Abstract
The purpose of this study was to investigate the therapeutic effect of denosumab, an anti-RANKL monoclonal antibody for the treatment of bone loss in indolent systemic mastocytosis (ISM) patients intolerant to bisphosphonates. Four patients underwent upon informed consent a treatment with denosumab 60 mg administered subcutaneously every 6 months with the same regimen used for postmenopausal osteoporosis. Bone mineral density (BMD) was measured at lumbar and femoral sites at baseline and after 1 year. C-terminal telopeptide of collagen type I (CTX), bone alkaline phosphatase (bALP) and tryptase serum level were determined at baseline and after 12 months with fasting blood samples withdrawals. BMD increased significantly at both sites during the 12 months; all the patients had an important decrease of serum CTX and of lesser extent of bALP serum levels. After denosumab treatment, a decrease in serum tryptase level was observed in all the patients. No adverse events or new fractures occurred. Denosumab seems to be a valid alternative for the treatment of bone loss in ISM. RANKL might be of key importance in the pathogenesis of ISM bone involvement.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mastocytosis includes different expressions of an uncommon disease caused by an abnormal proliferation and invasion of neoplastic mast cells (MCs) in many tissues with a predominant involvement of bone marrow and skin [1, 2]. Systemic mastocytosis is the most common variant in adults [3]. It is characterized by the involvement of at least one extracutaneous organ, frequently: bone, gastrointestinal tract, lymph nodes and spleen; in this form, cutaneous localization could not be present [4, 5]. The release of mediators can provoke diarrhoea, nausea, vomiting, anaphylaxis and has a role in bone loss. The World Health Organization recognizes several systemic mastocytosis variants; Indolent Systemic Mastocytosis (ISM) is the most frequent and is predominantly characterized by symptoms related to mast cell degranulation/mediator release and/or allergies or anaphylaxis [6, 7].
Bone manifestations are one of the most frequent clinical features of ISM, particularly in adults where they could be the only sign of ISM [8]. Patients may present with poorly localized bone pain, diffuse osteopenia or osteoporosis with fragility or pathological fractures, diffuse osteosclerosis or both focal osteolytic and osteosclerotic bone lesions [8, 9]. Moreover, in patients with ISM, the prevalence of at least one vertebral fracture is about 20% in men and 14% in women, and not infrequently vertebral fractures are multiple [9]. ISM patient are also very frequently vitamin D deficient and need supplementation [10].
Bone loss is the result of different pathways, not yet fully discovered. The main actor is the osteoclast with a relative or absolute predominance of bone resorption [11]. There are many clinical relevant mediators released by mast cells after activation that could have putative effects on bone: tryptase, histamine, prostaglandins, interleukin-6 and TNF-α are the most common mediators released by mast cells [11]. Among the stimuli that drive osteoclast activity, the most important one seems to be the RANK–RANKL signalling: expression of RANKL by mast cells directly controls regulation of osteoclast activity and is involved in osteoporosis associated to ISM [12–14].
The central role of osteoclasts made bisphosphonates, as antiresorptive drugs, the most rational treatment for bone involvement in systemic mastocytosis [15]. Currently, Zoledronate has the best evidence in terms of gain in bone mineral density and bone turnover suppression, two surrogate markers of antifracture efficacy [16].
In the last years, a biological antiresorptive drug, Denosumab, has been developed for the treatment of postmenopausal osteoporosis, and it has already shown significant efficacy [17]. This drug consists of monoclonal antibodies directed against RANKL in order to disrupt the RANK–RANKL activation pathway of the osteoclast. The pivotal role of this signalling in the pathogenesis of mastocytosis-related osteoporosis explains the rationale for a new approach with denosumab.
We report the first experiences of treatment with Denosumab injections in four patients affected by ISM. To our knowledge, this is the first report about patients affected by ISM treated with the RANKL antibody denosumab.
Patients
In this case series, we report our experience with denosumab treatment in four postmenopausal patients referred to the Multidisciplinary Mastocytosis Outpatient Clinic of Azienda Ospedaliera Universitaria Integrata of Verona and affected by severe osteoporosis (according with the WHO criteria: lumbar spine or hip bone mineral density T score ≤−2.5 SD and previous fragility fractures) due to ISM. Diagnosis of mastocytosis was proven by bone marrow biopsy, showing mast cell infiltrates expressing CD117, CD2 and CD25. Other causes of osteoporosis were excluded. All the patients had a previous treatment with an oral aminobisphosphonate, alendronate or risedronate, for few days and interrupted it due to intolerance (gastrointestinal symptoms, headache, skeletal pain) at least three months before denosumab administration. They also were all unwilling to take endovenous aminobisphosphonates partly due to concerns about acute phase reaction. The informed consent was obtained from all patients.
Methods
Denosumab was injected subcutaneously at a dose of 60 mg every 6 months.
Bone turnover markers (BTM) and tryptase serum levels were evaluated before starting treatment and after a year. Bone alkaline phosphatase (bALP) and C-terminal telopeptide of collagen type I (CTX) were measured in the serum with ELISA IDS Co. Bolden, UK. Tryptase was evaluated with UniCap 100, Phadia, Sweden.
