Abstract
Sudden limb displacement evokes a complex sequence of compensatory muscle activity. Following the short-latency reflex and preceding voluntary reactions is an epoch termed the medium-latency reflex (MLR) that could reflect spinal processing of group II muscle afferents. One way to test this possibility is oral ingestion of tizanidine, an alpha-2 adrenergic agonist that inhibits the interneurons transmitting group II signals onto spinal motor neurons. We examined whether group II afferents contribute to MLR activity throughout the major muscles that span the elbow and shoulder. MLRs of ankle muscles were also tested during walking on the same day, in the same participants as well as during sitting in a different group of subjects. In contrast to previous reports, the ingestion of tizanidine had minimal impact on MLRs of arm or leg muscles during motor actions. A significant decrease in magnitude was observed for 2/16 contrasts in arm muscles and 0/4 contrasts in leg muscles. This discrepancy with previous studies could indicate that tizanidine’s efficacy is altered by subtle changes in protocol or that group II afferents do not substantially contribute to MLRs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A central aim of sensorimotor research is identifying the neural pathways that underlie coordinated action including the ability to make corrective responses to external disturbances such as the downward force of coffee poured into a held cup. Corrective responses to a sudden displacement of a limb segment depend on multiple neural pathways acting at different rates. The fastest somatosensory-based correction is the short-latency reflex (SLR) which begins around 20 ms post-perturbation in the upper limb and around 40 ms in the lower limb (Corna et al. 1995; Deiner et al. 1983; Grey et al. 2001; Hammond 1956; Lee and Tatton 1982; Lewis et al. 2005; Matthews et al. 1990; Nakazawa et al. 1997; Prusyznski et al. 2008; Sinkjaer et al. 1996). Its rapid onset (somewhat longer for more distal muscles due to the longer nerve tracks) unambiguously implicates the effect of group I muscle afferents on a spinal circuit since this is the only route fast and short enough to be responsible. Subsequent to the SLR is the medium-latency reflex (MLR) beginning around 50 ms post-perturbation in the upper limb and 60–65 ms in the lower limb (Corna et al. 1995; Deiner et al. 1983; Grey et al. 2001; Hammond 1956; Lee and Tatton 1982; Lewis et al. 2005; Matthews et al. 1990; Nakazawa et al. 1997; Prusyznski et al. 2008; Sinkjaer et al. 1996).
Care must be taken that the MLR at the upper and lower limbs are not direct equivalents, however. At the upper limb, the MLR is due to the continued influence of the direct monosynaptic group I-spinal circuit (Lee and Tatton 1982; Lewis et al. 2005; Schuurmans et al. 2009; Kurtzer et al. 2010) along with a group I-transcortical circuit (Matthews et al. 1990; Day et al. 1991; Tsuji and Rothwell 2002; Pruszynski et al. 2011; Evarts and Fromm 1981) which likely enables sophisticated capabilities like multi-joint integration (Gielen et al. 1988; Soechting and Lacquaniti 1988; Kurtzer et al. 2008), scaling with mechanical instability (Doemges and Rack 1992; Kimura et al. 2006; Shemmell et al. 2009), and tuning to the task demands (Hammond 1956; Crago et al. 1976; Pruszynski et al. 2008).
Due to the relative proximity of the relevant spinal cord segments with the cortex, the different processing delays through spinal and transcortical pathways are minimal and responses at MLR latency can include slow or indirect spinal mechanisms as well as transcortical mechanisms. At the lower limb, there is considerably longer distance between the relevant spinal segments and the cortex and, at 60–65 ms latency, the lower limb MLR (or M2) has a latency which is now too short to include a transcortical component (see for instance Christensen et al. 2000, 2001, Petersen et al. 1998). A subsequent response is found at around 90 ms (called M3) and represents the processing done through the transcortical pathway. Therefore, group II and transcortical processing are specific to the M2 and M3 responses of the lower limb. This motivates using the lower limb as a control when testing the potential contribution of group II processing to upper limb MLRs.
Physiological recordings in cats indicate that tizanidine preferentially depresses the transmission of group II signals to interneurons within the intermediate zone (Bras et al. 1990; Skoog 1996). If these spinal networks remain effective in the awake behaving human, then tizanidine should also attenuate reflexes relying on group II afferents. Corna et al. (1995) first tested this possibility in healthy human subjects maintaining an upright stance on a tilting platform. Toe-down rotations evoked MLRs in the stretched tibialis anterior and these responses were indeed depressed following a single oral dose of tizanidine.
A number of subsequent studies have reported that tizanidine selectively attenuates MLRs in the lower limb including in muscles controlling the foot (Corna et al. 1995; Marque et al. 2005), ankle (Grey et al. 2001; Uysal et al. 2009; Af Klint et al. 2010) and knee (Marchand-Pauvert et al. 2005; Friemert et al. 2010). Note that this effect was observed for a range of motor tasks including walking, standing and passively sitting. For the upper limb, the evidence is restricted to the wrist flexor (Lourenco et al. 2006; Meskers et al. 2010; Uysal et al. 2012). The one study which examined proximal arm muscles reported depressed MLRs in elbow muscles following intramuscular injection (Mackel et al. 1984), but this occurred with a 50% decrease in background muscle activity which would automatically downscale reflex excitability (Matthews 1986; Pruszynski et al. 2009); in fact, the authors observed depressed SLRs suggesting that their procedure had a non-specific effect.
The goal of the present study was to use tizanidine to elucidate the relative contribution of group II afferents to the MLR of proximal upper limb muscles. To do so, MLR were elicited in six different elbow and shoulder muscles, before and after tizanidine ingestion. As a control, tizanidine’s effects were also assessed at the lower limb during gait in the same participants during the same session, and during sitting in a separate group of participants. Similar protocols to earlier studies were used, with the exception that muscle stretch parameters were optimized to obtain larger MLR responses in the leg muscles. We found infrequent effects of tizanidine on the MLR of proximal upper limb muscles, and no impact of tizanidine on the MLR of ankle muscles in either the walking or sitting, despite the usual large central effects (drowsiness) of taking the drug. Possible interpretations for these findings and for failure to replicate previous work are discussed.
