Abstract
Rationale
Neuropathic pain is characterised by hyperexcitability within nociceptive pathways that manifests behaviourally as allodynia and hyperalgesia and remains difficult to treat with standard analgesics. However, antidepressants have shown reasonable preclinical and clinical anti-nociceptive efficacy against signs and symptoms of neuropathic pain.
Objectives
To ascertain whether inhibition of serotonin (5-HT) and/or noradrenaline (NA) and/or dopamine (DA) re-uptake preferentially mediates superior anti-nociception in preclinical pain models.
Methods
The 5-HT re-uptake inhibitor fluoxetine (3–30 mg/kg), the NA re-uptake inhibitor reboxetine (3–30 mg/kg), the dual 5-HT and NA re-uptake inhibitor venlafaxine (3–100 mg/kg) and the dual DA and NA re-uptake inhibitor bupropion (3–30 mg/kg) were tested after intraperitoneal administration in rat models of acute, persistent and neuropathic pain.
Results
Reboxetine and venlafaxine dose-dependently attenuated second-phase flinching in the formalin test; fluoxetine attenuated flinching only at the highest dose tested, whereas bupropion was ineffective. In the chronic constriction injury (CCI) and spinal nerve ligation models of neuropathic pain, hindpaw mechanical allodynia was significantly attenuated by fluoxetine and particularly by bupropion. Reboxetine and venlafaxine were completely ineffective. In contrast, reboxetine and venlafaxine reversed thermal hyperalgesia in CCI rats, whereas bupropion and fluoxetine were either minimally effective or ineffective. Fluoxetine, reboxetine and venlafaxine transiently increased the tail-flick latency in uninjured animals. Anti-nociceptive doses of drugs had no effect on motor function.
Conclusions
Combined re-uptake inhibition of 5-HT and NA appears to confer a greater degree of anti-nociception in animal models of experimental pain than single mechanism of action inhibitors. The selective attenuation of mechanical allodynia by bupropion suggests that the additional re-uptake of DA may further augment 5-HT/NA re-uptake mediated anti-nociception after nerve injury.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Descending input from limbic and cortical structures involved in the cognitive appraisal of pain is integrated with ascending nociceptive transmission within the midbrain periaqueductal grey (PAG). Reciprocal connections are made via the PAG with the rostral ventromedial medulla (RVM) and the dorsolateral pontine tegmentum (DLPT), two structures which send serotonin (5-HT)-containing and noradrenaline (NA)-containing projections, respectively, to the spinal dorsal horn (Millan 2002). It is now well established that damage to nerves arising as a consequence of viral infection, metabolic disturbance or direct physical insult induces plasticity changes within the dorsal horn, which underlie central sensitisation and manifest behaviourally as allodynia and hyperalgesia (Woolf and Salter 2000; Blackburn-Munro 2004). Crucially, a shift in the balance between descending inhibitory and facilitatory inputs also appears to contribute to the mechanistic processes involved in the maintenance of central sensitisation (Ren and Dubner 2002; Burgess et al. 2002; Gardell et al. 2003).
Antidepressants can increase extracellular levels of 5-HT, NA and, to a lesser extent, dopamine (DA) via modulation of pre/postsynaptic receptor function or more commonly via inhibition of transporter function and subsequent block of presynaptic transmitter uptake (Stahl 1998). Tricyclic antidepressants act to non-selectively block the re-uptake of 5-HT and/or NA and are widely used in the clinical treatment of neuropathic pain (Sindrup and Jensen 2001). However, additional mechanisms of action mediated via muscarinic, histaminergic and α-adrenergic receptors contribute to a poor side effect profile and limited patient compliance (MacFarlane et al. 1997; Dworkin et al. 2003). Intuitively, therefore, it might be expected that administration of re-uptake inhibitors selective for either 5-HT or NA re-uptake [selective serotonin re-uptake inhibitors (SSRIs) and noradrenaline re-uptake inhibitors (NRIs), respectively] should circumvent this issue (Bymaster et al. 2003). However, a relative lack of evidence supporting the use of such drugs as typified by citalopram, fluoxetine and reboxetine in treating neuropathic pain (Sindrup et al. 1992; Smith 1998; Canavero et al. 2002) has paved the way for dual mechanism of action 5-HT and NA re-uptake inhibitors in this regard (Briley 2003). Thus, milnacipran, venlafaxine and duloxetine have all variously been reported to alleviate pain in patients with fibromyalgia, polyneuropathy and diabetic neuropathy (Sindrup et al. 2003; Sayar et al. 2003; Arnold et al. 2004; Rowbotham et al. 2004; Vitton et al. 2004). Bupropion is a selective NA and DA re-uptake inhibitor with no serotonergic activity (Stahl et al. 2004). Whilst bupropion has been shown to be effective and well tolerated in the clinical treatment of neuropathic pain (Semenchuk et al. 2001), to our knowledge, it has never been tested in animal models of persistent and neuropathic pain.
Recently, we and others have shown that antidepressants that act to increase both NA and 5-HT levels appear to have a more favourable anti-nociceptive profile than those which increase 5-HT alone in animal models of experimental pain (Iyengar et al. 2004; Bomholt et al. 2005). To further elucidate the relative contribution of 5-HT, NA and DA re-uptake mechanisms in anti-nociception, we have tested the antidepressants fluoxetine, reboxetine, venlafaxine and bupropion in rat models of acute, persistent and neuropathic pain. For comparative purposes, the anti-epileptic gabapentin was also tested.
Materials and methods
Animals
Adult male Sprague–Dawley rats (Harlan Scandinavia, Allerød, Denmark) were used. The animals were housed in groups (three to four per cage except where stated) on soft bedding with food and water available ad libitum in a temperature-controlled environment with a light/dark cycle of 12:12 h. The animals were allowed to habituate to the housing facilities for at least 1 week prior to surgery or behavioural testing. All experiments were performed according to the Ethical Guidelines of the International Association for the Study of Pain (Zimmermann 1983) and in accordance with the Danish legislation of animal use for scientific procedures as described in the ‘Animal Testing Act’.
