Abstract
Rationale
Mesocorticolimbic reactivity to alcohol-associated cues has been shown to be associated with relapse to renewed drinking and to be decreased by cue-exposure-based extinction training (CET). Evidence from preclinical studies suggests that the extinction of conditioned alcohol-seeking behavior might be facilitated by drugs increasing N-methyl-d-aspartate (NMDA) receptor-associated memory consolidation.
Objectives
In this study, we assessed the efficacy of CET treatment supplemented with the partial NMDA-receptor agonist d-cycloserine (DCS) at reducing mesolimbic cue reactivity (CR), craving, and relapse risk in alcoholism.
Methods
In a randomized, placebo-controlled, double-blind study, we recruited 76 recently detoxified abstinent alcohol-dependent patients. Thirty-two (16 DCS, 16 placebo) patients showed cue-induced ventral-striatal activation measured with functional magnetic resonance imaging (fMRI) prior to treatment and were thus included in the efficacy analyses. After inpatient detoxification, patients underwent nine sessions of CET spaced over 3 weeks, receiving either 50 mg DCS or placebo 1 h prior to each CET session. FMRI was conducted before treatment and 3 weeks after treatment onset.
Results
Following treatment with CET plus DCS, cue-induced brain activation in the ventral and dorsal striatum was decreased compared to treatment with CET plus placebo. Elevated posttreatment ventral striatal CR and increased craving (assessed using the Obsessive Compulsive Drinking Scale) were associated with increased relapse risk.
Conclusions
DCS was shown to augment the effect of CET for alcohol-dependent subjects. The interaction between craving and ventral-striatal CR on treatment outcome suggests that CET might be especially effective in patients exhibiting both high craving and elevated CR.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alcoholism is a chronic relapsing disorder. Even after long periods of abstinence, the risk of relapse, often precipitated by alcohol-associated cues, remains high (Heilig et al. 2011; O’Brien et al. 1998). Cues and contexts predicting the availability of alcohol can initiate alcohol seeking, craving, and relapse (Heilig and Egli 2006). A substantial body of research suggests that there are several types of neuroadaptation that occur in alcoholism (Sullivan and Pfefferbaum 2005), including synapse-specific adaptations of the type thought to underlie specific long-term associative memory (Hyman et al. 2006; Koob and Volkow 2010). Thus, any intervention that aims at the extinction of cue-associated responses should also be useful in the context of relapse prevention. As part of their treatment, patients with substance use disorders can be exposed to conditioned drug stimuli in order to extinguish their drug-associated responses and thereby reduce their craving for drugs (Drummond et al. 1990). Neural cue reactivity was suggested as an endophenotype for alcohol use disorder risk (Claus et al. 2011; Filbey et al. 2008). In a recent functional magnetic resonance imaging (fMRI) study, we showed neural cue reactivity (CR) to be reduced more after cue-exposure treatment (CET) than after standard treatment (Vollstädt-Klein et al. 2011). This result indicates that CET affects mesocorticolimbic reward pathways in addition to other brain areas relevant to addiction memory and attentional focus on alcohol-associated cues in a way that is beneficial for the treatment of alcoholism. Furthermore, Monti and colleagues (Monti et al. 1993) reported craving to be significantly reduced after CET, but only for patients who were classified as “urge reactors” during the pretreatment assessment. Similar findings have also been reported by Scheurich et al. (2004). These results suggest that CET may only be an effective treatment for patients displaying CR, which could be decreased as a treatment goal.
CET is already suggested as a treatment of alcohol addiction (Conklin and Tiffany 2002; Drummond et al. 1990; Monti et al. 1993). The Task Force on Promotion and Dissemination of Psychological Procedures of Division 12 (Clinical Psychology) of the American Psychological Association recommends CET as a Category II of Empirical Support treatment approach (i.e., “probably efficacious/efficacious/or possibly efficacious”) for alcohol abuse and dependence (Chambless and Ollendick 2001). However, for example, the meta-analytical review by Conklin and Tiffany did not show a “consistent evidence for the efficacy of cue-exposure treatment as currently implemented.” They suggest attempts to increase the efficacy of CET in addiction treatment. Pharmacological compounds strengthening consolidation of new memory during extinction might offer such an extension as a novel treatment option. A growing body of evidence suggests that the initiation of reward learning following exposure to an addictive drug depends on N-methyl-d-aspartate (NMDA) receptor-dependent long-term potentiation (LTP) at glutamatergic synapses in the mesolimbic dopamine system (Kauer 2004). One of the potential compounds currently under discussion, d-cycloserine (DCS), a partial agonist at the glycine binding site of the NMDA receptor, has been shown to facilitate extinction processes. Another rationale for examining DCS in enhancing CET effects might be a potential insufficient glutamatergic activity during extinction in alcohol dependence. DCS might increase excitatory NMDA neurotransmission yielding augmentation of extinction by CET. On the other hand, in the present study, we focus on detoxified patients where the glutamatergic state should be normalized (Hermann et al. 2012).
