Abstract
Parkinson’s disease is a neurodegenerative disease often characterized by motor deficits and most commonly treated with dopamine replacement therapy. Despite its benefits, chronic use of L-DOPA results in abnormal involuntary movements known as L-DOPA-induced dyskinesia. Growing evidence shows that with burgeoning dopamine cell loss, neuroplasticity in the serotonin system leads to the development of L-DOPA-induced dyskinesia through the unregulated uptake, conversion, and release of L-DOPA-derived dopamine into the striatum. Previous studies have shown that coincident 5-HT1A agonism and serotonin transporter inhibition may have anti-dyskinetic potential. Despite this, few studies have explicitly focused on targeting both 5-HT1A and the serotonin transporter. The present study compares the 5-HT compounds Vilazodone, YL-0919, and Vortioxetine which purportedly work as simultaneous 5-HT1A receptor agonists and SERT blockers. To do so, adult female Sprague Dawley rats were rendered hemiparkinsonian and treated daily for two weeks with L-DOPA to produce stable dyskinesia. The abnormal involuntary movements and forehand adjusting step tests were utilized as measurements for L-DOPA-induced dyskinesia and motor performance in a within-subjects design. Lesion efficacy was determined by analysis of striatal monoamines via high-performance liquid chromatography. Compounds selective for 5-HT1A/SERT target sites including Vilazodone and Vortioxetine significantly reduced L-DOPA-induced dyskinesia without compromising L-DOPA pro-motor efficacy. In contrast, YL-0919 failed to reduce L-DOPA-induced dyskinesia, with no effects on L-DOPA-related improvements. Collectively, this work supports pharmacological targeting of 5-HT1A/SERT to reduce L-DOPA-induced dyskinesia. Additionally, this further provides evidence for Vilazodone and Vortioxetine, FDA-approved compounds, as potential adjunct therapeutics for L-DOPA-induced dyskinesia management in Parkinson’s patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since its introduction in the late 1960s, 1–3-4-dihydroxyphenylalanine (L-DOPA) has been the most effective pharmacotherapy in relieving Parkinson’s disease (PD) motor symptoms. Unfortunately, up to 90% of patients develop L-DOPA-induced dyskinesia (LID), often characterized by abnormal involuntary movements (AIMs) of the trunk, limb, and face, within 10 years of chronic L-DOPA treatment (Ahlskog and Muenter 2001; Connolly and Lang 2014; Schrag and Quinn 2000; Smith et al. 2009; Hely et al. 2005).
Growing evidence indicates that late-stage effects of L-DOPA are driven by neuroplasticity in the serotonergic system (Brown and Molliver 2000; Carta et al. 2007; Eskow et al. 2009; Politis et al. 2014). Numerous studies demonstrate serotonergic hyperinnervation in the striatum following dopamine (DA) denervation (Kannari et al. 2006; Politis et al. 2014; Rylander et al. 2010; Sellnow et al. 2019). Within the dorsal raphe nucleus (DRN), serotonin (5-HT) neurons possess the machinery necessary to convert and release DA from exogenous L-DOPA, contributing to its unregulated release within the raphe-striatal pathway (Brown and Molliver 2000; Tanaka et al. 1999; Lindgren et al., 2010; Sellnow et al. 2019; Fu et al. 2018). This process is thought to play a causal role in the development of LID, in part, through overstimulation of populations of DA D1 receptors on medium spiny neurons (MSNs) in the dorsal striatum (Lanza et al. 2018; Girasole et al. 2018; Fieblinger et al. 2018; Parker et al. 2018).
Interestingly, several 5-HT1A receptor agonists display anti-dyskinetic profiles in preclinical and clinical models (Bibbiani et al. 2001; Bishop et al. 2012; Eskow et al. 2007; Politis et al. 2014; Meadows et al. 2017). 5-HT1A autoreceptors and heteroreceptors are positioned on or in proximity to 5-HT neurons and, in the hemiparkinsonian rat brain, modify raphe-striatal neuron release of L-DOPA-derived DA and corticostriatal glutamate into the striatum (Kannari et al. 2006; Carta et al. 2007; Dupre et al. 2011; Lindgren et al., 2010). The partial 5-HT1A agonist buspirone, reduced LID and maintained motor improvement of L-DOPA in animal models (Dekundy et al. 2007; Eskow et al. 2007) but clinical studies have indicated that higher doses may worsen PD symptoms (Hammerstad et al. 1986; Ludwig et al., 1986; Schneider et al. 2020). Similarly, the more selective 5-HT1A agonists, such as 8-OH-DPAT, sarizotan, and NLX-112 were able to mitigate LID but resulted in susceptibility to 5-HT syndrome and/or reduced L-DOPA efficacy (Bibbiani et al. 2001; Fisher et al. 2020; Iravani et al. 2006; Lindenbach et al. 2015).
Inhibition of the 5-HT transporter (SERT) has also been shown to have anti-dyskinetic effects (Bishop et al. 2012, Inden et al. 2012; Kuan et al., 2008; Conti et al. 2014, Conti et al. 2016). Upregulation of striatal SERT during the progression of PD and particularly in subjects with LID suggest it may be a pharmacologically therapeutic target (Conti et al. 2016; Larsen et al. 2011; Rylander et al. 2010; Roussakis et al. 2016; Strecker et al. 2011). Selective serotonin reuptake inhibitors (SSRIs) have been shown to reduce LID and maintain L-DOPA’s promotor effects, possibly through indirectly targeting 5-HT1A autoreceptors while concomitantly inhibiting DA reuptake (Bishop et al. 2012; Kannari et al. 2006; Navailles et al. 2010). In the rat hemiparkinsonian model of PD, subchronic pharmacological treatment with SSRIs completely suppressed LID development and expression at relatively low doses without compromising L-DOPA’s therapeutic efficacy (Conti et al. 2014; Lindenbach et al. 2015). Conflicting results from non-human primate studies indicate acute impairment of L-DOPA efficacy that may or may not persist with chronic administration or lower doses (Fidalgo et al. 2015). Importantly, chronic SSRI treatment delayed LID onset in a small clinical trial as well as minimized comorbid affective disorders in PD patients (Mazzucchi et al. 2015).
Recent studies have focused on the dual action of 5-HT1A agonists and SERT blockers for LID management (Altwal et al. 2020; Meadows et al. 2018). Vilazodone is a US Food and Drug Administration (FDA)–approved antidepressant leveraging this simultaneous partial 5-HT1A agonism and potent SERT inhibition (Altwal et al. 2020; Cruz 2012; Meadows et al. 2018). Vortioxetine, a recently FDA-approved antidepressant, likewise targets 5-HT1A and SERT, but with a lower affinity for the 5-HT1A receptor in rodents than in humans (Okada et al. 2019). It also has a broad affinity for other serotonergic targets, including partial agonism for 5-HT1B, antagonism for 5-HT1D, 5-HT3, and 5-HT7 receptors, highlighting its potential in treating LID (Chen et al. 2018; Lanza and Bishop 2018). The compound YL-0919 has an affinity for both 5-HT1A and SERT but has not been previously tested in PD models (Chen et al. 2013).
The current study therefore primarily sought to determine whether the unique shared profiles of these compounds as 5-HT1A agonists and SERT blockers conferred anti-dyskinetic effects across a broad dose range. Secondarily, we hypothesized that differences in efficacy against LID across compounds could be conveyed through their divergent pharmacological properties of serotonergic modulation.
2. Materials and methods
Animals
Adult female Sprague-Dawley rats weighing 200–250g prior to surgery were used for all experiments (N=36). Animals had access to water and standardized lab chow (Rodent Diet 5001; Lab Diet, Brentwood, MO, USA) ad libitum. Rats were kept in the colony at a room temperature of 22 to 23°C on a 12-h light/12-h dark cycle beginning at 07:00h. Animals were cared for according to the Institutional Animal Care and Use Committee of Binghamton University and the “Guide for the Care and Use of Laboratory Animals” (Institute for Laboratory Animal Research, National Academic Press, 2011).
Surgical procedure
In all experiments, rats received a unilateral DA lesion using 6-hydroxydopamine hydrobromide (6-OHDA; Sigma, St. Louis, MO, USA) in the left medial forebrain bundle to produce extensive DA cell loss in the nigrostriatal pathway (Conti et al. 2014). Rats were anesthetized with inhalant Isoflurane (2–3%; Sigma) in oxygen (2.5L/min) following an injection of Buprenex (buprenorphine HCL: 0.03mg/kg, i.p., Hospira Inc., Lake Forest, IL, USA) and placed in a stereotaxic apparatus (David Kopf Instruments, Tujunga, CA, USA). A 10μL Hamilton syringe with a 26-gauge needle (Hamilton Company, Reno, NV) was lowered into the target site relative to bregma at the following coordinates: AP, −1.8mm; ML, −2.0mm; DV, −8.6mm (Paxinos and Watson 1998). The target site was reached by drilling a small hole into the skull. 6-OHDA (3μg/1μL; Sigma) dissolved in 0.9% NaCl + 0.1% ascorbic acid was injected slowly at a rate of 2μL/min for a total volume of 4μL over a 2-min period. The needle remained at the target site for 5 min after injection to ensure toxin diffusion. After the needle was withdrawn, sterile staples were used to close the surgical site. Following surgery, animals were pair-housed in clean thermoregulated cages for recovery from anesthesia. As a post-operative analgesic, Carprofen (Rimadyl: 5mg/kg, Zoetis Inc, Kalamazoo, MI, USA) was administered 12 and 24 h following the surgery. Rats were closely monitored post-operatively, receiving soft food, physiological saline (s.c.), and enrichment as needed over 10 days. To allow for sufficient recovery time, all experiments started 3 weeks post-surgery.
