Abstract
Rationale
Agonist-based pharmacologic intervention is an accepted approach in treatment of opioid and tobacco use disorders.
Objectives
We conducted a systematic review and meta-analysis to evaluate usefulness of an agonist approach as treatment of (psycho)stimulant use disorder (PSUD).
Methods
We reviewed PubMed/Medline, LILACS, and ClinicalTrials.gov databases searching for randomized, double-blind, placebo-controlled, parallel-design studies evaluating outcomes of individuals treated for cocaine- or amphetamine-type substance use disorder. We combined results of all trials that included the following prescription psychostimulants (PPs): modafinil, methylphenidate, or amphetamines (mixed amphetamine salts, lisdexamphetamine, and dextroamphetamine). The combined sample consisted of 2889 patients. Outcomes of interest included the following: drug abstinence (defined as 2–3 weeks of sustained abstinence and the average maximum days of consecutive abstinence), percentage of drug-negative urine tests across trial, and retention in treatment. We conducted random-effects meta-analyses and assessed quality of evidence using the GRADE system.
Results
Thirty-eight trials were included. Treatment with PPs increases rates of sustained abstinence [risk ratio (RR) = 1.45, 95% confidence interval (CI) = (1.10, 1.92)] and duration of abstinence [mean difference (MD) = 3.34, 95% CI = (1.06, 5.62)] in patients with PSUD, particularly those with cocaine use disorder (very low-quality evidence). Prescription amphetamines were particularly efficacious in promoting sustained abstinence in patients with cocaine use disorder [RR = 2.44, 95% CI = (1.66, 3.58)], and higher doses of PPs were particularly efficacious for treatment of cocaine use disorder [RR = 1.95, 95% CI = (1.38, 2.77)] (moderate-quality evidence). Treatment with prescription amphetamines also yielded more cocaine-negative urines [MD = 8.37%, 95% CI = (3.75, 12.98)]. There was no effect of PPs on the retention in treatment.
Conclusion
Prescription psychostimulants, particularly prescription amphetamines given in robust doses, have a clinically significant beneficial effect to promote abstinence in the treatment of individuals with PSUD, specifically the population with cocaine use disorder.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Global use of cocaine increased two-fold over the 5 years leading to 2017 reaching all-time high of an estimated 18 million that used cocaine in the past year, with an accelerating trend observed in Europe, North America, some South American countries, and Australia. Moreover, cocaine seizures reported in Asia and West Africa suggest that its use might be increasing in these regions as well (United Nations Office on Drugs and Crime 2019). Global market for amphetamine and methamphetamine continues to expand, and in 2017, an estimated 29 million used amphetamines in the past year, with an increasing trend seen in the United States and in East and South-East Asia (United Nations Office on Drugs and Crime 2019). A significant number of individuals who use stimulants will develop a (psycho) stimulant use disorder (PSUD), which includes a cocaine use disorder (CUD) and an amphetamine-type use disorder (AUD), which are among the most prevalent drug-related conditions around the world with highly burdensome health and social consequences (United Nations Office on Drugs and Crime 2019). The prevalence of CUD and AUD has raised globally at 39.7% and 22.5%, respectively, from 1990 to 2016. CUD accounts for 1153.6 thousand disability-adjusted life years (DALYs), a disease burden measure that comprises years of life lost (YLLs) and years of life lived with disability (YLDs), while AUD accounts for 881.4 thousand DALYs (Degenhardt et al. 2016). Only alcohol and opioids pose heavier burdens than CUD and AUD. Stimulant drugs have considerable potential of yielding use disorders among their users, with 16.7% of those with any lifetime cocaine use developing a use disorder. This proportion is of 11.2% for amphetamines, comparable to 15.4% for alcohol and 23.1% for heroin (Anthony et al. 1997). More recent publications also found a lifetime prevalence of PSUD of 1.7% (Grant et al. 2016) and that 15.6% of cocaine abusers transition to dependence at any point of their lives (Florez-Salamanca et al. 2013).
Despite the alarming public health impact of PSUD, the proportion of individuals with PSUD who are receiving treatment is extremely low (United Nations Office on Drugs and Crime 2019), with only 20% of patients with cocaine or amphetamine use disorder receiving specialty treatment in 2018 as patients with CUD and AUD and similarly low rates reported in patients with opioid use disorder (OUD) though rates of OUD treatment have been increasing in the past few years (Substance Abuse Mental Health Services Administration 2019). One of the reasons for such low treatment rates is the absence of the medication-based model of PSUD treatment. This is in contrast to much higher treatment rates among those with opioid use disorder, where medications are an essential treatment component (Schuckit 2016). In the absence of an approved and well-accepted pharmacological intervention to treat PSUD, psychosocial interventions remain the primary model of treatment (De Giorgi et al. 2018; Lee and Rawson 2008; Minozzi et al. 2016).
The most accepted pharmacological intervention for substance use disorders involves treatment with agonist-like medications, the approach known as a replacement or substitution therapy (Darke and Farrell 2016). Agonist-based treatment has been successfully implemented in treatment of opioid use disorder (Mattick et al. 2009) and tobacco use disorder (Hartmann-Boyce et al. 2014). A parallel approach has for long been regarded as a promising approach for treatment of PSUD (Shearer et al. 2002), and several medications were proposed as putative “stimulant agonists” (Amato et al. 2011; Castells et al. 2016; Rush and Stoops 2012; Stoops and Rush 2013).
An “agonist” medication would have a similar pharmacologic and behavioral effect as the drug of abuse, providing relief of craving and other symptoms of acute and protracted withdrawal, which are main factors responsible for the maintenance of drug use and for relapse following periods of abstinence (Darke and Farrell 2016). Another desired feature of an agonist medication is that it may function as a “blocker” in case of the use of the primary drug and therefore diminish euphoric effects and prevent further escalation of use (Shearer 2008). At the same time, for a medication to be acceptable for agonist-based treatment, it will need to have an acceptable safety profile and be feasible for clinical use (Darke and Farrell 2016). Medication taken orally with slow onset of action and a long elimination half-life will have less euphoric and discontinuation subjective effects reducing the risk of abuse, and stable blood concentrations will provide “pharmacological stability” (Darke and Farrell 2016). Moreover, the agonist medication should have few acute side effects and no behavioral organ toxicity in clinically used doses and therefore be acceptable for chronic administration. Preferably, it will have mildly positive subjective effects that will promote medication adherence and have acceptable safety profile when combined with the primary or other drugs of abuse (Darke and Farrell 2016). Effective treatment with agonist medication will facilitate initial abstinence with resulting improved adherence to treatment, as high rates of treatment dropout are one of the main challenges in working with this population. Improved treatment engagement will allow patients to benefit from cognitive and behavioral therapies offered in the treatment program to prevent relapse and extend benefits of drug abstinence, all of which would be difficult in patients who are actively using stimulants. Moreover, individuals receiving agonists are likely to become interested in and access other medical and social interventions, as well as other therapeutic services offered at the program, such as psychoeducation and harm-reduction services (Shearer et al. 2002).
All of the stimulants acutely increase brain levels of dopamine and noradrenaline, producing stimulating and pleasurable euphoric effects, and with chronic use produce long-lasting changes in brain circuits (Kalivas and O'Brien 2008). However, individuals with PSUD who use stimulants chronically have altered functioning of the dopaminergic system, which may be responsible for the clinical signs and symptoms observed in those individuals, such as low energy, low mood and anhedonia, increased impulsivity, as well as impaired cognition and decision making (London et al. 2015; Sabrini et al. 2019). Medications with diverse pharmacological effects increasing the dopaminergic activity have been proposed as candidates for agonist-type treatment of PSUD (Rush and Stoops 2012) and have been evaluated in controlled clinical trials over the past 30 years. An examination of this evidence appears to show that among the most effective of all tested dopaminergic medications are the prescription psychostimulants (PPs), such as amphetamine salts or methylphenidate. PPs have accepted medical use and favorable safety profile and may therefore be good candidate medications for PSUD agonist treatment (Goldstein and Volkow 2011; Goldstein et al. 2010).
Treatment with PPs should be implemented cautiously due to the potential for euphoric effects and the risk of misuse and diversion (Darke and Farrell 2016). Using extended-release preparations suitable for once-daily administration and administering medication under direct observation, similarly to treatment with opioid agonist methadone, can reduce potential of abuse (Nuijten et al. 2016). Toxicity of PPs when given chronically should also be considered (Darke and Farrell 2016) especially as individuals chronically using high doses of stimulants are at increased risk of cardiovascular disorders (Callaghan et al. 2018) and psychotic symptoms (Fiorentini et al. 2011). However, these medications are widely used for the treatment of attention-deficit hyperactivity disorder (ADHD) and have overall good cardiovascular and psychiatric safety profile when used in healthy children and adults (Cooper et al. 2011; Habel et al. 2011).
Many individuals with PSUD have other co-occurring psychiatric and substance use disorders, including ADHD that occurs in 5%–31% of adults seeking treatment for substance use disorders (van de Glind et al. 2014) and major depression which may affect treatment outcomes (Hellem et al. 2015; Rounsaville 2004; Rounsaville et al. 1991). Moreover, patients seeking treatment for PSUD often present with dependence on other drugs, notably opioids (Marsden et al. 2009). These co-occurring conditions may indicate greater severity of the PSUD, and those individuals may have worse health and treatment outcomes, and such comorbidities may modulate the impact of medications.
Cochrane reviews with meta-analyses assessing the efficacy of PPs on CUDs (Castells et al. 2016) and AUDs (Perez-Mana et al. 2013) were published in 2016 and 2013, respectively. Both publications pooled measures of effect from RCTs comparing PPs to placebo on sustained abstinence, drug use across the study period, and retention to treatment. In those analyses, PPs, especially prescription amphetamines, were found to significantly increase rates of sustained abstinence in patients with CUDs (Castells et al. 2016), but the quality of the evidence was very low due to heterogeneity and inconsistency of the estimates with a large number of medications included. However, no significant effect was found in patients with AUD on measures of drug use, sustained abstinence, or retention in treatment, though attrition for both medication and placebo was high (Perez-Mana et al. 2013). More recently, new high-quality trials with robust sample sizes, sound methodology, and up-to-date designs (e.g., monitored intake, extended-release formulations, and higher dosages) have been published, and therefore, a new meta-analysis is warranted.