Two milestone studies (Hofmann et al. 2006; Ressler et al. 2004) in anxiety research have shown that treatment approaches combining both CET and DCS are more effective than to CET alone. A recent review (Davis et al. 2006) and a meta-analysis (Norberg et al. 2008) support these initial observations, suggesting that treatment with DCS might increase the effectiveness of CET in addiction treatment.
Preclinical information about the effects of DCS on fear extinction is growing (Davis et al. 2006). But also in addiction paradigms, recent preclinical studies have found DCS to facilitate extinction, to reduce the context specificity of cue-induced reinstatement, to limit the spontaneous recovery of extinguished conditioned responses, and to impair reacquisition (Myers and Carlezon 2012). However, findings from clinical studies in addiction are heterogeneous with some studies reporting no or even a negative effect of DCS on cue-exposure-based extinction (Myers and Carlezon 2012).
DCS facilitated extinction of cue-elicited galvanic skin response (GSR) and craving in smokers (Santa Ana et al. 2009) but with no clinical significance regarding smoking behavior. Another study in smokers detected no significant DCS effects on GSR measured during CET (Kamboj et al. 2011). Price et al. (2009) examined non-treatment-seeking cocaine-dependent participants and found no significant effect of DCS on heart rate (HR) or craving during two CET sessions. However, they found a persisting craving increase in the first CET session only in the DCS group. For alcohol-dependence, there are three clinical studies examining DCS effects in CET. Kamboj et al. (2011) failed to demonstrate a significant effect of DCS on GSR measured during CET in non-treatment-seeking, non-alcohol-dependent volunteers. However, under DCS, they found increased contentedness and a tendency to increased euphoria suggesting an analeptic effect. In a study examining alcohol-dependent patients, Watson et al. (2011) did not find an effect of DCS on craving, mood states, blood pressure, and HR measured during CET sessions. Hofmann et al. (2012) examined heavy drinkers and also found no effect of DCS on HR and craving measured during CET but detected a craving increase in a later off-drug CET session in the DCS group.
This discrepancy in effectiveness between preclinical and clinical work is surprising at first sight. However, it is unlikely that DCS only affects CET in animals, especially when one considers that DCS is effective at augmenting CET at treating anxiety disorders (especially social anxiety disorders and specific phobia). One reason for the lack of DCS effects on CR reduction in humans might be the inclusion of patients showing no or little response to alcohol cues at baseline, which makes it difficult to detect any effect of DCS. Hence, the presence of CR was suggested to be considered as an inclusion criterion for further studies (Watson et al. 2011).
Another reason that previous studies may have failed to detect effects of DCS on CET in humans might be due to different definitions of outcomes. Whereas animal studies typically use established measures (e.g., lever presses) as behavioral CR proxies, human studies have focused on subjective craving or physiological measures of CR, such as galvanic skin response and heart rate. Usually, effect sizes when using these physiological outcome measures are small (around 0.2) (Carter and Tiffany 1999), making it difficult to identify the factors responsible for these effects. Although effect sizes for subjective craving for alcohol are higher (around 0.5 in general, including subclinical populations and untreated alcoholics), social desirability and impaired interoception might lead to a lack of alcohol-associated CR, especially in clinical populations of abstinent patients currently under treatment. To our knowledge, no study to date has examined neural mesolimbic alcohol-associated CR in alcohol dependence. Using neural CR as an outcome measure offers the possibility of assessing the functioning of the mesolimbic dopaminergic system as the neural basis for other cue-associated responses. In this study, we used fMRI to study the effectiveness of DCS at facilitating the extinction of cue-induced mesolimbic activation in alcohol-dependent patients who display mesolimbic CR at baseline. We hypothesized that, in the context of a 3-week CET program, DCS would help reduce neural CR when compared to treatment with CET alone. If confirmed, this finding would represent an important step forward in the treatment of addictive behavior.
