Abstract
Purpose
To examine the association between antihypertensive medication (AHTM) implementation adherence and healthcare utilisation in community-dwelling adults aged ≥ 50 years in Ireland.
Methods
This was a prospective cohort study. The Irish Longitudinal Study on Ageing (TILDA) was linked to pharmacy claims data for participants aged ≥ 50 years. Participants were included if they had ≥ 3 pharmacy claims for one or more AHTM (ATC codes ‘C02’, ‘C03’, ‘C07’, ‘C08’ or ‘C09’) within the year preceding the year of self-reported healthcare utilisation outcome occurrence. Outcomes included self-reported general practitioner (GP), emergency department (ED), outpatient department visits and hospital admissions. Implementation adherence was measured using proportion of days covered (PDC), with participants classified as adherent if the average PDC ≥ 0.8. Negative binomial models were used to analyse the association between AHTM adherence and number of GP, ED, outpatient visits and hospitalisations (adjusted IRR and 95% CI are presented).
Results
One thousand four hundred thirty-one participants were included. The majority of participants (72.6%) were considered adherent. Good implementation adherence to AHTM was associated with a significant decrease in self-reported GP visits (adjusted IRR 0.91, 95% CI 0.83–0.99). Adherence had no significant impact on the number of ED visits, outpatient visits or hospitalisations reported by TILDA participants.
Conclusions
Good adherence to AHTM was associated with less self-reported GP visits in this population, suggesting improved overall health status. However, the impact of medication non-adherence on the other self-reported healthcare utilisation outcomes (ED, outpatient visits and hospitalisations) was not evident in this study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The ABC taxonomy defines adherence to medicines as a process whereby patients take their medication as prescribed and consists of three core components: initiation, implementation and discontinuation [1]. Initiation refers to the patient taking the first dose as prescribed; implementation describes the fidelity the patient exhibits to the agreed therapeutic regimen, and discontinuation refers to when a patient stops taking their medicine [1].
Medication adherence ranges from 47 to 100% in older populations [2]. Medication non-adherence may represent a greater risk in older people, due to increasing drug burden and comorbidities [3, 4] resulting in poorer health outcomes for this cohort [4, 5]. Medication non-adherence in older populations is multi-faceted, compounded by a combination of drug-related factors such as dosing regimen, side effects and polypharmacy, patient-related factors such as cognitive function, health literacy and multi-morbidity, and the patient-physician relationship [6].
Non-adherence to antihypertensive medication (AHTM) is common, with some studies suggesting as many as 45% of patients are non-adherent [7], possibly due to the asymptomatic nature of the condition [4] and leading to an increased risk of uncontrolled blood pressure [7,8,9]. Hypertension is considered the strongest modifier of cardiovascular disease risk, with intensive treatment demonstrating superior benefit to standard antihypertensive therapy in adults aged ≥ 75 years [10]. Previous observational database studies have reported the association between AHTM non-adherence and cardiovascular outcomes such as stroke [11,12,13,14], congestive heart failure [13, 15], acute myocardial infarction [11, 12], cerebrovascular diseases [16] and all-cause mortality [11]. All studies reported an inverse relationship between good AHTM adherence and the risk of cardiovascular endpoints [11,12,13,14,15,16]. Studies conducted in the USA have demonstrated a significant relationship between cardiovascular medication adherence and all-cause hospitalisation [17, 18] and emergency department visits [18,19,20], with variability emerging when analysing therapeutic classes separately [17, 18]. There is limited evidence on the association between AHTM adherence and healthcare utilisation in middle and older aged adults within a European setting. There is uncertainty over the threshold for AHTM adherence required to achieve therapeutic success, with most studies opting for an arbitrary cutoff of 80% [21].
The aims of this study are to establish:
-
(i)
the level of AHTM implementation adherence measured using pharmacy refill claims data,
-
(ii)
the association between AHTM implementation adherence and healthcare utilisation outcomes and
-
(iii)
the impact altering the implementation adherence threshold has on the association between implementation adherence and healthcare utilisation outcomes
in community-dwelling adults aged ≥ 50 years in Ireland, who received medications as part of a state-subsidised scheme across a 12-month period.
Methods
Study design
This was a prospective cohort study using linked data from a national pharmacy claims database, the Health Service Executive-Primary Care Reimbursement Service (HSE-PCRS) and the first wave of The Irish Longitudinal study on Ageing (TILDA) [22, 23].
