Abstract
Rationale
Antipsychotics exert therapeutic effects by modulating various cellular signalling pathways and several types of receptors, including PKA- and GSK3β-mediated signalling pathways, and NMDA receptors. The ventral midbrain, mainly containing the ventral tegmental area (VTA) and substantia nigra (SN), are the nuclei with dopamine origins in the brain, which are also involved in the actions of antipsychotics. Whether antipsychotics can modulate these cellular pathways in the ventral midbrain is unknown.
Objective
This study aims to investigate the effects of antipsychotics, including aripiprazole (a dopamine D2 receptor (D2R) partial agonist), bifeprunox (a D2R partial agonist), and haloperidol (a D2R antagonist) on the PKA- and GSK3β-mediated pathways and NMDA receptors in the ventral midbrain.
Methods
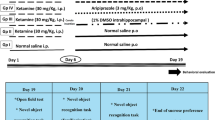
Male rats were orally administered aripiprazole (0.75 mg/kg, t.i.d. (ter in die)), bifeprunox (0.8 mg/kg, t.i.d.), haloperidol (0.1 mg/kg, t.i.d.) or vehicle for either 1 week or 10 weeks. The levels of PKA, p-PKA, Akt, p-Akt, GSK3β, p-GSK3β, Dvl-3, β-catenin, and NMDA receptor subunits in the ventral midbrain were assessed by Western Blots.
Results
The results showed that chronic antipsychotic treatment with aripiprazole selectively increased PKA activity in the VTA. Additionally, all three drugs elevated the activity of the Akt–GSK3β signalling pathway in a time-dependent manner, while only aripiprazole stimulated the Dvl-3–GSK3β–β-catenin signalling pathway in the SN. Furthermore, chronic administration with both aripiprazole and haloperidol decreased the expression of NMDA receptors.
Conclusion
This study suggests that activating PKA- and GSK3β-mediated pathways and downregulating NMDA receptor expression in the ventral midbrain might contribute to the clinical effects of antipsychotics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Schizophrenia is a devastating mental disorder. Currently, all antipsychotics control symptoms of schizophrenia mainly by targeting the dopamine D2 receptor (D2R) (Ginovart and Kapur 2012). The ventral midbrain, including ventral tegmental area (VTA) and substantia nigra (SN), is a centre of dopamine that contains the cell bodies of a large number of dopamine neurons projecting their axons to many other brain regions including the nucleus accumbens (NAc) and caudate putamen (CPu), forming mesolimbic (VTA–NAc) and nigrostriatal (SN–CPu) dopaminergic transmission pathways.
Dopamine neurons in the VTA receive excitatory glutamatergic inputs from various brain regions, including the prefrontal cortex, laterodorsal tegmental nucleus, and pedunculopontine tegmental nucleus (Morikawa and Paladini 2011). When these glutamatergic neurons are activated, the firing rates of dopamine neurons in the VTA are increased. Dopamine neurons in the SN also receive excitatory glutamatergic inputs from various brain areas. For example, a glutamatergic projection is sent to the pars reticulate from the subthalamic nucleus, exerting an excitatory effect on SN neurons (Morikawa and Paladini 2011). The ventral midbrain may be playing a pivotal role in the treatment of schizophrenia by antipsychotics either directly or indirectly; however, little attention has been paid to this brain area, and as a result, the ventral midbrain has generally not been studied as extensively as other brain areas such as the striatum.
Alternative mRNA splicing generates two isoforms of the dopamine D2 receptor: the long and short isoforms (Dal Toso et al. 1989). In the ventral midbrain, short-form dopamine D2 autoreceptors are largely presented at the pre-synapses, which generally provide a feedback mechanism that adjusts dopamine synthesis capacity and release (Carlsson and Lindqvist 1963; Sibley 1999; Wolf and Roth 1990). The G protein–dependent PKA (protein kinase A) pathway is a canonical D2R-downstream signalling pathway, and it has been shown that long-term activation of D2 autoreceptors decreases phosphorylation of tyrosine hydroxylase via PKA inducing reduced dopamine synthesis, packaging, and release (Ford 2014).
The Akt (protein kinase B)–GSK (glycogen synthase kinase)3β signalling pathway is a G protein–independent pathway of the D2R. It has been reported by many studies that various antipsychotics exerted their therapeutic effects via activating the Akt–GSK3β signalling pathway (Alimohamad et al. 2005a, b; Allen et al. 2011; Beaulieu et al. 2009; Li et al. 2007; Pan et al. 2016a, b). Additionally, a previous study reported that activating the short isoform of D2Rs leads to stimulation of Akt–GSK3β signalling in HEK (human embryonic kidney)-293/rD2S cells. However, whether short isoforms of D2Rs regulate Akt–GSK3β signalling in vivo remains unclear. Furthermore, the GSK3β-mediated Dvl-3–β-catenin signalling pathway is another GSK3β-mediated signalling pathway that is related to the effects of antipsychotics. Previous evidence indicates that many antipsychotics (including typical and atypical antipsychotics) are able to alter the expression of Dvl-3 and β-catenin in various brain regions (Alimohamad et al. 2005a, b; Pan et al. 2016a, b; Seo et al. 2015; Sutton and Rushlow 2011). However, whether antipsychotics modulate GSK3β-mediated Dvl-3–β-catenin signalling via short isoforms of D2Rs is unknown.
Therefore, the present study also investigated the effects of these antipsychotics on PKA, Akt–GSK3β, and Dvl-3–β-catenin signalling in the ventral midbrain, in order to understand the possible actions of D2R short isoforms in the ventral midbrain under the influences of antipsychotics. Since dopamine neurons in the ventral midbrain receive glutamatergic inputs, the present study also investigated antipsychotic modulation of the NMDA (N-methyl-D-aspartic acid) receptor in the ventral midbrain. Moreover, since patients always experience long-term antipsychotic treatment under clinical conditions, this project investigated the effects of not only short-term (1 week), but also chronic (10 weeks), administration of these antipsychotics on these signalling pathways and NMDA receptors.
