Abstract
Purpose
Bosutinib is an orally active, dual Src/Abl tyrosine kinase inhibitor that has demonstrated manageable safety and high response rates in patients with chronic phase (CP) chronic myeloid leukemia (CML). The current analysis evaluated potential bosutinib pharmacokinetic–pharmacodynamic relationships.
Methods
Bosutinib exposure metrics at steady state were estimated from a previously developed population pharmacokinetic model. Safety and efficacy metrics were from two clinical studies of bosutinib 500 mg/day in patients with CP CML.
Results
The analysis included 749 patients (aged 18–91 years; mean weight, 75 kg; 54 % male). An exposure–response relationship was identified for the pooled incidence (but not severity) of diarrhea, with predicted probability ranging from 0.575 to 0.797 for the lowest and highest area under the curve bins, respectively; a weak relationship was also observed for the incidence of rash (predicted probability, 0.216–0.419). There was no evidence of an exposure–response relationship for nausea, vomiting, neutropenia, thrombocytopenia, or elevated alanine and aspartate aminotransferases. Exposure–response relationships were observed in patients with newly diagnosed CP CML for complete cytogenetic response at 1 year (predicted probability, 0.476–0.650), major molecular response at 1 year (0.238–0.497), and cumulative complete hematologic response (CHR) at 1 year (0.605–0.763). Patients with previously treated CP CML showed no exposure–response relationship for major cytogenetic response at 24 weeks (0.320); for CHR, higher bosutinib exposure was associated with a lower probability of response (0.926–0.743).
Conclusions
The absence of exposure–response relationships for some safety and efficacy metrics may reflect bosutinib exposure metrics that exceeded the half-maximal inhibitory values and achieved a maximum effect.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
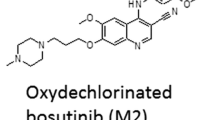
Bosutinib (SKI-606) is a potent, orally active, dual competitive Src and Abl tyrosine kinase inhibitor (TKI) in the development of the treatment for Philadelphia chromosome–positive (Ph+) leukemia [1, 2]. Bosutinib 500 mg once daily is associated with a manageable safety profile primarily characterized by transient and manageable gastrointestinal events and rash [3–6]. Bosutinib has also demonstrated good efficacy with high response rates in both newly diagnosed and imatinib-resistant or imatinib-intolerant patients with chronic phase (CP) chronic myeloid leukemia (CML) [4–6]. In a phase III study that evaluated treatment with bosutinib versus imatinib in patients with newly diagnosed CP CML, bosutinib demonstrated superior rates of major molecular response (MMR) at 1 year, similar rates of complete cytogenetic response (CCyR) and complete hematologic response (CHR) at 1 year, and fewer events of transformation to accelerated or blast phase CML compared with imatinib [6]. A phase I/II study evaluating the safety and efficacy of bosutinib in previously treated patients with CP CML has demonstrated high rates of CHR and major cytogenetic response (MCyR) in the second-line setting, following development of resistance or intolerance to imatinib [4], as well as in the third- and fourth-line settings following resistance or intolerance to imatinib as well as dasatinib and/or nilotinib [5].
Recently, a bosutinib population pharmacokinetic model was developed using pooled pharmacokinetic data from three bosutinib studies of patients with solid tumors or Ph+ CP CML [7], so as to better understand the pharmacokinetics of bosutinib and permit evaluation of pharmacokinetic–pharmacodynamic associations. The final bosutinib population pharmacokinetic model demonstrated relatively small variability within individuals, but large inter-individual variability in kinetics, possibly due to poor compliance in dosing and/or taking bosutinib with food. Overall, the pharmacokinetic model of bosutinib showed acceptable descriptive and predictive performance that was suitable for deriving individual exposure metrics for subsequent pharmacokinetic–pharmacodynamic analyses [7].
