Abstract
Rationale
Dysregulation of noradrenergic and dopaminergic systems is involved in the pathology of attention deficit hyperactivity disorder (ADHD). Carbonic anhydrase (CA) has been reported to affect monoamine transmission in the central nervous system.
Objectives
The aim of this study is to investigate the effect of CA inhibitors on the hyperactivity and impulsivity of the spontaneously hypertensive rat (SHR), which is currently the best-validated animal model of ADHD.
Methods
SHRs and Wistar Kyoto rats at 6 to 8 weeks of age were pretreated with intraperitoneal injections of acetazolamide and methazolamide, both carbonic anhydrase inhibitors, before the behavior tests. The open-field locomotion test and the electro-foot shock aversive water drinking test were then applied to quantify their hyperactivity and impulsivity, respectively. The Morris water maze test, on the other hand, monitored their spatial learning.
Results
Acetazolamide and methazolamide significantly inhibited the hyperactivity of SHRs but had no effects in Wistar Kyoto rats. Acetazolamide also inhibited the impulsivity of SHRs. Low doses of acetazolamide had the greater inhibitory effects on the hyperactivity and impulsivity, but did not impair the spatial learning of SHRs.
Conclusions
This is the first study to show that carbonic anhydrase inhibitors can strain-specifically antagonize the hyperactivity and impulsivity of SHRs. Under a low dose of acetazolamide, there was no cognition impairment in SHRs. Carbonic anhydrase inhibitors may be the novel drugs for treatment for patients with ADHD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Attention deficit hyperactivity disorder (ADHD) is the most common childhood psychiatric disorder, with a reported overall prevalence in children and adolescents of 5.9–7.1 % (Willcutt 2012). ADHD is a persistent pattern of inattention and/or hyperactivity-impulsivity that interferes with functioning or development (Jones and Dafny 2013). A meta-analysis and comparison of the biomarkers between ADHD and control children has shown that monoaminergic systems as well as the hypothalamic-pituitary-adrenal axis are dysregulated in children with ADHD (Del Campo et al. 2011; Scassellati et al. 2012). ADHD treatment is beneficial to the long-term life functioning of patients with ADHD (Shaw et al. 2012).
ADHD medications are available. However, their limited efficacy and possible adverse effects warrant the development of new drugs. Central nervous system stimulants such as methylphenidate (MPH) have response rates around 70 % (Spencer et al. 1996). The adverse effects of current ADHD medications include loss of appetite, growth delay, higher risk of cardiovascular events, sleep disturbance, tics, seizures, suicidal thoughts/behaviors, and psychotic symptoms (Cortese et al. 2013; Westover and Halm 2012).
The spontaneously hypertensive rat (SHR) model is currently the best-validated animal model of ADHD, and Wistar Kyoto (WKY) rats, the strain from which SHRs are derived, have been shown to be the most appropriate control of SHR (Meneses et al. 2011; Sagvolden and Johansen 2012). SHRs have been reported to display the major symptoms of ADHD (inattention, hyperactivity, and impulsivity) (Sagvolden and Johansen 2012). Hyperactivity and impulsivity in SHRs may be associated with a reduction in dopamine function, while poorer sustained attention may be associated with a reduction in norepinephrine activity (Sagvolden and Xu 2008). Nevertheless, the relationship between dopamine transmission and impulsivity is complex, and contradictory results have been reported (Dalley and Roiser 2012; Del Campo et al. 2011). Attenuation of the locomotion and impulsivity of SHRs has been used to investigate the efficacy of ADHD medication against hyperactivity and impulsivity (Kim et al. 2012; Umehara et al. 2013b).
Carbonic anhydrase (CA), a ubiquitous metalloenzyme in prokaryotes and eukaryotes, plays a role in the central nervous system. Acetazolamide (AZ), an inhibitor of CA, has been used as an anticonvulsant since 1952 (Bergstom et al. 1952), and the anticonvulsant activity of CA inhibitors, including AZ and methazolamide (MZ), has been reported to involve noradrenergic mechanisms (Gray and Rauh 1974; Torchiana et al. 1973). Zonisamide, another CA inhibitor and anticonvulsant, stimulates Ca2+-evoked monoamine release (Kawata et al. 1999; Tominaga et al. 2001) and has been shown to be beneficial for patients with Parkinson’s disease (Bermejo et al. 2010; Murata 2010). In addition, CA has been shown to affect the switching of gamma-aminobutyric acid (GABA)A receptors between excitation and inhibition (Ting et al. 2013). In short, the actions of CA in the central nervous system appear to involve the noradrenergic system, dopaminergic system, and GABAA receptors.
Based on the rationale that dysregulation of noradrenergic and dopaminergic systems is involved in the pathogenesis of ADHD and that CA can affect these systems, we were led to investigate the effects of CA inhibitors on the hyperactivity and impulsivity of SHR, an animal model of ADHD.