Materials and methods
Subjects
A total of 20 subjects performed different motor control tasks following informed consent to procedures approved by the ethics committee at New York Institute of Technology, Queen’s University and University of Copenhagen. 14 subjects were male and 6 subjects were female (median age = 27 years). Nine subjects stabilized their upper limb against mechanical perturbations (arm task) and also walked in the presence of sporadic mechanical perturbations applied at the ankle (walking task). Four additional subjects only performed the arm task. Seven subjects stabilized their ankle against mechanical perturbations applied during sitting (sitting task). Subjects were pre-screened by a neurologist specialized in motor dysfunction; exclusion criteria included liver disorders, medications affecting liver metabolism (esp. fluvoxamine and ciprofloxacin), oral birth control, pregnancy, breast feeding, and low blood pressure. Subjects were additionally screened for the lower limb task and excluded if: they weighed over 250 lbs (robotic gait orthosis limit), had larger than average lateral rotation of the feet during stance, or had neurological or orthopaedic history that could interfere with task execution. Experiments lasted ≈ 4 h and subjects were paid for their time.
Apparatus
We utilized programmable robotic devices to study the control of the upper and lower limbs (Fig. 1). The arm task involved an adjustable robotic exoskeleton (KINARM, BKIN Technologies Ltd, Kingston, ON) whose troughs encased the forearm and arm, rotating links allowed flexion/extension movements of the shoulder and elbow in the horizontal plane, and motors could selectively apply torques to each joint (Scott 1999; Singh and Scott 2003; Kurtzer et al. 2008); the right arm was examined in all cases. Visual targets and a hand-aligned cursor were presented in the horizontal plane via a virtual-reality system while a cloth bib and metal partition obscured direct vision of the subject’s arm.
Robotic manipulanda. a Subject is seated with his arm placed in the cuffs of the KINARM planar robot exoskeleton. The chair is directly in front of the horizontal video projector for displaying the target hand position in the arm’s plane of motion. b Subjects walking on treadmill while wearing the robotic exoskeleton fitted to their leg. The motor of the device is on the floor to the right of the treadmill
The lower limb tasks involved an adjustable robotic ankle–foot orthosis enabling unrestricted dorsiflexion/plantarflexion movements of the ankle and a motor to apply torques to that joint (Blanchette et al. 2011; Bouyer 2011; Noel et al. 2009). The robot used during the walking task is fully described in Noel et al. 2008. The robot used during the sitting task is fully described in Toft et al. (1991). The right leg was examined in all cases. During the walking task, subjects stood and stepped forward on a motorized treadmill (Horizon WT751) without holding the handle bar (arms free).
Muscle recordings
We recorded the surface EMG from several arm and leg muscles. Arm muscles included an elbow flexor (brachioradialis), elbow extensor (triceps lateral), shoulder flexor (pectoralis major), shoulder extensor (posterior deltoid), biarticular flexor (biceps brachii), and biarticular extensor (triceps longus). Leg muscles included the ankle plantarflexor (soleus) and ankle dorsiflexor (tibialis anterior). Two-bar (DE-2.1 Delsys Inc., Boston, MA) or disposable electrodes (Blue Sensor, Ambu Inc., USA) were affixed to the skin overlying the muscle bellies following light abrasion with alcohol. Ground electrodes were placed on the subject’s knee.
Perturbation conditions for the arm task
Each trial began with the appearance of a target (2.5 cm radius) and application of a background torque ramped up over 1000 ms. Subjects stabilized their hand-aligned cursor (0.5 cm radius) at the target’s center—corresponding to a shoulder angle of 45° and elbow angle of 90°. During the hold period subjects were told to avoid co-contracting their muscles. After a random time interval of 1–4 s, a 100 ms torque pulse was applied to their arm. To achieve task success subjects had to remain within the target for 500 of the subsequent 1500 ms. Corrections were guided without visual feedback of their hand although the target was coloured green or red when their hand was inside or outside the target, respectively. The total applied torque then ramped down to zero, remained off during an inter-trial period of 1500 ms, and the hand-aligned cursor reappeared.
All trials involved the same sequence described above. Several different background and perturbation torques were utilized (see Table 2). These conditions were randomly intermixed across trials. Note that the 4 subjects who only performed the arm task were exposed to 16 conditions whereas 9 subjects who performed the arm and leg task were exposed to 8 conditions. We focused on 8 conditions shared by all subjects (highlighted in bold). For each muscle we examined the two conditions which (1) required low and high levels of active compensation to the background torque and (2) required increased activity to counter the perturbation stretching that muscle. Elbow flexor (extensor) activity was examined with the two background extension (flexion) torques and the combined extension (flexion) torque perturbation; because of the arm’s intersegmental dynamics, pure elbow motion resulted from the combined shoulder-elbow torque perturbations (Graham et al. 2003; Kurtzer et al. 2008). Biarticulars were weakly modulated by shoulder torque and were examined in the same manner as elbow muscles. Shoulder flexor (extensor) activity was examined with the two background torques and the shoulder extension (flexion) torque perturbations. We also examined shoulder flexor (extensor) activity with the combined extension (flexion) torques since the MLR of shoulder muscles are evoked by pure elbow motion (Kurtzer et al. 2008; Pruszynski et al. 2011). We collected 30 repeats of each condition.