The aim of this study was to systematically review trials testing selected PPs as treatment for patients with cocaine or amphetamine-type substance use disorder (PSUD) and pool data with meta-analyses. We included studies that used either prescription amphetamines, methylphenidate, or modafinil. We summarized the evidence from the following outcomes: (a) sustained (2–3 weeks) drug abstinence, (b) percentage of drug-negative urine tests across trial, (c) maximum days of continuous abstinence, and (d) retention in treatment. When possible, we carried out subgroup analyses per drug of abuse, medication used, ADHD status, and comorbid opioid use disorder (OUD). We performed risk of bias and quality assessments and assessed the quality of the evidence using the GRADE system.
Methods
Medication selection
In contrast to previous systematic reviews on this topic (Castells et al. 2016; Perez-Mana et al. 2013), we restricted this analysis to trials with medications that are most analogous to cocaine or amphetamine-type substances, with similar behavioral effects and therefore most “potent” pharmacologically to be candidates for PSUD “agonist-based” treatment. This includes amphetamine isomers (dexamphetamine and methamphetamine), which are monoamine release enhancers, and methylphenidate, which is a monoamine transport blocker (Rush and Stoops 2012). Furthermore, we included modafinil, which also blocks dopamine transporter in doses used clinically exerting effect comparable to lower doses of methylphenidate (Kim et al. 2014; Madras et al. 2006; Volkow et al. 2009) and has a behavioral profile typical of psychostimulants, such as cocaine (Andersen et al. 2010). Despite these effects, modafinil generally has low abuse liability (Jasinski 2000; Jerry et al. 2016), and this combination of behavioral and pharmacological effects as a psychostimulant with limited abuse potential makes modafinil a worthwhile replacement drug candidate. All of the selected medications have similar behavioral effects as abused stimulants (Rush and Baker 2001) and are therefore on the list of controlled substances. This is in contrast to bupropion, another medication that binds to dopamine transporter but has lower receptor occupancy than modafinil or methylphenidate (Griffith et al. 1983; Learned-Coughlin et al. 2003; Meyer et al. 2002), has lower abuse liability (Griffith et al. 1983), and is not a controlled substance, and was therefore not included in this review.
We have also included in the analysis two publications that evaluated treatment with mixed amphetamine salts combined with topiramate (Levin et al. 2020; Mariani et al. 2012). Topiramate was found to have a positive effect on abstinence from cocaine (Singh et al. 2016), and therefore, it is possible that it had an added benefit; thus, we also evaluated the overall effect with these two studies excluded.
Search strategy and selection criteria
This review and meta-analysis was conducted following a pre-established protocol registered on PROSPERO under the number CRD42019129653 and following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines (Moher et al. 2009). We searched all publications in the following databases for bibliography: MEDLINE, PubMed, the Cochrane Library (Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials and Cochrane Methodology Register), Web of Science, and ClinicalTrials.gov. Also, the trial’s references were examined for additional references. No language restriction was used. Publications published up to September 2019 were included.
Our initial search strategy in PubMed/Medline was (“Prescription Psychostimulants” or modafinil or methylphenidate or dextroamphetamine or d-amphetamine or amphetamine or lisdexamphetamine or “mixed amphetamine salts”) and (cocaine or methamphetamine or stimulants). This search strategy was adapted for other databases.
We included randomized, parallel-grouped, double-blind, and placebo-controlled clinical treatment trials that used a PP as the pharmacological intervention. All trials included in this review were conducted in outpatient settings and lasted from 8 to 26 weeks. Non-treatment studies, such as human behavioral pharmacology studies, were not included because of differences in studied population and limited generalizability to clinical population.
RevMan 5 (The Nordic Cochrane Centre 2014) software was used to obtain pooled measures of effect as well as graphic displays of the meta-analytic illustrations. We used Cochrane’s Risk of Bias Assessment tool, included in RevMan 5, to generate methodological quality graphs and summaries. We used the GRADE (Grading of Recommendations Assessment, Development, and Evaluation) approach (Balshem et al. 2011), with help of the GRADEpro software (McMaster University (developed by Evidence Prime 2015) to assess the quality of evidence. A summary of findings (SoF) table is provided, and results are described according to GRADE judgment.
Data extraction and quality assessment
The initial plan for the analysis was developed by AB and GG and finalized with input from all authors. Titles or abstracts of publications obtained with the search strategy or from references list were screened independently by VST and FBA. Full texts were further analyzed by VST and FBA, and final decision about study inclusion included AB and TMF. A standardized form was applied to data extracted from the included publications to assess study quality and evidence synthesis. Information on this form included the following: substance of abuse, presence of comorbid substance use disorders, presence of comorbid mental health disorders, medication tested (with maximum dosages), follow-up period, outcome effect measures, and information about risk of bias. VST and FBA assessed the risk of bias of the included studies separately with the Cochrane tool (Higgins et al. 2011). Any discrepancies were resolved via a discussion with other authors until reaching a consensus. Data were extracted directly from each trial’s published results and study protocols, when available. If data for the outcomes of interest were not published or inserted in the protocols, authors were contacted or we used data included in the published Cochrane reviews (Castells et al. 2016; Perez-Mana et al. 2012, 2013).
Outcomes
We selected sustained stimulant abstinence as the primary outcome. Abstinence, particularly at the end of treatment, is an outcome strongly related to cocaine use during follow-up where it outperforms other measured of drug use, such as percent drug-negative urine screens (Carroll et al. 2014; Miguel et al. 2019), though there are also benefits to sustained low-level use during treatment on functioning following treatment (Roos et al. 2019b). Although most of the publications included in the review used a standardized measure of 3 weeks of consecutive abstinence at the end of the study, some publications used 2 weeks (Levin et al. 2007) or reported sustained abstinence at any time point throughout the trial period (Kampman et al. 2015). All studies except for Nuijten et al. (2016) used objective urine toxicology tests to confirm the abstinence, either alone or combined with self-report.
As for quantitative measures of abstinence, we measured and pooled percentage of drug-negative urine tests per group throughout trials and maximum days of sustained abstinence, using means and standard deviations to obtain a pooled mean difference. We chose mean difference over standardized mean difference because all studies included assessed the referred outcome using the same unit (percentage of drug-negative urine tests and maximum number of days of continuous abstinence). As a secondary outcome, we also assessed retention to treatment and compared the number of patients who finished the study in treatment and control groups. We decided not to include safety outcomes as earlier reviews found no medication and placebo differences in dropouts due to any adverse events, cardiovascular events, and serious adverse events (Castells et al. 2016; Perez-Mana et al. 2013), and the additional studies included in the present review did not report differences in such outcomes. Funnel plots for the three outcomes were not suggestive of publication bias and are available in the Appendix.
Statistical analysis
For the included studies, we calculated summary measures of intervention efficacy providing risk ratios for dichotomous outcomes (sustained stimulants abstinence and retention in treatment) and mean differences for the continuous outcome (percentage of drug-negative urine tests across trial and maximum days of consecutive abstinence).
For dichotomous outcomes, we selected risk ratios (RR) over risk differences (RD) since relative measures are normally more consistent among different studies than absolute measures (Deeks 2002; Engels et al. 2000). In addition, RR satisfy the following three criteria for summary statistics choice in meta-analyses: consistency, mathematical properties required for a proper meta-analysis, and ease of interpretation (Deeks 2002). Finally, RR are easier to interpret than odds ratios because odds ratios are frequently interpreted as if they were risk ratios, which inappropriately overestimates measures of effects (Viera 2008).
When trials used multiple treatment groups, we merged treatment groups into one when these groups used different doses of the same medication, as recommended by the Cochrane manual (Higgins and Green 2011). One study had the following three treatment groups: modafinil, dexamphetamine, and modafinil + dexamphetamine (Schmitz et al. 2012). In this case, we excluded the modafinil + dexamphetamine group from our comparison and included the other two treatment groups as separate analyses (using the same placebo group), as done previously (Castells et al. 2016).
For the percentage of drug-negative urine tests across trial and maximum days of consecutive abstinence outcomes, we used mean differences (MDs) as all trials provided the same unit (% of drug-negative urine tests and days). Trials differed on methods to impute missing data, but most of them imputed missing as positive. RevMan 5 uses the definition of SMD known as Hedges’ g, which is adjusted for possible bias caused by small sample sizes. If means and standard deviations were not reported, we contacted the study authors to obtain these and/or used other statistics to calculate the effect sizes according to the procedures implemented in our meta-analysis software. When necessary, we performed transformations on measures of mean spread to harmonize the results between trials.
If we were not able to obtain the desired data directly from the authors, we then used secondary data obtained from authors by the already published Cochrane meta-analyses cited before (Castells et al. 2016; Perez-Mana et al. 2013). In studies that compared individuals under different doses of the same medication as separate study groups, we merged sample sizes and calculated pooled standard deviations. When publications used different PPs as distinct study groups, we included that publication twice, as if each drug versus placebo comparison represented a single study.
We pooled studies comparing the same types of intervention and control and using the same outcome measure using random-effects models for meta-analysis to account for heterogeneity among the treatment effects of different trials (Borenstein and Higgins 2013). Our a priori tolerated alpha level for effect measures was 0.05. Statistical heterogeneity was assessed using Chi square and I2 statistics. An I2 value greater than 50% was regarded as indicative of substantial heterogeneity (Higgins and Green 2011). When dichotomous outcome data were missing, we assumed that patients who dropped out after randomization had a negative outcome. Missing continuous outcome data were analyzed on an endpoint basis, including only participants with a final assessment, as reported by the original study authors.
We also calculated the number needed to treat (NNT) from the measures of effect of the outcomes assessed in our meta-analysis. For risk ratios obtained from dichotomous variables, the computation of the NNT proceeds as follows: \( NNT=\left|\frac{1}{ACR\times \left(1- RR\right)}\right| \), where RR is the risk ratio for each outcome and ACR is the assumed control risk (ACR). There are many ways to set this parameter. We used the approach that divides the number of positive events in the control (placebo) group divided by the total number of events (Higgins and Green 2011).