Rotarod test
In normal, uninjured rats (body weight 250–350 g), changes in motor performance after drug administration were measured using an accelerating rotarod (Ugo Basile, Comero, Italy; Blackburn-Munro et al. 2004). The rotarod speed was increased from 3–30 rpm over a 180-s period, with the maximum time spent on the rod set at 180 s. Rats received two training trials (separated by 3–4 h) on 2 separate days prior to drug testing for acclimatisation purposes. On the day of testing, a baseline response was obtained, rats were subsequently administered drug or vehicle and the time course of motor performance was tested 30 and 60 min after injection. The minimum time possible to spend on the rod was 0 s.
Acute pain, tail-flick test
For the tail-flick test, a radiant heat source (Ugo Basile) was focused on the underside of the tail 3 cm from its distal end in normal, uninjured rats (body weight 230–320 g), as described previously (Blackburn-Munro et al. 2004). The apparatus was calibrated to give a tail-flick latency of approximately 4–6 s (15 s automatic cut-off) prior to drug injection, enabling increases or decreases in tail-flick latency to be measured to the nearest 0.1 s. Baseline measurements (two measurements separated by 5 min) were made 2 days prior to testing to familiarise the animals with the testing procedure. Two further baseline latency measurements were obtained on the day of drug testing to ensure that consistent reflex responses were present. Animals were then administered drug or vehicle according to the experimental paradigm, and the latency responses were determined between 30, 60, 90, 120 and 180 min post-injection depending on the drug administered.
Persistent pain, formalin test
Assessment of formalin-induced flinching behaviour in normal, uninjured rats (body weight 150–180 g) was made with the use of an Automated Nociception Analyser (University of California, San Diego, USA; Yaksh et al. 2001). Briefly, this involved placing a small C-shaped metal band (10 mm wide×27 mm long) around the hindpaw of the rat to be tested. Each rat (four rats were included in each testing session) was administered drug or vehicle according to the experimental paradigm being followed and then placed in a cylindrical acrylic observation chamber (diameter 30.5 cm and height 15 cm). Individual rats were then gently restrained, and formalin (5% in saline, 50 μl s.c.) was injected into the dorsal surface of the hindpaw using a 27G needle. They were then returned to their separate observation chambers, each of which were in turn situated upon an enclosed detection device consisting of two electromagnetic coils designed to produce an electromagnetic field in which movement of the metal band could be detected. The analogue signal was then digitised, and a software algorithm was applied to enable discrimination of flinching behaviour from other paw movements. A sampling interval of 1 min was used, and on the basis of the resulting response patterns, three phases of nociceptive behaviour were identified and scored: first phase (0–5 min), interphase (6–15 min) and second phase (16–30 min) (Blackburn-Munro et al. 2004).
Neuropathic pain, chronic constriction injury and spinal nerve ligation procedure
A chronic constriction injury (CCI) was performed in rats (body weight 180–220 g at the time of surgery), as described previously (Bennett and Xie 1988). Anaesthesia was induced and maintained by 2% isoflurane (Baxter, Denmark) and combined with oxygen (30%) and nitrous oxide (68%). The sciatic nerve was exposed at the mid-thigh level proximal to the sciatic trifurcation. Four chromic gut ligatures (4/0) (Ethicon, NJ, USA) were tied loosely around the nerve, 1–2 mm apart, such that the vascular supply was not compromised.
Segmental spinal nerve ligation (SNL) of the L5 spinal nerve was performed in rats (body weight 150–200 g at the time of surgery), as described previously (Kim and Chung 1992). Animals were anaesthetised with a Hypnorm–Dormicum–H2O mixture (1:1:2; 0.2 ml/100 g s.c.). A dorsal midline incision was made at the left lower lumbar and sacral levels, and blunt dissection was used to expose the L6 transverse process. After removal of the L6 transverse process (close to the body of the vertebrae), the L5 nerve was carefully freed and tightly ligated with 4/0 silk suture at a point just distal to the dorsal root ganglia.
In all CCI and SNL rats, the overlying muscle was closed in layers with 4/0 synthetic absorbable surgical suture. The skin was closed and sutured with 4/0 silk thread (CCI) or with wound clips (SNL). Any CCI or SNL rats that subsequently showed overt behavioural disturbances unrelated to the nerve injury procedure were excluded from further behavioural testing.
Behavioural testing of nerve-injured animals
Nerve-injured rats were routinely tested for the presence of pain-like behaviours for up to 14 days after surgery, according to previously described methods (Blackburn-Munro et al. 2004; Bomholt et al. 2005).
For testing of mechanical allodynia, individual rats were removed from their home cage and allowed to habituate for 15 min in a perspex chamber placed upon an elevated metal grid allowing access to the plantar surface of the injured hindpaw. The presence of mechanical allodynia was assessed using a series of calibrated von Frey hairs (0.059–19.4 g; Stoelting, IL, USA), which were applied to the plantar surface of the hindpaw with increasing force until the individual filament used just started to bend. The filament was applied for a period of 1–2 s and was repeated five times at 1–2 s intervals. The filament that induced a reflex paw withdrawal in three out of five applications was considered to represent the threshold level for a mechanical allodynic response to occur. To test for the presence of thermal hyperalgesia, the plantar surface of the paw was exposed to a beam of radiant heat through a transparent perspex surface (Ugo Basile). The withdrawal duration was recorded, with a minimal time of 0.5 s and a cut-off time of 15 s to prevent tissue damage from occurring. The heat stimulation was repeated enabling a mean value to be obtained for the paw withdrawal latency (s).
During an experimental testing session, six animals were observed in total. These were subdivided into two groups. After mechanical testing was completed at a given time point for three animals (5–10 min duration), they were placed in the thermal testing chamber and allowed to habituate for 5–10 min. The remaining three animals then underwent mechanical testing. Animals were allowed to recover for 2–3 min between von Frey and pinprick testing. After the second group of three animals had been tested, the first three animals were then ready for thermal testing. On the day of drug testing, this paradigm was repeated throughout the duration of the experiment. Drug injection between the two subgroups was delayed accordingly. All drug testing in nerve-injured animals was performed blind by the observer, using an escalating dose crossover paradigm. A 2- to 3-day drug washout period was allowed, and the studies were conducted between days 12 and 30 after surgery. Only those animals with distinct neuropathic behaviour were included in the study. On the day of testing, two baseline measurements were made prior to drug injection, and the effect of the drug on the behavioural response was monitored at 30- to 60-min intervals for a test period up to a maximum of 120–180 min.