Methods
Animals and drug administration
Male Sprague-Dawley rats (aged 8 weeks) were obtained from the Animal Resource Centre (Perth, Australia). After arrival, all rats were housed in individual cages under environmentally controlled conditions (temperature 22 °C, light cycle from 07:00 AM to 07:00 PM), with ad libitum access to water and standard laboratory chow diet. All experimental procedures were approved by the Animal Ethics Committee (AE11/02) of the University of Wollongong and complied with the Australian Code of Practice for the Care and Use of Animals for Scientific Purposes 2004. All efforts were made to minimise animal distress and prevent suffering.
The rats were randomly assigned to one of the following drug treatment groups (n = 6/group): aripiprazole (0.75 mg/kg, t.i.d. (ter in die); Otsuka, Japan), bifeprunox (0.8 mg/kg, t.i.d.; Otava, Ukraine), haloperidol (0.1 mg/kg, t.i.d.; Sigma, Australia), or vehicle. Drug powder mixed with the cookie dough pellets was delivered orally 3 times per day at 07:00 AM, 03:00 PM, and 11:00 PM for either 1 week or 10 weeks. This drug administration method aims to mimic the clinical scenario of oral administration and has been well-established by our laboratory (Pan et al. 2016a, b; Pan et al. 2016c). These dosages were transferred from the recommended dosages in clinic based on body surface area, according to the FDA guidelines for clinical trials ((Administration) 2005; Reagan-Shaw et al. 2008). Specifically, 2.25 mg/kg aripiprazole, 2.4 mg/kg bifeprunox, and 0.3 mg/kg haloperidol daily dosages in rats are equivalent to ~ 22 mg, ~ 24 mg, and ~ 3 mg in humans (60 kg body weight), respectively. The selected dosages are within the recommended clinical dosages (Casey et al. 2008; Gardner et al. 2010; Mace and Taylor 2009), which have physiological and behavioural effects in rodents, but do not induce motoric side-effects (Assie et al. 2006; Han et al. 2009; Natesan et al. 2006; Wadenberg 2007). On the sacrifice days, 2 h after the last drug administration, all animals were euthanised with CO2, followed by immediately collecting the brains and freezing in liquid nitrogen. All animals were sacrificed between 09:00 AM and 11:00 AM to minimise circadian-induced variation of protein expression.
Brain dissection
The brain microdissection puncture technique was employed as described previously (Pan et al. 2015; Pan et al. 2016c). According to the brain atlas (Paxinos and Watson 2005), the brain tissues through the ventral midbrain (bregma − 5.40 to − 6.30 mm) were dissected for the VTA and SN. Tissues collected were chilled on dry ice and kept at − 80 °C for future use.
Western Blots
Western Blot experiments were performed as described previously (Pan et al. 2015; Pan et al. 2016c). Briefly, frozen brain samples were homogenised in homogenising buffer (NP-40 cell lysis buffer (Invitrogen, #FNN0021) mixed with Protease Inhibitor Cocktail (Sigma-Aldrich, #P8340), β-glycerophosphate (Sigma-Aldrich, #G9422), and phenylmethylsulfonyl fluoride (Sigma-Aldrich, #P7626)). The protein concentration of each sample was determined by the DC Protein Assay (Bio-Rad, #500-0111). Each sample containing 10 μg of protein was loaded into 4–20% Criterion™ TGX™ Precast Gels (Bio-Rad, #5671095). The gels were run vertically using Criterion™ Vertical Electrophoresis Cells (Bio-Rad, #1656001), and then the proteins were electrophoretically transferred to polyvinylidene difluoride membranes using Criterion™ Blotters (Bio-Rad, #1704071). All membranes were blocked with 5% skim milk powder and incubated with primary antibodies. To visualise the immunoreactive bands, Amersham Hyperfilm ECL (GE Healthcare, #28-9068-36) and Luminata Classico Western HRP substrate (Millipore, #WBLUC0500) were used. All Western Blot experiments were performed in duplicate to ensure consistency.
The antibodies and their dilutions used in the present study included anti-PKA-C (1:2000; Santa Cruz, #SC-903), anti-phosphor-PKA-C (1:1000; Thr197) (Cell Signalling, #5661), anti-Akt (1:2000; Cell Signalling, #4691), anti-phosphor-Akt (Thr308) (1:1000; Cell Signalling, #13038), anti-GSK3β (1:2000; Cell Signalling, #5676), anti-phospho-GSK3β (Ser9) (1:1000; Cell Signalling, #9322), anti-Dvl-3 (1:1000; Santa Cruz Biotechnology, #SC-8027), anti-β-catenin (1:1000; Santa Cruz Biotechnology, #SC-7963), anti-CREB1 (1:2000, Abcam, #ab32515), anti-phospho-CREB1 (1:2000, Abcam, #ab32096), anti-NMDA NR1 (1:2000, Abcam, #ab109182), and anti-NMDA NR2A (1:500, Abcam, #ab124913). Mouse anti-actin primary polyclonal antibody (1:10000; Millipore, #MAB1501) was used to determine the actin levels. Secondary antibodies included HRP-conjugated anti-rabbit IgG antibody (1:3000; Cell Signalling, #7074) and HRP-conjugated anti-mouse IgG antibody (1:3000; Cell Signalling, #7076).
Statistics
All data were analysed using SPSS Statistics (Version 24). The immunoreactive signals were quantified using Bio-Rad Image Lab (Version 6). The data of every protein obtained by Bio-Rad Image Lab were corrected with their corresponding actin levels. Then, data normal distribution was examined using histograms and Kolmogorov-Smirnov Z tests, followed by one-way analysis of variance (ANOVA) if the data were normally distributed. The post hoc Dunnett’s test was selected to compare each drug administration group with their corresponding control group. The results were normalised and expressed by taking the value of the control group as 100%. Statistical significance was accepted when p ≤ 0.05.
