Abstract
Rationale
Current data indicate that the noradrenergic system plays a critical role in neuropathic pain treatment. Notably, drugs that directly affect this system may have curative potential in neuropathy-associated pain.
Objectives
The aim of this study was to evaluate the potential therapeutic efficacy of reboxetine, a potent and selective noradrenaline reuptake inhibitor, on hyperalgesia and allodynia responses in rats with experimental diabetes. Furthermore, mechanistic studies were performed to elucidate the possible mode of actions.
Methods
Experimental diabetes was induced by a single dose of streptozotocin. Mechanical hyperalgesia, mechanical allodynia, thermal hyperalgesia, and thermal allodynia responses in diabetic rats were evaluated by Randall–Selitto, dynamic plantar, Hargreaves, and warm plate tests, respectively.
Results
Reboxetine treatment (8 and 16 mg/kg for 2 weeks) demonstrated an effect comparable to that of the reference drug, pregabalin, improving the hyperalgesic and allodynic responses secondary to diabetes mellitus. Pretreatment with phentolamine, metoprolol, SR 59230A, and atropine did not alter the abovementioned effects of reboxetine; however, the administration of α-methyl-para-tyrosine methyl ester, propranolol, ICI-118,551, SCH-23390, sulpiride, and naltrindole significantly inhibited these effects. Moreover, reboxetine did not induce a significant difference in the rat plasma glucose levels.
Conclusions
Our findings indicate that the antihyperalgesic and antiallodynic effects of reboxetine are mediated by the catecholaminergic system; β2-adrenoceptors; D1-, D2/D3-dopaminergic receptors; and δ-opioid receptors. The results suggest that this analgesic effect of reboxetine, besides its neutral profile on glycemic control, may be advantageous in the pharmacotherapy of diabetic neuropathy–induced pain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetic neuropathy is a highly complex syndrome that develops solely on the basis of diabetes, affecting the sensory, somatic, and autonomic components of the nervous system (Vinik and Casellini 2013; Singh et al. 2014). Among the most common chronic complications of diabetes mellitus (DM), diabetic neuropathy is one of the leading causes of increased morbidity and mortality in the diabetic population (Barrett et al. 2007).
Neuropathic pain is an important outcome of diabetic neuropathy. Damage to the Aδ and C-type thin nerve fibers due to sustained exposure to hyperglycemia causes symptoms such as hyperalgesia, allodynia, dysesthesia, hyperesthesia, and numbness. Sensory deficits, including hyperalgesia and allodynia, appear at disease onset; however, in the later stages, these deficits may decrease pain sensitization due to neuronal degeneration, demyelination, and axonopathy, especially in patients with poor glycemic control. In addition, damage to the thick Aα and Aβ fibers may also cause symptoms such as diminished vibratory and position senses, reduced tendon reflexes, ataxia, and muscle weakness (Singh et al. 2014).
Ensuring glycemic control with lifestyle changes and appropriate drug therapies are the most effective approaches to prevent diabetes-related neuropathic changes (Pop-Busui et al. 2013; Ang et al. 2014). On the other hand, neuropathy-induced chronic pain is generally drastic for patients, and its relief becomes one of the primary goals of treatment. In clinics, the first-line drugs for the symptomatic treatment of pain are anticonvulsants such as pregabalin and gabapentin, tricyclic antidepressants (TCAs) such as amitriptyline and nortriptyline, and serotonin noradrenaline reuptake inhibitors (SNRI) such as duloxetine and venlafaxine. Furthermore, opioids (tramadol) and topical capsaicin preparations are available pharmacotherapeutic options (Cegielska-Perun et al. 2013). Insufficient efficacy in pain management, development of tolerance, and drug-induced side effects, which are difficult to tolerate, are major challenges limiting the use of clinically prescribed drugs in neuropathic pain treatment (Schreiber et al. 2015). These problems have led to the discovery of newer agents for the pharmacotherapy of neuropathic pain or drug repositioning for the concerned indication.
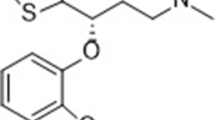
Notably, reboxetine (REB) is a potent and selective inhibitor of noradrenaline reuptake in the synaptic cleft (Preskorn 2004). This molecule was firstly approved in the UK in 1997, for the acute treatment of major depression and as maintenance therapy in patients who respond to the initial treatment. Since approval in 1997, it is available in many European countries such as Austria, Denmark, Finland, Germany, Ireland, Italy, and Sweden (Page 2003; Preskorn 2004). On the other hand, REB has not been approved in the USA due to insufficient evidence of its efficacy in the treatment of depression (Page 2003; Preskorn 2004; Braithwaite 2015).
Although the only indication of REB is major depression, various studies have suggested that REB may have beneficial effects in acute and chronic pain (Schüler et al. 2002; Krell et al. 2005; Schreiber et al. 2009; Hughes et al. 2015). In addition to these studies that emphasize the analgesic potential of REB, it is also evident that the drug may demonstrate effects similar to TCAs and SNRIs in neuropathic pain as it is a selective noradrenaline reuptake inhibitor. Therefore, our study aimed to investigate the potential effect of REB in diabetes-induced neuropathic pain. Following the evaluation of the antihyperalgesic and antiallodynic effects of this drug on diabetic rats, various mechanistic studies were performed to elucidate the mechanisms underlying the demonstrated effects. Due to the potential effects of antidepressants on glycemia, we also investigated the possible effects of REB on plasma glucose levels in diabetic animals.
Materials and methods
Drugs and reagents
Pregabalin, metformin hydrochloride, α-methyl-para-tyrosine methyl ester (AMPT), phentolamine, propranolol, SCH-23390, sulpiride, atropine, and streptozotocin (STZ) used in this study were obtained from Sigma (St. Louis, MO, USA); ICI-118,551, SR 59230A, and naltrindole were procured from Tocris (Bristol, UK); citric acid and trisodium citrate were obtained from Merck (Darmstadt, Germany); and physiological saline solution was from Adeka (Samsun, Turkey). Edronax® (Pfizer, NY, USA) and Beloc® (AstraZeneca, Cambridge, UK) preparations were used for REB and metoprolol, respectively.
Experimental animals
The experiments were conducted using inbred Sprague-Dawley rats (male, 300–350 g) obtained from the Anadolu University Research Unit for Experimental Animals, Eskişehir, Turkey. The animals were maintained in well-ventilated rooms, at a temperature of 24 ± 1 °C under a 12-h light/dark cycle (lights were on between 8:00 and 20:00). The rats were fed standard pellet feeds, with food and water provided ad libitum. The experimental protocol was approved by the Animal Experiments Local Ethics Committee of Anadolu University.
Establishment of streptozotocin-induced experimental diabetes model
STZ, a glucose analog toxic to pancreatic β cells, was used to induce an experimental diabetes model (Lenzen 2008). The rats to be rendered diabetic were fasted overnight and then injected with STZ (50 mg/kg) in 0.1 M citrate buffer (pH = 4.5) through the tail vein. The rats in the control group were intravenously (i.v.) administered an equal volume of citrate buffer. In order to prevent the risk of hypoglycemic shock, water bowls containing 5 mmol/L glucose solution were placed in animal cages after the STZ injection. Blood samples were collected 72 h later, and the measurements were performed with the Accu-Chek® Performa Nano (Roche, Basel, Switzerland) device. Rats with a plasma glucose level higher than 300 mg/dL were categorized as diabetic (Üçel et al. 2015; Aydın et al. 2016; Barbaros et al. 2018).
Rats were housed for 4 weeks after inducing the experimental diabetes model to permit the development of neuropathic pain (Üçel et al. 2015; Aydın et al. 2016; Barbaros et al. 2018).
Pharmacotherapy
REB was administered to the diabetic rats at doses of 8 mg/kg and 16 mg/kg (p.o.) for 2 weeks (Pedersen et al. 2005; Cegielski-Perun et al. 2014). Rats in the healthy and diabetic control groups were administered physiological saline solution (0.9% sodium chloride), used to dissolve REB. Pregabalin at a dose of 10 mg/kg (Thiagarajan et al. 2014) was administered as a reference drug for neuropathic pain assessments. Physiological saline, REB, and pregabalin treatments were administered every morning between 9:45 and 10:00 A.M. throughout the experimental protocol.
In accordance with the administration protocol, 5 different experimental groups (n = 8 in each) were formed and a total of 40 rats were used for the following neuropathic pain and activity cage tests.
