Abstract
Microfluidic-based biosensors have been developed for their precise automatic reaction control. However, these biosensors require external devices that are difficult to transport and use. To overcome this disadvantage, our group made an easy-to-use, cheap, and light pumpless three-dimensional photo paper–based microfluidic analytical device (3D-μPAD; weight: 1.5 g). Unlike conventional paper-based microfluidic analytical devices, the 3D-μPAD can be used to control fluid flow in a 3D manner, thus allowing sophisticated multi-step reaction control. This device can control fluid flow speed and direction accurately using only the capillary-driven flow without an external device like a pump. The flow speed is controlled by the width of the microfluidic channel and its surface property. In addition, fluid speed control and 3D-bridge structure enable the control of fluid flow direction. Using these methods, multi-step enzyme-linked immunosorbent assay (ELISA) can be done automatically in sequence by injecting solutions (sample, washing, and enzyme’s substrate) at the same time in the 3D-μPAD. All the steps can be performed in 14 min, and data can be analyzed immediately. To test this device, thioredoxin-1 (Trx-1), a biomarker of breast cancer, is used as the target. In the 3D-μPAD, it can detect 0–200 ng/mL of Trx-1, and the prepared 3D-μPAD Trx-1 sensor displays excellent selectivity. Moreover, by analyzing the concentration of Trx-1 in real patients and healthy individuals’ blood serum samples using the 3D-μPAD, and comparing results to ELISA, it can be confirmed that the 3D-μPAD is a good tool for cancer diagnosis.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Microfluidic devices have been widely used in many fields such as food chemistry, environmental monitoring, and health diagnostic [1, 2]. As a fluid automatic control system, microfluidic devices have been developed and researched for the lab-on-a-chip-based application [3, 4]. By transporting and mixing the fluid regents, the devices can be used for chemical and biomolecule reagent detection. However, for sophisticated and easy detection at the point-of-care (POC), multiple fluidic regent control system should be automated and controllable without the need for external devices such as fluid pumps, electro-osmosis, or electro-wetting [5,6,7].
Paper-based analytical devices (PAD), which transport fluid using the capillary wicking flow of fluid, have been focused on the POC-based diagnose field [8, 9]. Commonly, chromatography paper and filter paper have been used as main materials for the easy and cheap fabrication of microfluidic PAD (μPAD) [10]. Since these materials contain porous fiber matrix that passively allow fluid to wick and absorb in their porous network, they can make passively capillary fluid flow. Many paper-based chips have created channels for fluid flow using hydrophobic wax-printing or hydrophilic materials because these methods were easy to mass-produce at low cost [11, 12]. Through this formed fluid channel, the fluid could flow without external power, and while it flows, it meets other fluids to produce reactions like immuno-reaction or enzyme reaction [13]. However, since these techniques only used the force exerted by the paper during capillary absorbing action, it was difficult to control the flow direction and speed. Because the power to absorb the fluid on the paper was the fluid flow direction, it was difficult to let the fluid flow to one side without external power when a two-way channel appears. This absorption made hard to control the multi-step reaction order such as separating the flow of signal-inducing enzyme and its substrate, which were used in enzyme-linked immunosorbent assay (ELISA)–based μPAD. Without the separation of these substrates, it caused non-specific reactions as the substrate passed through the path through which the enzyme already flows, thereby increasing the noise signal [14]. In addition, absorbing fluid speed in matrix of paper differed from the distance of fluid flow, because absorbance power of paper was decreased by the length of fluid flow [15, 16]. This inconsistent speed was not suitable for controlling time-dependent reaction in μPAD. To overcome those disadvantages, Glavan’s team developed pressure-driven microfluidic devices using omniphobic paper to control the fluid flow in microfluidic channel [17]. The combination of omniphobic paper and a craft cutter enabled the development of fluid flow controlling system like valve system or generation of droplet in microchannel. However, this type of μPAD needed external pump to control the speed and direction of microfluidic flow, which made it difficult to use the device easily.
Among the various developmental approaches of μPAD for controlling the fluid flow without external devices, we proposed a photo paper–based microfluidic analytical device as a novel platform of μPAD, which consists of a cropped channel between the stacked layers that consist of photo paper and polyethylene terephthalate (PET) film [18]. The fluid flow in a channel made of hydrophobic nanoparticle-coated photo paper was likely to occur on the surface of the channel rather than in its porous matrix [19] This type of lateral flow was called capillary-driven flow and was induced by the interfacial surface energy of the fluid and the channel [20, 21] The fluid flow system had advantages for some reasons. For example, the fabrication of photo paper–based μPAD was easy, fast, and cost-effective [22]. And, the flow speed in the photo paper–based channel was constant, which differ from flow in chromatography paper channel that showed decreasing speed according to the distance [23]. In addition, the flow speed can be easily controlled by increasing or decreasing width of channel and modification of surface of photo paper with hydrophobic or hydrophilic materials. Moreover, the system does not need external device or force to make a fluid flow because the fluid was passively flowed by capillary-driven force between surface of photo paper and fluid. The advantages were suitable for the development of a POC test system that needs easy fabrication steps, and sophisticated reaction time control.
