Abstract
Diabetes is associated with increased skeletal fragility, despite higher bone mineral density (BMD). Alternative measures are necessary to more accurately determine fracture risk in individuals with diabetes. Therefore, we aimed to describe the relationship between trabecular bone score (TBS) and normoglycaemia, impaired fasting glucose (IFG) and diabetes and determine whether TBS-adjusted FRAX (Aus) score differed between these groups. This study included 555 men (68.7 ± 12.2 years) and 514 women (62.0 ± 12.0 years), enrolled in the observational Geelong Osteoporosis Study. IFG was considered as fasting plasma glucose (FPG) ≥ 5.5 mmol/L and diabetes as FPG ≥ 7.0 mmol/L, with the use of antihyperglycaemic medication and/or self-report. Using multivariable regression, the relationship between groups and TBS was determined. Men and women (all ages) with diabetes had lower mean TBS compared to those with normoglycaemia, in models adjusted for age, height and weight/waist circumference (all p < 0.05). Men with IFG had lower mean TBS in the age-adjusted models only (all p < 0.05). The addition of TBS to the FRAX score improved the discrimination between glycaemia groups, particularly for younger women (< 65 years). There was no difference in TBS detected between normoglycaemia and IFG; however, those with diabetes had lower TBS. Thus, the increased fracture risk in men and women with diabetes may be a result of BMD-independent bone deterioration. TBS adjustment of FRAX scores may be useful for younger women (< 65 years) with diabetes. This suggests that halting or reversing progression from IFG to diabetes could be important to prevent skeletal fragility in diabetes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes is associated with an increased fracture risk [1, 2], increased mortality, as well as longer time and increased complications during fracture healing [3, 4]. Yet, diabetes is also associated with higher bone mineral density (BMD) [1]. In addition, fracture risk prediction using the FRAX tool underestimates the risk for individuals with diabetes [5]. To date, impaired fasting glucose (IFG) has not been extensively studied in terms of fracture risk.
The increased skeletal fragility associated with diabetes may be due to poorer bone quality including altered material properties [6], or structure, which can be assessed using several different methods, such as magnetic resonance imaging (MRI) or computed tomography (CT); however these are expensive, sensitive to movement artefacts and not readily available [7]. Trabecular bone score (TBS) is a grey-level textural metric that is obtained from lumbar spine dual energy X-ray absorptiometry (DXA) images [8, 9]. Higher TBS indicates stronger bone with a higher fracture resistance, and TBS has been shown to correlate with three-dimensional parameters of bone microarchitecture independently of BMD and clinical risk factors [10,11,12,13]. One strength of TBS is that it can be useful in assessment of fracture risk for individuals who do not have osteoporosis on bone density criteria [14]. This is valuable because most of the population burden of fractures occurs in individuals with moderate deficiency in BMD (osteopenia) [15, 16]. TBS is also useful for fracture risk assessments for individuals with secondary osteoporosis (e.g. diabetes or glucocorticoid-induced osteoporosis), where BMD does not effectively capture the increased fracture risk [8, 9].
The FRAX tool is a fracture risk assessment algorithm developed by the University of Sheffield that utilises clinical risk factors (age, body mass index (BMI), prior fracture, parental hip fracture, smoking, glucocorticoid use, rheumatoid arthritis, secondary osteoporosis and alcohol intake) and femoral neck BMD to assess 10-year fracture probability in men and women aged 40–90 years [14, 17, 18]. TBS has also been shown to improve fracture risk assessments in some populations [8,9,10, 14, 18] and has recently been incorporated into FRAX, allowing a TBS-adjusted score to be calculated [14, 18]. The European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis and the International Society of Clinical Densitometry have endorsed the use of TBS into clinical practice and incorporated it into their recommendations [7, 19].
To date, there have been several studies that have investigated the utility of TBS in distinguishing between individuals with and without diabetes [20,21,22,23,24,25], as well as the ability of TBS adjustment to improve fracture risk predictions using the FRAX tool [26]. These studies, however, have been limited by the number of incident fractures, focussed mainly on postmenopausal women and not all have reported a lower TBS in those with diabetes. Additionally, to our knowledge, no studies have included IFG.
Therefore, this study aimed to describe the relationship between TBS, TBS-adjusted FRAX score and glycaemia status (normoglycaemia, impaired fasting glucose and diabetes) in Australian men and women.
