Abstract
Summary
In this study, we characterized longitudinal changes of volumetric bone mineral density and cortical and trabecular microstructure at the distal radius using HR-pQCT in female systemic lupus erythematosus (SLE) patients on long-term glucocorticoids. Cortical thinning and increased cortical porosity are the major features of longitudinal microstructural deterioration in SLE patients.
Introduction
The study aims to characterize longitudinal changes of volumetric bone mineral density (vBMD) and bone microstructure at distal radius in female systemic lupus erythematosus (SLE) patients on long-term glucocorticoids.
Methods
This 2-year case-control study consisted of 166 premenopausal subjects (75 SLE patients and 91 controls) and 79 postmenopausal subjects (44 SLE patients and 35 controls). We obtained areal BMD (aBMD) by dual-energy X-ray absorptiometry at multiple skeletal sites and indices of vBMD and microstructure at distal radius by high-resolution peripheral quantitative computed tomography (HR-pQCT) at baseline, 12 and 24 months.
Results
In either premenopausal or postmenopausal subjects, changes in aBMD did not differ between patients and controls except that decrease in aBMD at total hip at 24 months in premenopausal patients was significantly higher. In premenopausal subjects, decrease in cortical area (−0.51 vs. −0.06 %, p = 0.039) and thickness (−0.63 vs. 0.02 %, p = 0.031) and increase in cortical porosity (21.7 vs. 7.16 %, p = 0.030) over study period were significantly larger in patients after adjustment of age and body mass index. Decreased in trabecular vBMD was significantly less (−0.63 vs. −2.32 %, p = 0.001) with trabecular microstructure better maintained in patients. In postmenopausal subjects, decrease in cortical vBMD (−2.66 vs. −1.56 %, p = 0.039) and increase in cortical porosity (41.6 vs. 16.3 %, p = 0.021) were significantly higher in patients, and there was no group-wise difference in change of trabecular microstructure.
Conclusion
Longitudinal microstructural deterioration in SLE is characterized by cortical thinning and increased cortical porosity. Cortical bone is an important source of bone loss in SLE patients on glucocorticoids.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Systemic lupus erythematosus (SLE) is a chronic debilitating autoimmune disease with heterogeneous manifestations that can involve multiple organ systems simultaneously or sequentially [1]. SLE predominantly affects females of childbearing age and over time, uncontrolled disease activity leads to irreversible organ damage [2]. Osteoporosis is a common and important comorbidity associated with SLE. SLE patients are at a heightened risk of osteoporosis for various reasons, including active inflammation, use of glucocorticoids, biochemical abnormalities, and decreased physical activity [3]. These factors have become more prominent with improved survival of SLE in the past 5 decades [2].
Areal bone mineral density (aBMD) obtained by dual-energy X-ray absorptiometry (DXA) is currently the standard imaging technique used to define osteoporosis and assess fracture risk. Although aBMD explains approximately 70 % of bone strength, fragility fractures occur frequently in the absence of osteoporotic aBMD in SLE patients [4, 5]. As a two-dimensional projectional imaging technique, aBMD reveals little regarding compartmental differences in bone mass and other structural features critical to the maintenance of bone strength [6]. High-resolution peripheral quantitative computed tomography (HR-pQCT) is a dedicated peripheral imaging technique capable of in vivo quantification of compartmental volumetric BMD (vBMD) and microstructure at the distal radius and tibia [7]. Several clinical studies have shown that HR-pQCT reveals bone microstructural features that can improve both fracture discrimination [8] and the monitoring of therapeutic effect [9, 10].
We previous reported a cross-sectional HR-pQCT study in a group of Chinese female SLE patients on long-term glucocorticoids and a group of age-matched female controls without SLE [11]. Our results showed that microstructural deficits at the distal radius in SLE predominantly occurred in the cortical compartment with thinner cortices and higher cortical porosity [11]. These deficits were most pronounced in patients with organ damage [11–13]. Prospective studies investigating longitudinal bone loss in SLE patients are scanty, and bone loss could not be specifically attributed to SLE disease as none of these studies employed a matched control group [14–17].
To address these questions, in this 2-year case-control longitudinal study, HR-pQCT was used to evaluate changes of vBMD and cortical and trabecular microstructure at the distal radius in female SLE patients on long-term glucocorticoids. Our aims were (1) to characterize longitudinal changes of compartmental bone density, geometry, and microstructure in Chinese female SLE patients on long-term glucocorticoids and to compare these changes with those seen in age-matched females without SLE, and (2) to investigate the relationship between these changes and disease characteristics including organ damage and use of glucocorticoids.