TILDA is a nationally representative cohort of Irish community-dwelling individuals aged ≥ 50 years and records information relating to the health, economic and social circumstances of this cohort as they progress through the ageing process. The first wave of data collection began in October 2009 through to February 2011, resulting in a sample size of 8504 (participants and proxies). There were 8176 participants aged ≥ 50 years. The sampling framework is described in detail elsewhere [22]. Participants complete a computer-aided personal interview (CAPI) as part of the study.
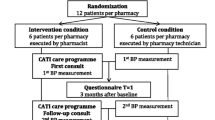
The study population included adults aged ≥ 50 years (at time of CAPI), who had participated in wave 1 of TILDA and have a general medical services (GMS) card. Data regarding prescription dispensing claims from GMS patients is collected from the (HSE-PCRS) [24]. The HSE-PCRS GMS scheme provides free health services and prescribed medications to eligible persons in Ireland. At the time of prescription data collection, there was no medication co-payment associated with the scheme. Eligibility of the GMS scheme is based on income-related means-testing, with the exception of those aged ≥ 70 years, who were automatically eligible for the scheme until January 2009 [24]. Eligible participants were those who received ≥ 3 pharmacy claims for an AHTM within the 12 months preceding the time period referred to in the CAPI interview in wave 1 were included (see Fig. 1) in the study. AHTM were identified from the World Health Organization Anatomical Therapeutic Chemical (ATC) codes, as those with second level codes C02 (anti-hypertensives), C03 (diuretics), C07 (beta blockers), C08 (calcium channel blockers) and C09 (agents acting on the renin-angiotensin system), in line with previous studies [11]. Participants were both incident and prevalent users of AHTM.
The EMERGE (ESPACOMP Medication Adherence Reporting Guideline) guideline was followed in the reporting of this study [25].
Exposure variables
Implementation adherence to AHTM was calculated using the proportion of days covered (PDC), which has been validated for providing accurate estimates of adherence using administrative claims databases [26]. The PDC represents the sum of days’ supply of each prescription refill, divided by the days in the observation period, taking into consideration overlapping supplies.
Implementation adherence was measured as a dichotomous variable. A patient with a PDC value ≥ 0.8 was considered adherent, which is the conventionally used cutoff for adherence [27]. If patients had been taking more than one class of AHTM during the study period, the PDC used was an average of all values across the different classes.
Implementation adherence was calculated for the year preceding the time period (12 months) for which the respondent is referring to in the CAPI, as per the methodology used in a previous study (see Fig. 1). [28]
Outcome variables
The main outcome(s) was self-reported healthcare utilisation in the 12 months prior to the date of participants CAPI interview including:
-
1.
General practitioner (GP) visits
-
2.
Emergency department (ED) visits
-
3.
Outpatient department visits
-
4.
Number of occasions admitted to hospital overnight (hospitalisations)
The responses were reported on a continuous scale (up to a maximum 200 for GP, ED and outpatient visits and up to a maximum of 50 for hospitalisations). Dichotomous variables were generated for each healthcare utilisation outcome e.g. one or more GP visits, ED visits, outpatient visits or hospitalisations based on the distribution of the data, respectively, in the year prior to the CAPI interview (see Fig. 1).
Covariates
Sociodemographic and clinical covariates identified as influencing both medication adherence and healthcare utilisation were identified from the literature [4]. Covariates included (i) age group, (ii) gender, (iii) polypharmacy (≥ 5 medications), (iv) level of educational attainment, (v) memory score, (vi) functional disability, (vii) depressive symptoms and (viii) social support. Covariates were based on responses in the CAPI.
Data analysis
Descriptive statistics including means, medians and variance were calculated for implementation adherence, healthcare utilisation outcomes and covariates. Comparisons between adherent or non-adherent participants for categorical covariates were analysed using chi-squared tests, and Wilcoxon rank sum tests were used for continuous covariates.
Regression models were used to calculate the unadjusted and adjusted association between adherence and healthcare utilisation, including both dichotomous (logistic regression) and count outcomes (negative binomial). For count outcomes with an excessive number of zeros, standard negative binomial regression models and zero inflation negative binomial models were constructed and model fit was compared using the Vuong test [29] and criteria for assessing goodness to fit (AIC and BIC).
Sensitivity analyses were conducted by altering the PDC cutoff for adherence to PDC ≥ 0.7 and PDC ≥ 0.9, respectively, to analyse the impact of different adherence levels on healthcare utilisation outcomes. Analyses were performed using SAS version 9.4 (SAS Institute, Inc., Cary, NC).
