Abstract
Purpose
Bosutinib is an oral, dual Src and Abl tyrosine kinase inhibitor (TKI) approved for the treatment of Philadelphia chromosome—positive chronic myeloid leukemia resistant or intolerant to prior TKI therapy. Bosutinib is primarily metabolized by cytochrome P450 (CYP) 3A4, suggesting drug interaction potential with other CYP3A4 modulators. This open-label, randomized, 2-sequence, 2-period crossover study assessed the effect of single-dose aprepitant, a moderate CYP3A4 inhibitor, on the single-dose pharmacokinetic profile of oral bosutinib 500 mg.
Methods
Nineteen healthy, fed adults received bosutinib (100 mg × 5) alone or coadministered with aprepitant (125 mg × 1) in each treatment period (with a ≥14-day washout); serial blood samples were analyzed. Safety was evaluated.
Results
Following coadministration of aprepitant with bosutinib, the area under the concentration-time curve from time zero extrapolated to infinity (AUCinf) and maximum plasma concentration (C max) were higher than in bosutinib alone (AUCinf, 4719 and 2268 ng•h/mL; C max, 146.0 and 94.94 ng/mL). For bosutinib with aprepitant versus bosutinib alone, mean terminal elimination half-life was similar (25.99 vs 27.79 h), time to C max was longer (6.02 vs 4.15 h), and apparent oral clearance (CL/F) was decreased (105.9 vs 220.4 L/h). The ratio of adjusted geometric means of AUCinf and C max for bosutinib with aprepitant relative to bosutinib alone were 199 % (90 % confidence interval, 167–237 %) and 153 % (127–184 %), respectively. Both treatments were well tolerated.
Conclusion
In healthy volunteers, administering a single dose of aprepitant increased the AUC and C max following a single dose of bosutinib by 99 and 53 %, respectively. These results are consistent with a moderate CYP3A4 inhibitor effect of aprepitant on bosutinib (Trial Registration: ClinicalTrials.gov NCT02058277).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
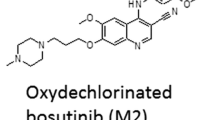
Bosutinib is an oral active, dual Src and Abl tyrosine kinase inhibitor (TKI) that has demonstrated efficacy in a single-arm phase I/II trial as a second-line treatment for patients with Philadelphia chromosome–positive (Ph+), chronic phase (CP), chronic myeloid leukemia (CML) resistant or intolerant to imatinib [1, 2], and as third-/fourth-line treatment in patients with CP CML or advanced leukemias after failure of imatinib and dasatinib and/or nilotinib therapy [3, 4]. The recommended dose of bosutinib is 500 mg once daily with food, with dose escalation to 600 mg daily considered for some patients with suboptimal response and no grade ≥3 toxicities [5].
The pharmacokinetic (PK) profile of bosutinib after oral administration has been well characterized. Following administration of bosutinib with food in healthy volunteers, the median time to maximum concentration (t max) was 6 h; mean clearance (CL/F) was 197 L/h and the mean terminal phase elimination half-life (t 1/2) was 33.8 h [6]. In addition, administration of bosutinib with food results in a ~2-fold increase in exposure and in improved tolerability [6]. A pooled population PK analysis indicated that bosutinib PK is described by a linear 2-compartment model with first-order absorption and an absorption lag time [7]. A high degree of PK variability was also evident in this model (percent coefficient of variance ranged from 63 to 66 % for AUC; 58 to 62 % for C max). This was, in part, attributed to the fact that bosutinib is primarily metabolized by cytochrome P450 (CYP) 3A4 [7, 8] and that CYP3A4 is differentially expressed across different patient subpopulations [9, 10].