Methods
Participants
This study used data collected as part of the Geelong Osteoporosis Study (GOS), which is a population-based cohort study including residents of the Barwon Statistical Division, located in south-eastern Australia. The region is ideal for conducting epidemiological studies as it has a large population (n ~ 280,000) and includes individuals from a range of social, cultural and geographical settings, which are representative of the wider Australian population. Full details of the cohort have been previously published [27]. GOS participants were randomly selected from Commonwealth electoral rolls, which effectively capture all adults within the region, as voting is compulsory in Australia from age 18 years. The data from this study for men are drawn from baseline (2001–2006, n = 399) or the 5-year follow-up (2006–2011, n = 156) dependent on when the first lumbar spine scan was completed for retrospective assessment of TBS, together with coincident data for determining diabetes status. For women, TBS data were drawn from the 15-year follow-up (2011–2014) as this was the first follow-up where DXA scans were performed on a Lunar Prodigy scanner. However, diabetes status was determined at 10-year follow-up, as there were insufficient data to determine diabetes status at the 15-year follow-up. Prior to this, DXA scans were performed using a DPX-L machine and the software for retrospective determination of TBS is not available for these older DXA devices. Phantom scans were conducted at least three times per week and quality control scans were conducted every day that a participant was scanned. The long-term reproducibility, coefficient of variation, assessed over 180 days using a phantom was 0.23% [28]. All participants provided written, informed consent and Barwon Health Human Research Ethics Committee approved the study.
Clinical Measurements and Questionnaire Data
BMD (g/cm2) was measured using DXA (Lunar Prodigy, GE, Madison, WI, USA). TBS (unitless) was determined retrospectively using TBS iNsight software (Version 2.1, Med-Imaps, Merignac, France). Age referred to the age at TBS assessment. Weight and height were measured to the nearest 0.1 kg and 0.1 cm, respectively. Waist circumference was measured to the nearest 0.5 cm at the minimum circumference between the lowest ribs and the iliac crest. Previous fractures, medication use, rheumatoid arthritis and current smoking were determined by self-report. Ex-smokers were considered as non-smokers. Alcohol consumption was determined from a food frequency questionnaire developed by the Victorian Cancer Council [29] and dichotomised into ≥ 3 or < 3 standard drinks of alcohol per day. A standard glass of beer (285 mL), a single measure of spirits (30 mL) or a medium-sized glass of wine (120 mL) were considered equal to one standard alcohol drink (FRAX Aus guidelines). Physical activity (high/low) was determined by self-report; participants were considered to have “high” physical activity if they had an active lifestyle including light exercise or more undertaken several times per week. Secondary osteoporosis was also identified by self-report, which included insulin-treated diabetes, osteogenesis imperfecta in adults, untreated long-standing hyperthyroidism, malabsorption or chronic liver disease. In this study we were unable to determine chronic malnutrition; instead we applied a previously published method of considering those with BMI less than 18.5 kg/m2 (underweight category) to be malnourished [30].
Socio-economic status (SES) was ascertained using Socio-Economic Indexes for Areas (SEIFA) index scores, based on the 2006 Australian Bureau of Statistics Census data; SEIFA scores were used to determine the level of SES via the Index of Relative Socio-Economic Advantage and Disadvantage (IRSAD). The IRSAD accounts for parameters measured at the area-level, including high and low income, and type of occupation. A low score using the IRSAD identifies the most disadvantaged (quintile 1), while a high score identifies the most advantaged (quintile 5).
Venous blood samples were collected after an overnight fast. Fasting glucose was measured using an adaptation of the hexokinase–glucose-6-phosphate dehydrogenase method [31]. Diabetes was classified if fasting plasma glucose (FPG) ≥ 7.0 mmol/L (126 mg/dL), self-reporting diabetes or use of antihyperglycaemic agents (antihyperglycaemic medication use referred to medications taken regularly and currently at baseline). IFG was considered present if FPG level was between 5.5 and 6.9 mmol/L (100–125 mg/dL); according to the 2003 ADA diagnostic criteria [32]. Medical records and self-report were also used to determine whether any women had developed diabetes since 10-year follow-up. Any women who were diagnosed with diabetes between the 10- and 15-year follow-up were considered to have diabetes.
