Abstract
In bipedal gait, the initiation of the first step is preceded by a complex sequence of movements which shift the centre of mass of the body towards the stance foot to allow for a step of the swing foot. These anticipatory postural adjustments (APAs) have been investigated in order to elucidate movement strategies in healthy and diseased persons. We studied the influence of several external parameters (age, type of step initiation) on APAs and investigated whether Parkinsonian patients may have different APAs. As a result, we found that externally elicited steps were preceded by faster and larger APAs than self-timed steps. Parkinsonian patients without the freezing of gait (FOG) phenomenon showed overall slightly reduced APAs but did not clearly differ from patients with FOG. Multiple APAs were seen in up to 25 % of the steps of the patients and in a much lower percentage of the steps of control subjects. The results indicate that APAs are significantly influenced by the timing of a step, i.e. are larger in externally elicited steps. The patients showed an overall preserved APA pattern but slowed movements and amplitude, indicating that increased bradykinesia due to progressive illness is a plausible explanation for these findings. The freezing phenomenon is not explained by a general absence or massive reduction in APA measures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anticipatory postural adjustments (APAs) consist of muscular synergies to prepare the body either to react to an upcoming event that may challenge postural equilibrium or to take a step. Only this second type of APA will be considered in this paper.
Recently, APAs have attracted attention because they are crucial for initiating a step, and gait initiation failure is frequent in patients with neurodegenerative diseases, especially Parkinson’s disease (PD) (Nutt et al. 2011). Therefore, the question of whether reduced APAs may be crucial for step initiation failure is the main topic of this paper. To this end, we investigated two alternative hypotheses. The first hypothesis was that APAs show a gradual decline in this order: young subjects > elderly subjects > PD patients > PD patients with gait initiation failure (freezers). The alternative hypothesis was that freezers have absent or massively reduced APAs which then could be taken as the major reason for the freezing phenomenon. Because steps can be elicited by external cues or an internal command, we also assessed the effect of external cueing on the APAs in the different groups.
APA subdivisions
Before taking a step, the swing foot must be cleared off the ground and the body must be enabled to fall forward. This is achieved by first unloading the stance foot which can be seen as a transient lateral shift of the centre of pressure towards the swing foot. This pushes the centre of mass towards the stance foot and unloads the swing foot. Simultaneously with this lateral CoP shift, the forefeet are actively lifted, whereby the CoP moves towards the heels (backwards). This strategy moves the centre of mass in front of the CoP and thus causes the body to fall forward, supported by the stance foot only. The first phase of the CoP shift towards the swing foot was termed the ‘imbalance phase’ and the second (towards the stance foot) the ‘unloading phase’ (Crenna et al. 2006). Here, we use APA1 and APA2 for these two phases. The end of the APA1 phase was labelled ‘release’ by Halliday et al. (1998) and was shown to correspond to the ‘heel-off’ instance of the swing foot. APAs can be monitored with a force plate on which the subject stands and which records the characteristic excursions of the CoP. APAs can also be recorded with electromyography from leg muscles (Crenna and Frigo 1991) or by accelerometers (Mancini et al. 2016).
APA and age
Children seem to develop adult typical APAs no earlier than age 4–5 (Assaiante et al. 2000), but they are still incomplete at the age of 4–6 (Malouin and Richards 2000). The elderly need more time for postural adjustments during gait while approaching an obstacle (Laessoe and Voigt 2013) and APAs related to external pertubation are slow and delayed (Woollacott and Manchester 1993; Kanekar and Aruin 2014a). Step initiation APAs have been investigated without clear evidence of age-related changes (Halliday et al. 1998). Another study by Uemura et al. (2012) detected more prolonged APAs in older adults with a fear of falling (FoF) than without FoF. We are not aware of further systematic investigations of age-related changes in step initiation APAs.
