Abstract
Rationale
Histamine H3 receptors (H3Rs) are co-expressed with dopamine D1 receptors (D1Rs) by striato-nigral medium spiny GABAergic neurons, where they functionally antagonize D1R-mediated responses.
Objectives and methods
We examined whether the chronic administration of the H3R agonist immepip modifies dyskinesias induced by l-3,4-dihydroxyphenylalanine, l-Dopa (LIDs), in rats lesioned with 6-hydroxydopamine in the substantia nigra pars compacta, and the effect of D1R and H3R co-activation on glutamate and GABA content in dialysates from the dorsal striatum of naïve rats.
Results
The systemic administration (i.p.) of l-Dopa for 14 days significantly increased axial, limb, and orolingual abnormal involuntary movements (AIMs) compared with the vehicle group. The chronic administration of the H3R agonist immepip alongside l-Dopa significantly decreased axial, limb, and orolingual AIMs compared with l-Dopa alone, but AIMs returned to previous values on immepip withdrawal. Chronic immepip was ineffective when administered prior to l-Dopa. The chronic administration of immepip significantly decreased GABA and glutamate content in striatal dialysates, whereas the administration of l-Dopa alone increased GABA and glutamate content.
Conclusions
These results indicate that chronic H3R activation reduces LIDs, and the effects on striatal GABA and glutamate release provide evidence for a functional interaction between D1Rs and H3Rs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parkinson’s disease, the second most common neurodegenerative disease worldwide (Connolly and Lang 2014), is originated by the progressive loss of dopaminergic neurons located in the substantia nigra pars compacta, SNc (Surmeier et al. 2017), one of the neuronal nuclei that form the basal ganglia, a group of sub-cortical structures critically involved in the learning and execution of motor programs (Bolam et al. 2000). Although no available therapies modify the underlying neurodegenerative process, symptomatic treatment improves the patient quality of life (Connolly and Lang 2014). In spite of new therapeutic strategies, the administration of l-3,4-dihydroxyphenylalanine (l-Dopa) remains the most effective symptomatic treatment of Parkinson’s disease. However, the majority of patients eventually develop dyskinesia, abnormal involuntary movements (AIMs) related to long-term l-Dopa administration (Ahlskog and Muenter 2001; Bastide et al. 2015; Hely et al. 2005; Huot et al. 2013).
l-Dopa-induced dyskinesias (LIDs) are related to increased striatal dopamine levels, alterations in the cellular distribution of dopamine D1 receptors (D1Rs), sensitization of their intracellular signaling and abnormal gene expression in D1R-expressing neurons, leading to changes in basal ganglia dopaminergic transmission at the pre- and post-synaptic levels (Bastide et al. 2015; Carta and Bezard 2011; Fuente-Fernandez et al. 2004; Porras et al. 2014; Spigolon and Fisone 2018).
The basal ganglia are innervated by histaminergic fibers (Panula et al. 1989), and the striatum, globus pallidus, and substantia nigra pars reticulata (SNr) express a high density of histamine H3 receptors, H3Rs (Pillot et al. 2002). D1Rs and H3Rs are co-expressed by the sub-population of striatal GABAergic medium spiny neurons (MSNs) that originates the direct pathway of the basal ganglia (González-Sepúlveda et al. 2013), and several studies have shown a D1R/H3R functional interaction in these neurons (Arias-Montaño et al. 2001; Garcia et al. 1997; Moreno et al. 2011; Ryu et al. 1994). At the pre-synaptic level, in rat striatum and SNr slices, H3R activation by the agonist immepip selectively inhibited the component of depolarization-evoked [3H]-GABA release that depends on concomitant D1R stimulation (Arias-Montaño et al. 2001; Garcia et al. 1997). At the post-synaptic level, H3R activation inhibits D1R-induced cAMP accumulation (Sanchez-Lemus and Arias-Montano 2004), and D1Rs play a permissive role in H3R-mediated activation of mitogen-activated protein kinases, MAPKs (Moreno et al. 2011).
A previous study reported that the systemic administration of a single dose of immepip (1, 5, and 10 mg/kg, s.c.) did not reduce l-Dopa-induced axial, lingual, or oral AIMs in rats lesioned with 6-hydroxydopamine (6-OHDA) in the SNc (Papathanou et al. 2014). However, these authors mention that in common marmosets lesioned with 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MTPT) and primed with l-Dopa, immepip produced a marked decrease in motor disability and the onset of moderate dyskinesia, although the study generated limited behavioral data because immepip and other H3R agonist, imetit (1, 5 or 10 mg/kg, s.c.), produced retching and vomiting that disrupted motor behavior. Because this study only explored the effect of single doses of H3R agonists, both in rats and marmosets, we have studied whether the chronic administration (14 days) of a low dose of immepip (1 mg/kg, i.p.) could have beneficial effect on LIDs in rats unilaterally lesioned with 6-OHDA in the SNc.
Materials and methods
Subjects
Adult male Wistar rats (280–310 g), provided by the UPEAL-Bioterio of UAM-Xochimilco, were acclimatized to laboratory conditions and maintained on a 12-h/12-h light/dark cycle. All experimental procedures were conducted in accordance with the recommendations of the Guide for the Care and Use of Experimental Animals (Olfert et al. 1993). We used the minimum possible number of animals needed according to the bioethical and statistical criteria established by Festing (1994), and all procedures were approved by the Animal Care Committee of Instituto Nacional de Rehabilitación.
6-OHDA lesion
Rats were anesthetized with a mixture of ketamine-xylazine (80–10 mg/kg; i.p.) and positioned in a stereotaxic frame (Stoelting Corp., Wood Dale, IL). The skull was exposed, and a trephine hole (~ 1 mm diameter) was drilled according to the following coordinates (mm): anteroposterior (AP), − 5 mm from bregma; lateral (L), − 2 mm from the midline; and vertical (V), 7.2 mm below the duramadre (Paxinos and Watson 2007). For the SNc lesion, 6-OHDA (8 μg/μl of saline solution containing 0.1% ascorbic acid) was injected unilaterally at a flow rate of 0.4 μl/min for 5 min using an injection pump (CMA/400, CMA/Microdialysis, Kista, Sweden), and the needle (30 gauge) was left in place for 5 min before being withdrawn. Two weeks after the lesion, animals were tested for contralateral rotation in response to the systemic administration of apomorphine hydrochloride (0.5 mg/kg, s.c.). Only rats with six or more contralateral turns per min, were included in the study.