FRAX Calculations
The Australian version of FRAX (FRAX Aus®) was used in this study and includes the risk factors of age (ranging from 40 to 90 years), sex, weight, height, previous fracture, parental hip fracture, current smoking, glucocorticoid use, rheumatoid arthritis, secondary osteoporosis, alcohol consumption of ≥ 3 units/day and femoral neck BMD. These data were entered into the FRAX (Aus) online tool [33] for each participant and four 10-year probability scores were generated: (i) major osteoporotic fracture (MOF) with BMD, (ii) MOF with BMD, adjusted for TBS, (iii) Hip fracture with BMD and (iv) Hip fracture with BMD, adjusted for TBS. Since FRAX scores are affected by age, and there is a significant age difference between the dysglycaemia groups, ratios were calculated as TBS-adjusted versus unadjusted scores.
Statistical Analyses
The ANOVA or Kruskal–Wallis test was used to determine differences for continuous variables according to glycaemia status. A Chi-Square test or Fisher’s exact test was used for categorical variables.
Using multivariable regression, the relationship between glycaemia status and TBS was assessed for men and women separately, using three different models. The models were first adjusted for age only (age-adjusted model), then for age, weight and height (adjusted model 1). Since TBS is affected by abdominal thickness [34], another model was also developed including age, height and waist circumference (adjusted model 2). Interaction terms were tested in the models to check for effect modification.
Differences between FRAX score ratios with and without TBS adjustment were investigated using a Kruskal–Wallis test for non-parametric data, as FRAX scores were skewed. No clinical measure or lifestyle factor data were missing; however, seven women (6 normoglycaemia and 1 IFG) did not have a femoral neck BMD assessment due to bilateral hip replacement and thus were not included in the FRAX score analysis.
In a model adjusted only for age, we detected a glycaemic status and age interaction term (p = 0.009), and thus both the multivariable regression and FRAX score analyses were also assessed in two age categories; < 65 and ≥ 65 years. All statistical analyses were performed using Minitab (version 16, Minitab, State College, PA, USA).
Results
There were 555 men and 514 women aged 40–90 years with complete TBS, glycaemia status and FRAX clinical risk factor data included in this study. There were 318 men (57.3%) and 381 (73.7%) women with normoglycaemia, 172 (31.0%) men and 85 (16.5%) women with IFG and 65 men (11.7%) and 48 women (9.3%) with diabetes.
For both sexes, those with IFG and diabetes were older than those with normoglycaemia (Table 1), and had higher mean weight and BMI. Mean femoral neck BMD or lumbar spine BMD was not different between the glycaemia groups; however, there was a trend for a higher mean lumbar spine BMD in women with diabetes (p = 0.055). Few men and women were using bisphosphonates, and many of those with diabetes were treated using medication (43.1% of men and 62.5% of women).
MEN: TBS and Glycaemia Status, All Ages
The mean age-adjusted TBS was higher in men with normoglycaemia, compared to men with IFG and diabetes (Table 2).
In the model adjusted for age, weight and height, the relationship between TBS and glycaemia status was attenuated for IFG. However, men with diabetes had lower mean TBS compared to the normoglycaemia group (Table 2).
When adjusted for age, height and waist circumference, results were similar to the model adjusted for age, weight and height (Table 2).
We also detected an association between femoral neck BMD and TBS in men (unadjusted: r = 0.25, p < 0.001), which persisted after adjustment for age, weight and height (r = 0.41, p < 0.001).
WOMEN: TBS and Glycaemia Status, All Ages
In the age-adjusted model for women, diabetes was associated with a lower mean TBS compared to the normoglycaemia group (Table 2); however, there was no difference observed between IFG and normoglycaemia.
In the model adjusted for age, weight and height, women with diabetes had a lower mean TBS compared to normoglycaemia. There was again no difference between TBS for women with IFG compared to normoglycaemia (Table 2).
The model adjusted for age, height and waist circumference showed the same results; compared to normoglycaemia, those with diabetes had a lower TBS, and those with IFG were not different.
There was also an association between femoral neck BMD and TBS in women (unadjusted: r = 0.32, p < 0.001), which also persisted after adjustment for age, weight and height (r = 0.49, p < 0.001). The pattern of the association was similar to that in men; higher femoral neck BMD values corresponded to higher TBS values.