Results
Antipsychotic modulation of PKA activity
In the VTA, after 1-week antipsychotic administration, it was shown that the expression of PKA-C (F3, 20 = 10.097, p < 0.01) and the ratio of p-PKA-C/PKA-C (F3, 20 = 2.357, p < 0.05) was significantly affected. Post hoc tests indicated that all three chemicals reduced the protein levels of total PKA-C (aripiprazole, − 20.0%, p < 0.05; bifeprunox, − 16.6%, p < 0.05; haloperidol, − 39.0%, p < 0.01); however, only haloperidol significantly affected the ratio of p-PKA-C/PKA-C (p < 0.05) (Fig. 1A, B, C).
The modulations by three antipsychotics of PKA activity. The effects of aripiprazole (ARI), bifeprunox (BIF), and haloperidol (HAL) on PKA activity were measured in the ventral tegmental area (VTA) and substantia nigra (SN): VTA 1 week (A), VTA 10 weeks (B), SN 1 week (C), and SN 10 weeks (D). The representative bands of Western Blot are shown in (E). PKA was quantified at 42 kDa; p-PKA was quantified at 42 kDa. The sample size is six per group. The data were normalised by taking the average value of the control group as 100% and expressed as mean ± S.E.M. (*p ≤ 0.05, **p < 0.01 vs the control)
Also, in the VTA, after 10-week antipsychotic administration, ANOVA tests indicated that the levels of p-PKA-C (F3, 20 = 3.134, p < 0.05) and the ratio of p-PKA-C/PKA-C (F3, 20 = 5.536, p < 0.01) were significantly affected. In comparison with the controls, aripiprazole decreased the levels of p-PKA-C (− 17.6%, p < 0.05) as well as the ratio of p-PKA-C/PKA-C (p < 0.01) (Fig. 1B, C, E).
In the SN, after 1-week antipsychotic administration, the results showed that the levels of PKA-C (F3, 20 = 10.090, p < 0.01) and p-PKA-C (F3, 20 = 4.821, p < 0.05) were significantly altered. Post hoc tests revealed that both aripiprazole and haloperidol significantly elevated the levels of total PKA-C (aripiprazole, + 20.6%, p < 0.01; haloperidol, + 27.2%, p < 0.01), and haloperidol also increased p-PKA-C (+ 41.7%, p < 0.01) (Fig. 1C, E). However, no drug changed the ratio of p-PKA-C/PKA-C (all p > 0.05). After 10-week antipsychotic administration, no antipsychotic drug significantly altered PKA activity in the SN (Fig. 1D, E, F).
Antipsychotic modulation of Akt–GSK3β signalling pathway
In the VTA, after 1-week antipsychotic administration, it was revealed that the levels of total Akt, p-Akt, and the ratio of p-Akt/Akt was significantly affected (Akt, F3, 20 = 4.622, p < 0.05; p-Akt, F3, 20 = 2.958, p < 0.05; p-Akt/Akt, F3, 20 = 3.056, p < 0.05). In addition, short-term antipsychotic administration significantly influenced the levels of total GSK3β (F3, 20 = 25.330, p < 0.01), p-GSK3β (F3, 20 = 8.692, p < 0.01), and the ratio of p-GSK3β/GSK3β (F3, 20 = 11.154, p < 0.01). Post hoc analyses demonstrated that both aripiprazole and haloperidol significantly inhibited Akt expression (aripiprazole, − 55.1%, p < 0.01; haloperidol, − 56.9%, p < 0.01), respectively, and short-term administration with bifeprunox increased p-Akt protein levels by + 21.4% (p < 0.05); in addition, the ratio of p-Akt/Akt was increased by all three drugs (aripiprazole, p < 0.05; bifeprunox, p < 0.05; haloperidol, p < 0.05) (Fig. 2A, E). Furthermore, GSK3β activity was shown to be affected in a similar manner as Akt activity. Specifically, aripiprazole and bifeprunox significantly changed the levels of GSK3β (− 40.8%, p < 0.01) and p-GSK3β (+ 42.9%, p < 0.01), respectively; and the ratio of p-GSK3β/GSK3β was elevated by all three drugs (aripiprazole, p < 0.01; bifeprunox, p < 0.05; haloperidol, p < 0.05) (Fig. 3A, B, C, E).
The modulation by three antipsychotics of Akt activity. The effects of aripiprazole (ARI), bifeprunox (BIF), and haloperidol (HAL) on Akt activity were measured in the ventral tegmental area (VTA) and substantia nigra (SN): VTA 1 week (A), VTA 10 weeks (B), SN 1 week (C), and SN 10 weeks (D). The representative bands of Western Blot are shown in (E). The sample size is six per group. Akt was quantified at 60 kDa; p-Akt was quantified at 60 kDa. The data were normalised by taking the average value of the control group as 100% and expressed as mean ± S.E.M. (*p ≤ 0.05, **p < 0.01 vs control)
The modulation by three antipsychotics of GSK3β activity. The effects of aripiprazole (ARI), bifeprunox (BIF), and haloperidol (HAL) on GSK3β activity were measured in the ventral tegmental area (VTA) and substantia nigra (SN): VTA 1 week (A), VTA 10 weeks (B), SN 1 week (C), and SN 10 weeks (D). The representative bands of Western Blot are shown in (E). The sample size is six per group. GSK3β was quantified at 46 kDa; p-GSK3β was quantified at 46 kDa. The data were normalised by taking the average value of the control group as 100% and expressed as mean ± S.E.M. (*p ≤ 0.05, **p < 0.01 vs control)
After 10-week antipsychotic administration, the chronic antipsychotic administration had no significant effect on the levels of Akt, p-Akt, GSK3β, and p-GSK3β, nor on the ratio of p-Akt/Akt and p-GSK3β/GSK3β in the VTA, compared with the controls (all p > 0.05) (Figs. 2A, B, C, G; 3A, B, C, G).
