Abstract
Most prospective studies of bone mineral density (BMD) in systemic lupus erythematosus (SLE) patients have been of relatively short duration, with a maximum of 6 years. To describe long-term changes in BMD in women with SLE and identify risk factors associated with BMD loss. We retrospectively evaluated 132 adult Mexican-Mestizo women with SLE who underwent dual X-ray absorptiometry (DXA). Demographic and clinical data were collected and BMD at the lumbar spine (L1–L4) and total hip were collected at baseline and during the follow up. At baseline, the mean age of participants was 43.4 ± 12.5 years, 50.8% had osteopenia and 11% osteoporosis. The median follow-up was 13 (IQR 10.2–14.0) years. During follow up, 79% of patients used glucocorticoid (GCT). The mean percentage of changes in BMD during follow up were: − 14.03 ± 11.25% (− 1.49%/year) at the lumbar spine, and − 15.77 ± 11.57% (− 1.78%/year) at the total hip, with significant changes (p < 0.001 for both comparisons). Multivariate analysis showed older age, GCT use at baseline, and transition to the menopause during the follow-up were significantly associated with greater reductions in BMD. This retrospective longitudinal study found significant BMD loss at the lumbar spine and hip. Older age, menopausal transition and GCT use were independently associated with BMD decline in women with SLE.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
International experts recommend that all individuals with systemic lupus erythematosus (SLE) should be screened and monitored for bone loss according to present guidelines for postmenopausal women and/or patients on glucocorticoid (GCT) therapy [1, 2]. Cross-sectional studies of bone mineral density (BMD) have reported that low BMD and osteoporosis are frequent in SLE patients [3,4,5,6,7]. However, few longitudinal cohort studies have evaluated BMD changes over time [8,9,10,11], with most being of short to medium duration.
Subjects with SLE, especially those with a long disease duration, are at risk of several factors such as persistent inflammation, low levels of vitamin D, decreased physical activity and GC exposure that adversely affect bone health [12]. Likewise, SLE survival rates have improved in recent decades, meaning an increase in accumulated organ damage.
Longitudinal studies of SLE patients show short-term accelerated BMD loss of 1.22–5.54% per year [8, 9], while medium-term (5–6 years) follow-up studies demonstrated relative BMD stability, with a percentage of loss ranging from 0.08 to 0.20% per year [10] and a mean overall loss of up to 2.41%, depending on the site evaluated [11]. Although the short- and medium-term effects of SLE on BMD are well described, there are no reports on the long-term effect. Therefore, the aims of the present study were to evaluate longitudinal changes in BMD in women with SLE and identify determinants associated with BMD changes.
Patients and Methods
Study Population
The study methods, particularly the baseline inclusion and exclusion criteria are described in detail in other reports [7, 13, 14]. Briefly, in this observational, longitudinal cohort study, Mexican-Mestizo women with SLE attending our outpatient clinic were consecutively enrolled. Adult patients who fulfilled the American College of Rheumatology revised classification criteria [15] and the 2012 Systemic Lupus International Collaborating Clinic (SLICC) validated criteria [16] were recruited. Exclusion criteria were renal impairment (creatinine > 2 mg/dl), pregnancy and untreated thyroid disease. The study was approved by our local ethical research committee, and informed consent acquired from participants.
Clinical Measurements
Patients were entered between 2006 and 2016. Follow-up evaluations were made between 2009 and 2020. Demographic and clinical data were documented at inclusion and during follow up by structured interview and clinical examinations. Demographic and clinical characteristics included age, body mass index (BMI), smoking (yes or no) and drinking (≥ 3 U of alcohol per day), self-reported fractures (vertebral and non-vertebral), menstrual status, disease duration and medications. Menopause was stated as amenorrhea for at least 1 year and transitional menstrual status (whether women had undergone a permanent change in menstrual status) during the follow up was also recorded. Premature menopause was defined as amenorrhea for at least 12 months at age < 40 years [17].