The current pharmacokinetic–pharmacodynamic analysis investigated the relationship between bosutinib exposure at steady state and key safety endpoints (i.e., diarrhea, thrombocytopenia, rash, alanine aminotransaminase [ALT], aspartate aminotransaminase [AST], nausea, vomiting, and neutropenia) using data pooled from the phase III and phase I/II clinical studies of bosutinib monotherapy in patients with newly diagnosed CP CML and in patients with CP CML resistant to or intolerant of prior imatinib therapy, respectively. Associations between bosutinib exposure at steady state and key efficacy endpoints from each of the two studies were also investigated.
Materials and methods
Included clinical studies
The pharmacokinetic–pharmacodynamic analysis used safety and efficacy data collected from two clinical studies of bosutinib monotherapy. Patients with paired pharmacokinetic and pharmacodynamic data were included in the current analysis.
The first study was a randomized, open-label, active-controlled (versus imatinib) phase 3 trial [6] in patients with newly diagnosed (≤6 months) Ph+ CP CML and no prior antileukemia treatment (except anagrelide or hydroxyurea). Bosutinib 500 mg was administered once daily with food.
The second study was an open-label, two-part, phase 1/2 trial [4, 5] of bosutinib in patients with confirmed Ph+ leukemia and resistance or intolerance to prior imatinib (and possibly prior dasatinib and/or nilotinib) therapy; only patients with CP CML were included in the current analysis. Part 1 was a dose-escalation study of bosutinib 400–600 mg administered once daily with food to determine the recommended starting dose for Part 2. Part 2 evaluated the safety and efficacy of bosutinib 500 mg once daily with food (recommended dose determined in Part 1 of the study).
Pharmacokinetic metrics
Previously, a population pharmacokinetic model of bosutinib was successfully developed using pooled pharmacokinetic data from 870 patients enrolled in three clinical studies that evaluated bosutinib monotherapy [7]. The final pharmacokinetic model was a two-compartment model with first-order elimination, first-order absorption, and an absorption lag. Relative bioavailability, which was incorporated into the structural pharmacokinetic model, was dose dependent, and the model estimated that bosutinib levels approached steady state after 4 days. Model simulations showed that a dose of bosutinib 500 mg/day was associated with high inter-individual variability that could not be accounted for by baseline characteristics (including body size) or laboratory results. A summary of the pharmacokinetic model values is provided in Appendix Table A1 (online only).
Bosutinib exposure metrics (e.g., area under the curve [AUC], maximal plasma concentration [C max], and minimal plasma concentration [C min]) used in the current analysis were derived from a population pharmacokinetic model [7]. Exposure metrics were binned to accommodate an equal number of observations per bin, and greater than or equal to 20 observations were included per bin; the label of each bin was the mean value of the observations in the bin.
Safety metrics
Safety endpoints were analyzed for an exposure–response relationship using data pooled from the bosutinib phase III study in patients with newly diagnosed CP CML and phase I/II study in patients with CP CML following prior TKI therapy. Primary safety endpoints included diarrhea, thrombocytopenia, rash, increased ALT, and increased AST. Secondary safety endpoints included nausea, vomiting, and neutropenia.
To evaluate the severity of an adverse event (AE), ordinal values were assigned based on a 5-point scale, from 0 to 4, where 0 corresponded to no AE and 1, 2, 3, and 4 corresponded to the National Cancer Institute Common Terminology Criteria for Adverse Events severity grades; the value recorded for each patient was the highest severity of AE grade reported during the treatment period. The incidence of an AE was defined as the presence or absence of any AE, regardless of severity grade, coded as binary variables (i.e., scored as 0 for no event and 1 for any event [severity grades ≥1]). A summary of pooled safety metrics is provided in Appendix Table A2 (online only).