Perturbation conditions for the walking task
The walking task followed standard procedures (Grey et al. 2001; af Klint et al. 2010). Subjects walked on the treadmill at their preferred pace (3.2–3.6 km/h) within a fully illuminated room. Every 4–6 gait cycles the subject received a perturbation of their right ankle. 300 ms ramp-hold-release displacements of ~ 6° with a rise rate ≈ 110°/s were used. The specific amplitude and speed was varied during a pre-experimental period to find the subject-specific setting to produce the largest MLR. During the walking experiments, we found the optimal stretch velocity, timing and range based on trial and error and picked the one where we saw the largest M2 (area) response distinguishable from M1 (and M3) that also were clearly distinguishable from no perturbation trials. We used average traces overlying no perturbation average traces to make this decision. We started with 8° perturbation, 800 ms trigger delay and a velocity of 450°/s. Then we worked around from there, changing on parameter at the time, doing ten stretches each.
The dorsiflexing perturbation rotated the ankle upwards and was triggered ≈ 200 ms after heel strike: 5.5° (0.4SD) at 105°/s (11 SD). The plantarflexing perturbation rotated the ankle downwards and was triggered in mid-swing: 7° (0.4 SD) at 116°/s (6 SD). Note that these perturbations were slower than most earlier studies examining gait, 300–400°/s (Grey et al. 2001; af Klint et al. 2010) to optimize for an MLR response (see Fig. 3 in Grey et al. 2001). We collected 20 repeats of each condition.
Examples of torque perturbations applied to the arm during postural maintenance. a Constant flexion torque (low level) was applied at both joints prior to a 100 pulse of additional shoulder flexion torque; this perturbation was utilized to stretch the shoulder extensor muscle. b The shoulder torque pulse initially flexed the shoulder and extended the elbow from the arm’s starting position. c Constant extension torque was applied at both joints (high level) prior to a 100 pulse of additional extension torque at both joints; this perturbation was utilized to stretch the elbow flexor muscles. d The combined torque pulse initially extended the elbow from the arm’s starting position
Perturbation conditions for the sitting task
Subjects were resting in a comfortable chair as described by Toft et al. (1991) with their right foot placed on and firmly strapped to a platform capable of producing perturbations in both plantar and dorsiflexion directions with adjustable speed and range. Five hundred ms ramp-hold-release perturbations of 6° from the neutral position were used. The rise time was adjusted to produce the largest MLR possible (80–120 ms) with a background of 20% maximum voluntary contraction; the stretch velocity varied from 300 to 500°/s. A similar searching procedure was used as described above. We collected 20 repeats in trains of 10 trials with a frequency of 1 Hz while subjects maintained the background contraction throughout the session.
Protocol for tizanidine exposure and testing
The 8-condition arm task took 35 min (one average) whereas completing the 16-condition arm task took 65 min (on average). The walking task required 10–15 min to complete. We were able to transition between the two tasks within 5–10 min. The sitting task took 10–15 min to complete. The tasks were performed before and 90 min after a single oral dose of tizanidine. When the arm and walking task were both employed, then the walking task was always tested at the earliest time following the dosage. Dose magnitude was determined by body weight as 150 μg/kg, according to most previous studies (see Table 1), leading to an absolute dosage of 8–12 mg.
Data analysis
We processed the kinematic and electromyographic data following procedures described in previous papers (Kurtzer et al. 2008; Pruszynski et al. 2008). Angular positions were lowpass filtered (25 Hz, 2-pass, 6th order Butterworth). Processing of the EMG signals included an amplification (gain = 1–10 K), bandpass filter (10–350 Hz), digital sampling at 1000 Hz (PCI 6071E, National Instruments, Austin, TX), rectification, and normalization by the muscle’s mean baseline activity during the pre-drug phase. Baseline activity for the arm task occurred during the hold period with the smaller load. Baseline activity for the leg task occurred during mid-stance and mid-swing of the gait cycle for the dorsiflexion and plantarflexion perturbations, respectively. The data were normalized to baseline and analysed as normalized units (nu).
We focused on a post-perturbation epoch alternately termed the M2, R2, or medium-latency reflex. We adopt the MLR nomenclature for this epoch spanning 50–75 ms in the arm (Crago et al. 1976; Lee and Tatton 1982; Marsden et al. 1983; Nakazawa et al. 1997; Prusyznski et al. 2008) and starting between 60 and 85 ms in the leg (Christensen et al. 2000); note that for the lower limb, we selected a 20 ms window centered at each subject’s peak response (Af Klint et al. 2010; Grey et al. 2001). These narrow windows were chosen to examine the MLR as specifically as possible since previous claims have focused on the MLR and preceding and subsequent muscle responses may not include significant contributions from the group II afferents. Analyses also considered an earlier time termed M1, R1, or short-latency reflex, 20–45 ms in the upper limb and ~ 40–60 ms in the lower limb.
Our experimental design allowed us to make straight-forward comparisons between conditions to determine whether tizanidine impacted the MLR epoch. For the arm perturbations, we utilized repeated-measures ANOVAs to tests for a main effect of background load and dosage. For the arm and leg perturbations, we utilized paired t-tests to ascertain significant evoked activity against background and significant changes in evoked activity with dosage. Significance was set at P < 0.05.
Results
Arm task
The arm task required subjects to maintain their hand within a small target by countering a constant background torque followed by a torque pulse of random onset and direction. Figure 2 shows two examples of the applied loads and induced motion from a representative subject. In one condition, the subject countered a small flexion background torque at both the shoulder and elbow followed by a flexion torque suddenly applied to just the shoulder. Because of the arm’s intersegmental dynamics this single-joint torque displaced both the shoulder joint (flexion movement) and the elbow joint (extension movement). In other trials, the subject countered a large background extension torque at both joints followed by an extension torque suddenly applied to both joints. Because of the arm’s intersegmental dynamics this multi-joint torque initially displaced only the elbow joint (extension movement). For our primary analysis we used shoulder torques to study the stretch-related activity in the subject’s shoulder muscles and multi-joint torques to study the stretch-related activity in the subject’s elbow and biarticular muscles.