In the SN, after 1-week antipsychotic administration, it was found that antipsychotic administration significantly affected the levels of Akt (F3, 20 = 19.949, p < 0.01), p-Akt (F3, 20 = 12.136, p < 0.01), p-GSK3β (F3, 20 = 27.905, p < 0.01), and the ratio of p-Akt/Akt (F3, 20 = 2.819, p < 0.05) and p-GSK3β/GSK3β (F3, 20 = 10.030, p < 0.01). Post hoc analyses of short-term administration revealed that aripiprazole reduced the expression of Akt (− 41.8%, p < 0.01), while bifeprunox enhanced the levels of p-Akt (+ 44.3%, p < 0.01); and, both drugs increased the ratio of p-Akt/Akt (aripiprazole, p < 0.05; bifeprunox, p < 0.05) (Fig. 2D, E, F, G). Furthermore, both aripiprazole and bifeprunox increased the levels of p-GSK3β (aripiprazole, + 62.1%, p < 0.01; bifeprunox, + 47.7%, p < 0.01) and the ratio of p-GSK3β/GSK3β (aripiprazole, p < 0.01; bifeprunox, p < 0.05) (Fig. 3D, E, F, G).
In the SN after 10-week antipsychotic administration, it was observed that p-Akt (F3, 20 = 10.074, p < 0.01) and the ratio of p-Akt/Akt (F3, 20 = 8.932, p < 0.01) in the SN were changed by drug administration; the levels of p-GSK3β (F3, 20 = 3.101, p < 0.05) and the ratio of p-GSK3β/GSK3β (F3, 20 = 3.133, p < 0.05) were also significantly altered by 10-week antipsychotic administration in the SN. Post hoc tests showed that only bifeprunox increased the levels of p-Akt (+ 52.6%, p < 0.01) and the ratio of p-Akt/Akt (p < 0.01) (Fig. 2E, F); hence, aripiprazole and bifeprunox increased the levels of p-GSK3β (aripiprazole, + 74.6%, p < 0.05; bifeprunox, + 64.7%, p < 0.05); and also, the ratio of p-GSK3β/GSK3β was elevated by these two chemicals (aripiprazole, p < 0.05; bifeprunox, p < 0.05) (Fig. 3E, F).
Antipsychotic modulation of Dvl-3 and β-catenin expression
Short-term antipsychotic administration had no observable effects on the expression of Dvl-3 (F3, 20 = 1.858, p > 0.05) and β-catenin (F3, 20 = 2.313, p > 0.05) in the VTA; however, the expression of Dvl-3 (F3, 20 = 5.657, p < 0.01) and β-catenin (F3, 20 = 6.202, p < 0.01) in the SN was significantly changed after 1-week antipsychotic administration. Similarly, after chronic administration, both Dvl-3 (F3, 20 = 3.878, p < 0.05) and β-catenin (F3, 20 = 6.151, p < 0.01) expressions were significantly altered in the SN, but not in the VTA (both p > 0.05). Post hoc tests indicated that 1-week administration with aripiprazole (but not bifeprunox and haloperidol) significantly increased the protein levels of Dvl-3 (+ 31.8%, p < 0.05) and β-catenin (+ 49.3%, p < 0.01) in the SN, respectively; in addition, 10-week aripiprazole administration also significantly elevated the expression of Dvl-3 (+ 42.2%, p < 0.05) and β-catenin (+ 24.4%, p < 0.05) in the SN (Fig. 4C, D, E). No drug significantly affected the expression of Dvl-3 and β-catenin in the VTA (Fig. 4A, B, E).
The modulation by three antipsychotics of Dvl-3 and β-catenin expression. The effects of aripiprazole (ARI), bifeprunox (BIF), and haloperidol (HAL) on Dvl-3 and β-catenin expression were measured in the ventral tegmental area (VTA) and substantia nigra (SN): VTA 1 week (A), VTA 10 weeks (B), SN 1 week (C), and SN 10 weeks (D). The representative bands of Western Blot are shown in (E). The sample size is six per group. Dvl-3 was quantified at 85 kDa; β-catenin was quantified at 92 kDa. The data were normalised by taking the average value of the control group as 100% and expressed as mean ± S.E.M. (*p ≤ 0.05, **p < 0.01 vs control)
Antipsychotic modulation of the expression of NMDA receptor subunits
The present study revealed that the protein expression of NMDA receptor subunits NR1 and NR2A in both the VTA and SN was significantly affected by 10-week antipsychotic administration (NR1 in VTA, F3, 20 = 10.301, p < 0.01; NR2A in VTA, F3, 20 = 5.226, p < 0.01; NR1 in SN, F3, 20 = 33.785, p < 0.01; NR2A in SN, F3, 20 = 15.356, p < 0.01), whereas short-term administration exerted no influence on NMDA receptor expression in the two brain regions (all p > 0.05). In comparison with the controls, 10-week administration with aripiprazole and haloperidol reduced the expression of NMDA NR1 subunit in the VTA (aripiprazole, − 59.9%, p < 0.01; haloperidol, − 30.5%, p < 0.05); additionally, chronic aripiprazole administration also decreased NR2A expression in the VTA (− 31.9%, p < 0.01) (Fig. 5A, B, E). In the SN, the protein levels of both NMDA NR1 and NR2A were inhibited by aripiprazole (NR1, − 45.2%, p < 0.01; NR2A, − 56.9%, p < 0.01) and haloperidol (NR1, − 47.5%, p < 0.01; NR2A, − 38.3%, p < 0.01) (Fig. 5C, D, E).