By using the new fabrication method of photo paper–based μPAD, our group developed a pumpless three-dimensional microfluidic photo paper–based analytical device (3D-μPAD). Our new 3D-μPAD was possible to create the desired fluid channel pattern easily, and by adding a 3D structure, the 3D-μPAD could be used for novel attempts (e.g., flow jump to another channel) which could not be done in a traditional 2D-μPAD. In addition, our device could do not only control the speed using chemical and physical treatments but also control the direction of flow using a 3D structure modification.
ELISA has been widely used as a bio-detection method for its high specificity using antigen–antibody-specific binding and highly sensitive colorimetric enzymes [24]. However, if the unreacted enzyme-antibody complex in the signal-developed part was not fully washed, strong noise signals could be developed due to its high reactivity with the enzyme–substrate. Moreover, the enzyme reaction signal depended on the reaction time, so control of accurate reaction time was required [25, 26] With advanced speed and direction control of capillary-driven fluid flow, we could fabricated a 3D-μPAD, which can complicate multi-step of ELISA automatically. Our fabricated 3D-μPAD could do and control three steps of ELISA such as the antigen and antibody binding step, the washing step, and the enzyme–substrate reaction step in order and on time without an external device.
To make sure that the 3D-μPAD works well, our group targeted a biomarker, thioredoxin-1 (Trx-1). Trx-1 is a relatively recently discovered breast cancer biomarker, compared to conventional breast biomarkers such as human epidermal growth factor receptor 2 (HER-2) and carcinoembryonic antigen (CEA) [27, 28]. Using the target biomarker, Trx-1, we tested the fabricated 3D-μPAD for automatically controlling the ELISA reaction to diagnose breast cancer. Furthermore, the real samples, coming from the serum of patients and healthy people, were analyzed by the 3D-μPAD to show the precision of the device, and applicable for actual commercial use by comparing the results from conventional ELISA and 3D-μPAD.
Materials and methods
Chemical and materials
A4 size photo paper (Epson, S042187), A4 size double adhesive tape (Formtec, BS-210), and adhesive PET film (Printec, G2140) and overhead transparency film (OHP film) (Printec, V2300) were bought from a local store. Silver nanoparticle (AgNP) ink (Silver jet ink, 14.20 cP, DGP 40LT-15C) was obtained from Advance Nano Products. Polytetrafluoroethylene (Teflon) preparation (665,800—100 mL) was purchased from Sigma-Aldrich (Korea). Capture antibody (rabbit anti-trx-1 antibody, 14,999–1-AP) was purchased from Proteintech. Detection antibody, which is linked with HRP (mouse anti-thioredoxin-antibody-HRP, sc-166393), was bought from Santa Cruz Biotechnology, and rabbit anti-mouse IgG antibody (SA5-10,192) for control signal dot was purchased from Thermo Fisher Scientific. Trx-1 (human thioredoxin-1, 10,384-HNAE-200) was purchased from Sino Biological. Nitrocellulose membrane (HF13502S25), glass fiber membrane (PT-R1), and absorbance pad (AP080) were obtained from MDI. Bovine serum albumin (BSA) (A2153-50G); Tween 20 (P9416—100 mL); phosphate-buffered saline (PBS, P3813-10PAK); 3,3,5,5-tetramethylbenzidine (TMB, T0440—100 mL); and trehalose (PHR1344-500MG) were bought from Sigma-Aldrich (Korea). To test selectivity, prostate tumor antigen (PSA) (P3338—25 μg) and human serum albumin (HSA) (A1653—10 g) were bought from Sigma-Aldrich (Korea).
Preparation of 3D-μPAD
The 3D paper-based microfluidic device was made by stacking layers. The first layer was photo paper. It helped fluid flow in a microfluidic channel by capillary-driven force. Middle layers were pattern-cropped, double-sided adhesive films. The conventional adhesive PET film had an adhesive only on one side. Thus, the double-sided tape was used to give adhesive property to both sides of the PET. These layers made microfluidic channels. Each film’s thickness was 100 μm. To cover and make a 3D structure, OHP film, which was the last layer, was attached at the top of the device. Each pattern-cropped PET layers was prepared using the cutting machine Cricut explore Air 2 (Provo craft & Novelty, Inc.) [29].
Paper surface treatment
To control the flow speed, surface wettability of photo paper was modified by drawing silver nanoparticle (AgNP) and Teflon pattern with ballpoint pens, which were filled by AgNP and Teflon ink, respectively. We used a 0.5-mm-diameter ballpoint for the manual drawing. The patterns of each material on the photo paper were designed and patterned by a commercial digital plotter “Cricut explore Air 2.”
Preparation of immuno-chromatography system using ELISA
To make an immunochromatographic system, three pads (conjugate pad, signal generation pad, and absorbance pad) were needed. The conjugate pad composed of 0.5% BSA solution (1 μL, v/v), 40% trehalose (2.5 μL, v/v), 0.01% Tween 20 (20.6 μL, v/v), and anti-Trx-1 antibody-conjugated with HRP (0.12 μL, 0.2 mg/mL). This mixture was poured on a 7 mm × 4-mm glass fiber membrane and dried at 4 °C for 12 h. The signal generation pad was made by dropping antibody solution, rabbit anti-thioredoxin-1 antibody, 1 μL (0.2 mg/mL) for test dot (size r = 1 mm) at the bottom of the nitrocellulose membrane (10 μm pore size; 4 mm × 25 mm). A control dot was made by a rabbit anti-mouse IgG antibody (1 μL, 0.1 mg/mL) at the top of the nitrocellulose membrane. Thereafter, this was allowed to dry for 20 min. This membrane was kept in a desiccator or a refrigerator until used. The absorbance pad comprised a cellulose membrane. This pad was shaped like a bent pipe (14 mm × 20 mm square size and erased square size is 5 mm × 15 mm). This was kept in a desiccator until use.