Quality of evidence
Quality of evidence was determined using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach (Balshem et al. 2011). “Quality” is defined as a measure of confidence in the effect estimate provided. Evidence is rated as of high, moderate, low, or very low quality. A quality rating of “high” means that it is very likely that the true effect lies close to the estimate, while “very low” means that the true effect is likely to be different from the estimated effect. Randomized trials begin with a quality rating of high, and observational studies begin with a quality rating of low. These ratings can be downgraded based on the following five criteria: risk of bias in the included studies; inconsistency in results; indirectness of evidence; imprecision of effect estimates; and risk of publication bias. However, ratings can be upgraded if the effect size is large, there is evidence of a dose–response effect, or all plausible confounding is controlled for.
Subgroup analyses
We pre-specified subgroup analysis per drug of abuse (cocaine and methamphetamines) providing sensitivity analysis for results overall and for cocaine use disorder when removing trials with add-on topiramate; treatment drug (prescription amphetamines, modafinil, and methylphenidate); and comorbid OUD and attention deficit hyperactivity disorder (ADHD) status, where prescription psychostimulants are notably effective (De Crescenzo et al. 2017). We considered that these factors could partially explain heterogeneity between trials and that the subpopulations specified could respond differently to treatment (Oxman and Guyatt 1992).
In addition, we defined two dose categories for PPs; low and high. We used maximum doses currently approved by the FDA (60 mg/day for prescription amphetamines, 400 mg/day for modafinil, and 60 mg/day for methylphenidate) as the threshold for separating low (below that limit) vs. high doses. We hypothesize that patients with PSUD may be cross-tolerant to PPs and may thus require higher doses and more potent agents to achieve therapeutic response. To explore whether there is a dose–response effect, we conducted a subgroup analysis for the primary outcome of sustained abstinence by the dose. Finally, we performed sensitivity analyses to (a) exclude trials with immediate-release PPs to evaluate its impact on sustained abstinence and (b) elucidate whether the presence of contingency management (CM) (either abstinence or compliance-targeted) changed the effect of PPs on retention to treatment.
Risk of bias
We assessed the validity of the included studies using criteria from the Risk of Bias Assessment tool, developed by the Cochrane Collaboration (Higgins and Green 2011). The tool analyzes risk of bias by classifying it in the following six different domains: generation of allocation sequence, concealment of treatment allocation, blinding of patients and personnel, blinding of outcome assessors, data incompleteness, selective reporting, and other sources of bias.
The risk of bias for each specific domain is assessed either as “low risk,” “unclear risk,” or “high risk.” We assumed that all of the included trials had unclear risk of bias from blinding of patients and personnel since study medications had behavioral effects that could be noticed by both patients and clinicians. Risk of bias graph and summary with author’s judgments for each trial are available in the Appendix.
Results
Study selection
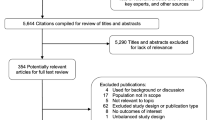
Of the 164 abstracts retrieved from the initial search, 21 studies were included in the full-text review stage. After screening of reference lists from included original publications and reviews, 31 additional studies were added to the full-text reading stage (Fig. 1). At this initial stage, we excluded studies that did not include outcomes of interest or did not meet methodological requirements. A total of 16 studies were excluded after full-text review. Initial discrepancies at the abstract and full-text review stages were later resolved by consensus of study authors.
Thirty-eight RCTs were included in the final analysis with 26 trials conducted in patients with cocaine use disorder (CUD) and 12 in patients with amphetamine-type use disorder (AUD). Eighteen trials used as an outcome 3-week sustained abstinence and one trial assessed 2-week sustained abstinence. Out of those, seven trials evaluated prescription amphetamines, eight evaluated modafinil, and four evaluated methylphenidate. Five trials included patients with comorbid substance use disorders, and four trials included patients with ADHD.
Characteristics of all trials included are described in Table 1.
Effect of prescription psychostimulants on abstinence: overall and in patients with CUD vs AUD
We found an overall significant benefit of PPs when compared to placebo on promoting 2–3 weeks of sustained abstinence (risk ratio [RR] = 1.45, 95% confidence interval [CI] (1.10, 1.92), I2 = 37%); NNT = 16, 95% CI (8, 70) (Fig. 2). When analyzing subgroups per drug of abuse (CUD vs. AUD), this benefit is dragged away from the null by CUD studies. The effect in CUD studies is not only statistically significant but also clinically meaningful considering both confidence interval bounds (RR = 1.70, 95% CI (1.26, 2.31), I2 = 24%); NNT = 12, 95% CI (7, 32). No benefit is shown for AUD studies (RR = 0.89, 95% CI (0.62, 1.27), I2 = 0%).
We performed sensitivity analysis to evaluate whether the benefit of PPs for PSUDs remained when removing two trials that administered topiramate as an add-on medication, both for the treatment of CUDs and conducted by the same research team (Levin et al. 2020; Mariani et al. 2012). The overall effect of PPs for PSUDs remained statistically significant (RR = 1.34, 95% CI (1.01, 1.79), I2 = 34%); NNT = 20, 95% CI (9, 660). The effect of PPs for CUDs also remained statistically significant (RR = 1.59, 95% CI (1.14, 2.23), I2 = 26%); NNT = 14, 95% CI (7, 58), compared to RR = 1.70, 95% CI (1.26, 2.31), I2 = 24%); NNT = 12, 95% CI (7, 32) when the studies were included. See the Appendix for details.
We conducted an additional analysis of studies that reported abstinence in the final 3 weeks, which is an outcome measure adopted in the recent trials, and four trials were included (Dackis et al. 2012; Kampman et al. 2015; Levin et al. 2015b; Levin et al. 2020). We found a significant effect of PP abstinence with a very high RR (RR = 3.01, 95% CI (1.58, 5.75), I2 = 0%). See the Appendix for details.
We performed sensitivity analysis excluding a trial with immediate-release methylphenidate for CUD (Dursteler-MacFarland et al. 2013) from the overall and drug-specific analyses. The overall effect of PPs for PSUD remained statistically significant (RR = 1.47, 95% CI (1.10, 1.96), I2 = 41%); NNT = 18, 95% CI (9, 81). The effect of PPs for CUDs also remained statistically significant (RR = 1.74, 95% CI (1.27, 2.39), I2 = 28%); NNT = 11, 95% CI (6, 30).
Effect by the medication type
A subgroup analysis by medication shows a clinically and statistically significant effect for prescription amphetamines (see Fig. 3), when compared to placebo (RR = 2.44, 95% CI (1.66, 3.58), I2 = 0%); NNT = 7, 95% CI (4, 14). There was no effect for modafinil (RR = 1.22, 95% CI (0.83, 1.77), I2 = 29%) or methylphenidate (RR = 0.90, 95% CI (0.60, 1.37), I2 = 0%).
The effect of co-occurring disorders
To assess whether patients with co-occurring ADHD or OUD had a different response to PPs, we conducted separate analyses for trials where patients had a co-occurring disorder vs. those that did not (Fig. 4). We found a significant benefit of PPs in trials that did not report an ADHD diagnosis (RR = 1.55, 95% CI (1.14, 2.11), I2 = 33%); NNT = 14, 95% CI (7, 53), while no benefit was observed in trials that included patients with comorbid ADHD (RR = 1.17, 95% CI (0.61, 2.25), I2 = 48%). When restricting analyses to prescription amphetamines, there was a significant benefit in the non-ADHD group (RR = 2.33, 95% CI (1.55, 3.51), I2 = 0%); NNT = 7, 95% CI (4, 15). We did not conduct this analysis for the ADHD group as there was only one trial (Levin et al. 2015b) with these characteristics.
To assess the impact of the co-occurring OUD, we separately evaluated three trials where patients also had an OUD and were treated with an opioid agonist (methadone or diacetylmorphine) and those that did not include co-occurring OUD (Fig. 5). The effect of psychostimulants in trials with comorbid OUD was robust (RR = 2.03, 95% CI (1.24, 3.33), I2 = 0%); NNT = 8, 95% CI (4, 32) while there was no benefit of PPs in trials without co-occurring OUD (RR = 1.34, 95% CI (0.98, 1.83), I2 = 39%). However, when restricting analyses to prescription amphetamines, the statistically significant results were detected in both the OUD+ (RR = 2.41, 95% CI (1.39, 4.17), I2 = 0%); NNT = 6, 95% CI (3, 21) and the OUD− (RR = 2.46, 95% CI (1.43, 4.24), I2 = 0%); NNT = 6, 95% CI (3, 19) groups.
The effect of the dose
To assess the impact of the PP dose, we separately evaluated trials that used low doses and those that used high doses. Four of the 17 trials included used dose of PPs that are lower than FDA’s maximum recommended doses (for approved conditions) while 15 used the maximum doses or higher. One trial (Dackis et al. 2012) tested two different doses of modafinil, a low 200 mg/d dose and a high 400 mg/d dose, and we included effect estimates of each of those groups compared to placebo separately. One trial (Levin et al. 2015b) tested two doses of dexamphetamine, 60 and 80 mg/d, but since both were in the high dose range, we merged both treatment groups into a same comparison as recommended by the Cochrane handbook (Higgins and Green 2011).
Trials that use low doses did not show benefit on promoting sustained abstinence (RR = 1.25; 95% CI [0.71, 2.21]), with low heterogeneity (I2 = 0%). Trials with that used high doses showed a statistically significant benefit (RR = 1.50; 95% CI [1.10, 2.06]); NNT = 14, 95% CI (7, 67); however, the clinical benefit was marginal as the confidence interval’s lower bound was not considered clinically meaningful and heterogeneity was intermediate (I2 = 44%) (see Fig. 6). On the other hand, there is moderate quality evidence for the benefit of PPs in maximum higher dosages when restricting analyses to CUDs (RR = 1.95; 95% CI [1.38, 2.77]); NNT = 9, 95% CI (5, 22), with a clinically meaningful CI lower bound and low heterogeneity (I2 = 30%) (see Fig. 7).
Percentage of drug-negative urine tests across trials
We analyzed data from 15 trials to compare the percentage of drug-free urine tests across trials in PPs vs. placebo groups (see Fig. 8). We found a significant difference of 2.40% (95% CI (0.07, 4.73), I2 = 29%) favoring PPs when compared to placebo.
As the main effects found in the dichotomous abstinence analyses were from prescription amphetamines for CUD, we conducted a separate analysis for this subgroup (see Fig. 9). We found a more robust difference of 8.37% (95% CI (3.75, 12.98), I2 = 0%) favoring PPs.