The modulation by three antipsychotics of expression of NMRA receptor subunits. The effects of aripiprazole (ARI), bifeprunox (BIF), and haloperidol (HAL) on the expression of NMRA receptor subunits were measured in the ventral tegmental area (VTA) and substantia nigra (SN): VTA 1 week (A), VTA 10 weeks (B), SN 1 week (C), and SN 10 weeks (D). The representative bands of Western Blot are shown in (E). The sample size is six per group. NR1 was quantified at 105 kDa; NR2A was quantified at 165 kDa. The data were normalised by taking the average value of the control group as 100% and expressed as mean ± S.E.M. (*p ≤ 0.05, **p < 0.01 vs control)
Discussion
The present study investigated the effects of 1-week and 10-week treatment with three antipsychotics on PKA, Akt–GSK3β, Dvl-3–β-catenin signalling, as well as the expression of the NMDA receptor in the ventral midbrain (e.g., the VTA and SN). To the best of our knowledge, this is the first study to examine the in vivo effects of these antipsychotic drugs on cellular signalling and receptor expression in the ventral midbrain. The results have shown that antipsychotics could alter the signalling activity of PKA, Akt–GSK3β, Dvl-3–β-catenin, and the expression of the NMDA receptor in a time-dependent manner (Table 1), revealing possible patterns of how antipsychotics regulate dopamine neurons in the ventral midbrain.
The selective effects of aripiprazole on PKA activity in the VTA
The PKA signalling pathway is a canonical D2R-downstream signalling pathway which mediates diverse cellular responses via activating the cAMP-associated PKA kinase (Beaulieu and Gainetdinov 2011). Previous studies indicated that enhancement of PKA activity via antagonising D2Rs is associated with the effects of antipsychotics in various brain regions, regardless of the type of antipsychotic drug (Dwivedi et al. 2002; Pan et al. 2015; Turalba et al. 2004). In the present study, we found that 1-week administration with haloperidol increased PKA activity in the VTA, whereas 10-week administration with aripiprazole reduced it.
Short-form dopamine D2 autoreceptors are largely expressed at the pre-synapses of the ventral midbrain. These autoreceptors are located on the soma and dendrites of midbrain dopamine neurons (Ford 2014), and negatively regulate the phosphorylation/activation (Ser40) of tyrosine hydroxylase (TH), a rate-limiting enzyme in dopamine synthesis in the pre-synaptic nerve terminals, through acting on the PKA pathway (Harada et al. 1996; Lindgren et al. 2003; Roskoski Jr and Roskoski 1987) and release (el Mestikawy and Hamon 1986; Strait and Kuczenski 1986). Han et al. (2009) reported that 12-week administration with aripiprazole reduced TH mRNA expression in the VTA, but not in the SN, and haloperidol had no effects on TH mRNA expression. Taken together, our findings suggest that dopamine synthesis capacity in the VTA can be suppressed by chronic aripiprazole administration via inhibiting the PKA pathway and these results further confirm that chronic aripiprazole administration is very likely to have selective effects on dopaminergic activity in the VTA.
As a partial agonist for D2Rs, bifeprunox did not show the selective effects on PKA activity that aripiprazole showed. Thus, D2R partial agonism cannot fully explain the mechanism of aripiprazole. Also, in comparison with haloperidol, a potent D2R antagonist, it seems that potently antagonising D2Rs does not contribute to modulation of PKA activity in this study, either. Therefore, this unique activity of aripiprazole requires a novel explanation. It has been proposed that aripiprazole possesses functional selectivity at D2Rs (Mailman and Murthy 2010); however, this notion has not been completely validated. Our findings may possibly add new evidence of the functionally selective effects of aripiprazole.
Antipsychotics modulated the GSK3β-mediated signalling pathways in the ventral midbrain
GSK3β-mediated signalling pathways (including Akt–GSK3β and Dvl-3–GSK3β–β-catenin signalling pathways) have been implicated in schizophrenia (Emamian 2012; Singh 2013). Previous studies including our own studies indicated that GSK3β-mediated signalling pathways can be modulated by various antipsychotics (including aripiprazole and haloperidol) in a wide range of brain regions (Alimohamad et al. 2005a; Alimohamad et al. 2005b; Beaulieu et al. 2009; Emamian 2012; Li et al. 2007; Pan et al. 2016a, b; Park et al. 2011; Seo et al. 2015; Sutton and Rushlow 2011). However, the effects of antipsychotics on GSK3β-mediated signalling pathways in the ventral midbrain have not been examined before the present study.
In this study, we found that short-term administration with all three drugs increased the phosphorylation levels of Akt in parallel with the elevation in GSK3β phosphorylation in the VTA; in addition, 1-week administration with both aripiprazole and bifeprunox, but not haloperidol, significantly increased the phosphorylation of Akt and GSK3β in the SN; furthermore, after 10-week administration, the influences of all three drugs on Akt and GSK3β phosphorylation in the VTA disappeared; in contrast, the effects of aripiprazole and bifeprunox on GSK3β phosphorylation in the SN persisted, although their effect on Akt in the SN cannot be observed after 10-week administration; moreover, both 1-week and 10-week administration with aripiprazole increased Dvl-3 and β-catenin expression in the SN only. These findings together suggest that GSK3β-mediated signalling pathways in the ventral midbrain can be affected by antipsychotic administration; these data are generally consistent with the results of most previous studies that activation of these GSK3β-mediated signalling pathways contributes to the effects of various types of antipsychotics. It is interesting that aripiprazole also displayed selective effects on the Dvl-3–GSK3β–β-catenin signalling pathway in the SN. Whether this selective modulation of the Dvl-3–GSK3β–β-catenin signalling pathway is related to the functionally selective profile of aripiprazole still needs to be verified.
It is worth noting that although GSK3β-mediated signalling pathways can be regulated by D2Rs, these D2Rs in previous reports were primarily long-form D2 receptors and there is no evidence that D2 autoreceptors also function via these GSK3β-mediated pathways. Therefore, whether these GSK3β-mediated signalling pathways are regulated by short-form dopamine D2 receptors, and the exact role of GSK3β-mediated signalling pathways in the actions of antipsychotics in the ventral midbrain, require further exploration.