Materials and methods
Subjects
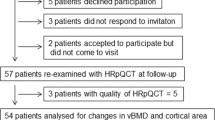
A cohort of Chinese female SLE patients were recruited from the outpatient rheumatology clinics at the Prince of Wales Hospital and Alice Ho Miu Ling Nethersole Hospital, Hong Kong, and a cohort of age-matched (±3 years) females without SLE were invited from the hospital staff and local community as the control group. The detailed baseline characteristics of this study cohort have been reported elsewhere [11]. All SLE patients fulfilled the American College of Rheumatology revised criteria for the classification of SLE [18] and were receiving oral glucocorticoids of not less than 5 mg daily (prednisolone-equivalent) continuously for at least 1 year prior to the entry of the study. Exclusion criteria were as follows: (1) history of a disorder that could affect bone metabolism, including chronic renal impairment (chronic kidney disease stage IV or V), type 1 DM, unstable cardiovascular disease, thyroid or parathyroid disease, malignancy, or chronic liver disease; (2) history of using thyroid or parathyroid hormone, anti-osteoporosis therapy including anti-resorptive drugs, calcitonin, fluoride, estrogen, or selective estrogen receptor modulator; and (3) pregnant or breastfeeding. Age-matched female controls were subjected to the above exclusion criteria and, in addition, had no history of any autoimmune disease and had no history of use of glucocorticoids. Calcium and vitamin supplements were allowed for patients and controls. A total of 149 SLE patients and 139 controls agreed to participate in this 2-year longitudinal study and received annual assessments by DXA and HR-pQCT. In order to exclude the drastic effect of the event of menopause, participants who had undergone change from premenopausal to postmenopausal status during the study period (12 patients and 13 controls) were excluded from the longitudinal analyses. During the study period, glucocorticoids were stopped in five patients, and 13 patients received anti-osteoporosis therapies (bisphosphonates). These patients were further excluded from the longitudinal analyses. No controls received anti-osteoporosis therapies during the study period. The final cohort for the current study therefore consisted of 119 SLE patients and 126 controls (66 and 70 %, respectively, of the baseline cohort). The study was approved by the Joint Chinese University of Hong Kong—New Territories East Cluster Clinical Research Ethics Committee with written informed consent obtained from all study subjects.
Assessment of demographics and disease characteristics
The following demographics were recorded: age, body weight, body height, menopausal status, smoking, and drinking habit. Body mass index (BMI) was calculated. Menopause was defined as amenorrhea for at least one complete year and the age of menopause as the age of the last menstrual flow of any amount.
At baseline, disease activity was measured by the SLE Disease Activity Index (SLEDAI), with a higher score indicating higher disease activity [19]. Cumulated organ damage was measured by the Systemic Lupus International Collaborating Clinics/American College of Rheumatology Damage Index (SDI), with a higher score indicating more organ damage [20]. Cumulative dose and duration of oral glucocorticoids were calculated since onset of disease until entry to the study. All doses of oral glucocorticoids were prednisolone-equivalent.
Assessment by DXA
aBMD of the hip (total left hip and femoral neck), lumbar spine (L1–L4), and ultradistal radius of the nondominant forearm was performed on a standard DXA system (Hologic Delphi W, Bedford, MA, USA) at baseline, 12 and 24 months. aBMD of the hip could not be performed in one SLE patients due to bilateral hip replacements, while two controls did not undergo DXA scan at 24 months. DXA scan of the ultradistal radius spanned for 15 mm starting 10 mm proximal to the ulnar tip. Follow-up measures were obtained on the same scanner for each subject. aBMD results were expressed in grams per squared centimeters. Changes at 12 and 24 months were expressed as the percentage difference from baseline and compared between groups in premenopausal and postmenopausal subjects, respectively. Our short-term precision error of aBMD by DXA, expressed as the root mean square coefficient of variance (RMSCV), ranges from 0.72 to 1.5 % [21].
Assessment by HR-pQCT
Imaging and image registration
Cross-sectional geometry, vBMD, and microstructure were measured at the distal radius of the nondominant forearm using HR-pQCT (Scanco Medical AG, Brüttisellen, Switzerland) at baseline, 12 and 24 months. The participant’s forearm was immobilized in a carbon fiber cast, and a dorsal-palmer projection image was obtained to define the tomographic scan region. The scan region was fixed 9.5 mm proximal from the mid-joint line and spanned 9.02 mm proximally in length, equivalent to a stack of 110 slices. All longitudinal image analyses were subjected to the same volume of interest (VOI) matching the baseline, 12- and 24-months measurements. Identification of the same region was conducted using the software provided by the manufacturer, which matches corresponding images by their total cross-section area. Only the bone volume common to the baseline, 12- and 24-months measurements, was used for the image analyses. The average number of slices utilized for longitudinal image analyses was 104 (range 93–109) slices per subject with an average common region of 93.4 (range 84–99 %). Changes at 12 and 24 months for all parameters were expressed as the percentage difference from baseline and compared between groups in premenopausal and postmenopausal subjects, respectively.
Standard analysis
Evaluation of 3D scan data was performed by Image Processing Language (IPL v5.08b, Scanco Medical AG, Brüttisellen, Switzerland). Images were first analyzed using a standard evaluation protocol [7]. The entire VOI was automatically separated into cortical and trabecular region using a threshold-based algorithm. The threshold used to discriminate cortical from trabecular bone was set to one third of the apparent cortical density value. By this segmentation, we obtained cross-sectional area for cortical and trabecular bone (mm2). Cortical thickness was calculated as the mean cortical volume divided by the outer bone surface. Integral and trabecular vBMD in milligram hydroxyapatite (HA) per cubic centimeter was computed as the average mineral density within the entire and trabecular VOI, respectively. The trabecular compartment was divided into two subregions: inner 60 % subregion located at the central medullary cavity and outer 40 % subregion located adjacent to the cortex. Trabecular bone volume fraction (BV/TV) was derived from trabecular vBMD assuming a fixed mineralization of 1.2 g HA/cm3. Trabecular number was defined as the mean inverse distance between 3D ridges (the centroid of trabeculae). Trabecular thickness and separation were then derived from BV/TV and trabecular number using standard stereological relations. Our short-term HR-pQCT reproducibility, expressed as RMSCV, ranged from 0.38 to 1.03 % for density measures, from 0.28 to 1.10 % for geometric measures, and from 1.72 to 3.73 % for microstructural measures [22].