Drug-drug interactions are particularly important in clinical practice because an association may potentially alter drug activity, efficacy, and/or possibly exacerbate or cause unexpected adverse events (AEs) [11]. The centrality of CYP3A4 in the metabolism of bosutinib raises the possibility that other drugs that interact with CYP3A4 may affect bosutinib PK. Such a drug-drug interaction could result in an overdosage of bosutinib and in subsequently higher rates of AEs. Coadministration of bosutinib with the strong CYP3A4 inhibitor, ketoconazole, has been shown to increase C max and AUC 5.2-fold and 8.6-fold, respectively [12]; coadministration with the strong CYP3A4 inducer, rifampin, has been shown to decrease C max and AUC by 7-fold and approximately 13-fold, respectively [13].
Aprepitant is a selective, high-affinity P/neurokinin 1 receptor antagonist used to prevent chemotherapy-induced nausea and vomiting that is also primarily metabolized by CYP3A4, and is a dose-dependent inhibitor and weak inducer of this isozyme [14–16]. Aprepitant undergoes extensive metabolism and its PK are non-linear across the clinical dose range [16]. Following a single oral dose of aprepitant 125 mg on day 1 and single doses of aprepitant 80 mg on days 2 and 3, AUC0–24h was ~19.6 and 21.2 μg/h/mL on days 1 and 3, respectively [16]. C max values of 1.6 and 1.4 μ/mL were reached ~4 h postdose [16]. The apparent t 1/2 of aprepitant ranged from approximately 9 to 13 h and its mean absolute bioavailability was 60 to 65 % over the 80 to 125 mg dose range [16]. Therefore, the present open-label, randomized, crossover study evaluated the effect of a single oral dose of aprepitant, which acts predominantly as a moderate CYP3A4 inhibitor in this setting, on the PK and safety profile of bosutinib in healthy subjects.
Methods
Study design
In this phase I, single-site, open-label, randomized, single-dose, 1-cohort, 2-sequence, 2-period crossover study (ClinicalTrials.gov ID: NCT02058277), healthy volunteers were randomized to one of two treatment sequences: oral bosutinib (100 mg × 5) alone in period 1 followed by bosutinib (100 mg × 5) in combination with single-dose aprepitant (125 mg × 1) in period 2, or bosutinib (100 mg × 5) in combination with single-dose aprepitant (125 mg × 1) in period 1 followed by oral bosutinib (100 mg × 5) alone in period 2. Treatment periods were separated by a minimum 14-day washout period. After fasting overnight for ≥10 h, subjects received study medication ≤5 min after completion of a standard breakfast that was consumed within 20 min on day 1 of each treatment period. No food was allowed ≤4 h postdose. Water could be consumed without restriction, except 1 h before and 1 h after dosing.
The protocol was approved by an independent ethics committee and was conducted in compliance with the ethical principles from the Declaration of Helsinki and with all International Conference on Harmonisation Good Clinical Practice guidelines. All subjects signed an informed consent document prior to enrollment.
Subjects
Eligible subjects were healthy men or women (aged 18–55 years) weighing >45 kg with a body mass index (BMI) of 17.5 to 30.5 kg/m2. Exclusion criteria included the following: clinically relevant abnormalities identified by medical history and full physical examination performed at screening; any laboratory abnormality that could increase the risk associated with study participation or could interfere with the interpretation of study results; any condition potentially affecting drug absorption; blood pressure ≥140 mm Hg (systolic) or ≥90 mm Hg (diastolic); QTc duration ≥450 msec; positive urine illicit drug screen; consumption of alcoholic beverages or use of tobacco or nicotine-containing products ≤24 h before first dose; investigational drug therapy ≤30 days (or 5 half-lives) before first dose; use of prescription or nonprescription drugs or dietary supplements ≤7 days before first dose; history of sensitivity to heparin or heparin-induced thrombocytopenia.