Assessment of neuropathic pain
Evaluation of mechanical hyperalgesia
A Randall–Selitto device (Ugo Basile, 37215, Varese, Italy) was used to evaluate mechanical hyperalgesia. In this test, linearly increasing pressure was applied on the dorsal surface of the hind paw and the force (expressed in grams) that caused paw withdrawal was accepted as the mechanical nociceptive threshold. The maximum force was limited to 250 g to avoid paw injuries (Üçel et al. 2015; Aydın et al. 2016; Barbaros et al. 2018).
Evaluation of mechanical allodynia
A dynamic plantar aesthesiometer device (Ugo Basile, 37450, Varese, Italy) that measures the response to non-painful mechanical stimulus in grams was used to evaluate mechanical allodynia. The device consists of 6 plexiglass compartments (17 × 69 × 14 cm) placed on an elevated perforated metal platform and a movable piece under the platform that can apply the mechanical stimulus with increasing force using a metal rod of 0.5 mm diameter. Prior to experimentation, the animals were adapted in these compartments for 30 min. This was followed by pressure application on the plantar surface of the hind paws with increasing force (2.5 g/s) using the device. The mechanical stimulus was automatically stopped when rats withdrew their paws, and force was recorded by the device with a precision of 0.1 g.
The paw withdrawal threshold of the experimental animal was calculated by obtaining the mean value of three measurements performed at 5-min intervals. The maximum force was limited to 50 g to prevent paw injury (Üçel et al. 2015; Aydın et al. 2016).
Evaluation of thermal hyperalgesia
Hargreaves (plantar) test device (Ugo Basile, 37370, Varese, Italy) was used to evaluate thermal hyperalgesia. The device consists of 6 plexiglass compartments (17 × 69 × 14 cm) placed on an elevated glass surface and a movable radiant heat source under the surface. Prior to experimentation, the animals were adapted in these compartments for 30 min. The device was turned on after positioning the movable radiant heat source to face the plantar surface of the hind paws during measurements. The paw withdrawal latency values were recorded by the device with a precision of 0.1 s. Thermal stimulus exposure time was limited to 20 s to prevent paw damage. Measurements were conducted on the same paw, and the paw withdrawal latency value of each rat was calculated by obtaining the mean value of three measurements obtained at 5-min intervals (Üçel et al. 2015; Aydın et al. 2016; Barbaros et al. 2018).
Evaluation of thermal allodynia
The “hot/cold plate test device” (Ugo Basile, 35100, Varese, Italy) was used to evaluate thermal allodynia. For the warm plate test, the rats were placed on an aluminum plate set to 38 °C temperature. The time until the first reaction was recorded. The cut-off time was set as 30 s (Üçel et al. 2015; Aydın et al. 2016).
Evaluation of locomotor activity
An activity cage with transparent walls and 40 × 40 × 31 cm dimensions (Ugo Basile, 7420, Varese, Italy) was used to evaluate spontaneous locomotor activity. Vertical and horizontal movements of the animals interrupted the infrared beams, detected by two sets of emitter/sensor arrays. These interruptions were automatically recorded by the device. In this study, the vertical and horizontal movements of the rats were recorded for 10 min (Pitsikas et al. 2008).
Neuropathic pain and locomotor activity studies were repeated for four times: At the beginning of the experiments without any administration (week 0); 4 weeks after the induction of diabetes and just before the beginning of treatment protocols (week 4); following the 1-week treatment protocol (week 5); and following the two-week treatment protocol (week 6).
Studies to elucidate the mechanism
In order to investigate the contribution of the catecholaminergic system to the antihyperalgesic and antiallodynic effects of REB, AMPT, a catecholamine synthesis inhibitor, was used. AMPT was administered twice (24 h and 1 h before the last dose) via intraperitoneal (i.p.) route, at a dose of 200 mg/kg (Fulford and Marsden 2007; Üçel et al. 2015).
In order to investigate the possible contribution of adrenergic receptors to the antihyperalgesic and antiallodynic effects of REB, phentolamine (a nonselective α-adrenergic receptor blocker, 5 mg/kg, i.p.), propranolol (a nonselective β-adrenergic receptor blocker, 5 mg/kg, i.p.) (Barbaros et al. 2018), metoprolol (a β1-adrenoceptor blocker, 15 mg/kg, i.p.) (Béïque et al. 2000), ICI-118,551 (a β2-adrenoceptor blocker, 1 mg/kg, i.p.) (Njung’e et al. 1993), and SR 59230A (a β3-adrenoceptor blocker, 7.5 mg/kg, i.p.) (Zhu et al. 2015) were used. Moreover, the possible contributions of the dopaminergic, cholinergic, and δ-opioidergic receptors were investigated using SCH-23390 (a dopamine D1 receptor blocker, 0.5 mg/kg, i.p.), sulpiride (a dopamine D2/D3 receptor blocker, 30 mg/kg, i.p.) (Forman 1999), atropine (a nonselective muscarinic receptor blocker, 5 mg/kg, i.p.) (Di Cesare Mannelli et al. 2009), and naltrindole (a δ-opioid receptor blocker, 3 mg/kg, i.p.) (Juárez-Rojop et al. 2015). In the mechanistic studies, each antagonist was tested on a separate set of animals (4 groups × 8 rats = 32 animals per set, a total of 320 rats for 10 different agents).
Plasma glucose level monitoring
At the end of the experimental protocol, plasma glucose levels of animals used in the behavioral studies were measured following an 8-h fasting period. Metformin was administered as a reference drug in a separate experimental group of 8 animals, at a dose of 1000 mg/kg (Ong et al. 2011).
Statistical evaluation
Data were statistically analyzed using the GraphPad Prism version 6.01 (GraphPad Software, Inc., La Jolla, CA, USA). The data obtained from the plasma glucose measurements were analyzed using one-way analysis of variance (ANOVA) followed by Tukey’s HSD multiple comparison test. The data acquired from Randall–Selitto, dynamic plantar, Hargreaves, warm plate, and activity cage tests were evaluated using two-way repeated measures ANOVA followed by the Bonferroni multiple comparison test. Data obtained from mechanistic studies were evaluated using two-way ANOVA followed by the Bonferroni multiple comparison test. The results are expressed as mean ± standard error of mean (SEM). The significance threshold was set at 0.05, and a p value < 0.05 was considered statistically significant.
Results
Results of the neuropathic pain tests
Figure 1 shows the effects of pregabalin (10 mg/kg) and REB (8 and 16 mg/kg) treatments on mechanical hyperalgesia, mechanical allodynia, thermal hyperalgesia, and thermal allodynia responses in rats assessed in the Randall–Selitto (Fig. 1a), dynamic plantar (Fig. 1b), Hargreaves (plantar) (Fig. 1c), and warm plate tests (Fig. 1d), respectively.
Effects of daily 8 mg/kg reboxetine (REB 8 + DM), 16 mg/kg reboxetine (REB 16 + DM) and 10 mg/kg pregabalin (PRG + DM) administrations on neuropathic pain parameters in diabetic rats in the Randall–Selitto (paw withdrawal thresholds) (a), dynamic plantar (paw withdrawal thresholds) (b), Hargreaves (plantar) test (paw withdrawal latency) (c), and warm plate test (reaction time) (d). Within groups: significant difference against week 0 ***p < 0.001; week 4 &&p < 0.01; &&&p < 0.001. Between groups: significant difference against 4th week of the control group ¥¥¥p < 0.001; 5th week of the control group £££p < 0.001; 6th week of control group ɸɸp < 0.01; ɸɸɸp < 0.001; 5th week of the DM group Σp < 0.05, ΣΣΣp < 0.001; 6th week of DM χχχp < 0.001. Two-way repeated ANOVA, post hoc Bonferroni test, n = 8
The results obtained from the two-way repeated measures ANOVA demonstrated that both treatment and the time factors affected paw withdrawal thresholds measured in the Randall–Selitto tests ([F(4,35) = 15.21; p < 0.001] and [F(3,105) = 40.60; p < 0.001]); on paw withdrawal thresholds measured in the dynamic plantar test ([F(4,35) = 24.17; p < 0.001] and [F(3,105) = 62.67; p < 0.001]); on paw withdrawal latency measured in Hargreaves test ([F(4,35) = 23.56; p < 0.001] and [F(3,105) = 55.71; p < 0.001]); and on the reaction time measured in the warm plate test ([F(4,35) = 9.44; p < 0.001] and [F(3,105) = 53.17; p < 0.001]). Furthermore, significant interactions were observed between these treatments and time factors ([F(12,105) = 8.41; p < 0.001]; [F(12,105) = 11.86; p < 0.001]; [F(12,105) = 11.77; p < 0.001]; and [F(12,105) = 9.96; p < 0.001]) in the above-mentioned tests, respectively.