Results
Eight thousand one hundred seventy-six participants aged ≥ 50 years were identified from wave 1 of TILDA. Three thousand one hundred seventy-six participants had consented to have their GMS pharmacy claims data linked to their TILDA data, and 1431 (45%) participants had received ≥ 3 pharmacy claims for an antihypertensive medication within the previous 12 months. Over half of participants were women (55%). The average age of participants was 72 years, and 45% of participants were aged ≥ 75 years. The average PDC was 0.84 (SD 0.21), and 73% had a PDC ≥ 0.80 (adherent). There was no significant gender difference in whether participants were considered adherent or non-adherent. However, there was a significant age difference, with a higher proportion of those aged ≥ 75 years considered adherent, compared with the younger cohorts (see Table 1).
Outcome data
Table 2 presents the univariate (unadjusted) and multivariate (adjusted) incident rate ratios (IRR) and 95% confidence intervals for the association between implementation adherence (PDC ≥ 0.80) and healthcare utilisation. Supplementary Table 1 presents the results of logistic regression models (odds ratios and 95% CI).
General practitioner visits
Ninety-eight percent of participants reported visiting the GP at least once in the 12 months subsequent to adherence measurement (n = 1404). The mean number of GP visits reported for the previous 12 months was 4 (SD 6.58).
A negative binomial regression analysis demonstrated that adherence was associated with a significant decrease in the number of GP visits in the following year (9% versus non-adherence). This relationship remained significant after adjustment for covariates. Participants who reported being on ≥ 5 medications had significantly more GP visits in comparison to those who were on fewer medications, as did those who reported having a functional disability or depression. Being older, female and living with others was associated with fewer GP visits.
Emergency department visits
One thousand four hundred twenty-eight participants reported the number of ED visits they had in the year preceding the CAPI. Twenty percent of participants reported having ≥ 1 ED visit.
A zero inflation negative binomial regression model showed that adherence was not significantly associated with the number of ED visits, either in the unadjusted or adjusted analysis (Table 2). Participants aged ≥ 75 years had significantly fewer ED visits than participants aged 50–64 years in adjusted analysis. Adherence was not significantly associated the liklihood of having an ED visit or not (Supplementary Table 1).
Outpatient visits
One thousand four hundred twenty-eight participants reported the number of outpatient visits they had in the year preceding CAPI measurement. Fifty-four percent of participants reported having one or more outpatient visits. Adherence to AHTM was not a significant predictor of the number of outpatient visits, (Table 2) but was significantly associated with a reduced likelihood of experiencing an outpatient visit or not, in comparison to non-adherence (Supplementary Table 1).
Polypharmacy, higher level of education and functional disability were significant independent predictors of a higher rate of outpatient visits.
Hospitalisations
One thousand four hundred thirty participants responded to the CAPI question regarding the number of hospital overnight admissions they had experienced in the past year. Twenty percent of participants reported having at least one hospitalisation in the past year.
Implementation adherence to AHTM was not significantly associated with the number of hospital admissions (Table 2). Being on more than 5 medications, having a higher level of education, having a functional disability and subclinical depression were all significantly associated with a greater number of hospitalisations. Implementation adherence was not significantly associated with the risk of having a hospital admission, either in the univariate or adjusted logistic model (Supplementary Table 1).
Sensitivity analyses
Adherence (PDC ≥ 0.7)
Similar to the traditional cutoff point, having a PDC ≥ 0.7 was not significantly associated with either the number of ED visits or the likelihood of having an ED visit (Supplementary Table 2). Implementation adherence (PDC ≥ 0.7) was associated with a similar rate of GP visits as the standardised PDC ≥ 0.80 cutoff point (Supplementary Table 3). Adherence was associated with a significantly lower likelihood of experiencing ≥ 1 outpatient visit (adjusted OR 0.63, 0.47–0.85), but not with the number of outpatient visits reported. Having a PDC ≥ 0.70 was also significantly associated with a lower risk of hospitalisation (adjusted OR 0.65, 95% CI 0.47–0.91) and less overnight admissions (adjusted IRR 0.64, 95% CI 0.45–0.91).
Adherence (PDC ≥ 0.9)
Adherence was not significantly associated with the number of ED visits experienced or the likelihood of experiencing ≥ 1 ED admission when set at PDC ≥ 0.90 (Supplementary Table 4). Adherence at the higher cutoff of PDC ≥ 0.90 was associated with a slightly lower rate of GP visits than the standardised cutoff (Supplementary Table 5). No significant relationship was observed between either the likelihood of experiencing an outpatient visit or the number of outpatient visits reported. Adherence at PDC ≥ 0.9 was not significantly associated with of a lower risk of hospitalisation or number of admissions.