Drugs
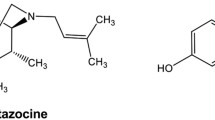
Gabapentin [1-(aminomethyl)cyclohexaneacetic acid] was obtained from capsules containing 21 w/w% lactose (United Nordic Pharma A/S, Hørsholm, Denmark). Fluoxetine hydrochloride [(±)-N-methyl-3-phenyl-3-[(α,α,α-trifluoro-p-tolyl)oxy]propylamine, HCl] was obtained from Siegfried Ltd., Zofingen, Germany. Reboxetine [(±)-(2R*)-2-[(αR*)-α-(o-ethoxyphenoxy)benzyl]morpholine] was obtained as the fumarate salt after purification from Edronax tablets (United Nordic Pharma A/S) within the Department of Chemistry at NeuroSearch A/S. Bupropion hydrochloride [(±)-1-[3-chlorophenyl]-2-[(1,1-dimethyl)amino]-1-propanone, HCl] was obtained from Sigma-Aldrich, Steinheim, Germany. Venlafaxine hydrochloride [(±)-1-[(dimethyl-amino)methyl]-p-methoxybenzyl] cyclohexanol, HCl] was obtained from Cadila Healthcare Limited, Gujarat, India. All drugs were administered intraperitoneally (i.p.) with the doses expressed as milligram salt per kilogram body weight (mg/kg).
Calculation of percent maximum possible effect values and statistical analysis
To enable a comparison of drug effects between injured and non-injured rats across the battery of behavioural tests employed in the current study, raw data was converted to percent maximum possible effect (%MPE) according to the equation:\(\% {\text{MPE = }}{\left( {{\left[ {{\text{Post - treatment}}\,{\text{value}}} \right]} - {\left[ {{\text{Pre - treatment}}\,{\text{value}}} \right]}} \right)} \times {100} \mathord{\left/ {\vphantom {{100} {{\text{ceiling}}\,{\text{value}}\,{\text{of}}\,{\text{assay}} - {\left[ {{\text{Pre - treatment}}\,{\text{value}}} \right]}.}}} \right. \kern-\nulldelimiterspace} {{\text{ceiling}}\,{\text{value}}\,{\text{of}}\,{\text{assay}} - {\left[ {{\text{Pre - treatment}}\,{\text{value}}} \right]}.}\)
Subsequent analysis of the data was performed using Statistica 6.1 for Windows and Sigmastat for Windows (v2.03; SPSS Inc.). All data are presented as mean±SEM. One-way analysis of variance (ANOVA) was used to analyse the overall effects of treatments. When the F value was significant, this was followed by Dunnett's test or Bonferroni's t test, respectively. P<0.05 was considered to be statistically significant.
Results
Rotarod test
To rule out the possibility that rats were unable to initiate a reflex nociceptive response as a result of drug-induced ataxia, general motor function was measured in the rotarod test. One-way ANOVA revealed that motor function was similar between individual experiments as assessed in separate groups of normal, uninjured rats subsequently administered injection of vehicle [range 130±21–172±8 s, treatment effect F(4,39)=1.617, P=0.192] (Table 1). Administration of gabapentin (50–200 mg/kg i.p.) failed to impair motor performance up to 180 min after injection [treatment effect F(3,31)=1.519, P=0.231] (Table 1). Similarly, fluoxetine, reboxetine, bupropion (all 3–30 mg/kg i.p.) and venlafaxine (10–100 mg/kg i.p.) had no significant effect on motor performance at any of the doses tested at 30 or up to 120 min after administration when compared with corresponding vehicle treatment [F(3,31)=0.628, P=0.603; F(3,31)=1.203, P=0.317; F(3,31)=0.222, P=0.880 and F(3,37)=1.429, P=0.251, respectively].
Tail-flick test
To test for a possible spinal site of analgesic action on acute nociceptive processing, drugs were administered to normal, uninjured rats in the tail-flick test (Le Bars et al. 2001). A significant effect of gabapentin treatment on the reflex latency response in normal, uninjured rats was observed [F(3,31)=3.038, P<0.05]. However, the %MPE response was relatively small for rats administered 100 mg/kg gabapentin (Table 1). Administration of fluoxetine and reboxetine also significantly increased the response to noxious stimulation of the tail [treatment effect F(3,31)=2.980, P<0.05 and F(3,31)=4.946, P<0.01, respectively]. Although one-way ANOVA revealed a significant effect of bupropion treatment on tail-flick latency [treatment effect F(3,31)=0.222, P<0.05], post hoc analysis failed to reveal a selective effect of dose (Table 1). In contrast, no significant effect of venlafaxine administration on tail-flick latency was observed (treatment effect F(3,37)=0.807, P=0.499].
Formalin test
Formalin injection into the rat hindpaw initiates biphasic spontaneous nociceptive behaviours consisting of either flinching and licking and/or biting of the injected paw, which can be tentatively suggested to reflect the sensory and emotional aspects of pain processing, respectively. The first phase in turn can be attributed to direct chemical stimulation of nociceptors, and the second phase can be attributed to peripheral inflammatory processes and subsequent sensitisation of nociceptive spinal neurones (Coderre et al. 1993). Systemic injection of gabapentin (50–200 mg/kg i.p.) 120 min prior to hindpaw formalin injection had no effect on either first-phase or interphase flinching compared with vehicle (Table 2). Second-phase flinching was significantly reduced by prior administration of gabapentin [treatment effect F(3,31)=7.710, P<0.001]. Analysis of the cumulative number of flinches showed that this increase was significantly different from vehicle for rats administered either 50, 100 or 200 mg/kg gabapentin (all P<0.05; Table 2).