The results acquired from the Bonferroni multiple comparison tests demonstrated that the measured neuropathic pain parameters in untreated diabetic rats were significantly lower than the corresponding values in normoglycemic animals. However, the administration of pregabalin and REB (8 and 16 mg/kg) for 2 weeks significantly ameliorated the observed hyperalgesia and allodynia responses in diabetic rats (Fig. 1).
Results of the activity cage tests
Figure 2 shows the effects of REB (8 and 16 mg/kg) treatments on the horizontal (Fig. 2a) and vertical (Fig. 2b) locomotor activity counts of rats assessed in the activity cage tests.
Horizontal (a) and vertical (b) locomotor activities of rats administered 8 mg/kg reboxetine (REB 8 + DM) and 16 mg/kg reboxetine (REB 16 + DM) in the activity cage test. Within groups: significant difference against week 0 *p < 0.05; **p < 0.01; ***p < 0.001. Between groups: significant difference against 4th week of the control group ¥p < 0.05; ¥¥p < 0.01; ¥¥¥p < 0.001; 5th week of the control group £££p < 0.001; 6th week of the control group ɸp < 0.05; ɸɸp < 0.01; ɸɸɸp < 0.001. Two-way repeated ANOVA, post hoc Bonferroni test, n = 8
The two-way repeated measures ANOVA indicated that both treatment and the time factors demonstrated effects on the number of horizontal ([F(3,28) = 20.23; p < 0.001] and [F(3,84) = 30.40; p < 0.001]) and vertical ([F(3,28) = 13.16; p < 0.001] and [F(3,84) = 17.08; p < 0.001]) locomotor activities in rats. Furthermore, significant interactions between the treatment and time factors were observed in tests measuring horizontal [F(9,84) = 5.01; p < 0.001] and vertical [F(9,84) = 3.12; p < 0.01] activities.
The Bonferroni multiple comparison test results indicated that the spontaneous locomotor activity in untreated diabetic rats was significantly lower than the corresponding values observed in normoglycemic animals. Moreover, the administration of REB (8 and 16 mg/kg) did not induce any additional changes in the locomotor activity of diabetic rats (Fig. 2).
Results of the mechanism studies
Effects of AMPT, phentolamine, and propranolol administration
Figure 3 shows the effects of AMPT, phentolamine, and propranolol pretreatments on the antihyperalgesic and antiallodynic responses induced by the administration of 8 mg/kg REB in the Randall–Selitto, dynamic plantar, Hargreaves (plantar), and warm plate tests.
The effects of α-methyl-para-tyrosine methyl ester (AMPT; 200 mg/kg i.p., 2 times), phentolamine (5 mg/kg i.p.), and propranolol (5 mg/kg i.p.) pretreatments on the antihyperalgesic and antiallodynic responses induced by the administration of 8 mg/kg REB in the Randall–Selitto (a), dynamic plantar (b), Hargreaves (plantar) (c), and warm plate (d) tests. Significant difference against the diabetic control group **p < 0.01; ***p < 0.001; Significant difference against the 8 mg/kg reboxetine-administrated diabetic group &&p < 0.01; &&&p < 0.001. Two-way ANOVA, post hoc Bonferroni test, n = 8
The results obtained from the two-way repeated measures ANOVA are as follows:
Pretreatments | Factors | Randall–Selitto test | Dynamic plantar test | Hargreaves (plantar) test | Warm plate tests |
|---|---|---|---|---|---|
AMPT | Treatment | F(1,28) = 55.17; p < 0.001 | F(1,28) = 20.29; p < 0.001 | F(1,28) = 30.87; p < 0.001 | F(1,28) = 5.33; p < 0.05 |
Antagonist | F(1,28) = 40.74; p < 0.001 | F(1,28) = 27.82; p < 0.001 | F(1,28) = 16.30; p < 0.001 | F(1,28) = 17.32; p < 0.001 | |
Interaction | F(1,28) = 20.40; p < 0.001 | F(1,28) = 11.33; p < 0.01 | F(1,28) = 27.61; p < 0.001 | F(1,28) = 8.95; p < 0.01 | |
Phentolamine | Treatment | F(1,28) = 183.0; p < 0.001 | F(1,28) = 30.61; p < 0.001 | F(1,28) = 59.70; p < 0.001 | F(1,28) = 44.69; p < 0.001 |
Antagonist | F(1,28) = 0.94; p > 0.05 | F(1,28) = 0.01; p > 0.05 | F(1,28) = 1.05; p > 0.05 | F(1,28) = 1.22; p > 0.05 | |
Interaction | F(1,28) = 0.74; p > 0.05 | F(1,28) = 1.26; p > 0.05 | F(1,28) = 1.66; p > 0.05 | F(1,28) = 0.38; p > 0.05 | |
Propranolol | Treatment | F(1,28) = 54.56; p < 0.001 | F(1,28) = 58.99; p < 0.001 | F(1,28) = 56.66; p < 0.001 | F(1,28) = 18.65; p < 0.001 |
Antagonist | F(1,28) = 17.26; p < 0.001 | F(1,28) = 4.20; p < 0.05 | F(1,28) = 4.52; p < 0.05 | F(1,28) = 18.95; p < 0.001 | |
Interaction | F(1,28) = 15.60; p < 0.001 | F(1,28) = 9.23; p < 0.01 | F(1,28) =10.12; p < 0.01 | F(1,28) = 22.73; p < 0.001 |
The Bonferroni multiple comparison test results suggested that pretreatment with AMPT and propranolol abolished the antihyperalgesic and antiallodynic effects of REB in the evaluated neuropathic pain tests. However, phentolamine administration did not alter the mentioned effects of REB (Fig. 3).
Effects of metoprolol, ICI-118,551, and SR 59230A administration
Figure 4 shows the effects of metoprolol, ICI-118,551, and SR 59230A pretreatments on the antihyperalgesic and antiallodynic responses induced by administration of 8 mg/kg REB in the Randall–Selitto, dynamic plantar, Hargreaves (plantar), and warm plate tests.
The effects of metoprolol (15 mg/kg i.p.), ICI-118,551 (1 mg/kg i.p.) and SR 59230A (7.5 mg/kg i.p.) pretreatments on the antihyperalgesic and antiallodynic responses induced by the administration of 8 mg/kg REB in the Randall–Selitto (a), dynamic plantar (b), Hargreaves (plantar) (c), and warm plate (d) tests. Significant difference against the diabetic control group ***p < 0.001. Significant difference against the 8 mg/kg reboxetine-administrated diabetic group &p < 0.05; &&&p < 0.001. Two-way ANOVA, post hoc Bonferroni test, n = 8
The results obtained from the two-way repeated measures ANOVA are as follows:
Pretreatments | Factors | Randall–Selitto test | Dynamic plantar test | Hargreaves (plantar) test | Warm plate tests |
|---|---|---|---|---|---|
Metoprolol | Treatment | F(1,28) = 224.9; p < 0.001 | F(1,28) = 135.5; p < 0.001 | F(1,28) = 65.87; p < 0.001 | F(1,28) = 43.88; p < 0.001 |
Antagonist | F(1,28) = 0.30; p > 0.05 | F(1,28) = 0.74; p > 0.05 | F(1,28) = 0.11; p > 0.05 | F(1,28) = 0.01; p > 0.05 | |
Interaction | F(1,28) = 0.08; p > 0.05 | F(1,28) = 1.32; p > 0.05 | F(1,28) = 0.06; p > 0.05 | F(1,28) = 0.31; p > 0.05 | |
ICI-118,551 | Treatment | F(1,28) = 17.58; p < 0.001 | F(1,28) = 30.86; p < 0.001 | F(1,28) = 40.90; p < 0.001 | F(1,28) = 20.60; p < 0.001 |
Antagonist | F(1,28) = 12.82; p < 0.01 | F(1,28) = 4.94; p < 0.05 | F(1,28) = 4.45; p < 0.05 | F(1,28) = 20.69; p < 0.001 | |
Interaction | F(1,28) = 17.13; p < 0.001 | F(1,28) = 4.33; p < 0.05 | F(1,28) = 7.32; p < 0.05 | F(1,28) = 17.75; p < 0.001 | |
SR 59230A | Treatment | F(1,28) = 139.5; p < 0.001 | F(1,28) = 106.9; p < 0.001 | F(1,28) = 65.54; p < 0.001 | F(1,28) = 57.80; p < 0.001 |
Antagonist | F(1,28) = 0.03; p > 0.05 | F(1,28) = 0.38; p > 0.05 | F(1,28) = 1.72; p > 0.05 | F(1,28) = 0.15; p > 0.05 | |
Interaction | F(1,28) = 1.61; p > 0.05 | F(1,28) = 0.03; p > 0.05 | F(1,28) = 0.25; p > 0.05 | F(1,28) = 0.47; p > 0.05 |
The Bonferroni multiple comparison test results suggested that pretreatment with ICI-118,551 abolished the antihyperalgesic and antiallodynic effects of REB in the evaluated neuropathic pain tests. However, metoprolol and SR 59230A administration did not alter the mentioned effects of REB (Fig. 4).