Methods
Animals
Six-to-eight-week-old male SHRs (inbred SHRs from the National Institutes of Health, USA) and WKY rats (inbred WKY rats from the National Institutes of Health, USA) were used in this study. The animals were supplied from BioLASCO (Taiwan Co., Ltd.), and housed and maintained on a 12-h-on/12-h-off light/dark cycle at the Animal Center of Medical College, National Taiwan University. All of the animals were allowed free access to food and water, except during the electro-foot shock aversive water drinking test (EFSDT). All efforts were made to minimize animal suffering and to reduce the number of animals used. All housing and procedures conformed to the Guide for the Care and Use of Laboratory Animals (National Research Council 2011) as well as the current version of the Animal Protection Act of the Republic of China, and were approved by the Institutional Animal Care and Use Committee of National Taiwan University College of Medicine.
Drugs
Acetazolamide (AZ) was from Sigma-Aldrich (St. Louis, MO, USA). Methazolamide (MZ) was from Santa Cruz Biotechnology (Dallas, TX, USA). Methylphenidate (MPH) was from Novartis Pharmaceuticals Co. (East Hanover, NJ, USA), and atomoxetine (ATX) was from Lilly S.A. (Madrid, Spain).
Open-field locomotor test
Hyperactivity revealed by open-field locomotor test in SHRs has been shown to be similar to hyperactivity of children with ADHD (Sagvolden 2000). The rats received intraperitoneal injection of AZ, MPH, ATX, or MZ before the open-field locomotor test. The doses were 0.1 to 10 mg/kg of AZ, 0.1 mg/kg of MPH, 5 mg/kg of ATX, and 10 mg/kg of MZ. The pretreatment durations before the locomotor test were 60 min for AZ as our previous study (Yang et al. 2013) and 30 min for MPH, ATX, and MZ. The doses and pretreatment durations of MPH and ATX were determined from prior studies (Carmack et al. 2014; Paterson et al. 2011). The control group received an equal volume of vehicle (double-distilled water). Locomotor activity was monitored using 16 × 16 photobeams (beam interval, 1 in.) with a sampling rate of once per second in the Plexiglas cage (16 × 16 × 15 in.; San Diego Instruments, San Diego, CA, USA). The patterns of beam breaks were computed (Photobeam Activity System—Open Field; San Diego Instruments, San Diego, CA, USA) to obtain the parameters of locomotor activity. The central zone was defined as an arena-center area, four beam-intervals away from the arena wall, and the peripheral zone was defined as the area within four beam-intervals of the arena wall. Rearing was defined as the number of times when an animal stood upon its hind legs with the forelegs in the air or against the wall. Each animal was tested for 30 min.
Electro-foot shock aversive water drinking test
The electro-foot shock aversive water drinking test (EFSDT) was used to measure impulsive behavior in SHRs as reported by Kim et al. (2012) with some modifications. The SHRs and WKY rats received 1 mg/kg (i.p.) of AZ 1 h before EFSDT, and the control group received an equal volume of vehicle (double-distilled water). The black EFSDT Plexiglas box, sized 60 × 60 × 30 cm, was divided into three compartments (start area, water area, and free area, as shown in the supplementary figure, Fig. S1). The floor of the water area was made of electrified grid wire. In the water area, a water bottle with a stainless steel nozzle, extending 4 cm into the box at a height of 12 cm above the floor, was fitted from outside of the box. The EFSDT consisted of two phases: a training phase which lasted for 2 days and a testing phase which lasted for 1 day. Rats were deprived of water for at least 18 h in their home cages before the training phase. During the training phase (day 1 and day 2), the rats were placed in the start area initially. Whenever the rats licked water from the bottle for at least 5 s, the experimenter would remove the rats and place them back to the start area. The training session lasted for 10 min per trial, two trials (separated by at least 60 min) a day for two consecutive days. The rats were kept deprived of water in their home cages after training each day. During the testing phase (day 3), the rats began at the start area, an electro-foot shock (2 mA, 0.5 s from the stimulator, Model 2100; A-M Systems, Carlsborg, WA, USA) was given whenever the rats licked water from the bottle for at least 5 s. The testing session lasted for 10 min. Impulsive drinking was quantified by the number of drinking resulting in electroshocks, and the impulsive drinking attempt was quantified by the frequency of the rats in the water (shock) area analyzed by the EthoVision 3 (Noldus Information Technology Inc., Wageningen, The Netherlands).
Morris water maze test
The SHRs received 3 mg/kg (i.p.) of AZ 1 h before the Morris water maze test each day. The control group received an equal volume of vehicle (double-distilled water). The Morris water maze test was performed in a circular pool (diameter of 180 cm and height of 70 cm) located in a room with distinctive visual cues. A transparent plastic platform (12 cm in diameter, 48 cm in height) was located at the center of a fixed quadrant and submerged about 1 cm below the water surface. Training started by acclimating the rat to the task environment with 1 day of free-swimming in the pool with no platform. Each session lasted for 2 min, after which the rat was removed from the pool by the experimenter. The rats then received training of four trials per day for four consecutive days. The intervals between trials were 60 s. In each trial, the rat was placed into the water randomly in one of the four quadrants. The rats then had to swim until it climbed onto the platform submerged underneath the water. The duration from the time when the rats entered the water to the time when they climbed onto the platform was recorded and defined as the escape latency. Swim distance and swim speed were also recorded. If the rat failed to find the platform by 120 s, it was placed on the platform by the experimenter. The rat stayed on the platform for 60 s. At the end of each day’s training, the rat was dried with a towel and an electric heater before being placed into its home cage. The navigation of the rats was tracked by EthoVision 3 (Noldus Information Technology Inc., Wageningen, The Netherlands).