Sampling and analysis methods
Blood samples (3 mL) were collected in potassium ethylenediamine tetraacetic acid (K3-EDTA)-treated tubes to determine bosutinib PK on 2 h predose and at 1, 2, 3, 4, 6, 8, 12, 18, 24, 36, 48, 60, 72, and 96 h postdose. Blood samples were immediately stored on ice pending centrifugation at approximately 1700×g for about 10 min at 4 °C. The resultant K3-EDTA plasma samples were stored in screw capped polypropylene tubes at approximately –80 °C within 1 h of collection and were analyzed for bosutinib concentrations by inVentiv Health Clinical Lab, Inc. (East Princeton, NJ) using a validated high performance liquid chromatography-tandem mass spectrometry method. Calibration standard responses were linear over the range of 1 to 200 ng/mL using a (L/concentration2) linear least squares regression. The lower limit of quantification for bosutinib was 1 ng/mL (further details are provided in Supplementary Materials). The PK of aprepitant was not determined.
Assessments
Bosutinib PK parameters were calculated for each subject and treatment from a standard noncompartmental analysis of plasma concentration-time data using internally validated electronic noncompartmental analysis software (further details are provided in the online-only Supplementary Material).
Safety and tolerability was assessed from clinically significant signs and symptoms, laboratory tests (hematology, chemistry, urinalysis, and others), physical examinations, vital signs, and 12-lead electrocardiograms. Adverse events (AEs) were monitored during the study period and serious AEs (SAEs) of any causality were monitored from the time of informed consent to 28 days after study drug administration. Drug-induced liver injury was assessed based on elevations of aspartate or alanine transaminase levels concurrent with elevations in total bilirubin.
Statistical analyses
A sample size of approximately 14 subjects was required to provide 90 % confidence intervals (CI) for treatment-differences in loge AUCinf and C max of ±0.1752 and ±0.1535, respectively, with 80 % coverage probability. This calculation was based on corresponding estimates of within subject standard deviations (SD) of 0.2266 and 0.2779, respectively [8].
All PK parameters were summarized descriptively by treatment. Estimates of the adjusted mean differences between bosutinib plus aprepitant (test) and bosutinib alone (reference) in AUCinf (or AUClast) and C max for all subjects with corresponding 90 % CIs were obtained using a mixed effect model with sequence, period, and treatment as fixed effects and subject within sequence as a random effect. The adjusted mean differences and 90 % CIs for the differences were exponentiated to provide point estimates of the ratio of adjusted geometric means (test/reference) and 90 % CIs for the ratios.
Results
Subjects
A total of 20 subjects were randomized. Most of the subjects were male (12/20), white (14/20) with a mean age of 35.4 years (range 19 to 55 years), and mean weight and BMI of 76.5 kg (range 56.3 to 96.8 kg) and 25.9 kg/m2 (range 20.6 to 30.4 kg/m2; Table 1), respectively. Among the 20 subjects randomized, 1 subject from each treatment group discontinued the study (both withdrew consent between the treatment phase and washout period due to family emergencies). All 20 randomized subjects were analyzed for PK and safety; although 4 subjects receiving bosutinib alone were excluded from the PK analysis due to vomiting within a time period corresponding to 2 × median t max and within 6 h after drug administration.
Pharmacokinetics
Higher median plasma bosutinib concentration-time profiles were observed following administration of bosutinib plus aprepitant than with bosutinib alone (Fig. 1). Mean values of C max and AUCinf were ~1.5- and 2.1-fold higher, respectively, following bosutinib plus aprepitant administration than with bosutinib alone (Table 2). Among other PK parameters assessed for bosutinib in combination with aprepitant alone and bosutinib alone, respectively, t 1/2 was similar, t max was ~1.5-fold longer, and CL/F was ~2.1-fold lower.
Median plasma bosutinib concentration versus time profiles following single oral doses. A linear plot (a) and a semi-logarithmic plot (b) are shown in the panels. The PK data derived from 4 subjects receiving bosutinib treatment alone were excluded from this analysis because these subjects vomited within 6 h (2 × t max) postdose
Statistical comparisons of bosutinib PK parameters are summarized in Table 3. The adjusted geometric means of AUCinf and C max were ~2.0-fold and ~1.5-fold higher, respectively, following bosutinib with aprepitant relative to bosutinib alone. Moderate to high intersubject variabilities in bosutinib geometric mean AUCinf and C max was observed with percent coefficient of variation ranging from 31 to 51 % and 55 to 59 %, respectively Fig. 2.