Discussion
Implementation adherence to AHTM was high at 73% in this community-based population aged ≥ 50 years and was found to be associated with fewer GP visits and less likelihood of having an outpatient visit. Implementation AHTM adherence (PDC ≥ 0.8) was not significantly associated with a lower number of ED visits or hospitalisations in this cohort.
This study estimates that over a quarter of middle and older aged adults who received AHTM as part of a state-subsidised scheme are non-adherent to their AHTM. This is similar to previous analyses using pharmacy refill claims data [28, 31] and self-report questionnaires [32]. The older sub-population in our study showed higher levels of adherence in comparison to participants’ ≤ 65 years, in concordance with previous literature [28].
Adherence to AHTM was associated with less GP visits, which may be indicative of better health status [33]. In this population, all participants had access to free GP care; therefore cost barriers do not explain a reduced number of visits reported. Many participants were prevalent, chronic users, and their adherence estimate are likely to be an indicator of long-term adherence, contributing to this protective effect. The results are similar to a recent study of AHTM adherence in Irish adults aged ≥ 65 years recruited from community pharmacies, although only 70% of the cohort were GMS eligible [34]. In Ireland, GPs are reimbursed at a capitation rate per GMS patient treated and not paid per patient consultation [35]. Thus, it is not possible to estimate the direct cost of an increase in GP visits to the Irish healthcare payer. However, the burden on GP resource use (i.e increased workload, waiting times) and indirect costs to the healthcare payer should be considered.
Implementation adherence did not significantly influence the number of ED visits reported or the likelihood of experiencing an ED visit in this cohort. This is in contrast to smaller studies in socio-economically disadvantaged cohorts in the USA that documented a significant inverse association between chronic heart failure (CHF) medication adherence and ED visit rate [18,19,20]. Similar findings were reported in a large scale administrative database study in the USA; non-adherent hypertensive adults had more ED visits, and the rate of ED visits increased with the extent of non-adherence [36]. In general, the literature detailing the relationship between medication non-adherence and ED visits is mixed. A study of high-risk COPD patients found that those who were adherent were more likely to have an ED visit, but non-adherent were more likely to have higher ICU use and healthcare costs [37]. The authors postulated that adherent patients may exhibit more health-seeking behaviours and thus attending the ED even when symptoms are mild or manageable.
There is a deficit in the literature in relation to the association between AHTM adherence and outpatient visits or use of ancillary care services. In contrast to the results obtained in this analysis, a previous study showed that non-adherence (MPR < 0.80) was associated with a significantly reduced risk of both generic and osteoporosis-related outpatient service utilisation in women aged ≥ 55 years [38]. This may signal the presence of the “healthy adherer” bias referred to previously [39]. However, a study of anti-epileptic medication adherence in adults aged ≥ 65 years did not find a statistically significant association between non-adherence (MPR < 0.80) and both the risk and number of ancillary care visits [40].
With regard to hospitalisation, previous evidence has suggested that sub-optimal adherence to β blockers and calcium channel blockers in adults aged ≥ 66 years predicts an increase in the likelihood of all-cause readmissions, respectively [17]. Participants in this study were using these medications for secondary prevention of cardiovascular events, whereas in the current study, there was no distinction between primary or secondary prevention. Adherence in secondary prevention may be more influential on health outcomes and healthcare utilisation. A statistically significant increase in hospitalisation rate was associated with a 10% increase in AHTM adherence measured using PDC in a study of older Irish community pharmacy patients [34]. However, covariates such as functional disability and depression, found to be significantly associated with hospitalisation rate in the current analysis, were not adjusted for.
Cohort studies in the USA have found that poor adherence to AHTM was significantly associated with an increased risk of cardiovascular-related healthcare utilisation and costs in patients [13, 28]. A Korean study found that poor, but not intermediate adherence to AHTM, measured using cumulative medication adherence was associated with an increased risk of the first hospitalisation for CVD in new users of AHTM [31].
There are several strengths to this study. Firstly, there is little evidence in the literature on the impact of suboptimal implementation of AHTM on healthcare utilisation. AHTM adherence was calculated using a large nationally representative sample of middle and older aged Irish people, and its association with self-reported healthcare utilisation was reported. Our findings provide useful information to researchers conducting economic evaluations of adherence interventions in community settings.