Statistical analysis
All data were analyzed using SPSS® software version 19.0 (IBM Inc., Somers, NY, USA). All values were expressed as mean ± standard deviation (SD). All tests were two-tailed, and a p value less than 0.05 was considered to be statistically significant.
Two-way ANOVA model was conducted to compare the locomotor activities, impulsive drinking, and drinking attempts between different strains and treatments. In this model, total activity, rearing, impulsive drinking, and drinking attempt were assigned as the dependent variables, while treatment group (control, AZ) and strain (WKY, SHR) were entered as the independent variables. If significant interaction between independent variables existed, simple main effects analysis was used and followed by post hoc comparison with Bonferroni method.
To examine the locomotor activity by phase, a general linear model repeated measures with Greenhouse-Geisser correction was used with recording time (0–5, 5–10, 10–15, 15–20, 20–25, and 25–30 min) as the within-subject factor, the treatment group (control, AZ_0.1, AZ_1, AZ_3, AZ_10, MPH, ATX) as the between-subject factor, and the locomotor activity as the dependent variable. Overall differences between the different treatment groups and the control group were compared by post hoc Dunnett test. On the basis of the results of the general linear model repeated measures, group differences were further examined by one-way ANOVA and post hoc Dunnett test for pair comparisons on the same recording phase. Unpaired two-sample t test was used to compare the locomotor activity between the control and the MZ group in SHR.
The differences between the groups regarding the escape latency, traveled distance, and swimming speed during the Morris water maze test were also evaluated by a general linear model repeated measures with Greenhouse-Geisser correction, with the training day (day 1 to day 4) as the within-subject factor and the treatment group (control, AZ) as the between-subject factor.
Results
Strain-specific attenuation of locomotor activity by acetazolamide (AZ)
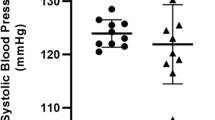
As reported in previous studies, SHRs were more active than WKY rats (Fig. 1). For total locomotor activity, there were significant main effects of strain (F(1,59) = 173.096, p < 0.001) and treatment group (F(1,59) = 8.167, p = 0.006). There was a statistically significant interaction between strain and treatment group for the total activity (F(1,59) = 5.722, p = 0.020). The total locomotor activity of SHRs was 2801.6 ± 491.3 (n = 31), and that of WKY rats was 865.9 ± 346.7 (n = 12) (Fig. 1a). AZ (10 mg/kg) significantly decreased the total activity in SHRs (2148.0 ± 315.6, n = 10, 76.7 % of the control SHRs, p < 0.001), but not in WKY rats (Fig. 1a). Therefore, AZ could strain-specifically attenuate the hyperactivity of SHRs.
Strain-specific attenuation of the locomotor activity by acetazolamide (AZ). Wistar Kyoto (WKY) rats (n = 10) and spontaneously hypertensive rats (SHRs) (n = 10) received intraperitoneal injections of AZ (10 mg/kg) 1 h before the open-field locomotor test. The control group of WKY rats (n = 12) and SHRs (n = 31) received equal volumes of vehicle. a Total activity of SHR, but not WKY rats, was significantly inhibited by AZ. b The number of rearings of SHR, but not WKY rats, was significantly inhibited by AZ. ***p < 0.001; *p < 0.05, compared with the control groups. Data are presented as mean ± SEM
For the rearing, there were significant main effects of strain (F(1,59) = 57.821, p < 0.001). The main effect of treatment group and the interaction between strain and treatment group on the rearing were marginal (Fig. 1b). The numbers of rearing were 148.0 ± 61.3 and 18.9 ± 11.0 for SHRs and WKY rats, respectively (Fig. 1b). AZ (10 mg/kg) significantly decreased the rearing in SHRs (96.6 ± 50.0, n = 10, 65.3 % of the control SHRs, p = 0.021, paired t test), but not in WKY rats.
Attenuation of the locomotor activity of SHR by methylphenidate (MPH), atomoxetine (ATX), and acetazolamide (AZ)
As mentioned previously, AZ at 10 mg/kg attenuated the hyperactivity of SHRs. We further investigated the effects of AZ at different doses and also compared with the well-known anti-ADHD drugs, MPH and ATX (Fig. 2). The locomotor activities of SHRs significantly differed among the recording phases (F(3.451,179.449) = 80.581; p < 0.001) and among the control and treatment groups (F(3,52) = 5.802; p = 0.002) (Fig. 2a). As the recording proceeded, the locomotor activities per recording phase gradually decreased. The locomotor activities of SHRs were inhibited by AZ (most significantly at 1 mg/kg) from 5 to 30 min of the testing. The locomotor activities of SHRs were inhibited significantly at 1 mg/kg AZ to 57, 35, 38, 27, and 32 % of control from 10 to 30 min of the testing. In addition, 10 mg/kg AZ significantly attenuated the locomotor activities of SHRs to 59 % of control in the interval of 10–15 min.