APA in Parkinson’s disease
Parkinson’s disease (PD) patients generally show a reduced APA magnitude and a longer APA duration (Lee et al. 1995; Burleigh-Jacobs et al. 1997; Mancini et al. 2009; Rocchi et al. 2012) and a reduced ability to adjust APAs in relation to a wider initial stance as compared to healthy subjects (Rocchi et al. 2006). The reduction in APA measures in PD is partially compensated by administration of levodopa (Rocchi et al. 2006). Reduced APAs in PD have therefore been discussed as a possible cause of the freezing of gait phenomenon (Nutt et al. 2011). In fact, patients with freezing had absent APAs more frequently than patients without freezing (Delval et al. 2014). However, this hypothesis was challenged by the findings that a freezing episode may be preceded by multiple APAs which associates the freezing problem with the failure to initiate a step (Jacobs et al. 2009b). This hypothesis is supported by an investigation by Mensink et al. (2014) who found an influence of load weights on (increased) freezing episodes but not on the actual APA mechanism.
Several factors can influence APAs of PD patients. Gantchev et al. (1996) found a positive influence on APAs of PD patients with a specified restriction of the movement initiation such as a single step in comparison with starting walking. When steps are initiated in response to an external command, CoP excursions during the APA phase are larger. This has been shown for acoustic stimuli (Delval et al. 2014) as well as for electric stimuli applied to the hand or earlobe (Burleigh-Jacobs et al. 1997). However, another group found no effect of acoustic stimuli in gait initiation in a group of PD patients (Jiang and Norman 2006). Cognitive influences also seem to have an influence on stepping behaviour. Threatening emotions involved a higher speed of step initiation in PD patients but also healthy older controls (Naugle et al. 2012). Dual-tasking was also shown to have implications on APAs with less displacement of the APA and a lower velocity, while no differences were found concerning different kinds of dual-tasking (Nocera et al. 2013). Our study addresses whether normal ageing is associated with a significant reduction in APAs and/or what influence the stage of Parkinson’s disease may have on APAs in this group. Finally, the impact of the mode of elicitation of the first step (externally/internally triggered) on parameters of APA in different groups was also assessed.
Methods
Subjects
Sixty healthy control subjects of different ages (40–73 years), and 16 PD patients with and 10 PD patients without the freezing phenomenon were recruited from relatives of the hospital staff and from the outpatient clinic for movement disorders at our university hospital. Written informed consent was obtained from all individual participants included in the study. This study was approved by the local research ethics committee and was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. All subjects answered the freezing of gait questionnaire (Giladi et al. 2000) and the International Physical Activity Questionnaire (IPAQ) and underwent a neurological assessment. Persons with evidence of dementia, polyneuropathy, arthrosis or other gait-impairing conditions or who needed to use walking aids were excluded. Patients with brain stimulators were not included. UPDRS part III scores were obtained immediately prior to testing. Parkinsonian patients were divided into ‘freezers’ (PD-FZ) and ‘non-freezers’ (PD) on the basis of scoring above 0 on question 3 of the FOG-Q (Giladi et al. 2000) (‘Do you feel that your feet get glued to the floor while walking…?’) or scoring 7 or above in the FOG-Q. All patients took their regular medication. All subjects were divided into five groups according to age, disease and presence or absence of freezing episodes.
Data acquisition
To obtain APAs, the CoP in the epoch before a step was recorded on a treadmill (FDM-T, Zebris medical GmbH, Isny, Germany) which was equipped with an array of pressure-sensitive sensors (each 8.5 × 8.5 mm, 100 Hz sampling rate) underneath the belt, which was stationary during all tests. Subjects were asked to first stand comfortably. They were allowed to choose the foot distance, but heels had to be at the same point on the sagittal axis. Ten self-paced steps and ten steps immediately after the flash of a light (external trigger) were made. The order of the blocks of self-paced and cued steps was varied randomly between subjects. Subjects were asked to ‘start walking’ up to the security bar of the treadmill, which was reached after one or two steps. There were no instructions concerning which foot to use, velocity speed or number of steps in either of the conditions.