Effects of SCH-23390 and sulpiride administration
Figure 5 shows the effects of SCH-23390 and sulpiride pretreatments on the antihyperalgesic and antiallodynic responses induced by the administration of 8 mg/kg REB in the Randall–Selitto, dynamic plantar, Hargreaves (plantar), and warm plate tests.
The effects of SCH-23390 (0.5 mg/kg i.p.) and sulpiride (30 mg/kg i.p.) pretreatments on the antihyperalgesic and antiallodynic responses induced by the administration of 8 mg/kg REB in the Randall–Selitto (a), dynamic plantar (b), Hargreaves (plantar) (c), and warm plate (d) tests. Significant difference against the diabetic control group **p < 0.01;***p < 0.001. Significant difference against the 8 mg/kg reboxetine-administrated diabetic group &&p < 0.01; &&&p < 0.001. Two-way ANOVA, post hoc Bonferroni test, n = 8
The results obtained from the two-way repeated measures ANOVA are as follows:
Pretreatments | Factors | Randall–Selitto test | Dynamic plantar test | Hargreaves (plantar) test | Warm plate tests |
|---|---|---|---|---|---|
SCH-23390 | Treatment | F(1,28) = 41.38; p < 0.001 | F(1,28) = 62.76; p < 0.001 | F(1,28) =4 .35; p < 0.05 | F(1,28) = 29.77; p < 0.001 |
Antagonist | F(1,28) = 26.95; p < 0.001 | F(1,28) = 4.30; p < 0.05 | F(1,28) = 5.20; p < 0.05 | F(1,28) = 29.25; p < 0.001 | |
Interaction | F(1,28) = 37.33; p < 0.001 | F(1,28) = 5.75; p < 0.05 | F(1,28) = 7.52; p < 0.05 | F(1,28) = 30.90; p < 0.001 | |
Sulpiride | Treatment | F(1,28) = 90.99; p < 0.001 | F(1,28) = 14.55; p < 0.001 | F(1,28) = 18.00; p < 0.001 | F(1,28) = 18.36; p < 0.001 |
Antagonist | F(1,28) = 11.57; p < 0.01 | F(1,28) = 6.95; p < 0.05 | F(1,28) = 4.49; p < 0.05 | F(1,28) = 10.48; p < 0.01 | |
Interaction | F(1,28) = 9.42; p < 0.01 | F(1,28) = 4.73; p < 0.05 | F(1,28) = 10.19; p < 0.01 | F(1,28) = 5.92; p < 0.05 |
The Bonferroni multiple comparison test results suggested that SCH-23390 and sulpiride pretreatments abolished the antihyperalgesic and antiallodynic effects of REB in the tests performed (Fig. 5).
Effects of atropine and naltrindole administration
Figure 6 shows the effects of atropine and naltrindole pretreatments on the antihyperalgesic and antiallodynic responses induced by the administration of 8 mg/kg REB in the Randall–Selitto, dynamic plantar, Hargreaves (plantar), and warm plate tests.
The effects of atropine (5 mg/kg i.p.) and naltrindole (3 mg/kg i.p.) pretreatments on the antihyperalgesic and antiallodynic responses induced by the administration of 8 mg/kg REB in the Randall–Selitto (a), dynamic plantar (b), Hargreaves (plantar) (c), and warm plate (d) tests. Significant difference against the diabetic control group ***p < 0.001. Significant difference against the 8 mg/kg reboxetine-administrated diabetic group &&p < 0.01; &&&p < 0.001. Two-way ANOVA, post hoc Bonferroni test, n = 8
The results obtained from the two-way repeated measures ANOVA are as follows:
Pretreatments | Factors | Randall–Selitto test | Dynamic plantar test | Hargreaves (plantar) test | Warm plate tests |
|---|---|---|---|---|---|
Atropine | Treatment | F(1,28) = 173.0; p < 0.001 | F(1,28) = 85.24; p < 0.001 | F(1,28) = 89.66; p < 0.001 | F(1,28) = 113.3; p < 0.001 |
Antagonist | F(1,28) = 0.85; p > 0.05 | F(1,28) = 0.01; p > 0.05 | F(1,28) = 1.66; p > 0.05 | F(1,28) = 0.83; p > 0.05 | |
Interaction | F(1,28) = 0.31; p > 0.05 | F(1,28) = 3.87; p > 0.05 | F(1,28) = 0.01; p > 0.05 | F(1,28) = 1.76; p > 0.05 | |
Naltrindole | Treatment | F(1,28) = 22.06; p < 0.001 | F(1,28) = 71.58; p < 0.001 | F(1,28) = 42.50; p < 0.001 | F(1,28) = 11.06; p < 0.01 |
Antagonist | F(1,28) = 16.01; p < 0.001 | F(1,28) = 4.80; p < 0.05 | F(1,28) = 4.36; p < 0.05 | F(1,28) = 11.38; p < 0.01 | |
Interaction | F(1,28) = 7.73; p < 0.01 | F(1,28) = 6.38; p < 0.05 | F(1,28) = 10.01; p < 0.01 | F(1,28) =7.03; p < 0.05 |
The Bonferroni multiple comparison test results indicated that pretreatment with naltrindole abolished the antihyperalgesic and antiallodynic effects of REB in all evaluated neuropathic pain tests. However, atropine treatment did not alter the demonstrated REB effects (Fig. 6).
Results of plasma glucose measurements
Figure 7 shows the effects of metformin (1000 mg/kg) and REB (8 and 16 mg/kg) on plasma glucose levels in diabetic rats (F(4,35) = 49.88; p < 0.001). The results demonstrated that the plasma glucose levels in diabetic rats were significantly higher than those in the control group. As expected, metformin demonstrated an anti-hyperglycemic effect. On the other hand, REB (both at 8 and 16 mg/kg doses) did not significantly alter the hyperglycemic levels in diabetic rats (Fig. 7).
Plasma glucose levels in rats administered 8 mg/kg reboxetine (REB 8 + DM), 16 mg/kg reboxetine (REB 16 + DM), and 1000 mg/kg metformin (MET + DM) daily. Significant difference against the control group ***p < 0.001; significant difference against the DM group &&&p < 0.001. One-way ANOVA, post hoc Tukey’s test, n = 8
Discussion
It is well known that TCAs and SNRIs, the first-choice drugs in the treatment of neuropathic pain, increase the monoamine concentration in the synaptic cleft by inhibiting noradrenaline and serotonin transporters in neurons (Attal et al. 2010; Dworkin et al. 2010). The beneficial effects of these drugs in neuropathic pain have been attributed to their capacity to enhance monoaminergic neurotransmission. In contrast to TCAs and SNRIs, selective serotonin reuptake inhibitors (SSRIs), inhibiting solely serotonin reuptake in neurons, have a weak efficacy profile in neuropathic pain, leading to the hypothesis that the noradrenergic system, but not the serotonergic system, plays a critical role in neuropathic pain pathophysiology and thereby its pharmacotherapy (Max et al. 1992; Benbouzid et al. 2008a; Attal et al. 2010; Dworkin et al. 2010). Notably, recent findings have indicated that the noradrenergic system plays a dominant role in neuropathic pain pharmacotherapy, whereas the serotonergic and dopaminergic systems only have modulatory effects (Webster 2015; Obata 2017). This suggests that drugs affecting the noradrenergic system may have curative potential in neuropathic pain. Therefore, we investigated the potential efficacy of REB, a potent and selective noradrenaline reuptake inhibitor, in diabetes-induced neuropathic pain.
In this study, data obtained from the Randall–Selitto, dynamic plantar, Hargreaves, and warm plate tests suggested that the diabetic rats developed hyperalgesia and allodynia in response to mechanical and thermal stimulus. Notably, the REB treatment reported an effect comparable to the reference drug pregabalin, improving the neuropathic pain responses in diabetic rats (Fig. 1). These findings are in agreement with the following previous studies which reported that REB: (i) produced an acute antinociceptive effect in the hot plate test performed in mice (Schreiber et al. 2009), (ii) reduced mechanical allodynia in rats with neuropathic pain induced by sciatic nerve damage (Yalcin et al. 2009a), (iii) reduced thermal hyperalgesia in rats with chronic constriction injury (Pedersen et al. 2005), and (iv) reduced pain and allodynia associated with tibial nerve transection (Hughes et al. 2015). In addition to these preclinical results, some clinical studies reported that REB is effective in treating pain associated with capsaicin-induced irritation (Schüler et al. 2002); furthermore, it alleviates fibromyalgia and chronic back pain in patients (Krell et al. 2005).