The peak joint displacement induced by the torque pulses varied between subjects, by perturbation direction, and by background load due to the different sizes of the subjects’ arms, each arm’s inertial anisotropy, and automatic scaling of evoked activity to the muscle’s background activity/motor neuron activity. Regardless, the peak displacements were relatively small and transient. Across subjects and conditions the minimum peak displacement was ≈ 3° and the maximum peak displacement was ≈ 9°.
The low and high background torques for each perturbation (Table 2) led to lower and higher background muscle activity. The high background torque was twice the magnitude as the low background torque leading to a ratio of high to low background activity of 1.8 (0.4 SD) across subjects and muscles. A two-way ANOVA confirmed a significant effect of background load (P < 0.001) for all muscles (posterior deltoid, F(1,12) = 23.3; triceps lateral, F(1,12) = 123.7; triceps longus, F(1,11) = 35.9; pectoralis major, F(1,12) = 43.4; brachioradialis, F(1,12) = 31.1; and biceps brachii, F(1,11) = 25.7). In contrast to the substantial difference in background muscle activity with background torque there was a negligible impact of the tizanidine dosage—ratio of pre-dosage to post-dosage background activity was 0.98 (0.19 SD) across subjects and muscles (P > 0.05, F(1,11−12) < 4.5). This pattern is evident in the two sample muscles presented in Fig. 3.
Examples of evoked activity in arm muscles. a Evoked activity in an exemplar subject’s shoulder extensor during a low background torque and shoulder torque pulse, same perturbation depicted in Fig. 2a, b. Black and grey traces show muscle activity obtained before and after tizanidine intake, respectively. Data normalized to background activity with low background torque, normalized units (nu). The grey window indicates the R2 time epoch spanning 50–75 ms. b Group data of shoulder muscle activity to the same conditions. c Evoked activity in an exemplar subject’s elbow flexor with a high background torque and combined torque pulse, same perturbation depicted in Fig. 2c, d. d Group data of shoulder muscle activity to the same conditions
The selected perturbations reliably evoked MLR activity in all the examined muscles. Prior to the tizanine dosage, the perturbation evoked an increase from baseline with the low background load (P1 − sided < 0.001, t(11−12) > 7.9) and high background load (P1 − sided < 0.001, t(11−12) > 5.7). Likewise, following the tizanine dosage, the perturbation evoked an increase from baseline with the low background load (P1 − sided < 0.001, t(11−12) > 5.8) and high background load(P1 − sided < 0.005, t(11−12) > 4.3). For example muscles see Fig. 3; for group data of all muscles see Fig. 4.
Mean R2 activity in arm muscles before and after tizanidine intake. Data from six muscles controlling the elbow and/or shoulder. Each bar shows the group average baseline activity and evoked R2 separated by a horizontal line, vertical black line is the standard error of the evoked response. Black and grey bars indicate muscle activity obtained before and after tizanidine intake, respectively. Data shown for the low and high background torque conditions. P values for each paired t-test are presented, bold italics for P < 0.05
The MLR activity was often increased with the high background load compared to the low background load (Fig. 4). A main-effect of background load was significant (P < 0.05) for the elbow and biarticular muscles (F(1,11−12) > 6.9). The shoulder muscles gave weaker changes that were not significant (posterior deltoid, F(1,12) = 1.45) or a significant trend in the opposite direction (pectoralis major, F(1,12) = 13.3).
The impact of tizanidine on the arm’s MLRs was inconsistent (Fig. 4). A significant main effect (P < 0.05) of tizanidine dosage was found in one elbow muscle and one biarticular (triceps lateral, F(1,12) = 7.8; triceps longus, F(1,11) = 6.5). In the other four muscles, a main effect of tizanidine was not significant (P > 0.05, F(1,11−12) < 1.8). Although there was a mean decrease in MLR in most comparisons with a particular background load (8/12), these changes were weak and variable. A significant difference was only obtained in 2 of 12 comparisons (P2 − sided < 0.05) which occurred with the two extensor muscles previously mentioned, triceps lateral and triceps longus. This pattern was not altered when examining the first 10 trials post-dosage, nor was a significant difference found between the MLRs observed for the first 10 and last 10 trials post-dosage (P2 − sided > 0.05). Furthermore, no changes were present in the earlier SLR epoch generated by a group I-spinal pathway (P2 − sided > 0.05).
As shown in several previous studies (Kurtzer et al. 2008; Pruszynski et al. 2011) the shoulder muscle’s MLR was evoked by perturbations causing initial motion at just the elbow (P1 − sided < 0.001, t(12) > 7.2) (Fig. 5). These multi-joint reflexes increased with the high background load compared to the low background load (P < 0.001, F(1,12) > 22), but did not vary with tizanidine exposure (P > 0.10, F(1,12) < 1.9). Nor did any comparisons at a particular background load indicate a significant change with tizanidine (P2 − sided > 0.05).
Mean R2 activity in shoulder muscles to elbow displacement. a Group evoked activity in the shoulder extensor to 100 pulse of flexion torque at both joints, a perturbation which initially caused motion at just the elbow. Black and grey traces show muscle activity obtained before and after tizanidine intake, respectively. b Each bar shows the group average baseline activity and evoked R2 (with standard error) separated by a horizontal line. Black and grey bars indicate muscle activity obtained before and after tizanidine intake, respectively. P value’s of each paired t-test are presented, bold italics for P < 0.05
Walking task
The walking task required subjects to freely walk at a natural pace while ramp-hold-release displacements were intermittently applied to their right ankle. These unpredictable perturbations (dorsiflexing at mid-stance to stretch soleus and plantarflexing at midswing to stretch tibialis anterior) did not disrupt their walking pattern before or after ingesting tizanidine. Figure 6 shows two examples of ankle motion with and without the perturbations. Nor was the activity of the two ankle muscles impacted by tizanidine during unperturbed trials (P2 − sided > 0.5, t < |0.6|).