Experimental design
Experiment 1
Sixty hemi-parkinsonian rats were divided into the following six groups (10 animals per group): (a) the vehicle group received a daily intraperitoneal (i.p.) injection of saline solution for 14 days (vehicle); (b) the l-Dopa alone group received a daily dose of carbidopa (15 mg/kg) followed by l-Dopa (6.25 mg/kg) 20 min later, for 14 days; (c) the acute immepip group received a daily dose of l-Dopa for 14 days and a daily injection of the H3R agonist immepip (1 mg/kg; i.p.) on days 12, 13, and 14 (l-Dopa + immepip/acute); (d) the subchronic immepip group received a daily dose of l-Dopa for 14 days and a daily injection of immepip on day 8 and thereafter for 7 consecutive days (l-Dopa + immepip/subchronic); (f) the chronic immepip group received a daily dose of l-Dopa + immepip for 14 days (l-Dopa + immepip/chronic); (g) the pre-treatment immepip group received a daily dose of l-Dopa for 14 days and a daily injection of immepip 5 days before the first l-Dopa dose, and thereafter for 19 days (l-Dopa + immepip/pre-treatment).
Experiment 2
Eight rats were used to confirm the effects of the chronic administration of immepip + l-Dopa for 14 days, but on day 15, immepip was withdrawn. Thereafter, rats received a daily dose of l-Dopa alone for 7 consecutive days.
Experiment 3
For the quantification of GABA and glutamate contents in striatal dialysates, 20 hemi-parkinsonian rats underwent the treatments described in ‘Experiment 1’, and at day 14 were divided into the following five groups (4 animals per group): (1) parkinsonian; (2) l-Dopa alone; (3) acute immepip group; (4) subchronic immepip; (5) chronic immepip. A sham group (non-lesioned rats) was included to examine the effect of a single dose of l-Dopa at day 15.
Behavioral analysis
AIMs were evaluated with a previously validated scale (Andersson et al. 1999; Cenci et al. 1998; Johansson et al. 2001; Lundblad et al. 2002; Papathanou et al. 2014), according to which AIMs are classified into four subtypes: axial, limb, orolingual, and locomotive. Each AIM subtype was scored on a scale from 0 to 4, based on the following criteria: 0 = not present; 1 = present during less than half of the observation time; 2 = present during more than half of observation time; 3 = present all the time, but suppressible by threatening stimuli; 4 = present all the time and not suppressible. AIMs were scored daily and counted for 1 min every 20 min from 20 to 120 min after drug or vehicle administration. In each session, the AIM scores obtained in the six observation recordings were summed (maximum score 24) and expressed per subtype (axial, limb, or orolingual) or the sum of the three subtypes (ALO, maximum score 72). Locomotive dyskinesia was excluded from the analysis because its interpretation is still controversial (Cenci et al. 1998). For total AIMs per subtype, each AIM (axial, limb, orolingual, or locomotive) was counted and then summed per session. For total AIMs per subtypes, ALO were summed, excluding locomotive dyskinesia. All rats were videotaped during the test, and an investigator blind to the treatment reviewed the videotapes (see Supplementary videos).
Microdialysis and HPLC analysis
Striatal microdialysis was performed as previously reported (Alfaro-Rodriguez et al. 2013). After completion of the treatments described above (day 14), a guide cannula was implanted into the striatum according to the following coordinates (mm): AP + 0.24 mm from bregma, L + 2.8 mm from the midline, DV 6.8 mm below the duramadre (Paxinos and Watson 2007). After the surgery, animals were housed individually and allowed to recover for 20–24 h. For the microdialysis experiments, the probe was continuously perfused (30 min) with Ringer’s solution (in mM: 146 NaCl, 4 KCl, 1.2 CaCl2, 2 NaH2PO4; pH 7.4 with NaOH) at a flow rate of 1.25 μl/min using an injection pump (CMA/400, CMA/Microdialysis, Kista, Sweden) coupled to a system for freely moving animals (CMA/120, CMA/Microdialysis AB, Kista, Sweden). The probe had an outer diameter of 0.5 mm and contained a polycarbonate membrane (molecular weight cutoff 20 kDa). The length of the exposed part of the probe was 4 mm. The dialysis probe was carefully inserted, and the rat was then placed in the system for freely moving animals. After 90–120 min of stabilization, dialysate samples were collected in a refrigerated fraction collector (CMA/470, CMA/Microdialysis AB, Kista, Sweden) every 30 min for 180 min. After collection, samples were injected into a high-performance liquid chromatograph (HPLC).
GABA and glutamate contents were determined as reported in detail elsewhere (Montes et al. 2003), using an HPLC system (Alltech, binary HPLC pump, model 626, Grace Discovery Science, Deerfield, IL) coupled to a fluorescence detector (Linear Fluor LC-305, ESA, Chelmsford, MA) with an Adsorbosphere OPA column (Alltech, Adsorbosphere OPA HS, 100 × 4.6 mm, 5-μm particle size). The mobile phase consisted of sodium acetate buffer (50 mM, pH 3.2) containing 1.5% tetrahydrofuran, and HPLC-grade methanol. Separation was achieved with a linear gradient of 20 min from 10 to 65% methanol. Pre-column derivatization was performed by mixing 37.5 μl of sample and 37.5 μl of ortho-phthalaldehyde reagent (5 mg ortho-phthalaldehyde dissolved in a mixture of 625 μl methanol, 5.6 ml borate buffer, pH 9.5, and 25 μl mercaptoethanol). The concentrations of GABA and glutamate were calculated by interpolation of the sample chromatograms to the chromatograms from five standards of known concentrations of GABA or glutamate.
Drugs
The following drugs were purchased from Sigma-Aldrich (St. Louis, MO): immepip dihydrobromide, 3,4-dihidroxy-l-phenylalanine (l-Dopa), S-(-)-carbidopa, 6-hydroxydopamine hydrobromide, and apomorphine hydrochloride.