Bone mineral density (BMD) was measured by Dual Energy X-ray Absorptiometry (DEXA) technique (Hologic QDR Delphi) at the lumbar spine and at the proximal hip at baseline and after 12 months. In case of vertebral osteoarthritis, the evaluation of BMD at lumbar spine was excluded from the analysis.
Results
Patients were all females, aged 55 to 84. Serum CTX range was 0.15–0.74 ng/l, bALP one was 12–22 U/l and tryptase one 19.6–35.4 µg/l. Baseline T score BMD at lumbar site was between −2.5 and −3.6 and at femoral site between −0.6 and −3.0. Two patients had two vertebral fractures, one had one vertebral and one femoral fractures, one had pelvic, wrist and multiple vertebral fractures.
Fracture risk in 10 years time assessed by FRAX of the four patients was 22, 23, 33 and 15%.
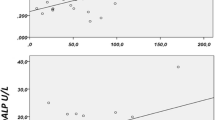
The results of the treatment with denosumab are shown in Figs. 1 and 2. All the patients had a BMD increase, particularly at the lumbar site. BTM remarkably decreased, in particular the reabsorption markers, which were completely suppressed after a year from the beginning of the treatment, regardless of baseline values.
A decrease in serum tryptase level was observed in all the patients after denosumab treatment.
Discussion
This is the first report about the use of denosumab, an anti-RANKL monoclonal antibody, in patients with low BMD secondary to systemic mastocytosis, with encouraging preliminary results.
Currently, mastocytosis-related osteoporosis is treated orally or intravenously with bisphosphonates, with evidence of efficacy on BMD and BTM [16]. These drugs are not well tolerated in ISM, both per os due to worsening of digestive symptoms by mast cells activation, and intravenously. After zoledronate infusion, ISM patients have more frequent and severe acute phase responses than the ones with postmenopausal osteoporosis with 100% of occurrence compared to 42.4%, respectively [16, 18, 19]. In addition, the use of bisphosphonates brings the issue of their long-term persistence in bone for several years or even decades, particularly worrying in women of childbearing age. Among different treatments available for postmenopausal osteoporosis, the use of an anti-RANKL antibody, denosumab, in ISM-associated osteoporosis could be attractive. This treatment is practically administered every 6 months by a subcutaneous injection with very few side effects, and its biological half-life is shorter than bisphosphonates ones, particularly of zoledronate [20]. However, there are some safety concerns about the risk of anaphylaxis with the use of this antibody that still need to be ruled out.
The evident BTM drop in those four patients proves indirectly the effect of denosumab treatment on bone cells, especially on osteoclast, with a substantial decrease of the resorption marker, CTX. The BTM changes agree with the observed improvement of bone BMD, mainly at spine site but also at femoral ones. The extent of this effect is similar to what is reported after zoledronate administration [16]. So, denosumab treatment appears to be suitable as a new anti-resorption approach both in the treatment and prevention of mastocytosis-related osteoporosis, especially in patients with high serum levels of CTX, known risk factor for fragility fractures and bone loss in ISM patients [10, 16].
Our results are in line with the pathophysiological hypothesis of a key importance of the RANKL–RANK pathway: it seems that in ISM, different stimuli end in an upregulation of RANKL signalling, making it an optimal therapeutic target.
Together with BTM decrease, we observed with great interest a decrease in tryptase serum levels in all patients. These data have no pathophysiological explanation yet, but it leads to the hypothesis of some kind of negative feedback on MCs originated from the suppressed osteoclast activity or even a direct effect of denosumab on MCs number or activity. This makes even more interesting the approach with denosumab opening to the possibility of a positive effect also on the underlying hematologic disease. However, it has to be investigated how the effect takes place and whether it is on MCs function or number.
Conclusion
In reason of the positive effects on BMD and BTM, surrogates of anti-fracture efficacy, denosumab might be a particularly valid alternative in the treatment of mastocytosis-related osteoporosis in case of bisphosphonate intolerance or contraindications.