Behavioral analyses
Abnormal involuntary movements
Rat dyskinesia was evaluated using the abnormal involuntary movement (AIM) rating scale as previously described (Dekundy et al. 2007). Ten minutes following L-DOPA injections, rats were placed in clear Plexiglas cylinders with bedding. A trained and blinded observer-rated dyskinesia duration according to the presence of axial, limb, and orolingual behaviors (ALO) for 1 min every 10 min for 180 min total (Dekundy et al. 2007; Bishop et al. 2012; Bhide et al. 2015). Specifically, “axial” is identified by an uncontrolled torsion of the trunk contralateral to the lesion, “limb” is characterized by dystonic, repetitive movement of the limb contralateral to the lesion, and “orolingual” is defined by side-to-side jaw movements accompanied with tongue protrusions. Behaviors were ranked on a scale from zero to four according to the duration of the observed behavior using the following qualifications: zero (absent), one (present for less than 30s), two (present between 30 and 59s), three (present for 60s but interrupted by stimulus), and four (present for 60s and not interrupted by stimulus). During the first 14 days of L-DOPA treatment the development of LID was tracked by measuring AIMs on days 1, 8, and 14. A criterion summed ALO score >25 correlates with a striatal DA loss of 95% (Taylor et al., 2005). Animals that did not meet this threshold, were excluded from the study.
Forepaw adjusting steps
The forepaw adjusting step (FAS) test is a measure of forepaw akinesia utilized to verify lesion post-surgery and monitor drug-induced changes to motor performance. Rats with >80% striatal DA loss perform poorly on this test; hence, it is used to verify 6-OHDA lesion efficacy (Chang et al. 1999). Importantly, L-DOPA and DA agonists improve FAS performance (Olsson et al., 1995), making it a useful test to measure treatment-related effects on motor performance. During testing, a trained and blinded experimenter held each rat so that one paw was restrained, and the opposite forepaw rested on a flat platform. Rats were moved laterally so that the forepaw steps were counted at a rate of 90 cm/10 s. Rats were dragged in the forehand (medial) and backhand (lateral) direction for each forepaw in 3 trials each test day. Rats were exposed to at least three acclimations to the procedure prior to data collection. FAS tests were employed prior to L-DOPA priming to record a baseline measure of motor impairment, as well as during treatment while exhibiting peak dyskinesia during the AIMs test 70 min after receiving L-DOPA. Forehand percent intact (FPI) was calculated by dividing forehand lesioned paw steps by forehand intact paw steps and multiplying by 100. Total percent intact (TPI) was calculated to estimate the degree of the lesion by dividing lesioned stepping by intact stepping and multiplying by 100. Animals with ≥25% FPI were deemed to have insufficient lesions to become dyskinetic and were removed from the study.
Experimental design
Pharmacological treatments
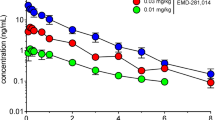
As depicted in Fig. 1A, following 3 weeks of recovery, all rats (n=36) went through FAS testing to establish baseline motor performance and evaluate lesion severity. Lesioned animals (<25% FPI) then received L-DOPA methyl ester (hereafter L-DOPA; 6 mg/kg, s.c.; Sigma) + DL-serine 2-(2,3,4-trihydroxybenzyl) hydrazide hydrochloride (benserazide; 15 mg/kg, s.c.; Sigma) dissolved in 0.9% NaCl + 0.1% ascorbic acid once daily for 14 days to induce stable LID (Conti et al. 2014; Lindgren et al., 2006; Putterman et al., 2007). ALO AIMs were assessed on days 1, 8, and 14 of daily L-DOPA treatment (n=24). On testing days, one of three serotonergic drugs that act as 5-HT1A agonists and SERT blockers, Vilazodone, YL-0919, and Vortioxetine, were administered 5 min prior to L-DOPA to determine their anti-dyskinetic efficacy. Each drug was administered in a within-subjects counterbalanced fashion to ensure each rat received each drug at every dose. Each drug was tested within a given cohort, run sequentially. Vilazodone doses were chosen using previous studies (Meadows et al. 2018; Page et al. 2015). Given that YL-0919 and Vortioxetine had not been previously tested in parkinsonian animal models, doses were selected based on effective doses that modulate the 5-HT system in depression rat models (Ran et al. 2018; Zhang et al. 2017, Jensen et al., 2014; Okada et al. 2019). Vilazodone was dissolved in 50% DMSO + dH2O (vehicle) for all experiments. YL-0919 was dissolved in dH2O (vehicle). Lastly, Vortioxetine was dissolved in 20% beta-cyclodextrin + saline (vehicle). All drugs were administered subcutaneously at a volume of 1ml/kg.
Experimental timeline and design and axial, limb and orolingual (ALO) abnormal involuntary movement (AIMs) development during chronic L-DOPA treatment. A In all 3 experiments, female Sprague Dawley rats received a unilateral medial forebrain bundle (MFB) lesion with 6-hydroxydopamine (6-OHDA). Rats were acclimated for at least 1 week and handled for a minimum of 4 days pre-surgery. Surgery was followed by a 3-week recovery period after which lesion efficacy was assessed using the forepaw adjusting steps (FAS) test. Thereafter, all rats received daily L-DOPA (hereafter, 6 mg/kg + 12 mg/kg benserazide, s.c.) to produce stable L-DOPA-induced dyskinesia (LID). B When monitoring the development of AIMs in all subjects, analyses revealed increased AIMs from days 1 to 8 that were maintained on day 14 (*p < 0.05 vs. Day 1). Thereafter rats meeting an ALO criterion score of > 25 by day 14 were tested in drug-specific cohorts in a within-subjects counterbalanced design. In experiment 1 rats were injected with Vehicle or Vilazodone (VZD; 5, 10, 20 mg/kg, s.c.) 5 min prior to L-DOPA. In experiment 2, rats were injected with Vehicle or YL-0919 (0.625, 1.25, 2.5 mg/kg, s.c.) 5 min prior to L-DOPA. In experiment 3, rats received Vehicle or Vortioxetine (VXT; 2.5, 5, 10 mg/kg, s.c.) 5 min prior to L-DOPA. During treatment, rats were rated on the observed ALO AIMs scale every 10 min for 180 min. Sixty min after their first AIMs rating, FAS was used to evaluate motor performance. Each treatment day was followed by a 3-day washout. A week after testing, left and right striata were harvested off-treatment to measure monoamine levels and confirm lesion via high-performance liquid chromatography (HPLC)
Neurochemical analyses
High-performance liquid chromatography
After subjects completed experiments, their brains were harvested following rapid decapitation, flash-frozen in 2-methylbutane on dry ice, and stored at -80°C for subsequent tissue dissection. HPLC was used to analyze striatal levels of 5-HT, and DA for lesion verification as previously described (Conti et al. 2014). DA was electrochemically detected with a limit of detection of 10-10M. Final oxidation current values were plotted on a standard curve with concentrations ranging from 10-6 and 10-10M. Values were adjusted for tissue weight. Monoamine levels were expressed as a picogram of monoamine per milligram of tissue.
Statistical analyses
Group AIMs data were represented as medians + median absolute deviations (M.A.D.) and analyzed using non-parametric Friedman ANOVAs for effects on overall ALO AIMs and for individual ALO AIMs timepoints. When significant main effects of treatment were revealed, Wilcoxon post hocs were used to examine differences amongst treatment conditions. FAS and HPLC data were represented as mean percent intact + standard error of the mean (S.E.M.). FAS data were analyzed using ANOVAs and Fisher LSD for pairwise comparisons. HPLC data were analyzed using paired t-tests. The SPSS statistics software (Chicago, IL, USA) was used for all statistical analyses with an alpha of p< 0.05.
Results
FAS baseline and development of LID in hemiparkinsonian rats
The AIMs test was used to monitor LID development in 6-OHDA-lesioned rats that demonstrated significant stepping deficits on the FAS (<25% FPI). Of the original 36 rats that started the study, 6 rats did not meet FAS criteria and were removed prior to chronic L-DOPA treatment (n=30, µ = 2.25 ± 0.55). Six additional rats did not meet ALO AIMs threshold (>25) after 14 days of L-DOPA treatment and were also withdrawn prior to the start of interventional studies with the 5-HT compounds (n=24). When analyzing ALO AIMs development in the remaining rats, an effect of treatment day was revealed (n=9; Fig. 1Bχ2 (2) = 28.80, p<0.05). Post hoc analyses indicated a significant increase in LID from day 1 to 8 (p<0.05) which was maintained on day 14 (p<0.05 vs. day).
Experiment 1: Effects of Vilazodone on L-DOPA-induced behaviors
Vilazodone attenuates LID expression
In experiment 1 (n=9), AIMs were quantified in dyskinesia-primed rats that received various doses (5, 10, 20mg/kg) of Vilazodone, 5 min prior to L-DOPA (6 mg/kg, s.c.). As depicted in Fig. 2, Vilazodone significantly reduced dyskinetic behavior. Across the entire 3h testing period, the moderate (10mg/kg) and high (20mg/kg) doses significantly differed from vehicle (Fig. 2A inset; χ2 (3) = 15.13, p<0.05). Analysis across time further revealed dose-dependent differences. The high dose (20mg/kg) reduced ALO AIMs from time points 40-130 min when compared to vehicle (all p<0.05). The moderate dose (10mg/kg) reduced ALO AIMs at time points 40, 60, 70, 90, 100, 110, and 130min (all p<0.05). The low dose (5mg/kg) differed from the vehicle at time points 40 and 130min (both p<0.05).