Attenuation of the locomotor activity of spontaneously hypertensive rat (SHR) by methylphenidate (MPH), atomoxetine (ATX), and acetazolamide (AZ). Six-to-eight-week-old SHR received intraperitoneal injections of vehicle (control, n = 31), MPH (0.1 mg/kg, n = 8), ATX (5 mg/kg, n = 8), and AZ (0.1–10 mg/kg), n = 29) before the open-field locomotor test. Each animal was tested for 30 min. a Phase analysis showed that the locomotor activity of the SHR was significantly inhibited by 1 mg/kg AZ from 5 to 30 min. b Total locomotor activity of the SHR was significantly inhibited by AZ (1, 3, and 10 mg/kg), MPH (0.1 mg/kg), and ATX (5 mg/kg). c The peripheral locomotor activity of SHR was significantly inhibited by AZ (1, 3, and 10 mg/kg), MPH, and ATX. The central locomotor activity of the SHR was also significantly inhibited by AZ and MPH. d The number of rearings of the SHR was inhibited by AZ, MPH, and ATX. ***p < 0.001; **p < 0.01; *p < 0.05, compared with the control group. Data are presented as mean ± SEM
The total activities of the SHRs were significantly inhibited by AZ (1–10 mg/kg), MPH (0.1 mg/kg), and ATX (5 mg/kg) (Fig. 2b). The total activities were 2801.6 ± 491.3 (n = 31) in the control group, 1707.6 ± 792.4 (n = 8) (61.0 % of control) in the 1 mg/kg AZ group, 2078.6 ± 421.3 (n = 7) (74.19 % of control) in the 3 mg/kg AZ group, 2148.0 ± 315.6 (n = 10) (76.7 % of control) in the 10 mg/kg AZ group, 2228.4 ± 655.6 (n = 8) (79.5 % of control) in the MPH group, and 2029.0 ± 540.7 (n = 8) (72.4 % of control) in the ATX group.
The peripheral activities of the SHRs were also significantly inhibited by AZ (1–10 mg/kg), MPH (0.1 mg/kg), and ATX (5 mg/kg) (Fig. 2c). The peripheral activities were 2209.8 ± 414.3 in the control group, 1279.8 ± 526.2 (57.9 % of control) in the 1 mg/kg AZ group, 1553.3 ± 220.3 (70.3 % of control) in the 3 mg/kg AZ group, 1742.7 ± 227.2 (78.9 % of control) in the 10 mg/kg AZ group, 1696.1 ± 391.2 (76.8 % of control) in the MPH group, and 1570.5 ± 412.4 (71.1 % of control) in the ATX group. The central activities of the SHRs were significantly inhibited by AZ (1–10 mg/kg) and MPH (Fig. 2c).
The numbers of rearing of the SHRs were also significantly inhibited by AZ, MPH, and ATX (Fig. 2d).
Attenuation of the locomotor activity of SHR by methazolamide (MZ)
To confirm the inhibition of the locomotor activity by carbonic anhydrase inhibition, we applied MZ, another carbonic anhydrase inhibitor, to the SHR (Fig. 3). The locomotor activity of the SHR significantly differed among the recording phases (F(5,175) = 11.802; p < 0.001) and between the control and treatment groups (F(2,35) = 9.023; p = 0.001) (Fig. 3a). As the recording proceeded, the locomotor activity per recording phase gradually decreased. The locomotor activity of the SHR was inhibited by 10 mg/kg MZ from 5 to 30 min and inhibited by MZ to 74, 55, 40, 57, 32, and 34 % of control from 0 to 30 min.
Attenuation of the locomotor activity of spontaneously hypertensive rat (SHR) by methazolamide (MZ). Six-to-eight-week-old SHRs received intraperitoneal injections of vehicle (control, n = 31) and MZ (10 mg/kg, n = 6) 30 min before the open-field locomotor test. Each animal was tested for 30 min. a Phase analysis showed that the locomotor activity of the SHR was significantly inhibited by 10 mg/kg MZ from 5 to 30 min. b Total locomotor activity of the SHR was significantly inhibited by MZ. c The peripheral and central locomotor activities of SHR were significantly inhibited by MZ. d The rearing activity of SHR was inhibited by MZ. ***p < 0.001; **p < 0.01; *p < 0.05, compared with the control group. Data are presented as mean ± SEM
The total activity, central activity, peripheral activity, and number of rearing of the SHR were significantly inhibited by MZ (Fig. 3b, c, d). The total activities were 2801.6 ± 491.3 (n = 31) in the control group and 1801.9 ± 292.1 (n = 6) (64.3 % of control) in the MZ group (p < 0.001). The central activities were 681.4 ± 189.1 in the control group and 327.9 ± 145.8 (48.1 % of control) in the MZ group (p < 0.001). The peripheral activities were 2209.8 ± 414.3 in the control group and 1463.9 ± 215.1 (66.3 % of control) in the MZ group (p < 0.001). The numbers of rearing were 148.0 ± 61.3 in the control group and 84.3 ± 41.9 (56.9 % of control) in the MZ group (p = 0.021).