References
Krishnaswamy G, Ajitawi O, Chi DS (2006) The human mast cell: an overview. Methods Mol Biol 315:13–34
Arock M, Valent P (2010) Pathogenesis, classification and treatment of mastocytosis: state of the art in 2010 and future perspectives. Expert Rev Hematol 3:497–516
Sperr WR, Valent P (2012) Diagnosis, progression patterns and prognostication in mastocytosis. Expert Rev Hematol 5:261–274
Valent P (2013) Mastocytosis: a paradigmatic example of a rare disease with complex biology and pathology. Am J Cancer Res 3:159–172
Lee JK, Whittaker SJ, Enns RA, Zetler P (2008) Gastrointestinal manifestations of systemic mastocytosis. World J Gastroenterol 14:7005–7008
Pardanani A (2016) Systemic mastocytosis in adults: 2017 update on diagnosis, risk stratification and management. Am J Hematol 91:1146–1159
Valent P, Akin C, Escribano L, Fodinger M, Hartmann K, Brockow K, Castells M, Sperr WR, Kluin-Nelemans HC, Hamdy NA, Lortholary O, Robyn J, van Doormaal J, Sotlar K, Hauswirth AW, Arock M, Hermine O, Hellmann A, Triggiani M, Niedoszytko M, Schwartz LB, Orfao A, Horny HP, Metcalfe DD (2007) Standards and standardization in mastocytosis: consensus statements on diagnostics, treatment recommendations and response criteria. Eur J Clin Invest 37:435–453
Rossini M, Zanotti R, Bonadonna P, Artuso A, Caruso B, Schena D, Vecchiato D, Bonifacio M, Viapiana O, Gatti D, Senna G, Riccio A, Passalacqua G, Pizzolo G, Adami S (2011) Bone mineral density, bone turnover markers and fractures in patients with indolent systemic mastocytosis. Bone 49:880–885
Rossini M, Zanotti R, Viapiana O, Tripi G, Orsolini G, Idolazzi L, Bonadonna P, Schena D, Escribano L, Adami S, Gatti D (2014) Bone involvement and osteoporosis in mastocytosis. Immunol Allergy Clin North Am 34:383–396
Artuso A, Caimmi C, Tripi G, Viapiana O, Bonifacio M, Idolazzi L, Gavioli I, Gatti D, Zanotti R, Rossini M (2016) Longitudinal evaluation of bone mineral density and bone metabolism markers in patients with indolent systemic mastocytosis without osteoporosis. Calcif Tissue Int
Frenzel L, Hermine O (2013) Mast cells and inflammation. Joint Bone Spine 80:141–145
Rabenhorst A, Christopeit B, Leja S, Gerbaulet A, Kleiner S, Forster A, Raap U, Wickenhauser C, Hartmann K (2013) Serum levels of bone cytokines are increased in indolent systemic mastocytosis associated with osteopenia or osteoporosis. J Allergy Clin Immunol 132(1234–1237):e1237
Guillaume N, Desoutter J, Chandesris O, Merlusca L, Henry I, Georgin-Lavialle S, Barete S, Hirsch I, Bouredji D, Royer B, Gruson B, Lok C, Sevestre H, Mentaverri R, Brazier M, Meynier J, Hermine O, Marolleau JP, Kamel S, Damaj G (2013) Bone complications of mastocytosis: a link between clinical and biological characteristics. Am J Med 126(75):e71–e77
Ali AS, Lax AS, Liljestrom M, Paakkari I, Ashammakhi N, Kovanen PT, Konttinen YT (2006) Mast cells in atherosclerosis as a source of the cytokine RANKL. Clin Chem Lab Med 44:672–674
Rossini M, Zanotti R, Orsolini G, Tripi G, Viapiana O, Idolazzi L, Zamo A, Bonadonna P, Kunnathully V, Adami S, Gatti D (2016) Prevalence, pathogenesis, and treatment options for mastocytosis-related osteoporosis. Osteoporos Int 27:2411–2421
Rossini M, Zanotti R, Viapiana O, Tripi G, Idolazzi L, Biondan M, Orsolini G, Bonadonna P, Adami S, Gatti D (2014) Zoledronic acid in osteoporosis secondary to mastocytosis. Am J Med 127(1127):e1121–e1124
Papapoulos S, Lippuner K, Roux C, Lin CJ, Kendler DL, Lewiecki EM, Brandi ML, Czerwinski E, Franek E, Lakatos P, Mautalen C, Minisola S, Reginster JY, Jensen S, Daizadeh NS, Wang A, Gavin M, Libanati C, Wagman RB, Bone HG (2015) The effect of 8 or 5 years of denosumab treatment in postmenopausal women with osteoporosis: results from the FREEDOM Extension study. Osteoporos Int 26:2773–2783
Rossini M, Adami G, Adami S, Viapiana O, Gatti D (2016) Safety issues and adverse reactions with osteoporosis management. Expert Opin Drug Saf 15:321–332
Reid IR, Gamble GD, Mesenbrink P, Lakatos P, Black DM (2010) Characterization of and risk factors for the acute-phase response after zoledronic acid. J Clin Endocrinol Metab 95:4380–4387
Kumagai Y, Hasunuma T, Padhi D (2011) A randomized, double-blind, placebo-controlled, single-dose study to evaluate the safety, tolerability, pharmacokinetics and pharmacodynamics of denosumab administered subcutaneously to postmenopausal Japanese women. Bone 49:1101–1107
Acknowledgements
The authors thank Sara Rossini who provided editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Giovanni Orsolini, Irene Gavioli, Gaia Tripi, Ombretta Viapiana, Davide Gatti, Luca Idolazzi, Roberta Zanotti, Maurizio Rossini declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
All patients gave an informed consent to the treatment.
Rights and permissions
About this article
Cite this article
Orsolini, G., Gavioli, I., Tripi, G. et al. Denosumab for the Treatment of Mastocytosis-Related Osteoporosis: A Case Series. Calcif Tissue Int 100, 595–598 (2017). https://doi.org/10.1007/s00223-017-0241-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-017-0241-z