Individual and geometric mean plasma bosutinib AUCinf (a) and C max (b). Star represents the geometric mean and circles represent individual values. Box plot provides median and 25/75 % quartiles with whiskers to the last point within 1.5× interquartile range. The PK data derived from 4 subjects receiving bosutinib treatment alone were excluded from this analysis because these subjects vomited within 6 h (2 × t max) postdose. AUC inf area under the plasma concentration-time profile from zero time extrapolated to infinite time, C max maximum observed concentration
Safety assessment
A total of 25 treatment-emergent AEs (TEAEs) were reported by 13 (68 %) subjects receiving bosutinib alone and a total of 22 TEAEs were reported by 12 (63 %) subjects receiving bosutinib plus aprepitant. Twenty-three of the 25 TEAEs reported by subjects receiving bosutinib only and all 22 TEAEs received by bosutinib plus aprepitant were considered treatment related by the investigator. All TEAEs were of mild or moderate severity. There were no SAEs, deaths, discontinuations, dose reductions, or dose delays due to AEs in the study.
The most frequent TEAEs were gastrointestinal events (Table 4); primarily diarrhea, which was reported by 10 subjects receiving bosutinib only (mild severity, n = 2; moderate severity, n = 8) and 11 subjects receiving bosutinib plus aprepitant (mild severity, n = 1; moderate severity, n = 10). Nausea was reported by 7 subjects receiving bosutinib alone (mild severity, n = 1; moderate severity, n = 6) and 5 subjects receiving bosutinib plus aprepitant (mild severity, n = 2; moderate severity, n = 3). Vomiting was reported by 4 subjects receiving bosutinib only and by no subjects receiving bosutinib plus aprepitant. Two headache TEAEs among subjects receiving bosutinib alone were considered not treatment related by the investigator.
Discussion
The results of this study show that coadministration of bosutinib with aprepitant resulted in an increase in AUCinf and C max by approximately 100 and 50 %, respectively. In keeping with this increase in exposure, there was an approximately 50 % decrease in apparent CL/F and apparent volume of distribution (Vz/F) of bosutinib. There were no apparent differences in t 1/2, but t max was more prolonged in the presence of aprepitant than with bosutinib alone (6.02 and 4.15 h, respectively). Values of PK parameters observed here were similar to those reported previously for bosutinib 500 mg in healthy subjects [13]. Together, these results are consistent with a moderate CYP3A4 inhibitor effect of aprepitant on bosutinib metabolism. The similar decrease in CL/F and Vz/F in the presence of aprepitant indicates that aprepitant changed the bioavailability of bosutinib through the reduction of first-pass metabolism, but did not change the clearance and volume of distribution of bosutinib.
When used for the prevention of chemotherapy-induced nausea or vomiting, the recommended dose of aprepitant is 125 mg on day 1 and 80 mg on days 2 and 3 of treatment [16]. However, since the AUC0–24h and C max are similar after a single dose of 125 mg on day 1 and 80 mg once daily on days 2 and 3 (all 3 daily doses comprise the approved dose) [16], the highest dose and exposures of aprepitant were used in this study to maximize the inhibitory effect of aprepitant. Bosutinib can be administered to healthy volunteers only as a single dose because of potential safety concerns. Thus, bosutinib exposures in this study were lower than steady-state levels, likely resulting in a stronger or similar CYP3A4 inhibition by aprepitant, and a more conservative assessment of CYP3A4 inhibition than studies in which bosutinib exposure is at steady-state.