Activity cage experiments were used to evaluate the locomotor activities of experimental animals, demonstrating that the diabetic rats had significantly reduced horizontal (Fig. 2a) and vertical (Fig. 2b) activities compared with normoglycemic ones. These findings are consistent with the results from previous studies, indicating that the rodents with experimental diabetes have impaired motor activity and motor coordination abilities (Niknia et al. 2018; Rasoulian et al. 2018). The administration of REB did not induce any change in the locomotor activity of diabetic rats. These results are significant, proving that the antihyperalgesic and antiallodynic effects induced by the administration of REB are not associated with changes in the motor activity of rats.
After demonstrating the antiallodynic and antihyperalgesic effects of REB on diabetic rats, the possible underlying mechanisms were investigated. REB at a dose of 8 mg/kg was used in mechanistic studies as the 16 mg/kg dose of REB was not superior to the 8 mg/kg dose in terms of the activity.
Reportedly, antidepressants show their analgesic effects primarily by inhibiting monoamine reuptake in supraspinal descending pathways, which suppresses pain (Bannister et al. 2009; Yarnitsky 2015). Since REB is a selective inhibitor of noradrenaline reuptake, antihyperalgesic and antiallodynic effects of this drug could be associated with the capacity to utilize noradrenergic neurotransmission. Therefore, our mechanistic studies were initially performed using AMPT. This agent reduces noradrenaline and dopamine synthesis by selectively inhibiting tyrosine hydroxylase, a rate-limiting enzyme in catecholamine synthesis (Widerlov and Lewander 1978; Onal et al. 2007). The administration of AMPT twice with a 23-h interval, at a dose of 200 mg/kg (as in this study), reduces noradrenaline levels in the central nervous system (CNS) by 50–60% (Corrodi and Hanson 1966; Onal et al. 2007). In the present study, since AMPT completely abolished the antihyperalgesic and antiallodynic effects induced by REB (Fig. 3), it could be suggested that the effect of REB on neuropathic pain is sensitive to decreased central catecholamine levels. In other words, the catecholaminergic system plays a role in the antihyperalgesic and antiallodynic effects of REB. Hence, it is possible to consider that REB demonstrates its effects on neuropathic pain by increasing neurotransmission in the supraspinal descending noradrenergic pathway, suppressing nociceptive signal transmission from primary afferent neurons to the spinal dorsal horn. However, this hypothesis needs confirmation with additional studies. Furthermore, it should be emphasized that, due to its catecholaminergic neurotransmission enhancing mechanism, REB may have a unique potential to improve the diabetes-induced dysfunctions in supraspinal inhibitory noradrenergic pathways (Malcangio and Tomlinson 1998) known to suppress the transmission of neuropathic pain.
The possible role of catecholaminergic receptors on antihyperalgesic and antiallodynic effects was investigated after demonstrating that the effect of REB in neuropathic pain was mediated through the modulation of the catecholaminergic system.
It is well established that α-adrenergic receptors, one of the receptors that mediate the effects of noradrenaline on the CNS, play a pivotal role in the pathways associated with nociception and pain (Taylor 2009; Pertovaara 2013; Zhu et al. 2013). Therefore, phentolamine, a nonselective α-adrenergic receptor blocker, was used to investigate the potential role of α-adrenergic receptors on the antihyperalgesic and antiallodynic effects of REB on diabetic rats. Our findings indicated that phentolamine pretreatment does not abolish the effects of REB (Fig. 3). Therefore, it can be suggested that α-adrenergic receptors do not participate in the antihyperalgesic and antiallodynic effects of REB.
Furthermore, β-adrenoceptors, another class of adrenergic receptors, are closely associated with nociception and analgesia (Hartung et al. 2014; Zhang et al. 2018). Therefore, propranolol, a nonselective β-adrenergic receptor antagonist, was used to investigate the possible role of β-adrenergic receptors in the antihyperalgesic and antiallodynic effects of REB in diabetic rats. Antagonization of the antihyperalgesic and antiallodynic effects by propranolol pretreatment (Fig. 3) indicated that β-adrenergic receptors possibly mediate the effects of REB. Further mechanistic studies with sub-type selective agents, metoprolol, ICI-118,551, and SR 59230A (Fig. 4), indicated that the antihyperalgesic and antiallodynic effects of REB were mediated only by β2-adrenoceptors.
In accordance with our findings, it has been reported that REB administration at a daily dose of 0.8 mg/kg for 4 weeks reduced sciatic nerve damage–induced mechanical allodynia in rats. This antiallodynic action was reversed by the β2-adrenergic receptor blocker ICI-118,551; however, it was not affected by the administration of yohimbine (α2-adrenoceptor antagonist) (Yalcin et al. 2009a). Nortriptyline, another antidepressant drug effectively enhancing the noradrenergic neurotransmission in the CNS, has been reported for its efficacy in neuropathic pain. Furthermore, the antiallodynic effect of this drug was not reversed by yohimbine (α2-adrenoceptor antagonist), atenolol/metoprolol (β1-adrenergic receptor antagonists), or SR 59230A (β3-adrenergic receptor blocker). However, the nonselective β-adrenergic receptor antagonists propranolol and sotalol, β1/β2-adrenergic receptor antagonists alprenolol and pindolol, and the specific β2-adrenergic receptor blocker ICI-118,551, successfully antagonized the antiallodynic effect of nortriptyline. Moreover, it was observed that nortriptyline was completely ineffective in alleviating neuropathic pain in β-adrenergic receptor knockout animals (Yalcin et al. 2009b). In accordance with these results, it was also observed that the β2-adrenoceptor blocker, ICI-118,551, antagonized the antiallodynic effect induced by nortriptyline in ob/ob mice with diabetic polyneuropathy (Choucair-Jaafar et al. 2014). Additionally, the antidepressants desipramine and venlafaxine have reported β2-adrenoceptor-mediated antiallodynic actions in rats with neuropathic pain (Yalcin et al. 2009a, b).
In parallel to these findings, it has been demonstrated that the chronic administration of several β2-mimetics could successfully treat neuropathic pain (Barrot et al. 2009; Yalcin et al. 2010; Choucair-Jaafar et al. 2014). A study investigating metaproterenol, procaterol, formoterol, and clenbuterol demonstrated that the antiallodynic effects of these β2-adrenergic agonists on animals with neuropathy could be reversed by the β2-adrenergic receptor blocker ICI-118,551; the β1-adrenergic receptor agonist xamoterol or β3-adrenergic receptor agonist BRL 37344 was ineffective (Yalcin et al. 2010).
The results demonstrating the importance of β2-adrenoceptors in neuropathic pain pharmacotherapy support our findings that the effects of REB in experimental diabetes-induced neuropathic pain. Further studies investigating the roles of β2-adrenergic receptors in the relief of neuropathic pain have highlighted the presence of an indirect anti-tumor necrosis factor α (TNFα) action. More specifically, enhanced noradrenergic neurotransmission has been known to activate β2-adrenergic receptors expressed by non-neuronal satellite cells in dorsal root ganglia. This stimulation has been shown to decrease the neuropathy-induced production of membrane-bound TNFα (Bohren et al. 2013). In parallel to these findings, the antiallodynic actions of duloxetine and amitriptyline in mice with neuropathic pain have been associated with the inhibition of neuroimmune mechanisms accompanying nerve injury, including the downregulation of the TNFα–NF-ĸB signaling pathway in DRGs (Kremer et al. 2018). Therefore, the possible involvement of this downstream mechanism, in the antihyperalgesic and antiallodynic actions of REB, needs further clarification.
Notably, dopaminergic receptors, another receptor of the catecholaminergic system, are closely associated with nociception, neuropathic pain, and analgesia (Taylor et al. 2016; Chen et al. 2017; Obata 2017). Therefore, the possible roles of dopaminergic receptors in the antihyperalgesic and antiallodynic effects of REB were investigated. The roles of D1-dopaminergic receptors were investigated using a selective D1-dopaminergic receptor blocker, SCH-23390, and the roles of D2- and D3-dopaminergic receptors were examined using sulpiride, a nonselective D2-/D3-dopaminergic receptor blocker. Based on the results, pretreatment with SCH-23390 and sulpiride potently antagonized the antihyperalgesic and antiallodynic effects of REB (Fig. 5), indicating the participation of D1-, D2-, and D3-dopaminergic receptor subtypes in these effects.