Data analysis
The CoP of each foot and the CoP of both feet were calculated by software supplied by the treadmill manufacturer (Fig. 1a, b). To standardize the foot distance, all medio-lateral CoP data were scaled with a factor (20/foot distance in cm). From these data, MATLAB (MathWorks, Natick, MA) algorithms (Fig. 1c, d) computed the following outcome parameters: the beginning of APA was defined as the moment when the CoP velocity of both feet (x or y) was above 1.5 mm/10 ms. This proved to be very reliable and could be corrected manually if necessary. The end of APA was at the beginning of the first step (toe-off of swing foot). From these instances, APA duration was calculated. This epoch was divided into APA1 (imbalance phase, CoP shift towards the swing foot) and APA2 (unloading phase, lateral displacement of the CoP towards stance foot) (Crenna et al. 2006). The length of the APA CoP excursion (APA CoP length) and the peak APA velocity were computed by calculating the Euclidic distance between adjacent CoP points and referencing this to Δt. Peak APA in a medio-lateral direction (max. APA lateral) was marked and denoted as the separation point between APA1 and APA2 (Fig. 1d). Peak APA in a posterior (Max APA post) direction was marked as well. Additionally, first step duration, first step velocity and first step length were calculated. To detect multiple APAs, oscillations (peak or trough) of the CoP in the lateral direction occurring before the APA which immediately preceded the step were manually marked when they exceeded ±10 mm of the preceding baseline (Fig. 2). The occurrence of these pre-APA oscillations was statistically evaluated.
Recording of a two-step sequence and preceding APAs. a Trace of the CoP in ant–post position (right foot, green; left foot, red; both feet, blue). The right foot takes the first step. APA onset is marked with a vertical bar and denotes the beginning of the backward excursion of the CoP. Step onset and end are marked with arrows. b Medio-lateral position of CoP, colours as in a. Vertical bar denotes the beginning of APA, here the lateral excursion of the CoP towards the swing foot (green). This phase is called APA1. c CoP in x–y axis, colours as in a. The blue trace shows the CoP of both feet as it moves from the centre towards the swing foot (APA1) and then to the stance foot. d Red CoP trace (both feet) during APA in medio-lateral direction. The peak of the red curve (marked with a cross) denotes the maximum CoP excursion towards the swing foot and is called ‘Max APA lateral’. This is the end of the APA1-phase. The green trace shows the CoP excursion in an ant–post direction. The cross denotes ‘Max APA post’, which is always negative
Different types of pre-APA oscillations. Representative samples of lateral pre-APA CoP oscillations (multiple APAs). Time ‘0’ denotes the incidence when the swing foot lifts off. a ‘Normal APA’ with no or minimum pre-APA oscillation, b one pre-APA oscillation (arrow), c four pre-APA oscillations in a patient with advanced disease
Statistics
Clinical scores of the patients were correlated with several APA parameters (averaged for each patient) by computing Pearson’s correlation coefficient (MATLAB). Statistics were performed with MATLAB on data of individual steps (raw data) of all healthy subjects (correlation analyses to determine age-related differences only) and on averaged data of all subjects which consisted of the averaged results of 8–10 self-paced and 8–10 externally triggered steps per person with SPSS 22 (Microsoft). APA and step variables were checked for normal distribution with the MATLAB routine ‘jbtest’, and, if necessary, transformed using the Box–Cox power transformation by applying appropriate exponents to the variable. Each variable was analysed once with a mixed linear models ANOVA with the factors ‘group’ (five levels) and ‘trigger’ (two levels: cued or self-paced step). If significant differences were found between groups, Scheffé post hoc tests were carried out.
Results
Subjects
Sixty healthy control subjects (CONT) were split into three groups according to age (40–50, 51–60 and >60) with 20 subjects in each group. Two more groups consisted of Parkinsonian patients without freezing (PD; n = 10) and with freezing (PD-FZ; n = 16). The mean age of the two PD groups were not significantly different (PD: 63.6 years; PD-FZ: 65.7 years). The mean Hoehn and Yahr score was 2.55 (s.d. 0.44) in the PD group and 2.88 (s.d. 0.62) in the PD-FZ group. The mean disease duration of the patients was not significantly shorter in the PD group without freezing (7.67, vs. 11.00). Further details are provided in Table 1.
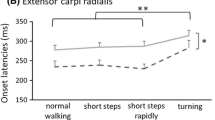
Step latency in externally triggered steps
Latency between the trigger signal and the first step are listed in Table 1. An ANOVA revealed a significant effect of ‘group’ (F = 25, df = 4; p = 0.0001). Post hoc tests revealed significant differences between PD-FZ and all other groups (p < 0.05), i.e. freezers were slower (Table 1).
Correlation of APA with age and trigger mode, healthy subjects (n = 60)
Step length, step velocity, APA duration, lateral and ant–post APA were investigated for their possible correlation with age (Pearson’s correlation). The only significant correlation was found between age and duration of APA1 during externally elicited steps (r = −0.33, p = 0.01). Thus, in this group, older subjects showed a shorter APA1 duration, but age had no significant influence on any other APA parameter or on step length or step velocity.