Efficacy metrics
Exposure–response relationships for the efficacy endpoints were evaluated separately for the phase III and phase I/II studies. For the phase III study in patients with newly diagnosed CP CML, efficacy endpoints included CCyR at 1 year, MMR at 1 year, and CHR at 1 year. For the phase I/II study in patients with CP CML following prior TKI therapy, efficacy endpoints were MCyR at 24 weeks and cumulative CHR. Efficacy metrics for each study were coded as binary variables, where 0 corresponded to no response and 1 corresponded to response. A summary of efficacy metrics for each study is provided in Appendix Table A3 (online only).
Modeling
The incidence (i.e., presence or absence) of safety or efficacy metrics was examined using logistic regression, while the severity of safety metrics when scored using an ordinal scale was examined using ordered logistic regression.
Logistic regression was conducted by testing five candidate models (i.e., constant probability, linear, log-linear, maximum possible drug effect [E max], and sigmoid E max models) of the exposure–response relationship, using the $PRED subroutine of NONMEM 7 (Icon Development Solutions, Dublin, Ireland). The general form of the logistic regression model was as follows:
where Y denotes a safety or efficacy metric and g{x} denotes the logit transform of the odds of occurrence of the metric; CONST defines the baseline constant probability of the metric, while f(DRUG) is a function relating the log-odds of the metric to bosutinib exposure.
The exposure–effect models used for the logistic regression analysis were also used for the ordered regression analysis. However, for these models, the CONST parameter in the model was replaced by four parameters (i.e., B1, B2, B3, and B4). B1 was analogous to CONST in the logistic regression models, but represented the probability of a metric grade ≥1. The parameters B2, B3, and B4 represented the difference in log-odds for scores that were ≥2, ≥3, and 4, respectively.
Models were selected on the basis of goodness of fit, as judged by changes in the minimum objective function value (OFV). Akaike Information Criteria (AIC) were calculated from the OFV as:
where nPar was the number of parameters in the model. Competing models were ranked by AIC (lower is better); models with an AIC of <2 units difference were declared substantially equivalent, and the simpler model was selected. In addition, models were not considered if they did not pass the covariance step of NONMEM 7, which was taken to indicate imprecise parameter estimates (i.e., percent standard error was not estimable for any parameter). Models that passed the covariance step but had a percent standard error >51.02 % were also not considered, consistent with the asymptotic 95 % confidence intervals of the parameter including 0.
Results
Patient characteristics
Key patient characteristics for both the safety and efficacy analyses are provided in Table 1. A total of 749 patients were included in the pooled safety analysis. For the efficacy analysis, 245 patients with newly diagnosed CP CML and 266 patients with CP CML and prior TKI therapy were included. Overall, enrolled patients were 54 % males, aged 18–91 years old, and had a mean baseline weight of 75.0 kg.
Bosutinib exposure
Exposure metrics for bosutinib 500 mg/day were obtained from the recently developed bosutinib pharmacokinetic model [7]. The post hoc pharmacokinetic parameters for the final pharmacokinetic model were estimated using the POSTHOC option of the $ESTIMATION step of NONMEM 7. The parameters were then merged with a database of the most frequent (mode) dose used for each patient, with sample times from 0 to 24 h at 0.5-hour intervals, representing the inter-dose interval. The final model was used to estimate C max, time to C max (t max), and C min from the simulated individual bosutinib concentration–time curves. AUC was estimated as Dose i /CL i , where the subscript i represents the individual values of mode dose and post hoc clearance. Median C max at steady state was 215 ng/mL (range, 43.9–1,019 ng/mL), median C min at steady state was 147 ng/mL (range, 16.2–841 ng/mL), and median AUC at steady state was 4,322 ng/mL h (range, 735–22,326 ng/mL h).
Safety parameters
Data from the pooled safety analysis (Appendix Table A2) demonstrated that although gastrointestinal toxicities (e.g., diarrhea [76 %], nausea [40 %], and vomiting [35 %]) were frequently reported across the two studies, most events were of low severity grade. Other toxicities of clinical interest included thrombocytopenia (29 %), rash (25 %), ALT elevation (21 %), AST elevation (17 %), and neutropenia (16 %).