Statistical analysis
All values are expressed as means ± standard error (SEM). The statistical analysis of AIM scores was performed with the nonparametric Kruskal-Wallis test followed by Mann-Whitney U test to compare the mean rank of the treatment groups. The analysis of total AIMs was performed with repeated-measures ANOVA followed by Bonferroni’s post hoc test to compare the means of the drug treatment groups. The analysis of AIM scores from the chronic immepip/withdrawal group was performed with the Wilcoxon test for repeated measures to compare the ranks of means between drug treatments, and the analysis of total AIMs was performed with Student’s t test. Differences were regarded statistically significant at P < 0.05.
Results
AIM expression
In the l-Dopa alone group, dyskinetic effects were observed in all rats, with scores within the range 1–3. In the chronic immepip group, dyskinesias were observed in 35% of rats, with scores in the range 0–1. In the subchronic and acute immepip groups, dyskinetic effects were observed in 100% of rats, with scores 1–2. In the pre-treatment immepip group, these effects were observed in all animals, with scores 0–2. In the vehicle group, dyskinetic effects were not observed in any animal.
Effect of the chronic administration of immepip on LIDs
Figures 1, 2, 3, and 4 show that the daily systemic administration of l-Dopa alone for 14 days significantly increased (P < 0.05) the AIM scores and total AIMs for the four subtypes analyzed (axial, limb, orolingual, and locomotive) at days 3, 6, 9, 12, and 14 in comparison with the respective vehicle group (daily injection of saline solution for 14 days). These data indicate that the dose of l-Dopa tested in this study (6.25 mg/kg) resulted in LIDs in 6-OHDA-lesioned rats with high reproducibility.
Effect of the systemic administration of the H3R agonist immepip (1 mg/kg) on axial AIM scores (A) and total axial AIMs (B) induced by l-Dopa (6.25 mg/kg; carbidopa 15 mg/kg). The acute immepip group received a daily dose of immepip for 3 consecutive days from day 12. The sub-chronic immepip group received a daily dose of immepip 7 consecutive days from day 8. The chronic immepip group received a daily dose of immepip for 14 consecutive days (days 1–14). All values are expressed as means ± SEM. In each session per day, the axial AIM scores received in the six observation points were summed (A), whereas for total axial AIMs, each axial AIM was counted and then summed per session (B). The statistical analysis of AIM scores was performed with the nonparametric Kruskal-Wallis test, followed by the Mann-Whitney U test to compare the mean rank of the drug treatment groups. The analysis of total AIMs was performed with repeated-measures ANOVA followed by Bonferroni’s post hoc test to compare the means of the drug treatment groups. The insert shows the comparison of the l-Dopa, l-Dopa + immepip and l-Dopa + chronic immepip groups. *, #P < 0.05; **, ##P < 0.01; ***P < 0.0001; when compared with l-Dopa
Effect of the systemic administration of the H3R agonist immepip (1 mg/kg) on limb AIM scores (A) and total limb AIMs (B) induced by l-Dopa (6.25 mg/kg; carbidopa 15 mg/kg). Drug administration was as described for Fig. 1. All values are expressed as the mean ± SEM. In each session per day, the limb AIM scores received in the six observation points were summed (A), whereas for total limb AIMs, each limb AIM was counted and then summed per session (B). The statistical analysis was performed as described for Fig. 1. The insert shows the comparison of the l-Dopa, l-Dopa + immepip, and l-Dopa + chronic immepip groups. *P < 0.05; **, ##P < 0.01; ***, ###P < 0.0001; when compared with l-Dopa
Effect of the systemic administration of the H3R agonist immepip (1 mg/kg) on orolingual AIM scores (A) and total orolingual AIMs (B) induced by l-Dopa (6.25 mg/kg; carbidopa 15 mg/kg). Drug administration was as described for Fig. 1. All values are expressed as means ± SEM. In each session per day, the orolingual AIM scores received in the six observation points were summed (A), whereas for total orolingual AIMs, each orolingual AIM was counted and then summed per session (B). The statistical analysis was performed as described for Fig. 1. The insert shows the comparison of the l-Dopa, l-Dopa + immepip, and l-Dopa + chronic immepip groups. *, #P < 0.05; **, ##P < 0.01; ***, ###P < 0.0001; when compared with l-Dopa
Effect of the systemic administration of the H3R agonist immepip (1 mg/kg) on locomotive AIM scores (A) and total locomotive AIMs (B) induced by l-Dopa (6.25 mg/kg; carbidopa 15 mg/kg). Drug administration was as described for Fig. 1. All values are expressed as means ± SEM. In each session per day, the locomotive AIM scores received in the six observation points were summed (A), whereas for total locomotive AIMs, each locomotive AIM was counted and then summed per session (B). The statistical analysis was performed as described for Fig. 1. The insert shows the comparison of the l-Dopa, l-Dopa + immepip, and l-Dopa + chronic immepip groups. **P < 0.01; ***P < 0.0001; when compared with l-Dopa
Figure 1a shows that the chronic administration of immepip (a daily dose of l-Dopa + immepip for 14 days) significantly decreased axial AIM scores (− 79, − 71, − 84, − 89, and − 90% at 3, 6, 9, 12, and 14 days, respectively; P < 0.01 for all values) compared with the l-Dopa alone group. The subchronic and acute administration of immepip did not affect axial AIM scores compared with the corresponding l-Dopa alone group. In contrast, pre-treatment with immepip significantly decreased axial AIMs (− 83, − 42, and − 32% at 3, 6, and 9 days, respectively; P < 0.01 for all values; Fig. 1a) compared with the l-Dopa alone group, indicating that the anti-dyskinetic affect was present only at the initial time points. The administration of immepip alone on days − 5 and − 2 did not produce a significant effect on axial AIM scores and total AIMs (Fig. 1a, b).
Figure 1b shows that the chronic administration of immepip (l-Dopa + immepip for 14 days) significantly decreased total axial AIMs (− 76, − 70, − 78, − 80, and − 86% at 3, 6, 9, 12, and 14 days, respectively; P < 0.05 for all values) compared with the l-Dopa alone group. In contrast, the chronic administration of immepip + l-Dopa did not produce a significant effect on total axial AIMs at 3, 6, 9, 12, and 14 days compared with the vehicle group. The subchronic and acute administration of immepip had no significant effect on total axial AIMs compared with the l-Dopa alone group. An anti-dyskinetic effect was observed for the pre-treatment with immepip, which significantly decreased total axial AIMs (− 94 and − 74% at 3 and 6 days, respectively; P < 0.05 for both values) compared with the l-Dopa alone group (Fig. 1b).