A physiologically-based pharmacokinetic (PBPK) model of bosutinib was developed in a previous study based on in vitro absorption, distribution, metabolism, and excretion (ADME) data to assess potential effects of moderate CYP3A4 inhibitors on systemic exposures of bosutinib following multiple oral dose administration [17]. Bosutinib exposures predicted by the PBPK model were in reasonable agreement with increases and decreases in bosutinib exposure resulting from coadministration with ketoconazole or rifampin, respectively, observed in phase 1 clinical trials [12, 13]. Simulation results also predicted that bosutinib exposures increased significantly upon coadministration of moderate CYP3A4 inhibitors, such as fluconazole and erythromycin. A similar approach has been used to assess potential drug-drug interactions involving a variety of CYP3A4 inhibitors and drug substrates [18]. Examples include the effects of 4-{(R)-(3-Aminophenyl)[4-(4-fluorobenzyl)-piperazin-1-yl]methyl}-N,N-diethylbenzamide (AZD2327), lanicemine (AZD6765), and telithromycin on midazolam exposure [19–21]; fluconazole on ruxolitinib exposure [22]; and ketoconazole and rifampin on alisporivir exposure [23]. However, with clinical interaction data for both strong and moderate CYP3A4 inhibitors and a strong CYP3A4 inducer, the PBPK model of bosutinib would be more robust and refined in a future analysis in which the present aprepitant-bosutinib PK interaction data were added. This could provide a powerful tool for quantitatively predicting bosutinib exposures resulting from PK interactions with other CYP3A4 inhibitors or inducers.
Overall, coadministration of bosutinib with aprepitant was safe and well tolerated in these healthy subjects; the incidence of TEAEs in subjects receiving bosutinib plus aprepitant was similar to that in subjects receiving bosutinib alone (68 and 63 %, respectively). Mild to moderately severe gastrointestinal TEAEs were the most commonly reported events in both treatment groups (68 and 63 %), with diarrhea being most frequent (53 and 58 %), which is consistent with bosutinib toxicity profiles reported previously in studies recruiting healthy volunteers [6, 12, 13, 24–26] or patients with Ph + CML receiving bosutinib [1, 3, 4, 27–29]. It is also notable that no vomiting events were reported among subjects receiving bosutinib plus aprepitant, compared with 4 subjects receiving bosutinib alone. Although this single-dose study was not designed to assess the antiemetic efficacy of aprepitant and the small sample sizes limit interpretation of these data, the data are consistent with the mode of action of aprepitant.
In conclusion, in healthy volunteers, administration of a single dose of aprepitant increased the AUC and C max following a single dose of bosutinib by 99 and 53 %, respectively.
References
Cortes JE, Kantarjian HM, Brummendorf TH, Kim DW, Turkina AG, Shen ZX, Pasquini R, Khoury HJ, Arkin S, Volkert A, Besson N, Abbas R, Wang J, Leip E, Gambacorti-Passerini C (2011) Safety and efficacy of bosutinib (SKI-606) in chronic phase Philadelphia chromosome-positive chronic myeloid leukemia patients with resistance or intolerance to imatinib. Blood 118(17):4567–4576
Brummendorf TH, Cortes JE, Khoury HJ, Kantarjian HM, Kim DW, Schafhausen P, Conlan MG, Shapiro M, Turnbull K, Leip E, Gambacorti-Passerini C, Lipton JH (2016) Factors influencing long-term efficacy and tolerability of bosutinib in chronic phase chronic myeloid leukaemia resistant or intolerant to imatinib. Br J Haematol 172(1):97–110