Attenuation of the impulsivity of SHR by acetazolamide (AZ)
As mentioned previously, ADHD includes three core symptoms: inattention, hyperactivity, and impulsivity. We further investigated the effect of AZ on the impulsivity of SHRs (Fig. 4). For the impulsive drinking, significant main effects of strain (F(1,24) = 11.707, p = 0.002) and treatment (F(1,24) = 8.369, p = 0.008) were noted. The two-way interaction between strain and treatment was also significant (F(1,24) = 7.928, p = 0.001). SHRs showed more impulsive drinking than WKY rats (p = 0.006). The baseline impulsive drinking numbers were 18.4 ± 6.9 and 6.9 ± 3.2 for SHRs and WKY rats, respectively. Furthermore, the impulsive drinking numbers of SHRs were attenuated by AZ (1 mg/kg) significantly (p = 0.006). As to the drinking attempt, there were no significant differences between different strains and between different treatments. The baseline drinking attempts were 39.1 ± 17.5 and 35.4 ± 10.6 for SHRs and WKY rats, respectively. AZ did not affect the drinking attempts of neither SHRs nor WKY rats.
Attenuation of the impulsivity of spontaneously hypertensive rat (SHR) by acetazolamide (AZ). Six-to-eight-week-old Wistar Kyoto (WKY) rats (n = 7) and spontaneously hypertensive rats (SHRs) (n = 6) received intraperitoneal injections of AZ (1 mg/kg) 1 h before the electro-foot shock aversive water drinking test. The control group of WKY rats (n = 7) and SHRs (n = 8) received equal volumes of vehicle. a SHR had more impulsive drinking than WKY rats. The impulsive drinking of SHR was attenuated by AZ (1 mg/kg). b The drinking attempts were similar between SHRs and WKY rats. AZ did not affect the drinking attempt in both WKY rats and SHRs. **p < 0.01. Data are presented as mean ± SEM (n)
No impairment of spatial learning at a low dose of acetazolamide (AZ)
Our previous study has shown that a high dose (10 mg/kg, i.p.) of AZ impairs the fear memory in rodents (Yang et al. 2013), and Sun and Alkon (2001) reported that AZ inhibits spatial memory in rats. If AZ is to be used clinically in children with ADHD, it is important to prove that lower doses of AZ are effective for attenuating ADHD symptoms as well as are safe for their cognition. Since AZ inhibited the hyperactivity and impulsivity in SHR, we thus examined the effect of low dose of AZ (3 mg/kg) on the spatial learning using Morris water maze test. The escape latencies and the swim distances differed significantly among different training days [F(1.418,11.343) = 23.189, p < 0.001 for escape latency; F(1.197,9.576) = 24.051, p < 0.001 for swim distance] (Fig. 5). As shown in Fig. 5, the decreasing escape latencies (Fig. 5a) and swim distances (Fig. 5b) day by day in both groups reflected their intact spatial learning. The swim speeds showed no differences among different training days (Fig. 5c). There were no differences of the escape latencies, the swim distances, and the swim speeds between control and AZ groups. Therefore, a low dose of 3 mg/kg AZ had no adverse effects on the spatial learning of SHR.
No impairment of spatial learning and swim speed at a low dose of acetazolamide (AZ). Six-to-eight-week-old spontaneously hypertensive rats received intraperitoneal injections of 3 mg/kg/day of AZ (n = 5) 1 h before the Morris water maze test. The control group received an equal volume of vehicle (n = 5). Each point represents the average escape latency (a), swim distance (b), and swim speed (c) of each daily training session. Note that the escape latency, swim distance, and swim speed showed no difference between the two groups. Data are presented as mean ± SEM
Discussion
The results of this study are summarized in Table 1. This study showed that inhibition of locomotor activity and impulsive drinking by AZ was strain-specific in SHRs, but not in WKY rats. In addition, we have also previously shown that 10 mg/kg of AZ did not inhibit the locomotor activity in adult male Wistar rats (Yang et al. 2013). This strain-specific inhibition of hyperactivity by AZ in SHR is consistent with strain-specific inhibition of hyperactivity by methylphenidate and atomoxetine in SHR (Umehara et al. 2013a).
Figures 2 and 3 show that both AZ and MZ attenuated the locomotor activities of SHRs, which implied that this inhibitory effect is universal within CA inhibitors, rather than specific to AZ. Besides the attenuation of locomotor activity, this study showed that AZ inhibited the impulsivity of SHRs (Fig. 4). To summarize briefly, AZ and other CA inhibitors may be the promising drugs for the treatment of ADHD, at least in the hyperactivity-impulsivity domain.
Figures 2 and 3 show that AZ influences only the hyperactivity of SHRs after habituation to the novel environment but not the initial hyperactivity. The novelty of environment can induce active exploration both in normal children and in animals. Children with ADHD and SHRs compared with their controls have similar activity levels at the initiation of testing (Russell 2011). After habituation, however, only the children with ADHD and SHRs showed hyperactivity (Russell 2011). Just as in Fig. 1, AZ strain-specifically inhibited the hyperactivity of SHR, but not the locomotor activity of WKY rat, and AZ did not inhibit the normal exploration of novel environment but inhibited the abnormal hyperactivity after habituation.