Comparison between groups
The following parameters were analysed with a mixed linear models ANOVA to detect possible differences between groups (n = 5) and mode of step initiation (trigger: self-paced/cued): step duration, step length, step velocity, APA1 duration, APA2 duration, peak APA CoP in a lateral direction (max. APA lateral) and peak APA in a posterior direction (max. APA post).
Step length differed between groups (F = 4.6, df = 4, p = 0.002). Post hoc tests revealed significant differences between young CONT and PD-FZ (p = 0.014) as well as between middle-aged CONT and PD-FZ (p = 0.013). Externally elicited steps were significantly longer than self-paced steps (F = 11; df = 1, p < 0.001) (Fig. 3).
Step velocity differed between groups (F = 4.6, df = 4, p = 0.002). Post hoc tests revealed significant differences between young CONT and PD-FZ (p = 0.015) as well as between middle-aged CONT and PD-FZ (p = 0.008). Externally elicited steps were significantly faster than self-paced steps (F = 115; df = 1, p < 0.000).
Step duration did not differ significantly between the five groups. Externally elicited steps were of significantly shorter duration than self-paced steps (F = 67, df = 1, p = 0.0001).
Max. APA lateral: the factor ‘group’ was highly significant (F = 7.1; df = 4; p = 0.001) as was the factor ‘trigger’ (F = 15; df = 1; p = 0.001), meaning that externally elicited steps had larger lateral APA amplitudes (Fig. 4). Post hoc tests showed that APA lateral was significantly smaller in PD-FZ when compared to the three groups of healthy subjects (p = 0.06; p = 0.003; p = 0.001) but PD-FZ did not differ from PD (p = 0.64).
Max. APA post showed a significant influence of ‘group’ (F = 2.6; df = 4; p = 0.042) but no single post hoc test showed significant differences between the groups (PD vs. PD-FZ: p = 0.47, elderly CONT vs. PD-FZ: p = 0.056).
APA-1 duration was not significantly different between groups. The effect of ‘trigger’ was significant (F = 13; df = 1, p < 0.000), meaning that duration was shorter in externally triggered steps.
APA-2 duration was significantly different between groups (F = 3.9, df = 4; p = 0.005) and post hoc tests showed significant differences between PD-FZ and elderly healthy persons only. The effect of ‘trigger’ was significant (F = 170; df = 1, p < 0.000) (duration shorter in externally triggered steps).
Correlation between clinical scores and APA data
The scores of three clinical rating scales (UPDRS III, Hoehn and Yahr, FOG questionnaire) were correlated (Pearson’s correlation coefficient) with several APA and step parameters of the patients (PD and PD-FZ, n = 26). The UPDRS III scores were significantly negatively correlated with the length of the CoP shift in externally triggered steps (r = −0.54, p = 0.005), meaning that more severely affected patients had smaller CoP excursions during the APA phase. The Hoehn and Yahr score was significantly correlated with the APA duration in externally triggered steps (r = 0.4; p = 0.043). The FOG score was negatively correlated with maximum velocity during the APA-1 phase in self-initiated steps (r = −0.39; p = 0.047), meaning that patients with a higher freezing score had a lower peak CoP velocity during the APA-1 phase.
Pre-APA oscillations of the CoP in a lateral direction
In several CoP traces, we noted lateral oscillations before the beginning of the APA (Fig. 2). Before externally triggered steps, control subjects (all ages) had at least one oscillation in 5 % of steps but in 25 % of self-elicited steps (Fig. 5). Multiple APAs (3 or 4 pre-APA oscillations) were seen in 24 (PD) and 25 % (PD-FZ) before self-elicited steps. A statistical comparison (ANOVA) was performed on the number of pre-APA oscillations for each step (range: 0–4). The factors were ‘group’ and ‘trigger’ (self-paced vs. extr. triggered step). It became clear that both factors were significant (group: F = 7.4, df = 2, p = 0.001; trigger: F = 54, df = 1, p < 0.001), meaning that self-initiated steps showed more pre-APA oscillations. Concerning the effect of ‘group’, post hoc tests revealed that CONT (all ages) differed significantly from PD and PD-FZ (more pre-APA oscillations in both PD groups), but both PD groups showed no significant differences in the number of pre-APA oscillations. The correlation between the number of pre-APA oscillations in the PD-FZ group and the FOG score was not significant (p = 0.36).