Materials and methods
Participants
We recruited 76 abstinent alcohol-dependent patients from the Department of Addictive Behavior and Addiction Medicine at the Central Institute of Mental Health in Mannheim, Germany. Eligibility criteria are described in the supplementary material. Clinical and questionnaire data were acquired 1 day before the first fMRI examination. Anxiety was measured using the State-Trait Anxiety Inventory (STAI, German version (Laux et al. 1981)). Craving for alcohol during the patient’s most recent drinking phase was measured using the Obsessive Compulsive Drinking Scale (OCDS (Mann and Ackermann 2000)).
After enrolment (MK, AJ), each patient was randomly assigned to either the DCS or the control group. Patient assignment to treatment arms was based on a randomization code (permutated blocked randomization, block size 10, allocation ratio 1/1) generated using the software package RITA (Version 1.20, StatSol, Lübeck, Germany), provided by the pharmacy delivering DCS and placebo in identical pill boxes. Patients, clinicians, and researchers were blinded for the allocated intervention. Sealed emergency envelopes including treatment arm assignment were also provided by the pharmacy. Data from five participants were excluded from analysis because of heavy movement in the scanner, technical difficulties, or brain abnormalities. Fifteen patients dropped out because they relapsed during treatment (five in the DCS group, ten in the control group, details see CONSORT flow chart in supplementary material). Of the remaining 56 patients, N = 32 patients exhibited a cue-induced activation in the ventral striatum (VS) at baseline, the condition that was defined a priori as the target marker for the intervention (for definition see “Statistical analysis” section, supplementary material). Table 1 displays clinical characteristics of patients with versus those without CR in the VS. The sample we analyzed in order to address our main research question consisted of 16 patients in the DCS group and 16 control patients. In previous fMRI studies on cue reactivity, similar sample sizes had sufficient power to obtain group activations as well as group differences (Grüsser et al. 2004; Hermann et al. 2006). The groups did not differ at baseline in terms of any of the variables reported in Table 1. The study was approved by the Ethics Committee of the University of Heidelberg and the Federal Institute for Drugs and Medical Devices (Bundesinstitut für Arzneimittel und Medizinprodukte, BfArM, Bonn, Germany). All participants provided written informed consent in accordance with the Declaration of Helsinki.
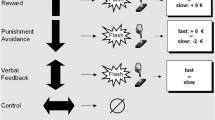
Procedure and cue-exposure-based extinction training
All patients completed medically supervised detoxification before being admitted into the study. During the following 3 weeks, they underwent a qualified alcohol detoxification treatment in our clinic comprising health education, psychotherapeutic treatment in single and group sessions, competence training, relaxation exercises, sport programs, occupational therapy, and sociotherapy. The planned schedule included nine standardized CET sessions (mean 7.68, SD 1.13) spread out over 3 weeks. The reason why not all patients received CET over the complete period of 3 weeks was that CET took place during inpatient treatment, which regularly lasted 3 weeks. In some cases of controlled abstinence, patients were discharged earlier. The patients in the DCS group received a 50-mg dose of DCS 1 h prior to each CET session (Myers and Carlezon 2012). Control patients received a placebo. As in our previous study (Vollstädt-Klein et al. 2011), the CET was administered according to a previously validated (Loeber et al. 2006) treatment manual (Mann et al. 2006). The CET sessions were conducted by a clinically trained psychologist at our institute and supervised regularly to ensure that CET was provided according to the manual. As a treatment extension, CET took place in individual therapy settings. In the first CET session, the concept of CET was explained to the patients. Patients were informed that the exposure could evoke conditioned drug-associated reactions (e.g., increased craving and physiological arousal) and that it is intended to enable the patient to experience changes in these reactions over time, both during each session and over the course of repeated sessions. Furthermore, they were told that the CET session would not end before craving would have vanished. In this first session, the patients developed a hierarchy of personally relevant situations that might trigger a relapse. In each session, the patients were instructed to imagine a situation of the upper third of this hierarchy. When a good imagination was reached, patients were exposed to their favorite alcoholic drink. They were instructed to handle the alcohol bottle, pour a drink, and smell the drink without consuming it. During the CET session, the patients were asked several times about their cognitions, emotions, and physical reactions. They were instructed not to use coping strategies but to leave their attention to the situation they had imagined. The CET session ended when the patient believably assured that no more craving was present. To measure craving before and after the CET session, we used a visual analogue scale described in the “Assessment of alcohol craving” section. One session lasted about 30–90 min and was terminated when the patient reported a craving reduction to zero, a result which all patients were able to achieve. However, for safety reasons, all sessions were scheduled for the morning or early afternoon to assure that patients from the day clinic facility spent some time in the clinic before leaving home and could easily contact a therapist in case of any further craving experience. Using this procedure meant that the CET used in the study was standardized with regard to the way that patients were exposed to their preferred alcoholic beverages, while being individualized with regard to session duration and the individual relapse-provoking situations, the patients were asked to imagine.