Fabrication of one-shot 3D-μPAD for detection of Trx-1
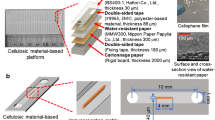
The 3D-μPAD comprising five layers and lateral flow immune-chromatography is shown in Fig. 1a. The first layer was a photo paper, which helped each fluid flow with constant speed and control fluid flow speed by control hydrophilicity. The next two layers were both adhesive PET films, which were designed for fluid flow speed and direction control. The fourth layer was the OHP film. This layer covers the fluid channel and prevents the fluid from overflowing in the microfluidic channel. The last layer was the adhesive film, and this layer had a role in flow direction control and giving more height of the sample pot. Between the third and fourth layers, antibody-treated nitrocellulose membrane, absorbance pad, and conjugate pad were inserted to generate a signal according to the Trx-1 concentration. All layers were laminated together in a correct order to provide strong binding between each layer and to form a 3D channel. Once the assembly was over, it was left at 4 °C without light. The cropped pattern of each film and coated materials on each film are described in Fig. 1b. The cropped pattern of each film was designed to control the direction and velocity of each fluid when moving the fluid with power using only the capillary-driven force. In particular, each film was designed to control flow direction for blocking unintended reactions in the flow channels, as shown in Fig. 1c. When enzyme solution leaks into the enzyme–substrate channel, most of the substrate reacts in its own flow channel with the enzyme. This phenomenon increased the noise and decreased the signal development rate. A washing solution was used for pushing the remaining antigen and enzyme on the reaction site (nitrocellulose membrane). If sample and washing solutions got mixed in the washing solution channel, the antigen was diluted by the washing solution, and the concentration of the antigen thus decreased. In addition, the cleaning effect was good when the cleaning solution was pushed from the back after the sample solution had completely flown in the reaction site (nitrocellulose membrane). However, if the fluids got mixed in the channel, the washing effect may reduce, thus decreasing the signal-to-noise ratio. The role of each layer’s pattern will be described in detail in the data section.
a A schematic of the 3D-μPAD that consists of five different patterned layers and a reaction site for automatic ELISA reaction control. b The cropped pattern of each film and coated materials on each film. c A schematic for the need to control capillary-driven microfluidic flow direction to prevent non-specific and unwanted reactions
ELISA to know real blood sample’s concentration of Trx-1
ELISA was performed to determine the concentration of Trx-1 in real blood samples, and the following procedure was performed. The capture antibody was coated on a 96-well plate (5 μg/mL, 100 μL) for 4 h at 24 °C and washed four times using a washing buffer, 0.1% Tween 20 in PBS (v/v). The plate surface was blocked by blocking buffer, 3% BSA in PBS (w/v), to avoid non-specific reactions. After 2 h at 24 °C, plate was washed four times using a washing buffer. Then, samples of known concentrations for calibration and blood serum were added, and the plate was incubated for 1 h in a slowly shaking incubator. Thereafter, it was washed four times. The detection antibody-HRP probe (100 ng/mL, 100 μL) was added and incubated for 30 min at 24 °C. After washing five times, the TMB solution was added as a substrate of the HRP. Then, 13 min later, the reaction was stopped using 1 M HCl, and the signal intensity was read using a microplate reader. By comparing the signal and calibration curves of the blood serum, the Trx-1 concentration of the real samples was analyzed.
Overall reaction in 3D-μPAD
The overall reaction in the 3D-μPAD comprised five steps as shown in Fig. 2a, b. First, three solutions (sample, washing, and enzyme–substrate) were injected at the same time. Second, sample solution reached the conjugate pad, and Trx-1 antigen reacted with the detection antibody in conjugate pad. After then, antigen–antibody complexes and unreacted proteins entered the reaction part by the absorbing force of nitrocellulose membrane. During this step, the antigen–antibody complexes were captured by the capture antibody on the reaction membrane. Third, the remaining antigen and detection antibody were removed by the washing solution. Fourth, the TMB solution reached the reaction part and reacted with detection antibody’s enzyme after all washing steps are over. Fifth, HRP, which is linked with the detection antibody, and TMB reacted and developed a signal according to the concentration of Trx-1. Each samples’ reaction time was set by experimental optimization.