Maximum days of consecutive abstinence
We gathered data from seven trials to compare average maximum days of consecutive abstinence between PPs and placebo groups (see Fig. 10). Due to the scarcity of studies available, subgroup analyses were not possible. We found a significant difference of 3.34 (95% CI (1.06, 5.62), I2 = 41%) days favoring psychostimulants when compared to placebo.
Retention in treatment
All but one of the 38 trials included in this review included the outcome of retention in treatment (see Fig. 11). We did not find a significant benefit of psychostimulants when compared to placebo on promoting retention to treatment in overall stimulants use disorders (RR = 1.04, 95% CI (0.97, 1.11), I2 = 10%), CUD (RR = 1.03, 95% CI (0.96, 1.11), I2 = 7%) and AUD (RR = 1.08, 95% CI (0.93, 1.27), I2 = 22%). No differences were found when analyzing subgroups by medication drug, ADHD status, or comorbid dependences. We also compared retention in treatment between treatment groups using number of days in treatment as outcome. Again, we did not find a statistically significant difference between PPs and placebo (SMD = 0.11, 95% CI (−0.27, 0.50), I2 = 65%). See the Appendix for more details.
We conducted a separate analysis to assess whether providing CM to the patients undergoing treatment with PPs would modify their effect on retention to treatment. The retention in treatment was comparable in the studies with CM vs. those that did not use CM (61.4% vs. 52.0%, t = 1.09, p = 0.28). In the trials where CM was provided for all study participants, PPs were not efficacious on promoting retention to treatment vs. placebo (RR = 0.95, 95% CI (0.84, 1.07), I2 = 0%). This analysis was included in the Appendix.
Medication adherence
We conducted an analysis to address the possible impact of medication adherence on abstinence. Of the 13 trials that included sustained abstinence outcome, all reported overall medication adherence mostly using direct pill count. Medication adherence ranged from 51% to 99% but was generally high with a median of 91%, and we did a median split to compare abstinence in trials with adherence below vs. above the median. Trials above the median had significantly higher rates of abstinence (RR = 1.74, CI = (1.01, 3.00)) as compared to those below the median (RR = 1.26, CI = (0.83, 1.91)). This analysis is included in the Appendix as Fig. 10.
Grade
We conducted GRADE evaluation of the quality of evidence. Evidence was of moderate quality for the following: (1) benefit of prescription amphetamines for treatment of patients with CUD; (2) benefit of PPs for treatment of patients with CUD and comorbid heroin dependence; (3) benefit of higher doses of PPs for treatment of patients with CUD; (4) benefit of prescription amphetamines for CUD patients with and without comorbid opioid use disorder; and (5) benefit of prescription amphetamines for patients with PSUD and no ADHD.
We found low-quality evidence of the benefit of prescription amphetamines on increasing cocaine-negative urines across trials.
Evidence was of very low-quality for the following: (1) overall benefit of PPs on promoting sustained abstinence from stimulants; (2) benefit of PPs on increasing drug-negative urine tests across study; (3) and benefit of PPs for patients with PSUD on promoting maximum days of continuous abstinence. It is unlikely that PPs will have beneficial effect on retention in treatment in patients with PSUD.
The level of evidence for RCTs was downgraded twice for all outcomes due to risk of bias caused by high attrition rates in most of the studies and by potential detection bias due to the behavioral effects of the medication that could hinder blinding. Approximately half of the trials included had significantly more behavioral side effects (most frequently sleep disturbances, anxiety, headache, and dizziness) in the treatment group compared to placebo, and the few trials that evaluated blinding directly had mixed findings. No studies included an active control which might have minimized the risk of detection bias. Downgrades were made also due to inconsistency and imprecision. Upgrades in the level of evidence judgment were made solely based on large effects (RR > 2.0). GRADEPro objective criteria were used to assess quality of evidence of each of the pre-specified outcomes and subgroup analyses. See the summary of findings (SoF) for further information. A summary of the main findings can be seen in Table 2.
Discussion
This meta-analysis found that prescription psychostimulants likely promote sustained drug abstinence and may reduce stimulant use throughout trial and extend duration of abstinence when used in treatment of individuals with PSUDs. The overall effect is primarily influenced by studies that used prescription amphetamines, mostly dextroamphetamine, for treatment of individuals with cocaine use disorder. The present analysis offers preliminary evidence that medications with a more “potent” agonist effect (i.e., dextroamphetamine) are more effective than medications that are less “potent” (i.e., modafinil) and that patients treated with higher doses of agonist medications benefit more than patients treated with lower doses, further supporting the hypothesis that the “agonist effect” is mainly responsible for the clinical benefit.
The quality of evidence that supports results of this meta-analysis varies depending on the medication, condition, and outcome. A moderate quality evidence supports the large benefits of using prescription amphetamines and the benefit of higher doses of prescription psychostimulants when used in the treatment of individuals with cocaine use disorder where the achievement of sustained abstinence is the desired treatment outcome.
The results of this study are consistent with and further extend results of prior meta-analyses published by the Cochrane editorial group of PP efficacy in the treatment of cocaine (Castells et al. 2016) and amphetamine use disorders (Perez-Mana et al. 2013). Similar to Castells et al. (2016), we found that treatment with prescription amphetamines improved sustained abstinence in patients with cocaine use disorder, and we found similar results analyzing subgroups per medication, ADHD status, and concurrent opioid use disorders. We further show that PPs increase maximum days of sustained abstinence from stimulants, though with a small number of studies. This is particularly relevant in light of the association between sustained abstinence and maximum days of abstinence during treatment for cocaine use disorder and the decreased cocaine use and better functioning in the long term (Carroll et al. 2014). However, contrary to the previous reviews, this new meta-analysis shows a significant benefit of PPs on reducing drug use across trial period. This efficacy is more pronounced in trials with prescription amphetamines for patients with CUD.
Unlike studies done by the Cochrane investigators, we evaluated a more restricted range of psychostimulant medications. We limited them to prescription amphetamines, methylphenidate, and modafinil, all controlled substances, to rule out medications with insufficient dopaminergic potency, thereby ensuring a clinically meaningful “agonist effect” (Herin et al. 2010). Among those, the results of trials with modafinil were consistently disappointing, and this may not be a PP with promise on promoting abstinence of cocaine and amphetamines. Our publication included studies published after the most recent review (Castells et al. 2016), most of which used higher doses and extended-release preparations of PPs (Levin et al. 2020; Nuijten et al. 2016). Both of these features had been recommended for clinical use by recent trials (Mariani et al. 2012) and reviews (Mariani and Levin 2012; Rush and Stoops 2012) on this topic.
Similar to Pérez-Mañá and colleagues (2013), we found no effect of PPs on promoting sustained amphetamine abstinence, which is expected since none of the trials published after that review used sustained amphetamine abstinence as an outcome, though we evaluated fewer medications. It should be noted however that earlier studies with methylphenidate used formulations with poor bioavailability which may account for negative findings (Levin et al. 2007; Levin et al. 2006) or used lower, less-effective doses (Konstenius et al. 2010). In addition, there are studies which showed beneficial effects of methylphenidate (Konstenius et al. 2014; Ling et al. 2014; Tiihonen et al. 2007) but did not report sustained abstinence as an outcome and were therefore not included in this analysis. Results of future studies that use improved methodology (Ezard et al. 2018) may change the overall assessments of PP effectiveness in patients with AUD. We found low-quality evidence that PPs increase sustained abstinence for patients with PSUDs in general, but that was attributable to results of studies in cocaine rather than amphetamine use disorder.
As with the earlier finding (Castells et al. 2016), we did not find evidence that treatment with PPs increases the retention in treatment. Retention was measured as a binary variable for treatment completion, and we also carried an additional analysis of retention as a continuous variable of duration in treatment; none of them revealed differences between the treatment and control groups. Subgroup analyses per drug and per medication also did not find significance for treatment retention for any subgroup. This further strengthens the positive effect found on abstinence, especially at the end of treatment, as differential retention might bias toward the treatment arm with the better retention.
There is very limited evidence that any medication improves retention to treatment (Chan et al. 2019; Indave et al. 2016) for PSUDs, unlike the effect of opioid agonists that does increase retention in treatment for opioid use disorder (Mattick et al. 2009). On the other hand, CM is a psychosocial intervention that has been shown to increase treatment retention rates in many different contexts (Garcia-Rodriguez et al. 2009; Miguel et al. 2016; Petry et al. 2005). Combining pharmacotherapy with CM for PSUDs may be an effective strategy to decrease attrition and promote further treatment benefits (Tardelli et al. 2018) as the usually high attrition rates undermine the effect of any therapeutic intervention for PSUDs, though it can be challenging to implement. Nonetheless, PPs had a significant effect on promoting cocaine abstinence, and trials with lower attrition rates found greater effect on sustained abstinence (Nuijten et al. 2016).
Maximum days of continuous abstinence during treatment is an outcome measure predicting long-term endpoints on cocaine use and global functioning (Carroll et al. 2014), but it is not often used in clinical trials. A pooled estimate of this outcome is included in our meta-analysis, but we were limited by the small number of trials and high heterogeneity, partially explained by the fact that we merged CUD and AUD trials. Also, pooled continuous variables usually carry more heterogeneity than binary outcomes in meta-analyses (Alba et al. 2016). But, even with these limitations, we found a significant effect of PPs on the continuous abstinence, and we recommend it for inclusion in the future trials of PSUD pharmacotherapy.
Our review brings an innovative dose range subgroup comparison. The necessity to use higher doses of PPs for PSUDs than those established for other conditions has been a matter of debate (Levin et al. 2015a), as people with PSUDs may be cross-tolerant to the psychostimulant effect of these medications. Our meta-analysis has confirmed that higher but not lower doses of PPs promoted sustained abstinence. Results of trials that used low doses may have underestimated the true potential of PPs, especially for treatment of CUD. Dose of the “agonist” medication plays a major role in its effectiveness as it has been shown with opioid agonists (Faggiano et al. 2003) and also shown in preclinical and human laboratory studies which further underscores the benefit of agonist approach (Czoty et al. 2016). According to the GRADE guidelines, the presence of a dose–response gradient increases the quality of the evidence of a treatment (Higgins and Green 2011). Therefore, since this dose-range analysis is novel, it lowers the risk of bias of results that are already more statistically consistent than those shown in prior analyses which already regarded PPs for CUD as a “promising treatment for cocaine dependence” (Castells et al. 2016). Our findings elevate the quality of the evidence supporting the use of PPs, particularly prescription amphetamines for promoting abstinence in patients with CUD. The NNT of 7 for prescription amphetamines on the treatment of CUDs and 8 for PPs in the treatment of patients with co-occurring OUD is comparable to that found for acamprosate (NNT = 8) and naltrexone (NNT = 9), medications approved for the treatment of alcohol use disorder (Maisel et al. 2013).