In addition, the sensitivity of the arbitrary adherence threshold of 80% was tested in this study. We found that lowering this adherence threshold to 70% resulted in a significant reduction in hospitalisation risk and the rate of hospitalisations reported for those who were considered adherent.
We separated the adherence exposure period from the outcome measurement period, therefore minimising the risk of contamination bias. Previous studies have assessed the impact of medication adherence on healthcare utilisations using cross-sectional designs. Of course, by using observational methods, one cannot conclude that non-adherence was the causal factor in healthcare utilisation if a significant association is observed. However, by having the correct temporality one can be more confident in the direction of the relationship.
This study has several potential limitations. Firstly, the study population only includes participants who are eligible to receive medications and healthcare as part of a state-subsided scheme, and so may include a more socially disadvantaged population in those aged 50–69 years. However, 69% of the study cohort was aged ≥ 70 years. The HSE-PCRS scheme is representative of 90% of this population [24]. Education level was used as a proxy variable for socioeconomic status and was controlled for in the multivariate analysis.
Secondly, using pharmacy claims data is an indirect method of measuring adherence as dispensation data reflects medication availability as opposed to true exposure. However, it is considered objective, inexpensive, and not subject to the same degree of recall bias as self-reported methods and cost as Medication Event Monitoring Systems (MEMs) [21]. Studies have indicated that information regarding medication use from the pharmacy claims database is more accurate in comparison to other methods [41].
Thirdly, information on participants’ healthcare utilisation in the year preceding medication adherence measurement was not available and could not be accounted for in multivariate analyses. Self-reported outcome measurement was used in this study, which may be subject to recall bias. However, a recent Irish study using TILDA data has shown good reliability between self-reported and electronically measured GP and outpatient visits, but not for ED visits [42]. Future research will document the change in adherence from wave 1 of TILDA to subsequent waves, accounting for baseline self-reported healthcare utilisation.
While we adjusted for a number of covariates in the analysis, there may be unmeasured confounding due to lack of control for illness severity, psychosocial variables such as self-efficacy and health-seeking behaviours (healthy adherer bias). However, including engagement with preventative healthcare screening services in post hoc sensitivity analyses did not significantly alter the results.
Finally, the reasons for the healthcare utilisation episode remain unknown and whether it was cardiovascular-related. Availability of clinical notes would facilitate judgement of this, but the lack of an integrated electronic healthcare record in Ireland prevents the availability of this information.
Implications for future research
Further population studies, using a combination of adherence measures and disease-specific outcome measures should be conducted to establish the association between non-adherence and healthcare utilisation. Studies should test the validity of the arbitrary 80% adherence threshold across different therapeutic areas, as we have shown that different thresholds may significantly impact association estimates. Consideration should be given to the temporality of medication adherence measurement with respect to health outcome measurement. Finally, over half of the population in this sample of middle and older aged adults were using ≥ 5 medications, indicating the presence of multi-morbidity. Future research should endeavour to estimate adherence to all chronic medications in people with multi-morbidity and establish the association with healthcare utilisation outcomes.
Conclusion
Irish adults in receipt of state-subsidised healthcare, who are adherent to their antihypertensive medication, report visiting their GP less frequently and are less likely to visit outpatient departments than those who are non-adherent. Having good adherence may represent overall improved health status for the patient and decreased resource burden on the physician. However, no significant relationship was evident between implementation adherence and tertiary healthcare utilisation in this population, which may be due to the lack of specificity for disease-specific healthcare events.
Data availability
The data that support the findings of this study are available from TILDA and the HSE-PCRS but restrictions apply to the availability of these datasets, which were used under license for the current study, and so are not publicly available. Researchers interested in using TILDA data may access the anonymised dataset for free from the following sites: Irish Social Science Data Archive (ISSDA) at University College Dublin http://www.ucd.ie/issda/data/tilda/; Interuniversity Consortium for Political and Social Research (ICPSR) at the University of Michigan http://www.icpsr.umich.edu/icpsrweb/ICPSR/studies/34315.