Numerous studies have reported the role of dopaminergic receptors in the treatment of neuropathic pain. For instance, Chen et al. induced a hyperalgesia model by spinal nerve ligation in rats to study the possible role of the dopaminergic system in the antihyperalgesic effects of amitriptyline, duloxetine, milnacipran, and fluoxetine. This study reports that the antihyperalgesic effects of these four antidepressants were reversed by sulpiride pretreatments. Microdialysis studies performed to investigate changes in dopamine concentration in the spinal dorsal horn indicated that the dopamine levels were significantly increased after administering each of these antidepressants at a dose of 10 mg/kg (i.p.). Based on these findings, it has been suggested that the efficacy of antidepressants in neuropathic pain therapy was not only mediated by the noradrenergic and serotonergic systems but also through the modulation of dopamine levels in the spinal cord (Chen et al. 2017). Moreover, our study group previously reported that atomoxetine, a drug similar to REB in terms of its mechanism of action, demonstrated beneficial effects in diabetes-induced hyperalgesia mediated via the D2/D3 receptors (Barbaros et al. 2018), in parallel to the findings of our current study.
Furthermore, besides the catecholaminergic system, the cholinergic system and particularly the muscarinic receptors are associated with the modulation of acute and chronic pain and analgesia (Kimura et al. 2012; Lee et al. 2016; Pecikoza et al. 2018). Accordingly, mechanistic studies were performed using atropine, a nonselective muscarinic receptor antagonist, to investigate the role of muscarinic receptors in the antihyperalgesic and antiallodynic effects of REB in diabetic rats. Our findings demonstrated that atropine pretreatment was ineffective on the evaluated effects of REB (Fig. 6), indicating that the antihyperalgesic and antiallodynic effects of this drug were not mediated by muscarinic receptors.
Another system that is closely associated with pain and analgesia is the opioidergic system. It is well known that the noradrenergic system activates the endogenous opioid system, and the opioid system plays an important role in inhibitory pain control via μ-, δ-, and ĸ-opioid receptors (Mogil et al. 2000; Gaveriaux-Ruff and Kieffer 2002; Dierich and Kieffer 2004). Recent studies have primarily focused on the relationship between δ-opioid receptors and neuropathic pain (Castany et al. 2016; McDonnell et al. 2017; Saitoh and Nagase 2018). Therefore, naltrindole, a highly potent and selective δ-opioid receptor antagonist, was used in mechanistic studies to investigate the possible role of the δ-opioid receptors in the antihyperalgesic and antiallodynic effects of REB.
We observed that naltrindole pretreatment potently antagonized the effects of REB in diabetic rats (Fig. 6). Accordingly, it could be postulated that these effects were mediated by δ-opioid receptors. Previously, similar results have also been demonstrated for nortriptyline. Reportedly, this TCA has been shown to possess δ-opioid receptor–mediated antiallodynic effects in rats with neuropathic pain induced by diabetes (Choucair-Jaafar et al. 2014) or sciatic nerve damage (Benbouzid et al. 2008a; Bohren et al. 2010; Yalcin et al. 2010). Moreover, it has been observed that chronic nortriptyline administration did not demonstrate any beneficial effects in mechanical allodynia in δ-opioid receptor knockout mice (Benbouzid et al. 2008b). These results, evidencing the roles of δ-opioid receptors in neuropathic pain treatment, are supportive of our findings on δ-opioid receptor–mediated antihyperalgesic and antiallodynic effects of REB. Nevertheless, in a recent study (Ceredig et al. 2018), loss of peripheral δ-opioid receptors in small peptidergic neurons in the DRG and enhanced δ-opioid receptor expression at the plasma membrane have been suggested as the mechanisms underlying the neuropathic conditions induced by the cuff surgery. Moreover, chronic treatment with duloxetine has been shown to alleviate neuropathic allodynia symptoms, probably by counteracting the mentioned subcellular distributions of δ-opioid receptors in neuropathic mice. Similar mechanisms may also be valid for REB, which was shown to possess its antihyperalgesic and antiallodynic effects via δ-opioid receptors. However, this assumption needs further investigation.
Another remarkable finding concerning the role of δ-opioid receptors in neuropathic pain is the potential of these receptors to interact with β2-adrenoceptors. Naltrindole pretreatment has been shown to eliminate the beneficial effects of β2-adrenoceptor agonists terbutaline (Choucair-Jaafar et al. 2014) and clenbuterol (Yalcin et al. 2010) in neuropathic pain. Moreover, recently, Kremer et al. defined a peripheral, delayed, and long-lasting mechanism for the antiallodynic effects of antidepressant drugs duloxetine and amitriptyline, which require noradrenaline from peripheral sympathetic endings and β2-adrenoceptors, as well as the δ-opioid receptor component of the opioid system (Kremer et al. 2018). These findings, indicating an association between the β2-adrenoceptors and δ-opioid receptors in the treatment of neuropathic pain, are noteworthy as they lend support to our results.
As the efficacy of REB was investigated in a diabetes-induced neuropathic pain model, the possible effects of REB were examined on the plasma glucose levels in diabetic rats. The obtained data demonstrated that REB did not induce any significant changes in the hyperglycemia levels of diabetic animals (Fig. 7). These results are in parallel to the findings of a previous report which demonstrated that the regular administration of REB in diabetic rats, at a dose of 2.5 mg/kg for 21 days, did not alter the plasma glucose or insulin levels (Khanam and Pillai 2005).
The evaluation of neuropathic pain test data, in conjunction with the plasma glucose measurements, indicates a clinically interesting picture. Previously, reports have indicated that noradrenaline reuptake inhibitors, including SNRIs and TCAs, demonstrated a relatively higher adverse effect potential on glycemic control than SSRIs. Hence, SSRIs should be preferred in the treatment of diabetes-induced neuropathic pain (Deuschle 2013; Whiskey and Taylor 2013). In contrast, SSRIs are not as effective as TCAs or dual inhibitors in the treatment of neuropathic pain (Attal et al. 2010; Finnerup et al. 2015; Kremer et al. 2016). This study has demonstrated that REB shows strong antihyperalgesic and antiallodynic effects without inducing a significant change in the plasma glucose concentration of diabetic rats. Based on this perspective, REB could provide a unique advantage in the pharmacotherapy of diabetes-related neuropathic pain.
Nevertheless, these findings should be considered valuable and informative as they imply a novel indication for REB, while its clinical efficacy as an antidepressant has been questionable in recent years (Eyding et al. 2010; Sepede et al. 2012; Braithwaite 2015).
Our study demonstrated the beneficial effects of REB, a selective noradrenaline reuptake inhibitor, in diabetes-induced neuropathic pain, indicating the involvement of the catecholaminergic system, β2-adrenoceptors, D1- and D2/D3- dopaminergic receptors, and δ-opioid receptors as the underlying pharmacological mechanisms. Furthermore, these preclinical observations need to be confirmed in well-designed clinical studies in order to indicate REB in the treatment of neuropathic pain, which commonly observed in the diabetic population.