Effects of Vilazodone (VZD) on L-DOPA (LD)-induced axial, limb, and orolingual abnormal involuntary movements (ALO AIMs) and motor performance on the forepaw adjusting steps test (FAS). In a counterbalanced within-subjects design, unilaterally 6-hydroxydopamine-lesioned rats (N = 9) received Vehicle (Veh) or VZD (5, 10, 20 mg/kg, s.c.) 5 min prior to LD (6 mg/kg + 15 mg/kg benserazide, both s.c.). A ALO AIMs were recorded and are shown every 10 min for 180 min and summed over the entire testing period (see inset). B To examine the effects of VZD on LD improvements on the FAS test, 60 min after treatments on AIMs test days, rats’ stepping was assessed. AIMs data are expressed as medians + median absolute deviation (M.A.D.), FAS data were calculated as a percent of forehand stepping on the lesioned vs. intact side and shown as means + standard error of the mean (S.E.M.). *p < 0.05 VZD(20) vs. VEH, ^p < 0.05 VZD(10) vs. VEH, + p < 0.05 VZD(5) vs. VEH, @p < 0.05 vs. baseline)
Vilazodone maintains L-DOPA motor efficacy
Vilazodone maintains L-DOPA motor efficacy
FAS was conducted to evaluate motor performance during drug treatments. Analysis revealed a significant main effect of treatment compared to baseline (F(1,4) = 23.321, p<0.05). Post hoc comparisons showed that compared to baseline, all rats showed significant improvements in motor performance (Fig. 2B; all p<0.05). Moreover, there were no significant differences in motor performance between Vilazodone and L-DOPA treatments, indicating Vilazodone treatment maintained L-DOPA-induced motor improvements at all doses.
Experiment 2: Effects of YL-0919 on L-DOPA-induced behaviors
YL-0919 fails to reduce LID expression
In experiment 2 (n=9), shown in Fig. 3A, YL-0919 across all doses (0.625, 1.25, 2.5mg/kg), failed to significantly reduce overall ALO AIMs (Fig 3A. inset; χ2 (3) = 3.305; ns). Further timepoint analyses revealed that while there was an overall effect of treatment at 100min (p<0.05), there was no effect of any YL-0919 dose compared to vehicle.
Effects of YL-0919 (YL) on L-DOPA (LD)-induced axial, limb, and orolingual abnormal involuntary movements (ALO AIMs) and motor performance on the forepaw adjusting steps test (FAS). In a counterbalanced within-subjects design, unilaterally 6-hydroxydopamine-lesioned rats (N = 9) received Vehicle (Veh) or YL (0.625, 1.25, 2.5 mg/kg, s.c.) 5 min prior to LD (6 mg/kg + 15 mg/kg benserazide, both s.c.). A ALO AIMs were recorded and are shown every 10 min for 180 min and summed over the entire testing period (see inset). B To examine the effects of YL on LD improvements on the FAS test, 60 min after treatments on AIMs test days, rats’ stepping was assessed. AIMs data are expressed as medians + median absolute deviation (M.A.D.), FAS data were calculated as a percent of forehand stepping on the lesioned vs. intact side and shown as means + standard error of the mean (S.E.M.). @p < 0.05 vs. baseline)
YL-0919 maintains L-DOPA motor efficacy
When examining the effects of YL-0919 on the FAS test, an ANOVA demonstrated a significant main effect of treatment (F(1,4) = 21.694, p<0.05). Post hoc analyses revealed that all treatments that included L-DOPA were effective in reversing lesion-induced deficits seen at baseline (Fig. 3B; all p<0.05), indicating YL-0919 at all doses also maintained the benefits of L-DOPA administration.
Experiment 3: effects of Vortioxetine on L-DOPA-induced behaviors
Vortioxetine reduces LID expression
In experiment 3 (n=6) shown in Fig. 4A, Vortioxetine (2.5, 5, 10mg/kg) significantly reduced overall ALO AIMs (Fig. 4A inset; χ2 (3) = 18.0, p<0.05). Post hoc analyses revealed that each Vortioxetine treatment significantly reduced LID in a dose-dependent manner versus L-DOPA alone (all p<0.05). Analyses of timepoints across the 180min of testing revealed significant differences between treatment groups. The high dose (10mg/kg) suppressed ALO AIMs from 10 to 110min and 130min when compared to vehicle pretreatment (all p<0.05). At the moderate dose (5mg/kg), ALO AIMs were significantly lower from vehicle pretreatment at time points 20-70min, 90-110min, and 130min (all p<0.05). The low dose (2.5mg/kg) reduced ALO AIMs from the vehicle at time points 60min and 100–130min (all p<0.05).
Effects of Vortioxetine (VXT) on L-DOPA (LD)-induced axial, limb, and orolingual abnormal involuntary movements (ALO AIMs) and motor performance on the forepaw adjusting steps test (FAS). In a counterbalanced within-subjects design, unilaterally 6-hydroxydopamine-lesioned rats (N = 6) received Vehicle (Veh) or VXT (2.5, 5, 10 mg/kg, s.c.) 5 min prior to LD (6 mg/kg + 15 mg/kg benserazide, both s.c.). A ALO AIMs were recorded and are shown every 10 min for 180 min and summed over the entire testing period (see inset). B To examine the effects of VXT on LD improvements on the FAS test, 60 min after treatments on AIMs test days, rats’ stepping was assessed. AIMs data are expressed as medians + median absolute deviation (M.A.D.), FAS data were calculated as a percent of forehand stepping on the lesioned vs. intact side and shown as means + standard error of the mean (S.E.M.). *p < 0.05 VXT (10) vs. VEH, ^p < 0.05 VXT(5) vs. VEH, + p < 0.05 VXT(2.5) vs. VEH, @p < 0.05 vs. baseline)
Vortioxetine maintains L-DOPA motor efficacy
Upon analysis of the effects of Vortioxetine on FAS (Fig. 4B), an ANOVA revealed a significant main effect of treatment (F(1,4) = 5.48, p<0.001). Post hoc analyses demonstrated that any pretreatment paired with L-DOPA improved stepping versus baseline, while there were no significant differences in forehand percent intact between these treatments (all p<0.05).
Neurochemical analyses
High-performance liquid chromatography
Severity of lesion was assessed post-mortem by analysis of DA and DOPAC levels in the left (lesion) and right (intact) striata via reverse-phase HPLC (Table 1). Rats displayed a significant reduction in pg/mg tissue of DA (Mlesion= 64.60, Mintact= 10799.18; t23= −23.37, p<0.05) and DOPAC (Mlesion= 106.88, Mintact= 4038.90; t23= −21.99, p<0.05) levels in the lesioned striatum compared to the intact side (99.40% and 97.35% respectively). DA turnover revealed a main effect of lesion (Mlesion= 1.97, Mintact = 0.38; t23= −5.98, p<0.05). Upon analysis of non-DA monoamines and metabolites, 5-HT was significantly lower in lesioned striata (Mlesion= 47.07, Mintact= 138.15; t23= −7.03, p<0.05) while no significant difference in NE (Mlesion= 1.33, Mintact= 10.02; t14= −1.95, p>0.05) or 5-HIAA (Mlesion= 815.25, Mintact= 651.28; t23= 1.10, p>0.05) were observed. 5-HT turnover showed no significant effects of lesion (Mlesion= 18.50, Mintact= 9.82; t23= –1.43, p>0.05).
Discussion
Despite advances in drug formulation and deep brain stimulation, LID remains an intractable problem for a subset of PD patients. (Ahlskog and Muenter 2001; Cenci et al. 2020; Fisher et al. 2020). Although various mechanisms are involved in LID development, growing evidence points to aberrant neuroplastic changes within the 5-HT system that lead to striatal DA fluctuations and eventual LID expression (Carta et al. 2007; De La Fuente-Fernández et al. 2004; Eskow et al. 2009; Politis et al. 2014; Sellnow et al. 2019). Over the last two decades, investigations of the 5-HT system in LID have provided various targets for therapeutic intervention (for review, see Lanza and Bishop 2018). Yet, translation of serotonergic compounds to the clinic to provide beneficial LID relief has not yet been realized.
Prior studies have examined upregulation of SERT and several 5-HT receptors in the basal ganglia, 5-HT1A and 5-HT1B, all of which have shown potential modulation of LID (Carta et al. 2007; Hamadjida et al. 2018; Huot et al. 2012; Eskow et al. 2009; Rylander et al. 2010; Morin et al. 2015; Conti et al. 2016; Padovan-Neto et al. 2020). Many compounds such as Buspirone, Eltoprazine, Sarizotan, and NLX-112, act as agonists at the 5-HT1A receptor and have been shown to significantly reduce LID (Bezard et al. 2013; Depoortere et al. 2020; Eskow et al. 2007; Iderberg et al. 2015; Paolone et al., 2015; Svenningsson et al., 2015; McCreary et al 2016. However, approval of 5-HT1A compounds, like Sarizotan which progressed all the way to Phase III clinical trials (NCT00105521), was not procured due to intrinsic side effects and/or reduction of L-DOPA’s motor benefits (Goetz et al. 2007; Grégoire et al. 2009; Marin et al. 2009). Compounds that act as SERT inhibitors, including Citalopram and Fluoxetine, reduce the reuptake of 5-HT and, in the PD brain, L-DOPA-derived DA, and have also successfully reduced LID in preclinical models (Kannari et al. 2006; Bishop et al. 2012; Conti et al. 2014; Fidalgo et al. 2015). Unfortunately, even though SSRIs are used in PD patients for a myriad of non-motor symptoms, they have also been reported to reduce L-DOPA motor efficacy when given acutely to non-human primates (Fidalgo et al. 2015). Although studies of 5-HT1B receptors is limited, agonists of this target including CP94253 and Eltoprazine, have indicated some ability to reduce LID (Carta et al. 2007; Jackson et al. 2004; Jaunarajs et al. 2009; Zhang et al. 2008). Indeed, 5-HT1B receptor stimulation may lessen LID by directly reducing striatal medium spiny neuron (MSN) overactivity (Jackson et al. 2004; Zhang et al., 2007; Morin et al. 2015; Padovan-Neto et al. 2020). Even so, it also has been suggested that 5-HT1B receptor agonism alone may have minimal effects on LID attenuation (Carta et al. 2007; Jackson et al. 2004).