MEN: TBS and Glycaemia Status, Stratified at Age 65 years
When the analysis was stratified by age, a similar pattern was observed. In the age-adjusted model, younger (< 65 years) men with diabetes had lower mean TBS than the normoglycaemia group (Table 2); however, there was no difference between normoglycaemia and IFG. The associations remained the same after adjustment for age, weight and height. In the model adjusted for age, height and waist circumference, the association for lower TBS in those with diabetes was attenuated (p = 0.051).
For older (≥ 65 years) men, mean TBS was not different for IFG or diabetes compared to normoglycaemia in either the age-adjusted or two adjusted models (Table 2).
An association was also observed between femoral neck BMD and TBS in younger men (unadjusted: r = 0.16, p = 0.023), which remained after adjustment for age, weight and height (r = 0.44, p = 0.021). A similar association was also detected for older men (unadjusted: r = 0.21, p < 0.001; adjusted: r = 0.29, p < 0.001).
WOMEN: TBS and Glycaemia Status, Stratified at Age 65 years
In younger (< 65 years) women, age-adjusted mean TBS was lower in those with diabetes compared to normoglycaemia, but not for those with IFG (Table 2). This association was also observed after adjustment for age, height and weight/waist circumference.
For older women (≥ 65 years), TBS values for those with IFG or diabetes were not different to the normoglycaemia group in any of the models.
There was an association detected between femoral neck BMD and TBS in younger (< 65 years) women (unadjusted: r = 0.27, p < 0.001), as well as older (≥ 65 years) women (unadjusted: r = 0.18, p = 0.007), where higher BMD corresponded to a higher TBS. These associations were sustained after adjustment for age, weight and height in younger (r = 0.46, p < 0.001) and older (r = 0.34, p = 0.006) women.
Further adjustment for other variables such as smoking status, alcohol consumption and physical activity did not affect the relationship between glycaemia status and TBS in men or women.
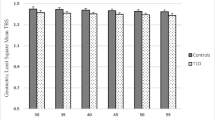
FRAX (Aus) Scores for Men and Women with Impaired Fasting Glucose and Diabetes
All Ages
For both men and women, the assessment of the ratios for TBS-adjusted versus unadjusted MOF and hip FRAX scores resulted in higher values for those with diabetes, compared to normoglycaemia (Table 3). This indicates that TBS adjustment has increased FRAX scores in the individuals with diabetes to a greater extent than in those with normoglycaemia or IFG, which more accurately reflects fracture risk across the groups.
Stratified by Age 65 years
In both younger (≥ 65 years) and older (65 + years) men, the ratios for TBS-adjusted versus unadjusted MOF and hip FRAX scores were not different across the three groups. However, in women, there was a difference between the glycaemia groups in the MOF and hip FRAX score ratios for younger (≥ 65 years) individuals (Table 3), but not those in the older age group (65 + years). This could indicate that TBS-adjusted FRAX scores may be more effective at differentiating between the glycaemia groups in younger (< 65 years) women.
Discussion
This study reports that in both men and women, age-adjusted TBS was lower in those with diabetes, particularly in younger individuals. However, there were no differences observed between IFG and normoglycaemia. The ratios of TBS-adjusted versus unadjusted FRAX scores were different between glycaemia groups in both men and women. For women, ratios were higher for those with diabetes in the younger age group (≤ 65 years), but not the older age group (65 + years).
Several other studies have examined TBS in individuals with diabetes. One such study by Dhaliwal et al. [23] reported that TBS was lower in women with type 2 diabetes (age-adjusted mean ± SD: 1.228 ± 0.140) compared to controls (1.298 ± 0.132, p = 0.013). In a study of 141 overweight and obese men, Romagnoli et al. [34] also report significant associations between measures of HbA1c and TBS, as well as FPG and TBS in participants with BMI > 35 kg/m2. Similar to this study, other research has shown that the effect of diabetes on hip fracture risk and bone fragility is stronger at younger ages [35]. A study by Kim et al. [25] showed this result in women, reporting that TBS was lower in women with diabetes compared to controls for the younger age group (aged < 65 years), but there was no difference observed in TBS for the older age group (≥ 65 years).