Percentage of one, two, three or four pre-APA oscillations in five groups. Oscillations (peak or trough) of the CoP in the lateral direction occurring before APA start were manually marked when they exceeded ±10 mm of the preceding baseline. The maximum number of oscillations was four (i.e. two full circles of sinusoidal oscillations). It is evident that self-initiated steps are preceded by more oscillations and that up to four pre-APA oscillations also occur in healthy control subjects
Discussion
Our results indicate that the ability to generate ‘normal’ APAs does not decline with age, is not significantly different in healthy subjects and moderately affected PD patients (without freezing) and is not significantly different between patients with and without freezing. Additionally, we found that cued steps are different from self-paced steps and a difference was also found between APAs preceding cued and self-paced steps.
Self-paced versus cued steps
Externally elicited steps were larger (on average 5 %), faster and of shorter duration than self-triggered steps and show a clear difference in several APA parameters: APAs are of shorter duration but the CoP excursions are larger in the ant–post as well as in the lateral direction. It seems as if the external command is able to elicit a faster and more efficient preparation of the first step. The biomechanical explanation for this observation is probably very simple: to quickly initiate a step it is necessary to shift the CoP of the feet far back to the heels and very laterally towards the swing foot (during APA1) so that the body will quickly fall into the desired direction. An EMG analysis of self-initiated and externally triggered stepping involving healthy subjects and PD patients was reported (Hiraoka et al. 2006). The authors found that the EMG burst of the tibialis anterior muscle of the swing foot was much higher in externally elicited movements and this was true for both groups, but PD patients had overall reduced tibialis anterior muscle activity. When steps of different velocity were required (after an external command), the magnitude of the M. tibialis ant activation as well as the amount of posterior CoP shift depended on the velocity of the steps they had to make (slow/natural/fast) (Crenna and Frigo 1991). Therefore, APA measures clearly correlate with the timing of a step and this mechanism of intentionally generating larger and faster APAs after the imperative stimulus was preserved in our study in PD patients both with and without the freezing phenomenon. Similar results were found when auditory cueing was used to initiate a step (Delval et al. 2014). These authors showed that auditory cueing improved start hesitation in freezers. Most likely, as was reported for gait on a treadmill with two different visual cues (Hanakawa et al. 1999), the lateral premotor cortex is also active in externally elicited postural adjustments and generates faster movements even in the ‘off-medication’ state or ‘off-stimulation’ state (Schenk et al. 2003; Michely et al. 2015) as compared to the mesial premotor system (supplementary motor area, SMA). The same is true for the administration of Levodopa in PD. Externally triggered steps did not have larger APAs in the medically treated PD patients as compared to when the patients were in the off-drug state, whereas there was a difference when no levodopa had been given (Burleigh-Jacobs et al. 1997). It is interesting to note that Jacobs et al. (2009a) found faster APAs with the same amplitude after inhibitory transcranial magnetic stimulation of the SMA and this APA acceleration was pronounced in subjects with PD. This would indicate that the SMA has no impact on the amplitude of the APA but an inhibitory function with respect to APA timing. Preceding the actual APA, self-timed steps had many more pre-APA oscillations in our sample (in 25 % of steps in healthy subjects), indicating that the decision to take a step may be embedded within a transitory phase in which several small APAs are common even in healthy people and much more in the patients due to their reduced ability to initiate a proper leg movement.
Are APAs affected by age?
When APAs are generated in preparation for an externally applied stimulus that affects postural stability (which is not under discussion in this work), advanced age significantly delays their beginning, reduces their amplitude and increases the intensity of compensatory postural adjustments as a reaction to the perturbation (Woollacott and Manchester 1993; Kanekar and Aruin 2014b). The effect of age on APAs as preparation for a step has not yet been systematically investigated in larger groups. A comparison between APA parameters and step size in young (mean 27 years) and elderly healthy subjects (mean 60 years) showed that anterior–posterior displacement of the CoP was significantly reduced in the elderly but other parameters were not and the authors concluded: ‘There is a trend for the variables to be smaller, slower and less forceful when comparing the young to the elderly…’ (Halliday et al. 1998). Our youngest subject was 40 years old, and therefore, comparability to the mentioned study is limited. Our sample comprises the largest group of healthy subjects in whom an age effect on APAs was investigated. Like the previous study, we found that age in the range investigated here had no significant influence on any APA parameter with the exception of one (duration of APA1). Thus, APA seems to be a fairly stable motor sequence unaffected by age.