Given the evidence for 5-HT1A and SERT as potential LID targets, our laboratory sought out compounds that were designed to act at both targets, albeit with different affinities. Of those available, we identified Vilazodone, Vortioxetine, and YL-0919 (Altwal et al. 2020; Meadows et al. 2018). Prior work with Vilazodone (Meadows et al. 2018) established the potential of this multimodal approach. Here we extended that work by demonstrating that compounds acting as both 5-HT1A receptor agonists and SERT blockers including Vilazodone and Vortioxetine reduced dyskinesia in hemiparkinsonian rats and maintained L-DOPA motor efficacy. Contrary to our hypothesis, YL-0919 did not show any effect on established LID and maintained L-DOPA motor improvements.
We tested Vilazodone on established LID and duplicated previous findings (Meadows et al. 2018; Altwal et al., 2020) which support its potential for clinical translatability given that it is already an FDA approved drug for depression. Currently, Amantadine is the only FDA approved drug for LID treatment; however, it is limited, particularly in later stages of disease by a range of aversive side effects including hallucinations, psychosis, or worsening of existing cognitive impairment/dementia (Crosby et al. 2003; Dashtipour et al. 2019). Vilazodone is postulated to dampen 5-HT neuron-derived DA release during 5-HT1A autoreceptor activation in DRN neurons that project to the striatum. While this is the main mechanism thought to lead to reductions in dyskinesia, 5-HT1A heteroreceptor activation located post-synaptically in the cortex or presynaptically in the striatum may also reduce overstimulation of the corticostriatal glutamatergic projections (Antonelli et al. 2005; Carta et al. 2007; Bishop et al. 2009; Dupre et al. 2007; Ostock et al. 2011; Suh et al. 2012; Yamada et al. 1988).
Our findings demonstrated that Vilazodone dose-dependently reduced ALO AIMs scores over time across all doses tested (Fig. 2A). Fortunately, unlike other 5-HT1A agonists, intrinsic side effects such as 5-HT syndrome have not been reported with Vilazodone; in fact, Vilazodone has been shown to reverse 5-HT syndrome induced by the selective 5-HT1A agonist 8-OH-DPAT (Page et al., 2002; Lindenbach et al. 2015; Fisher et al. 2020). Similar to our prior work, few additional motor benefits were seen when exceeding the 10mg/kg dose (Meadows et al. 2018). To add to this point, Vilazodone at the 10 mg/kg dose has been shown to have 100% occupancy at SERT sites in the hippocampus and cortex of rats (Hughes et al. 2005). As such, further studies should seek to expand the lower range of Vilazodone dose efficacy in LID attenuation.
A relatively novel drug, YL-0919, with purported partial agonism at 5-HT1A receptor and SERT inhibition, was also investigated in this study. While YL-0919 has been effective in pre-clinical models of depression and clinical depression (Chen et al. 2013; Ran et al. 2018; Zhang et al. 2017), we are the first lab to test it in a hemiparkinsonian rodent model of LID. Similar to Vilazodone, dose selection of 0.625–2.5mg/kg for YL-0919 was based on experiments establishing bioactivity on rodent depression assays (Owen 2011; Meadows et al. 2018; Ran et al. 2018; Zhang et al. 2017). Despite YL-0919’s reported pharmacological similarity to Vilazodone, ALO AIMs were not affected at any dose. Neither was motor performance on L-DOPA when evaluated on FAS.
While the differences between Vilazodone and YL-0919 were surprising, the recent discovery of YL-0919’s activity at the 5-HT6 receptor may have contributed to the lack of treatment effects in LID. The 5-HT6 heteroreceptor is an excitatory Gs protein-coupled receptor that positively stimulates the adenylate cyclase-cAMP-PKA cascade (Ohno et al. 2015). It is abundantly located in the striatum and is thought to influence extrapyramidal motor function (Ohno et al. 2015). In fact, a study of graft-induced dyskinesia, a condition that sometimes occurs following striatal DA cell transplantation, demonstrated that 5-HT6 receptor activation was a potential causal factor (Aldrin-Kirk et al. 2016). Another study showed that 5-HT6 receptor stimulation in the frontal cortex can modulate 5-HT terminal release in neurons within 5-HT cell bodies (Gérard et al. 1996; Gérard et al. 1997; Ward et al. 1995; Zhang et al., 2011, Brouard et al. 2015). In our study, increased 5-HT firing and terminal activity via YL-0919-induced 5-HT6 receptor stimulation may have activated prolonged 5-HT-derived DA release and promoted hyperkinetic effects.
Another explanation for differences in dyskinesia expression following administration of YL-0919 or Vilazodone may be due to actions on local drug targets on SERT. Chronic L-DOPA treatment significantly increases SERT expression (Conti et al. 2016; Roussaki et al., 2015; Rylander et al. 2010), and SSRIs have been shown to reduce LID (Bishop et al. 2012; Conti et al. 2014; Huot et al. 2015). Although the mechanism(s) by which SERT inhibition reduces LID are not entirely understood, some have suggested that blocking SERT increases peri-synaptic 5-HT and indirect activation of 5-HT1A autoreceptors that regulate 5-HT neurons to inhibit raphe-striatal L-DOPA-derived DA release (Conti et al. 2014, 2016; Kanari et al. 2006). Notably, opposite effects are observed if SSRIs are locally administered into the striatum, which SERT blockade can prevent DA uptake into 5-HT terminals thereby perpetuating local DA signaling and LID (Kanari et al. 2006; Larsen et al. 2011). From this understanding, YL-0919 may possibly act preferentially on striatal SERT and counteract its antidyskinetic 5-HT1A receptor actions. There is some evidence of differential SERT actions across SSRIs. For example, compared to other SSRIs (Fluvoxamine and Paroxetine), Sertraline was the only SSRI to increase DA in the striatum (Bishop et al 2012; Kitaichi et al. 2010). Further analyses using microdialysis would be able to elucidate the scope of DA release in the striatum during YL-0919 treatment.
Similar to Vilazodone, Vortioxetine is a recently FDA-approved drug for the treatment of major depression and has multimodal effects within the 5-HT system. In alignment with many SSRIs, Vortioxetine has a strong antidepressant profile. Previous doses of Vortioxetine showing antidepressant effects in rodent models ranged from 2.5 to 10mg/kg (Mørk et al. 2012). This effective pharmacological range was used in this study and produced a significant dose-dependent reduction on ALO AIMs and like Vilazodone, maintained L-DOPA efficacy for reversing lesion-induced motor deficits (Fig. 4). Until recently, it had not been tested on pre-clinical LID models.
In contrast to Vilazodone and YL-0919, Vortioxetine has a more promiscuous profile, targeting the 5-HT1B and 5-HT3 receptors with a lower affinity for the 5-HT1A and 5-HT7 receptor in rats compared to humans (Chen et al. 2018). In humans, Vortioxetine’s affinity for 5-HT1A (Ki=15nM) significantly differs from rats (Ki = 230nM). Additionally, it’s a potent 5-HT3 receptor antagonist (Ki=3.7nM), a modest 5-HT7 antagonist (Ki=200nM), and a partial agonist at 5-HT1B (Ki = 33nM), suggesting possible alternative mechanisms that inhibit LID development (Okada et al. 2019).
Despite its lower affinity for the 5-HT1A receptor in the rat brain, previous work has shown that at high doses (10mg/kg) Vortioxetine establishes approximately 35% receptor occupancy (Mørk et al. 2013). The greatest reduction in ALO AIMs (Fig 4A) may be attributed to increased 5-HT1A receptor occupation at the high dose. This suggests Vortioxetine tested in clinical trials may show a greater effect in LID reduction than what is apparent in rodent models. This also highlights alternative mechanisms which may indirectly stimulate 5-HT1A autoreceptors in the DRN to dampen exogenous DA release. Moreover, previous work showed that subacute administration of Vortioxetine demonstrated a lack of intrinsic 5-HT1A activity; however, antagonism of the 5-HT1A receptor reduced Vortioxetine effects (Bétry et al. 2013). This further suggests indirect action at other 5-HT receptors that modulate 5-HT1A receptor activation. In the case of SERT inhibition, 80% receptor occupancy was detected in rodents at a 10mg/kg dose (Mørk et al. 2013). This supports previous work that attributes enhanced LID reduction to the synergistic dual action at the 5-HT1A receptor and SERT (Meadows et al. 2018; Atwal et al., 2020).
While 5-HT1A action is present with Vortioxetine administration, it is likely that action at a combination of 5-HT receptors contributes to overall LID reductions in rats observed at lower doses (2.5 and 5 mg/kg). Another possibility that may account for observed LID attenuation is the activation of 5-HT1B auto- and hetero- receptors on 5-HT terminals in the striatum and PFC (Carta et al. 2007). 5-HT1B receptors regulate terminal 5-HT release on MSNs and inhibit GABA release that innervates the striatum and globus pallidus (Ceci et al. 1994; Carta et al. 2007; Lanza et al. 2018). Increased 5-HT1B expression in the striatum has been reported in response to DA loss and L-DOPA administration in 6-OHDA rodent models and MPTP non-human primate models (Jackson et al. 2004; Zhang et al., 2007; Morin et al. 2015). 5-HT1B receptor stimulation may counter this overexpression by normalizing 5-HT release from terminals thus dampening the release of DA from 5-HT neurons. Future work is needed to explore the mechanism by which 5-HT1B agonism works, either alone or in concert with other 5-HT receptors, though it ultimately offers an alternative mechanism for LID attenuation during Vortioxetine treatment.