Bonaccorsi [21] have reported that TBS-adjusted FRAX scores did not differ compared to TBS alone (0.74 vs. 0.71, p = 0.65) in predicting fractures in women with diabetes. This indicates that TBS may be a useful for fracture prediction in women with diabetes, compared to unadjusted FRAX. Another study by Leslie et al. [22] also investigated the ability of TBS to aid in fracture risk prediction for women aged 50 years or older and reported that TBS predicted fractures in those with diabetes, independent of BMD.
This study has some major strengths. Our study population is randomly selected from the Australian population. We also were able to include both men and women in this study, where many other studies examined only women. We had sufficient information to calculate FRAX scores, including self-report of parental hip fracture, which was not available in some other studies. This study also has some limitations. First, diabetes status for women was determined at the 10-year follow-up, whereas the other data were obtained at the 15-year follow-up. However, this is unlikely to have impacted the number of women that we classified as having diabetes. We have shown across a 10-year time period, that women with diabetes did not revert to IFG or normoglycaemia [36]. However, we may have misclassified some women with IFG. Additionally, we were not able to determine which individuals had type 1 or type 2 diabetes, but it is likely that most had type 2 diabetes. As we did not have information about the duration of diabetes, it is possible that diabetes-related bone changes had not had enough time to manifest in those with newly diagnosed diabetes. The statistical power for age-stratified analyses is lower due to smaller sample size, and may have impacted the reported associations. Finally, it has been shown that diabetes does not affect fracture risk the same across different ethnicities [37], and thus our study, which included mainly Caucasian individuals [27] may not be generalisable to other populations.
To conclude, there was no difference detected in BMD for men and women with diabetes compared to normoglycaemia; however, TBS was lower. We did not detect a difference in TBS between normoglycaemia and IFG. Fracture risk assessment using the FRAX (Aus) tool was better able to distinguish between glycaemia groups after TBS adjustment, particularly in younger women (< 65 years). Overall, these data underscore the importance of halting or reversing the transition from IFG to diabetes to prevent the increase in fracture risk due to diabetes.
References
Sealand R, Razavi C, Adler RA (2013) Diabetes mellitus and osteoporosis. Curr Diabetes Rep 13:411–418
Napoli N, Strotmeyer ES, Ensrud KE, Sellmeyer DE, Bauer DC, Hoffman AR, Dam TT, Barrett-Connor E, Palermo L, Orwoll ES, Cummings SR, Black DM, Schwartz AV (2014) Fracture risk in diabetic elderly men: the MrOS study. Diabetologia 57:2057–2065
Shibuya N, Humphers JM, Fluhman BL, Jupiter DC (2013) Factors associated with nonunion, delayed union, and malunion in foot and ankle surgery in diabetic patients. J Foot Ankle Surg 52:207–211
Gehling DJ, Lecka-Czernik B, Ebraheim NA (2016) Orthopedic complications in diabetes. Bone 82:79–92
Giangregorio LM, Leslie WD, Lix LM, Johansson H, Oden A, McCloskey E, Kanis JA (2012) FRAX underestimates fracture risk in patients with diabetes. J Bone Miner Res 27:301–308
Farr JN, Drake MT, Amin S, Joseph Melton L III, McCready LK, Khosla S (2014) In vivo assessment of bone quality in postmenopausal women with type 2 diabetes. J Bone Miner Res 29:787–795
Harvey NC, Gluer CC, Binkley N, McCloskey EV, Brandi ML, Cooper C, Kendler D, Lamy O, Laslop A, Camargos BM, Reginster JY, Rizzoli R, Kanis JA (2015) Trabecular bone score (TBS) as a new complementary approach for osteoporosis evaluation in clinical practice. Bone 78:216–224