Reaction steps occurring in 3D-μPAD. a A step-by-step schematic of fluid movement in 3D-μPAD. b A step-by-step schematic of ELISA reaction occurring at the ELISA-reaction part; each step comprised five steps (i–v): (i) solution injection step, (ii) immuno-reaction step, (iii) washing step, (iv) enzyme–substrate reaction step, and (v) signal development step
Quantification of Trx-1 in 3D-μPAD
The developed signal was analyzed by a custom-made reader device. After 14 min from the three solutions (sample, washing, and enzyme–substrate) injected in the 3D-μPAD, a camera captured the image of developed signal in the reaction part automatically. The image was stored as BMP file. The captured image was analyzed using an image-analyzing software “Bio-value.” In this program, developed color, as a form of dot, was manually selected and the pixel intensity was individually stored as three colors such as red, green, and blue (RGB). To attain the consistent results, the RGB signal was normalized by Park’s method [30]. The average RGB pixel intensity value of the test dot (pixel size = 8 × 8) was normalized by the background portion of the assay membrane (pixel size = 8 × 8), and normalized RGB average signal was used as a developed signal intensity. In this program, the RGB average value was lower when the developed signal was higher. So, we calculated the signal value by an inverse form of normalized RGB average signal (signal = 1/RGB average).
Results and discussion
Capillary-driven flow direction control using difference of flow speed
To automatically perform ELISA reaction inside the device, it is necessary to adjust the speed and direction of the fluid flow. However, without a mechanical pump, capillary-driven flow speed and direction control were difficult because of their tendency to flow in all directions. This phenomenon was solved by controlling the capillary-driven flow speed by surface modification of the photo paper. The velocity of the fluid in a capillary channel varied with the width of the channel and its surface properties. Figure 3a shows the contact angle of PBS for each material. PET film showed mildly hydrophilic (Ɵ = 74.9°) and photo paper showed hydrophilic properties (Ɵ = 46.1°). When the photo paper was coated with silver nanoparticles, which were hydrophilic, the paper exhibited even stronger hydrophilic properties (Ɵ = 20.1°). Conversely, when the photo paper was coated with Teflon, which was a hydrophobic material, the surface property of the photo paper was changed to hydrophobic (Ɵ = 105°). The results confirmed that by patterning these materials on the paper surface, we could easily transform the properties of the paper surface. Capillary-driven flow speed was controlled by the width of the channel and surface hydrophilicity. Wider channels allowed for faster flow, which was the same result of our previous study. Silver coating enhanced surface hydrophilicity and accelerated capillary-driven flow speed on the paper. The fluid flow speed according to the width of the channel without silver line is shown in Fig. 3b and with a silver line is shown in Fig. 3c. When the width of the channel was 0.5 mm, the flow speed was 0.41 mm/s without silver line and 3.67 mm/s with silver line. However, in a 1-mm-wide channel, the flow speed was 0.46 mm/s without silver line and 5.24 mm/s with silver line. In a 1.5-mm-wide channel, the flow speed was 0.5 mm/s without silver line and 7.90 mm/s with silver line. Taken together, the fluid moved faster in wider channels. In addition, when the photo paper was treated with silver, the flow in the microfluidic channel was accelerated. Using this speed control, the direction of capillary-driven flow can be controlled. A schematic of this process is shown in Fig. 3d. One side of the channel rapidly accelerated because of the silver line, while the other channel was slower. The fluids were dropped initially at the same time. Due to the capillary effect, the fluid in the faster channel tried to enter the slower channel; however, as the slow fluid also flowed in the direction of the intersection, a wall of air which was a kind of a big bubble was formed inside. This wall of air, formed in the channel, prevented the fast flow to enter another channel. It also consequently prevented the slow fluid from mixing with the fast fluid. This wall of air kept without permeability through photo paper until the fast fluid flows out in a forward direction. When all the fast fluid went through forward direction, the wall of air was pushed by slow fluid flow, and the slow fluid could proceed accordingly. The slow flow then faces a two-pronged channel, which can also be controlled to move in one direction. If the flow reaches a bifurcation point of two channels, the fluid tended to go through the faster flowing channel. This was because the flow rate of the fluid depends on the velocity of the flow when the channels had the same width. The silver lining increased the flow speed by eight times, and thus, if only one of the two channels was treated with silver, most of the fluid would flow towards the silver-treated channel (Fig. 3e). In this figure, it can be confirmed that the fast-flowing fluid (blue ink) cannot enter the slow fluid flow channel (red ink) because of the wall of air. Then, the blue fluid totally flowed forward, and the red fluid pushed the wall of air and went through the intersection. At the intersection, the red ink can move in two directions, forward and backward, but because there was a silver line in the forward direction, much of the fluid moved in a forward direction.