Administration of fluoxetine (3–30 mg/kg i.p.) 60 min prior to formalin injection significantly attenuated both first-phase [F(3,31)=3.499, P<0.05] and second-phase [F(3,31)=3.256, P<0.05] flinching behaviour (Table 2). During the second phase of the test, only the highest dose of fluoxetine (30 mg/kg) significantly reduced the cumulative number of flinches compared with vehicle (P<0.05). Injection of reboxetine attenuated hindpaw flinching behaviour across all three phases of the formalin test [F(3,33)=3.622, P<0.05; F(3,33)=4.168, P<0.05; F(3,33)=4.106, P<0.05 for first phase, interphase and second phase, respectively]. More specifically, the total number of flinches measured during interphase and the second phase was significantly attenuated by 10 and 30 mg/kg reboxetine (both P<0.05), compared with injection of vehicle (Table 2). Bupropion injection (3–30 mg/kg i.p.) had no effect on flinching behaviour during either the first phase, interphase or second phase of the test as compared with vehicle (Table 2). Injection of venlafaxine (10–100 mg/kg i.p.) attenuated flinching behaviour during interphase [F(3,31)=3.502, P<0.05]. Furthermore, venlafaxine dose-dependently reduced second-phase flinching [F(3,31)=9.486, P<0.001]. Analysis of the cumulative number of flinches showed that this increase was significantly different from vehicle for rats administered 30 and 100 mg/kg venlafaxine (both P<0.05; Table 2).
Neuropathic pain, chronic constriction injury and spinal nerve ligation
General observations
To assess whether re-uptake inhibition of either 5-HT, NA or DA is associated with selective attenuation of specific neuropathic pain behaviours, antidepressants were tested in the CCI and SNL models of peripheral nerve injury. Following surgery, both CCI and SNL rats developed behavioural signs of mechanical allodynia (observed as an increase in the paw withdrawal threshold in response to von Frey hair stimulation) of the ipsilateral hindpaw (1±0.1 and 0.8±0.1 g, respectively), compared to pre-surgery levels that typically ranged from 8.4–19.4 g. Signs of thermal hyperalgesia (observed as a decrease in the paw withdrawal duration in response to thermal stimulation) of the ipsilateral hindpaw were also observed in CCI and SNL rats (4.8±0.3 and 6.5±0.2 s, respectively), compared to pre-surgery levels that typically ranged from 8–9.4 s.
Effects of gabapentin on mechanical allodynia and thermal hyperalgesia
Systemic administration of gabapentin (50–200 mg/kg i.p.) dose-dependently attenuated mechanical allodynia in both CCI and SNL rats [F(3,46)=10.201, P<0.001 and F(3,28)=11.214, P<0.001, respectively] (Fig. 1a), with the %MPE for anti-allodynia observed from 120–180 min after injection. In contrast, gabapentin had no significant effect on thermal hyperalgesia in either model (Fig. 1b).
The effects of gabapentin on mechanical and thermal hypersensitivity in nerve-injured rats. Immediately after a baseline response had been obtained, either gabapentin (50–200 mg/kg) or vehicle was injected intraperitoneally and the time course of anti-nociceptive actions followed in CCI and SNL rats. a Paw withdrawal threshold (g) in response to von Frey hair stimulation. Typical pre-surgery paw withdrawal threshold levels were 8.4–19.4 g. b Paw withdrawal latency (s) in response to thermal stimulation. Typical pre-surgery paw withdrawal duration levels ranged from 8–9.4 s. Gabapentin produced a dose-dependent reversal of mechanical allodynia in CCI and SNL rats, whereas thermal hyperalgesia was unaffected by administration of gabapentin. Data are presented as mean±SEM %MPE. Eight to 14 rats were included in each group. *P<0.05, **P<0.01 and ***P<0.001 vs. baseline (one-way ANOVA followed by Bonferroni's test)
Effects of re-uptake inhibitors on mechanical allodynia
Fluoxetine (3–30 mg/kg i.p.) injection attenuated mechanical allodynia in CCI rats [F(3,20)=28.543, P<0.001] (Fig. 2a). Although the maximal anti-allodynic action observed for the highest dose of fluoxetine tested was similar between CCI and SNL rats (25.4±3.3 and 21.2±12.5%, respectively), this effect was not significant in SNL rats. Administration of reboxetine (3–30 mg/kg i.p.) had no effect on hindpaw mechanical allodynia in either model (Fig. 2b). In contrast, bupropion (3–30 mg/kg i.p.) administration dose-dependently reversed mechanical allodynia in CCI [F(3,20)=11.144, P<0.001] and SNL (F(3,28)=6.618, P<0.01] rats (Fig. 2c). However, the anti-allodynic action of bupropion was both more potent and pronounced in the SNL model (34.9±7.4%, 3 mg/kg) than in the CCI model (23.2±4.8%, 30 mg/kg). Injection of venlafaxine (3–30 mg/kg i.p.) had no effect on hindpaw mechanical allodynia in either CCI or SNL rats at the doses tested in this study (Fig. 2d). In CCI rats, venlafaxine was also administered at 100 mg/kg (i.p.), but again had no effect on hindpaw mechanical allodynia, compared with vehicle [17±4.2 vs 0±0%, F(4,42)=2.324, P=0.074].
The effects of selective monoamine re-uptake inhibitors on mechanical allodynia in nerve-injured rats. Immediately after a baseline response had been obtained, either drug or vehicle was injected intraperitoneally and the time course of drug actions followed in CCI and SNL rats. Paw withdrawal threshold (g) in response to von Frey hair stimulation is expressed as %MPE. a Fluoxetine (3–30 mg/kg), b reboxetine (3–30 mg/kg), c bupropion (3–30 mg/kg) and d venlafaxine (3–30 mg/kg). Mechanical allodynia of the injured hindpaw was partially reversed by fluoxetine and bupropion in CCI rats. Bupropion also produced a marked reversal of mechanical allodynia in SNL rats. Data are presented as mean±SEM. Six to ten rats were included in each group. *P<0.05, **P<0.01 and ***P<0.001 vs baseline (one-way ANOVA followed by Bonferroni's test)
Effects of re-uptake inhibitors on thermal hyperalgesia
Administration of fluoxetine (3–30 mg/kg) was associated with a small but significant attenuation of hindpaw thermal hyperalgesia in CCI rats [F(3,20)=3.749, P<0.05] only; thermal hyperalgesia was unaffected by fluoxetine in SNL rats (Fig. 3a). Injection of reboxetine, on the other hand, reversed thermal hyperalgesia in both models [F(3,28)=6.859, P<0.001 and F(3,28)=3.913, P<0.05 for CCI and SNL, respectively] (Fig. 3b). For CCI rats in particular, the magnitude of reversal was almost identical in rats administered either the lowest (3 mg/kg, 53.3±10.5%) or highest dose of reboxetine (30 mg, 52.2±11.4%). Administration of bupropion (3–30 mg/kg) was also associated with a small but significant attenuation of hindpaw thermal hyperalgesia in CCI rats [F(3,20)=5.918, P<0.01]; thermal hyperalgesia was unaffected by bupropion in SNL rats (Fig. 3c). In CCI rats, thermal hyperalgesia was dose-dependently reversed [F(4,43)=11.055, P<0.001] by administration of venlafaxine (3–100 mg/kg i.p.), with the magnitude of reversal similar for rats administered either 30 mg/kg [28.5±5.1%, P<0.001] or 100 mg/kg [33.7±6.1%, P<0.001] venlafaxine (Fig. 3d). In contrast, venlafaxine had no effect on thermal hypersensitivity in SNL rats.