References
Vrijens B, De Geest S, Hughes DA, Przemyslaw K, Demonceau J, Ruppar T, Dobbels F, Fargher E, Morrison V, Lewek P, Matyjaszczyk M, Mshelia C, Clyne W, Aronson JK, Urquhart J, for the ABCPT (2012) A new taxonomy for describing and defining adherence to medications. Br J Clin Pharmacol 73(5):691–705. https://doi.org/10.1111/j.1365-2125.2012.04167.x
Vik SA, Maxwell CJ, Hogan DB (2004) Measurement, correlates, and health outcomes of medication adherence among seniors. Ann Pharmacother 38(2):303–312. https://doi.org/10.1345/aph.1D252
Bjerrum L, Søgaard J, Hallas J, Kragstrup J (1998) Polypharmacy: correlations with sex, age and drug regimenA prescription database study. Eur J Clin Pharmacol 54(3):197–202. https://doi.org/10.1007/s002280050445
Hughes CM (2004) Medication non-adherence in the elderly: how big is the problem? Drugs Aging 21(12):793–811. https://doi.org/10.2165/00002512-200421120-00004
Vik SA, Hogan DB, Patten SB, Johnson JA, Romonko-Slack L, Maxwell CJ (2006) Medication nonadherence and subsequent risk of hospitalisation and mortality among older adults. Drugs Aging 23(4):345–356. https://doi.org/10.2165/00002512-200623040-00007
Gellad WF, Grenard JL, Marcum ZA (2011) A systematic review of barriers to medication adherence in the elderly: looking beyond cost and regimen complexity. Am J Geriatr Pharmacother 9(1):11–23. https://doi.org/10.1016/j.amjopharm.2011.02.004
Abegaz TM, Shehab A, Gebreyohannes EA, Bhagavathula AS, Elnour AA (2017) Nonadherence to antihypertensive drugs: a systematic review and meta-analysis. Medicine 96(4):e5641. https://doi.org/10.1097/md.0000000000005641
Chobanian AV (2009) Impact of nonadherence to antihypertensive therapy. Circulation 120:1558–1560. https://doi.org/10.1161/CIRCULATIONAHA.109.906164
Oliveira-Filho AD, Barreto-Filho JA, Neves SJ, Lyra Junior DP (2012) Association between the 8-item Morisky medication adherence scale (MMAS-8) and blood pressure control. Arq Bras Cardiol 99(1):649–658 https://doi.org/10.1590/S0066-782X2012005000053
Williamson JD, Supiano MA, Applegate WB, Berlowitz DR, Campbell RC, Chertow GM, Fine LJ, Haley WE, Hawfield AT, Ix JH, Kitzman DW, Kostis JB, Krousel-Wood MA, Launer LJ, Oparil S, Rodriguez CJ, Roumie CL, Shorr RI, Sink KM, Wadley VG, Whelton PK, Whittle J, Woolard NF, Wright JT Jr, Pajewski NM, for the SPRINT Research Group (2016) Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years: a randomized clinical trial. JAMA 315(24):2673–2682. https://doi.org/10.1001/jama.2016.7050
Degli Esposti L, Saragoni S, Benemei S, Batacchi P, Geppetti P, Di Bari M, Marchionni N, Sturani A, Buda S, Degli Esposti E (2011) Adherence to antihypertensive medications and health outcomes among newly treated hypertensive patients. Clinicoecon Outcomes Res 3:47–54. https://doi.org/10.2147/ceor.s15619
Mazzaglia G, Ambrosioni E, Alacqua M, Filippi A, Sessa E, Immordino V, Borghi C, Brignoli O, Caputi AP, Cricelli C, Mantovani LG (2009) Adherence to antihypertensive medications and cardiovascular morbidity among newly diagnosed hypertensive patients. Circulation 120(16):1598–1605. https://doi.org/10.1161/circulationaha.108.830299
Yang Q, Chang A, Ritchey MD, Loustalot F (2017) Antihypertensive medication adherence and risk of cardiovascular disease among older adults: a population-based cohort study. J Am Heart Assoc 6(6). https://doi.org/10.1161/jaha.117.006056
Perreault S, Yu AY, Cote R, Dragomir A, White-Guay B, Dumas S (2012) Adherence to antihypertensive agents after ischemic stroke and risk of cardiovascular outcomes. Neurology 79(20):2037–2043. https://doi.org/10.1212/WNL.0b013e3182749e56
Corrao G, Rea F, Ghirardi A, Soranna D, Merlino L, Mancia G (2015) Adherence with antihypertensive drug therapy and the risk of heart failure in clinical practice. Hypertension 66(4):742–749. https://doi.org/10.1161/hypertensionaha.115.05463
Kettani FZ, Dragomir A, Cote R, Roy L, Berard A, Blais L, Lalonde L, Moreau P, Perreault S (2009) Impact of a better adherence to antihypertensive agents on cerebrovascular disease for primary prevention. Stroke 40(1):213–220. https://doi.org/10.1161/strokeaha.108.522193