Kantarjian HM, Cortes JE, Kim DW, Khoury HJ, Brummendorf TH, Porkka K, Martinelli G, Durrant S, Leip E, Kelly V, Turnbull K, Besson N, Gambacorti-Passerini C (2014) Bosutinib safety and management of toxicity in leukemia patients with resistance or intolerance to imatinib and other tyrosine kinase inhibitors. Blood 123(9):1309–1318
Khoury HJ, Cortes JE, Kantarjian HM, Gambacorti-Passerini C, Baccarani M, Kim DW, Zaritskey A, Countouriotis A, Besson N, Leip E, Kelly V, Brummendorf TH (2012) Bosutinib is active in chronic phase chronic myeloid leukemia after imatinib and dasatinib and/or nilotinib therapy failure. Blood 119(15):3403–3412
BOSULIF® (bosutinib) (2016) Full prescribing information. Pfizer Labs, Pfizer Inc, New York, NY, USA
Abbas R, Hug BA, Leister C, Gaaloul ME, Chalon S, Sonnichsen D (2012) A phase I ascending single-dose study of the safety, tolerability, and pharmacokinetics of bosutinib (SKI-606) in healthy adult subjects. Cancer Chemother Pharmacol 69(1):221–227
Hsyu PH, Mould DR, Abbas R, Amantea M (2014) Population pharmacokinetic and pharmacodynamic analysis of bosutinib. Drug Metab Pharmacokinet 29(6):441–448
Pfizer Inc. (2015): New York, NY. Data on file
Zhu B, Liu ZQ, Chen GL, Chen XP, Ou-Yang DS, Wang LS, Huang SL, Tan ZR, Zhou HH (2003) The distribution and gender difference of CYP3A activity in Chinese subjects. Br J Clin Pharmacol 55(3):264–269
Lin YS, Lockwood GF, Graham MA, Brian WR, Loi CM, Dobrinska MR, Shen DD, Watkins PB, Wilkinson GR, Kharasch ED, Thummel KE (2001) In-vivo phenotyping for CYP3A by a single-point determination of midazolam plasma concentration. Pharmacogenetics 11(9):781–791
Pfizer Inc. (2015) Dosage and administration instructions for oral dosing of 75, 100, and 125 mg PD-0332991 formulated capsules as a suspension in water. New York, NY
Abbas R, Hug BA, Leister C, Burns J, Sonnichsen D (2011) Effect of ketoconazole on the pharmacokinetics of oral bosutinib in healthy subjects. J Clin Pharmacol 51(12):1721–1727
Abbas R, Boni J, Sonnichsen D (2015) Effect of rifampin on the pharmacokinetics of bosutinib, a dual Src/Abl tyrosine kinase inhibitor, when administered concomitantly to healthy subjects. Metabol Drug Pers Ther 30(1):57–63
Aapro MS, Walko CM (2010) Aprepitant: drug-drug interactions in perspective. Ann Oncol 21(12):2316–2323
Sarcev T, Secen N, Zaric B, Milovancev A (2008) Aprepitant—where do we stand in the control of chemotherapy-induced nausea and vomiting? J BUON 13(3):333–339
US Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER) (2002) Guidance for industry: food-effect bioavailability and fed bioequivalence studies. Silver Spring, MD
Ono C, Hsyu P-H, Abbass R, Loi C-M, Yamazaki S (2015) Application of physiologically-based pharmacokinetic modeling to bosutinib pharmacokinetics: prediction of drug-drug interactions as CYP3A substrate. American Society for Clinical Pharmacology and Therapeutics (ASCPT). New Orleans, LA:Poster 51
Wagner C, Pan Y, Hsu V, Grillo JA, Zhang L, Reynolds KS, Sinha V, Zhao P (2015) Predicting the effect of cytochrome P450 inhibitors on substrate drugs: analysis of physiologically based pharmacokinetic modeling submissions to the US Food and Drug Administration. Clin Pharmacokinet 54(1):117–127
Vieira ML, Zhao P, Berglund EG, Reynolds KS, Zhang L, Lesko LJ, Huang SM (2012) Predicting drug interaction potential with a physiologically based pharmacokinetic model: a case study of telithromycin, a time-dependent CYP3A inhibitor. Clin Pharmacol Ther 91(4):700–708
Bui KH, Zhou D, Agbo F, Guo J (2015) Effect of multiple intravenous doses of lanicemine (AZD6765) on the pharmacokinetics of midazolam in healthy subjects. J Clin Pharmacol 55(9):1024–1030