The effects of selective monoamine re-uptake inhibitors on thermal hyperalgesia in nerve-injured rats. Immediately after a baseline response had been obtained, either drug or vehicle was injected intraperitoneally and the time course of drug actions followed in CCI and SNL rats. Paw withdrawal latency (s) in response to thermal stimulation is expressed as %MPE. a Fluoxetine (3–30 mg/kg), b reboxetine (3–30 mg/kg), c bupropion (3–30 mg/kg) and d venlafaxine (3–30 mg/kg). Thermal hyperalgesia of the injured hindpaw was partially reversed by bupropion and more markedly by reboxetine and venlafaxine in CCI rats. In contrast, thermal hyperalgesia was largely unaffected by any of the drugs tested in SNL rats with only reboxetine having any effect on this measure of nociception. Data are presented as mean±SEM. Six to ten rats were included in each group. *P<0.05, **P<0.01 and ***P<0.001 vs. baseline (one-way ANOVA followed by Bonferroni's test)
Discussion
The present study describes the comparative anti-nociceptive actions of four monoamine re-uptake inhibitors with diverse mechanisms of action in rat models of persistent and neuropathic pain. In the formalin test, second-phase flinching behaviour was attenuated to a greater extent by the dual re-uptake inhibitor venlafaxine than by the selective re-uptake inhibitors reboxetine or fluoxetine, indicating that combined 5-HT and NA re-uptake inhibition mediates greater anti-nociception in this model. After nerve injury, inhibition of NA re-uptake appeared to preferentially mediate anti-nociception in response to noxious thermal but not innocuous mechanical stimulation. In contrast, whilst mechanical allodynia was minimally attenuated by the SSRI fluoxetine, the DA and NA re-uptake inhibitor bupropion produced a much more robust anti-allodynic effect. Thus, selective monoamine re-uptake inhibitors appear to preferentially attenuate selective nociceptive behaviours in rat models of persistent and neuropathic pain.
As expected, systemic administration of the anti-epileptic gabapentin produced a dose-dependent attenuation of formalin-induced second-phase flinching behaviour in the current study (Singh et al. 1996; Field et al. 1997). Similarly, hindpaw mechanical allodynia was robustly reversed by gabapentin in both CCI and SNL rats (Hunter et al. 1997; Abdi et al. 1998; Field et al. 2002; Luo et al. 2002). Importantly, under the conditions tested here, gabapentin minimally affected acute nociceptive behaviours as represented by either first-phase flinching behaviour in the formalin test or tail-flick latency. Although no motor impairment was observed in the rotarod test, other studies have shown that gabapentin can impair motor function when administered at doses similar to those employed here (≥100 mg/kg) (Hunter et al. 1997). Multiple randomised, controlled clinical trials demonstrating that gabapentin significantly reduces pain compared with placebo have propelled gabapentin into the first-line medications for treatment of neuropathic pain (Backonja et al. 1998; Rowbotham et al. 1998; Morello et al. 1999). Thus, we feel confident that the behavioural assays and models employed herein are sufficiently predictive to enable a preclinical anti-nociceptive profile with relevance to clinical efficacy to be discriminated.
The modulatory actions of descending brainstem monoaminergic pathways have traditionally been considered to dampen pain behaviours, presumably to aid facilitation of escape and survival in response to threatening stimuli (Fields and Basbaum 1999; Martin et al. 1999). However, recent studies indicate that hyperalgesia in animal models of inflammatory and neuropathic pain is also closely correlated with descending pathways which facilitate nociceptive transmission (Millan 2002; Ren and Dubner 2002; Porreca et al. 2002). Thus, the net effect of descending modulation depends on the balance between inhibitory and facilitatory input to the spinal cord (Ren and Dubner 2002). Correspondingly, antidepressants may act to increase descending inhibitory tone or alternatively attenuate the increase in descending facilitatory drive involved in maintaining pain after peripheral nerve injury (Burgess et al. 2002).
Despite the obvious benefits conferred by tricyclic antidepressants in alleviating signs and symptoms of neuropathic pain (Max et al. 1987; Sindrup and Jensen 2001), side effect issues suggest that drugs capable of selectively attenuating the re-uptake of 5-HT and/or NA may provide a more desirable therapeutic profile in neuropathic pain patients. Only limited evidence exists to suggest that SSRIs, such as fluoxetine and citalopram, have analgesic efficacy in neuropathic pain patients (Sindrup et al. 1992; Smith 1998). Similarly, the preclinical evidence demonstrating attenuation of nociceptive behaviours after administration of SSRIs in the formalin test and in animals with peripheral nerve injury is somewhat sparse and not always convincing (Jett et al. 1997; Otsuka et al. 2001). Nevertheless, we have shown here that fluoxetine does partially attenuate formalin-induced and nerve injury-induced nociceptive behaviours, in agreement with previous studies (Nayebi et al. 2001). Indeed, these findings agree closely with those recently reported for the more selective SSRI citalopram in the same animal models (Bomholt et al. 2005). Moreover, the similarity in binding affinities for the human 5-HT transporter reported for fluoxetine and citalopram (K i=1.16 and 0.81 nM, respectively) suggests that selective inhibition of 5-HT re-uptake is the probable mechanism responsible for the comparatively modest degree of anti-nociception observed.