Disease activity was measured using the Mexican Systemic Lupus Erythematosus Disease Activity Index (mexSLEDAI), which is a validated activity index adjusted for the Mexican-Mestizo population [18]. Cumulated organ damage was evaluated using the Systemic Lupus International Collaborating Clinic/ACR Damage Index (SLICC/ACR DI) [19]. Organ damage was collected at baseline and new organ damage during the follow up was recorded. Use of medications during the follow up, including the cumulative dose of GCT, antimalarials, immunosuppressive drugs, calcium and vitamin D supplements and anti-osteoporotic agents, were collected by chart review. Oral GCT use was collected in milligram (mg)/day. The cumulative dose of GCT at baseline and follow-up were calculated as the total milligrams (mg) of prednisone plus intravenous methylprednisolone (IV MP). The dose of IV MP, in mg was multiplied by 1.25 to convert the quantity to prednisone counterparts.
At baseline, circulating levels of 25-hydroxyvitamin D (25[OH]D in μ/ml were assessed by chemiluminescent immunoassay (Abbot Architect, Wiesbaden, Germany). 25(OH)D serum level of < 20 μ/ml defined vitamin D deficiency [20].
BMD Measurements
BMD measurements at the lumbar spine and total hip were made using the same dual X-ray absorptiometry equipment (DXA) (Lunar, Prodigy densitometer, Madison, WI, USA) at baseline and during follow up. All determinations were made by experienced operators using standardised methods for patient positioning. The coefficients of variation of precision in all sites were < 1%. BMD evaluations at the lumbar spine (anteroposterior projection at L1–L4) and total hip were expressed as the grams of bone mineral per square centimetre (g/cm2). The World Health Organization (WHO) definitions to define osteopenia and osteoporosis were used to interpret the T-score (number of standard deviations [SD] from the normal mean obtained from young healthy adults) for menopausal women. Osteopenia and osteoporosis were defined as a T-score ranging from − 1 to − 2.5 and a T-score ≤ − 2.5, respectively. A Z-score number of SD from normal of − 2.0 or lower is defined as below the expected range for age and a Z-score above − 2.0 is within the expected age range for females prior to menopause according to the 2019 International Society of Clinical Densitometry (ISCD) consensus [21].
Statistical Analysis
Normally distributed continuous variables were expressed as mean ± SD and non-normally distributed variables as median and interquartile range. Categorical variables were described in percentages. Comparisons of baseline and follow-up BMD values, Z and T scores were made using a paired-sample t test. McNemar’s test was used to compare the percentages of patients with osteopenia, osteoporosis and low BMD at baseline and during follow-up. Annual BMD change was calculated in each participant as [(BMD2 − BMD1/BMD1]*100/time (in years)] between assessments. Relationships between the percentage of change in BMD and numerical variables such as age, BMI, and cumulative GCT were made using Pearson correlations. Risk factors with bivariate associations of p < 0.2 were entered in a multiple linear regression analysis. A two-tailed p value < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS Statistics for Mac V25.0 (SPSS Inc, Chicago, Ill, USA).
Results
Characteristics of Women with SLE
Of the 225 original participants, 132 had BMD measurements available at the end of follow up (Online Resource 1). The median follow up was 13.0 years (IRQ 10.2–14.0) from the first BMD measurement to the second. Baseline demographic and clinical characteristics of patients lost and those who completed the follow up are shown in Online Resource 2. Attrition analysis shows that participants who had significantly more prevalent vertebral fractures and bisphosphonate use at baseline were more likely to be lost to follow-up. However, BMD measurements were not significantly different between the two groups.
Table 1 shows the main characteristics of the 132 women with SLE included in the final analysis. Nearly half the participants were postmenopausal, with mild disease activity and a median (IQR) disease duration of 6.0 years (1.0–9.7) at inclusion. At the end of follow up, 71.6% of the participants were postmenopausal. Twenty-five patients (18.9%) had premature menopause (before 40 years). At baseline, 44.7% had organ damage and new organ damage during the follow-up was recorded in 70 patients (either no previous organ damage or increased organ damage). At inclusion, 50.8% and 11.7% of patients had osteopenia and osteoporosis, respectively. During follow-up, 79% were taking oral GCT, with a mean (SD) cumulative dose of 39.8 (22.7) g. Use of antimalarials and immunosuppressive drugs were recorded in 87.3% and 50% of patients, respectively. The most common immunosuppressants used (current or ever) were azathioprine (28%), methotrexate (18%), cyclophosphamide (8%) and mycophenolic acid (5%). Bisphosphonates (alendronate and risedronate) were administrated in 20 patients, of whom 15 had criteria for osteoporosis and five osteopenia plus either high dose prednisone and/or a history of vertebral fractures. No patients had received hormone replacement therapies. Patients with osteopenia and/or osteoporosis compared to those with normal BMD measurements at baseline were treated with bisphosphonates more frequently at the end of follow-up (40.3% vs 22.4%; p = 0.03).