Samples of servo-displacements applied to the ankle during walking. a Changing ankle position during walking on a treadmill at a natural speed. Thin and thick black traces show data obtained during unperturbed and perturbed trials, respectively. Perturbed trials involved a dorsiflexing servo-displacement triggered 200 ms after heel strike. b Changing ankle position during mid-swing. Perturbations involved a plantarflexing servo-displacement applied mid-swing
The dorsiflexing and plantarflexing perturbations reliably evoked MLRs in the stretched ankle muscles. Both muscles exhibited increased activity from baseline under normal conditions (P1 − sided < 0.01, t > 3.5) and following the tizanidine dosage (P1 − sided < 0.005, t > 4.3). However, these MLRs did not change with drug intake (P2 − sided > 0.3, t < |1.0|). Examples of individual subjects and group data are presented in Fig. 7.
Evoked activity in ankle muscles before and after tizanidine intake. a Evoked activity in an exemplar subject’s plantarflexor muscle stretched by the dorsiflexing servo-displacement shown in Fig. 6a, b. Data normalized to the peak activity of unperturbed gait (mid-stance), normalized units (nu). Thin and thick black traces show data obtained during unperturbed and perturbed trials, respectively, prior to tizanidine intake. Thin and thick grey traces show data obtained during unperturbed and perturbed trials, respectively, after tizanidine intake. Grey window indicates the MLR time epoch. b Group data of the plantarflexor’s MLR to these same conditions. Each bar shows the group average baseline activity and R2 separated by a horizontal line, vertical line is the standard error of the evoked response. Black and grey bars indicate muscle activity obtained before and after tizanidine intake, respectively. P value’s of two-sided paired t-test are presented. c Evoked activity in an exemplar subject’s dorsiflexor muscle stretched by the plantarflexing servo-displacement shown in Fig. 6c, d. Data normalized to the peak activity of unperturbed gait (mid-swing), normalized units (nu). Same format as a. d Group data of the dorsiflexor’s MLR to these same conditions
Sitting task
The sitting task required subjects to produce a dorsiflexion or plantarflexion torque at 20% MVC in the presence of unpredictable stretch perturbations. The dorsiflexing perturbation reliably evoked a MLR in the soleus (P1 − sided < 0.05, t = 2.1) whereas the plantarflexing perturbation had a less reliable impact on the MLR of tibialis anterior (P1 − sided = 0.12, t = 1.8). In either case, the ingestion of tizanidine did not diminish these reflex responses (P2 − sided > 0.4, t < |0.7|).
Subjective experience of tizanidine
Most subjects (18/20) reported alterations of their experiential state following tizanidine ingestion. These changes involved the common side-effects of somnolence, dry mouth, and dizziness. Altered experiences were first noticed within 30 min of dosing and were noticeably lessened by the end of data collection, approximately 150 min after ingestion.
Discussion
The primary purpose of our study was to use tizanidine, an alpha-2 adrenegric agonist that preferentially depresses transmission of group II signals to interneurons within the intermediate zone of the spinal cord, to quantify the relative contribution of group II afferents to the MLR of proximal upper limb muscles. We also examined the MLR of ankle muscles, initially as a control, since previous studies reported decreased MLR activity with tizanidine. As the MLR response is relatively small, we adjusted our muscle stretch parameters (higher amplitude and lower velocity) to optimize MLR response size (Grey et al. 2001).
The experiment yielded inconsistent effects: lowered responses in the elbow extensors, but not in the elbow flexors, shoulder muscles, or ankle muscles. Except for the stretch profile, there was no obvious difference in our procedures from previous work, however (Table 1). We utilized mechanical perturbations which elicited robust MLRs in all examined muscles. We provided a drug dosage identical to most previous studies and examined a post-ingestion period that overlapped with previous studies. To further guard against missing a transient effect we examined the earliest perturbations in the post-ingestion period and found no change in the pattern of responses, nor between the earliest and last batch of trials, nor in the multi-joint response of shoulder muscles. Our two-sided threshold of significance could be slighted as too severe but would make no difference for most contrasts including the ankle muscles.
A potential interpretation of our observations could be that MLRs of elbow extensors are more sensitive to tizanidine than for shoulder or ankle muscles. This would be consistent with a group II-spinal role in reflex activity of wrist flexion-elbow extension reminiscent of decerebrate posturing following severe damage below the red nucleus (Davis and Davis 1981). However, the fact that we failed to reproduce the tizanidine depressive effects on the MLRs of ankle muscles in 2 separate groups of subjects tested independently in two laboratories when optimizing for a large MLR response was unexpected.
Looking at the literature, previous studies have not reported uniform reliability of this drug on ankle muscle MLRs. For example, Corna et al. (1995) reported a depressed response in tibalis anterior during toe-down platform rotations but not in soleus during toe-up platform rotations. Yet, Grey and colleagues (2001) reported depressed soleus MLR to toe-up perturbations during walking (but did not examine tibialis responses to toe-down perturbations). These results suggest that tizanidine could have a more idiosyncratic effect than previously recognized. It is quite possible that such variable effects of tizanidine might be under-reported, as what may initially seem to be negative results are difficult to publish.
We adjusted stretch parameters to get an optimal MLR response during walking or sitting. This experimental choice was made to better quantify MLR modulation. It is also an attempt to recruit more group II afferents in the middle latency reflex response. We are aware that due to overlap in the sensitivity of the two muscle spindle systems (Edin and Vallbo 1990), the MLR still included contributions from both Group I and Group II inputs. Different stretch velocity profiles were needed during walking and sitting, and tuning was also done between participants. However, despite these methodological differences, no change in MLR amplitude was reported, suggesting that our findings are robust when the MLR is optimized. To compare with other experiments where MLR was not optimized would require applying a wide range of perturbations velocities in the same participants and the same experiment. This was not possible in the current experiment due to time constraints (we were already testing the arm and the leg in the same participants), but could constitute a logical next step in better characterizing the relationship between Group I and II inputs and tizanidine effects.