Extended cortical bone analyses
The cortical bone analyses obtained from the standard evaluation protocol have been reported to perform poorly for subjects with very thin or porous cortices, and the coarse segmentation precludes quantification of intracortical porosity, which is an important determinant of cortical microstructure [23, 24]. Therefore, a fully automated cortical compartment segmentation technique adapted from the algorithm described by Buie et al [23] was applied [25]. The software for the extended cortical bone analyses was implemented within the manufacturer’s IPL and was incorporated via extension into the manufacturer’s visualization (μCT Evaluation v6.0, Scanco Medical AG) and analysis software [25]. Based on this segmentation, cortical vBMD was calculated as the mean mineralization value for all voxels in the cortical VOI. A volumetric index of intracortical porosity, denoted Ct.Po (%), was calculated based on the cortical pore volume (Ct. PoV) and the mineralized intracortical bone volume (Ct. BV): Ct. Po = Ct. PoV / (Ct. PoV + Ct. BV). In addition, a direct 3D calculation of cortical thickness, namely apparent cortical thickness, was performed on composite segmentations of the mineralized cortex and porosity, disregarding intracortical pore surfaces in the calculations. This apparent cortical thickness represents a direct 3D measure of endosteal-periosteal distance.
Statistical analyses
Statistical analyses were performed using the IBM Statistics Package for Social Sciences (IBM SPSS Statistics 20, SPSS Inc, Chicago, IL, USA). Demographics of SLE patients and controls were compared using Student’s t test or Mann-Whitney U test or chi-square test depending on the type and distribution of the data. Analyses of time-related changes were performed in premenopausal and postmenopausal subjects, separately. Changes at 12 and 24 months for all parameters were expressed as the percentage difference from baseline. Statistical significance of the changes with respect to baseline of all parameters and group-wise differences in these changes was analyzed using repeated measure analysis of variance (RMANOVA) with Bonferroni-corrected pairwise comparisons. Normality was tested for all parameters. For nonnormally distributed parameters (trabecular separation, cortical pore volume, Ct.Po), transformation was performed by box-cox analysis to assume normality. Between-group differences in percentage changes were further adjusted by age and BMI in premenopausal subjects and adjusted by age, BMI, and age of menopause in postmenopausal subjects. Correlations between percentage changes in vBMD, geometric and microstructural indices, and indices of disease characteristics, including disease duration, organ damage, and use of glucocorticoids, were analyzed using Spearman’s correlation and were performed in all SLE patients. All hypotheses were two-tailed, and a p < 0.05 was considered statistically significant.
Results
Demographics and disease characteristics
Table 1 shows the baseline demographics and disease characteristics of the study subjects. The study cohort consisted of middle-aged females. One hundred and sixty-six subjects were premenopausal (75 SLE patients and 91 controls), and 79 subjects were postmenopausal (44 SLE patients and 35 controls). The percentage of postmenopause did not differ between patients and controls (37 vs. 27.8 %, p = 0.124). In either premenopausal or postmenopausal subjects, SLE patients were significantly younger than controls and BMI was significantly lower in SLE patients. Menopause occurred at a significantly younger age in patients. Smoking and drinking habit did not differ between the two groups. At baseline, the mean (SD) disease duration of all SLE patients was 11.8 years (6.9). Disease activity at baseline was low. The most common organ damage was ocular (10.9 %), neuropsychiatric (10.1 %), and renal (6.7 %) damage. Four (3.4 %) patients had musculoskeletal damage at baseline. All patients were on oral glucocorticoids at baseline with a median daily dose of 5 mg, a median cumulative dose of 19.7 g, and a median duration of 9.8 years.
During the study period, new organ damage occurred in 12 (10.9 %) of 119 SLE patients (Table 1). The most common new organ damage was ocular damage (four patients), skin damage (four patients), and neuropsychiatric damage (two patients). All patients received oral glucocorticoids during the study period with a median cumulative dose of 4.1 g (prednisolone-equivalent). One hundred and thirteen (95 %) patients received calcium supplement and/or vitamin D during the study period. Twenty-two (17.5 %) controls reported use of calcium and/or vitamin D supplement, and no control received anti-osteoporotic therapy during the study period.
Premenopausal subjects
Change of aBMD
In SLE patients, there was no significant overtime change of aBMD at the femoral neck, total hip, lumbar spine, or ultradistal radius (Table 2). In controls, increase in aBMD at the total hip (0.38 %, p = 0.030) and lumbar spine (0.72 %, p = 0.002) at 12 months, as well as decrease in aBMD at the ultradistal radius (−1.84 %, p < 0.0001) at 24 months was significant. There was significant group-wise difference in change of aBMD at the total hip at 24 months (patients vs. controls: −0.58 vs. 0.17 %, p = 0.045), and such difference remained significant after adjustment of age and BMI (p = 0.043). Otherwise, there was no group-wise difference in changes of aBMD.
Changes of vBMD
In SLE patients, at 12 months, there were small but significant increases in integral, trabecular, and cortical vBMD (0.28 to 0.72 %, all p < 0.05) (Fig. 1). However, at 24 months, integral vBMD decreased significantly from baseline (−0.71 %, p = 0.004), while trabecular and cortical vBMD returned to baseline levels (both p > 0.05). In controls, integral, trabecular, and cortical vBMD decreased significantly at 24 months (−0.42 to −2.32 %, all p < 0.0001). At 12 months, there was also a small increase in cortical vBMD (0.29 %, p = 0.002). Group-wise difference was only observed in changes of trabecular vBMD. Decrease in trabecular vBMD was significantly less in patients than in controls for the whole region (0.72 vs. −0.39 % at 12 months, −0.63 vs. −2.32 % at 24 months, both p = 0.001), the outer subregion (0.83 vs. −0.25 % at 12 months, −0.61 vs. −2.09 % at 24 months, both p < 0.0001), and the inner subregion (0.61 vs. −0.64 % at 12 months, −0.63 vs. −2.7 % at 24 months, both p < 0.05). These differences remained significant after adjustment of age and BMI.