Silva BC, Leslie WD, Resch H, Lamy O, Lesnyak O, Binkley N, McCloskey EV, Kanis JA, Bilezikian JP (2014) Trabecular bone score: a noninvasive analytical method based upon the DXA image. J Bone Miner Res 29:518–530
Ulivieri FM, Silva BC, Sardanelli F, Hans D, Bilezikian JP, Caudarella R (2014) Utility of the trabecular bone score (TBS) in secondary osteoporosis. Endocrine 47:435–448
Iki M, Fujita Y, Tamaki J, Kouda K, Yura A, Sato Y, Moon J-S, Winzenrieth R, Okamoto N, Kurumatani N (2015) Trabecular bone score may improve FRAX® prediction accuracy for major osteoporotic fractures in elderly Japanese men: the Fujiwara-kyo osteoporosis risk in Men (FORMEN) cohort study. Osteoporos Int 26:1841–1848
Hans D, Barthe N, Boutroy S, Pothuaud L, Winzenrieth R, Krieg MA (2011) Correlations between trabecular bone score, measured using anteroposterior dual-energy X-ray absorptiometry acquisition, and 3-dimensional parameters of bone microarchitecture: an experimental study on human cadaver vertebrae. J Clin Densitom 14:302–312
Muschitz C, Kocijan R, Haschka J, Pahr D, Kaider A, Pietschmann P, Hans D, Muschitz GK, Fahrleitner-Pammer A, Resch H (2015) TBS reflects trabecular microarchitecture in premenopausal women and men with idiopathic osteoporosis and low-traumatic fractures. Bone 79:259–266
Roux JP, Wegrzyn J, Boutroy S, Bouxsein ML, Hans D, Chapurlat R (2013) The predictive value of trabecular bone score (TBS) on whole lumbar vertebrae mechanics: an ex vivo study. Osteoporos Int 24:2455–2460
McCloskey EV, Odén A, Harvey NC, Leslie WD, Hans D, Johansson H, Kanis JA (2015) Adjusting fracture probability by trabecular bone score. Calcif Tissue Int 96:500–509
Pasco JA, Seeman E, Henry MJ, Merriman EN, Nicholson GC, Kotowicz MA (2006) The population burden of fractures originates in women with osteopenia, not osteoporosis. Osteoporos Int 17:1404–1409
Pasco JA, Lane SE, Brennan SL, Timney EN, Bucki-Smith G, Dobbins AG, Nicholson GC, Kotowicz MA (2014) Fracture risk among older men: osteopenia and osteoporosis defined using cut-points derived from female versus male reference data. Osteoporos Int 25:857–862
Bauer D (2011) FRAX, falls, and fracture prediction: predicting the future. Arch Intern Med 171:1661–1662
Leslie WD, Johansson H, Kanis JA, Lamy O, Oden A, McCloskey EV, Hans D (2014) Lumbar spine texture enhances 10-year fracture probability assessment. Osteoporos Int 25:2271–2277
Silva BC, Broy SB, Boutroy S, Schousboe JT, Shepherd JA, Leslie WD (2015) Fracture risk prediction by non-BMD DXA measures: the 2015 ISCD official positions part 2: trabecular bone score. J Clin Densitom 18:309–330
Neumann T, Lodes S, Kastner B, Lehmann T, Hans D, Lamy O, Muller UA, Wolf G, Samann A (2016) Trabecular bone score in type 1 diabetes–a cross-sectional study. Osteoporos Int 27:127–133
Bonaccorsi G, Fila E, Messina C, Maietti E, Ulivieri FM, Caudarella R, Greco P, Guglielmi G (2016) Comparison of trabecular bone score and hip structural analysis with FRAX(R) in postmenopausal women with type 2 diabetes mellitus. Aging Clin Exp Res. doi:10.1007/s40520-016-0634-2
Leslie WD, Aubry-Rozier B, Lamy O, Hans D (2013) TBS (trabecular bone score) and diabetes-related fracture risk. J Clin Endocrinol Metab 98:602–609
Dhaliwal R, Cibula D, Ghosh C, Weinstock RS, Moses AM (2014) Bone quality assessment in type 2 diabetes mellitus. Osteoporos Int 25:1969–1973
Zhukouskaya VV, Eller-Vainicher C, Gaudio A, Privitera F, Cairoli E, Ulivieri FM, Palmieri S, Morelli V, Grancini V, Orsi E, Masserini B, Spada AM, Fiore CE, Chiodini I (2016) The utility of lumbar spine trabecular bone score and femoral neck bone mineral density for identifying asymptomatic vertebral fractures in well-compensated type 2 diabetic patients. Osteoporos Int 27:49–56
Kim JH, Choi HJ, Ku EJ, Kim KM, Kim SW, Cho NH, Shin CS (2015) Trabecular bone score as an indicator for skeletal deterioration in diabetes. J Clin Endocrinol Metab 100:475–482