This raises the question as to whether a selective NRI, such as reboxetine, may be more effective in animal pain models (Obata et al. 2005), a hypothesis we have tested directly in the current study. Systemic administration of reboxetine attenuated flinching behaviour in the formalin test and thermal hyperalgesia in CCI rats with a minimal effective dose of 10 and 3 mg/kg, respectively. However, a caveat of our findings is that first-phase flinching behaviour was also attenuated by reboxetine and that the %MPE against second-phase flinching behaviour and thermal hyperalgesia was almost identical in rats administered either 3 or 30 mg/kg reboxetine. Ex vivo binding data obtained for reboxetine in-house (ED50=5.3 mg/kg for inhibition of 3H-NA re-uptake) suggest that the NA transporter may be fully occupied at doses >3 mg/kg. Thus, maximal inhibition of NA re-uptake after acute drug administration does not appear to confer a level of anti-nociception comparable with that observed for gabapentin in animal models of persistent pain.
Various lines of evidence exist to suggest that monoamine re-uptake inhibitors that act to selectively enhance extracellular levels of 5-HT and NA may preferentially mediate superior anti-nociception in animal models of persistent and neuropathic pain. Recently, Iyengar et al. (2004) have shown that administration of low doses of either the NRI thionisoxetine or the SSRI paroxetine fail to attenuate second-phase nociceptive behaviours in the rat formalin test. Crucially, however, when sub-effective doses of these compounds were administered in combination, a significant attenuation of formalin-induced nociceptive behaviour was attained (Iyengar et al. 2004). In extension of these findings, venlafaxine dose-dependently attenuated formalin-induced second-phase nociceptive behaviours in the current study. Venlafaxine has weak affinity for 5-HT and NA transporters (K i=82 and 2,483 nM, respectively) in comparison with other dual re-uptake inhibitors such as duloxetine (K i=0.8 and 7.5 nM, respectively) (Koch et al. 2003). Thus, in rats, venlafaxine may essentially act as an SSRI when administered at low doses (<10 mg/kg i.p.) and only begin to exhibit dual re-uptake properties at doses >30 mg/kg i.p. Consequently, we would propose that the maximal anti-nociceptive effect obtained with venlafaxine in the formalin test was when it was acting a dual re-uptake inhibitor. Similar observations were obtained in CCI rats where thermal hyperalgesia was maximally reversed by 30 and 100 mg/kg venlafaxine, in agreement with previous studies (Lang et al. 1996). Other lines of evidence suggest that the combined involvement of 5-HT and NA pathways mediates maximal anti-nociception in animal models of sustained nociception. For example, the administration of selective inhibitors of both 5-HT or NA synthesis have been shown to reverse the anti-nociceptive actions of venlafaxine in CCI rats (Marchand et al. 2003). Moreover, whereas the dual re-uptake inhibitor duloxetine and the non-selective re-uptake inhibitor amitriptyline attenuate mechanical hyperalgesia and fully reverse thermal hyperalgesia in CCI rats, the SSRI citalopram only partially reverses thermal hyperalgesia (Bomholt et al. 2005). This apparently contrasts with acute nociception since administration of venlafaxine at doses presumed to inhibit re-uptake of 5-HT and NA failed to increase the %MPE measured in the tail-flick test, compared with either lower doses of venlafaxine or indeed with fluoxetine or reboxetine.
Acute administration of bupropion decreases the re-uptake of DA and NA into rat and mouse synaptosomes, reduces the firing rate of central NA- and DA-containing neurones and increases extracellular striatal DA levels (Nomikos et al. 1989; Cooper et al. 1994). The present results indicate that the anti-allodynic action observed for bupropion was consistent between CCI and SNL rats (being more robust in the latter model), in contrast to the other re-uptake inhibitors tested. The inability of reboxetine to reverse mechanical allodynia, in combination with in vitro binding data demonstrating that bupropion is a much weaker inhibitor of NA re-uptake than reboxetine (Wong et al. 2000; Miller et al. 2002; Hajos et al. 2004), might tentatively suggest that inhibition of DA re-uptake accounted for the anti-allodynic action of bupropion. Correspondingly, the inability of bupropion, in contrast to reboxetine, to attenuate formalin-induced nociceptive behaviours and thermal hyperalgesia in CCI rats might similarly be explained by its weak micromolar affinity for the NA transporter in contrast to reboxetine (IC50=0.4 and 0.0002 μM, respectively).
A more circumspect analysis of the data raises the issue that none of the drugs tested have been compared directly against each other within a single experiment in the current study. Thus, we cannot rule out the possibility that random sampling variation within the expected limits of error may account for the different levels of anti-nociception conferred against the varying sensory modalities tested. Ultimately, such a prudent appreciation of the data can arguably only be countered by those cases where drug-mediated anti-nociception was clearly dose-dependent, for example, venlafaxine attenuation of formalin-induced flinching and thermal hyperalgesia in CCI rats. Another mitigating factor in the apparent lack of profound anti-nociceptive actions observed for the different re-uptake inhibitors in the current study may relate to the experimental parameters chosen. We administered drugs at doses that were both shown to be devoid of motor impairing qualities and that minimally attenuated tail-flick latency responses in normal, uninjured rats. As such, it remains possible that a greater degree of anti-nociception may have been obtained either by administering a larger single dose of any of the drugs tested or by utilising a chronic dosing paradigm as has been shown previously for venlafaxine (Marchand et al. 2003).
Conclusions
Whilst fluoxetine, reboxetine and venlafaxine at best minimally attenuated mechanical allodynia after nerve injury, bupropion administration dose-dependently reversed hindpaw withdrawal threshold in CCI rats and more markedly in SNL rats. Although not directly tested in the current study, these observations, when taken together with the contrasting reversal of formalin-induced flinching and nerve-injury-induced thermal hyperalgesia observed with either reboxetine or venlafaxine, suggest that drugs which can inhibit re-uptake of 5-HT, NA and DA may provide a broader spectrum pain relief in animal models of experimental pain than single mechanism of action of re-uptake inhibitors.
