study adds
• Dosage regimens recommended in the literature (1 g/6 h, 1 g/8 h) are not always suitable for real-world critically ill populations.
• 60% and 89% of patients attained free drug concentrations 4 times above the MIC for P. aeruginosa and E. coli respectively
• Dosing regimens depending on renal clearance strata and the MIC of the germ targeted are proposed.
Electronic supplementary material
ESM 1
(PNG 376 kb)
Rights and permissions
About this article
Cite this article
Idoate Grijalba, A.I., Aldaz Pastor, A., Marquet, P. et al. Evaluation of a non-parametric modelling for meropenem in critically ill patients using Monte Carlo simulation. Eur J Clin Pharmacol 75, 1405–1414 (2019). https://doi.org/10.1007/s00228-019-02716-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-019-02716-y