Antipsychotics suppressed the expression of NMDA receptors in the ventral midbrain
The cell body of dopaminergic neurons in the ventral midbrain expresses NMDA receptors, receiving glutamatergic afferents from various brain areas (Beier et al. 2015; Lerner et al. 2015). Glutamate is an excitatory neurotransmitter that stimulates neuron activity. In the present study, decreased NMDA receptor expression in the ventral midbrain might indicate inhibited activity of dopaminergic neurons, suggesting that in addition to blocking D2Rs, inhibiting dopaminergic neuron activity in the ventral midbrain might also be a route through which antipsychotics exert their therapeutic effects. However, whether this inhibition could affect dopamine synthesis and release requires further investigation.
The present study demonstrated that aripiprazole and haloperidol, but not bifeprunox, decreased the expression of NMDA NR1 and/or NR2A subunits in the ventral midbrain after 10-week administration only, indicating a time-dependent manner in which antipsychotics modulate NMDA receptors. It is worth noting that antipsychotics have very low affinity with NMDA receptors (Roth and Driscol 2018). Thus, these modulations of NMDA receptors are primarily indirect, which probably require long-term treatment to achieve.
In comparison with aripiprazole and haloperidol, bifeprunox did not modulate NMDA receptor expression in the ventral midbrain in the current study. The cause of this discrepancy is unclear. Due to the fact that the modulation by these antipsychotics of NMDA receptors is indirect and that the three chemicals used in the present study share a common mechanism—interacting with D2Rs, the alteration of NMDA receptor expression is very likely to be associated with their actions on D2Rs. Haloperidol is a potent D2R antagonist, whereas aripiprazole and bifeprunox are D2R partial agonists. Previous studies revealed that the intrinsic activity of aripiprazole at D2Rs is weaker than that of bifeprunox (intrinsic activity at D2Rs: aripiprazole vs. bifeprunox vs. dopamine = 86.0% vs. 95.1% vs. 100%) (Tadori et al. 2007; Tadori et al. 2005). It is possible that by competing with endogenous dopamine in the normal brain, aripiprazole would exert an overall antagonistic effect like haloperidol due to its relatively low intrinsic activity at D2Rs. Therefore, a low intrinsic activity at D2Rs might be associated with antipsychotic modulation of NMDA receptors. However, this hypothesis needs further validation.
It should be noted that antipsychotics exerted time-dependent effects on these signalling pathways and NMDA receptor expression in the VTA. For example, both aripiprazole and haloperidol elevated the activity of Akt–GSK3β signalling in the VTA after 1-week but not 10-week administration, while these two drugs downregulated the NMDA receptor expression after 10-week administration only (Table 1). The possible reason could be that the regulation of aripiprazole and haloperidol on the Akt–GSK3β signalling pathway through D2Rs was compromised due to the adaptive changes on D2Rs followed chronic antipsychotic treatment which has been well reported in both clinical and preclinical studies (El Hage et al. 2015; Li 2016; Moran-Gates et al. 2006). On the other hand, since these antipsychotics do not bind directly with NMDA receptors (Correll 2010), it might require a longer time for antipsychotics to modulate the expression of NMDA receptors via indirect signalling pathways (Beaulieu and Gainetdinov 2011; Pan et al. 2016b). It is also worthy to note that several other cellular pathways might become targets of current and/or potential antipsychotic drugs. For example, Long et al. (2017) reported that overexpression of Mash1 to activate the Mash1-dependent Notch signalling pathway in stem cells through genetic engineering could generate GABAergic neuron-like cells to treat neurological disorders including schizophrenia. Furthermore, the Sonic hedgehog (Shh) signalling pathway is associated with the pathophysiology of schizophrenia (Boyd et al. 2015), and abnormal tectonic 3 disrupts the Shh signalling (Wang et al. 2018), which enables the Shh pathways to be a potential target of future antipsychotic treatment.
In conclusion, the present study examined the short-term and long-term effects of antipsychotics on the activity of PKA- and GSK3β-mediated signalling pathways, as well as NMDA receptor expression in the ventral midbrain of rats. The findings suggest that aripiprazole might have selective effects on the PKA activity and Dvl-3–GSK3β–β-catenin signalling pathway in the ventral brain and that upregulation of the Akt–GSK3β signalling pathway and suppression of the NMDA receptor in the ventral midbrain might be the major routes through which antipsychotics exert their clinical effects. It is worth noting that the current study was conducted in healthy rats without any affection of the disease, showing the in vivo effects of aripiprazole and haloperidol on these pathways in the ventral midbrain; therefore, future studies are important to further validate these findings using animal models (such as Poly I:C models) for schizophrenia.