Longitudinal Changes in BMD
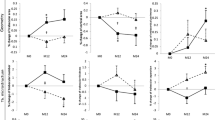
Table 2 shows BMD measurements at baseline and follow-up. The proportion of osteoporosis (in postmenopausal women) at lumbar spine was almost the double from the initial scan to the second scan. In premenopausal women at baseline, the proportion of low BMD (z-score ≤ 2) slightly increased over time only at the total hip. The mean (SD) percentage changes in BMD of the participants over a median follow up of 13 years were − 14.03 ± 11.25% (− 1.49%/year) at the lumbar spine and − 15.77 ± 11.57 (− 1.78%/year) at the total hip (both comparisons p < 0.001). A significant decrease in the T-score was seen at the lumbar spine (p < 0.001) but not at the total hip (p = 0.07; Table 2).
Risk Factors Associated with Changes in BMD
Significant negative correlations between age and BMI at baseline and the percentage change in BMD at the total hip (r = − 0.26, p = 0.002 and r = − 0.17, p = 0.04, respectively) but not for the lumbar spine (p = 0.69 and p = 0.43, respectively) were found. Menstrual status at baseline was not related to percentage change in BMD either at the lumbar spine or hip (Table 3).However, SLE women with transitional menstrual status during follow-up presented significantly higher reductions in BMD at the lumbar spine but not at the total hip. Baseline accrual damage was associated with a reduction in BMD at the total hip (p = 0.01) but not the lumbar spine (p = 0.39). The baseline lupus activity score did not correlated with BMD changes at either site (p = 0.93 and p = 0.43, respectively). New organ damage was not significantly related to BMD change either at the lumbar spine or the total hip. When baseline daily prednisone dose was correlated to BMD changes at any site, we found no significant correlations (p = 0.53 and p = 0.96, respectively). Similarly, there was no significant correlation between the cumulative SLICC at the end of follow-up and BMD loss (p = 0.35 and p = 0.82, respectively). 25[OH]D levels at baseline were not correlated with BMD changes at any site (p = 0.98 and p = 0.29, respectively).
Patients with higher daily GCT (≥ 7.5 mg for ≥ 3 months) at baseline tended to have a larger reduction in BMD, particularly at the lumbar spine, but this was not significant at the total hip (Table 3). No correlations were found between the cumulative dose of GCT and changes in BMD at any site (p = 0.06 and p = 0.031, respectively). Antimalarials and immunosuppressants were not associated with a greater decrease in BMD at the lumbar spine, but immunosuppressants were significantly associated with a lower BMD decrease at the total hip (Table 3). Bisphosphonate use at baseline was not significantly associated with BMD changes at any site (Table 3).
Multivariate Analysis of Factors Associated with BMD Changes
Table 4 shows the findings of the multivariate linear regression analysis. Transitional menstrual status and daily oral GCT ≥ 7.5 mg for ≥ 3 months at the beginning of the study were independently associated with BMD loss at the lumbar spine. Only older age at baseline was independently correlated with BMD changes at the total hip.
Discussion
To the best of our knowledge, this observational retrospective study is the longest and largest longitudinal analysis evaluating changes in BMD and potential risk factors in women with SLE. We found a significant decrease in BMD at either the lumbar spine or total hip after a median follow up of 13 years. Patients with transitional menstrual status and daily oral prednisone of ≥ 7.5 mg for ≥ 3 months had greater BMD loss at the lumbar spine. However, only older age was independently associated with BMD loss at the total hip.