Are APAs different in PD?
In our study, no differences were found in the backward CoP shift (post APA component) between groups, and lateral CoP shift towards the swing foot was reduced in severely affected PD patients (freezers) only, but not in moderately affected patients. This pattern is similar to a study investigating untreated PD patients in an early stage of the disease as far as backward CoP shift is concerned (Mancini et al. 2009); however, these authors also saw significantly reduced lateral CoP shift in untreated early-stage PD patients. Lateral shift was also reduced in moderately affected PD patients in the study by Jacobs et al. (2009a), whereas the APA timing was normal. In summary, our data suggest that APAs are rather well preserved in moderately affected and treated PD patients without freezing. Small differences (not significant in our sample) can be attributed to disease-associated bradykinesia (which is accessible to levodopa treatment) but not to a general deficit in generating APAs.
Are APAs different in freezers?
The freezing phenomenon in Parkinson’s disease is far from being understood. Reduced APAs could serve as an explanation for why a step cannot be initiated. However, exaggerated APA movements in the form of ‘trembling in place’ have also been postulated as possible sources of freezing (Jacobs et al. 2009b). In our study, there was no evidence for substantially different APAs in the freezers as compared to PD patients without freezing: not a single APA parameter showed a statistically significant difference between patients with and without the freezing phenomenon. The discrepancies between these results and results of other groups cannot easily be resolved: in the work of Delval et al. (2014). the authors noted that APAs were more frequently absent in freezers as compared to non-freezers. In our study, ‘absence’ was not a criterion, but reduced or absent APAs entered the statistical evaluation as very low amplitudes. We found similar results as the Delval group concerning multiple APAs. Obviously, there is no fundamental reduction or absence of the mechanisms which are responsible for APA generation in freezers. The freezing phenomenon may thus be related to other abnormalities: Freezers seem to have pathoanatomical abnormalities in the form of significantly reduced right hemisphere pedunculopontine nucleus fibre tract volume compared with healthy controls (Fling et al. 2013). Also, dual task interference during gait is higher in freezers than in non-freezers and correlates with pedunculopontine nucleus structural connectivity in freezers (Peterson et al. 2015). This observation supports the notion that freezers may have a frontal lobe disconnection from subcortical structures critical for gait which interferes with automatic as well as cognitively controlled motor processes (Vandenbossche et al. 2012; Fling et al. 2014). These observations lead to two conclusions: first, in PD, APAs are smaller and slower due to a bradykinetic state. The freezing phenomenon cannot be explained by reduced APAs because freezers and non-freezers did not have significantly different APAs.
The problem of start-hesitation freezing is the initiation of a step, i.e. the shift from the cortically driven or facilitated APA motor programme to the stepping programme. This reduced ability to change from one programme to the other has been extensively studied in the past (Benecke et al. 1987). Recently, the concept of ‘movement synergy’, which holds that the stability of the performance of one motor programme has to be actively reduced to allow for the initiation of another programme, has been introduced and this process may be reduced in PD (Latash and Huang 2015). The APA programme is consequently locked in an inflexible motor system and performed repetitively with little or no bradykinetic features. Support for this notion comes from the observation that multiple APAs are of considerable amplitude and speed, as has been shown in stepping tasks which include a challenge to postural stability movement (Jacobs et al. 2009b). Multiple APAs have also been observed in healthy subjects in a complex task involving backward translations of the surface together with a command for which foot to use for a compensatory step (Jacobs and Horak 2007). Our study shows that multiple APAs may also precede ‘normal’ stepping in healthy subjects. Apparently, no more than two APAs have been reported in the literature in healthy subjects (Nutt et al. 2011). In our large sample, up to four pre-APA oscillations were observed in very rare instances in healthy subjects which supports the assumption that processes similar to those seen in freezers are active here, i.e. the inability to quickly change from the APA motor programme to the stepping programme.