Figure 2a shows that the chronic administration of immepip significantly decreased limb AIM scores (− 69, – 70, − 83, − 82, and − 83% at 3, 6, 9, 12, and 14 days, respectively; P < 0.01 for all values) compared with the l-Dopa alone group. The subchronic and acute administration of immepip did not affect limb AIM scores compared whit the l-Dopa alone group. The administration of immepip alone on days − 5 and − 2 did not produce a significant effect on limbic AIM scores and total AIMs (Fig. 2a, b), but an anti-dyskinetic effect was observed at days 3 and 6 with a significant decrease in AIMs (− 85 and − 43%, respectively; P < 0.01 for both values) compared with the l-Dopa alone group (Fig. 1a).
With respect to total limb AIMs, the chronic immepip group showed a significant decrease in limb AIMs (− 76, − 74, − 80, − 84 and − 82% at 3, 6, 9, 12, and 14 days, respectively; P < 0.0001 for all values; Fig. 2b) compared with the l-Dopa alone group, but no difference with the vehicle group. The subchronic and acute administration of immepip did not produce a significant difference in total limb AIMs compared with the l-Dopa alone group (Fig. 2b). However, pre-treatment with immepip significantly decreased total limb AIMs (− 95 and − 63% at 3 and 6 days, respectively; P < 0.0001 for both values; Fig. 2b) compared with the l-Dopa alone group, indicating that the anti-dyskinetic effect was produced only at the initial time points.
As shown in Fig. 3a, the chronic administration of immepip significantly decreased orolingual AIM scores (− 75, − 69, − 68, − 89, and − 82% at 3, 6, 9, 12, and 14 days, respectively; P < 0.01 for all values) compared with the l-Dopa alone group. The administration of immepip alone on days − 5 and − 2 did not produce a significant effect on orolingual AIM scores and total AIMs, but on days 3 and 6, an anti-dyskinetic effect was observed with a significant decrease in orolingual AIMs (− 86 and − 51%, respectively; P < 0.05 for both values; Fig. 3a) compared with the l-Dopa alone group.
Figure 3b shows that in the chronic immepip group, there was a significant decrease in total orolingual AIMs (− 87, − 83, − 82, − 86, and − 77% at 3, 6, 9, 12, and 14 days, respectively; P < 0.01 for all values) compared with the l-Dopa alone group, but no significant difference when compared with the vehicle group. The subchronic and acute administration of immepip did not affect total orolingual AIMs compared with the corresponding l-Dopa alone groups. However, pre-treatment with immepip significantly decreased total orolingual AIMs (− 96 and − 73% at 3 and 6 days, respectively; P < 0.001 for both values; Fig. 3b) compared with the l-Dopa alone group.
Figure 4a and b show that the chronic administration of immepip + l-Dopa did not affect the locomotive AIM scores and total AIMs compared with the respective l-Dopa alone groups. The acute administration significantly increased the locomotive AIM scores (69, 83, 87, and 68% at 3, 6, 12, and 14 days, respectively; P < 0.05 for all values; Fig. 4a), whereas the subchronic administration had no significant effect compared with the l-Dopa group. Furthermore, the administration of immepip alone on days − 5 and − 2 had no significant effect on locomotive AIM scores and total AIMs, and the concomitant administration with l-Dopa at 3, 6, 9, 12, and 14 days failed to affect locomotive AIM scores and total AIMs (Fig. 4a, b) compared with the vehicle group. The chronic administration of immepip + l-Dopa did not produce a significant effect on total locomotive AIMs at 3, 6, 9, 12, and 14 days compared with the vehicle group (Fig. 4b). The subchronic and acute administration of immepip did not produce a significant difference in total locomotive AIMs compared with the l-Dopa alone group (Fig. 4b).
As shown in Fig. 5a, the chronic administration of immepip significantly decreased ALO AIM scores (− 75, − 70, − 80, − 86, and − 84% at 3, 6, 9, 12, and 14 days, respectively; P < 0.01 for all values) compared with the l-Dopa alone group. The administration of immepip alone on days − 5 and − 2 did not produce a significant effect on ALO AIM scores and total ALO AIMs, but on days 3 and 6 showed an anti-dyskinetic effect with a significant decrease in ALO AIM scores (− 85 and − 45%, respectively; P < 0.05 for both values; Fig. 5a) compared with the l-Dopa alone group. Figure 5b shows that the chronic immepip group presented a significant decrease in total ALO AIMs (− 79, − 77, − 81, − 85, and − 80% at 3, 6, 9, 12, and 14 days, respectively; P < 0.001 for all values) compared with the l-Dopa alone group, but no significant difference with the vehicle group.
Effect of the systemic administration of the H3R agonist immepip (1 mg/kg) on ALO AIM scores (A) and total ALO AIMs (B) induced by l-Dopa (6.25 mg/kg; carbidopa 15 mg/kg). Drugs administration was as described for Fig. 1. All values are expressed as means ± SEM. In each session per day, the ALO AIM scores received in the six observation points were summed (A), whereas for total ALO AIMs, each ALO AIM was counted and then summed per session (B). The statistical analysis was performed as described for Fig. 1. The insert shows the comparison of the l-Dopa, l-Dopa + immepip, and l-Dopa + chronic immepip groups. *P < 0.05; **P < 0.01; ***, ###P < 0.0001; when compared with l-Dopa
The subchronic and acute administration of immepip did not affect ALO AIM scores compared whit the corresponding l-Dopa alone groups. However, pre-treatment with immepip significantly decreased total ALO AIMs (− 95 and − 70% at 3 and 6 days, respectively; P < 0.001 for both values; Fig. 5b) compared with the l-Dopa alone group, indicating that the anti-dyskinetic effect was produced only at the initial time points.