EFSDT, the impulsivity test, uses electric shock as an aversive stimulus. The pain sensitivity to electric shock is thus a confounding factor for evaluating the impulsive drinking. Our previous study has reported that AZ has no effect on the sensitivity to electric shock (0.2 to 1.8 mA) under high dose in rats (10 mg/kg) and in mice (30 mg/kg) (Yang et al. 2013). Furthermore, we only used low dose of AZ at 1 mg/kg for the impulsivity test. Therefore, inhibition of the impulsivity of SHR by AZ is not related to the change of pain sensitivity.
EFSDT has been proposed to reflect the impulsivity in animals (Kim et al. 2012). Recently, both impulsivity and compulsivity, although conceptually different, have been proposed to invoke the same concept of top-down inhibitory control over behavior (Bari and Robbins 2013; Robbins et al. 2012). Impulsivity is defined as the tendency to act prematurely without foresight (Dalley et al. 2011). The major difference of compulsivity from impulsivity is that the repetitive or perseverative behaviors of compulsivity often occur without reference to the original goal, that is purposelessly, and are driven by an obsession or according to a rigid rule (American Psychiatric Association 2013; Dalley et al. 2011; Robbins et al. 2012). The EFSDT does reflect the impulsivity rather than the compulsivity, and this is grounded on the fact that the drinking in EFSDT is driven by physiological need (thirst) rather than some unrealistic rigid rules. In addition, compulsive behavior is not done for pleasure and aims to prevent a feared event although in an unrealistic way (American Psychiatric Association 2013). The aim of the drinking in EFSDT is to satisfy the rats’ physiological need and not to prevent a feared event, like the electric shock in EFSDT.
If CA inhibitors are to be used in the treatment of ADHD, it is important to identify possible adverse reactions. No clinically significant adverse effects with the long-term usage of AZ in children with refractory epilepsy have been reported, except for transient drowsiness in some patients (Katayama et al. 2002). A meta-analysis of zonisamide, another CA inhibitor, also revealed no obvious adverse effects (Verrotti et al. 2013). Our previous study has shown that AZ at a dose of 10 mg/kg (i.p.) inhibits the fear memory of Wistar rats (Yang et al. 2013). However, the administration of AZ at a dose of 3 mg/kg did not inhibit the spatial learning of SHR in this study (Fig. 4). This dose-dependent impairment of cognition is consistent with the study by Loring et al. (2011) in that topiramate, an antiepileptic drug with CA inhibitor activity, impairs cognition in normal adults only at higher doses.
It has been reported that dysfunctional monoaminergic signalings, especially the dopaminergic and noradrenergic function, contribute to the pathogenesis of ADHD (Del Campo et al. 2011). The current anti-ADHD drugs are mixed dopamine/norepinephrine reuptake inhibitors such as methylphenidate and norepinephrine reuptake inhibitors such as atomoxetine. Here, we showed that CA inhibitors antagonized the hyperactivity and the impulsivity of SHRs. The possible mechanisms of this effect may involve the dopaminergic system, the noradrenergic system, and GABAA receptors. CA affects GABA neurons in ventral tegmental area via GABAA receptors, and AZ has been reported to prevent the switching of inhibitory GABAA receptors to excitatory GABAA receptors because of the decreased production of bicarbonate (Laviolette et al. 2004; Ting-A-Kee et al. 2013). Presynaptic GABAA receptors facilitate GABAergic transmission to dopaminergic neurons in ventral tegmental area and inhibit dopamine release (Chaudieu et al. 1994; Xiao et al. 2007). Therefore, CA inhibitors can increase dopamine release in ventral tegmental area, which involves in the delayed reward system and the pathogenesis of ADHD (Dichter et al. 2012; Sonuga-Barke 2005). In addition, zonisamide, an antiepileptic drug with CA inhibitory activity, has been reported to increase extracellular and intracellular dopamine concentration in rodents (Okada et al. 1995; Tominaga et al. 2001). Furthermore, zonisamide is used to treat impulsivity control disorder in Parkinson’s disease (Bermejo et al. 2010). Besides the dopaminergic system, the noradrenergic system has been reported to be involved in the anticonvulsant activities of CA inhibitors (Gray and Rauh 1974; Torchiana et al. 1973). The anticonvulsant activity of MZ is antagonized by the α-adrenergic blocking agents (Gray and Rauh 1974). Therefore, CA inhibitors may affect the neuronal transmission of dopamine and norepinephrine, and show the beneficial action to treat hyperactivity and impulsivity.
Conclusion
Current ADHD drugs still have limited efficacy, and some patients with ADHD cannot tolerate the adverse effects. This is the first preclinical animal study which demonstrated that CA inhibitors are strain-specifically effective to antagonize the hyperactivity and the impulsivity of SHRs, and this is what inspires us to carry on the clinical trial of CA inhibitors in patients with ADHD.