A significantly increased step latency of the freezers in externally triggered steps lends further support to the notion of an inability to initiate a step. While these considerations may apply for start-hesitation freezing, freezing during gait, however, cannot easily be reconciled with the concept of reduced instability of motor programmes. In these instances, the sequence effect (Iansek et al. 2006) could be responsible for a progressively reduced step size and freezing may occur as start-hesitation freezing after a complete standstill of leg movements.
References
Assaiante C, Woollacott M, Amblard B (2000) Development of postural adjustment during gait initiation: kinematic and EMG analysis. J Mot Behav 32:211–226
Benecke R, Rothwell JC, Dick JP, Day BL, Marsden CD (1987) Disturbance of sequential movements in patients with Parkinson’s disease. Brain 110(Pt 2):361–379
Burleigh-Jacobs A, Horak FB, Nutt JG, Obeso JA (1997) Step initiation in Parkinson’s disease: influence of levodopa and external sensory triggers. Mov Disord 12:206–215
Crenna P, Frigo C (1991) A motor programme for the initiation of forward-oriented movements in humans. J Physiol 437:635–653
Crenna P, Carpinella I, Rabuffetti M, Rizzone M, Lopiano L, Lanotte M, Ferrarin M (2006) Impact of subthalamic nucleus stimulation on the initiation of gait in Parkinson’s disease. Exp Brain Res 172:519–532
Delval A, Moreau C, Bleuse S, Tard C, Ryckewaert G, Devos D, Defebvre L (2014) Auditory cueing of gait initiation in Parkinson’s disease patients with freezing of gait. Clin Neurophysiol 125:1675–1681
Fling BW, Cohen RG, Mancini M, Nutt JG, Fair DA, Horak FB (2013) Asymmetric pedunculopontine network connectivity in parkinsonian patients with freezing of gait. Brain 136:2405–2418
Fling BW, Cohen RG, Mancini M, Carpenter SD, Fair DA, Nutt JG, Horak FB (2014) Functional reorganization of the locomotor network in Parkinson patients with freezing of gait. Plos One 9:e100291
Gantchev N, Viallet F, Aurenty R, Massion J (1996) Impairment of posturo-kinetic co-ordination during initiation of forward oriented stepping movements in parkinsonian patients. Electroencephalogr Clin Neurophysiol 101:110–120
Giladi N, Shabtai H, Simon ES, Biran S, Tal J, Korczyn AD (2000) Construction of freezing of gait questionnaire for patients with Parkinsonism. Parkinsonism Relat Disord 6:165–170
Halliday SE, Winter DA, Frank JS, Patla AE, Prince F (1998) The initiation of gait in young, elderly, and Parkinson’s disease subjects. Gait Posture 8:8–14
Hanakawa T, Fukuyama H, Katsumi Y, Honda M, Shibasaki H (1999) Enhanced lateral premotor activity during paradoxical gait in Parkinson’s disease. Ann Neurol 45:329–336
Hiraoka K, Matuo Y, Iwata A, Onishi T, Abe K (2006) The effects of external cues on ankle control during gait initiation in Parkinson’s disease. Parkinsonism Relat Disord 12:97–102
Iansek R, Huxham F, McGinley J (2006) The sequence effect and gait festination in Parkinson disease: contributors to freezing of gait? Mov Disord 21:1419–1424
Jacobs JV, Horak FB (2007) External postural perturbations induce multiple anticipatory postural adjustments when subjects cannot pre-select their stepping foot. Exp Brain Res 179:29–42
Jacobs JV, Lou JS, Kraakevik JA, Horak FB (2009a) The supplementary motor area contributes to the timing of the anticipatory postural adjustment during step initiation in participants with and without Parkinson’s disease. Neuroscience 164:877–885
Jacobs JV, Nutt JG, Carlson-Kuhta P, Stephens M, Horak FB (2009b) Knee trembling during freezing of gait represents multiple anticipatory postural adjustments. Exp Neurol 215:334–341
Jiang Y, Norman KE (2006) Effects of visual and auditory cues on gait initiation in people with Parkinson’s disease. Clin Rehabil 20:36–45
Kanekar N, Aruin AS (2014a) Aging and balance control in response to external perturbations: role of anticipatory and compensatory postural mechanisms. Age (Dordr) 36:9621