It is noteworthy that we have found PPs to be ineffective for AUDs, with no heterogeneity between studies. However, very few trials with AUDs have used sustained abstinence as an outcome, so that only three trials, one with methylphenidate (unpublished data) (Konstenius et al. 2010) and two with modafinil (Anderson et al. 2012; Heinzerling et al. 2010), were pooled, while studies with positive findings were not included (Konstenius et al. 2014; Ling et al. 2014; Longo et al. 2010).
In the analysis per medication, neither modafinil nor methylphenidate was effective on promoting sustained abstinence for PSUDs. Prescription amphetamines were responsible for the overall effect of PPs; however, only two trials up to this point used prescription amphetamines to treat AUDs (Galloway et al. 2011; Longo et al. 2010), and while findings were partially positive, none assessed sustained abstinence. On the other hand, a study conducted in patients with amphetamine use disorder and ADHD found that high dose of extended-release methylphenidate reduced use of amphetamine as compared to placebo, though this study was not included in the efficacy outcomes of this meta-analysis as it did not include the outcome of abstinence (Konstenius et al. 2014). It is possible that, as for CUD, trials with high doses and extended release formulation of prescription amphetamines could promote sustained abstinence from methamphetamine, and at least one of such studies is ongoing (Ezard et al. 2018).
PPs were particularly efficacious on promoting sustained abstinence for the subgroup of individuals with comorbid cocaine and opioid use disorders. Studies in this patient population included potent medications (dextroamphetamine) given at higher doses which is likely the main contributor to overall findings. Moreover, patients already taking methadone could have better adherence to a new medication and a synergic effect between opioid agonist and PPs could promote higher abstinence rates. Higher efficacy of PPs in a population with OUDs could also be explained by a different model of care. The opioid treatment program (OTP) model requires daily attendance to clinic, where study staff could motivate patients at a regular basis and supervise methadone intake, features that ensure patients are highly adherent to the experimental treatment. The OTP model has likely enhanced the adherence to medication in these trials, which could have partially explained the positive results among this specific subgroup (especially when considering that the overall quality of evidence for PPs for PSUD was severely undermined by elevated attrition rates). Nuijten and colleagues conducted a trial using high doses of extended-release dexamphetamine for individuals dependent on crack-cocaine using a structure similar to those of the OTP and found significant results for sustained abstinence and maximum days of abstinence, with low attrition rates for both groups (Nuijten et al. 2016). Beyond the effect of medication itself, this well-designed trial successfully addressed common problems in trials with PSUDs, such as elevated dropout rates. This suggests that a structured model of care using PPs similar to methadone clinics could be an alternative for outpatient medication-based intervention for patients with PSUDs, yet other studies have shown that prescription amphetamines can be effective when given in a traditional outpatient treatment setting.
Patients with ADHD are more prone than the general population to develop substance use disorders, and ADHD is a common comorbidity among patients seeking treatment for substance use disorders (Lee et al. 2011; van Emmerik-van Oortmerssen et al. 2012). PPs are the gold standard treatment for ADHD (Faraone and Buitelaar 2010) and were found to improve ADHD symptoms in trials with comorbid ADHD and SUDs (Konstenius et al. 2010; Levin et al. 2007). However, the impact on PSUD is mixed. Factors that might have led to early negative results include use of medications with poorer bioavailability (Levin et al. 2006, 2007) or inadequate dosing (Levin et al. 2006). Levin and colleagues hypothesized that patients with ADHD and heavy cocaine use could require even higher dosages of dopaminergic medications than those with high cocaine use but no ADHD and conducted a trial comparing a regimen of 80 mg/day of dextroamphetamine to the usual dose of 60 mg/day and placebo (Levin et al. 2015b). Both medication groups achieved significantly higher rates of sustained abstinence compared to placebo; the 80 mg groups had larger odds of sustained abstinence than the 60 mg group, although that difference was not significant. Consistent with this approach, Konstenius et al. (2014) found that high doses of extended-release methylphenidate (up to 180 mg/day) resulted in clinically significant improvement in ADHD and reduction in amphetamine use among those with amphetamine use disorder (Konstenius et al. 2014) whereas the lower dose of 72 mg/day did not result in a reduction in ADHD symptoms or amphetamine use (Konstenius et al. 2010). Because the 2014 study with higher doses of methylphenidate did not provide data on the sustained abstinence outcome, their efficacy measures were not included in this meta-analysis. Low dosages in the other two trials pooled might explain PPs’ low efficacy in the ADHD subgroup. Importantly, patients in the PPs group showed improvements in the ADHD outcomes in all of three trials mentioned above which refutes the argument that drug-related clinical improvements in patients with ADHD are mostly mediated by treatment of the ADHD symptoms. Another caveat of this subgroup analysis is that most studies reported did not assess ADHD status and did not exclude these individuals. This way, it is possible that many patients seeking treatment for PSUDs also have ADHD but are not diagnosed. Given that there are limited though encouraging data, further studies with higher PPs dosages are necessary to evaluate the effect of PPs in patients with co-occurring PSUD and ADHD (Woon et al. 2018).
Psychosocial treatments, particularly CM targeting abstinence and treatment adherence, have shown benefits in patients with PSUD (Kampman 2019; Lussier et al. 2006). Using CM in combination with a pharmacologic treatment has been shown to have synergic effect in decreasing drug use and enhancing treatment (Penberthy et al. 2010; Tardelli et al. 2018). However, in the present meta-analysis, we did not find that CM (targeting either abstinence or adherence) improved treatment retention. Incorporating CM elements to decrease treatment attrition may be considered in future trials as high rates of treatment attrition remain a prominent issue in trials conducted in patients with PSUD although it is possible that the effect of well-designed and implemented CM may create the ceiling effect, with increase in placebo response, which lowers the possibility of detecting the medication effect.
The current meta-analysis has several limitations. Many of the trials included were likely underpowered, which might have hindered positive findings about the efficacy of PPs when looking at the trials individually but the meta-analysis that also includes adequately powered trials usually corrects this limitation (Nuesch et al. 2010). Since almost all of the trials evaluated excluded individuals with severe psychiatric comorbidities from their sample or did not assess for other common conditions, such as ADHD, it was not possible to conduct sub-group analyses on depression or other highly prevalent conditions in patients with PSUD. Due to the heterogeneity of outcome measurement among the included studies, it was not possible to pool relevant outcomes, such as other continuous drug use variables, e.g., reduction in drug use, reduction in drug use category (Roos et al. 2019a), or other non-abstinence endpoints. Also, due to the scarcity of data, it was not possible to compare trials using higher dosages of PPs to those using the current maximum dosages approved by the FDA for other conditions. The duration of sustained abstinence as an outcome differed across trials. Moreover, elevated attrition rates might have underestimated treatment effects and decisively influenced on the GRADE judgment of the quality of evidence. Few trials with features that are known to improve adherence in trials of pharmacologic treatment of substance use disorders, such as CM targeting drug use or attendance (Tardelli et al. 2018) and daily supervised intake and motivational enhancement (Weiss 2004), were available. Also, quality assessment was downgraded for all outcomes due to possible detection bias, since the intervention has potential behavioral effects that may hinder blinding of clinicians, patients, and outcome assessors. Therefore, it is vital that the interpretations of our findings for clinical practice consider that the nature of the intervention makes high-quality evidence methodologically impossible at this point. This warrants future trials with comparable methods to those that showed best evidence (prescription amphetamines in higher dosages for CUD, for example), since downgrades in the quality of evidence are not due to lack of efficacy but to properties of the intervention and to methodological issues of the trials included which may be difficult to overcome.
The present meta-analysis has several strengths. We included the GRADE approach for each of the subgroup analyses which might help in dealing with group specificities when elaborating new public policies and in designing future clinical trials on this field. The new subgroup analysis by dose range suggests a dose–response relationship and strengthens the quality of the evidence supporting PPs for PSUDs. Lastly, calculating NNTs provides a clinically translatable measure of effect that might facilitate the dissemination findings in clinician guiding activities, though the NNT obtained from meta-analyses should be interpreted with caution due to differences in treatment effects between studies (Marx and Bucher 2003).
The results of the present study have implications for further trials that aim to test the efficacy of PPs for PSUDs. An optimal trial should test at least one high dose of PPs with extended-release formulations to ensure the maximum potential benefit and to test efficacy of the agonist-based therapy. Moreover, features that minimize attrition and maximize adherence with the medication, a common problem of trials with PSUDs, are warranted and may include CM, daily attendance to clinic, and supervised medication intake. Use of extended-release preparations and once-daily dosing, preferably under direct observation, should be considered to maximize safety and minimize diversion potential. Unstable cardiovascular disorder and a history of a psychotic disorder should be considered as exclusionary. Abstinence-based outcomes (sustained abstinence and maximum days of abstinence) should be combined with continuous drug use outcomes.
Trials with higher dosages of PPs, especially prescription amphetamines, are particularly needed for the treatment of AUD. The combination of PPs with topiramate has shown promise on the treatment of PSUD, and therefore, combination treatments should be considered for future trials. We believe that feasibility studies of the “agonist-type” pharmacological intervention, namely outpatient-based supervised treatment with high-dose, extended-release preparation of amphetamines, should be considered particularly in countries with high rates of PSUDs that currently do not provide any medical treatment for those individuals. In real-world scenarios, one possible strategy is to offer treatment with prescription amphetamines in the setting of an OTP. Many patients with PSUD are already enrolled in OTPs (those with co-occurring OUD and PSUD), and others can be referred to OTPs for the medical management of PSUD as the traditional PSUD outpatient programs do not offer consistent medical and multi-professional oversight. Alternatively, mobile technology solutions for monitoring and increasing adherence to the medication may be considered.