One should be careful to not over-interpret our results. This paper provides evidence that the effect of tizanidine on MLR attenuation might be more variable, and/or more sensitive to experimental conditions than initially expected. Interestingly, our results share interesting parallels with older work trying to tease out a group II contribution to the stretch reflex that used rapid stretches, vibration and nerve cooling (Matthews 1970, 1984, 1989; Desmedt 1978; Evart and Fromm 1981; Wiesendanger and Miles 1982; Mathews 1986). The conclusions from this work after many years of debate was that group II contribution is difficult to tease out and may vary according to several factors, including the experimental conditions used for testing (Matthews 1989a, b).
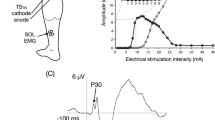
We do not posit that tizanidine is ineffectual. Specifically, the ambiguity of MLR attenuation in healthy subjects does not minimize tizanidine’s efficacy in ameliorating spasticity exhibited in clinical conditions (Wagstaff and Bryson 1997; Malanga et al. 2008; Mirbagheri et al. 2010). Brain trauma uncovers a number of reflex patterns that are normally suppressed, including group II transmission under descending control (Noga et al. 1995; Riddell et al. 1993, 1995). Tizanidine returns these patterns closer to normal, possibly by decreasing the MLR responsiveness (Maupas et al. 2004). Furthermore, resolving the ambiguity of MLR attenuation in healthy subjects does not eliminate the other lines of evidence for a group II-spinal contribution to the MLR. These include: (1) greater delay by nerve cooling for the MLR than SLR (Schieppati and Nardone1997; Simonetta-Moreau et al. 1999; Grey et al. 2001; Marque et al. 2005; Friemert et al. 2010; Uysal et al. 2009), (2) greater delay for the MLR than SLR for muscles with longer peripheral nerves (Chan et al. 1979; Nardone and Schiepatti 1998), (3) higher threshold for electrical stimulation of MLR than SLR (Lourenco et al. 2006; Marque et al. 2005; Simonetta-Moreau et al. 1999), and (4) less sensitivity to muscle vibration and presumably presynaptic inhibition by the MLR than SLR (Hendrie and Lee 1978; Bove et al. 2003). Still not all the evidence is consistent since securing a tourniquet to the limb has led to SLRs decreasing more than MLRs (Cody et al. 1987; Grey et al. 2001; Friemert et al. 2010), MLRs decreasing more than SLRs (Hayashi et al. 1987), and the two responses showing an equal decrease (Fellows et al. 1993). In conclusion, the impact of tizanidine on MLRs is relevant to a host of issues, but induces idiosyncratic effects in healthy subjects. We hope future studies will determine whether this indicates that tizanidine’s efficacy is altered by subtle changes in protocol or that group II afferents do not substantially contribute to MLRs.
References
Af Klint R, Mazzaro N, Nielsen JB, Sinkjaer T, Grey MJ (2010) Load rather than length sensitive feedback contributes to soleus muscle activity during human treadmill walking. J Neurophysiol 103:2747–2756
Blanchette A, Lambert S, Richards CL, Bouyer LJ (2011) Walking while resisting a perturbation: effects on ankle dorsiflexor activation during swing and potential for rehabilitation. Gait Posture 34:358–363
Bouyer LJ (2011) Chap. 8—challenging the adaptive capacity of rhythmic movement control: from denervation to force field adaptation. Prog Brain Res 188:119–134
Bove M, Nardone A, Schieppati M (2003) Effects of leg muscle tendon vibration on group Ia and group II reflex responses to stance perturbation in humans. J Physiol 550:617–630
Bras H, Jankowska E, Noga B, Skoog B (1990) Comparison of effects of various types of NA and 5-HT agonists on transmission from group II muscle afferents in the cat. Eur J Neurosci 2:1029–1039
Chan CW, Jones GM, Kearney RE, Watt DG (1979) The ‘late’ electromyographic response to limb displacement in man. I. Evidence for supraspinal contribution. Electroencephalogr Clin Neurophysiol 46:173–181
Christensen LO, Petersen N, Andersen JB, Sinkjaer T, Nielsen JB (2000) Evidence for transcortical reflex pathways in the lower limb of man. Prog Neurobiol 62(3):251–272
Christensen LO, Andersen JB, Sinkjaer T, Nielsen J (2001) Transcranial magnetic stimulation and stretch reflexes in the tibialis anterior muscle during human walking. J Physiol 531(Pt 2):545–557
Cody FW, Goodwin CN, Richardson HC (1987) Effects of ischaemia upon reflex electromyographic responses evoked by stretch and vibration in human wrist flexor muscles. J Physiol 391:589–609
Corna S, Grasso M, Nardone A, Schieppati M (1995) Selective depression of medium-latency leg and foot muscle responses to stretch by an alpha 2-agonist in humans. J Physiol 484:803–809
Crago PE, Houk JC, Hasan Z (1976) Regulatory actions of human stretch reflex. J Neurophysiol 39:925–935
Davis RA, Davis L (1981) Decerebrate rigidity in animals. Neurosurgery 9:79–89
Day BL, Riescher H, Struppler A, Rothwell JC, Marsden CD (1991) Changes in the response to magnetic and electrical stimulation of the motor cortex following muscle stretch in man. J Physiol 433:41–57
Desmedt JE (ed) (1978) Cerebral motor control in man: long loop mechanisms. Progress in clinical neurophysiology, vol. 4, Karger, Basel
Diener HC, Bootz F, Dichgans J, Bruzek W (1983) Variability of postural “reflexes” in humans. Exp Brain Res 52:423–428