Choi YJ, Ock SY, Chung YS (2016) Trabecular bone score (TBS) and TBS-adjusted fracture risk assessment tool are potential supplementary tools for the discrimination of morphometric vertebral fractures in postmenopausal women with type 2 diabetes. J Clin Densitom 19:507–514
Pasco JA, Nicholson GC, Kotowicz MA (2012) Cohort profile: Geelong osteoporosis study. Int J Epidemiol 41:1565–1575
Sanders KM, Pasco JA, Ugoni AM, Nicholson GC, Seeman E, Martin TJ, Skoric B, Panahi S, Kotowicz MA (1998) The exclusion of high trauma fractures may underestimate the prevalence of bone fragility fractures in the community: the Geelong osteoporosis study. J Bone Miner Res 13:1337–1342
Giles G, Ireland P (1996) Dietary questionnaire for epidemiological studies (version 2). Melbourne, The Cancer Council Victoria
Brennan S, Quirk S, Hosking S, Kotowicz M, Holloway K, Moloney D, Dobbins A, Pasco JA (2015) Is There an interaction between socioeconomic status and FRAX 10-year fracture probability determined with and without bone density measures? Data from the Geelong osteoporosis study of female cohort. Calcif Tissue Int 96:138–144
Kunst ADB, Ziegenhorn J (1984) UV-methods with hexokinase and glucose-6-phosphate dehydrogenase. Chemie, Weinheim
Genuth S, Alberti KG, Bennett P, Buse J, Defronzo R, Kahn R, Kitzmiller J, Knowler WC, Lebovitz H, Lernmark A, Nathan D, Palmer J, Rizza R, Saudek C, Shaw J, Steffes M, Stern M, Tuomilehto J, Zimmet P (2003) Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care 26:3160–3167
University of Sheffield UK (2011) FRAX® WHO fracture risk assessment tool 2011 [cited August 2017]. Available from: http://www.shef.ac.uk/FRAX/
Romagnoli E, Lubrano C, Carnevale V, Costantini D, Nieddu L, Morano S, Migliaccio S, Gnessi L, Lenzi A (2016) Assessment of trabecular bone score (TBS) in overweight/obese men: effect of metabolic and anthropometric factors. Endocrine 54:342–347
Schwartz AV (2016) Epidemiology of fractures in type 2 diabetes. Bone 82:2–8
de Abreu L, Holloway K, Kotowicz M, Pasco J (2015) Dysglycaemia and other predictors for progression or regression from impaired fasting glucose to diabetes or normoglycaemia. J Diabetes Res. doi:10.1155/2015/373762
Looker AC, Eberhardt MS, Saydah SH (2016) Diabetes and fracture risk in older US adults. Bone 82:9–15
Acknowledgements
Study was supported by the National Health and Medical Research Council (NHMRC) of Australia (251638, 299831, 628582), the Geelong Regional Medical Foundation, Arthritis Foundation of Australia and Perpetual Trustees. NKH is supported by an Australian Postgraduate Award. KLH is supported by an Alfred Deakin Postdoctoral Research Fellowship. LLFA and MAS are supported by Deakin Postgraduate Scholarships.
Author information
Authors and Affiliations
Contributions
KLH, MAK and JAP conceived the original plan for the study. DH provided TBS data for the study. KLH and JAP carried out the statistical analysis. KLH, MAK, DH and JAP interpreted the results. KLH wrote the original draft of the manuscript and all other authors provided expertise and advice to produce the final version of the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
Kara L. Holloway, Lelia L. F. De Abreu, Didier Hans, Mark A. Kotowicz, Muhammad A. Sajjad, Natalie K. Hyde, and Julie A. Pasco have no conflicts of interest to declare.
Human and Animal Rights and Informed Consent
The study was approved by the Barwon Health Human Research Ethics Committee, and written informed consent was obtained from all participants.
Rights and permissions
About this article
Cite this article
Holloway, K.L., De Abreu, L.L.F., Hans, D. et al. Trabecular Bone Score in Men and Women with Impaired Fasting Glucose and Diabetes. Calcif Tissue Int 102, 32–40 (2018). https://doi.org/10.1007/s00223-017-0330-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-017-0330-z