Vortioxetine’s multimodal pharmacological profile also presents another, less-explored mechanism at the 5-HT3 receptor as a potential target to modulate 5-HT activity in LID. Investigation of the 5-HT3 receptor in LID is limited; nevertheless, previous studies that focus on Vortioxetine’s antidepressant outcomes attribute its pharmacological effects primarily to 5-HT3 antagonism and SERT inhibition (Bétry et al. 2013; Okada et al. 2019; Bhatt et al., 2020). In PD patients, Ondansetron, a selective 5-HT3 antagonist, co-administered with L-DOPA has been shown to have antidyskinetic effects in 6-OHDA-lesioned rats (Aboulghasemi et al. 2018) and reduce psychosis in PD patients (Zoldan et al. 1995). These effects have been ascribed to 5-HT3 receptor modulation of nigrostriatal DA (Alex and Pehek 2007; Porras et al. 2003). 5-HT3 is the only known 5-HT receptor that is not G-protein coupled and instead exists as an excitatory ligand-gated channel expressed post-synaptically (Leiser et al. 2015). Notably, 5-HT3 receptors are not expressed in the DRN (Koyama et al. 2017), yet are highly expressed in the frontal cortex (Leiser et al. 2015). Furthermore, studies that have examined 5-HT3 receptors in the frontal cortex suggest that they are expressed on GABAergic interneurons (Puig et al. 2004). Inhibition of PFC activity via 5-HT3 receptor antagonism promoted regional 5-HT release due to GABAergic disinhibition (Okada et al. 2019). This regional release may suggest the use of indirect 5-HT1A activation to reduce LID development.
Although the anti-dyskinetic effects of Vilazodone and Vortioxetine were confirmed, there are a few limitations to this work that should be addressed. First, this study utilized only female rats and there are well-documented sex differences in response to 5-HT compounds (Damoiseaux, et al. 2014; LeGates et al. 2019). While we have not tested all of these compounds in both sexes, prior work from our lab and others using Vilazodone indicate similar responses across sexes in rats (Meadows et al. 2018; Altwal et al. 2020; 2021). Whether this holds for Vortioxetine remains an open question. Second, experiments were designed to establish dose-responses, but not chronic efficacy. Given the known lag in antidepressant activity of 5-HT pharmacotherapy (Frazer and Benmansour 2002), future research should further investigate the long-term effectiveness of these compounds. To date, only Vilazodone has been given sub-chronically, demonstrating evidence of prophylactic and interventional anti-LID effects (Meadows et al. 2018). Lastly, the exact mechanisms through which these multimodal 5-HT compounds exert their effects remain enigmatic. In addition to altering L-DOPA-derived DA presynaptically, less canonical mechanisms may also contribute and deserve mention. For example, SSRIs share a common action with the fast-acting antidepressant ketamine, increasing brain-derived neurotrophic factor (BDNF) and action at its cognate receptor Tropomyosin receptor kinase B (TrkB; Saarelainen et al. 2003; Aleksandrova and Phillips 2021; Casarotto et al. 2021). Since ketamine also reduces LID (Bartlett et al. 2016; 2020), a convergent neurotrophic mechanism that may normalize aberrant neuroplasticity is an intriguing, though untested, possibility.
In conclusion, we found that Vilazodone and Vortioxetine displayed dose-dependent anti-dyskinetic effects, whereas YL-0919 displayed no effects, despite having a somewhat similar pharmacological profile. Collectively, these results are consistent with the notion that targeting aberrant serotonergic neuroplasticity is feasible without compromising L-DOPA efficacy. Further translational efforts should ultimately uncover the true promise of these compounds (Jenner 2018). Indeed, recent reports of unique features of Vilazodone as an allosteric SERT inhibitor open novel avenues for drug development (Plenge et al. 2021), while our current work supports repositioning these FDA-approved drugs to serve as supplemental treatments that optimize L-DOPA therapy in PD patients.
Abbreviations
- DA:
-
Dopamine
- Benserazide:
-
DL-Serine 2-(2,3,4-trihydroxybenzyl) hydrazide hydrochloride
- DOPAC:
-
3,4-Dihydroxyphenylacetic acid
- DRN:
-
Dorsal raphe nucleus
- L-DOPA:
-
L-3,4-dihydroxyphenylalanine methyl ester
- 5-HT:
-
Serotonin
- 5-HT1A :
-
Serotonin 1A receptor
- 5-HT1B :
-
Serotonin 1B receptor
- 5-HT3 :
-
Serotonin 3 receptor
- 5-HT6 :
-
Serotonin 6 receptor
- 5-HT7 :
-
Serotonin 7 receptor
- SERT:
-
Serotonin transporter
- SSRI:
-
Selective serotonin reuptake inhibitor
- LID:
-
L-DOPA-induced dyskinesia
- MFB:
-
Medial forebrain bundle
- 6-OHDA:
-
6-Hydroxydopamine hydrobromide
- AIMs:
-
Abnormal involuntary movements
- ALO:
-
Axial, limb, and orolingual
- FAS:
-
Forehand adjusting steps
- PD:
-
Parkinson’s disease
- Veh:
-
Vehicle
- HPLC:
-
High-performance liquid chromatography
- M.A.D.:
-
Median absolute deviation
- S.E.M.:
-
Standard error of the mean
References
Aboulghasemi N, Hadipour Jahromy M, Ghasemi A (2018) Anti-dyskinetic efficacy of 5-HT3 receptor antagonist in the hemi-parkinsonian rat model. IBRO Rep 6:40–44. https://doi.org/10.1016/j.ibror.2018.12.001
Ahlskog JE, Muenter MD (2001) Frequency of levodopa-related dyskinesias and motor fluctuations as estimated from the cumulative literature. Movement Disorders: official journalof the movement disorder society, 16(3):448–458. https://doi.org/10.1002/mds.1090
Alex KD, Pehek EA (2007) Pharmacologic mechanisms of serotonergic regulation of dopamine neurotransmission. Pharmacol Ther 113(2):296–320. https://doi.org/10.1016/j.pharmthera.2006.08.004
Aldrin-Kirk P, Heuer A, Wang G, Mattsson B, Lundblad M, Parmar M, Björklund T (2016) DREADD Modulation of transplanted DA Neurons Reveals a Novel Parkinsonian Dyskinesia Mechanism Mediated by the Serotonin 5-HT6 Receptor. Neuron 90(5):955–968. https://doi.org/10.1016/j.neuron.2016.04.017
Antonelli T, Fuxe K, Tomasini MC, Bartoszyk GD, Seyfried CA, Tanganelli S et al (2005) Effects of sarizotan on the corticostriatal glutamate pathways. Synapse 58:193–199. https://doi.org/10.1002/syn.20195
Aleksandrova LR, Phillips AG (2021) Neuroplasticity as a convergent mechanism of ketamine and classical psychedelics. Trends Pharmacol Sci 42(11):929–942. https://doi.org/10.1016/j.tips.2021.08.003
Altwal F, Moon C, West AR, Steiner H (2020) The Multimodal Serotonergic Agent Vilazodone Inhibits L-DOPA-Induced Gene Regulation in Striatal Projection Neurons and Associated Dyskinesia in an Animal Model of Parkinson’s Disease. Cells 9(10):2265. https://doi.org/10.3390/cells9102265 (MDPI AG)
Altwal F, Padovan-Neto FE, Ritger A, Steiner H, West AR (2021) Role of 5-HT1A Receptor in Vilazodone-Mediated Suppression of L-DOPA-Induced Dyskinesia and Increased Responsiveness to Cortical Input in Striatal Medium Spiny Neurons in an Animal Model of Parkinson’s Disease. Molecules 26(19):5790. https://doi.org/10.3390/molecules26195790
Bartlett MJ, Joseph RM, LePoidevin LM, Parent KL, Laude ND, Lazarus LB, Heien ML, Estevez M, Sherman SJ, Falk T (2016) Long-term effect of sub-anesthetic ketamine in reducing l-DOPA-induced dyskinesias in a preclinical model. Neurosci Lett 612:121–125. https://doi.org/10.1016/j.neulet.2015.11.047
Bartlett M J, Flores AJ, Ye T, Smidt SI, Dollish HK, Stancati JA, Farrell DC, Parent KL, Doyle KP, Besselsen DG, Heien ML, Cowen SL, Steece-Collier K, Sherman SJ, Falk T (2020) Preclinical evidence in support of repurposing sub-anesthetic ketamine as a treatment for L-DOPA-induced dyskinesia. Experimental Neurology, 333. https://doi.org/10.1016/j.expneurol.2020.113413
Bétry C, Pehrson AL, Etiévant A, Ebert B, Sánchez C, Haddjeri N (2013) The rapid recovery of 5-HT cell firing induced by the antidepressant vortioxetine involves 5-HT(3) receptor antagonism. Int J Neuropsychopharmacol 16(5):1115–1127. https://doi.org/10.1017/S1461145712001058
Bezard E, Tronci E, Pioli EY, Li Q, Porras G, Björklund A, Carta M (2013) Study of the antidyskinetic effect of eltoprazine in animal models of levodopa-induced dyskinesia. Mov Disord 28(8):1088–1096. https://doi.org/10.1002/mds.25366