Plots of average percentage change at 12 and 24 months of indices of volumetric bone mineral density (vBMD), geometry, trabecular (Tb.), and cortical (Ct.) microstructure in premenopausal systemic lupus erythematosus (SLE) patients (solid line, black box) and premenopausal controls (dotted line, open triangle). Bars represent standard error of means. *p < 0.05 compared with baseline of respective group. †p < 0.05 between SLE patients and controls. ‡p < 0.05 after adjustment of age and body mass index
Changes of bone geometry
In SLE patients, trabecular area increased and cortical area decreased over the study period, with significant changes seen at 12 months (0.13 and −0.46 %, respectively, both p < 0.05) (Fig. 1). Endocortical perimeter increased significantly at 24 months in patients (0.23 %, p = 0.001). In contrast, there was no significant overtime changes in bone geometry over the study period in controls. Increase in trabecular area and decrease in cortical area were significantly larger in patients at 12 months, and such differences remained significant after adjustment of age and BMI. Decrease in cortical area was also significantly greater in patients at 24 months after adjustment of age and BMI.
Plots of average percentage change at 12 and 24 months of indices of volumetric bone mineral density (vBMD), geometry, trabecular (Tb.), and cortical (Ct.) microstructure in postmenopausal systemic lupus erythematosus (SLE) patients (solid line, black box) and postmenopausal controls (dotted line, open triangle). Bars represent standard error of means. *p < 0.05 compared with baseline of respective group. †p < 0.05 between SLE patients and controls
Changes of bone microstructure
In SLE patients, there was no significant overtime change in indices of trabecular microstructure such as trabecular number, thickness, and separation (Fig. 1). In controls, trabecular number decreased (−1.56 %, p = 0.030) and trabecular separation increased (2.46 %, p = 0.009) significantly at 24 months. There were significant group-wise differences in changes of trabecular separation and number (following adjustment of age and BMI) at 12 months, where patients showed better preservation of trabecular microstructure.
Cortical thickness decreased significantly at 12 (−0.51 %, p = 0.001) and 24 months (−0.63 %, p = 0.034) in SLE patients but showed maintenance in controls. Group-wise comparison showed significant difference at 12 months (p = 0.002), and difference at 24 month was significant after adjustment of age and BMI (adjusted p = 0.031). In contrast, apparent cortical thickness showed significant increase in controls (0.88 % at 12 months, 0.63 % at 24 months, both p < 0.05) but maintenance in patients (0.36 % at 12 months, 0.61 % at 24 months, both p > 0.05). There was no group-wise difference in changes of apparent cortical thickness. Cortical pore volume and Ct.Po showed significant increase in both groups at 24 months with significantly greater increase in patients after adjustment of age and BMI.
Postmenopausal subjects
Changes of aBMD
In both groups, over the study period, there were significant declines in aBMD at the femoral neck, total hip, lumbar spine, and ultradistal radius with no significant group-wise difference at any time point (Table 2).
Changes of vBMD
In SLE patients, integral, trabecular, and cortical vBMD decreased significantly over the study period (−2.61 to −5.43 % at 24 months, all p < 0.0001) (Fig. 2). Similar trends of decrease were also found in controls (−1.56 to −4.36 % at 24 months, all p < 0.0001). Decrease in trabecular vBMD at 12 months was significantly less (0.57 vs. −0.57 %, p = 0.025), and decrease in cortical vBMD at 24 months was significantly greater (−2.66 vs. −1.56 %, p = 0.039) in patients than in controls. Subregion analyses showed no group-wise differences in change of trabecular vBMD of inner region (−5.32 vs. −4.14 % at 24 months, p > 0.05) but significantly less decrease in the outer region in patients at 24 months (−1.15 vs. −2.75 %, p = 0.041). These differences remained significant after adjustment of age, BMI, and age of menopause.
Changes of bone geometry
In both groups, trabecular area increased significantly and cortical area decreased significantly over the study period with no group-wise difference (Fig. 2). Endocortical perimeter increased significantly at 24 months in SLE patients but was preserved in controls. Change of endocortical perimeter did not differ between groups.
Changes of bone microstructure
There was no significant overtime change or group-wise difference in changes of trabecular microstructural indices (Fig. 2). Cortical thickness and apparent cortical thickness decreased significantly in both groups. Decrease in apparent cortical thickness was comparable between patients and controls (−3.83 vs. −3.38 % at 24 months, p > 0.05). Decrease in cortical thickness tended to be larger in patients (−5.88 vs. −3.81 % at 24 months). However, group-wise difference was not significant. Cortical pore volume and Ct.Po increased significantly in both group over the study period with significantly larger increase seen in patients at 24 months (both p < 0.05). These differences remained significant after adjustment of age, BMI, and age of menopause. Figure 3 shows representative images of 3D visualization of the cortices of a postmenopausal SLE patient and an age-matched postmenopausal control.