Effect of the withdrawal of chronic immepip administration on LIDs
Figure 6 shows that immepip withdrawal significantly increased axial AIMs (265, 233, 244, and 223% at 16, 18, 20, and 21 days, respectively; P < 0.02 for all values; Fig. 6a), limb AIMs (135, 155, 140, and 124% at 16, 18, 20, and 21 days, respectively; P < 0.02 for all values; Fig. 6c), orolingual AIMs (325, 313, 300, and 350% at 16, 18, 20, and 21 days, respectively; P < 0.02 for all values; Fig. 6e) and locomotive AIMs (180, 170, and 170% at 18, 20, and 21 days, respectively; P < 0.05 for all values; Fig. 6g) scores compared with l-Dopa + immepip for 3, 6, 9, 12, and 14 days.
Effect of the systemic administration for 7 consecutive days of l-Dopa (6.25 mg/kg; carbidopa 15 mg/kg) after immepip withdrawal on day 15, on axial (A), limb (C), orolingual (E), and locomotive (G) AIM scores and the respective total AIMs (B, D, F, H). The chronic immepip group received a daily dose of l-Dopa + immepip for 14 days (l-Dopa + immepip/chronic). All values are expressed as means ± SEM. In each session per day, the AIM scores received in the five observation points were summed and represented per subtype, whereas for total AIMs per subtype, each AIM was counted and then summed per session. The statistical analysis of AIMs scores was performed with Wilcoxon test. The insert shows the comparison of total AIMs between the l-Dopa + immepip and l-Dopa groups. The bars correspond to the means ± SEM of AIM scores and total AIMs from days 3, 6, 9, 12, and 14 for the withdrawal of chronic immepip (l-Dopa + immepip), and days 16, 18, 20, and 21 for the after-withdrawal of chronic immepip (l-Dopa alone). The statistical analysis was performed with the Wilcoxon test (A, C, E, and G) or Student’s t test (B, D, F, and H). *P < 0.05; **P < 0.01; ***P < 0.0001; when compared with l-Dopa + immepip values
For total AIMs, the systemic administration of l-Dopa alone after immepip withdrawal significantly increased axial AIMs (265, 256, 190, and 226% at 16, 18, 20, and 21 days, respectively; P < 0.02 for all values; Fig. 6b), limb AIMs (85, 121, 107, and 92% at 16, 18, 20, and 21 days, respectively; P < 0.05 for all values; Fig. 6d), orolingual AIMs (482, 709, 468, and 501% at 16, 18, 20, and 21 days, respectively; P < 0.001 for all values; Fig. 6f), and locomotive AIMs (179% at 20 day; P < 0.05; Fig. 6h) compared with the l-Dopa + immepip values from 3, 6, 9, 12, and 14 days.
Effect of immepip on GABA and glutamate contents in striatal dialysates
In the l-Dopa alone group, the systemic administration of l-Dopa (6.25 mg/kg) on day 15 significantly increased glutamate levels in striatal dialysates to 150, 134, and 127% of the values for the parkinsonian rats that received the same treatment, at 120, 150, and 180 min, respectively (P < 0.05 for all values; Fig. 7a). A similar effect was observed for GABA levels (195, 185, and 176% of the values for the parkinsonian rats, at 120, 150, and 180 min, respectively; P < 0.05 for all values; Fig. 7b). In contrast, in the chronic immepip + l-Dopa group, l-Dopa administration significantly decreased striatal glutamate levels compared with the parkinsonian rats (− 40, − 41, and − 35% at 120, 150, and 180 min, respectively; P < 0.05 for all values; Fig. 7a), whereas striatal GABA levels were not affected (Fig. 7b).
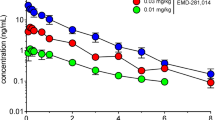
Effect of the systemic administration of the H3R agonist immepip (1 mg/kg) on glutamate (A) and GABA (B) release in the striatum. Values are expressed as means ± SEM. The sham, parkinsonian, and l-Dopa groups received a single dose of l-Dopa (6.25 mg/kg; carbidopa 15 mg/kg). The acute, subchronic, and chronic immepip groups received single doses of l-Dopa and immepip (1 mg/kg). All drugs were administered at min 87, except for carbidopa, administered at min 67. All values are expressed as means ± SEM. The statistical analysis was performed with the nonparametric Kruskal-Wallis test, followed by Mann-Whitney U test to compare the mean rank of the drug treatment groups. *P < 0.05; when compared with parkinsonian values. #P < 0.05; when compared with chronic immepip values
Discussion
The main finding of this study is that the chronic administration of the H3R agonist immepip reduces LIDs in 6-OHDA-lesioned rats.
In agreement with the report of Papathanou et al. (2014), who showed that in 6-OHDA-lesioned rats, a single dose of immepip had no effect on LIDs, in our study, the acute administration of immepip failed to modify LIDs in 6-OHDA-lesioned rats. Likewise, a high dose of immepip or imetit (10 mg/kg) significantly decreased l-Dopa-induced chorea, but had no effect on motor disability and dyskinesia in marmosets lesioned with MPTP (Gomez-Ramirez et al. 2006). In spite of the lack of effect on LIDs, the systemic administration of imetit (5 mg/kg) decreased l-Dopa-induced dopamine release in the striatum of 6-OHDA-lesioned rats, and reduced stereotyped behaviors induced by l-Dopa (Nowak et al. 2008), indicating that acute H3R activation opposes l-Dopa-induced dopaminergic transmission but not LIDs, presumably due to the presence of chronic alterations in dopaminergic transmission induced by l-Dopa, as discussed below.
In contrast to the acute administration, immepip decreased axial, orolingual, and limb AIMs when it was co-administered with l-Dopa from day 1 (chronic administration), although not when administered afterwards (subchronic and acute groups, administered at days 8 and 12, respectively), when LIDs were already established. These results suggest that immepip acts to prevent the generation of LIDs and is thus ineffective once LIDs are established.
Related to the differences between dyskinetic and non-dyskinetic animals, patients with Parkinson’s disease who developed LIDs showed increased striatal dopamine levels after the administration of l-Dopa in comparison to stable responders, and the observed difference correlated positively with the duration of symptoms for the caudate and putamen nuclei (De la Fuente-Fernandez et al. 2004). The increase in dopamine levels could therefore be associated to the reduction of the dopamine transporter (DAT) reported by Pagano et al. (2017), which leads to increased dopamine concentrations in the extracellular space.