References
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders: DSM-5. American Psychiatric Association, Arlington
Bari A, Robbins TW (2013) Inhibition and impulsivity: behavioral and neural basis of response control. Prog Neurobiol 108:44–79
Bergstom WH, Carzoli RF, Lombroso C, Davidson DT, Wallace WM (1952) Observations on the metabolic and clinical effects of carbonic-anhydrase inhibitors in epileptics. AMA Am J Dis Child 84:771–772
Bermejo PE, Ruiz-Huete C, Anciones B (2010) Zonisamide in managing impulse control disorders in Parkinson’s disease. J Neurol 257:1682–1685
Carmack SA, Howell KK, Rasaei K, Reas ET, Anagnostaras SG (2014) Animal model of methylphenidate’s long-term memory-enhancing effects. Learn Mem 21:82–89
Chaudieu I, St-Pierre JA, Quirion R, Boksa P (1994) GABAA receptor-mediated inhibition of N-methyl-d-aspartate-evoked [3H] dopamine release from mesencephalic cell cultures. Eur J Pharmacol 264:361–369
Cortese S, Holtmann M, Banaschewski T, Buitelaar J, Coghill D, Danckaerts M, Dittmann RW, Graham J, Taylor E, Sergeant J (2013) Practitioner review: current best practice in the management of adverse events during treatment with ADHD medications in children and adolescents. J Child Psychol Psychiatry 54:227–246
Dalley JW, Roiser JP (2012) Dopamine, serotonin and impulsivity. Neuroscience 215:42–58
Dalley JW, Everitt BJ, Robbins TW (2011) Impulsivity, compulsivity, and top-down cognitive control. Neuron 69:680–694
Del Campo N, Chamberlain SR, Sahakian BJ, Robbins TW (2011) The roles of dopamine and noradrenaline in the pathophysiology and treatment of attention-deficit/hyperactivity disorder. Biol Psychiatry 69:e145–e157
Dichter GS, Damiano CA, Allen JA (2012) Reward circuitry dysfunction in psychiatric and neurodevelopmental disorders and genetic syndromes: animal models and clinical findings. J Neurodev Disord 4:19
Gray WD, Rauh CE (1974) The anticonvulsant action of the carbonic anhydrase inhibitor methazolamide: possible involvement of a noradrenergic mechanism. Eur J Pharmacol 28:42–54
Jones Z, Dafny N (2013) Dose response effect of methylphenidate on ventral tegmental area neurons and animal behavior. Brain Res Bull 96:86–92
Katayama F, Miura H, Takanashi S (2002) Long-term effectiveness and side effects of acetazolamide as an adjunct to other anticonvulsants in the treatment of refractory epilepsies. Brain Dev 24:150–154
Kawata Y, Okada M, Murakami T, Mizuno K, Wada K, Kondo T, Kaneko S (1999) Effects of zonisamide on K+ and Ca2+ evoked release of monoamine as well as K+ evoked intracellular Ca2+ mobilization in rat hippocampus. Epilepsy Res 35:173–182
Kim P, Choi I, Pena IC, Kim HJ, Kwon KJ, Park JH, Han SH, Ryu JH, Cheong JH, Shin CY (2012) A simple behavioral paradigm to measure impulsive behavior in an animal model of attention deficit hyperactivity disorder (ADHD) of the spontaneously hypertensive rats. Biomol Ther (Seoul) 20:125–131
Laviolette SR, Gallegos RA, Henriksen SJ, van der Kooy D (2004) Opiate state controls bi-directional reward signaling via GABAA receptors in the ventral tegmental area. Nat Neurosci 7:160–169
Loring DW, Williamson DJ, Meador KJ, Wiegand F, Hulihan J (2011) Topiramate dose effects on cognition: a randomized double-blind study. Neurology 76:131–137
Meneses A, Perez-Garcia G, Ponce-Lopez T, Tellez R, Gallegos-Cari A, Castillo C (2011) Spontaneously hypertensive rat (SHR) as an animal model for ADHD: a short overview. Rev Neurosci 22:365–371
Murata M (2010) Zonisamide: a new drug for Parkinson’s disease. Drugs Today 46:251–258
National Research Council (2011) Guide for the care and use of laboratory animals. National Academies Press, Washington, DC
Okada M, Kaneko S, Hirano T, Mizuno K, Kondo T, Otani K, Fukushima Y (1995) Effects of zonisamide on dopaminergic system. Epilepsy Res 22:193–205
Paterson NE, Ricciardi J, Wetzler C, Hanania T (2011) Sub-optimal performance in the 5-choice serial reaction time task in rats was sensitive to methylphenidate, atomoxetine and d-amphetamine, but unaffected by the COMT inhibitor tolcapone. Neurosci Res 69:41–50
Robbins T, Curran H, de Wit H (2012) Special issue on impulsivity and compulsivity. Psychopharmacology (Berl) 219:251–252
Russell VA (2011) Overview of animal models of attention deficit hyperactivity disorder (ADHD). Curr Protoc Neurosci Chapter 9: Unit9 35
Sagvolden T (2000) Behavioral validation of the spontaneously hypertensive rat (SHR) as an animal model of attention-deficit/hyperactivity disorder (AD/HD). Neurosci Biobehav Rev 24:31–39