References
(Administration) FUSFaD (2005) Guidance for industry on estimating the maximum safe starting dose in initial clinical trials for therapeutics in adult healthy volunteers. In: Services USDoHaH, Administration FaD, (CDER) CfDEaR (eds) Estimating the Maximum Safe Starting Dose in Initial Clinical Trials for Therapeutics in Adult Healthy Volunteers, Rockville, Maryland, USA
Alimohamad H, Rajakumar N, Seah YH, Rushlow W (2005a) Antipsychotics alter the protein expression levels of beta-catenin and GSK-3 in the rat medial prefrontal cortex and striatum. Biol Psychiatry 57:533–542
Alimohamad H, Sutton L, Mouyal J, Rajakumar N, Rushlow WJ (2005b) The effects of antipsychotics on beta-catenin, glycogen synthase kinase-3 and dishevelled in the ventral midbrain of rats. J Neurochem 95:513–525
Allen JA, Yost JM, Setola V, Chen X, Sassano MF, Chen M, Peterson S, Yadav PN, Huang XP, Feng B, Jensen NH, Che X, Bai X, Frye SV, Wetsel WC, Caron MG, Javitch JA, Roth BL, Jin J (2011) Discovery of beta-arrestin-biased dopamine D2 ligands for probing signal transduction pathways essential for antipsychotic efficacy. Proc Natl Acad Sci U S A 108:18488–18493
Assie MB, Dominguez H, Consul-Denjean N, Newman-Tancredi A (2006) In vivo occupancy of dopamine D2 receptors by antipsychotic drugs and novel compounds in the mouse striatum and olfactory tubercles. Naunyn Schmiedeberg’s Arch Pharmacol 373:441–450
Beaulieu JM, Gainetdinov RR (2011) The physiology, signaling, and pharmacology of dopamine receptors. Pharmacol Rev 63:182–217
Beaulieu JM, Gainetdinov RR, Caron MG (2009) Akt/GSK3 signaling in the action of psychotropic drugs. Annu Rev Pharmacol Toxicol 49:327–347
Beier KT, Steinberg EE, DeLoach KE, Xie S, Miyamichi K, Schwarz L, Gao XJ, Kremer EJ, Malenka RC, Luo L (2015) Circuit architecture of VTA dopamine neurons revealed by systematic input-output mapping. Cell 162:622–634
Boyd PJ, Cunliffe VT, Roy S, Wood JD (2015) Sonic hedgehog functions upstream of disrupted-in-schizophrenia 1 (disc1): implications for mental illness. Biol Open 4:1336–1343
Carlsson A, Lindqvist M (1963) Effect of chlorpromazine or haloperidol on formation of 3-methoxytyramine and normetanephrine in mouse brain. Acta Pharmacol Toxicol (Copenh) 20:140–144
Casey DE, Sands EE, Heisterberg J, Yang HM (2008) Efficacy and safety of bifeprunox in patients with an acute exacerbation of schizophrenia: results from a randomized, double-blind, placebo-controlled, multicenter, dose-finding study. Psychopharmacology 200:317–331
Correll CU (2010) From receptor pharmacology to improved outcomes: individualising the selection, dosing, and switching of antipsychotics. Eur Psychiatry 25(Supplement 2):S12–S21
Dal Toso R, Sommer B, Ewert M, Herb A, Pritchett DB, Bach A, Shivers BD, Seeburg PH (1989) The dopamine D2 receptor: two molecular forms generated by alternative splicing. EMBO J 8:4025–4034
Dwivedi Y, Rizavi HS, Pandey GN (2002) Differential effects of haloperidol and clozapine on [(3)H]cAMP binding, protein kinase A (PKA) activity, and mRNA and protein expression of selective regulatory and catalytic subunit isoforms of PKA in rat brain. J Pharmacol Exp Ther 301:197–209
El Hage C, Bédard A-M, Samaha A-N (2015) Antipsychotic treatment leading to dopamine supersensitivity persistently alters nucleus accumbens function. Neuropharmacology 99:715–725
el Mestikawy S, Hamon M (1986) Is dopamine-induced inhibition of adenylate cyclase involved in the autoreceptor-mediated negative control of tyrosine hydroxylase in striatal dopaminergic terminals? J Neurochem 47:1425–1433
Emamian ES (2012) AKT/GSK3 signaling pathway and schizophrenia. Front Mol Neurosci 5:33
Ford CP (2014) The role of D2-autoreceptors in regulating dopamine neuron activity and transmission. Neuroscience 282C:13–22
Gardner DM, Murphy AL, O'Donnell H, Centorrino F, Baldessarini RJ (2010) International consensus study of antipsychotic dosing. Am J Psychiatry 167:686–693
Ginovart N, Kapur S (2012) Role of dopamine D(2) receptors for antipsychotic activity. Handb Exp Pharmacol:27–52
Han M, Huang XF, Deng C (2009) Aripiprazole differentially affects mesolimbic and nigrostriatal dopaminergic transmission: implications for long-term drug efficacy and low extrapyramidal side-effects. Int J Neuropsychopharmacol 12:941–952
Harada WJ, Haycock JW, Goldstein M (1996) Regulation of L-DOPA biosynthesis by site-specific phosphorylation of tyrosine hydroxylase in AtT-20 cells expressing wild-type and serine 40-substituted enzyme. J Neurochem 67:629–635
Lerner TN, Shilyansky C, Davidson TJ, Evans KE, Beier KT, Zalocusky KA, Crow AK, Malenka RC, Luo L, Tomer R, Deisseroth K (2015) Intact-brain analyses reveal distinct information carried by SNc dopamine subcircuits. Cell 162:635–647
Li M (2016) Antipsychotic-induced sensitization and tolerance: behavioral characteristics, developmental impacts, and neurobiological mechanisms. J Psychopharmacol 30:749–770
Li X, Rosborough KM, Friedman AB, Zhu W, Roth KA (2007) Regulation of mouse brain glycogen synthase kinase-3 by atypical antipsychotics. Int J Neuropsychopharmacol 10:7–19
Lindgren N, Usiello A, Goiny M, Haycock J, Erbs E, Greengard P, Hokfelt T, Borrelli E, Fisone G (2003) Distinct roles of dopamine D2L and D2S receptor isoforms in the regulation of protein phosphorylation at presynaptic and postsynaptic sites. Proc Natl Acad Sci U S A 100:4305–4309
Long Q, Luo Q, Wang K, Bates A, Shetty AK (2017) Mash1-dependent notch signaling pathway regulates GABAergic neuron-like differentiation from bone marrow-derived mesenchymal stem cells. Aging Dis 8:301–313