Previous longitudinal reports on repeated BMD determinations in patients with SLE have shown mean annual rates of bone loss of between − 0.08% and − 4.2% at the lumbar spine and − 0.2% to − 3.59% at the total hip [8,9,10,11, 22,23,24,25]. The magnitude of annual bone loss at the lumbar spine (− 1.49%) and total hip (− 1.78%) in our study did not differ from previous reports from lupus cohort with different ethnic backgrounds. Studies longitudinally evaluating BMD loss in Mexican or Latin America populations are lacking; however, a Mexican study, that included persons aged > 50 years, reported the incidence increased by 1% per year between 2000 and 2006, similar to other countries [26].
Some traditional risk factors for osteoporosis, such as menopause and transitional menopause, have been associated with BMD loss in patients with SLE [11, 25]. We confirm that transitional menopause, which was present in 33 patients during the follow up, was associated with BMD decline at the lumbar spine. Menstrual transition is a crucial phase in the modification of bone strength in women, and determines the period for the development of osteoporosis and fracture risk at older ages [27]. Menstrual transition is accompanied by changes in oestrogens resulting in bone remodelling. It has been suggested that menstrual transition is a time-limited window of opportunity for interventions to prevent rapid bone decline and microarchitectural damage to avoid osteoporosis in later years [28]. Although bone loss at the total hip was higher in patients with transitional menstrual status than in those without, the difference was not significant. The reasons for this finding are unclear. In the same context, the impact of premature menopause on bone loss, for which patients with SLE are at higher risk [17] has been associated with a higher 10-year probability of fracture [29], but we found that BMD changes did not differ between patients with and without premature menopause. The reasons for this finding are unclear. As expected, age correlated with bone loss, particularly at the total hip.
We also analysed disease-related factors, as have previous studies. Some cross-sectional and longitudinal studies have identified a relationship between organ damage and reduced BMD [5, 11, 30]. A recent longitudinal study found that new organ damage during follow up was associated with bone decline at the total hip and femoral neck [11]. In our study, patients with organ damage at baseline had a greater BMD reduction than those without, but this association was lost in the multivariate regression analysis. Other factors, like older age and GCT use were potential confounders in this relationship. In cross-sectional studies, some contradictory results on the link between GCs and BMD loss in SLE have been described [31]. A systematic review and meta-analysis of cross-sectional studies found no association between GCT and reduced BMD [32]. However, more recent longitudinal analyses have consistently reported that bone loss occurs predominantly in patients with SLE treated with GCT [8, 10, 11, 24]. Our long-term follow up showed that patients treated at baseline with ≥ 7.5 mg of prednisone daily had greater reduction in BMD at the lumbar spine in the multivariate analysis. This may be because GCT particularly affect areas with trabecular bone such as the spine [33].
BMD loss and the risk of fractures can be prevented in patients with SLE. Guidelines for the screening and management of GCT-induced osteoporosis have been reported from different countries and/or medical societies. Many guidelines address users of long-term (3 months) oral GCT, and the daily threshold dose ranges between 5 and 7.5 mg daily of prednisone or equivalent. Some guidelines highlight the relevance of initiating protective bone treatment early in high-risk subjects (BMD T-score ≤ − 2.5, or 10 year fracture probability of ≥ 20% (major osteoporotic fracture) or ≥ 3% (hip fracture) [34, 35]. However, it has been reported that care according to quality indicators for osteoporosis in SLE is suboptimal [36, 37]. Although our study was not designed to identify optimal therapies in the prevention and treatment of osteoporosis/osteopenia due mainly to the retrospective design and restricted sample size, we cannot rule out the possibility of suboptimal prevention/treatment in our cohort since most patients were under glucocorticoid therapy and only around one third were taking bisphosphonates at the end of follow up. Various factors that might influence the quality of care have been analysed [38].