FMRI assessment of CR
CR was assessed before treatment as well as 3 weeks after treatment had begun (mean 17.98 days, SD 5.10, range 10–31) using a previously established fMRI cue-reactivity paradigm (Vollstädt-Klein et al. 2010). FMRI assessment, acquisition, and analyses are described in the supplementary material.
Assessment of alcohol craving
The Obsessive Compulsive Drinking Scale (OCDS, German version (Mann and Ackermann 2000)) was used to examine craving during the most recent drinking period. It does not measure short-term or cue-induced craving, but rather mean craving levels over a week long period.
To measure cue-induced craving, patients were asked to rate their craving for alcohol on a visual analogue scale ranging from 0 (“no craving”) to 100 (“extremely extensive craving”) as well as their intention to drink alcohol ranging from 0 (“no intention”) to 100 (“extremely strong intention”) right before and after each session in the scanner and each CET session.
Assessment of alcohol consumption during the follow-up period
Treatment outcomes were measured in terms of time until the first severe relapse in a planned follow-up period of at least 90 days following the first assessment. For that purpose, patients’ drinking patterns were assessed every 4 weeks with self-reports acquired using the Alcohol Timeline Followback (TLFB) method (Sobell et al. 1996). The first two interviews were conducted by telephone, while the third was an in-person interview. The outcome criterion measuring relapse during the follow-up period was defined in terms of time to first heavy relapse, itself defined as an alcohol intake of more than 60 g/day for men and more than 48 g/day for women on at least one drinking occasion.
Statistical analysis
Our main research question examined the effects of combined DCS/CET treatment on CR and this treatment’s outcomes. When looking at effects on a reduction of CR in the mesolimbic system, it is necessary to focus on patients demonstrating any fMRI CR at baseline. Hence, for all analyses including DCS effects, we included only patients with pretreatment VS CR (N = 32), defined as described above. For additional analyses that did not need to examine the effects of DCS treatment, we also included patients who displayed no VS activation to increase our power by maximizing variance in the VS CR measure (all patients N = 56). All analyses that included VS CR as a covariate were run for both the pretreatment and the posttreatment scanner sessions. The following analyses were conducted in Statistical Package of the Social Sciences (SPSS, Version 20, IBM Corp., Somers, NY, USA).
The relationship between VS CR and craving was assessed using linear correlations between mean VS activation and both pretreatment craving, as measured by the OCDS, as well as cue-induced craving (increase in craving or intention to drink after the scanner session, respectively). To examine differences in treatment outcomes with respect to survival functions between the DCS and placebo groups in the subsample of patients who exhibited CR during the first scanner session, we conducted a log-rank test with the time to first severe relapse as the outcome measure and the factor medication. Following this, a Cox regression was performed incorporating the medication factor and VS CR as a covariate along with an interaction term between the two. In addition to these two analyses that we restricted to the subsample initially exhibiting CR, we also ran three additional analyses on both this subsample (N = 32) as well as for the entire sample (N = 56). In the first of these, we assessed the effect of VS CR on treatment outcomes. A second Cox model, also using treatment outcome as the dependent variable, contained OCDS scores or VS CR as a covariate. A further Cox regression featured both of these covariates (VS CR and OCDS scores) together along with the corresponding interaction term. Finally, to further assess possible interactions between pretreatment VS CR, OCDS craving, and medication, we applied a Cox regression with these three variables as covariates including all possible interaction terms in the entire sample VS CR (N = 56). Although analysis of DCS effects was primarily intended for the patients demonstrating pretreatment VS CR (N = 32), here, we used the entire sample because of statistical reasons. When using complex models with high degrees of freedom to examine three-way interactions, one has to supply a dataset covering a broad range of data.
Results
FMRI data
During the first fMRI session, alcohol-dependent patients showed higher activation in response to alcohol cues than in response to control cues in a widespread network, including areas of the visual system, the insula, the amygdala, the thalamus, the hippocampus/parahippocampus, in mesocorticolimbic areas such as the VS and the DS, in the inferior, middle and superior prefrontal cortices (PFC), in the anterior cingulate cortex (ACC), and in the orbitofrontal cortex (OFC) (see supplementary Table 1 and Fig. 1).