Mace S, Taylor D (2009) Aripiprazole: dose-response relationship in schizophrenia and schizoaffective disorder. CNS Drugs 23:773–780
Mailman RB, Murthy V (2010) Third generation antipsychotic drugs: partial agonism or receptor functional selectivity? Curr Pharm Des 16:488–501
Moran-Gates T, Gan L, Park YS, Zhang K, Baldessarini RJ, Tarazi FI (2006) Repeated antipsychotic drug exposure in developing rats: dopamine receptor effects. Synapse 59:92–100
Morikawa H, Paladini CA (2011) Dynamic regulation of midbrain dopamine neuron activity: intrinsic, synaptic, and plasticity mechanisms. Neuroscience 198:95–111
Natesan S, Reckless GE, Nobrega JN, Fletcher PJ, Kapur S (2006) Dissociation between in vivo occupancy and functional antagonism of dopamine D2 receptors: comparing aripiprazole to other antipsychotics in animal models. Neuropsychopharmacology 31:1854–1863
Pan B, Chen J, Lian J, Huang XF, Deng C (2015) Unique effects of acute aripiprazole treatment on the dopamine D2 receptor downstream cAMP-PKA and Akt-GSK3beta signalling pathways in rats. PLoS One 10:e0132722
Pan B, Huang XF, Deng C (2016a) Aripiprazole and haloperidol activate GSK3beta-dependent signalling pathway differentially in various brain regions of rats. Int J Mol Sci 17:459
Pan B, Huang XF, Deng C (2016b) Chronic administration of aripiprazole activates GSK3beta-dependent signalling pathways, and up-regulates GABAA receptor expression and CREB1 activity in rats. Sci Rep 6:30040
Pan B, Lian J, Huang XF, Deng C (2016c) Aripiprazole increases the PKA signalling and expression of the GABAA receptor and CREB1 in the nucleus accumbens of rats. J Mol Neurosci 59:36–47
Park SW, Seo MK, Cho HY, Lee JG, Lee BJ, Seol W, Kim YH (2011) Differential effects of amisulpride and haloperidol on dopamine D2 receptor-mediated signaling in SH-SY5Y cells. Neuropharmacology 61:761–769
Paxinos G, Watson C (2005) The rat brain in stereotaxic coordinates. Elsevier Academic Press, San Diego
Reagan-Shaw S, Nihal M, Ahmad N (2008) Dose translation from animal to human studies revisited. FASEB J 22:659–661
Roskoski R Jr, Roskoski LM (1987) Activation of tyrosine hydroxylase in PC12 cells by the cyclic GMP and cyclic AMP second messenger systems. J Neurochem 48:236–242
Roth BL, Driscol J (2018) PDSP Ki database Psychoactive Drug Screening Program (PDSP). University of North Carolina at Chapel Hill and the United States National Institute of Mental Health
Seo MK, Lee CH, Cho HY, You YS, Lee BJ, Lee JG, Park SW, Kim YH (2015) Effects of antipsychotic drugs on the expression of synapse-associated proteins in the frontal cortex of rats subjected to immobilization stress. Psychiatry Res 229:968–974
Sibley DR (1999) New insights into dopaminergic receptor function using antisense and genetically altered animals. Annu Rev Pharmacol Toxicol 39:313–341
Singh KK (2013) An emerging role for Wnt and GSK3 signaling pathways in schizophrenia. Clin Genet 83:511–517
Strait KA, Kuczenski R (1986) Dopamine autoreceptor regulation of the kinetic state of striatal tyrosine hydroxylase. Mol Pharmacol 29:561–569
Sutton LP, Rushlow WJ (2011) The effects of neuropsychiatric drugs on glycogen synthase kinase-3 signaling. Neuroscience 199:116–124
Tadori Y, Miwa T, Tottori K, Burris KD, Stark A, Mori T, Kikuchi T (2005) Aripiprazole's low intrinsic activities at human dopamine D2L and D2S receptors render it a unique antipsychotic. Eur J Pharmacol 515:10–19
Tadori Y, Kitagawa H, Forbes RA, McQuade RD, Stark A, Kikuchi T (2007) Differences in agonist/antagonist properties at human dopamine D(2) receptors between aripiprazole, bifeprunox and SDZ 208-912. Eur J Pharmacol 574:103–111
Turalba AV, Leite-Morris KA, Kaplan GB (2004) Antipsychotics regulate cyclic AMP-dependent protein kinase and phosphorylated cyclic AMP response element-binding protein in striatal and cortical brain regions in mice. Neurosci Lett 357:53–57
Wadenberg M-LG (2007) Bifeprunox: a novel antipsychotic agent with partial agonist properties at dopamine D2 and serotonin 5-HT1A receptors. Future Neurol 2:153–165
Wang B, Zhang Y, Dong H, Gong S, Wei B, Luo M, Wang H, Wu X, Liu W, Xu X, Zheng Y, Sun M (2018) Loss of Tctn3 causes neuronal apoptosis and neural tube defects in mice. Cell Death Dis 9:520
Wolf ME, Roth RH (1990) Autoreceptor regulation of dopamine synthesis. Ann N Y Acad Sci 604:323–343
Acknowledgments
We would like to thank Dr. Jiamei Lian and Dr. Michael De-Santis for their technical assistance.
Funding
This study was supported by the Australian National Health and Medical Research Council project grant (APP1008473) to Chao Deng. Bo Pan was supported by the Natural Science Foundation of the Higher Education Institutions of Jiangsu Province, China (17KJB310018), the China Postdoctoral Science Foundation (2018 M632401), and the Natural Science Foundation of Jiangsu Province of China (BK20171290).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All experimental procedures were approved by the Animal Ethics Committee (AE11/02) of the University of Wollongong and complied with the Australian Code of Practice for the Care and Use of Animals for Scientific Purposes (2004).
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pan, B., Deng, C. Modulation by chronic antipsychotic administration of PKA- and GSK3β-mediated pathways and the NMDA receptor in rat ventral midbrain. Psychopharmacology 236, 2687–2697 (2019). https://doi.org/10.1007/s00213-019-05243-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-019-05243-x