In the current pharmacokinetic–pharmacodynamic analysis, the ordered logistic regression models revealed that a higher number of patients with a diarrhea score of 0 (i.e., no diarrhea AE reported) were observed for the lower bosutinib exposure bins, regardless of whether bosutinib AUC, C max, or C min was used (Fig. 1a). For evaluation of a relationship between bosutinib exposure and diarrhea severity, an E max model was the preferred exposure–response model for both AUC and C max. A logistic regression analysis of the incidence of diarrhea (probability of grade ≥1 AE) versus bosutinib AUC confirmed the findings of the ordered regression analysis of diarrhea severity. An exposure–response relationship (sigmoid E max model) was identified for the incidence of diarrhea, with a predicted probability of diarrhea incidence ranging from 0.575 for the lowest bosutinib AUC bin (1,384 ng/mL h) to 0.797 for the highest bosutinib AUC bin (12,919 ng/mL h; Fig. 1b and Table 2).
Probability of safety events versus bosutinib exposure. a Observed probability of grade 0–4 diarrhea. b Calculated probability of grade ≥1 diarrhea. c Observed probability of grade 0–4 rash. d Calculated probability of grade ≥1 rash. e Observed probability of grade 0–4 ALT elevation. f Calculated probability of grade ≥1 ALT elevation. For all figure parts, bosutinib exposure is shown as AUC, derived from a previously developed bosutinib population pharmacokinetic model. For a, c, and e, ordinal values were assigned such that 0 corresponded to no AE and 1, 2, 3, and 4 corresponded to the maximum NCI Common Terminology Criteria for Adverse Events severity grade reported. For b, d, and f, data were coded as binary variables, where 0 corresponded to no AE and 1 corresponded to an AE of grade ≥1. Solid lines are predictions of the best models. ALT alanine aminotransferase, AUC area under the curve, AE adverse event
A weak exposure–response relationship (log-linear model) was identified for the incidence (but not severity) of rash (Fig. 1c–d). The logistic regression analysis, which focused on the incidence of rash (probability of grade ≥1 AE) versus bosutinib AUC, showed that lower AUC bins were associated with a lower probability of rash, with the predicted probability of rash incidence ranging from 0.216 for the lowest AUC bin to 0.419 for the highest AUC bin.
There was no evidence supporting an exposure–response relationship for the incidence or severity of elevated ALT (Fig. 1e–f), elevated AST, thrombocytopenia, nausea, vomiting, or neutropenia (Table 2).
Efficacy parameters for patients with newly diagnosed CP CML
Data from the phase III study found that for the 245 patients with newly diagnosed CP CML who were included in the analysis, the overall probability of achieving a CCyR at 1 year was 0.698, achieving a MMR at 1 year was 0.400, and achieving/maintaining a CHR at 1 year was 0.714 (Appendix Table A3).
The current analysis found an exposure–response relationship for each of these response types (i.e., CCyR, MMR, and CHR) at 1 year (Table 3). Achievement of a CCyR at 1 year could be related to AUC and C min (sigmoid E max model), but not C max, with a predicted probability of achieving a CCyR ranging from 0.476 to 0.650 for the lowest (1,521 ng/mL h) and highest (10,806 ng/mL h) AUC bins, respectively (Fig. 2a–c). The exposure–response relationship for achieving a MMR at 1 year was described using an E max model for AUC and C max or a log-linear model for C min, with a predicted probability of achieving a MMR ranging from 0.238 to 0.497 for the lowest and highest AUC bins, respectively (Fig. 2d–f). Achieving/maintaining a CHR at 1 year could be related to AUC and C min (E max model), but not C max, with a predicted probability of achieving/maintaining a CHR ranging from 0.605 to 0.763 (Fig. 2g–i).