Guo J, Zhou D, Li Y, Khanh BH (2015) Physiologically based pharmacokinetic modeling to predict complex drug-drug interactions: a case study of AZD2327 and its metabolite, competitive and time-dependent CYP3A inhibitors. Biopharm Drug Dispos 36(8):507–519
Shi JG, Fraczkiewicz G, Williams WV, Yeleswaram S (2015) Predicting drug-drug interactions involving multiple mechanisms using physiologically based pharmacokinetic modeling: a case study with ruxolitinib. Clin Pharmacol Ther 97(2):177–185
Xia B, Barve A, Heimbach T, Zhang T, Gu H, Wang L, Einolf H, Alexander N, Hanna I, Ke J, Mangold JB, He H, Sunkara G (2014) Physiologically based pharmacokinetic modeling for assessing the clinical drug-drug interaction of alisporivir. Eur J Pharm Sci 63:103–112
Abbas R, Leister C, Sonnichsen D (2013) A clinical study to examine the potential effect of lansoprazole on the pharmacokinetics of bosutinib when administered concomitantly to healthy subjects. Clin Drug Investig 33(8):589–595
Abbas R, Leister C, El Gaaloul M, Chalon S, Sonnichsen D (2012) Ascending single-dose study of the safety profile, tolerability, and pharmacokinetics of bosutinib coadministered with ketoconazole to healthy adult subjects. Clin Ther 34(9):2011–2019
Hsyu PH, Mould DR, Upton RN, Amantea M (2013) Pharmacokinetic-pharmacodynamic relationship of bosutinib in patients with chronic phase chronic myeloid leukemia. Cancer Chemother Pharmacol 71(1):209–218
Cortes JE, Kim DW, Kantarjian HM, Brummendorf TH, Dyagil I, Griskevicius L, Malhotra H, Powell C, Gogat K, Countouriotis AM, Gambacorti-Passerini C (2012) Bosutinib versus imatinib in newly diagnosed chronic-phase chronic myeloid leukemia: results from the BELA trial. J Clin Oncol 30(28):3486–3492
Gambacorti-Passerini C, Brummendorf TH, Kim DW, Turkina AG, Masszi T, Assouline S, Durrant S, Kantarjian HM, Khoury HJ, Zaritskey A, Shen ZX, Jin J, Vellenga E, Pasquini R, Mathews V, Cervantes F, Besson N, Turnbull K, Leip E, Kelly V, Cortes JE (2014) Bosutinib efficacy and safety in chronic phase chronic myeloid leukemia after imatinib resistance or intolerance: minimum 24-month follow-up. Am J Hematol 89(7):732–742
Brummendorf TH, Cortes JE, de Souza CA, Guilhot F, Duvillie L, Pavlov D, Gogat K, Countouriotis AM, Gambacorti-Passerini C (2015) Bosutinib versus imatinib in newly diagnosed chronic-phase chronic myeloid leukaemia: results from the 24-month follow-up of the BELA trial. Br J Haematol 168(1):69–81
Acknowledgments
This study was sponsored by Pfizer Inc. Medical writing support was provided by Simon Slater, PhD, of Complete Healthcare Communications, LLC., and was funded by Pfizer Inc. Disclosures: PHH, DSP, and KM are employees of Pfizer Inc.
The protocol was approved by an independent ethics committee and was conducted in compliance with the ethical principles from the Declaration of Helsinki and with all International Conference on Harmonisation Good Clinical Practice Guidelines. Informed consent was obtained from all individual participants included in the study.
Contributions of authors
PH conceived and designed the study; PH provided the study material or patients; DSP, PH, KM analyzed and interpreted the data; PH and KM wrote the manuscript; and all authors approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
ESM 1
(DOCX 22 kb)
Rights and permissions
About this article
Cite this article
Hsyu, PH., Pignataro, D.S. & Matschke, K. Effect of aprepitant, a moderate CYP3A4 inhibitor, on bosutinib exposure in healthy subjects. Eur J Clin Pharmacol 73, 49–56 (2017). https://doi.org/10.1007/s00228-016-2108-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-016-2108-z