Representative HR-pQCT images of 3D visualization of the cortices (baseline, 12 months, and 24 months) of the distal radius of a postmenopausal systemic lupus erythematosus (SLE) patient and a postmenopausal control. Cortical bone is depicted in transparent gray and cortical pores in solid red. Progressive cortical porosity is more prominent in SLE patient than in control (color figure online)
Relationship with baseline disease characteristics in SLE patients
Table 3 presents the correlation coefficients between changes of indices of vBMD, geometry, and microstructure over 24 months and indices of baseline disease characteristics in SLE patients. Longer disease duration at baseline was only significantly associated with a larger decrease in cortical area. Baseline organ damage (higher SDI score) was significantly associated with larger decrease in integral and cortical vBMD, cortical area, and apparent cortical thickness, as well as larger increase in trabecular area. Longer duration of use of glucocorticoids was also associated with greater changes in bone geometry as well as larger decline in cortical thickness. Cumulative dose of glucocorticoids at baseline did not influence changes of any bone density or microstructure. In general, changes of trabecular microstructure and cortical porosity were not associated with disease characteristic indices.
Discussion
This is the first case-control prospective study investigating longitudinal changes of cortical and trabecular microstructure using HR-pQCT in Chinese SLE patients. Compared with controls, microstructural changes at the distal radius in SLE patients were characterized by significant deterioration in cortical microstructure, manifested as a decrease in cortical area and thickness and an increase in cortical porosity. This progressive structural deterioration was seen in both premenopausal and postmenopausal patients. Decrease in cortical vBMD relative to controls was also prominent in postmenopausal SLE patients. Trabecular vBMD and microstructure, both in the outer and inner subregions, appeared to be better maintained in SLE patients. Changes of bone density and microstructure in SLE patients were associated primarily with disease severity and, to a lesser extent, with the use of glucocorticoids.
This longitudinal study confirmed our previous findings from a cross-sectional study that structural deterioration at the distal radius in SLE patients mainly affected the cortical bone [11]. In premenopausal SLE patients, there was an accelerated decrease in cortical area and thickness as well as an accelerated increase in cortical porosity after adjustment of age and BMI. Compared to controls, in postmenopausal SLE patients, decrease in cortical vBMD and increase in cortical porosity were significantly more prominent. Decrease in cortical area and thickness was also larger in postmenopausal patients than in controls, albeit not statistically significant. Cortical thinning seemed to be the result of continued endocortical bone resorption evidenced by a significant increase in endocortical perimeter that was only found in SLE patients. Reduced concurrent periosteal apposition, which fails to offset the endocortical bone loss, might also contribute to the cortical thinning [26]. In contrast to cortical thickness, changes of apparent cortical thickness were comparable between SLE patients and controls. In premenopausal patients, cortical thickness decreased significantly, while apparent cortical thickness showed an increasing trend over time, despite not statistically significant. In postmenopausal patients, decreased in apparent cortical thickness was less than that in cortical thickness, and the decrease was similar to that in controls. This discrepancy could be explained by the difference in segmentation techniques employed in the two analyses protocol. The standard analysis protocol, which yields cortical thickness, uses a fixed threshold to separate cortex from background [7]. This segmentation risks losing thin cortical shell that is undistinguished from the trabeculae, especially in subjects with very thin and highly porous cortices [23]. The apparent cortical thickness, which disregards intracortical pore surfaces in the local calculation, may partially correct such loss and downsize the extent of cortical thinning [25]. Therefore, this discordance between changes of cortical thickness and those of apparent cortical thickness, which is most noticeably in SLE patients, might be reflecting progressive cortical porosity, particularly on the endocortical surface, in these patients.
This significant cortical bone loss at the distal radius in SLE patients was accompanied by better maintenance of trabecular vBMD, significantly enlarged trabecular area, and preserved trabecular microstructure. This was more prominent in premenopausal SLE patients in whom relative to controls, trabecular number and separation improved significantly at 12 months. In both trabecular subregions, loss in trabecular vBMD was less in SLE patients than in controls, and such loss appeared to be even less in the outer than in the inner subregion. These compartmental differences in changes in vBMD and structure could be due to compensatory adaptation from the trabecular compartment for the bone loss in the cortical compartment and/or endocortical resorptive activity which “trabecularizes” cortical bone, leaving bone fragments and expanding a well-trabeculated trabecular area [27, 28]. However, scanning electron microscope studies on postmortem hip specimens showed that these cortical remnants had chaotic architecture and may not confer the same mechanical strength as healthy trabeculae [28]. Instead, their presence may lead to overestimation of trabecular density, obscuring the true trabecular bone loss.
In contrast to the findings by HR-pQCT, changes of aBMD at multiple skeletal sites assessed by DXA did not show any group-wise differences, except for aBMD at total hip which decreased to a significantly larger extent at 24 months in premenopausal patients compared to their counterparts. aBMD ultradistal radius appeared to be better maintained in premenopausal patients than in controls. As a 2D integral measure, aBMD is confounded by bone size and is unable to detect compartmental changes in bone density and structure, and the resolution of DXA is not sufficient to detect microstructural features such as cortical porosity. The seemingly preserved aBMD at the distal radius in SLE patients might be reflecting the preserved trabecular vBMD in this group, which is most likely the result of aggressive endocortical remodeling and an expanded trabecular region.