The influence of hydroxychloroquine (HCQ) on bone mass is unclear. HCQ use has been associated with increased BMD in both the lumbar spine [39, 40] and hip [39] according to evidence from cross-sectional studies in women with SLE. However, a study (also cross-sectional) in male SLE patients described significantly lower BMD in the lumbar spine and hip in patients who had received HCQ compared with those who had not [41]. A 6-year Dutch prospective study demonstrated a significant decrease in hip BMD in patients receiving HCQ [10], but a 5-year longitudinal study in Chinese SLE patients found no impact on bone mass [11]. We found that patients receiving antimalarials (either HCQ or chloroquine) at baseline had a non-significantly higher BMD at both sites (lumbar spine and total hip) than those who did not. Although HCQ regulate the conversion of 25(OH)D to 1,25(OH)2D by inhibiting hydroxylation α1 [42], both chloroquine and HCQ prevent TRAF3 (tumour necrosis factor receptor associated factor 3) degradation in osteoclast precursors and inhibit osteoclast formation in vitro [43, 44]. Thus, the role of antimalarials on the bone balance in SLE patients need to be clarified in larger longitudinal studies.
In our study, patients receiving immunosuppressive agents at baseline had a non-significantly lower BMD reduction over time at both sites than those who did not. Immunosuppressive therapy may reduce inflammation-induced bone loss and minimize the dose and duration of GC treatment. A previous longitudinal study reported that immunosuppressive agents were associated with BMD gain at the hip [10].
Our study has several limitations. First, it was a retrospective analysis and BMD measurements were collected only at baseline and at the end of follow-up, with no annual or periodic evaluation during the follow-up, meaning a more accurate assessment of BMD changes over time was not recorded. In addition, in our study, the definition of menopause was based on only clinical criteria, without evaluation of hormone levels to confirm the menopausal status, since it was not possible to retrospectively collect these measurements in all participants.
Secondly, lupus activity may influence bone loss: in our retrospective evaluation, the total number of flares during the long follow up was incompletely recorded in many cases, making their evaluation difficult to include as a risk factor for BMD changes, even though this would have enriched the longitudinal analysis. Thirdly, most of the patients had mild SLE disease activity at study entry, and therefore our findings should not be generalized to other SLE patients with more-severe lupus. Moreover, all participants were Mexican-Mestizo, also limiting the generalizability of the results to patients with other ethnic backgrounds. Fourthly, not all patients underwent DXA measurements at the femoral neck and the percentage of missing data were relatively high, limiting the analysis of this BMD site. Fifthly, attrition bias can not be ruled out, since patients lost during the follow up were not significantly older but had more prevalent vertebral fractures at baseline. In addition, we cannot be certain that patients with more-severe disease were not lost to follow-up, adding a higher risk of bias. Finally, it was not a prospective randomised study, so many other confounders such as vitamin D levels and modifications over time were difficult to obtain.
In conclusion, BMD changes at the lumbar spine and the total hip over a period of > 10 years was shown in women with SLE. Older age, menopausal transition and GCT use contributed independently to BMD decline. Our analysis supports the relevance of attempting to reduce GCT use in patients with SLE. In addition, screening and preventive measures according to validated guidelines should be used, particularly in patients transiting to the menopause.
References
Mosca M, Tani C, Aringer M, Bombardieri S, Boumpas D, Brey R et al (2010) European League Against Rheumatism recommendations for monitoring patients with systemic lupus erythematosus in clinical practice and in observational studies. Ann Rheum Dis 69:1269–1274. https://doi.org/10.1136/ard.2009.117200