Bhatt S, Devadoss T, Manjula SN, Rajangam J (2020) 5-HT3 receptor antagonism a potential therapeutic approach for the treatment of depression and other disorders. Curr Neuropharmacol. https://doi.org/10.2174/1570159X18666201015155816.Advanceonlinepublication.10.2174/1570159X18666201015155816
Bhide N, Lindenbach D, Barnum CJ, George JA, Surrena MA, Bishop C (2015) Effects of the beta-adrenergic receptor antagonist Propranolol on dyskinesia and L-DOPAinduced striatal DA efflux in the hemi-parkinsonian rat. J Neurochem 134(2):222–232. https://doi.org/10.1111/jnc.13125
Bibbiani F, Oh JD, Chase TN (2001) Serotonin 5-HT1A agonist improves motor complications in rodent and primate parkinsonian models. Neurology 57(10):1829–1834. https://doi.org/10.1212/WNL.57.10.18hls9
Bishop C, Krolewski DM, Eskow KL, Barnum CJ, Dupre KB, Deak T, Walker PD (2009) Contribution of the striatum to the effects of 5-HT1A receptor stimulation in L-DOPA-treated hemiparkinsonian rats. J Neurosci Res 87(7):1645–1658. https://doi.org/10.1002/jnr.21978
Bishop C, George JA, Buchta W, Goldenberg AA, Mohamed M, Dickinson SO, Eissa S, Eskow Jaunarajs KL (2012) Serotonin transporter inhibition attenuates l-DOPA induced dyskinesia without compromising l-DOPA efficacy in hemi-parkinsonian rats. Eur J Neurosci 36(6):2839–2848. https://doi.org/10.1111/j.1460-9568.2012.08202.x
Brouard JT, Schweimer JV, Houlton R, Burnham KE, Quérée P, Sharp T (2015) Pharmacological Evidence for 5-HT6 Receptor Modulation of 5-HT Neuron Firing in Vivo. ACS Chem Neurosci 6(7):1241–1247. https://doi.org/10.1021/acschemneuro.5b00061
Brown P, Molliver ME (2000) Dual serotonin (5-HT) projections to the nucleus accumbens core and shell: relation of the 5-HT transporter to amphetamine-induced neurotoxicity. J Neurosci 20(5):1952–1963. https://doi.org/10.1523/JNEUROSCI.20-05-01952.2000
Carta M, Carlsson T, Kirik D, Bjorklund A (2007) Dopamine released from 5-HT terminals is the cause of l-DOPA-induced dyskinesia in parkinsonian rats. Brain 130:1819–1833. https://doi.org/10.1093/brain/awm082
Casarotto PC, Girych M, Fred SM, Kovaleva V, Moliner R, Enkavi G, Biojone C, Cannarozzo C, Sahu MP, Kaurinkoski K, Brunello CA, Steinzeig A, Winkel F, Patil S, Vestring S, Serchov T, Diniz C, Laukkanen L, Cardon I, Antila H, Rog T, Petteri T, Piepponen B, C. R., Normann, C., Lauri, S. E., Saarma, M. Vattulainen, I., Castrén, E. (2021) Antidepressant drugs act by directly binding to TRKB neurotrophin receptors. Cell 184(5):1299-1313.e19. https://doi.org/10.1016/j.cell.2021.01.034
Ceci A, Baschirotto A, Borsini F (1994) The inhibitory effect of 8-OH-DPAT on the firing activity of dorsal raphe serotoninergic neurons in rats is attenuated by lesion of the frontal cortex. Neuropharmacology 33:709–713. https://doi.org/10.1016/0028-3908(94)90177-5
Chang JW, Wachtel SR, Young D, Kang UJ (1999) Biochemical and anatomical characterization of forepaw adjusting steps in rat models of Parkinson’s disease: Studies on medial forebrain bundle and striatal lesions. Neuroscience 88(2):617–628. https://doi.org/10.1016/S0306-4522(98)00217-6
Chen G, Højer AM, Areberg J, Nomikos G (2018) Vortioxetine: Clinical Pharmacokinetics and Drug Interactions. Clin Pharmacokinet 57(6):673–686. https://doi.org/10.1007/s40262-017-0x612-7
Chen HX, Jin ZL, Zhang LM, Xue R, Xu XD, Zhao N et al (2013) Antidepressant -like activity of YL-0919: a novel combined selective serotonin reuptake inhibitor and 5-HT1A receptor agonist. PLoS ONE 8:e83271. https://doi.org/10.1371/journal.pone.0083271
Cruz MP (2012) Vilazodone HCl (Viibryd): a serotonin partial agonist and reuptake inhibitor for the treatment of major depressive disorder. P & T: a peer-reviewed journal for formulary management, 37(1):28–31
Connolly BS, Lang AE (2014) Pharmacological treatment of Parkinson disease: a review. JAMA 311:1670–1683. https://doi.org/10.1001/jama.2014.3654
Conti MM, Meadows SM, Melikhov-sosin M, Lindenbach D, HallmarkJ WDF, Bishop C (2016) Monoamine transporter contributions to l-DOPA effects in hemi-parkinsonian rats. Neuropharm 110:125–134. https://doi.org/10.1016/j.neuropharm.2016.07.025
Conti MM, Ostock CY, Lindenbach D, Goldenberg AA, KamptonDell’isola ER, Bishop C (2014) Effects of prolonged selective serotonin reuptake inhibition on the development and expression of l-DOPA-induced dyskinesia in hemi- parkinsonian rats. Neuropharm 77:1–8. https://doi.org/10.1016/j.neuropharm.2013.09.017
Crosby NJ, Deane KH, Clarke CE (2003) Amantadine for dyskinesia in Parkinson’s disease. Cochrane Database Syst Rev 2:CD003467. https://doi.org/10.1002/14651858.CD003467
Damoiseaux VA, Proost JH, Jiawan VCR, Melgert BN (2014) Sex differences in the pharmacokinetics of antidepressants: influence of female sex hormones and oral contraceptives. Clin Pharmacokinet 53:509–519. https://doi.org/10.1007/s40262-014-0145-2
Dashtipour K, Tafreshi AR, Pahwa R, Lyons KE (2019) Extended-Release Amantadine for Levodopa-Induced Dyskinesia. Expert Rev Neurother 19(4):293–299. https://doi.org/10.1080/14737175.2019.1592677
Dekundy A, Lundblad M, Danysz W, Cenci MA (2007) Modulation of L-DOPA-induced abnormal involuntary movements by clinically tested compounds: further validation of the rat dyskinesia model. Behav Brain Res 179(1):76–89. https://doi.org/10.1016/j.bbr.2007.01.013
De La Fuente-Fernández R, Sossi V, Huang Z, Furtado S, Lu JQ, Calne DB, Stoessl AJ (2004) Levodopa-induced changes in synaptic dopamine levels increase with progression of Parkinson’s disease: implications for dyskinesias. Brain 127(12):2747–2754. https://doi.org/10.1093/brain/awh290
Depoortere R, Johnston TH, Fox SH, Brotchie JM, Newman-Tancredi A (2020) The selective 5-HT1A receptor agonist, NLX-112, exerts anti-dyskinetic effects in MPTP-treated macaques. Parkinsonism Relat Disord 78:151–157. https://doi.org/10.1016/j.parkreldis.2020.08.009
Dupre KB, Eskow KL, Negron G, Bishop C (2007) The differential effects of 5-HT1A receptor stimulation on dopamine receptor-mediated abnormal involuntary movements and rotations in the primed hemiparkinsonian rat. Brain Res 1158(1):135–143. https://doi.org/10.1016/j.brainres.2007.05.005
Dupre KB, Ostock CY, Eskow Jaunarajs KL, Button T, Savage LM, Wolf W, Bishop C (2011) Local modulation of striatal glutamate efflux by serotonin 1A receptor stimulation in dyskinetic, hemiparkinsonian rats. Exp Neurol 229(2):288–299. https://doi.org/10.1016/j.expneurol.2011.02.012
Eskow KL, Dupre KB, Barnum CJ, Dickinson SO, Park JY, Bishop C (2009) The role of the dorsal raphe nucleus in the development, expression, and treatment of L-dopa induced dyskinesia in hemiparkinsonian rats. Synapse 63(7):610–620. https://doi.org/10.1002/syn.20630
Eskow KL, Gupta V, Alam S, Park JY, Bishop C (2007) The partial 5-HT1A agonist buspirone reduces the expression and development of l-DOPA-induced dyskinesia in rats and improves l-DOPA efficacy. Pharmacol Biochem Behav 87(3):306–314. https://doi.org/10.1016/j.pbb.2007.05.002
Fidalgo C, Ko WKD, Tronci E, Li Q, Stancampiano R, Chuan Q, Carta M (2015) Effect of serotonin transporter blockade on L-DOPA-induced dyskinesia in animal models of Parkinson’s disease. Neuroscience 298:389–393. https://doi.org/10.1016/j.neuroscience.2015.04.027
Fieblinger T, Zanetti L, Sebastianutto I, Breger LS, Quintino L, Lockowandt M, Cenci MA (2018) Striatonigral neurons divide into two distinct morphological-physiological phenotypes after chronic L-DOPA treatment in parkinsonian rats. Sci Rep 8(1):1–11. https://doi.org/10.1038/s41598-018-28273-5
Fisher R, Hikima A, Morris R, Jackson MJ, Rose S, Varney MA, Depoortere R, Newman-Tancredi A (2020) The selective 5-HT1A receptor agonist, NLX-112, exerts anti-dyskinetic and anti-parkinsonian-like effects in MPTP-treated marmosets. Neuropharmacology 167:107997. https://doi.org/10.1016/j.neuropharm.2020.107997
Frazer A, Benmansour S (2002) Delayed pharmacological effects of antidepressants. Mol Psychiatry 7:S23–S28. https://doi.org/10.1038/sj.mp.4001015
Fu JF, Klyuzhin I, Liu S, Shahinfard E, Vafai N, McKenzie J, Sossi V (2018) Investigation of serotonergic Parkinson’s disease-related covariance pattern using [11C]-DASB/PET. NeuroImage Clin 19:652–660. https://doi.org/10.1016/j.nicl.2018.05.022