Kanekar N, Aruin AS (2014b) The effect of aging on anticipatory postural control. Exp Brain Res 232:1127–1136
Laessoe U, Voigt M (2013) Step adjustments among young and elderly when walking toward a raised surface. Aging Clin Exp Res 25:299–304
Latash ML, Huang X (2015) Neural control of movement stability: lessons from studies of neurological patients. Neuroscience 301:39–48
Lee RG, Tonolli I, Viallet F, Aurenty R, Massion J (1995) Preparatory postural adjustments in parkinsonian patients with postural instability. Can J Neurol Sci 22:126–135
Malouin F, Richards CL (2000) Preparatory adjustments during gait initiation in 4-6-year-old children. Gait Posture 11:239–253
Mancini M, Zampieri C, Carlson-Kuhta P, Chiari L, Horak FB (2009) Anticipatory postural adjustments prior to step initiation are hypometric in untreated Parkinson’s disease: an accelerometer-based approach. Eur J Neurol 16:1028–1034
Mancini M, Chiari L, Holmstrom L, Salarian A, Horak FB (2016) Validity and reliability of an IMU-based method to detect APAs prior to gait initiation. Gait Posture 43:125–131
Mensink SH, Nonnekes J, van Bon G et al (2014) Additional weight load increases freezing of gait episodes in Parkinson’s disease; an experimental study. J Neurol 261:999–1008
Michely J, Volz LJ, Barbe MT et al (2015) Dopaminergic modulation of motor network dynamics in Parkinson’s disease. Brain 138:664–678
Naugle KM, Hass CJ, Bowers D, Janelle CM (2012) Emotional state affects gait initiation in individuals with Parkinson’s disease. Cogn Affect Behav Neurosci 12:207–219
Nocera JR, Roemmich R, Elrod J, Altmann LJ, Hass CJ (2013) Effects of cognitive task on gait initiation in Parkinson disease: evidence of motor prioritization? J Rehabil Res Dev 50:699–708
Nutt JG, Bloem BR, Giladi N, Hallett M, Horak FB, Nieuwboer A (2011) Freezing of gait: moving forward on a mysterious clinical phenomenon. Lancet Neurol 10:734–744
Peterson DS, Fling BW, Mancini M, Cohen RG, Nutt JG, Horak FB (2015) Dual-task interference and brain structural connectivity in people with Parkinson’s disease who freeze. J Neurol Neurosurg Psychiatry 86:786–792
Rocchi L, Chiari L, Mancini M, Carlson-Kuhta P, Gross A, Horak FB (2006) Step initiation in Parkinson’s disease: influence of initial stance conditions. Neurosci Lett 406:128–132
Rocchi L, Carlson-Kuhta P, Chiari L, Burchiel KJ, Hogarth P, Horak FB (2012) Effects of deep brain stimulation in the subthalamic nucleus or globus pallidus internus on step initiation in Parkinson disease: laboratory investigation. J Neurosurg 117:1141–1149
Schenk T, Baur B, Steude U, Botzel K (2003) Effects of deep brain stimulation on prehensile movements in PD patients are less pronounced when external timing cues are provided. Neuropsychologia 41:783–794
Uemura K, Yamada M, Nagai K, Tanaka B, Mori S, Ichihashi N (2012) Fear of falling is associated with prolonged anticipatory postural adjustment during gait initiation under dual-task conditions in older adults. Gait Posture 35:282–286
Vandenbossche J, Deroost N, Soetens E et al (2012) Freezing of gait in Parkinson’s disease: disturbances in automaticity and control. Front Hum Neurosci 6:356
Woollacott MH, Manchester DL (1993) Anticipatory postural adjustments in older adults: are changes in response characteristics due to changes in strategy? J Gerontol 48:M64–M70
Acknowledgments
This project was supported financially by the Lüneburg heritage (no involvement in the study design, the collection, analysis and interpretation of data, the writing of the manuscript or the decision to submit the manuscript for publication). We are also grateful to Mrs. K. Ogston for careful proofreading the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Plate, A., Klein, K., Pelykh, O. et al. Anticipatory postural adjustments are unaffected by age and are not absent in patients with the freezing of gait phenomenon. Exp Brain Res 234, 2609–2618 (2016). https://doi.org/10.1007/s00221-016-4665-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00221-016-4665-x