Probability of response at 1 year versus bosutinib exposure in patients with newly diagnosed CP CML. a, b, and c are the probability of achieving a CCyR at 1 year versus AUC, C max, and C min, respectively. d, e, and f are the probability of achieving a MMR versus AUC, C max, and C min, respectively. g, h, and i are the probability of achieving/maintaining a CHR versus AUC, C max, and C min, respectively. Response data were coded as binary variables, where 0 corresponded to no response and 1 corresponded to response; exposure metrics were derived from a previously developed bosutinib population pharmacokinetic model. Solid lines are predictions of the best models. Solid lines are predictions of the best models. CP CML chronic phase chronic myeloid leukemia, CCyR complete cytogenetic response, AUC area under the curve, C max maximal plasma concentration, C min minimum plasma concentration, MMR major molecular response, CHR complete hematologic response
Efficacy parameters for patients with CP CML and prior TKI therapy
For the 266 patients from the phase I/II study with CP CML and prior TKI therapy who were included in the analysis, the overall probability of achieving a MCyR at 24 weeks was 0.320 and achieving/maintaining a CHR was 0.861 (Appendix Table A3).
A summary of exposure–response relationships for MCyR at 24 weeks and cumulative CHR efficacy parameters is provided in Table 3. No evidence was found for an exposure–response relationship for achievement of a MCyR at 24 weeks (Fig. 3a–c). A graphical analysis of the relationship between bosutinib exposure and the probability of achieving a MCyR showed a tendency for the lowest exposure bin to have the lowest probability of achieving a MCyR for AUC and C max. However, because the logistic regression analysis was unable to quantify this trend, with the constant probability model being the preferred model for all three exposure metrics, it was concluded that the predicted probability of achieving a MCyR was the same regardless of bosutinib exposure and that the observed difference between exposure bins was consistent with random variability. The predicted probability of achieving a MCyR at 24 weeks across patients with prior TKI therapy was 0.320.
Probability of response versus bosutinib exposure in patients with CP CML and prior therapy. a, b, and c are the probability of achieving a MCyR at 24 weeks versus AUC, C max, and C min, respectively. d, e, and f are the probability of achieving/maintaining a cumulative CHR versus AUC, C max, and C min, respectively. Response data were coded as binary variables, where 0 corresponded to no response and 1 corresponded to response; exposure metrics were derived from a previously developed bosutinib population pharmacokinetic model. Solid lines are predictions of the best models. CP CML chronic phase chronic myeloid leukemia, MCyR major cytogenetic response, AUC area under the curve, C max maximal plasma concentration, C min minimum plasma concentration, CHR complete hematologic response
An exposure–response relationship was observed for achieving/maintaining a cumulative CHR with AUC (log-linear model) and C max (linear model), but not C min (Fig. 3d–f). However, the relationship was paradoxical, with higher bosutinib exposures associated with a lower probability of achieving/maintaining a cumulative CHR. The predicted probability of achieving/maintaining a cumulative CHR ranged from 0.926 to 0.743 for the lowest (1,650 ng/mL h) and highest (11,943 ng/mL h) AUC bins, respectively.
Discussion
Bosutinib has previously demonstrated good efficacy with high response rates and manageable tolerability among patients with CP CML. The objectives of the current pharmacokinetic–pharmacodynamic analysis were to investigate potential relationships between bosutinib exposure at steady state and data for key safety and efficacy endpoints from two bosutinib clinical studies of patients with newly diagnosed CP CML and those with imatinib-resistant or imatinib-intolerant CP CML. The analysis used standard graphical, logistic regression, and ordered logistic regression techniques and demonstrated exposure–response relationships for some, but not all, of the safety and efficacy endpoints evaluated.
For the safety endpoints, an exposure–response relationship was identified for the incidence, but not severity, of diarrhea, described by an E max model. A weak exposure–response relationship (log-linear model) was also identified for the incidence, but not severity, of rash. However, there was no evidence to support an exposure–response relationship for the incidence or severity of the other evaluated bosutinib toxicities, including thrombocytopenia, ALT elevation, AST elevation, nausea, vomiting, and neutropenia, which were all best described by a constant probability model.