Conclusion
Recent trials with extended-release formulations and higher dosages of PPs, particularly prescription amphetamines, have shown promising results promoting abstinence from cocaine and reducing drug use. PPs’ potential as an “agonist-type” treatment seems to be better explored with higher dosage regimens and at clinical settings that have direct observed dosing available. The results from patients with comorbid opioid use disorders are particularly encouraging, and this may be due to the fact that high dosages of potent PPs were used, and this population is already enrolled to a healthcare facility that offers daily attendance, supervised medication intake, evidence-based psychosocial interventions, and a wide-range of ancillary services. A widely used and successful model of treating opioid use disorder or incorporating mobile technology solutions to monitor and enhance medication adherence may now be assessed for treatment of individuals with psychostimulant use disorder and incorporate prescription amphetamines as an agonist intervention. Considering the major public health impact of untreated PSUD, and the absence of the widely accepted pharmacological intervention, there is an urgent need to conduct implementation studies of this treatment approach.
References
Alba AC, Alexander PE, Chang J, MacIsaac J, DeFry S, Guyatt GH (2016) High statistical heterogeneity is more frequent in meta-analysis of continuous than binary outcomes. J Clin Epidemiol 70:129–135
Amato L, Minozzi S, Pani PP, Solimini R, Vecchi S, Zuccaro P, Davoli M (2011) Dopamine agonists for the treatment of cocaine dependence. Cochrane Database Syst Rev:CD003352
Andersen ML, Kessler E, Murnane KS, McClung JC, Tufik S, Howell LL (2010) Dopamine transporter-related effects of modafinil in rhesus monkeys. Psychopharmacology (Berl) 210:439–448
Anderson AL, Reid MS, Li SH, Holmes T, Shemanski L, Slee A, Smith EV, Kahn R, Chiang N, Vocci F, Ciraulo D, Dackis C, Roache JD, Salloum IM, Somoza E, Urschel HC 3rd, Elkashef AM (2009) Modafinil for the treatment of cocaine dependence. Drug Alcohol Depend 104:133–139
Anderson AL, Li SH, Biswas K, McSherry F, Holmes T, Iturriaga E, Kahn R, Chiang N, Beresford T, Campbell J, Haning W, Mawhinney J, McCann M, Rawson R, Stock C, Weis D, Yu E, Elkashef AM (2012) Modafinil for the treatment of methamphetamine dependence. Drug Alcohol Depend 120:135–141
Anthony JC, Warner LA, Kessler RC (1997) Comparative epidemiology of dependence on tobacco, alcohol, controlled substances, and inhalants: basic findings from the National Comorbidity Survey.
Balshem H, Helfand M, Schunemann HJ, Oxman AD, Kunz R, Brozek J, Vist GE, Falck-Ytter Y, Meerpohl J, Norris S, Guyatt GH (2011) GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 64:401–406
Borenstein M, Higgins JP (2013) Meta-analysis and subgroups. Prev Sci 14:134–143
Callaghan RC, Halliday M, Gatley J, Sykes J, Taylor L, Benny C, Kish SJ (2018) Comparative hazards of acute myocardial infarction among hospitalized patients with methamphetamine- or cocaine-use disorders: a retrospective cohort study. Drug Alcohol Depend 188:259–265
Carroll KM, Kiluk BD, Nich C, DeVito EE, Decker S, LaPaglia D, Duffey D, Babuscio TA, Ball SA (2014) Toward empirical identification of a clinically meaningful indicator of treatment outcome: features of candidate indicators and evaluation of sensitivity to treatment effects and relationship to one year follow up cocaine use outcomes. Drug Alcohol Depend 137:3–19
Castells X, Cunill R, Perez-Mana C, Vidal X, Capella D (2016) Psychostimulant drugs for cocaine dependence. Cochrane Database Syst Rev 9:CD007380
Chan B, Kondo K, Freeman M, Ayers C, Montgomery J, Kansagara D (2019) Pharmacotherapy for cocaine use disorder—a systematic review and meta-analysis. J Gen Intern Med. 34:2858–2873
Cooper WO, Habel LA, Sox CM, Chan KA, Arbogast PG, Cheetham TC, Murray KT, Quinn VP, Stein CM, Callahan ST, Fireman BH, Fish FA, Kirshner HS, O'Duffy A, Connell FA, Ray WA (2011) ADHD drugs and serious cardiovascular events in children and young adults. N Engl J Med 365:1896–1904
Czoty PW, Stoops WW, Rush CR (2016) Evaluation of the "pipeline" for development of medications for cocaine use disorder: a review of translational preclinical, human laboratory, and clinical trial research. Pharmacol Rev 68:533–562
Dackis CA, Kampman KM, Lynch KG, Pettinati HM, O'Brien CP (2005) A double-blind, placebo-controlled trial of modafinil for cocaine dependence. Neuropsychopharmacology 30:205–211
Dackis CA, Kampman KM, Lynch KG, Plebani JG, Pettinati HM, Sparkman T, O'Brien CP (2012) A double-blind, placebo-controlled trial of modafinil for cocaine dependence. J Subst Abuse Treat 43:303–312
Darke S, Farrell M (2016) Which medications are suitable for agonist drug maintenance? Addiction 111:767–774
De Crescenzo F, Cortese S, Adamo N, Janiri L (2017) Pharmacological and non-pharmacological treatment of adults with ADHD: a meta-review. Evid Based Ment Health 20:4–11
De Giorgi R, Cassar C, Loreto D'alo G, Ciabattini M, Minozzi S, Economou A, Tambelli R, Lucchese F, Saulle R, Amato L, Janiri L, De Crescenzo F (2018) Psychosocial interventions in stimulant use disorders: a systematic review and qualitative synthesis of randomized controlled trials. Riv Psichiatr 53:233–255
Deeks JJ (2002) Issues in the selection of a summary statistic for meta-analysis of clinical trials with binary outcomes. Stat Med 21:1575–1600
Degenhardt L, Charlson F, Stanaway J, Larney S, Alexander LT, Hickman M, Cowie B, Hall WD, Strang J, Whiteford H, Vos T (2016) Estimating the burden of disease attributable to injecting drug use as a risk factor for HIV, hepatitis C, and hepatitis B: findings from the Global Burden of Disease Study 2013. Lancet Infect Dis 16:1385–1398
Dursteler-MacFarland KM, Farronato NS, Strasser J, Boss J, Kuntze MF, Petitjean SA, Burki C, Wiesbeck GA (2013) A randomized, controlled, pilot trial of methylphenidate and cognitive-behavioral group therapy for cocaine dependence in heroin prescription. J Clin Psychopharmacol 33:104–108
Engels EA, Schmid CH, Terrin N, Olkin I, Lau J (2000) Heterogeneity and statistical significance in meta-analysis: an empirical study of 125 meta-analyses. Stat Med 19:1707–1728
Ezard N, Dunlop A, Hall M, Ali R, McKetin R, Bruno R, Phung N, Carr A, White J, Clifford B, Liu Z, Shanahan M, Dolan K, Baker AL, Lintzeris N (2018) LiMA: a study protocol for a randomised, double-blind, placebo controlled trial of lisdexamfetamine for the treatment of methamphetamine dependence. BMJ Open 8:e020723
Faggiano F, Vigna-Taglianti F, Versino E, Lemma P (2003) Methadone maintenance at different dosages for opioid dependence. Cochrane Database Syst Rev:CD002208
Faraone SV, Buitelaar J (2010) Comparing the efficacy of stimulants for ADHD in children and adolescents using meta-analysis. Eur Child Adolesc Psychiatry 19:353–364
Fiorentini A, Volonteri LS, Dragogna F, Rovera C, Maffini M, Mauri MC, Altamura CA (2011) Substance-induced psychoses: a critical review of the literature. Curr Drug Abuse Rev 4:228–240
Florez-Salamanca L, Secades-Villa R, Hasin DS, Cottler L, Wang S, Grant BF, Blanco C (2013) Probability and predictors of transition from abuse to dependence on alcohol, cannabis, and cocaine: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Am J Drug Alcohol Abuse 39:168–179
Galloway GP, Buscemi R, Coyle JR, Flower K, Siegrist JD, Fiske LA, Baggott MJ, Li L, Polcin D, Chen CY, Mendelson J (2011) A randomized, placebo-controlled trial of sustained-release dextroamphetamine for treatment of methamphetamine addiction. Clin Pharmacol Ther 89:276–282
Garcia-Rodriguez O, Secades-Villa R, Higgins ST, Fernandez-Hermida JR, Carballo JL, Errasti Perez JM, Al-halabi Diaz S (2009) Effects of voucher-based intervention on abstinence and retention in an outpatient treatment for cocaine addiction: a randomized controlled trial. Exp Clin Psychopharmacol 17:131–138
Goldstein RZ, Volkow ND (2011) Oral methylphenidate normalizes cingulate activity and decreases impulsivity in cocaine addiction during an emotionally salient cognitive task. Neuropsychopharmacology 36:366–367
Goldstein RZ, Woicik PA, Maloney T, Tomasi D, Alia-Klein N, Shan J, Honorio J, Samaras D, Wang R, Telang F, Wang GJ, Volkow ND (2010) Oral methylphenidate normalizes cingulate activity in cocaine addiction during a salient cognitive task. Proc Natl Acad Sci U S A 107:16667–16672
Grabowski J, Schmitz J, Roache J, Rhoades H, Elk R, Creson D (1994) Methylphenidate (MP) for initial treatment of cocaine dependence and a model for medication evaluation. NIDA Research Monograph 141:436–436
Grabowski J, Roache JD, Schmitz JM, Rhoades H, Creson D, Korszun A (1997) Replacement medication for cocaine dependence: methylphenidate. J Clin Psychopharmacol 17:485–488
Grabowski J, Rhoades H, Schmitz J, Stotts A, Daruzska LA, Creson D, Moeller FG (2001) Dextroamphetamine for cocaine-dependence treatment: a double-blind randomized clinical trial. J Clin Psychopharmacol 21:522–526