a Contact angle of PBS on different material surfaces. b Capillary-driven flow speed depends on the width of the channel without silver coating and c with silver coating. d Scheme of flow direction control using flow speed using the different color inks (faster flow, blue; slower flow, red). e Pumpless capillary-driven flow direction control using silver coating on paper and speed difference
Flow direction control using a 3D-bridge structure
To produce an enzyme reaction, appropriate enzymes and substrates must meet only in the reaction area. However, using only capillary phenomena can cause noise as enzyme solution can flow through the substrate channel. To solve this problem, a 3D-bridge structure was added to our 3D-μPAD. The fabricated 3D-bridge structure is shown in Fig. 4a. This bridge can separate the pathway of each solution. The principle was as follows. Sample and washing solutions flowing into the channel were absorbed by the conjugate pad, and these solutions flow back to the nitrocellulose membrane with the enzyme. The fluids flowed into the nitrocellulose membrane and remained there until it reached the absorbance pad. At the bottom of the structure, an adhesive PET film with patterns was used to prevent the fluid absorbed by the conjugate pad from entering the substrate channel. In addition, the use of hydrophobic materials, such as Teflon coating, prevented the enzyme and antigen solutions from entering the substrate flow channel. Because of the hydrophobic material Teflon and the physical blockage “bridge structure,” the sample cannot overflow into the substrate channel. In addition, there was a hole on the conjugate pad, which was located in the top layer. When a fluid flowing under the effect of the capillary-driven force suddenly encounters a perforated ceiling, the force is reduced and the fluid stops. This phenomenon also helps block overflow to the substrate channel. To see the effect of blocking overflow from other channels, the substrate channel, blue ink was injected in the bridge and non-bridge structures. After the ink flowed, the side condition was checked. With the bridge structure, the ink flowed only in the nitrocellulose membrane without leaking to the bottom, thus creating an empty space underneath. However, without the bridge structure, the empty space is not identified because the ink leaked to the channel below (Fig. 4b). This can be checked even when observing from the top. Figure 4c shows the blue ink flow pattern when using the bridge structure. Once the blue ink flow has completed, the cover film and the nitrocellulose membrane were removed to check the condition of the bottom paper surface to know whether the blue ink leaked from the nitrocellulose membrane to the bottom of the photo paper surface. As shown in Fig. 4c, the blue ink did not leak from the nitrocellulose membrane when using the bridge structure in the 3D-μPAD. In contrast, without the bridge structure, blue ink flowed not only in nitrocellulose membrane but also on the surface of photo paper (Fig. 4d). If this blue ink was the HRP enzyme, most of TMB would have reacted with the adhered HRP enzyme on reaching the reaction part. This phenomenon increased the noise and caused the expense of the substrate, which reacted with the antibody-binding HRP enzyme. Consequently, using this bridge structure, we could block the fluid from leaking into the substrate channel and prevent non-specific reactions with the substrate.
Fluid flow time for automatic ELISA reaction
To check the time when the washing was complete, 200 ng/mL of Trx-1 was put into the sample pot to cause an immune reaction, and 25 s later, the washing solution was added. Thereafter, the TMB solution was added at the reaction part directly, and the signal-to-noise ratio was checked according to the washing time. On washing for 4 min, the signal and noise could not be distinguished because cleaning was not done properly. However, as the washing progressed, the unreacted antibodies and enzymes were removed and the signal-to-noise ratio gradually increased. Therefore, it was decided that the TMB solution should arrive 10 min after the washing step begins in the reaction part (Fig. S1). The reason for adjusting the TMB reaction time was that if TMB and enzyme reaction time was too short, the colorimetric signal would not develop properly, thus resulting in an unclear signal. Conversely, if the reaction time was too long, it could react with the few remaining enzymes as well, and the color of the TMB itself would change over time regardless of the presence or absence of the desired enzymes. These phenomena lead to a low signal-to-noise ratio. To test the optimal TMB reaction time, TMB was put in the reaction part where immuno-reaction was performed, and 10 min of washing step was completed. Thereafter, the signal-to-noise ratio according to the reaction time was checked. It was confirmed that the signal continued to increase because of enzymes, which are fixed to the reaction part by an immune reaction, for 3 min. However, after 3 min, the noise signal gets stronger, and the signal-to-noise ratio decreases (Fig. S2). Therefore, to show the optimal signal on the device, it is necessary to wash more than 10 min of residual antibodies and enzymes by a washing solution, and a 3-min TMB reaction must be carried out after cleaning was completed. These results set when each solution should reach the reaction part. The component of each solution, the time to reach the reaction part from the injection time, and the required volume could be determined as shown in Table S1.