References
Abdi S, Lee DH, Chung JM (1998) The anti-allodynic effects of amitriptyline, gabapentin, and lidocaine in a rat model of neuropathic pain. Anesth Analg 87:1360–1366
Arnold LM, Lu Y, Crofford LJ, Wohlreich M, Detke MJ, Iyengar S, Goldstein DJ (2004) A double-blind, multicenter trial comparing duloxetine with placebo in the treatment of fibromyalgia patients with or without major depressive disorder. Arthritis Rheum 50:2974–2984
Backonja M, Beydoun A, Edwards KR, Schwartz SL, Fonseca V, Hes M, LaMoreaux L, Garofalo E (1998) Gabapentin for the symptomatic treatment of painful neuropathy in patients with diabetes mellitus: a randomized controlled trial. JAMA 280:1831–1836
Bennett GJ, Xie YK (1988) A peripheral mononeuropathy in rat that produces disorders of pain sensation like those seen in man. Pain 33:87–107
Blackburn-Munro G (2004) Pain-like behaviours in animals—how human are they? Trends Pharmacol Sci 25:299–305
Blackburn-Munro G, Bomholt SF, Erichsen HK (2004) Behavioural effects of the novel AMPA/GluR5 selective receptor antagonist NS1209 after systemic administration in animal models of experimental pain. Neuropharmacology 47:351–362
Bomholt SF, Mikkelsen JD, Blackburn-Munro G (2005) Antinociceptive effects of the antidepressants amitriptyline, duloxetine, mirtazapine and citalopram in animal models of acute, persistent and neuropathic pain. Neuropharmacology 48:252–263
Briley M (2003) New hope in the treatment of painful symptoms in depression. Curr Opin Investig Drugs 4:42–45
Burgess SE, Gardell LR, Ossipov MH, Malan TP Jr, Vanderah TW, Lai J, Porreca F (2002) Time-dependent descending facilitation from the rostral ventromedial medulla maintains, but does not initiate, neuropathic pain. J Neurosci 22:5129–5136
Bymaster FP, McNamara RK, Tran PV (2003) New approaches to developing antidepressants by enhancing monoaminergic neurotransmission. Expert Opin Investig Drugs 12:531–543
Canavero S, Bonicalzi V, Paolotti R (2002) Reboxetine for central pain: a single-blind prospective study. Clin Neuropharmacol 25:238–239
Coderre TJ, Fundytus ME, McKenna JE, Dalal S, Melzack R (1993) The formalin test: a validation of the weighted-scores method of behavioural pain rating. Pain 54:43–50
Cooper BR, Wang CM, Cox RF, Norton R, Shea V, Ferris RM (1994) Evidence that the acute behavioral and electrophysiological effects of bupropion (Wellbutrin) are mediated by a noradrenergic mechanism. Neuropsychopharmacology 11:133–141
Dworkin RH, Backonja M, Rowbotham MC, Allen RR, Argoff CR, Bennett GJ, Bushnell MC, Farrar JT, Galer BS, Haythornthwaite JA, Hewitt DJ, Loeser JD, Max MB, Saltarelli M, Schmader KE, Stein C, Thompson D, Turk DC, Wallace MS, Watkins LR, Weinstein SM (2003) Advances in neuropathic pain: diagnosis, mechanisms, and treatment recommendations. Arch Neurol 60:1524–1534
Field MJ, Oles RJ, Lewis AS, McCleary S, Hughes J, Singh L (1997) Gabapentin (neurontin) and S-(+)-3-isobutylgaba represent a novel class of selective antihyperalgesic agents. Br J Pharmacol 121:1513–1522
Field MJ, Gonzalez MI, Tallarida RJ, Singh L (2002) Gabapentin and the neurokinin(1) receptor antagonist CI-1021 act synergistically in two rat models of neuropathic pain. J Pharmacol Exp Ther 303:730–735
Fields HL, Basbaum AI (1999) Central nervous system mechanisms of pain modulation. In: Wall PD, Melzack R (eds) Textbook of pain, 4th edn. Churchill-Livingstone, Edinburgh, pp 309–330
Gardell LR, Vanderah TW, Gardell SE, Wang R, Ossipov MH, Lai J, Porreca F (2003) Enhanced evoked excitatory transmitter release in experimental neuropathy requires descending facilitation. J Neurosci 23:8370–8379
Hajos M, Fleishaker JC, Filipiak-Reisner JK, Brown MT, Wong EH (2004) The selective norepinephrine reuptake inhibitor antidepressant reboxetine: pharmacological and clinical profile. CNS Drug Rev 10:23–44
Hunter JC, Gogas KR, Hedley LR, Jacobson LO, Kassotakis L, Thompson J, Fontana DJ (1997) The effect of novel anti-epileptic drugs in rat experimental models of acute and chronic pain. Eur J Pharmacol 324:153–160
Iyengar S, Webster AA, Hemrick-Luecke SK, Xu JY, Simmons RM (2004) Efficacy of duloxetine, a potent and balanced serotonin-norepinephrine reuptake inhibitor in persistent pain models in rats. J Pharmacol Exp Ther 311:576–584
Jett MF, McGuirk J, Waligora D, Hunter JC (1997) The effects of mexiletine, desipramine and fluoxetine in rat models involving central sensitization. Pain 69:161–169
Kim SH, Chung JM (1992) An experimental model for peripheral neuropathy produced by segmental spinal nerve ligation in the rat. Pain 50:355–363
Koch S, Hemrick-Luecke SK, Thompson LK, Evans DC, Threlkeld PG, Nelson DL, Perry KW, Bymaster FP (2003) Comparison of effects of dual transporter inhibitors on monoamine transporters and extracellular levels in rats. Neuropharmacology 45:935–944
Lang E, Hord AH, Denson D (1996) Venlafaxine hydrochloride (Effexor) relieves thermal hyperalgesia in rats with an experimental mononeuropathy. Pain 68:151–155
Le Bars D, Gozariu M, Cadden SW (2001) Animal models of nociception. Pharmacol Rev 53:597–652
Luo ZD, Calcutt NA, Higuera ES, Valder CR, Song YH, Svensson CI, Myers RR (2002) Injury type-specific calcium channel alpha 2 delta-1 subunit up-regulation in rat neuropathic pain models correlates with antiallodynic effects of gabapentin. J Pharmacol Exp Ther 303:1199–1205
MacFarlane BV, Wright A, O'Callaghan J, Benson HA (1997) Chronic neuropathic pain and its control by drugs. Pharmacol Ther 75:1–19