After treatment, cue-induced activation decreased in almost all of these areas (see Table 2 and Fig. 2), namely in the insula, the thalamus, the hippocampus/parahippocampus, in striatal/mesocorticolimbic areas, in the inferior, middle and superior PFC, and in the ACC). These decreases could be demonstrated in the whole group, as well as in the DCS and placebo group separately. Brain activation in the visual system, the amygdala, and the OFC did not differ from pretreatment activation. We did not find any brain regions with increased cue-induced activation after treatment.
Posttreatment control patients showed significantly stronger cue-induced fMRI activation than DCS patients in the VS [36 voxels, (x, y, z) = (12, 10, −6), t = 3.34, p = 0.001] as well as the DS [48 voxels, (x, y, z) = (−12, 12, 22), t = 2.94, p = 0.003; see Fig. 3]. DCS patients did not exhibit higher cue-induced activation than control patients in any brain region.
Larger striatal cue-induced activation (contrast “alcohol-neutral stimuli”) in alcohol-dependent patients after 3 weeks of treatment with CET and placebo (N = 16) compared to treatment with CET and DCS (N = 16), for illustration purposes; p < 0.05 uncorrected; cluster size ≥20 voxels; (x, y, z) = (12, 10, −6)
CR in the VS (our main region of interest) was not associated with either an increase in cue-induced craving, intention to drink alcohol, or the OCDS score at either of the two scanner sessions (p > .05, N = 32). When also including patients who did not exhibit VS CR during the first scanner session, we found positive associations between VS CR prior to treatment and increase in craving during the scanner session (r = .275, p = .042, N = 56) as well as increase in intention to drink (r = .280, p = .038, N = 56). At the posttreatment scanner session, we did not find any such associations (p > .05, N = 56).
Subjective craving data
Patients who exhibited VS CR before treatment began demonstrating a higher increase in craving at the first fMRI scanning session (with CR, increase of 4.31 ± 11.44; without CR, decrease of 2.48 ± 9.69; p = .025) as well as a higher increase in their intention to drink alcohol (with CR, increase of 0.69 ± 2.31; without CR, decrease of 2.78 ± 9.32; p = .048) compared to patients not exhibiting VS CR before treatment. At the second fMRI session, the groups did not differ with regard either to the increase in their craving or their intention to drink (p > .05).
Furthermore, we did not find a medication effect on cue-induced craving: DCS and placebo patients did not differ in cue-induced craving after treatment [i.e., craving increase during the scanner session (“craving,” p = .548; “intention to drink,” p = .856)].
The cue-induced craving before and after each CET session was close to zero: Mean craving at the beginning of the CET sessions was 2.26 ± 8.62. The average intention to drink was 1.76 ± 8.87. The CET session ended when the patient believably assured that no more craving was present. After the CET session, craving was 3.23 ± 8.33 on average. The mean intention to drink was 1.83 ± 5.35.
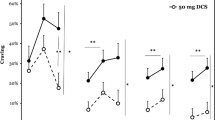
Treatment outcome and association with fMRI CR and craving
The medication groups did not differ significantly when comparing the survival distributions (p = .412, N = 32). Kaplan-Meier estimates for the relapse rates after the planned follow-up period of 90 days are 18.8 % in the control and 12.5 % in the DCS group. The sample size might have not provided enough power to reach statistical significance.
However, the evaluation of the relationship between VS CR and craving for the entire group (N = 56) as influencing variables revealed an interaction effect between posttreatment VS activation and OCDS scores on relapse behavior (p = .033), which was driven by an increased relapse risk in patients who had both high OCDS craving scores as well as elevated VS CR after treatment (no such effect was found for pretreatment fMRI data; p = .503). The main effect of the VS CR variable was also significant (p = .029) but not interpretable because of the interaction effect. In the subsample of patients exhibiting pretreatment VS CR, we did not find this interaction effect (pretreatment fMRI data p = .722; posttreatment p = .118).
Furthermore, we found a significant three-way interaction between pretreatment VS CR, medication, and OCDS craving (p = .0106). This interaction was driven by the following findings. In DCS patients with high OCDS craving, relapse risk decreases with increasing VS CR, whereas in control patients with low OCDS craving, relapse risk decreases with increasing VS CR. Furthermore, in control patients with high VS CR, the relapse risk increases with increasing OCDS. Finally, in patients with high OCDS craving and high VS CR, DCS is more efficacious compared to placebo.
Discussion
The main result of our study is that patients’ neural CR could be decreased by extinction training (CET) and that a combination of CET with a pharmacological treatment with DCS augmented these effects in the VS and DS. Furthermore, patients with high posttreatment VS CR and intense craving were also at higher risk of relapse.