References
Ang L, Jaiswal M, Martin C, Pop-Busui R (2014) Glucose control and diabetic neuropathy: lessons from recent large clinical trials. Curr Diab Rep 14(9):528
Attal N, Cruccu G, Baron R, Haanpää M, Hansson P, Jensen TS, Nurmikko T, European Federation of Neurological Societies (2010) EFNS guidelines on the pharmacological treatment of neuropathic pain: 2010 revision. Eur J Neurol 17(9):1113–1e88
Aydın TH, Can ÖD, Demir Özkay Ü, Turan N (2016) Effect of subacute agomelatine treatment on painful diabetic neuropathy: involvement of catecholaminergic mechanisms. Fundam Clin Pharmacol 30(6):549–567
Bannister K, Bee LA, Dickenson AH (2009) Preclinical and early clinical investigations related to monoaminergic pain modulation. Neurotherapeutics 6:703–712
Barbaros MB, Can ÖD, Üçel Uİ, Turan Yücel N, Demir Özkay Ü (2018) Antihyperalgesic activity of atomoxetine on diabetes-induced neuropathic pain: contribution of noradrenergic and dopaminergic systems. Molecules 23(8):E2072
Barrett AM, Lucero MA, Le T, Robinson RL, Dworkin RH, Chappell AS (2007) Epidemiology, public health burden, and treatment of diabetic peripheral neuropathic pain: a review. Pain Med 8(2):50–62
Barrot M, Yalcin I, Choucair-Jaafar N, Benbouzid M, Freund-Mercier MJ (2009) From antidepressant drugs to beta-mimetics: preclinical insights on potential new treatments for neuropathic pain. Recent Pat CNS Drug Discov 4(3):182–189
Béïque JC, Blier P, de Montigny C, Debonnel G (2000) Potentiation by (−)Pindolol of the activation of postsynaptic 5-HT(1A) receptors induced by venlafaxine. Neuropsychopharmacology 23(3):294–306
Benbouzid M, Choucair-Jaafar N, Yalcin I, Waltisperger E, Muller A, Freund-Mercier MJ, Barrot M (2008a) Chronic but not acute, tricyclic antidepressant treatment alleviates neuropathic allodynia after sciatic nerve cuffing in mice. Eur J Pain 12(8):1008–1017
Benbouzid M, Gavériaux-Ruff C, Yalcin I, Waltisperger E, Tessier LH, Muller A, Kieffer BL, Freund-Mercier MJ, Barrot M (2008b) Delta-opioid receptors are critical for tricyclic antidepressant treatment of neuropathic allodynia. Biol Psychiatry 63(6):633–636
Bohren Y, Karavelic D, Tessier LH, Yalcin I, Gavériaux-Ruff C, Kieffer BL, Freund-Mercier MJ, Barrot M (2010) Mu-opioid receptors are not necessary for nortriptyline treatment of neuropathic allodynia. Eur J Pain 14(7):700–704
Bohren Y, Tessier LH, Megat S, Petitjean H, Hugel S, Daniel D, Kremer M, Fournel S, Hein L, Schlichter R, Freund-Mercier MJ, Yalcin I, Barrot M (2013) Antidepressants suppress neuropathic pain by a peripheral β2-adrenoceptor mediated anti-TNFα mechanism. Neurobiol Dis 60:39–50
Braithwaite R (2015) Reboxetine has no antidepressant effect at all. BMJ 351:h5842
Castany S, Carcolé M, Leánez S, Pol O (2016) The antinociceptive effects of a δ-opioid receptor agonist in mice with painful diabetic neuropathy: involvement of heme oxygenase 1. Neurosci Lett 614:49–54
Cegielska-Perun K, Bujalska-Zadrożny M, Tatarkiewicz J, Gąsińska E, Makulska-Nowak HE (2013) Venlafaxine and neuropathic pain. Pharmacology 91(1–2):69–76
Cegielski-Perun K, Bujalska-Zadrożny M, Gasińska E, Makulska-Nowak HE (2014) Enhancement of antinociceptive effect of morphine by antidepressants in diabetic neuropathic pain model. Pharmacol Rep 66(2):228–234
Ceredig RA, Pierre F, Doridot S, Alduntzin U, Salvat E, Yalcin I, Gaveriaux-Ruff C, Barrot M, Massotte D (2018) Peripheral delta opioid receptors mediate duloxetine antiallodynic effect in a mouse model of neuropathic pain. Eur J Neurosci 48(5):2231–2246
Chen M, Hoshino H, Saito S, Yang Y, Obata H (2017) Spinal dopaminergic involvement in the antihyperalgesic effect of antidepressants in a rat model of neuropathic pain. Neurosci Lett 649:16–123
Choucair-Jaafar N, Salvat E, Freund-Mercier MJ, Barrot M (2014) The antiallodynic action of nortriptyline and terbutaline is mediated by β(2) adrenoceptors and δ opioid receptors in the ob/ob model of diabetic polyneuropathy. Brain Res 1546:18–26
Corrodi H, Hanson LC (1966) Central effects of an inhibitor of tyrosine hydroxylation. Psychopharmacologia 10:116–125
Deuschle M (2013) Effects of antidepressants on glucose metabolism and diabetes mellitus type 2 in adults. Curr Opin Psychiatry 26(1):60–65
Di Cesare Mannelli L, Ghelardini C, Calvani M, Nicolai R, Mosconi L, Toscano A, Pacini A, Bartolini A (2009) Neuroprotective effects of acetyl-L-carnitine on neuropathic pain and apoptosis: a role for the nicotinic receptor. J Neurosci Res 87(1):200–207
Dierich A, Kieffer BL (2004) Knockout mouse models in pain research. Methods Mol Med 99:269–299
Dworkin RH, O’Connor AB, Audette J, Baron R, Gourlay GK, Haanpää ML, Kent JL, Krane EJ, Lebel AA, Levy RM, Mackey SC, Mayer J, Miaskowski C, Raja SN, Rice AS, Schmader KE, Stacey B, Stanos S, Treede RD, Turk DC, Walco GA, Wells CD (2010) Recommendations for the pharmacological management of neuropathic pain: an overview and literatüre update. Mayo Clin Proc 85(3 Suppl):3–14
Eyding D, Lelgemann M, Grouven U, Härter M, Kromp M, Kaiser T, Kerekes MF, Gerken M, Wieseler B (2010) Reboxetine for acute treatment of major depression: systematic review and meta-analysis of published and unpublished placebo and selective serotonin reuptake inhibitor controlled trials. BMJ 341:c4737
Finnerup NB, Attal N, Haroutounian S, McNicol E, Baron R, Dworkin RH, Gilron I, Haanpää M, Hansson P, Jensen TS, Kamerman PR, Lund K, Moore A, Raja SN, Rice AS, Rowbotham M, Sena E, Siddall P, Smith BH, Wallace M (2015) Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol 14(2):162–173
Forman LJ (1999) NMDA receptor antagonism produces antinociception which is partially mediated by brain opioids and dopamine. Life Sci 64(21):1877–1887
Fulford AJ, Marsden CA (2007) An intact dopaminergic system is required for context-conditioned release of 5-HT in the nucleus accumbens of postweaning isolation-reared rats. Neuroscience 149(2):392–400
Gaveriaux-Ruff C, Kieffer BL (2002) Opioid receptor genes inactivated in mice: the highlights. Neuropeptides 36:62–71
Hartung JE, Ciszek BP, Nackley AG (2014) β2-and β3-adrenergic receptors drive COMT-dependent pain by increasing production of nitric oxide and cytokines. Pain 155:1346–1355
Hughes S, Hickey L, Donaldson LF, Lumb BM, Pickering AE (2015) Intrathecal reboxetine suppresses evoked and ongoing neuropathic pain behaviours by restoring spinal noradrenergic inhibitory tone. Pain 156(2):328–334
Juárez-Rojop IE, Morales-Hernández PE, Tovilla-Zárate CA, Bermúdez-Ocaña DY, Torres-Lopez JE, Ble-Castillo JL, Díaz-Zagoya JC, Granados-Soto V (2015) Celecoxib reduces hyperalgesia and tactile allodynia in diabetic rats. Pharmacol Rep 67(3):545–552
Khanam R, Pillai KK (2005) Lack of hypo/hyperglycemic effects of reboxetine in diabetic and non-diabetic rats. Fundam Clin Pharmacol 19(6):657–659
Kimura M, Saito S, Obata H (2012) Dexmedetomidine decreases hyperalgesia in neuropathic pain by increasing acetylcholine in the spinal cord. Neurosci Lett 529(1):70–74
Krell HV, Leuchter AF, Cook IA, Abrams M (2005) Evaluation of reboxetine, a noradrenergic antidepressant, for the treatment of fibromyalgia and chronic low back pain. Psychosomatics 46(5):379–384
Kremer M, Salvat E, Muller A, Yalcin I, Barrot M (2016) Antidepressants and gabapentinoids in neuropathic pain: mechanistic insights. Neuroscience 338:183–206
Kremer M, Yalcin I, Goumon Y, Wurtz X, Nexon L, Daniel D, Megat S, Ceredig RA, Ernst C, Turecki G, Chavant V, Théroux JF, Lacaud A, Joganah LE, Lelievre V, Massotte D, Lutz PE, Gilsbach R, Salvat E, Barrot M (2018) A dual noradrenergic mechanism for the relief of neuropathic allodynia by the antidepressant drugs duloxetine and amitriptyline. J Neurosci 38(46):9934–9954