Keeling SO, Alabdurubalnabi Z, Avina-Zubieta A, Barr S, Bergeron L, Bernatsky S et al (2018) Canadian Rheumatology Association recommendations for the assessment and monitoring of systemic lupus erythematosus. J Rheumatol 45:1426–1439. https://doi.org/10.3899/jrheum.171459
Kalla AA, Fataar AB, Jessop SJ, Bewerunge L (1993) Loss of trabecular bone mineral density in systemic lupus erythematosus. Arthritis Rheum 36:1726–1734
Pineau CA, Urowitz MB, Fortin PJ et al (2004) Osteoporosis in systemic lupus erythematosus: factors associated with referral for bone mineral density studies, prevalence of osteoporosis and factors associated with reduced bone density. Lupus 13:436–441. https://doi.org/10.1191/0961203303lu1036oa
Almehed K, Forsblad d’Elia H, Kvist G, Ohlsson C, Carlsten H (2007) Prevalence and risk factors of osteoporosis in female SLE patients—extended report. Rheumatology 46:1185–1190. https://doi.org/10.1093/rheumatology/kem105
Bultink IEM, Lems WF, Kostense PJ, Dijkmans B, Voskuyl AE (2005) Prevalence of and risk factors for low bone mineral density and vertebral fractures in patients with systemic lupus erythematosus. Arthritis Rheum 52:2044–2050. https://doi.org/10.1002/art.21110
Mendoza-Pinto C, García-Carrasco M, Sandoval-Cruz H, Escárcega RO, Jiménez-Hernández M, Etchegaray-Morales I et al (2009) Risks factors for low bone mineral density in pre-menopausal Mexican women with systemic lupus erythematosus. Clin Rheumatol. https://doi.org/10.1007/s10067-008-0984-z
Jardinet D, Lefebvre C, Depresseux G et al (2000) Longitudinal analysis of bone mineral density in pre-menopausal female systemic lupus erythematosus patients: deleterious role of glucocorticoid therapy at the lumbar spine. Rheumatology (Oxford, England) 39:389–392
Boyanov M, Robeva R, Popivanov P (2003) Bone mineral density changes in women with systemic lupus erythematosus. Clin Rheumatol 22:318–323. https://doi.org/10.1007/s10067-003-0743-0
Jacobs J, Korswagen LA, Schilder AM, Van Tuyl LH, Dijkmans BAC, Lems WF et al (2013) Six-year follow-up study of bone mineral density in patients with systemic lupus erythematosus. Osteoporos Int 24:1827–1833. https://doi.org/10.1007/s00198-012-2157-9
Zhu TY, Griffith JF, Au S-K, Tang X-L, Kwok AW, Leung P-C et al (2014) Bone mineral density change in systemic lupus erythematosus: a 5-year followup study. J Rheumatol 41:1990–1997. https://doi.org/10.3899/jrheum.131190
Bultink IEM, Lems WF (2015) Systemic lupus erythematosus and fractures. RMD Open 1:e000069. https://doi.org/10.1136/rmdopen-2015-000069
Mendoza-Pinto C, García-Carrasco M, Sandoval-Cruz H, Muñoz-Guarneros M, Escárcega RO, Jiménez-Hernández M et al (2009) Risk factors of vertebral fractures in women with systemic lupus erythematosus. Clin Rheumatol 28:579–585. https://doi.org/10.1007/s10067-009-1105-3
García-Carrasco M, Mendoza-Pinto C, León-Vázquez ML, Méndez-Martínez S, Etchegaray-Morales I, Montiel-Jarquín Á et al (2017) Incidence of vertebral fractures in women with systemic lupus erythematosus after 8 years of follow-up. Calcif Tissue Int. https://doi.org/10.1007/s00223-017-0286-z
Hochberg MC (1997) Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40:1725. https://doi.org/10.1002/art.1780400928
Petri M, Orbai A-M, Alarcón GS et al (2012) Derivation and validation of the systemic lupus international collaborating clinics classification criteria for systemic lupus erythematosus. Arthritis Rheum 64:2677–2686. https://doi.org/10.1002/art.34473.Derivation
Ceccarelli F, Orefice V, Perrone G, Pirone C, Perricone C, Truglia S et al (2020) Premature ovarian failure in patients affected by systemic lupus erythematosus: a cross-sectional study. Clin Exp Rheumatol 38:450–454
Guzman J, Cardiel MH, Arce-Salinas A, Sanchez-Guerrero J, Alarcon-Segovia D (1992) Measurement of disease activity in systemic lupus erythematosus. Prospective validation of 3 clinical indices. J Rheumatol 19:1551–1558