The AEs investigated in the current study were selected based on the safety profile of bosutinib observed in multiple clinical studies [3–6, 8]. Previous and ongoing clinical studies have demonstrated that bosutinib has an acceptable safety profile that is characterized primarily by transient and manageable gastrointestinal AEs (i.e., diarrhea, nausea, and vomiting) and rash [3–6, 8]. Grade 3/4 liver-related AEs, primarily ALT and AST elevations, have additionally been noted with bosutinib treatment [4–6, 8]. Grade 3/4 neutropenia and thrombocytopenia were commonly reported for patients with CP CML during bosutinib therapy [4–6]; however, hematologic toxicity is a class effect of Bcr-Abl inhibitors that has also been commonly reported during treatment with dasatinib [9–12] and nilotinib [13, 14]. However, despite the consistent observation of these events during bosutinib treatment across clinical studies, the current pharmacokinetic–pharmacodynamic analysis indicated that neither the incidence nor severity of most of these events (except the incidence of diarrhea and rash) was associated with changes in bosutinib exposure.
Bosutinib has demonstrated efficacy in a phase III study of patients with newly diagnosed CP CML, with a superior rate of MMR at 1 year and similar rates of CCyR and CHR at 1 year compared with imatinib [6]. Of note, the current analysis did demonstrate bosutinib exposure–response relationships for CCyR, MMR, and CHR rates at 1 year in these patients. An exposure–response relationship (sigmoid E max model) was identified for CCyR for AUC and C min, but not C max, while the exposure–response relationship for MMR could be described using an E max model (AUC and C max) or a log-linear model (C min). For CHR at 1 year, the exposure–response relationship (E max model) was identified for AUC and C min, but not C max. Overall, regardless of the specific model fit, those patients with the lowest bosutinib exposures were less likely to have responded to bosutinib treatment at 1 year. Although dose reductions and interruptions are important for the management of certain toxicities associated with bosutinib treatment [4–6], the current analysis suggests that the resulting reduced exposure may also result in a reduced probability of response at 1 year for patients with newly diagnosed CP CML.
In the phase I/II study, 31 % of patients who were resistant to or intolerant of prior imatinib only achieved a MCyR at 24 weeks, while 86 % of patients achieved/maintained a cumulative CHR after a median follow-up of 24.2 months. Similar responses were observed in patients with CP CML who were previously treated with imatinib plus dasatinib and/or nilotinib, with rates of 32 % for MCyR and 73 % for CHR after a median follow-up period of 28.5 months. These data compare favorably with the findings from previous studies of patients with CP CML treated with dasatinib or nilotinib in the second-, third-, and/or fourth-line settings [15–17]. However, the current analysis showed that the exposure–response relationships for bosutinib were unclear in this patient population. There was no evidence of an exposure–response relationship for MCyR at 24 weeks among patients with prior TKI therapy, with a predicted probability of 0.320 for achieving a MCyR regardless of bosutinib exposure. A paradoxical exposure–response relationship (linear or log-linear model) was identified for achieving/maintaining a cumulative CHR, such that higher bosutinib exposure was associated with lower probability of CHR. However, this finding was anomalous because the probability of achieving/maintaining a cumulative CHR response in all bins was close to 1 (average 0.861), suggesting that the response had reached a plateau and the negative correlation was not clinically relevant.
The most notable feature of the analysis was that an exposure–response relationship could not be identified for several of the safety and efficacy metrics, possibly due to bosutinib exposure metrics that exceeded the half-maximal inhibitory (IC50) values [1]. Thus, if exposure metrics were at the plateau of the exposure–response curve, it would become difficult to determine a concentration–response relationship.