Chronic l-Dopa administration induces D1R sensitization in the striatal projection neurons of the direct pathway, leading to excessive D1R signaling that through protein kinase A (PKA) and the cAMP-regulated protein of 32 kDa (DARPP-32) promotes the activation of additional intracellular signaling cascades resulting in abnormal gene expression (Spigolon and Fisone 2018). Accordingly, in severe-dyskinetic rats, but not in mild-dyskinetic animals, the chronic administration of l-Dopa increases D1R-mediated cAMP formation and depolarization-evoked [3H]-GABA release in slices of the SNr ipsilateral to 6-OH-lesioned pars compacta. Furthermore, in animals with mild dyskinesia, l-Dopa restored the content of adenylyl cyclase (type V/VI) in the 6-OH-DA-lesioned SNr, but had no effect in rats with severe dyskinesia (Rangel-Barajas et al. 2011).
The ineffectiveness of the acute administration of immepip to modify LIDs (Papathanou et al. 2014) could therefore rely on the previous generation of pre- and post-synaptic changes induced by chronic l-Dopa administration. However, if immepip is administered before the development of dyskinesias, as showed for the chronic immepip group, H3R activation was effective. This hypothesis is supported by the appearance of LIDs after the withdrawal of immepip administration (Fig. 6).
D1Rs and H3Rs are expressed by the MSNs of the direct pathway (González-Sepúlveda et al. 2013), both in their bodies and the axon terminals, and a functional interaction between these receptors has been reported by several studies (Arias-Montaño et al. 2001; Garcia et al. 1997; Moreno et al. 2011; Rapanelli 2017; Ryu et al. 1994). Pre-synaptically, in slices from the rat striatum and SNr, H3R activation with immepip selectively inhibited the component of depolarization-evoked [3H]-GABA release that depends on concomitant D1R stimulation (Arias-Montaño et al. 2001; Garcia et al. 1997), and the systemic administration of the H3R agonist imetit (5 mg/kg) decreases l-Dopa-induced dopamine release in the striatum of 6-OHDA-lesioned rats (Nowak et al. 2008), presumably by activating H3Rs located on striatal dopaminergic terminals (Schlicker et al. 1993).
Post-synaptically, H3R activation reduces D1R-induced cAMP formation (Sanchez-Lemus and Arias-Montano 2004). Furthermore, H3Rs can form heterodimers with D1Rs and heteroreceptor complexes with D1Rs and glutamate N-methyl-d-aspartate (NMDA) receptors. Whereas in the D1R/H3R dimer, H3R activation reduces D1R affinity for selective agonists and shifts the coupling of D1Rs from Gαs to Gαi/o proteins (Ferrada et al. 2009; Moreno et al. 2011); in the D1R/H3R/NMDA receptor complex, H3R activation prevents ERK-1/2 phosphorylation induced by D1R stimulation (Rodriguez-Ruiz et al. 2017).
Unexpectedly, our results showed that the administration of immepip alone (1 mg/kg) for 5 consecutive days prior to l-Dopa did not reduce axial, limb, orolingual, and locomotive AIM scores or total AIMs (Figs. 1, 2, 3, 4, and 5). We do not have an explanation for this result, but one possibility is that the continuous activation of H3Rs in the absence of D1R stimulation leads to desensitization of post-synaptic H3Rs, a phenomenon showed for transfected receptors by our group (Garcia-Galvez et al. 2018; Osorio-Espinoza et al. 2014).
In the microdialysis experiments, the systemic injection of l-Dopa (6.25 mg/kg; carbidopa 15 mg/kg) to animals of the l-Dopa alone group significantly increased striatal GABA and glutamate release compared with parkinsonian rats.
The increase in GABA release is consistent with the enhanced depolarization-induced [3H]-GABA release from SNr slices of dyskinetic rats (Rangel-Barajas et al. 2011), correlates with the increased AIMs in our study, and can be explained by the sensitization of D1R signaling (Fig. 8c). The chronic administration of immepip prevented the l-Dopa effect and can be associated with the functional interaction between H3Rs and D1Rs discussed before (Arias-Montaño et al. 2001; Garcia et al. 1997; Moreno et al. 2011; Rapanelli 2017).
Schematic representation of the basal ganglia synaptic circuitry in normal conditions (A), parkinsonism (B), the dyskinetic state (C), and the proposed action of the chronic administration of the H3R agonist immepip (D). Red lines indicate excitatory projections and black lines inhibitory projections. Dotted lines indicate dopaminergic depletion in the substantia nigra pars compacta (SNc). The striatum communicates with neurons in the substantia nigra pars reticulata (SNr) through a direct pathway, and to the external segment of the globus pallidus (GPe), which in turn projects to the subthalamic nucleus (STN) that projects to the SNr, forming the indirect pathway
The increase in glutamate release is in accord with the enhancement in glutamatergic transmission reported previously (Huot et al. 2013). Increased extracellular glutamate concentration and changes in the subcellular distribution of glutamate receptor subunits have also been associated with the development and expression of LIDs (Pagano et al. 2017) (Fig. 8c). The classic model of basal ganglia function (Albin et al. 1989) suggests that overactivity of glutamatergic cortico-striatal projections is critical for the hyperactivity of striato-nigral neurons that form the basal ganglia direct pathway (Fig. 8c). H3R activation inhibits glutamate release from cortico-striatal and thalamo-striatal nerve terminals (Doreulee et al. 2001; Ellender et al. 2011; Molina-Hernandez et al. 2001), and this effect could explain the effect of the immepip administration. Of note, whereas the acute and sub-chronic immepip administration only prevented the effect of l-Dopa, the chronic administration reduced glutamate levels to values below basal. One explanation for the latter effect could be the inhibition of the cortico-striatal pathway (Fig. 8d), which is highly dominant in the modulation of the activity of striatal neurons compared with the thalamo-cortical pathway (Ding et al. 2008; Silberberg and Bolam 2015; Smith et al. 2004).
Conclusion
Our results indicate that the chronic administration of the H3R agonist immepip prevents LIDs in 6-OHDA-lesioned rats, and that this effect requires the continuous administration of the agonist. The effect of immepip appears to rely on the H3R-mediated inhibition of D1R stimulatory actions on GABA and glutamate release in the striatum. These findings can contribute to the understanding of the role of D1Rs and H3Rs in the dysfunction of the basal ganglia that occurs in neurodegenerative diseases involving disturbances of the dopaminergic system.