Three-dimensional μPAD for Trx-1 detection and signal analysis
By adjusting the fluid speed and the length of the fluid channel, the solutions for each ELISA reaction step could reach the reaction part in time, and directional control using the speed could allow fluid flow such that it does not mix with each other, thus allowing for the sample and washing solutions to flow in turns without mixing. In addition, using the 3D-bridge structure, the sample and enzyme solutions were prevented from going to the substrate channel but the substrates could flow to the reaction part without interruption. Considering each samples’ flow time and direction, we designed and made the automatic 3D-μPAD for the detection of Trx-1. Completed 3D-μPAD is shown in Fig. 5a. The device’s size was 55 mm × 45 mm, and weight was 1.5 g. This device had three core channels. The three channels comprised a sample channel (1.5 mm × 8 mm) with silver line, a washing solution channel (1 mm × 20 mm) without silver line, and an enzyme–substrate channel (0.5 mm × 210 mm). To operate this device, these three solutions (sample solution 20 μL, washing solution 40 μL, and TMB solution 200 μL) should be dropped on the pot at the same time. If the three samples were not injected at the same time, it can make fluid flow control errors such as non-forming of air block or miss time control of washing time or enzyme reaction time. The apparatus was then left as it was for 14 min. In this time, all solutions flowed in an orderly manner, and the ELISA reaction resumed automatically without any external device or force. After the substrate reaction, the signal generated is shown in Fig. 5b. Signal analysis was done by a signal analysis device, which consists of custom-made device with camera as a hardware and the colorimetric image analysis program “Bio-value” as a software. The information of a custom-made device with a camera can be seen in Fig. S3. In this analysis program, the signal was inversely proportional to the RGB signal. RGB signal meant the average rate of the colors (red, green, and blue). This was because when color development analysis was performed, the test and control dot signals reveal not only blue color but also green and red. At high signal intensity, there was strong color development, and the RGB signal was low. Accordingly, the Trx-1 concentration was inversely proportional to the RGB average. In Fig. 5c, the Y-axis signal means 1/RGB average value. This device could detect Trx-1 range from 0 to 200 ng/mL of Trx-1 concentration Generally, calibration curve of ELISAs was expected to show a sigmoidal behavior in wide range of analyte concentration. However, in narrow specific range of concentration, the calibration of curve showed linearity [31]. For the high linearity of calibration curve, we optimized the condition of ELISA reaction (concentration of antibodies) that showed linear curve in the range from 0 to 200 ng/mL. In that range, the calibration curve equation was y = 9.7859 × 10−5 x + 0.0065 and R2 is 98.55%, which showed high linearity, and good alignment according to the concentration of Trx-1. Based on the results, the calculated limit of detection (LOD) and limit of quantitation (LOQ) of the biosensor were 4.1 ng/mL and 12.3 ng/mL, respectively (S/N = 3). These results confirm that the 3D-μPAD can accurately diagnose biomarkers that detect breast cancer with high sensitivity in a short time. To test the specificity for Trx-1 in the 3D-μPAD, we selected four different antigens: BSA, PSA, HSA, and Trx-1. Each antigen’s concentration was fixed as 10 nM. Their signal analysis data are shown in Fig. 5d. This figure shows that this device worked only when Trx-1 was used as the sample. Before this analysis, we set the baseline as the reading when there was no antigen in the sample. That baseline signal was 0.006511. Compared to the baseline signal, the three antigens (PSA, BSA, and HSA) revealed a signal minuscule enough to be negligible. One example, when the concentration of Trx-1 was 2.5 nM, the signal was 0.006742. This signal was higher than that of the other three extra antigen signals (10 nM, < 0.0066). Therefore, these results demonstrated that the 3D-μPAD could selectively detect Trx-1 according to the used antibodies in this device.
a Image of 3D-μPAD for detecting Trx-1. b Developed signal according to the concentration of Trx-1 at 0, 25, 50, 100, and 200 ng/mL in 3D-μPAD. c Quantitative calibration curve plot of signal (= 1/RGB average) (n = 4). d Comparison of signal analysis for different samples using 3D-μPAD at 10 nM (n = 4)
Real serum test using 3D-μPAD
Sera of patients and healthy individuals were used to verify that this chip was applicable for actual commercial use and that Trx-1 can be accurately detected in actual serum samples. ELISA was used to find out the exact concentration of Trx-1 before the analysis of actual sera using the 3D-μPAD. Serum samples were comprised of a group of four breast cancer patients and four healthy individuals and more detail information of each serum is presented in Table S2. All human blood sample were anonymized and named as P1 ~ P4 (sample from breast cancer patients) and H1 ~ H4 (sample from healthy individuals). The signal presented using a 3D-μPAD is shown in Fig. 6a. It was clearly identified between the patients and healthy individuals. For breast cancer patients’ sample, the signal was strongly displayed, and this showed that the concentration of Trx-1 was high. Conversely, healthy individuals’ samples display a weak signal compared to patients. For more accurate analysis, the signal from the 3D-μPAD was converted to the concentration of Trx-1 using a calibration curve, and the data were compared with the actual sera’s concentration of Trx-1, as identified by ELISA. The results are shown in Fig. 6b that the 3D-μPAD demonstrates an acceptable performance of detecting Trx-1 in the serum, and the performance of the 3D-μPAD can be found to be very similar to that of the conventional ELISA method. Analysis of signals from the 3D-μPAD shows that the difference in the concentration of Trx-1 between breast cancer patients and healthy individuals is very large. For breast cancer patients, the lowest concentration was 50 ng/mL, and the highest concentration for healthy individuals was 35 ng/mL. Because the 3D-μPAD can analyze the range from 0 to 200 ng/mL with LOD = 4.1 ng/mL, and LOQ = 12.3 ng/mL, breast cancer can be accurately diagnosed using the concentration of Trx-1 analyzed in the 3D-μPAD.
Real serum test results using 3D-μPAD for the breast patient (P1, P2, P3, P4) and healthy individuals (H1, H2, H3, H4). a Image of the signal shown by 3D-μPAD for each sample. b Comparison between the concentration of Trx-1 analyzed by ELISA and the concentration of Trx-1 obtained by analyzing images shown in 3D-μPAD for each sample
Conclusions
In summary, the fabricated 3D-μPADs can automatically deliver fluid samples and reagents in sequence for a multi-step assay detection without needing an external controlling device. In addition, a simple and user-friendly fabrication method enabled to fabricate 3D structure capillary microfluidic channel easily. The proposed platform could analyze the concentration of Trx-1 in a short time (14 min) and showed high performance in both qualitative and quantitative analysis with a linear range of 0–200 ng/mL. In addition, Trx-1 levels were successfully detected with ELISA-comparable performance in the blood serum of patients and healthy individuals. Consequently, the proposed device exhibits an alternative ELISA-based lab-on-a-chip comprising fast analysis, on-site-equipment-free measurements, and portability. Furthermore, this device breaks the traditional conception of a paper-based chip and 2D structure, and resolves the existing problems with 2D-based paper sensors. Consequently, we expect that this platform could be a promising platform for new immuno-analysis and clinical diagnosis.