Grabowski J, Rhoades H, Stotts A, Cowan K, Kopecky C, Dougherty A, Moeller FG, Hassan S, Schmitz J (2004) Agonist-like or antagonist-like treatment for cocaine dependence with methadone for heroin dependence: two double-blind randomized clinical trials. Neuropsychopharmacology 29:969–981
Grant BF, Saha TD, Ruan WJ, Goldstein RB, Chou SP, Jung J, Zhang H, Smith SM, Pickering RP, Huang B, Hasin DS (2016) Epidemiology of DSM-5 drug use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions—III. JAMA Psychiatry 73:39–47
Griffith JD, Carranza J, Griffith C, Miller LL (1983) Bupropion: clinical assay for amphetamine-like abuse potential. J Clin Psychiatry 44:206–208
Habel LA, Cooper WO, Sox CM, Chan KA, Fireman BH, Arbogast PG, Cheetham TC, Quinn VP, Dublin S, Boudreau DM, Andrade SE, Pawloski PA, Raebel MA, Smith DH, Achacoso N, Uratsu C, Go AS, Sidney S, Nguyen-Huynh MN, Ray WA, Selby JV (2011) ADHD medications and risk of serious cardiovascular events in young and middle-aged adults. JAMA 306:2673–2683
Hartmann-Boyce J, Stead LF, Cahill K, Lancaster T (2014) Efficacy of interventions to combat tobacco addiction: Cochrane update of 2013 reviews. Addiction 109:1414–1425
Heinzerling KG, Swanson AN, Kim S, Cederblom L, Moe A, Ling W, Shoptaw S (2010) Randomized, double-blind, placebo-controlled trial of modafinil for the treatment of methamphetamine dependence. Drug Alcohol Depend 109:20–29
Hellem TL, Lundberg KJ, Renshaw PF (2015) A review of treatment options for co-occurring methamphetamine use disorders and depression. J Addict Nurs 26:14–23 quiz E1
Herin DV, Rush CR, Grabowski J (2010) Agonist-like pharmacotherapy for stimulant dependence: preclinical, human laboratory, and clinical studies. Ann N Y Acad Sci 1187:76–100
Higgins JPT, Green S (2011) Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, Cochrane Bias Methods G, Cochrane Statistical Methods G (2011) The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Indave BI, Minozzi S, Pani PP, Amato L (2016) Antipsychotic medications for cocaine dependence. Cochrane Database Syst Rev 3:CD006306
Jasinski DR (2000) An evaluation of the abuse potential of modafinil using methylphenidate as a reference. J Psychopharmacology 14:53–60
Jerry JM, Shirvani N, Dale R (2016) Addiction to armodafinil and modafinil presenting with paranoia. J Clin Psychopharmacol 36:98–100
Kalivas PW, O'Brien C (2008) Drug addiction as a pathology of staged neuroplasticity. Neuropsychopharmacology 33:166–180
Kampman KM (2019) The treatment of cocaine use disorder. Sci Adv 5:eaax1532
Kampman KM, Lynch KG, Pettinati HM, Spratt K, Wierzbicki MR, Dackis C, O'Brien CP (2015) A double blind, placebo controlled trial of modafinil for the treatment of cocaine dependence without co-morbid alcohol dependence. Drug Alcohol Depend 155:105–110
Kim W, Tateno A, Arakawa R, Sakayori T, Ikeda Y, Suzuki H, Okubo Y (2014) In vivo activity of modafinil on dopamine transporter measured with positron emission tomography and [(1)(8)F]FE-PE2I. Int J Neuropsychopharmacol 17:697–703
Konstenius M, Jayaram-Lindstrom N, Beck O, Franck J (2010) Sustained release methylphenidate for the treatment of ADHD in amphetamine abusers: a pilot study. Drug Alcohol Depend 108:130–133
Konstenius M, Jayaram-Lindstrom N, Guterstam J, Beck O, Philips B, Franck J (2014) Methylphenidate for attention deficit hyperactivity disorder and drug relapse in criminal offenders with substance dependence: a 24-week randomized placebo-controlled trial. Addiction 109:440–449
Learned-Coughlin SM, Bergstrom M, Savitcheva I, Ascher J, Schmith VD, Langstrom B (2003) In vivo activity of bupropion at the human dopamine transporter as measured by positron emission tomography. Biol Psychiatry 54:800–805
Lee NK, Rawson RA (2008) A systematic review of cognitive and behavioural therapies for methamphetamine dependence. Drug Alcohol Rev 27:309–317
Lee SS, Humphreys KL, Flory K, Liu R, Glass K (2011) Prospective association of childhood attention-deficit/hyperactivity disorder (ADHD) and substance use and abuse/dependence: a meta-analytic review. Clin Psychol Rev 31:328–341
Levin FR, Evans SM, Brooks DJ, Kalbag AS, Garawi F, Nunes EV (2006) Treatment of methadone-maintained patients with adult ADHD: double-blind comparison of methylphenidate, bupropion and placebo. Drug Alcohol Depend 81:137–148
Levin FR, Evans SM, Brooks DJ, Garawi F (2007) Treatment of cocaine dependent treatment seekers with adult ADHD: double-blind comparison of methylphenidate and placebo. Drug Alcohol Depend 87:20–29
Levin FR, Mariani JJ, Bisaga A, Nunes EV (2015a) Ling et al.’s ‘sustained-release methylphenidate in a randomized trial of treatment of methamphetamine use disorder’. Addiction 110:875–876
Levin FR, Mariani JJ, Specker S, Mooney M, Mahony A, Brooks DJ, Babb D, Bai Y, Eberly LE, Nunes EV, Grabowski J (2015b) Extended-release mixed amphetamine salts vs placebo for comorbid adult attention-deficit/hyperactivity disorder and cocaine use disorder: a randomized clinical trial. JAMA Psychiatry 72:593–602
Levin FR, Mariani JJ, Pavlicova M, Choi CJ, Mahony AL, Brooks DJ, Bisaga A, Dakwar E, Carpenter KM, Naqvi N, Nunes EV, Kampman K (2020) Extended release mixed amphetamine salts and topiramate for cocaine dependence: a randomized clinical replication trial with frequent users. Drug Alcohol Depend 206:107700
Ling W, Chang L, Hillhouse M, Ang A, Striebel J, Jenkins J, Hernandez J, Olaer M, Mooney L, Reed S, Fukaya E, Kogachi S, Alicata D, Holmes N, Esagoff A (2014) Sustained-release methylphenidate in a randomized trial of treatment of methamphetamine use disorder. Addiction 109:1489–1500
London ED, Kohno M, Morales AM, Ballard ME (2015) Chronic methamphetamine abuse and corticostriatal deficits revealed by neuroimaging. Brain Res 1628:174–185
Longo M, Wickes W, Smout M, Harrison S, Cahill S, White JM (2010) Randomized controlled trial of dexamphetamine maintenance for the treatment of methamphetamine dependence. Addiction 105:146–154
Lussier JP, Heil SH, Mongeon JA, Badger GJ, Higgins ST (2006) A meta-analysis of voucher-based reinforcement therapy for substance use disorders. Addiction 101:192–203
Madras BK, Xie Z, Lin Z, Jassen A, Panas H, Lynch L, Johnson R, Livni E, Spencer TJ, Bonab AA, Miller GM, Fischman AJ (2006) Modafinil occupies dopamine and norepinephrine transporters in vivo and modulates the transporters and trace amine activity in vitro. J Pharmacol Exp Ther 319:561–569
Maisel NC, Blodgett JC, Wilbourne PL, Humphreys K, Finney JW (2013) Meta-analysis of naltrexone and acamprosate for treating alcohol use disorders: when are these medications most helpful? Addiction 108:275–293
Mariani JJ, Levin FR (2012) Psychostimulant treatment of cocaine dependence. Psychiatr Clin North Am 35:425–439
Mariani JJ, Pavlicova M, Bisaga A, Nunes EV, Brooks DJ, Levin FR (2012) Extended-release mixed amphetamine salts and topiramate for cocaine dependence: a randomized controlled trial. Biol Psychiatry 72:950–956
Marsden J, Eastwood B, Bradbury C, Dale-Perera A, Farrell M, Hammond P, Knight J, Randhawa K, Wright C, National Drug Treatment Monitoring System Outcomes Study G (2009) Effectiveness of community treatments for heroin and crack cocaine addiction in England: a prospective, in-treatment cohort study. Lancet 374:1262–1270
Marx A, Bucher HC (2003) Numbers needed to treat derived from meta-analysis: a word of caution. ACP J Club 138:A11–A12
Mattick RP, Breen C, Kimber J, Davoli M (2009) Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database Syst Rev:CD002209
McMaster University (developed by Evidence Prime I (2015) GRADEpro GDT: GRADEpro Guideline Development Tool [Software]
Meyer JH, Goulding VS, Wilson AA, Hussey D, Christensen BK, Houle S (2002) Bupropion occupancy of the dopamine transporter is low during clinical treatment. Psychopharmacology (Berl) 163:102–105
Miguel AQ, Madruga CS, Cogo-Moreira H, Yamauchi R, Simoes V, da Silva CJ, McPherson S, Roll JM, Laranjeira RR (2016) Contingency management is effective in promoting abstinence and retention in treatment among crack cocaine users in Brazil: a randomized controlled trial. Psychol Addict Behav 30:536–543
Miguel AQC, Kiluk BD, Babuscio TA, Nich C, Mari JJ, Carroll KM (2019) Short and long-term improvements in psychiatric symptomatology to validate clinically meaningful treatment outcomes for cocaine use disorders. Drug Alcohol Depend 198:126–132
Miles SW, Sheridan J, Russell B, Kydd R, Wheeler A, Walters C, Gamble G, Hardley P, Jensen M, Kuoppasalmi K, Tuomola P, Fohr J, Kuikanmaki O, Vorma H, Salokangas R, Mikkonen A, Kallio M, Kauhanen J, Kiviniemi V, Tiihonen J (2013) Extended-release methylphenidate for treatment of amphetamine/methamphetamine dependence: a randomized, double-blind, placebo-controlled trial. Addiction 108:1279–1286
Minozzi S, Saulle R, De Crescenzo F, Amato L (2016) Psychosocial interventions for psychostimulant misuse. Cochrane Database Syst Rev 9:CD011866
Modafinil and Naltrexone to Reduce Cocaine and Alcohol Dependence (n.d.) https://ClinicalTrials.gov/show/NCT00142818