References
Ahlskog JE, Muenter MD (2001) Frequency of levodopa-related dyskinesias and motor fluctuations as estimated from the cumulative literature. Mov Disord 16:448–458
Albin RL, Young AB, Penney JB (1989) The functional-anatomy of basal ganglia disorders. Trends Neurosci 12:366–375
Alfaro-Rodriguez A, Alonso-Spilsbury M, Arch-Tirado E, Gonzalez-Pina R, Arias-Montano J-A, Bueno-Nava A (2013) Histamine H3 receptor activation prevents dopamine D1 receptor-mediated inhibition of dopamine release in the rat striatum: a microdialysis study. Neurosci Lett 552:5–9
Andersson M, Hilbertson A, Cenci MA (1999) Striatal fosB expression is causally linked with L-DOPA-induced abnormal involuntary movements and the associated upregulation of striatal prodynorphin mRNA in a rat model of Parkinson's disease. Neurobiol Dis 6:461–474
Arias-Montaño JA, Floran B, Garcia M, Aceves J, Young JM (2001) Histamine H3 receptor-mediated inhibition of depolarization-induced, dopamine D1 receptor-dependent release of [3H]-gamma-aminobutryic acid from rat striatal slices. Br J Pharmacol 133:165–171
Bastide MF, Meissner WG, Picconi B, Fasano S, Fernagut PO, Feyder M, Francardo V, Alcacer C, Ding YM, Brambilla R, Fisone G, Stoessl AJ, Bourdenx M, Engeln M, Navailles S, De Deurwaerdere P, Ko WKD, Simola N, Morelli M, Groc L, Rodriguez MC, Gurevich EV, Quik M, Morari M, Mellone M, Gardoni F, Tronci E, Guehl D, Tison F, Crossman AR, Kang UJ, Steece-Collier K, Fox S, Carta M, Cenci MA, Bezard E (2015) Pathophysiology of L-dopa-induced motor and non-motor complications in Parkinson’s disease. Prog Neurobiol 132:96–168
Bolam JP, Hanley JJ, Booth PA, Bevan MD (2000) Synaptic organisation of the basal ganglia. J Anat 196(Pt 4):527–542
Carta M, Bezard E (2011) Contribution of pre-synaptic mechanisms to L-DOPA-induced dyskinesia. Neuroscience 198:245–251
Cenci MA, Lee CS, Bjorklund A (1998) L-DOPA-induced dyskinesia in the rat is associated with striatal overexpression of prodynorphin- and glutamic acid decarboxylase mRNA. Eur J Neurosci 10:2694–2706
Connolly BS, Lang AE (2014) Pharmacological treatment of Parkinson disease a review. Jama-J Am Med Assoc 311:1670–1683
De la Fuente-Fernandez R, Sossi V, Huang ZG, Furtado S, Lu JQ, Calne DB, Ruth TJ, Stoessl AJ (2004) Levodopa-induced changes in synaptic dopamine levels increase with progression of Parkinson’s disease: implications for dyskinesias. Brain 127:2747–2754
Ding J, Peterson JD, Surmeier DJ (2008) Corticostriatal and thalamostriatal synapses have distinctive properties. J Neurosci 28:6483–6492
Doreulee N, Yanovsky Y, Flagmeyer I, Stevens DR, Haas HL, Brown RE (2001) Histamine H3 receptors depress synaptic transmission in the corticostriatal pathway. Neuropharmacology 40:106–113
Ellender TJ, Huerta-Ocampo I, Deisseroth K, Capogna M, Bolam JP (2011) Differential modulation of excitatory and inhibitory striatal synaptic transmission by histamine. J Neurosci 31:15340–15351
Ferrada C, Moreno E, Casado V, Bongers G, Cortes A, Mallol J, Canela EI, Leurs R, Ferre S, Lluis C, Franco R (2009) Marked changes in signal transduction upon heteromerization of dopamine D1 and histamine H3 receptors. Br J Pharmacol 157:64–75
Festing MF (1994) Reduction of animal use: experimental design and quality of experiments. Lab Anim 28:212–221
Garcia M, Floran B, Arias-Montaño JA, Young JM, Aceves J (1997) Histamine H3 receptor activation selectively inhibits dopamine D1 receptor-dependent [3H]GABA release from depolarization-stimulated slices of rat substantia nigra pars reticulata. Neuroscience 80:241–249
Garcia-Galvez AM, Escamilla-Sanchez J, Flores-Maldonado C, Contreras RG, Arias JM, Arias-Montano JA (2018) Differential homologous desensitization of the human histamine H-3 receptors of 445 and 365 amino acids expressed in CHO-K1 cells. Neurochem Int 112:114–123
Gomez-Ramirez J, Johnston TH, Visanji NP, Fox SH, Brotchie JM (2006) Histamine H3 receptor agonists reduce L-dopa-induced chorea, but not dystonia, in the MPTP-lesioned nonhuman primate model of Parkinson’s disease. Mov Disord 21:839–846
González-Sepúlveda M, Rosell S, Hoffmann HM, Castillo-Ruiz MM, Mignon V, Moreno-Delgado D, Michel V, Díaz J, Sabriá J, Ortiz J (2013) Cellular distribution of the histamine H3 receptor in the basal ganglia: functional modulation of dopamine and glutamate neurotransmission. Basal Ganglia 3:109–121
Hely MA, Morris JGL, Reid WGJ, Trafficante R (2005) Sydney multicenter study of Parkinson’s disease: non-L-dopa-responsive problems dominate at 15 years. Mov Disord 20:190–199
Huot P, Johnston TH, Koprich JB, Fox SH, Brotchie JM (2013) The pharmacology of L-DOPA-induced dyskinesia in Parkinson’s disease. Pharmacol Rev 65:171–222
Johansson PA, Andersson M, Andersson KE, Cenci MA (2001) Alterations in cortical and basal ganglia levels of opioid receptor binding in a rat model of L-DOPA-induced dyskinesia. Neurobiol Dis 8:220–239
Lundblad M, Andersson M, Winkler C, Kirik D, Wierup N, Cenci MA (2002) Pharmacological validation of behavioural measures of akinesia and dyskinesia in a rat model of Parkinson’s disease. Eur J Neurosci 15:120–132
Molina-Hernandez A, Nunez A, Sierra JJ, Arias-Montano JA (2001) Histamine H3 receptor activation inhibits glutamate release from rat striatal synaptosomes. Neuropharmacology 41:928–934