The structural deterioration in cortical bone revealed by HR-pQCT provides a structural basis of the development and progression of osteoporosis in SLE patients, which is not evident on measurement of aBMD by DXA. In SLE patients on long-term glucocorticoids, fracture risk increases not only at the vertebrae but also at skeletal sites that are mainly cortical, such as hips [3, 29]. The significant cortical bone loss found at the distal radius in SLE patients may represent a common trait across skeletal sites and likely a contributor to the heightened fracture risk. Cortical thinning and porosity reduce compressive and bending strength and the resistance of bone to the initiation and propagation of microcracks [30]. Previous cross-sectional studies using HR-pQCT have shown that alterations in cortical microstructure were able to distinguish, independently of aBMD, postmenopausal females with and without fracture [31, 8]. Reduced cortical area and significant cortical thinning at the distal radius have also been associated with vertebral fracture in postmenopausal females [32] and in those on long-term glucocorticoids [33, 34]. Our results indicate cortical bone as an important source of bone loss in SLE patients on long-term glucocorticoids and that HR-pQCT has the potential to better characterize longitudinal microstructural changes of the bone that are associated with bone fragility.
Consistent with our previous findings, we found limited effect of glucocorticoids on vBMD and microstructure at the distal radius [11, 12]. A higher baseline cumulative dose of glucocorticoids had no influence on any changes of bone density and microstructure at the distal radius. Our results also confirmed our previous findings that disease severity contributes to bone loss in SLE patients [12]. Density and microstructural deterioration at cortical compartment was greater in SLE patients with more organ damage at the baseline. The presence of organ damage in SLE represents a more severe form of the disease, reflecting various aspects of the disease such as persistent inflammation, autoantibody production, elevated serum mediators, and genetic factors, as well as medications used to treat the disease [35–38]. Our results suggest that early detection and limitation of tissue damage before clinically overt organ damage may help to prevent osteoporosis in SLE.
There are several limitations in our study. First, only the distal radius was studied and not the distal tibia. The distal radius was chosen because unlike the tibia, the radius is a non-weight-bearing bone. Varied physical capability in a group of SLE patients with diverse disease severity could confound the bone turnover rate and, hence, measurements of density and microstructure at the distal tibia [39, 40]. Second, image analyses were conducted on the common region between baseline and follow-up scans which was determined by matching the two-dimensional cross-sectional area. This area-based image registration method has been criticized for obscuring changes in bone size, such as change in periosteal apposition, as a result of growth, disease, or therapy [41]. Third, biochemical parameters such parathyroid hormone and bone turnover markers were not measured in our study. Fourth, our study included only SLE patients on long-term glucocorticoids. Comparison with SLE patients not receiving glucocorticoids would be beneficial in segregating the effect of disease and the effect of glucocorticoids on longitudinal changes in vBMD and microstructure. However, as glucocorticoids remain the mainstay of treatment, the sample size of this third group is likely to be small, and this group is also likely to consist of SLE patients with mild disease and low-grade inflammation. Fifth, some changes in premenopausal subjects were within the RMSCV of the DXA or HR-pQCT measurements. A longer follow-up on these subjects will be needed to confirm our findings. Finally, our study was conducted in a group of Chinese females. Racial differences in bone density, geometry, and microstructure must be considered when applying our results on other races. A recent cross-sectional HR-pQCT study found that Caucasian SLE females compared to controls had fewer and more widely separated trabeculae but preserved cortical thickness and similar cortical porosity at the distal radius [42]. However, this study was conducted on a relatively small sample of patients (n = 33), and only 22 (67 %) patients were currently on glucocorticoids.
In conclusion, in this 2-year case-control study, microstructural changes at the distal radius in SLE patients were characterized by significant deterioration in cortical bone microstructure with an exaggerated decrease in cortical area and thickness and an exaggerated increase in cortical porosity. This progressive structural deterioration at the distal radius was seen in both premenopausal and postmenopausal patients. Decrease in cortical vBMD relative to controls was also prominent in postmenopausal patients. This deterioration in cortical bone structure was accompanied by a better maintenance of trabecular vBMD and relatively preserved trabecular microstructure. Our results indicate cortical bone as an important source of bone loss in SLE patients on long-term glucocorticoids and show that HR-pQCT can detect longitudinal compartmental differences in bone microstructure known to be associated with bone fragility beyond those revealed by aBMD.