Doemges F, Rack PM (1992) Task-dependent changes in the response of human wrist joints to mechanical disturbance. J Physiol 447:575–585
Edin BB, Vallbo AB (1990) Dynamic response of human muscle spindle afferents to stretch. J Neurophysiol 63(6):1297–1306
Evarts EV, Fromm C (1981) Transcortical reflexes and servo control of movement. Can J Physiol Pharmacol 59:757–775
Fellows SJ, Domges F, Topper R, Thilmann AF, Noth J (1993) Changes in the short- and long-latency stretch reflex components of the triceps surae muscle during ischaemia in man. J Physiol 472:737–748
Friemert B, Franke S, Gollhofer A, Claes L, Faist M (2010) Group I afferent pathway contributes to functional knee stability. J Neurophysiol 103:616–622
Gielen CC, Ramaekers L, van Zuylen EJ (1988) Long-latency stretch reflexes as co-ordinated functional responses in man. J Physiol 407:275–292
Graham KM, Moore KD, Cabel DW, Gribble PL, Cisek P, Scott SH (2003) Kinematics and kinetics of multijoint reaching in nonhuman primates. J Neurophysiol 89:2667–2677
Grey MJ, Ladouceur M, Andersen JB, Nielsen JB, Sinkjaer T (2001) Group II muscle afferents probably contribute to the medium latency soleus stretch reflex during walking in humans. J Physiol 534:925–933
Hammond PH (1956) The influence of prior instruction to the subject on an apparently involuntary neuro-muscular response. J Physiol 132:17–18
Hayashi R, Becker WJ, White DG, Lee RG (1987) Effects of ischemic nerve block on the early and late components of the stretch reflex in the human forearm. Brain Res 403:341–344
Hendrie A, Lee RG (1978) Selective effects of vibration on human spinal and long-loop reflexes. Brain Res 157:369–375
Kimura T, Haggard P, Gomi H (2006) Transcranial magnetic stimulation over sensorimotor cortex disrupts anticipatory reflex gain modulation for skilled action. J Neurosci 26:9272–9281
Kurtzer IL, Pruszynski JA, Scott SH (2008) Long-latency reflexes of the human arm reflect an internal model of limb dynamics. Curr Biol 18:449–453
Kurtzer I, Pruszynski JA, Scott SH (2010) Long-latency and voluntary responses to an arm displacement can be rapidly attenuated by perturbation offset. J Neurophysiol 103:3195–3204
Lee RG, Tatton WG (1982) Long latency reflexes to imposed displacements of the human wrist: dependence on duration of movement. Exp Brain Res 45:207–216
Lewis GN, Perreault EJ, MacKinnon CD (2005) The influence of perturbation duration and velocity on the long-latency response to stretch in the biceps muscle. Exp Brain Res 163:361–369
Lourenco G, Iglesias C, Cavallari P, Pierrot-Deseilligny E, Marchand-Pauvert V (2006) Mediation of late excitation from human hand muscles via parallel group II spinal and group I transcortical pathways. J Physiol 572:585–603
Mackel R, Brink EE, Nakajima Y (1984) Action of tizanidine on responses of forearm flexors and extensors to torque disturbances. J Neurol Neurosurg Psychiatry 47:1109–1116
Malanga G, Reiter RD, Garay E (2008) Update on tizanidine for muscle spasticity and emerging indications. Expert Opin Pharmacother 9:2209–2215
Marchand-Pauvert V, Nicolas G, Marque P, Iglesias C, Pierrot-Deseilligny E (2005) Increase in group II excitation from ankle muscles to thigh motoneurones during human standing. J Physiol 566:257–271
Marque P, Nicolas G, Simonetta-Moreau M, Pierrot-Deseilligny E, Marchand-Pauvert V (2005) Group II excitations from plantar foot muscles to human leg and thigh motoneurones. Exp Brain Res 161(4):486–501
Marsden CD, Rothwell JC, Day BL (1983) Long-latency automatic responses to muscle stretch in man: origin and function. Adv Neurol 39:509–539
Matthews PB (1970) A reply to criticism of the hypothesis that the group II afferents contribute excitation to the stretch reflex. Acta Physiol Scand 79(3):431–433
Matthews PB (1984) Evidence from the use of vibration that the human long-latency stretch reflex depends upon spindle secondary afferents. J Physiol 348:383–415
Matthews PB (1986) What are the afferents of origin of the human stretch reflex, and is it a purely spinal reaction? Prog Brain Res 64:55–66
Matthews PB (1989a) Analysis of human long-latency reflexes by cooling the peripheral conduction pathway; which afferents are involved? Prog Brain Res 80:103–112 (discussion 57–60)
Matthews PB (1989b) Long-latency stretch reflexes of two intrinsic muscles of the human hand analysed by cooling the arm. J Physiol 419:519–538
Matthews PB, Farmer SF, Ingram DA (1990) On the localization of the stretch reflex of intrinsic hand muscles in a patient with mirror movements. J Physiol 428:561–577
Maupas E, Marque P, Roques CF, Simonetta-Moreau M (2004) Modulation of the transmission in group II heteronymous pathways by tizanidine in spastic hemiplegic patients. J Neurol Neurosurg Psychiatry 75:130–135
Meskers CG, Schouten AC, Rich MM, de Groot JH, Schuurmans J, Arendzen JH (2010) Tizanidine does not affect the linear relation of stretch duration to the long latency M2 response of m. flexor carpi radialis. Exp Brain Res 201:681–688
Mirbagheri MM1, Chen D, Rymer WZ (2010) Quantification of the effects of an alpha-2 adrenergic agonist on reflex properties in spinal cord injury using a system identification technique. J Neuroeng Rehabil 7:29
Nakazawa K, Yamamoto SI, Yano H (1997) Short- and long-latency reflex responses during different motor tasks in elbow flexor muscles. Exp Brain Res 116:20–28