Gladman DD, Goldsmith CH, Urowitz MB, Bacon P, Fortin P, Ginzler E et al (2000) The systemic lupus International Collaborating Clinics/American College of Rheumatology (SLICC/ACR) Damage Index for Systemic Lupus Erythematosus International Comparison. J Rheumatol 27:373–376
Holick MF (2007) Vitamin D deficiency. N Engl J Med 357:266–281. https://doi.org/10.1136/bmj.318.7193.1284a
Shuhart CR, Yeap SS, Anderson PA, Jankowski LG, Lewiecki EM, Morse LR et al (2019) Executive summary of the 2019 ISCD position development conference on monitoring treatment, DXA cross-calibration and least significant change, spinal cord injury, peri-prosthetic and orthopedic bone health, transgender medicine, and pediatrics. J Clin Densitom Off J Int Soc Clin Densitom 22:453–471. https://doi.org/10.1016/j.jocd.2019.07.001
Pons F, Peris P, Guañabens N, Font J, Huguet M, Espinosa G et al (1995) The effect of systemic lupus erythematosus and long-term steroid therapy on bone mass in pre-menopausal women. Br J Rheumatol 34:742–746. https://doi.org/10.1093/rheumatology/34.8.742
Hansen M, Halberg P, Kollerup G, Pedersen-Zbinden B, Hørslev-Petersen K, Hyldstrup L et al (1998) Bone metabolism in patients with systemic lupus erythematosus. Effect of disease activity and glucocorticoid treatment. Scand J Rheumatol 27:197–206. https://doi.org/10.1080/030097498440813
Kipen Y, Briganti EM, Strauss BJ, Littlejohn GO, Morand EF (1999) Three year follow-up of body composition changes in pre-menopausal women with systemic lupus erythematosus. Rheumatology (Oxford) 38:59–65. https://doi.org/10.1093/rheumatology/38.1.59
Ho SC, Chan SG, Yip YB, Chan CSY, Woo JLF, Sham A (2008) Change in bone mineral density and its determinants in pre- and perimenopausal Chinese women: the Hong Kong Perimenopausal Women Osteoporosis Study. Osteoporos Int J Establ Result Coop Between Eur Found Osteoporos Natl Osteoporos Found USA 19:1785–1796. https://doi.org/10.1007/s00198-008-0614-2
Johansson H, Clark P, Carlos F, Oden A, McCloskey EV, Kanis JA (2011) Increasing age- and sex-specific rates of hip fracture in Mexico: a survey of the Mexican institute of social security. Osteoporos Int 22:2359–2364. https://doi.org/10.1007/s00198-010-1475-z
Karlamangla AS, Burnett-Bowie S-AM, Crandall CJ (2018) Bone health during the menopause transition and beyond. Obstet Gynecol Clin N Am 45:695–708. https://doi.org/10.1016/j.ogc.2018.07.012
Camacho PM, Petak SM, Binkley N, Clarke BL, Harris ST, Hurley DL et al (2016) American Association of Clinical Endocrinologists and American College of Endocrinology Clinical Practice Guidelines for the diagnosis and treatment of postmenopausal osteoporosis—2016. Endocr Pract Off J Am Coll Endocrinol Am Assoc Clin Endocrinol 22:1–42. https://doi.org/10.4158/EP161435.GL
Mak A, Lim JQ, Liu Y, Cheak AA, Ho RC (2013) Significantly higher estimated 10-year probability of fracture in lupus patients with bone mineral density comparable to that of healthy individuals. Rheumatol Int 33:299–307. https://doi.org/10.1007/s00296-012-2389-1
Lee C, Almagor O, Dunlop DD, Manzi S, Spies S, Chadha AB et al (2006) Disease damage and low bone mineral density: an analysis of women with systemic lupus erythematosus ever and never receiving corticosteroids. Rheumatology (Oxford) 45:53–60. https://doi.org/10.1093/rheumatology/kei079
Bultink IEM (2018) Bone disease in connective tissue disease/systemic lupus erythematosus. Calcif Tissue Int 102:575–591. https://doi.org/10.1007/s00223-017-0322-z
Mendoza-Pinto C, Rojas-Villarraga A, Molano-González N, Jiménez-Herrera EA, León-Vázquez ML, Montiel-Jarquín Á et al (2018) Bone mineral density and vertebral fractures in patients with systemic lupus erythematosus: a systematic review and meta-regression. PloS One 13:e0196113. https://doi.org/10.1371/journal.pone.0196113
McCloskey EV, Odén A, Harvey NC, Leslie WD, Hans D, Johansson H et al (2016) A meta-analysis of trabecular bone score in fracture risk prediction and its relationship to FRAX. J Bone Miner Res Off J Am Soc Bone Miner Res 31:940–948. https://doi.org/10.1002/jbmr.2734