References
D'Cruz DP, Khamashta MA, Hughes GR (2007) Systemic lupus erythematosus. Lancet 369(9561):587–596
Mak A, Isenberg DA, Lau CS (2013) Global trends, potential mechanisms and early detection of organ damage in SLE. Nat Rev Rheumatol 9(5):301–310. doi:10.1038/nrrheum.2012.208
Bultink IE (2012) Osteoporosis and fractures in systemic lupus erythematosus. Arthritis Care Res (Hoboken) 64(1):2–8. doi:10.1002/acr.20568
Li EK, Tam LS, Griffith JF, Zhu TY, Li TK, Li M, Wong KC, Chan M, Lam CW, Chu FS, Wong KK, Leung PC, Kwok A (2009) High prevalence of asymptomatic vertebral fractures in Chinese women with systemic lupus erythematosus. J Rheumatol 36(8):1646–1652
Bultink IE, Lems WF, Kostense PJ, Dijkmans BA, Voskuyl AE (2005) Prevalence of and risk factors for low bone mineral density and vertebral fractures in patients with systemic lupus erythematosus. Arthritis Rheum 52(7):2044–2050
Seeman E, Delmas PD (2006) Bone quality—the material and structural basis of bone strength and fragility. N Engl J Med 354(21):2250–2261
Boutroy S, Bouxsein ML, Munoz F, Delmas PD (2005) In vivo assessment of trabecular bone microarchitecture by high-resolution peripheral quantitative computed tomography. J Clin Endocrinol Metab 90(12):6508–6515
Sornay-Rendu E, Boutroy S, Munoz F, Delmas PD (2007) Alterations of cortical and trabecular architecture are associated with fractures in postmenopausal women, partially independent of decreased BMD measured by DXA: the OFELY study. J Bone Miner Res 22(3):425–433
Seeman E, Delmas PD, Hanley DA, Sellmeyer D, Cheung AM, Shane E, Kearns A, Thomas T, Boyd SK, Boutroy S, Bogado C, Majumdar S, Fan M, Libanati C, Zanchetta J (2010) Microarchitectural deterioration of cortical and trabecular bone: differing effects of denosumab and alendronate. J Bone Miner Res 25(8):1886–1894
Burghardt AJ, Kazakia GJ, Sode M, de Papp AE, Link TM, Majumdar S (2010) A longitudinal HR-pQCT study of alendronate treatment in postmenopausal women with low bone density: relations among density, cortical and trabecular microarchitecture, biomechanics, and bone turnover. J Bone Miner Res 25(12):2558–2571
Tang XL, Qin L, Kwok AW, Zhu TY, Kun EW, Hung VW, Griffith JF, Leung PC, Li EK, Tam LS (2013) Alterations of bone geometry, density, microarchitecture, and biomechanical properties in systemic lupus erythematosus on long-term glucocorticoid: a case-control study using HR-pQCT. Osteoporos Int 24(6):1817–1826. doi:10.1007/s00198-012-2177-5
Tang XL, Zhu TY, Hung VW, Qin L, Wong CK, Kun EW, Tam LS, Li EK (2012) Increased organ damage associated with deterioration in volumetric bone density and bone microarchitecture in patients with systemic lupus erythematosus on longterm glucocorticoid therapy. J Rheumatol 39(10):1955–1963. doi:10.3899/jrheum.120213
Tang XL, Griffith JF, Qin L, Hung VW, Kwok AW, Zhu TY, Kun EW, Leung PC, Li EK, Tam LS (2013) SLE disease per se contributes to deterioration in bone mineral density, microstructure and bone strength. Lupus 22(11):1162–1168. doi:10.1177/0961203313498802
Jacobs J, Korswagen LA, Schilder AM, van Tuyl LH, Dijkmans BA, Lems WF, Voskuyl AE, Bultink IE (2012) Six-year follow-up study of bone mineral density in patients with systemic lupus erythematosus. Osteoporos Int 24(6):1827–1833. doi:10.1007/s00198-012-2157-9
Jardinet D, Lefebvre C, Depresseux G, Lambert M, Devogelaer JP, Houssiau FA (2000) Longitudinal analysis of bone mineral density in pre-menopausal female systemic lupus erythematosus patients: deleterious role of glucocorticoid therapy at the lumbar spine. Rheumatology (Oxford) 39(4):389–392
Boyanov M, Robeva R, Popivanov P (2003) Bone mineral density changes in women with systemic lupus erythematosus. Clin Rheumatol 22(4–5):318–323
Zhu TY, Griffith JF, Au SK, Tang XL, Kwok AW, Leung PC, Li EK, Tam LS (2014) Bone mineral density change in systemic lupus erythematosus: a 5-year followup study. J Rheumatol 41(10):1990–1997. doi:10.3899/jrheum.131190
Hochberg MC (1997) Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40(9):1725
Bombardier C, Gladman DD, Urowitz MB, Caron D, Chang CH (1992) Derivation of the SLEDAI. A disease activity index for lupus patients. The committee on prognosis studies in SLE. Arthritis Rheum 35(6):630–640
Gladman D, Ginzler E, Goldsmith C, Fortin P, Liang M, Urowitz M, Bacon P, Bombardieri S, Hanly J, Hay E, Isenberg D, Jones J, Kalunian K, Maddison P, Nived O, Petri M, Richter M, Sanchez-Guerrero J, Snaith M, Sturfelt G, Symmons D, Zoma A (1996) The development and initial validation of the systemic lupus international collaborating clinics/American College of rheumatology damage index for systemic lupus erythematosus. Arthritis Rheum 39(3):363–369
Lynn HS, Lau EM, Au B, Leung PC (2005) Bone mineral density reference norms for Hong Kong Chinese. Osteoporos Int 16(12):1663–1668
Zhu TY, Griffith JF, Qin L, Hung VW, Fong TN, Au SK, Tang XL, Kwok AW, Leung PC, Li EK, Tam LS (2013) Structure and strength of the distal radius in female patients with rheumatoid arthritis: a case-control study. J Bone Miner Res 28(4):794–806. doi:10.1002/jbmr.1793
Buie HR, Campbell GM, Klinck RJ, MacNeil JA, Boyd SK (2007) Automatic segmentation of cortical and trabecular compartments based on a dual threshold technique for in vivo micro-CT bone analysis. Bone 41(4):505–515