Gérard C, Martres MP, Lefèvre K, Miquel MC, Vergé D, Lanfumey L, Doucet E, Hamon M, el Mestikawy S (1997) Immuno-localization of serotonin 5-HT6 receptor-like material in the rat central nervous system. Brain Res 746:207–219. https://doi.org/10.1016/S0006-8993(96)01224-3
Gérard C, el Mestikawy S, Lebrand C, Adrien J, Ruat M, Traiffort E, Hamon M, Martres MP (1996) Quantitative RTPCR distribution of serotonin 5-HT6 receptor mRNA in the central nervous system of control or 5,7-dihydroxytryptamine-treated rats. Synapse 23:164–173. https://doi.org/10.1002/(SICI)1098-2396(199607)23:3%3c164::AID-SYN5%3e3.0.CO;2-6
Girasole AE, Lum MY, Nathaniel D, Bair-Marshall CJ, Guenthner CJ, Luo L, Kreitzer AC, Nelson AB (2018) A Subpopulation of Striatal Neurons Mediates Levodopa-Induced Dyskinesia. Elselvier 97(4):787–795. https://doi.org/10.1016/j.neuron.2018.01.017
Goetz CG, Damier P, Hicking C, Laska E, Muller T, Olanow CW, Russ H (2007) Sarizotan as a treatment for dyskinesias in Parkinson’s disease: a double-blind placebo- controlled trial. Mov Disord 22(2):179–186. https://doi.org/10.1002/mds.21226
Grégoire L, Samadi P, Graham J, Bédard PJ, Bartoszyk GD, Di Paolo T (2009) Low doses of sarizotan reduce dyskinesias and maintain antiparkinsonian efficacy of L-Dopa in parkinsonian monkeys. Parkinsonism Relat Disord 15(6):445–452. https://doi.org/10.1016/j.parkreldis.2008.11.001
Hamadjida A, Nuara SG, Bédard D, Frouni I, Kwan C, Gourdon JC, Huot P (2018) Nefazodone reduces dyskinesia, but not psychosis-like behaviours, in the parkinsonian marmoset. Naunyn Schmiedebergs Arch Pharmacol 391(12):1339–1345. https://doi.org/10.1007/s00210-0181549-6
Hammerstad JP, Carter J, Nutt JG, Casten GC, Shrotriya RC, Alms DR, Temple D (1986) Buspirone in Parkinson’s Disease. pdf. Clinl Neuropharmacol 9(6):556–560
Hely MA, Morris JG, Reid WG, Trafficante R (2005) Sydney Multicenter Study of Parkinson’s disease: non-L-dopa-responsive problems dominate at 15 years. Mov Disord 20(2):190–199. https://doi.org/10.1002/mds.20324
Hughes ZA, Starr KR, Langmead CJ, Hill M, Bartoszyk GD, Hagan JJ, Middlemiss DN, Dawson LA (2005) Neurochemical evaluation of the novel 5-HT1A receptor partial agonist/serotonin reuptake inhibitor, Vilazodone. Eur J Pharmacol 510:49–57. https://doi.org/10.1016/j.ejphar.2005.01.018
Huot P, Johnston TH, Koprich JB, Winkelmolen L, Fox SH, Brotchie JM (2012) Regulation of cortical and striatal 5-HT 1A receptors in the MPTP-lesioned macaque. Neurobiol Aging 33:9–19. https://doi.org/10.1016/j.neurobiolaging.2010.09.011
Huot P, Johnston TH, Fox SH, Newman-Tancredi A, Brotchie JM (2015) The highly selective 5-HT1A agonist F15599 reduces l-DOPA-induced dyskinesia without compromising anti-parkinsonian benefits in the MPTP-lesioned macaque. Neuropharmacology 97:306–311. https://doi.org/10.1016/j.neuropharm.2015.05.033
Iderberg H, McCreary AC, Varney MA, Kleven MS, Koek W, Bardin L, Depoortère R, Cenci MA, Newman-Tancredi A (2015) NLX-112, a novel 5-HT1A receptor agonist for the treatment of L-DOPA-induced dyskinesia: behavioral and neurochemical profile in rat. Exp Neurol 271:335–350. https://doi.org/10.1016/j.expneurol.2015.05.021
Inden M, Abe M, Minamino H, Takata K, Yoshimoto K, Tooyama I, Kitamura Y (2012) Effect of selective serotonin reuptake inhibitors via 5-HT1A receptors on L-DOPA-induced rotational behavior in a hemiparkinsonian rat model. J Pharmacol Sci 119(1):10–19. https://doi.org/10.1254/jphs.12003fp
Iravani MM, Tayarani-binazir K, Chu WB, Jackson MJ, Jenner P (2006) Primates, the Selective 5-Hydroxytryptamine 1a Agonist ( R ) - ( ϩ ) -8-OHDPAT inhibits levodopa induced Dyskinesia but only with increased motor disability. Pharmacology 319(3):1225–1234. https://doi.org/10.1124/jpet.106.110429.glutamate
Jackson MJ, Al-Barghouthy G, Pearce RK, Smith L, Hagan JJ, Jenner P (2004) Effect of 5-HT1B/D receptor agonist and antagonist administration on motor function in haloperidol and MPTP-treated common marmosets. Pharmacol Biochem Behav 79(3):391–400. https://doi.org/10.1016/j.pbb.2004.07.015
Jenner P (2018) The treatment of levodopa-induced dyskinesias: surfing the serotoninergic wave. Mov Disord 33(11):1670–1672. https://doi.org/10.1002/mds.27525
Kannari K, Shen H, Arai A, Tomiyama M, Baba M (2006) Reuptake of l-DOPA-derived extracellular dopamine in the striatum with dopaminergic denervation via serotonin transporters. Neurosci Lett 402(1–2):62–65. https://doi.org/10.1016/j.neulet.2006.03.059
Kitaichi Y, Inoue T, Nakagawa S, Boku S, Kakuta A, Izumi T, Koyama T (2010) Sertraline increases extracellular levels not only of serotonin, but also of dopamine in the nucleus accumbens and striatum of rats. Eur J Pharmacol 647(1–3):90–96. https://doi.org/10.1016/j.ejphar.2010.08.026
Koyama Y, Kondo M, Shimada S (2017) Building a 5-HT3A Receptor Expression Map in the Mouse Brain. Sci Rep 9(7):42884. https://doi.org/10.1038/srep42884
Kuan WL, Zhao JW, Barker RA (2008) The role of anxiety in the development of levodopa-induced dyskinesias in an animal model of Parkinson’s disease, and the effect of chronic treatment with the selective serotonin reuptake inhibitor citalopram. Psychopharmacology 197(2):279–293. https://doi.org/10.1007/s00213-007-1030-6
Larsen MB, Sonders MS, Mortensen OV, Larson GA, Zahniser NR, Amara SG (2011) Dopamine transport by the serotonin transporter: A Mechanistically distinct mode of substrate translocation. J Neurosci 31(17):6605–6615. https://doi.org/10.1523/JNEUROSCI.0576-11.2011
Lanza K, Bishop C (2018) Serotonergic targets for the treatment of l-DOPA-induced dyskinesia. J Neural Transm 125(8):1203–1216. https://doi.org/10.1007/s00702-0171837-1
LeGates TA, Kvarta MD, Thompson SM (2019) Sex differences in antidepressant efficacy. Neuropsychopharmacol 44:140–154. https://doi.org/10.1038/s41386-018-0156z
Leiser SC, Li Y, Pehrson AL, Dale E, Smagin G, Sanchez C (2015) Serotonergic regulation of prefrontal cortical circuitries involved in cognitive processing: a review of individual 5-ht receptor mechanisms and concerted effects of 5-ht receptors exemplified by the multimodal antidepressant vortioxetine. ACS Chem Neurosci 6:970–986. https://doi.org/10.1021/cn500340j
Lindenbach D, Plaumbo N, Ostock CY, Vilceus N, Conti MM, Bishop C (2015) Side effect profile of 5-HT treatments for Parkinson’s disease and L-DOPA-induced dyskinesia in rats. Br J Pharmacol 172(1):119–130. https://doi.org/10.1111/bph.12894
Marin C, Aguilar E, Rodríguez-Oroz MC, Bartoszyk GD, Obeso JA (2009) Local administration of sarizotan into the subthalamic nucleus attenuates levodopa-induced dyskinesias in 6-OHDA-lesioned rats. Psychopharmacology 204(2):241–250. https://doi.org/10.1007/s00213-008-1452-9
Mazzucchi S, Frosini D, Ripoli A, Nicoletti V, Linsalata G, Bonuccelli U, Ceravolo R (2015) Serotonergic antidepressant drugs and L-dopa-induced dyskinesias in Parkinson’s disease. Acta Neurol Scand 131(3):191–195. https://doi.org/10.1111/ane.12314
McCreary AC, Varney MA, Newman-Tancredi A (2016) The novel 5-HT 1A receptor agonist, NLX-112 reduces l-DOPA-induced abnormal involuntary movements in rat: A chronic administration study with microdialysis measurements. Neuropharmacology 105:651–660. https://doi.org/10.1016/j.neuropharm.2016.01.013
Meadows SM, Chambers NE, Conti MM, Bossert SC, Tasber C, Sheena E, Bishop C (2017) Characterizing the differential roles of striatal 5-HT 1A auto- and hetero-receptors in the reduction of L-DOPA-induced dyskinesia. Exp Neurol 292:168–178. https://doi.org/10.1016/j.expneurol.2017.03.013
Meadows SM, Conti MM, Gross L, Chambers NE, Avnor Y, Ostock CY, Bishop C (2018) Diverse serotonin actions of Vilazodone reduce l-3,4-dihidroxyphenylalanine induced dyskinesia in hemi-parkinsonian rats. Mov Disord 33(11):1740–1749. https://doi.org/10.1002/mds.100
Mørk A, Montezinho LP, Miller S, Trippodi-Murphy C, Plath N, Li Y, Gulinello M, Sanchez C (2013) Vortioxetine (Lu AA21004), a novel multimodal antidepressant, enhances memory in rats. Pharmacol Biochem Behav 105:41–50. https://doi.org/10.1016/j.pbb.2013.01.019
Morin N, Morissette M, Grégoire L, Rajput A, Rajput AH, Di Paolo T (2015) Contribution of brain serotonin subtype 1B receptors in levodopa-induced motor complications. Neuropharmacology 99:356–368. https://doi.org/10.1016/j.neuropharm.2015.08.002