Buckley L, Guyatt G, Fink HA, Cannon M, Grossman J, Hansen KE et al (2017) 2017 American College of Rheumatology Guideline for the prevention and treatment of glucocorticoid-induced osteoporosis. Arthritis Care Res 69:1095–1110. https://doi.org/10.1002/acr.23279
Compston J, Cooper A, Cooper C, Gittoes N, Gregson C, Harvey N et al (2017) UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos 12:43. https://doi.org/10.1007/s11657-017-0324-5
Demas KL, Keenan BT, Solomon DH, Yazdany J, Costenbader KH (2010) Osteoporosis and cardiovascular disease care in systemic lupus erythematosus according to new quality indicators. Semin Arthritis Rheum 40:193–200. https://doi.org/10.1016/j.semarthrit.2010.01.001
Schmajuk G, Yelin E, Chakravarty E, Nelson LM, Panopolis P, Yazdany J (2010) Osteoporosis screening, prevention, and treatment in systemic lupus erythematosus: application of the systemic lupus erythematosus quality indicators. Arthritis Care Res 62:993–1001. https://doi.org/10.1002/acr.20150
Casey C, Chung CP, Crofford LJ, Barnado A (2017) Rheumatologists’ perception of systemic lupus erythematosus quality indicators: significant interest and perceived barriers. Clin Rheumatol 36:97–102. https://doi.org/10.1007/s10067-016-3487-3
Lakshminarayanan S, Walsh S, Mohanraj M, Rothfield N (2001) Factors associated with low bone mineral density in female patients with systemic lupus erythematosus. J Rheumatol 28:102–108
Mok CC, Mak A, Ma KM (2005) Bone mineral density in postmenopausal Chinese patients with systemic lupus erythematosus. Lupus 14:106–112. https://doi.org/10.1191/0961203305lu2039oa
Mok CC, Ying SKY, To CH, Ma KM (2008) Bone mineral density and body composition in men with systemic lupus erythematosus: a case control study. Bone 43:327–331. https://doi.org/10.1016/j.bone.2008.04.003
Huisman AM, White KP, Algra A, Harth M, Vieth R, Jacobs JW et al (2001) Vitamin D levels in women with systemic lupus erythematosus and fibromyalgia. J Rheumatol 28:2535–2539
Xiu Y, Xu H, Zhao C, Li J, Morita Y, Yao Z et al (2014) Chloroquine reduces osteoclastogenesis in murine osteoporosis by preventing TRAF3 degradation. J Clin Investig 124:297–310. https://doi.org/10.1172/JCI66947
Both T, Zillikens MC, Schreuders-Koedam M, Vis M, Lam W-K, Weel AEAM et al (2018) Hydroxychloroquine affects bone resorption both in vitro and in vivo. J Cell Physiol 233:1424–1433. https://doi.org/10.1002/jcp.26028
Acknowledgements
The authors thank all patients who participated in the study, which was, in part, supported by a grant from CONCYTEP (Consejo de Ciencia y Tecnologia del Estado de Puebla).
Funding
This study was partly supported by grant from FIS/IMSS/PROT 2018-2106-47. This funding source had no role in the design and conduct of the study, the collection, analysis, and interpretation of the data, or the preparation, review, or approval of the manuscript.
Author information
Authors and Affiliations
Contributions
CMP, MGC, DJM and PMR contributed to the conception and design of the study and wrote and revised the manuscript. DJM, PMR and MNS, IEM contributed to data collection and analysis. CMP and DMJ made the statistical analysis. IEM, JAA and SMM revised the manuscript. All authors contributed to the critical revision and approved the final version for publication.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest with respect to the content of the manuscript. Outside the submitted work, Dr García-Carrasco reports royalty payments from UCB for the publication of books/chapters. The remaining authors have no conflict of interests.
Human and Animal Rights and Informed Consent
The study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Local Ethics Committee, IMSS (R-2018-2106-035).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mendoza-Pinto, C., García-Carrasco, M., Juárez-Melchor, D. et al. A Retrospective Analysis of Longitudinal Changes in Bone Mineral Density in Women with Systemic Lupus Erythematosus. Calcif Tissue Int 109, 363–371 (2021). https://doi.org/10.1007/s00223-021-00845-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-021-00845-0