Whereas we found DCS to facilitate the effects of CET on VS CR, we detected no direct effect of DCS on subjective cue-induced craving. However, several previous studies have reported a lack of agreement between self-reported measures of cue reactivity and psychophysiological measures (Yalachkov et al. 2012).
In line with the results of our earlier studies (Heinz et al. 2004; Vollstädt-Klein et al. 2011; Vollstädt-Klein et al. 2012), alcohol-dependent patients in this study exhibited higher activation in response to alcohol-related cues than to control cues in a large network, including regions commonly implicated in CR (for a recent review see Schacht et al. (2013)), indicating that the CR paradigm we used worked well. As expected, cue-induced brain activation was reduced following CET in almost all brain regions, which is in agreement with the results of our previous CET study (Vollstädt-Klein et al. 2011).
As hypothesized, patients receiving DCS showed less cue-induced fMRI activation in the VS and DS than patients receiving placebo, whereas DCS patients were not found to have more cue-induced activation than placebo patients in any brain region. This finding supports the hypothesis that DCS augments the effects of CET in alcohol-dependent subjects and is in line with previous findings in the field of anxiety research (see review (Davis et al. 2006) and meta-analysis (Norberg et al. 2008)) as well as preclinical studies on addiction (see review (Myers and Carlezon 2012)). Results from clinical studies in addiction are heterogeneous (see review (Myers and Carlezon 2012)). The lack of effect of CET augmentation by DCS in addiction in contrast to anxiety disorders might be explained by less evidence for CET efficiency in addiction treatment. Besides this, the learning processes underlying addictions and the stimulus-outcome contingencies are different compared to anxiety disorder, which might impede efforts to extinguish cue reactivity in addiction. The discrepancy between preclinical and clinical work in the addiction field might also be a result of the heterogeneous samples assessed in the clinical studies. In this study, we focused on patients who exhibited VS CR before treatment because our study was intended to evaluate the extent to which combined DCS/CET treatment reduced CR. Another explanation for the lack of findings of DCS/CET effects on CR in the literature may be that most of the previous clinical studies have used peripheral physiological or self-rating measures of CR, which might not be appropriate to detect the effects of DCS. To our knowledge, no previous clinical study has examined the impact of DCS on CET treatment by measuring fMRI CR in alcohol-dependent patients, thereby assessing the functioning of the mesolimbic system, which is the origin of cue-associated responses. There is one fMRI study on DCS’s influence on the effects of CET, in the field of research on cocaine addiction (Prisciandaro et al. 2013). The authors of this study did not find lower levels of neural CR in N = 9 DCS patients than in the N = 12 placebo patients they examined. As the authors mention, only two sessions of CET might be “insufficient to produce a clinical effect.” Another reason for their failure to detect an effect could have been their small sample size. A recent review by Myers and Carlezon (2012) discussed other possible explanations for the divergent effects of DCS on CET in substance addiction. For future studies, they suggest applying DCS in low doses, administering DCS not more than 1 h before starting CET, spacing DCS dosages sufficiently far apart, and restricting the sample to abstinent participants who are not being treated with antidepressants. Furthermore, they suggest using clinical instead of subclinical samples, as well as conducting a follow-up assessment. These recommendations describe the setting of our study almost perfectly, which might explain why we found a positive DCS effect.
It should be noted that we observed a descriptive difference in relapse rates (18.8 % in the control versus 12.5 % in the DCS group), which was not statistically significant. A reason might be the lack of power in the 16 versus 16 patients. Hence, it might be that a main effect of DCS/CET on relapse risk remained undetected in our sample. Interestingly, we observed an interaction effect between OCDS scores and posttreatment VS activation on relapse behavior. Patients with both elevated CR and high OCDS craving scores were at higher risk for relapse. This group might benefit especially from combined treatment using both CET and DCS, because, as we have shown, DCS/CET treatment is more effective at decreasing VS CR than CET alone. The three-way interaction effect between pretreatment VS CR, OCDS, and medication supports this interpretation, because the interaction was driven by decreased relapse risk under DCS compared to placebo, especially in the patient group with elevated pretreatment CR and high OCDS craving.
Furthermore, the observed two-way interaction between OCDS scores and posttreatment VS activation indicates that high VS CR alone might not be sufficient to increase relapse risk and that high VS CR might therefore only pose a risk for those patients whose alcohol use is highly obsessive-compulsive—or rather those whose alcohol dependence is more severe, since the OCDS has been shown to be associated with the severity of alcohol dependence (Moak et al. 1998).