Modafinil Combined With Cognitive Behavior Therapy to Treat Cocaine Addiction—1 (n.d.) https://ClinicalTrials.gov/show/NCT00218387
Modafinil for Methamphetamine Dependence (n.d.) https://ClinicalTrials.gov/show/NCT00859573
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62:1006–1012
Mooney ME, Herin DV, Schmitz JM, Moukaddam N, Green CE, Grabowski J (2009) Effects of oral methamphetamine on cocaine use: a randomized, double-blind, placebo-controlled trial. Drug Alcohol Depend 101:34–41
Mooney ME, Herin DV, Specker S, Babb D, Levin FR, Grabowski J (2015) Pilot study of the effects of lisdexamfetamine on cocaine use: a randomized, double-blind, placebo-controlled trial. Drug Alcohol Depend 153:94–103
Morgan PT, Angarita GA, Canavan S, Pittman B, Oberleitner L, Malison RT, Mohsenin V, Hodges S, Easton C, McKee S, Bessette A, Forselius E (2016) Modafinil and sleep architecture in an inpatient-outpatient treatment study of cocaine dependence. Drug Alcohol Depend 160:49–56
Nuesch E, Trelle S, Reichenbach S, Rutjes AW, Tschannen B, Altman DG, Egger M, Juni P (2010) Small study effects in meta-analyses of osteoarthritis trials: meta-epidemiological study. BMJ 341:c3515
Nuijten M, Blanken P, van de Wetering B, Nuijen B, van den Brink W, Hendriks VM (2016) Sustained-release dexamfetamine in the treatment of chronic cocaine-dependent patients on heroin-assisted treatment: a randomised, double-blind, placebo-controlled trial. Lancet 387:2226–2234
Oxman AD, Guyatt GH (1992) A consumer's guide to subgroup analyses. Ann Intern Med 116:78–84
Penberthy JK, Ait-Daoud N, Vaughan M, Fanning T (2010) Review of treatment for cocaine dependence. Curr Drug Abuse Rev 3:49–62
Pérez-Mañá C, Llonch C, Farre M (2012) Transparency in clinical research: registration of clinical trials and publication of results. Med Clin (Barc) 139:593–597
Pérez-Mañá C, Castells X, Torrens M, Capella D, Farre M (2013) Efficacy of psychostimulant drugs for amphetamine abuse or dependence. Cochrane Database Syst Rev:CD009695
Petry NM, Peirce JM, Stitzer ML, Blaine J, Roll JM, Cohen A, Obert J, Killeen T, Saladin ME, Cowell M, Kirby KC, Sterling R, Royer-Malvestuto C, Hamilton J, Booth RE, Macdonald M, Liebert M, Rader L, Burns R, DiMaria J, Copersino M, Stabile PQ, Kolodner K, Li R (2005) Effect of prize-based incentives on outcomes in stimulant abusers in outpatient psychosocial treatment programs: a national drug abuse treatment clinical trials network study. Arch Gen Psychiatry 62:1148–1156
Pharmacotherapy & CM for Opioid and Cocaine Dependence (n.d.) https://ClinicalTrials.gov/show/NCT00838981
Pharmacotherapy Dosing Regimen in Cocaine and Opiate Dependent Individuals—8 (n.d.) https://ClinicalTrials.gov/show/NCT00218036
Rezaei F, Emami M, Zahed S, Morabbi MJ, Farahzadi M, Akhondzadeh S (2015) Sustained-release methylphenidate in methamphetamine dependence treatment: a double-blind and placebo-controlled trial. Daru 23:2
Roos CR, Nich C, Mun CJ, Babuscio TA, Mendonca J, Miguel AQC, DeVito EE, Yip SW, Witkiewitz K, Carroll KM, Kiluk BD (2019a) Clinical validation of reduction in cocaine frequency level as an endpoint in clinical trials for cocaine use disorder. Drug Alcohol Depend 205:107648
Roos CR, Nich C, Mun CJ, Mendonca J, Babuscio TA, Witkiewitz K, Carroll KM, Kiluk BD (2019b) Patterns of cocaine use during treatment: associations with baseline characteristics and follow-up functioning. J Stud Alcohol Drugs 80:431–440
Rounsaville BJ (2004) Treatment of cocaine dependence and depression. Biol Psychiatry 56:803–809
Rounsaville BJ, Anton SF, Carroll K, Budde D, Prusoff BA, Gawin F (1991) Psychiatric diagnoses of treatment-seeking cocaine abusers. Arch Gen Psychiatry 48:43–51
Rush CR, Baker RW (2001) Behavioral pharmacological similarities between methylphenidate and cocaine in cocaine abusers. Exp Clin Psychopharmacol 9:59–73
Rush CR, Stoops WW (2012) Agonist replacement therapy for cocaine dependence: a translational review. Future Med Chem 4:245–265
Sabrini S, Wang GY, Lin JC, Ian JK, Curley LE (2019) Methamphetamine use and cognitive function: a systematic review of neuroimaging research. Drug Alcohol Depend 194:75–87
Schmitz JM, Rathnayaka N, Green CE, Moeller FG, Dougherty AE, Grabowski J (2012) Combination of modafinil and d-amphetamine for the treatment of cocaine dependence: a preliminary investigation. Front Psychiatry 3:77
Schmitz JM, Green CE, Stotts AL, Lindsay JA, Rathnayaka NS, Grabowski J, Moeller FG (2014) A two-phased screening paradigm for evaluating candidate medications for cocaine cessation or relapse prevention: modafinil, levodopa-carbidopa, naltrexone. Drug Alcohol Depend 136:100–107
Schubiner H, Saules KK, Arfken CL, Johanson CE, Schuster CR, Lockhart N, Edwards A, Donlin J, Pihlgren E (2002) Double-blind placebo-controlled trial of methylphenidate in the treatment of adult ADHD patients with comorbid cocaine dependence. Exp Clin Psychopharmacol 10:286–294
Schuckit MA (2016) Treatment of opioid-use disorders. N Engl J Med 375:357–368
Shearer J (2008) The principles of agonist pharmacotherapy for psychostimulant dependence. Drug Alcohol Rev 27:301–308
Shearer J, Sherman J, Wodak A, van Beek I (2002) Substitution therapy for amphetamine users. Drug Alcohol Rev 21:179–185
Shearer J, Wodak A, van Beek I, Mattick RP, Lewis J (2003) Pilot randomized double blind placebo-controlled study of dexamphetamine for cocaine dependence. Addiction 98:1137–1141
Shearer J, Darke S, Rodgers C, Slade T, van Beek I, Lewis J, Brady D, McKetin R, Mattick RP, Wodak A (2009) A double-blind, placebo-controlled trial of modafinil (200 mg/day) for methamphetamine dependence. Addiction 104:224–233
Singh M, Keer D, Klimas J, Wood E, Werb D (2016) Topiramate for cocaine dependence: a systematic review and meta-analysis of randomized controlled trials. Addiction 111:1337–1346
Stoops WW, Rush CR (2013) Agonist replacement for stimulant dependence: a review of clinical research. Curr Pharm Des 19:7026–7035
Substance Abuse Mental Health Services Administration (2019) Key substance use and mental health indicators in the United States: results from the 2018 National Survey on Drug Use and Health. Rockville, MD: (HHS Publication No PEP19-5068, NSDUH Series H-54), Rockville, MD: Center for Behavioral Health Statistics and Quality
Tardelli VS, Lago M, Mendez M, Bisaga A, Fidalgo TM (2018) Contingency management with pharmacologic treatment for stimulant use disorders: a review. Behav Res Ther 111:57–63
The Nordic Cochrane Centre TCC (2014) Review Manager (RevMan) [Computer program] Version 5.3
Tiihonen J, Kuoppasalmi K, Fohr J, Tuomola P, Kuikanmaki O, Vorma H, Sokero P, Haukka J, Meririnne E (2007) A comparison of aripiprazole, methylphenidate, and placebo for amphetamine dependence. Am J Psychiatry 164:160–162
United Nations Office on Drugs and Crime (2019) World drug report 2019
van de Glind G, Konstenius M, Koeter MWJ, van Emmerik-van Oortmerssen K, Carpentier PJ, Kaye S, Degenhardt L, Skutle A, Franck J, Bu ET, Moggi F, Dom G, Verspreet S, Demetrovics Z, Kapitany-Foveny M, Fatseas M, Auriacombe M, Schillinger A, Moller M, Johnson B, Faraone SV, Ramos-Quiroga JA, Casas M, Allsop S, Carruthers S, Schoevers RA, Wallhed S, Barta C, Alleman P, Group IR, Levin FR, van den Brink W (2014) Variability in the prevalence of adult ADHD in treatment seeking substance use disorder patients: results from an international multi-center study exploring DSM-IV and DSM-5 criteria. Drug Alcohol Depend 134:158–166
van Emmerik-van Oortmerssen K, van de Glind G, van den Brink W, Smit F, Crunelle CL, Swets M, Schoevers RA (2012) Prevalence of attention-deficit hyperactivity disorder in substance use disorder patients: a meta-analysis and meta-regression analysis. Drug Alcohol Depend 122:11–19
Viera AJ (2008) Odds ratios and risk ratios: what's the difference and why does it matter? South Med J 101:730–734
Volkow ND, Fowler JS, Logan J, Alexoff D, Zhu W, Telang F, Wang GJ, Jayne M, Hooker JM, Wong C, Hubbard B, Carter P, Warner D, King P, Shea C, Xu Y, Muench L, Apelskog-Torres K (2009) Effects of modafinil on dopamine and dopamine transporters in the male human brain: clinical implications. JAMA 301:1148–1154
Weiss RD (2004) Adherence to pharmacotherapy in patients with alcohol and opioid dependence. Addiction 99:1382–1392
Woon LS, Hazli Z, Gan LLY (2018) Pharmacotherapy for comorbid adult attention-deficit hyperactivity disorder and stimulant dependence: a systematic review. International Medical Journal Malaysia 17:149–161
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to disclose.
Ethical approval
The present article does not necessarily express the view of the United Nations.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tardelli, V.S., Bisaga, A., Arcadepani, F.B. et al. Prescription psychostimulants for the treatment of stimulant use disorder: a systematic review and meta-analysis. Psychopharmacology 237, 2233–2255 (2020). https://doi.org/10.1007/s00213-020-05563-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-020-05563-3