Sagvolden T, Johansen E (2012) Rat models of ADHD. In: Stanford C, Tannock R (eds) Behavioral neuroscience of attention deficit hyperactivity disorder and its treatment (current topics in behavioral neurosciences). Springer Press, Berlin, pp 301–315
Sagvolden T, Xu T (2008) l-Amphetamine improves poor sustained attention while d-amphetamine reduces overactivity and impulsiveness as well as improves sustained attention in an animal model of attention-deficit/hyperactivity disorder (ADHD). Behav Brain Funct 4:3
Scassellati C, Bonvicini C, Faraone SV, Gennarelli M (2012) Biomarkers and attention-deficit/hyperactivity disorder: a systematic review and meta-analyses. J Am Acad Child Adolesc Psychiatr 51(1003–1019), e20
Shaw M, Hodgkins P, Caci H, Young S, Kahle J, Woods AG, Arnold LE (2012) A systematic review and analysis of long-term outcomes in attention deficit hyperactivity disorder: effects of treatment and non-treatment. BMC Med 10:99
Sonuga-Barke EJ (2005) Causal models of attention-deficit/hyperactivity disorder: from common simple deficits to multiple developmental pathways. Biol Psychiatry 57:1231–1238
Spencer T, Biederman J, Wilens T, Harding M, O’Donnell D, Griffin S (1996) Pharmacotherapy of attention-deficit hyperactivity disorder across the life cycle. J Am Acad Child Adolesc Psychiatry 35:409–432
Sun MK, Alkon DL (2001) Pharmacological enhancement of synaptic efficacy, spatial learning, and memory through carbonic anhydrase activation in rats. J Pharmacol Exp Ther 297:961–967
Ting-A-Kee R, Vargas-Perez H, Mabey JK, Shin SI, Steffensen SC, van der Kooy D (2013) Ventral tegmental area GABA neurons and opiate motivation. Psychopharmacology (Berl) 227:697–709
Tominaga M, Nagatomo I, Uchida M, Hashiguchi W, Akasaki Y, Takigawa M (2001) Alterations of nitric oxide and monoamines in the brain of the EL mouse treated with phenobarbital and zonisamide. Psychiatry Clin Neurosci 55:311–318
Torchiana ML, Lotti VJ, Stone CA (1973) The anticonvulsant effect of carbonic anhydrase inhibitors in mice—a noradrenergic mechanism of action. Eur J Pharmacol 21:343–349
Umehara M, Ago Y, Fujita K, Hiramatsu N, Takuma K, Matsuda T (2013a) Effects of serotonin-norepinephrine reuptake inhibitors on locomotion and prefrontal monoamine release in spontaneously hypertensive rats. Eur J Pharmacol 702:250–257
Umehara M, Ago Y, Kawanai T, Fujita K, Hiramatsu N, Takuma K, Matsuda T (2013b) Methylphenidate and venlafaxine attenuate locomotion in spontaneously hypertensive rats, an animal model of attention-deficit/hyperactivity disorder, through alpha2-adrenoceptor activation. Behav Pharmacol 24:328–331
Verrotti A, Loiacono G, Di Sabatino F, Zaccara G (2013) The adverse event profile of zonisamide: a meta-analysis. Acta Neurol Scand 128:297–304
Westover AN, Halm EA (2012) Do prescription stimulants increase the risk of adverse cardiovascular events?: a systematic review. BMC Cardiovasc Disord 12:41
Willcutt EG (2012) The prevalence of DSM-IV attention-deficit/hyperactivity disorder: a meta-analytic review. Neurotherapeutics 9:490–499
Xiao C, Zhou C, Li K, Ye J-H (2007) Presynaptic GABAA receptors facilitate GABAergic transmission to dopaminergic neurons in the ventral tegmental area of young rats. J Physiol 580:731–743
Yang MT, Chien WL, Lu DH, Liou HC, Fu WM (2013) Acetazolamide impairs fear memory consolidation in rodents. Neuropharmacology 67:412–418
Acknowledgments
The authors would like to thank Sau-Pin Won, MD, a native English speaker, for English editing of this manuscript to the standards of the journal. This work was supported by the Ministry of Science and Technology, Taiwan (NSC 102-2321-B-002-065).
Disclosure/conflicts of interest
The authors have no conflict of interest to be declared.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Fig. S1
Photograph of electro-foot shock aversive water drinking test (EFSDT) apparatus. The black Plexiglas box is divided into three compartments (start area, water area, and free area). During the testing phase (day 3), an electro-foot shock (2 mA, 0.5 s from the stimulator) was given whenever the rats licked water from the bottle for at least 5 s. Details of the apparatus and experimental protocol are described in the “Methods” section. (GIF 66 kb)
Rights and permissions
About this article
Cite this article
Yang, MT., Lu, DH., Chen, JC. et al. Inhibition of hyperactivity and impulsivity by carbonic anhydrase inhibitors in spontaneously hypertensive rats, an animal model of ADHD. Psychopharmacology 232, 3763–3772 (2015). https://doi.org/10.1007/s00213-015-4036-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-015-4036-5