In conclusion, this pharmacokinetic–pharmacodynamic analysis identified an exposure–response relationship for the incidence of diarrhea and rash, but not for the incidence or severity of other evaluated toxicities associated with bosutinib treatment. Additionally, an exposure–response relationship was found for CCyR, MMR, and CHR at 1 year in patients with newly diagnosed CP CML, but the relationship between bosutinib exposure and efficacy was unclear in patients with prior TKI therapy. The absence of exposure–response relationships for some safety and efficacy metrics may reflect bosutinib exposure metrics that exceeded the IC50 values and achieved a plateau effect.
References
Puttini M, Coluccia AM, Boschelli F, Cleris L, Marchesi E, Donella-Deana A, Ahmed S, Redaelli S, Piazza R, Magistroni V, Andreoni F, Scapozza L et al (2006) In vitro and in vivo activity of SKI-606, a novel Src-Abl inhibitor, against imatinib-resistant Bcr-Abl +neoplastic cells. Cancer Res 66:11314–11322
Golas JM, Arndt K, Etienne C, Lucas J, Nardin D, Gibbons J, Frost P, Ye F, Boschelli DH, Boschelli F (2003) SKI-606, a 4-anilino-3-quinolinecarbonitrile dual inhibitor of Src and Abl kinases, is a potent antiproliferative agent against chronic myelogenous leukemia cells in culture and causes regression of K562 xenografts in nude mice. Cancer Res 63:375–381
Daud AI, Krishnamurthi SS, Saleh MN, Gitlitz BJ, Borad MJ, Gold PJ, Chiorean EG, Springett GM, Abbas R, Agarwal S, Bardy-Bouxin N, Hsyu PH et al (2012) Phase I study of bosutinib, a Src/Abl tyrosine kinase inhibitor, administered to patients with advanced solid tumors. Clin Cancer Res 18:1092–1100
Cortes JE, Kantarjian HM, Brummendorf TH, Kim D-W, Turkina AG, Shen Z-X, Pasquini R, Khoury HJ, Arkin S, Volkert A, Besson N, Abbas R et al (2011) Safety and efficacy of bosutinib (SKI-606) in chronic phase Philadelphia chromosome-positive chronic myeloid leukemia patients with resistance or intolerance to imatinib. Blood 118:4567–4576
Khoury HJ, Cortes JE, Kantarjian HM, Gambacorti-Passerini CB, Baccarani M, Kim DW, Zaritskey A, Countouriotis A, Besson N, Leip E, Kelly V, Brummendorf TH (2012) Bosutinib is active in chronic phase chronic myeloid leukemia after imatinib and dasatinib and/or nilotinib therapy failure. Blood 119:3403–3412
Cortes JE, Kim Dong, Kantarjian HM, Brummendorf TH, Dyagil I, Griskevicus L, Malhotra H, Powell C, Gogat K, Countouriotis AM, Gambacorti-Passerini C (2012) Bosutinib versus imatinib in newly diagnosed chronic phase chronic myeloid leukemia: results from the BELA trial. J Clin Oncol (in press)
Hsyu P-H, Mould D, Abbas R, Pearce S, Amantea M (2011) A population pharmacokinetic model of bosutinib. Poster presented at: the AACR-EORTC-NCI molecular targets and cancer therapeutics conference; November 12–16, 2011; San Francisco, CA 2011. Abstract A195
Campone M, Bondarenko I, Brincat S, Hotko Y, Munster PN, Chmielowska E, Fumoleau P, Ward R, Bardy-Bouxin N, Leip E, Turnbull K, Zacharchuk C et al (2012) Phase II study of single-agent bosutinib, a Src/Abl tyrosine kinase inhibitor, in patients with locally advanced or metastatic breast cancer pretreated with chemotherapy. Ann Oncol 23:610–617
Talpaz M, Shah NP, Kantarjian H, Donato N, Nicoli J, Paquette R, Cortes J, O’Brien S, Nicaise C, Bleickardt E, Blackwood-Chirchir MA (2006) Dasatinib in imatinib-resistant Philadelphia chromosome-positive leukemias. N Engl J Med 354:2531–2541