This interpretation is in line with the results of previous studies of our group. For both light and heavy social drinkers, we found VS CR to be higher for drinkers whose OCDS scores were low, especially for light social drinkers (Vollstädt-Klein et al. 2010). In another study, we found that only patients whose dependence duration was short had an alcohol-related attentional bias, indicating that patients who had been dependent for longer might not respond to alcohol cues (Loeber et al. 2009).
Patients demonstrating neural CR in the VS showed less pretreatment alcohol consumption and had fewer detoxifications in their medical history. This might indicate that these patients are less severely dependent compared to their counterparts without VS CR who might not respond to appetitive alcohol cues but who might drink because of habitual alcohol consumption. This interpretation is in line with our previous study (Vollstädt-Klein et al. 2010), which found VS CR to be lower in patients whose alcohol use is obsessive-compulsive. Our results are also consistent with results from other fMRI CR studies, in which not all samples activated the VS, indicating that only subgroups of patients might demonstrate neural CR in the VS (Schacht et al. 2013; Yalachkov et al. 2012). Besides this, patients in our study were recently detoxified, which also might have decreased neural CR. However, as patients without neural VS CR might be more severely dependent, this interpretation is not very likely, because one would expect a CR decrease especially in less severe dependent patients.
Limitations
Our results should be replicated using larger samples, which would increase statistical power, especially when applying complex models including three-way interactions. The lack of association between VS CR and cue-induced craving in the subgroup of patients who exhibited VS CR at the initial screening might also be a consequence of low statistical power, particularly because we were able to detect this association in the sample including patients not initially displaying CR.
Since an fMRI-based treatment approach requires too many resources to make it into clinical practice, it is better seen as an indication that it is at least possible to use fMRI cue reactivity to study the effectiveness of future treatments (“proof of principle”). Further studies with larger sample sizes should be conducted to evaluate clinical effectiveness of DCS with CET with clinical outcome measures like relapse rates or amount of drinking.
Conclusions
In conclusion, this is the first fMRI study to demonstrate CET combined with DCS treatment to reduce neural alcohol-associated CR more than CET alone. Furthermore, our results indicate that this treatment may be especially beneficial to the subgroup of patients exhibiting both high VS CR and high OCDS craving. For patients with low CR, who may be more severely dependent and whose alcohol consumption may be more habitual and less responsive to cues (Vollstädt-Klein et al. 2010), other treatment options may be more appropriate (Litten et al. 2012).
References
Carter BL, Tiffany ST (1999) Meta-analysis of cue-reactivity in addiction research. Addiction 94:327–340
Chambless DL, Ollendick TH (2001) Empirically supported psychological interventions: controversies and evidence. Annu Rev Psychol 52:685–716
Claus ED, Ewing SW, Filbey FM, Sabbineni A, Hutchison KE (2011) Identifying neurobiological phenotypes associated with alcohol use disorder severity. Neuropsychopharmacology 36:2086–2096
Conklin CA, Tiffany ST (2002) Applying extinction research and theory to cue-exposure addiction treatments. Addiction 97:155–167
Davis M, Ressler K, Rothbaum BO, Richardson R (2006) Effects of D-cycloserine on extinction: translation from preclinical to clinical work. Biol Psychiatry 60:369–375
Drummond DC, Cooper T, Glautier SP (1990) Conditioned learning in alcohol dependence: implications for cue exposure treatment. Br J Addict 85:725–743
Filbey FM, Claus E, Audette AR, Niculescu M, Banich MT, Tanabe J, Du YP, Hutchison KE (2008) Exposure to the taste of alcohol elicits activation of the mesocorticolimbic neurocircuitry. Neuropsychopharmacology 33:1391–1401