Montes S, Alcaraz-Zubeldia M, Muriel P, Rios C (2003) Role of manganese accumulation in increased brain glutamine of the cirrhotic rat. Neurochem Res 28:911–917
Moreno E, Hoffmann H, Gonzalez-Sepulveda M, Navarro G, Casado V, Cortes A, Mallol J, Vignes M, McCormick PJ, Canela EI, Lluis C, Moratalla R, Ferre S, Ortiz J, Franco R (2011) Dopamine D-1-histamine H-3 receptor heteromers provide a selective link to MAPK signaling in GABAergic neurons of the direct striatal pathway. J Biol Chem 286:5846–5854
Nowak P, Bortel A, Dabrowska J, Biedka I, Slomian G, Roczniak W, Kostrzewa RM, Brus R (2008) Histamine H3 receptor ligands modulate L-dopa-evoked behavioral responses and L-dopa-derived extracellular dopamine in dopamine-denervated rat striatum. Neurotox Res 13:231–240
Olfert E, Cross B, Mc William A (1993) Guide for the care and use of experimental animals. Can Council Anim Care 1:211
Osorio-Espinoza A, Escamilla-Sanchez J, Aquino-Jarquin G, Arias-Montano JA (2014) Homologous desensitization of human histamine H3 receptors expressed in CHO-K1 cells. Neuropharmacology 77:387–397
Pagano G, Yousaf T, Politis M (2017) PET molecular imaging research of levodopa-induced dyskinesias in Parkinson’s disease. Curr Neurol Neurosci Reports 17:90
Panula P, Pirvola U, Auvinen S, Airaksinen MS (1989) Histamine-immunoreactive nerve-fibers in the rat-brain. Neuroscience 28:585–610
Papathanou M, Jenner P, Iravani M, Jackson M, Stockwell K, Strang I, Zeng B-Y, McCreary AC, Rose S (2014) The H3 receptor agonist immepip does not affect L-dopa-induced abnormal involuntary movements in 6-OHDA-lesioned rats. Eur J Pharmacol 741:304–310
Paxinos G, Watson C (2007) The rat brain in stereotaxic coordinates, 6th edn. Academic Press, London
Pillot C, Heron A, Cochois V, Tardivel-Lacombe J, Ligneau X, Schwartz JC, Arrang JM (2002) A detailed mapping of the histamine H3 receptor and its gene transcripts in rat brain. Neuroscience 114:173–193
Porras G, De Deurwaerdere P, Li Q, Marti M, Morgenstern R, Sohr R, Bezard E, Morari M, Meissner WG (2014) L-dopa-induced dyskinesia: beyond an excessive dopamine tone in the striatum. Sci Rep 4:3730
Rangel-Barajas C, Silva I, Lopez-Santiago LM, Aceves J, Erlij D, Floran B (2011) L-dopa-induced dyskinesia in hemiparkinsonian rats is associated with up-regulation of adenylyl cyclase type V/VI and increased GABA release in the substantia nigra reticulata. Neurobiol Dis 41:51–61
Rapanelli M (2017) The magnificent two: histamine and the H3 receptor as key modulators of striatal circuitry. Prog Neuro-Psychopharmacol Biol Psychiatry 73:36–40
Rodriguez-Ruiz M, Moreno E, Moreno-Delgado D, Navarro G, Mallol J, Cortes A, Lluis C, Canela EI, Casado V, McCormick PJ, Franco R (2017) Heteroreceptor complexes formed by dopamine D1, histamine H3, and N-methyl-D-aspartate glutamate receptors as targets to prevent neuronal death in Alzheimer’s disease. Mol Neurobiol 54:4537–4550
Ryu JH, Yanai K, Iwata R, Ido T, Watanabe T (1994) Heterogeneous distributions of histamine H3, dopamine D1 and D2 receptors in rat-brain. Neuroreport 5:621–624
Sanchez-Lemus E, Arias-Montano JA (2004) Histamine H3 receptor activation inhibits dopamine D1 receptor-induced cAMP accumulation in rat striatal slices. Neurosci Lett 364:179–184
Schlicker E, Fink K, Detzner M, Gothert M (1993) Histamine inhibits dopamine release in the mouse striatum via presynaptic-H3 receptors. J Neural Transm-Gen Sect 93:1–10
Silberberg G, Bolam JP (2015) Local and afferent synaptic pathways in the striatal microcircuitry. Curr Opin Neurobiol 33:182–187
Smith Y, Raju DV, Pare JF, Sidibe M (2004) The thalamostriatal system: a highly specific network of the basal ganglia circuitry. Trends Neurosci 27:520–527
Spigolon G, Fisone G (2018) Signal transduction in l-dopa-induced dyskinesia: from receptor sensitization to abnormal gene expression. J Neural Transm 125:1171–1186
Surmeier DJ, Obeso JA, Halliday GM (2017) Selective neuronal vulnerability in Parkinson disease. Nat Rev Neurosci 18:101–113
Acknowledgments
We thank MVZ Hugo Lecona Butrón for the support with housing, care, maintenance, and monitoring of the health of the experimental animals at the Instituto Nacional de Rehabilitación Luis Guillermo Ibarra Ibarra. We thank MVZ Javier Pérez Gallaga for the technical support. The authors wish to thank Dr. Ivonne M. Heuze de Icaza for her support with the experimental animals.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Effect of the administration of L-Dopa (6.25 mg/kg) and the co-administration of L-Dopa and the H3R agonist immepip (1 mg/kg) in 6-OHDA-lesioned rats. Note that the administration of immepip reduces LIDs in 6-OHDA-lesioned rats (MP4 38915 kb)
Effects of the chronic administration of immepip+L-Dopa for 14 days, and immepip withdrawal on day 15. Drugs administration was as described for Video 1 (MP4 31326 kb)
Rights and permissions
About this article
Cite this article
Avila-Luna, A., Ríos, C., Gálvez-Rosas, A. et al. Chronic administration of the histamine H3 receptor agonist immepip decreases l-Dopa-induced dyskinesias in 6-hydroxydopamine-lesioned rats. Psychopharmacology 236, 1937–1948 (2019). https://doi.org/10.1007/s00213-019-5182-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-019-5182-y