Nardone A, Schieppati M (1998) Medium-latency response to muscle stretch in human lower limb: estimation of conduction velocity of group II fibres and central delay. Neurosci Lett 249(1):29–32
Noel M, Cantin B, Lambert S, Gosselin CM, Bouyer LJ (2008) An electrohydraulic actuated ankle foot orthosis to generate force fields and to test proprioceptive reflexes during human walking. IEEE Trans Neural Syst Rehabil Eng 16:390–399
Noel M, Fortin K, Bouyer LJ (2009) Using an electrohydraulic ankle foot orthosis to study modifications in feedforward control during locomotor adaptation to force fields applied in stance. J Neuroeng Rehabil 6:16
Noga BR, Jankowska E, Skoog B (1995) Depression of transmission from group II muscle afferents by electrical stimulation of the cuneiform nucleus in the cat. Exp Brain Res 105:25–38
Petersen N, Christensen LO, Morita H, Sinkjaer T, Nielsen J (1998) Evidence that a transcortical pathway contributes to stretch reflexes in the tibialis anterior muscle in man. J Physiol 512 (Pt 1):267–276
Pruszynski JA, Kurtzer I, Scott SH (2008) Rapid motor responses are appropriately tuned to the metrics of a visuospatial task. J Neurophysiol 100:224–238
Pruszynski JA, Kurtzer I, Lillicrap TP, Scott SH (2009) Temporal evolution of “automatic gain-scaling. J Neurophysiol 102:992–1003
Pruszynski JA, Kurtzer I, Nashed JY, Omrani M, Brouwer B, Scott SH (2011) Primary motor cortex underlies multi-joint integration for fast feedback control. Nature 478:387–390
Riddell JS, Jankowska E, Eide E (1993) Depolarization of group II muscle afferents by stimuli applied in the locus coeruleus and raphe nuclei of the cat. J Physiol 461:723–741
Riddell JS, Jankowska E, Huber J (1995) Organization of neuronal systems mediating presynaptic inhibition of group II muscle afferents in the cat. J Physiol 483:443–460
Schieppati M, Nardone A (1997) Medium-latency stretch reflexes of foot and leg muscles analysed by cooling the lower limb in standing humans. J Physiol 503:691–698
Schuurmans J, de Vlugt E, Schouten AC, Meskers CG, de Groot JH, van der Helm FC (2009) The monosynaptic Ia afferent pathway can largely explain the stretch duration effect of the long latency M2 response. Exp Brain Res 193:491–500
Scott SH (1999) Apparatus for measuring and perturbing shoulder and elbow joint positions and torques during reaching. J Neurosci Methods 89:119–127
Shemmell J, An JH, Perreault EJ (2009) The differential role of motor cortex in stretch reflex modulation induced by changes in environmental mechanics and verbal instruction. J Neurosci 29:13255–13263
Simonetta-Moreau M, Marque P, Marchand-Pauvert V, Pierrot-Deseilligny E (1999) The pattern of excitation of human lower limb motoneurones by probable group II muscle afferents. J Physiol 517(Pt 1):287–300
Singh K, Scott SH (2003) A motor learning strategy reflects neural circuitry for limb control. Nat Neurosci 6:399–403
Sinkjaer T, Andersen JB, Larsen B (1996) Soleus stretch reflex modulation during gait in humans. J Neurophysiol 76:1112–1120
Skoog B (1996) A comparison of the effects of two antispastic drugs, tizanidine and baclofen, on synaptic transmission from muscle spindle afferents to spinal interneurones in cats. Acta Physiol Scand 156:81–90
Soechting JF, Lacquaniti F (1988) Quantitative evaluation of the electromyographic responses to multidirectional load perturbations of the human arm. J Neurophysiol 59:1296–1313
Toft E, Sinkjaer T, Andreassen S, Larsen K (1991) Mechanical and electromyographic responses to stretch of the human ankle extensors. J Neurophysiol 65(6):1402–1410
Tsuji T, Rothwell JC (2002) Long lasting effects of rTMS and associated peripheral sensory input on MEPs, SEPs and transcortical reflex excitability in humans. J Physiol 540:367–376
Uysal H, Larsson LE, Efendi H, Burke D, Ertekin C (2009) Medium-latency reflex response of soleus elicited by peroneal nerve stimulation. Exp Brain Res 193:275–286
Uysal H, Kizilay F, Inel SE, Ozen H, Pek G (2012) Medium-latency reflex response elicited from the flexor carpi radialis by radial nerve stimulation. Exp Brain Res 217:223–235
Wagstaff AJ, Bryson HM (1997) Tizanidine. A review of its pharmacology, clinical efficacy and tolerability in the management of spasticity associated with cerebral and spinal disorders. Drugs 53:435–452
Wiesendanger M, Miles TS (1982) Ascending pathway of low-threshold muscle afferents to the cerebral cortex and its possible role in motor control. PhysiolRev 62:1234–1270
Acknowledgements
The present research was supported by a grant from the Natural Sciences and Engineering Research Council of Canada and a grant from the Canadian Institute of Health Research (CIHR). SHS is supported by a GlaxoSmithKline-CIHR chair in Neuroscience. We wish to thank Kim Moore, Helen Bretzke, and Justin Peterson for technical and logistic support.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Isaac Kurtzer and Laurent J. Bouyer are co-first authors.
Rights and permissions
About this article
Cite this article
Kurtzer, I., Bouyer, L.J., Bouffard, J. et al. Variable impact of tizanidine on the medium latency reflex of upper and lower limbs. Exp Brain Res 236, 665–677 (2018). https://doi.org/10.1007/s00221-017-5162-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00221-017-5162-6