Rasmussen JN, Chong A, Alter DA (2007) Relationship between adherence to evidence-based pharmacotherapy and long-term mortality after acute myocardial infarction. JAMA 297(2):177–186. https://doi.org/10.1001/jama.297.2.177
Tu W, Morris AB, Li J, Wu J, Young J, Brater DC, Murray MD (2005) Association between adherence measurements of metoprolol and health care utilization in older patients with heart failure. Clin Pharmacol Ther 77(3):189–201. https://doi.org/10.1016/j.clpt.2004.10.004
Hope CJ, Wu J, Tu W, Young J, Murray MD (2004) Association of medication adherence, knowledge, and skills with emergency department visits by adults 50 years or older with congestive heart failure. Am J Health-Syst Pharm 61(19):2043–2049. https://doi.org/10.1093/ajhp/61.19.2043
Murray M, Tu W, Wu J, Morrow D, Smith F, Brater D (2009) Factors associated with exacerbation of heart failure include treatment adherence and health literacy skills. Clin Pharmacol Ther 85(6):651–658. https://doi.org/10.1038/clpt.2009.7
Osterberg L, Blaschke T (2005) Adherence to medication. N Engl J Med 353(5):487–497. https://doi.org/10.1056/NEJMra050100
Kenny RA, Whelan BJ, Cronin H, Kamiya Y, Kearney P, O’Regan C, Ziegel M (2010) The design of the Irish longitudinal study on ageing. Lenus the Irish Health Repository. https://www.lenus.ie/bitstream/handle/10147/301640/DesignReport2010.pdf;jsessionid=90014F67AA07262980411 E22BE26C4E3889?sequence=1. Accessed 10th October 2018
Barrett A, Burke H, Cronin H, Hickey A, Kamiya Y, Kenny RA, Layte R, Maty S, McGee H, Morgan K (2011) Fifty plus in Ireland 2011: first results from the Irish Longitudinal Study on Ageing (TILDA). Lenus the Irish Health Repository . https://www.lenus.ie/handle/10147/129741. Accessed 10th October 2018
Sinnott S-J, Bennett K, Cahir C (2017) Pharmacoepidemiology resources in Ireland—an introduction to pharmacy claims data. Eur J Clin Pharmacol 73(11):1449–1455. https://doi.org/10.1007/s00228-017-2358-4
De Geest S, Zullig LL, Dunbar-Jacob J, Helmy R, Hughes DA, Wilson IB, Vrijens B (2018) ESPACOMP medication adherence reporting guideline (EMERGE). Ann Intern Med 169(1):30–35. https://doi.org/10.7326/m18-0543
Karve S, Cleves MA, Helm M, Hudson TJ, West DS, Martin BC (2008) An empirical basis for standardizing adherence measures derived from administrative claims data among diabetic patients. Med Care 46(11):1125–1133. https://doi.org/10.1097/MLR.0b013e31817924d2
Andrade SE, Kahler KH, Frech F, Chan KA (2006) Methods for evaluation of medication adherence and persistence using automated databases. Pharmacoepidemiol Drug Saf 15(8):565–574; discussion 575-567. https://doi.org/10.1002/pds.1230
Pittman DG, Tao Z, Chen W, Stettin GD (2010) Antihypertensive medication adherence and subsequent healthcare utilization and costs. Am J Manag Care 16(8):568–576
Vuong QH (1989) Likelihood ratio tests for model selection and non-nested hypotheses. Econometrica 57(2):307–333
Radloff LS (1977) The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1(3):385–401
Kim S, Shin DW, Yun JM, Hwang Y, Park SK, Ko YJ, Cho B (2016) Medication adherence and the risk of cardiovascular mortality and hospitalization among patients with newly prescribed antihypertensive medications. Hypertension 67(3):506–512. https://doi.org/10.1161/hypertensionaha.115.06731
Haley WE, Gilbert ON, Riley RF, Newman JC, Roumie CL, Whittle J, Kronish IM, Tamariz L, Wiggers A, Morisky DE, Conroy MB, Kovalik E, Kressin NR, Muntner P, Goff DC (2016) The association between self-reported medication adherence scores and systolic blood pressure control: a SPRINT baseline data study. J Am Soc Hypertens 10(11):857–864.e852. https://doi.org/10.1016/j.jash.2016.08.009
Little P, Somerville J, Williamson I, Warner G, Moore M, Wiles R, George S, Smith A, Peveler R (2001) Psychosocial, lifestyle, and health status variables in predicting high attendance among adults. Br J Gen Pract 51(473):987–994