Navailles S, Bioulac B, Gross C, De Deurwaerdère P (2010) Serotonergic neurons mediate ectopic release of dopamine induced by L-DOPA in a rat model of Parkinson’s disease. Neurobiol Dis 38(1):136–143. https://doi.org/10.1016/j.nbd.2010.01.012
Ohno Y, Shimizu S, Tokudome K, Kunisawa N, Sasa M (2015) New insight into the therapeutic role of the serotonergic system in Parkinsons disease. Prog Neurobiol 134:104–121. https://doi.org/10.1016/j.pneurobio.2015.09.005
Okada M, Okubo R, Fukuyama K (2019) Vortioxetine subchronically activates serotonergic transmission via desensitization of serotonin 5-HT1A receptor with 5-HT3 receptor inhibition in rats. Int J Mol Sci 20(24):6235. https://doi.org/10.3390/ijms20246235
Ostock CY, Dupre KB, Eskow Jaunarajs KL, Walters H, George J, Krolewski D, Bishop C (2011) Role of the primary motor cortex in l-DOPA-induced dyskinesia and its modulation by 5-HT1A receptor stimulation. Neuropharmacology 61(4):753–760. https://doi.org/10.1016/j.neuropharm.2011.05.021
Owen RT (2011) Vilazodone: a new treatment option for major depressive disorder. Drugs of today (Barcelona, Spain: 1998) 47(7):531–537. https://doi.org/10.1358/dot.2011.47.7.1622076
Padovan-Neto FE, Patterson S, Voelkner NMF, Altwal F, Beverley JA, West AR, Steiner H (2020) Selective regulation of 5-HT1B serotonin receptor expression in the striatum by dopamine depletion and repeated L-DOPA treatment: relationship to L DOPA-induced Dyskinesias. Mol Neurobiol 57(2):736–751. https://doi.org/10.1007/s12035-019-01739-x
Page ME, Cryan JF, Sullivan A et al (2015) Behavioral and neurochemical effects of 5-{4-[4- (5 cyano-3-indolyl)-butyl)-butyl]-1-piperazinyl}- bunzofuran-2-carboxamide (EMD 68843): a combined selective inhibitor of serotonin reuptake and 5-hydroxytryptamine1A receptor partial agonist. Neuropharm 302(3):1220–1227. https://doi.org/10.1124/jpet.102.034280
Paolone G, Brugnoli A, Arcuri L, Mercatelli D, Morari M (2015) Eltoprazine prevents levodopa-induced dyskinesias by reducing striatal glutamate and direct pathway activity. Mov Disord 30(13):1728–1738. https://doi.org/10.1002/mds.26326
Parker JG, Marshall JD, Ahanonu B, Wu Y, Kim TH, Grewe BF, Zhang Y, Li JZ, Ding JB, Ehlers MD, Schnizer MJ (2018) Diametric neural ensemble dynamics in parkinsonian and dyskinetic states. Nature 557:177–182. https://doi.org/10.1038/s41586-018-0090-6
Paxinos G, Watson W (1998) The rat brain in stereotaxic coordinates, 4th edn. Academic Press, San Diego, pp 1–456
Plenge P, Yang D, Salomon K, Laursen L, Kalenderoglou IE, Newman AH, Loland CJ (2021) The antidepressant drug vilazodone is an allosteric inhibitor of the serotonin transporter. Nat Commun 12(1):1–12. https://doi.org/10.2210/pdb7LWD/pdb
Politis M, Wu K, Loane C, Brooks DJ, Kiferle L, Turkheimer FE, Piccini P (2014) Serotonergic mechanisms responsible for levodopa-induced dyskinesias in Parkinson’s disease patients. J Clin Invest 124(3):1340–1349. https://doi.org/10.1172/JCI71640
Porras G, De Deurwaerdere P, Moison D, Spampinato U (2003) Conditional involvement of striatal serotonin3 receptors in the Control of In Vivo dopamine outflow in the rat striatum. Eur J Neurosci 17:771–781. https://doi.org/10.1046/j.1460-9568.2003.02512.x
Ran Y, Jin Z, Chen X, Zhao N, Fang X, Zhang L, Li Y (2018) Hypidone Hydrochloride (YL-0919) Produces a fast-onset reversal of the behavioral and synaptic deficits caused by chronic stress exposure. Frontiers in Cellular Neuroscience, 12. https://doi.org/10.3389/fncel.2018.00395
Roussakis A, Politis M, Towey D and Piccini P (2016) Serotonin-to-dopamine transporter ratios in Parkinson disease: Relevance for dyskinesias. Neurology. 86(12):1152-8. https://doi.org/10.1212/WNL0000000000002494
Rylander D, Parent M, O-Sullivan SS, Dovero S, Lees AJ, Bezard E, Cenci MA (2010) Maladaptive plasticity of serotonin axon terminals in levodopa-induced dyskinesia. Ann Neurol 68(5):619–628. https://doi.org/10.1002/ana.22097
Saarelainen T, Hendolin P, Lucas G, Koponen E, Sairanen M, MacDonald E, Agerman K, Haapasalo A, Nawa H, Aloyz R, Ernfors P, Castren E (2003) Activation of the TrkB neurotrophin receptor is induced by antidepressant drugs and is required for antidepressant-induced behavioral effects. J Neurosci 23(1):349–357. https://doi.org/10.1523/JNEUROSCI.23-01-00349.2003
Schneider RB, Auinger P, Tarolli CG, Iourinets J, Gil-Diaz MC, Richard IH (2020) A trial of buspirone for anxiety in Parkinson’s disease: safety and tolerability. Elselvier 81:69–74. https://doi.org/10.1016/j.parkreldis.2020.10.020
Schrag A, Quinn N (2000) Dyskinesias and motor fluctuations in parkinson’s disease. A community based study. Brain 123(Pt 11):2297–2305. https://doi.org/10.1093/brain/123.11.2297
Sellnow RC, Newman JH, Chambers N, West AR, Steece-Collier K, Sandoval IM, Manfredsson FP (2019) Regulation of dopamine neurotransmission from serotonergic neurons by ectopic expression of the dopamine D2 autoreceptor blocks levodopa-induced dyskinesia. Acta Neuropathol Commun 7(1):8. https://doi.org/10.1186/s40478-018-0653-7
Smith GS, Ma Y, Dhawan V, Chaly T, Eidelberg D (2009) Selective serotonin reuptake inhibitor (SSRI) modulation of striatal dopamine measured with [11C]-raclopride and positron emission tomography. Synapse (New York, N.Y.) 63(1):1–6. https://doi.org/10.1002/syn.20574
Strecker K, Wegner F, Hesse S, Becker GA, Patt M, Meyer PM, Sabri O (2011) Preserved serotonin transporter binding in de novo Parkinson’s disease: negative correlation with the dopamine transporter. J Neurol 258(1):19–26. https://doi.org/10.1007/s00415-010-5666-5
Suh DC, Pahwa R, Mallya U (2012) Treatment patterns and associated costs with Parkinson’s disease levodopa induced dyskinesia. J Neurol Sci 319(1–2):24-31.s008. https://doi.org/10.1016/j.jns.2012.05.029
Svenningsson P, Rosenblad C, Arvidsson KE, Wictorin K, Keywood C, Shankar B, Widner H (2015) Eltoprazine counteracts l-DOPAinduced dyskinesias in Parkinson’s disease: a dose finding study. Brain. https://doi.org/10.1093/brain/awu409.10.1093/brain/awu409
Tanaka H, Kannari K, Maeda T, Tomiyama M, Suda T, Matsunaga M (1999) Role of serotonergic neurons in L-DOPA-derived extracellular dopamine in the striatum of 6-OHDA-lesioned rats. NeuroReport 10:631–634. https://doi.org/10.1097/00001756-199902250-00034
Ward RP, Hamblin MW, Lachowicz JE, Hoffman BJ, Sibley DR, Dorsa DM (1995) Localization of serotonin subtype 6 receptor messenger RNA in the rat brain by in situ hybridization histochemistry. Neuroscience 64:1105–1111. https://doi.org/10.1016/0306-4522(94)00439-C
Yamada J, Sugimoto Y, Horisaka K (1988) The behavioural effects of 8-hydroxy-2-(di-n propylamino)tetralin (8-OH-DPAT) in mice. Eur J Pharmacol 154:299–304. https://doi.org/10.1016/0014-2999(88)90205-1
Zhang LM, Wang XY, Zhao N, Wang YL, Hu XX, Ran YH et al (2017) Neurochemical and behavioural effects of hypidone hydrochloride (YL-0919): a novel combined selective 5-HT reuptake inhibitor and partial 5-HT1A agonist. J Pharmacol 174:769–780. https://doi.org/10.1111/bph.13675
Zhang X, Andren PE, Greengard P, Svenningsson P (2008) Evidence for a role of the 5HT1B receptor and its adaptor protein, p11, in L-DOPA treatment of an animal model of Parkinsonism. Proc Natl Acad Sci USA 105(6):2163–2168. https://doi.org/10.1073/pnas.0711839105
Zoldan J, Friedberg G, Livneh M, Melamed E (1995) Psychosis in advanced Parkinson’s disease: treatment with ondansetron, a 5-HT3 receptor antagonist. Neurology 45(7):1305–1308. https://doi.org/10.1212/wnl.45.7.1305
Funding
State University of New York Technology Accelerator Fund
Center of Development and Behavioral Neuroscience
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors have no conflicts of interest to declare.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlights
• The serotonin system has an important role in L-DOPA’s effects.
• Vilazodone and Vortioxetine attenuate dyskinesia in rat models of Parkinson’s disease.
• Targeting 5-HT1A receptors and 5-HT transporters maintains L-DOPA efficacy.
Rights and permissions
About this article
Cite this article
Smith, S., Sergio, J., Coyle, M. et al. The effects of Vilazodone, YL-0919 and Vortioxetine in hemiparkinsonian rats. Psychopharmacology 239, 2119–2132 (2022). https://doi.org/10.1007/s00213-022-06078-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-022-06078-9