Marchand F, Alloui A, Chapuy E, Jourdan D, Pelissier T, Ardid D, Hernandez A, Eschalier A (2003) Evidence for a monoamine mediated, opioid-independent, antihyperalgesic effect of venlafaxine, a non-tricyclic antidepressant, in a neurogenic pain model in rats. Pain 103:229–235
Martin WJ, Gupta K, Loo CM, Rohde DS, Basbaum AI (1999) Differential effects of neurotoxic destruction of descending noradrenergic pathways on acute and persistent nociceptive processing. Pain 80:57–65
Max MB, Culnane M, Schafer SC, Gracely RH, Walther DJ, Smoller B, Dubner R (1987) Amitriptyline relieves diabetic neuropathy pain in patients with normal or depressed mood. Neurology 37:589–596
Millan MJ (2002) Descending control of pain. Prog Neurobiol 66:355–474
Miller DK, Wong EH, Chesnut MD, Dwoskin LP (2002) Reboxetine: functional inhibition of monoamine transporters and nicotinic acetylcholine receptors. J Pharmacol Exp Ther 302:687–695
Morello CM, Leckband SG, Stoner CP, Moorhouse DF, Sahagian GA (1999) Randomized double-blind study comparing the efficacy of gabapentin with amitriptyline on diabetic peripheral neuropathy pain. Arch Intern Med 159:1931–1937
Nayebi AR, Hassanpour M, Rezazadeh H (2001) Effect of chronic and acute administration of fluoxetine and its additive effect with morphine on the behavioural response in the formalin test in rats. J Pharm Pharmacol 53:219–225
Nomikos GG, Damsma G, Wenkstern D, Fibiger HC (1989) Acute effects of bupropion on extracellular dopamine concentrations in rat striatum and nucleus accumbens studied by in vivo microdialysis. Neuropsychopharmacology 2:273–279
Obata H, Conklin D, Eisenach JC (2005) Spinal noradrenaline transporter inhibition by reboxetine and Xen2174 reduces tactile hypersensitivity after surgery in rats. Pain 113:271–276
Otsuka N, Kiuchi Y, Yokogawa F, Masuda Y, Oguchi K, Hosoyamada A (2001) Antinociceptive efficacy of antidepressants: assessment of five antidepressants and four monoamine receptors in rats. J Anesth 15:154–158
Porreca F, Ossipov MH, Gebhart GF (2002) Chronic pain and medullary descending facilitation. Trends Neurosci 25:319–325
Ren K, Dubner R (2002) Descending modulation in persistent pain: an update. Pain 100:1–6
Rowbotham M, Harden N, Stacey B, Bernstein P, Magnus-Miller L (1998) Gabapentin for the treatment of postherpetic neuralgia: a randomized controlled trial. JAMA 280:1837–1842
Rowbotham MC, Goli V, Kunz NR, Lei D (2004) Venlafaxine extended release in the treatment of painful diabetic neuropathy: a double-blind, placebo-controlled study. Pain 110:697–706
Sayar K, Aksu G, Ak I, Tosun M (2003) Venlafaxine treatment of fibromyalgia. Ann Pharmacother 37:1561–1565
Semenchuk MR, Sherman S, Davis B (2001) Double-blind, randomized trial of bupropion SR for the treatment of neuropathic pain. Neurology 57:1583–1588
Sindrup SH, Jensen TS (2001) Antidepressants in the treatment of neuropathic pain. In: Hansson PT, Fields HL, Hill RG, Marchettini P (eds) Neuropathic pain: pathophysiology and treatment. IASP Press, Seattle, pp 169–183
Sindrup SH, Bjerre U, Dejgaard A, Brosen K, Aaes-Jorgensen T, Gram LF (1992) The selective serotonin reuptake inhibitor citalopram relieves the symptoms of diabetic neuropathy. Clin Pharmacol Ther 52:547–552
Sindrup SH, Bach FW, Madsen C, Gram LF, Jensen TS (2003) Venlafaxine versus imipramine in painful polyneuropathy: a randomized, controlled trial. Neurology 60:1284–1289
Singh L, Field MJ, Ferris P, Hunter JC, Oles RJ, Williams RG, Woodruff GN (1996) The antiepileptic agent gabapentin (Neurontin) possesses anxiolytic-like and antinociceptive actions that are reversed by D-serine. Psychopharmacology 127:1–9
Smith AJ (1998) The analgesic effects of selective serotonin reuptake inhibitors. J Psychopharmacol 12:407–413
Stahl SM (1998) Basic psychopharmacology of antidepressants, part 1: antidepressants have seven distinct mechanisms of action. J Clin Psychiatry 59(Suppl 4):5–14
Stahl SM, Pradko JF, Haight BR, Modell JG, Rockett CB, Learned-Coughlin S (2004) A review of the neuropharmacology of bupropion, a dual norepinephrine and dopamine reuptake inhibitor. Prim Care Companion J Clin Psychiat 6:159–166
Vitton O, Gendreau M, Gendreau J, Kranzler J, Rao SG (2004) A double-blind placebo-controlled trial of milnacipran in the treatment of fibromyalgia. Hum Psychopharmacol 19(Suppl 1):S27–S35
Woolf CJ, Salter MW (2000) Neuronal plasticity: increasing the gain in pain. Science 288:1765–1769
Wong EH, Sonders MS, Amara SG, Tinholt PM, Piercey MF, Hoffmann WP, Hyslop DK, Franklin S, Porsolt RD, Bonsignori A, Carfagna N, McArthur RA (2000) Reboxetine: a pharmacologically potent, selective, and specific norepinephrine reuptake inhibitor. Biol Psychiatry 47:818–829
Yaksh TL, Ozaki G, McCumber D, Rathbun M, Svensson C, Malkmus S, Yaksh MC (2001) An automated flinch detecting system for use in the formalin nociceptive bioassay. J Appl Physiol 90:2386–2402
Zimmermann M (1983) Ethical guidelines for investigations of experimental pain in conscious animals. Pain 16:109–110
Acknowledgements
LHP was supported by the Danish Academy of Technical Sciences. Expert technical assistance was provided by Nete Ibsen, Helene Dyhr Pedersen and Paula Lindberg.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pedersen, L.H., Nielsen, A.N. & Blackburn-Munro, G. Anti-nociception is selectively enhanced by parallel inhibition of multiple subtypes of monoamine transporters in rat models of persistent and neuropathic pain. Psychopharmacology 182, 551–561 (2005). https://doi.org/10.1007/s00213-005-0120-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-005-0120-6