Dillon P, Smith SM, Gallagher P, Cousins G (2019) The association between pharmacy refill-adherence metrics and healthcare utilisation: a prospective cohort study of older hypertensive adults. Int J Pharm Pract. https://doi.org/10.1111/ijpp.12539
Prior S (2018) Budget 2019 papers: trends in general medical services (GMS). Department of Public Expenditure and Reform, Dublin. http://www.budget.gov.ie/Budgets/2019/Documents/Trends%20in%20General%20Medical%20Services%20(G454 MS)%20Scheme.pdf. Accessed on 20th December 2018
Butler RJ, Davis TK, Johnson WG, Gardner HH (2011) Effects of nonadherence with prescription drugs among older adults. Am J Manag Care 17(2):153–160
Kim J-A, Lim MK, Kim K, Park J, Rhee CK (2018) Adherence to inhaled medications and its effect on healthcare utilization and costs among high-grade chronic obstructive pulmonary disease patients. Clin Drug Investig 38(4):333–340. https://doi.org/10.1007/s40261-017-0612-2
Modi A, Siris ES, Tang J, Sen S (2015) Cost and consequences of noncompliance with osteoporosis treatment among women initiating therapy. Curr Med Res Opin 31(4):757–765. https://doi.org/10.1185/03007995.2015.1016605
Simpson SH, Eurich DT, Majumdar SR, Padwal RS, Tsuyuki RT, Varney J, Johnson JA (2006) A meta-analysis of the association between adherence to drug therapy and mortality. BMJ 333(7557):15. https://doi.org/10.1136/bmj.38875.675486.55
Ettinger AB, Manjunath R, Candrilli SD, Davis KL (2009) Prevalence and cost of nonadherence to antiepileptic drugs in elderly patients with epilepsy. Epilepsy Behav 14(2):324–329. https://doi.org/10.1016/j.yebeh.2008.10.021
Grimes T, Fitzsimons M, Galvin M, Delaney T (2013) Relative accuracy and availability of an Irish National Database of dispensed medication as a source of medication history information: observational study and retrospective record analysis. J Clin Pharm Ther 38(3):219–224. https://doi.org/10.1111/jcpt.12036
Wallace E, Moriarty F, McGarrigle C, Smith SM, Kenny R-A, Fahey T (2018) Self-report versus electronic medical record recorded healthcare utilisation in older community-dwelling adults: comparison of two prospective cohort studies. PLoS One 13(10):e0206201. https://doi.org/10.1371/journal.pone.0206201
Acknowledgements
The authors wish to thank TILDA staff at Trinity College Dublin and staff at the HSE-PCRS for collecting and providing the authors with the data used in this study.
Authors’ individual contributions
CW, CC and KB were involved in the concept and design of the study. Data was provided by TILDA and the HSE-PCRS. CW carried out the statistical analysis. All authors were involved in interpretation of the data. CW wrote the first draft of the manuscript and all authors contributed to subsequent drafts.
Funding
CW, CC and KB were funded by the Health Research Board (HRB), Research Leaders Award (HRB RL-2015-1579). This work was conducted as part of the SPHeRE Programme under Grant No. SPHeRE/2013/1. TILDA is supported by the Department of Health and Children, The Atlantic Philanthropies and Irish Life.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Ethical approval for each wave of TILDA was obtained from the Trinity College Research Ethics Committee. Provision was made within this application to allow for the linking of participants GMS dispensing data, subject to participants’ consent.
Disclaimer
The funding bodies had no role in this study design, data analysis, writing of the manuscript or the decision to submit for publication.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary Table 1
(PDF 259 kb)
Supplementary Table 2
(PDF 275 kb)
Supplementary Table 3
(PDF 278 kb)
Supplementary Table 4
(PDF 276 kb)
Supplementary Table 5
(PDF 276 kb)
Rights and permissions
About this article
Cite this article
Walsh, C.A., Cahir, C. & Bennett, K.E. Association between adherence to antihypertensive medications and health outcomes in middle and older aged community dwelling adults; results from the Irish longitudinal study on ageing. Eur J Clin Pharmacol 75, 1283–1292 (2019). https://doi.org/10.1007/s00228-019-02699-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-019-02699-w