References
Mitchell KR, Esene JE, Woolley AT. Advances in multiplex electrical and optical detection of biomarkers using microfluidic devices. Anal Bioanal Chem. 2021. https://doi.org/10.1007/s00216-021-03553-8.
Hernández-Rodríguez JF, Rojas D, Escarpa A. Rapid and cost-effective benchtop microfabrication of disposable carbon-based electrochemical microfluidic devices. Sens Actuators B Chem. 2020;324: 128679. https://doi.org/10.1016/j.snb.2020.128679.
Zhuang JJ, Yin JX, Lv SW, Wang B, Mu Y. Advanced “lab-on-a-chip” to detect viruses - current challenges and future perspectives. Biosens Bioelectron. 2020;163. https://doi.org/10.1016/j.bios.2020.112291
Dekker S, Buesink W, Blom M, Alessio M, Verplanck N, Hihoud M, et al. Standardized and modular microfluidic platform for fast lab on chip system development. Sens Actuators B Chem. 2018;272:468–78. https://doi.org/10.1016/j.snb.2018.04.005.
Ye WQ, Wei YX, Zhang YZ, Yang CG. Xu ZR Multiplexed detection of micro-RNAs based on microfluidic multi-color fluorescence droplets. Anal Bioanal Chem. 2020;412(3):647–55. https://doi.org/10.1007/s00216-019-02266-3.
Godinez-Brizuela OE, Niasar VJ. Simultaneous pressure and electro-osmosis driven flow in charged porous media: pore-scale effects on mixing and dispersion. J Colloid Interface Sci. 2020;561:162–72. https://doi.org/10.1016/j.jcis.2019.11.084.
Li J, Kim CJ. Current commercialization status of electrowetting-on-dielectric (EWOD) digital microfluidics. Lab Chip. 2020;20(10):1705–12. https://doi.org/10.1039/D0LC00144A.
Wang ML, Song ZH, Jiang YW, Zhang XL, Wang L, Zhao HY, Cui YT, Gu FR, Wang YH, Zheng GX. A three-dimensional pinwheel-shaped paper-based microfluidic analytical device for fluorescence detection of multiple heavy metals in coastal waters by rational device design. Anal Bioanal Chem. 2021;413(12):3299–313. https://doi.org/10.1007/s00216-021-03269-9.
Jin L, Hao Z, Zheng Q, Chen H, Zhu L, Wang C, et al. A facile microfluidic paper-based analytical device for acetylcholinesterase inhibition assay utilizing organic solvent extraction in rapid detection of pesticide residues in food. Anal Chim Acta. 2020;1100:215–24. https://doi.org/10.1016/j.aca.2019.11.067.
Calabria D, Calabretta MM, Zangheri M, Marchegiani E, Trozzi I, Guardigli M, et al. Recent advancements in enzyme-based lateral flow immunoassays. Sensors. 2021;21(10):3358. https://doi.org/10.3390/s21103358.
Sharifi H, Tashkhourian J, Hemmateenejad B. A 3D origami paper-based analytical device combined with PVC membrane for colorimetric assay of heavy metal ions: application to determination of Cu(II) in water samples. Anal Chim Acta. 2020;1126:114–23. https://doi.org/10.1016/j.aca.2020.06.006.
Noiphung J, Laiwattanapaisal W. Multifunctional paper-based analytical device for in situ cultivation and screening of Escherichia coli infections. Sci Rep. 2019;9(1):1555. https://doi.org/10.1038/s41598-018-38159-1.
Preechakasedkit P, Siangproh W, Khongchareonporn N, Ngamrojanavanich N, Chailapakul O. Development of an automated wax-printed paper-based lateral flow device for alpha-fetoprotein enzyme-linked immunosorbent assay. Biosens Bioelectron. 2018;102:27–32. https://doi.org/10.1016/j.bios.2017.10.051.
Shangguan J-W, Liu Y, Wang S, Hou Y-X, Xu B-Y, Xu J-J, et al. Paper capillary enables effective sampling for microfluidic paper analytical devices. Acs Sens. 2018;3(7):1416–23. https://doi.org/10.1021/acssensors.8b00335.
Shou D, Fan J. Design of nanofibrous and microfibrous channels for fast capillary flow. Langmuir. 2018;34(4):1235–41. https://doi.org/10.1021/acs.langmuir.7b01797.
Glavan AC, Martinez RV, Maxwell EJ, Subramaniam AB, Nunes RMD, Soh S, et al. Rapid fabrication of pressure-driven open-channel microfluidic devices in omniphobic R-F paper. Lab Chip. 2013;13(15):2922–30. https://doi.org/10.1039/C3LC50371B.
Yukird J, Soum V, Kwon OS, Shin K, Chailapakul O, Rodthongkum N. 3D paper-based microfluidic device: a novel dual-detection platform of bisphenol A. Analyst. 2020;145(4):1491–8. https://doi.org/10.1039/C9AN01738K.