Hochhaus A, Kantarjian HM, Baccarani M, Lipton JH, Apperley JF, Druker BJ, Facon T, Goldberg SL, Cervantes F, Niederwieser D, Silver RT, Stone RM et al (2007) Dasatinib induces notable hematologic and cytogenetic responses in chronic-phase chronic myeloid leukemia after failure of imatinib therapy. Blood 109:2303–2309
Kantarjian H, Pasquini R, Hamerschlak N, Rousselot P, Holowiecki J, Jootar S, Robak T, Khoroshko N, Masszi T, Skotnicki A, Hellmann A, Zaritsky A et al (2007) Dasatinib or high-dose imatinib for chronic-phase chronic myeloid leukemia after failure of first-line imatinib: a randomized phase 2 trial. Blood 109:5143–5150
Shah NP, Kantarjian HM, Kim DW, Rea D, Dorlhiac-Llacer PE, Milone JH, Vela-Ojeda J, Silver RT, Khoury HJ, Charbonnier A, Khoroshko N, Paquette RL et al (2008) Intermittent target inhibition with dasatinib 100 mg once daily preserves efficacy and improves tolerability in imatinib-resistant and -intolerant chronic-phase chronic myeloid leukemia. J Clin Oncol 26:3204–3212
Kantarjian H, Giles F, Wunderle L, Bhalla K, O’Brien S, Wassmann B, Tanaka C, Manley P, Rae P, Mietlowski W, Bochinski K, Hochhaus A et al (2006) Nilotinib in imatinib-resistant CML and Philadelphia chromosome-positive ALL. N Engl J Med 354:2542–2551
Kantarjian HM, Giles F, Gattermann N, Bhalla K, Alimena G, Palandri F, Ossenkoppele GJ, Nicolini FE, O’Brien SG, Litzow M, Bhatia R, Cervantes F et al (2007) Nilotinib (formerly AMN107), a highly selective BCR-ABL tyrosine kinase inhibitor, is effective in patients with Philadelphia chromosome-positive chronic myelogenous leukemia in chronic phase following imatinib resistance and intolerance. Blood 110:3540–3546
Quintas-Cardama A, Kantarjian H, Jones D, Nicaise C, O’Brien S, Giles F, Talpaz M, Cortes J (2007) Dasatinib (BMS-354825) is active in Philadelphia chromosome-positive chronic myelogenous leukemia after imatinib and nilotinib (AMN107) therapy failure. Blood 109:497–499
Garg RJ, Kantarjian H, O’Brien S, Quintas-Cardama A, Faderl S, Estrov Z, Cortes J (2009) The use of nilotinib or dasatinib after failure to 2 prior tyrosine kinase inhibitors: long-term follow-up. Blood 114:4361–4368
Giles FJ, Abruzzese E, Rosti G, Kim DW, Bhatia R, Bosly A, Goldberg S, Kam GL, Jagasia M, Mendrek W, Fischer T, Facon T (2010) Nilotinib is active in chronic and accelerated phase chronic myeloid leukemia following failure of imatinib and dasatinib therapy. Leukemia 24:1299–1301
Acknowledgments
Clinical studies 3160A4-200-WW and 3160A4-3000-WW were sponsored by Wyeth Research, which was acquired by Pfizer Inc in October 2009; the current pharmacokinetic–pharmacodynamic analysis was sponsored by Pfizer Inc. Poe-Hirr Hsyu and Michael Amantea are employees of and own stock in Pfizer. Diane Mould and Richard Upton are employees of Projections Research Inc and served as consultants/advisors to Pfizer through their employment. Medical writing support was provided by Janetricks N. Chebukati, PhD, of SciFluent and was funded by Pfizer Inc.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hsyu, PH., Mould, D.R., Upton, R.N. et al. Pharmacokinetic–pharmacodynamic relationship of bosutinib in patients with chronic phase chronic myeloid leukemia. Cancer Chemother Pharmacol 71, 209–218 (2013). https://doi.org/10.1007/s00280-012-1998-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-012-1998-4