Lee JH, Go D, Kim W, Lee G, Bae H, Quan FS, Kim SK (2016) Involvement of spinal muscarinic and serotonergic receptors in the anti-allodynic effect of electroacupuncture in rats with oxaliplatin-induced neuropathic pain. Korean J Physiol Pharmacol 20(4):407–414
Lenzen S (2008) The mechanisms of alloxan- and streptozotocin-induced diabetes. Diabetologia 51(2):216–226
Malcangio M, Tomlinson DR (1998) A pharmacologic analysis of mechanical hyperalgesia in streptozotocin/diabetic rats. Pain 76(1–2):151–157
Max MB, Lynch SA, Muir J, Shoaf SE, Smoller B, Dubner R (1992) Effects of desipramine, amitriptyline, and fluoxetine on pain in diabetic neuropathy. N Engl J Med 326(19):1250–1256
McDonnell C, Leánez S, Pol O (2017) The induction of the transcription factor Nrf2 enhances the antinociceptive effects of delta-opioid receptors in diabetic mice. PLoS One 12(7):e0180998
Mogil JS, Yu L, Basbaum AI (2000) Pain genes?: natural variation and transgenic mutants. Annu Rev Neurosci 23:777–811
Niknia S, Kaeidi A, Hajizadeh MR, Mirzaei MR, Khoshdel A, Hajializadeh Z, Fahmidehkar MA, Mahmoodi M (2018) Neuroprotective and antihyperalgesic effects of orexin-a in rats with painful diabetic neuropathy. Neuropeptides (18):30111–30112
Njung’e K, Critchley MA, Handley SL (1993) Effects of beta-adrenoceptor ligands in the elevated X-maze ‘anxiety’ model and antagonism of the ‘anxiogenic’ response to 8-OH-DPAT. J Psychopharmacol 7(2):173–180
Obata H (2017) Analgesic mechanisms of antidepressants for neuropathic pain. Int J Mol Sci 18(11):E2483
Onal A, Parlar A, Ulker S (2007) Milnacipran attenuates hyperalgesia and potentiates antihyperalgesic effect of tramadol in rats with mononeuropathic pain. Pharmacol Biochem Behav 88:171–178
Ong KW, Hsu A, Song L, Huang D, Tan BK (2011) Polyphenols-rich Vernonia amygdalina shows anti-diabetic effects in streptozotocin-induced diabetic rats. J Ethnopharmacol 133(2):598–607
Page ME (2003) The promises and pitfalls of reboxetine. CNS Drug Rev 9(4):327–342
Pecikoza U, Micov A, Tomić M, Stepanović-Petrović R (2018) Eslicarbazepine acetate reduces trigeminal nociception: possible role of adrenergic, cholinergic and opioid receptors. Life Sci 214:167–175
Pedersen LH, Nielsen AN, Blackburn-Munro G (2005) Anti-nociception is selectively enhanced by parallel inhibition of multiple subtypes of monoamine transporters in rat models of persistent and neuropathic pain. Psychopharmacology 182(4):551–561
Pertovaara A (2013) The noradrenergic pain regulation system: a potential target for pain therapy. Eur J Pharmacol 716:2–7
Pitsikas N, Boultadakis A, Georgiadou G, Tarantilis PA, Sakellaridis N (2008) Effects of the active constituents of Crocus sativus L., crocins, in an animal model of anxiety. Phytomed 15(12):1135–1139
Pop-Busui R, Lu J, Brooks MM, Albert S, Althouse AD, Escobedo J, Green J, Palumbo P, Perkins BA, Whitehouse F, Jones TL, BARI 2D Study Group (2013) Impact of glycemic control strategies on the progression of diabetic peripheral neuropathy in the bypass angioplasty revascularization investigation 2 diabetes (BARI 2D) cohort. Diabetes Care 36(10):3208–3215
Preskorn SH (2004) Reboxetine: a norepinephrine selective reuptake pump inhibitor. J Psychiatr Pract 10(1):57–63
Rasoulian B, Hajializadeh Z, Esmaeili-Mahani S, Rashidipour M, Fatemi I, Kaeidi A (2018) Neuroprotective and antinociceptive effects of rosemary (Rosmarinus officinalis L.) extract in rats with painful diabetic neuropathy. J Physiol Sci 69(1):57–64
Saitoh A, Nagase H (2018) Delta opioid receptor (dor) ligands and pharmacology: development of indolo- and quinolinomorphinan derivatives based on the message-address concept. Handb Exp Pharmacol 247:3–19
Schreiber S, Frishtick R, Volis I, Rubovitch V, Pick CG, Weizman R (2009) The antinociceptive properties of reboxetine in acute pain. Eur Neuropsychopharmacol 19(10):735–739
Schreiber AK, Nones CFM, Reis RC, Chichorro JG, Cunha JM (2015) Diabetic neuropathic pain: physiopathology and treatment. World J Diabetes 6(3):432–444
Schüler P, Seibel K, Chevts V, Schaffler K (2002) Analgesic effect of the selective noradrenaline reuptake inhibitor reboxetine. Nervenarzt 73(2):149–154
Sepede G, Corbo M, Fiori F, Martinotti G (2012) Reboxetine in clinical practice: a review. Clin Ter 163(4):e255–e262
Singh R, Kishore L, Kaur N (2014) Diabetic peripheral neuropathy: current perspective and future directions. Pharm Res 80:21–35
Taylor BK (2009) Spinal inhibitory neurotransmission in neuropathic pain. Curr Pain Headache Rep 13:208–214
Taylor AM, Becker S, Schweinhardt P, Cahill C (2016) Mesolimbic dopamine signaling in acute and chronic pain: implications for motivation, analgesia, and addiction. Pain 157(6):1194–1198
Thiagarajan VR, Shanmugam P, Krishnan UM, Muthuraman A (2014) Ameliorative effect of Vernonia cinerea in vincristine-induced painful neuropathy in rats. Toxicol Ind Health 30(9):794–805
Üçel Uİ, Can ÖD, Demir Özkay Ü, Öztürk Y (2015) Antihyperalgesic and antiallodynic effects of mianserin on diabetic neuropathic pain: a study on mechanism of action. Eur J Pharmacol 756:92–106
Vinik AI, Casellini CM (2013) Guidelines in the management of diabetic nerve pain: clinical utility of pregabalin. Diabetes Metab Syndr Obes 6:57–78
Webster M (2015) Pharmacologic basis for the use of selective norepinephrine reuptake inhibitors for the treatment of neuropathic pain conditions. Ment Health Clin 5(6):284–288
Whiskey E, Taylor D (2013) A review of the adverse effects and safety of noradrenergic antidepressants. J Psychopharmacol 27(8):732–739
Widerlov E, Lewander T (1978) Inhibition of the in vivo biosynthesis and changes of catecholamine levels in rat brain after a-methyl-ptyrosine; time-and dose–response relationships. Naunyn Schmiedeberg's Arch Pharmacol 304:111–123
Yalcin I, Tessier LH, Petit-Demoulière N, Doridot S, Hein L, Freund-Mercier MJ, Barrot M (2009a) Beta2-adrenoceptors are essential for desipramine, venlafaxine or reboxetine action in neuropathic pain. Neurobiol Dis 33(3):386–394
Yalcin I, Choucair-Jaafar N, Benbouzid M, Tessier LH, Muller A, Hein L, Freund-Mercier MJ, Barrot M (2009b) Beta(2)-adrenoceptors are critical for antidepressant treatment of neuropathic pain. Ann Neurol 65(2):218–225
Yalcin I, Tessier LH, Petit-Demoulière N, Waltisperger E, Hein L, Freund-Mercier MJ, Barrot M (2010) Chronic treatment with agonists of beta(2)-adrenergic receptors in neuropathic pain. Exp Neurol 221(1):115–121
Yarnitsky D (2015) Role of endogenous pain modulation in chronic pain mechanisms and treatment. Pain 156:24–31
Zhang X, Hartung JE, Bortsov AV, Kim S, O’Buckley SC, Kozlowski J, Nackley AG (2018) Sustained stimulation of β2- and β3-adrenergic receptors leads to persistent functional pain and neuroinflammation. Brain Behav Immun 73:520–532
Zhu JX, Xu FY, Xu WJ, Zhao Y, Qu CL, Tang JS, Barry DM, Du JQ, Huo FQ (2013) The role of adrenoceptor in mediating noradrenaline action in the ventrolateralorbital cortex on allodynia following spared nerve injury. Exp Neurol 248:381–386
Zhu L, Zhao L, Qu R, Zhu HY, Wang Y, Jiang X, Xu GY (2015) Adrenergic stimulation sensitizes TRPV1 through upregulation of cystathionine β-synthetase in a rat model of visceral hypersensitivity. Sci Rep 5:16109
Funding
This research was supported from the Anadolu University Scientific Research Projects Commission (Project no: 1606S549).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The experimental protocol was approved by the Animal Experiments Local Ethics Committee of Anadolu University.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Turan Yücel, N., Can, Ö.D. & Demir Özkay, Ü. Catecholaminergic and opioidergic system mediated effects of reboxetine on diabetic neuropathic pain. Psychopharmacology 237, 1131–1145 (2020). https://doi.org/10.1007/s00213-019-05443-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-019-05443-5