Songok J, Toivakka M. Enhancing capillary-driven flow for paper-based microfluidic channels. ACS Appl Mater Interfaces. 2016;8(44):30523–30. https://doi.org/10.1021/acsami.6b08117.
Hemmig E, Temiz Y, Gökçe O, Lovchik RD, Delamarche E. Transposing lateral flow immunoassays to capillary-driven microfluidics using self-coalescence modules and capillary-assembled receptor carriers. Anal Chem. 2020;92(1):940–6. https://doi.org/10.1021/acs.analchem.9b03792.
Hassan S-u, Zhang X. Design and fabrication of capillary-driven flow device for point-of-care diagnostics. Biosensors. 2020;10(4):39. https://doi.org/10.3390/bios10040039
Soum V, Park S, Brilian AI, Kwon O-S, Shin K. Programmable paper-based microfluidic devices for biomarker detections. Micromachines-Basel. 2019;10(8):516. https://doi.org/10.3390/mi10080516.
Soum V, Park S, Brilian AI, Choi JY, Lee Y, Kim W, et al. Quantitatively controllable fluid flows with ballpoint-pen-printed patterns for programmable photo-paper-based microfluidic devices. Lab Chip. 2020;20(9):1601–11. https://doi.org/10.1039/D0LC00115E.
Ma L, Abugalyon Y, Li XJ. Multicolorimetric ELISA biosensors on a paper/polymer hybrid analytical device for visual point-of-care detection of infection diseases. Anal Bioanal Chem. 2021;413(18):4655–63. https://doi.org/10.1007/s00216-021-03359-8.
Zhan S, Zheng L, Zhou Y, Wu K, Duan H, Huang X, et al. A gold growth-based plasmonic ELISA for the sensitive detection of fumonisin B1 in maize. Toxins. 2019;11(6):323. https://doi.org/10.3390/toxins11060323.
Shang C, Wang Z, Liu H. A terminal antibody method based on multiple factors that influence ELISA results for measurement of antibody affinity in clinical specimens. J Virol Methods. 2017;240:42–8. https://doi.org/10.1016/j.jviromet.2016.11.009.
Park B-J, Cha M-K, Kim I-H. Thioredoxin 1 as a serum marker for breast cancer and its use in combination with CEA or CA15-3 for improving the sensitivity of breast cancer diagnoses. BMC Res Notes. 2014;7(1):7. https://doi.org/10.1186/1756-0500-7-7.
Liu YP, Zhao Y, Wei ZH, Tao L, Sheng XB, Wang SL, et al. Targeting thioredoxin system with an organosulfur compound, diallyl trisulfide (DATS), attenuates progression and metastasis of triple-negative breast cancer (TNBC). Cell Physiol Biochem. 2018;50(5):1945–63. https://doi.org/10.1159/000494874.
Lee MJ, Yeom J, Choi JH, Shin JH, Kim TH, Jeon JW, et al. Pump-free glass-based capillary microfluidic immuno-assay chip for electrochemical detection of prostate-specific antigen. J Nanosci Nanotechnol. 2020;20(8):4629–33. https://doi.org/10.1166/jnn.2020.17831.
Park J. An optimized colorimetric readout method for lateral flow immunoassays. Sensors. 2018;18(12):4084. https://doi.org/10.3390/s18124084.
Dehus O, Zimmer J, Doring S, Fuhrer F, Hanschmann KM, Holzhauser T, Neske F, Strecker D, Trosemeier JH, Vieths S, Kaul S. Development and in-house validation of an allergen-specific ELISA for quantification of Bet v 4 in diagnostic and therapeutic birch allergen products. Anal Bioanal Chem. 2015;407(6):1673–83. https://doi.org/10.1007/s00216-014-8418-z.
Chaikhan P, Udnan Y, Sananmuang R, Ampiah-Bonney RJ, Chuachuad CW. A low-cost microfluidic paper-based analytical device (μPAD) with column chromatography preconcentration for the determination of paraquat in vegetable samples. Microchem J. 2020;159: 105355. https://doi.org/10.1016/j.microc.2020.105355.
Funding
This work was supported by Korea Environment Industry & Technology Institute (KEITI) through the program for the management of aquatic ecosystem health, funded by Korea Ministry of Environment (MOE) (2020003030001), and Korea Institute of Energy Technology Evaluation and Planning (KETEP) grant funded by the Korea government (MOTIE) (20214000000500, training program of CCUS for the green growth).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethics approval
The blood samples were obtained from “For YOU Moon’s” Maternity hospital. Written informed consent was obtained from each participant.
Conflict of interest
Sang-nam Lee was employed by the company Uniance Gene Inc. The remaining authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Published in the topical collection Point-of-Care Testing with guest editors Oliver Hayden, Peter B. Luppa, and Junhong Min.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lee, MJ., Soum, V., Lee, SN. et al. Pumpless three-dimensional photo paper–based microfluidic analytical device for automatic detection of thioredoxin-1 using enzyme-linked immunosorbent assay. Anal Bioanal Chem 414, 3219–3230 (2022). https://doi.org/10.1007/s00216-021-03747-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00216-021-03747-0