Kazakia GJ, Hyun B, Burghardt AJ, Krug R, Newitt DC, de Papp AE, Link TM, Majumdar S (2008) In vivo determination of bone structure in postmenopausal women: a comparison of HR-pQCT and high-field MR imaging. J Bone Miner Res 23(4):463–474
Burghardt AJ, Buie HR, Laib A, Majumdar S, Boyd SK (2010) Reproducibility of direct quantitative measures of cortical bone microarchitecture of the distal radius and tibia by HR-pQCT. Bone 47(3):519–528
Ahlborg HG, Johnell O, Turner CH, Rannevik G, Karlsson MK (2003) Bone loss and bone size after menopause. N Engl J Med 349(4):327–334. doi:10.1056/NEJMoa022464
Keshawarz NM, Recker RR (1984) Expansion of the medullary cavity at the expense of cortex in postmenopausal osteoporosis. Metab Bone Dis Relat Res 5(5):223–228
Zebaze RM, Ghasem-Zadeh A, Bohte A, Iuliano-Burns S, Mirams M, Price RI, Mackie EJ, Seeman E (2010) Intracortical remodelling and porosity in the distal radius and post-mortem femurs of women: a cross-sectional study. Lancet 375(9727):1729–1736. doi:10.1016/S0140-6736(10)60320-0
Bultink IE, Harvey NC, Lalmohamed A, Cooper C, Lems WF, van Staa TP, de Vries F (2014) Elevated risk of clinical fractures and associated risk factors in patients with systemic lupus erythematosus versus matched controls: a population-based study in the United Kingdom. Osteoporos Int 25(4):1275–1283. doi:10.1007/s00198-013-2587-z
Voide R, Schneider P, Stauber M, Wyss P, Stampanoni M, Sennhauser U, van Lenthe GH, Muller R (2009) Time-lapsed assessment of microcrack initiation and propagation in murine cortical bone at submicrometer resolution. Bone 45(2):164–173
Vico L, Zouch M, Amirouche A, Frere D, Laroche N, Koller B, Laib A, Thomas T, Alexandre C (2008) High-resolution pQCT analysis at the distal radius and tibia discriminates patients with recent wrist and femoral neck fractures. J Bone Miner Res 23(11):1741–1750
Sornay-Rendu E, Cabrera-Bravo JL, Boutroy S, Munoz F, Delmas PD (2009) Severity of vertebral fractures is associated with alterations of cortical architecture in postmenopausal women. J Bone Miner Res 24(4):737–743. doi:10.1359/jbmr.081223
Kaji H, Yamauchi M, Chihara K, Sugimoto T (2008) Glucocorticoid excess affects cortical bone geometry in premenopausal, but not postmenopausal, women. Calcif Tissue Int 82(3):182–190. doi:10.1007/s00223-008-9106-9
Li EK, Zhu TY, Tam LS, Hung VW, Griffith JF, Li TK, Li M, Wong KC, Leung PC, Kwok AW, Qin L (2010) Bone microarchitecture assessment by high-resolution peripheral quantitative computed tomography in patients with systemic lupus erythematosus taking corticosteroids. J Rheumatol 37(7):1473–1479
Wang Y, Qiao B, Wang Y, Han X, Chu Y, Xiong S (2006) Autoantibodies closely relate to the elevation level of in vivo hydrogen peroxide and tissue damage in systemic lupus erythematosus. DNA Cell Biol 25(10):563–570. doi:10.1089/dna.2006.25.563
Bultink IE, Teerlink T, Heijst JA, Dijkmans BA, Voskuyl AE (2005) Raised plasma levels of asymmetric dimethylarginine are associated with cardiovascular events, disease activity, and organ damage in patients with systemic lupus erythematosus. Ann Rheum Dis 64(9):1362–1365. doi:10.1136/ard.2005.036137
Sung YK, Park BL, Shin HD, Kim LH, Kim SY, Bae SC (2006) Interleukin-10 gene polymorphisms are associated with the SLICC/ACR Damage Index in systemic lupus erythematosus. Rheumatology (Oxford) 45(4):400–404. doi:10.1093/rheumatology/kei184
Zonana-Nacach A, Barr SG, Magder LS, Petri M (2000) Damage in systemic lupus erythematosus and its association with corticosteroids. Arthritis Rheum 43(8):1801–1808
Hung LK, Wu HT, Leung PC, Qin L (2005) Low BMD is a risk factor for low-energy Colles’ fractures in women before and after menopause. Clin Orthop Relat Res 435:219–225
Qin L, Choy W, Au S, Fan M, Leung P (2007) Alendronate increases BMD at appendicular and axial skeletons in patients with established osteoporosis. J Orthop Surg Res 2:9. doi:10.1186/1749-799X-2-9
Geusens P, Chapurlat R, Schett G, Ghasem-Zadeh A, Seeman E, de Jong J, van den Bergh J (2014) High-resolution in vivo imaging of bone and joints: a window to microarchitecture. Nat Rev Rheumatol. doi:10.1038/nrrheum.2014.23
Hansen S, Gudex C, Ahrberg F, Brixen K, Voss A (2014) Bone geometry, volumetric bone mineral density, microarchitecture and estimated bone strength in Caucasian females with systemic lupus erythematosus. A cross-sectional study using HR-pQCT. Calcif Tissue Int. doi:10.1007/s00223-014-9918-8
Acknowledgments
The work described in this paper was fully supported by a grant from the Research Grant Council of Hong Kong Special Administrative Region, China (CUHK471010). The authors are grateful to Ms. LI Siu Wan for her generous help in the recruitment of study controls.
Funding
The work described in this paper was fully supported by a grant from Research Grant Council of the Hong Kong Special Administrative Region, China (project no. CUHK471010).
Ethics approval
This study was conducted with the approval of the Joint Chinese University of Hong Kong—New Territories East Cluster Clinical Research Ethics Committee (Ref. no. CRE-2009.215).
Subject consent
Obtained
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhu, T.Y., Griffith, J.F., Qin, L. et al. Cortical thinning and progressive cortical porosity in female patients with systemic lupus erythematosus on long-term glucocorticoids: a 2-year case-control study. Osteoporos Int 26, 1759–1771 (2015). https://doi.org/10.1007/s00198-015-3077-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-015-3077-2