Grüsser SM, Wrase J, Klein S, Hermann D, Smolka MN, Ruf M, Weber-Fahr W, Flor H, Mann K, Braus DF, Heinz A (2004) Cue-induced activation of the striatum and medial prefrontal cortex predicts relapse in abstinent alcoholics. Psychopharmacology (Berlin) 175:296–302
Heilig M, Egli M (2006) Pharmacological treatment of alcohol dependence: target symptoms and target mechanisms. Pharmacol Ther 111:855–876
Heilig M, Goldman D, Berrettini W, O’Brien CP (2011) Pharmacogenetic approaches to the treatment of alcohol addiction. Nat Rev Neurosci 12:670–684
Heinz A, Siessmeier T, Wrase J, Hermann D, Klein S, Grüsser SM, Flor H, Braus DF, Buchholz HG, Gründer G, Schreckenberger M, Smolka MN, R”sch F, Mann K, Bartenstein P (2004) Correlation between dopamine D2 receptors in the ventral striatum and central processing of alcohol cues and craving. Am J Psychiatr 161:1783–1789
Hermann D, Smolka MN, Wrase J, Klein S, Nikitopoulos J, Georgi A, Braus DF, Flor H, Mann K, Heinz A (2006) Blockade of cue-induced brain activation of abstinent alcoholics by a single administration of amisulpride as measured with fMRI. Alcohol Clin Exp Res 30:1349–1354
Hermann D, Weber-Fahr W, Sartorius A, Hoerst M, Frischknecht U, Tunc-Skarka N, Perreau-Lenz S, Hansson AC, Krumm B, Kiefer F, Spanagel R, Mann K, Ende G, Sommer WH (2012) Translational magnetic resonance spectroscopy reveals excessive central glutamate levels during alcohol withdrawal in humans and rats. Biol Psychiatry 71:1015–1021
Hofmann SG, Meuret AE, Smits JA, Simon NM, Pollack MH, Eisenmenger K, Shiekh M, Otto MW (2006) Augmentation of exposure therapy with D-cycloserine for social anxiety disorder. Arch Gen Psychiatry 63:298–304
Hofmann SG, Huweler R, MacKillop J, Kantak KM (2012) Effects of D-cycloserine on craving to alcohol cues in problem drinkers: preliminary findings. Am J Drug Alcohol Abuse 38:101–107
Hyman SE, Malenka RC, Nestler EJ (2006) Neural mechanisms of addiction: the role of reward-related learning and memory. Annu RevNeurosci 29:565–598
Kamboj SK, Massey-Chase R, Rodney L, Das R, Almahdi B, Curran HV, Morgan CJ (2011) Changes in cue reactivity and attentional bias following experimental cue exposure and response prevention: a laboratory study of the effects of D-cycloserine in heavy drinkers. Psychopharmacology (Berlin) 217:25–37
Kauer JA (2004) Learning mechanisms in addiction: synaptic plasticity in the ventral tegmental area as a result of exposure to drugs of abuse. Annu Rev Physiol 66:447–475
Koob GF, Volkow ND (2010) Neurocircuitry of addiction. Neuropsychopharmacology 35:217–238
Laux L, Glanzmann P, Schaffner P, Spielberger CD (1981) STAI: Das State-Trait Angstinventar. Theoretische Grundlagen und Handanweisung [STAI: The State-Trait Anxiety. Theoretical Background and Manual]. Beltz, Weinheim
Litten RZ, Egli M, Heilig M, Cui C, Fertig JB, Ryan ML, Falk DE, Moss H, Huebner R, Noronha A (2012) Medications development to treat alcohol dependence: a vision for the next decade. Addict Biol 17:513–527
Loeber S, Croissant B, Heinz A, Mann K, Flor H (2006) Cue exposure in the treatment of alcohol dependence: effects on drinking outcome, craving and self-efficacy. Br J Clin Psychol 45:515–529
Loeber S, Vollstädt-Klein S, von der Goltz C, Flor H, Mann K, Kiefer F (2009) Attentional bias in alcohol-dependent patients: the role of chronicity and executive functioning. Addict Biol 14:194–203
Mann K, Ackermann K (2000) Die OCDS-G: Psychometrische Kennwerte der deutschen Version der Obsessive Compulsive Drinking Scale [The OCDS-G: Psychometric characteristics of the German Version of the Obsessive Compulsive Drinking Scale]. Sucht 46:90–100
Mann K, Loeber S, Croissant B, Kiefer F (2006) Qualifizierter Entzugsbehandlung von Alkoholabhängigen: Ein Manual zur Pharmako- und Psychotherapie [Extended alcohol detoxification: a manual for pharmaco- and psychotherapeutic treatment]. Deutscher Ärzteverlag, Köln
Moak DH, Anton RF, Latham PK (1998) Further validation of the obsessive-compulsive drinking scale (OCDS). Relationship to alcoholism severity. Am J Addict 7:14–23
Monti PM, Rohsenow DJ, Rubonis AV, Niaura RS, Sirota AD, Colby SM, Goddard P, Abrams DB (1993) Cue exposure with coping skills treatment for male alcoholics: a preliminary investigation. J Consult Clin Psychol 61:1011–1019
Myers KM, Carlezon WA Jr (2012) D-cycloserine effects on extinction of conditioned responses to drug-related cues. Biol Psychiatry 71:947–955
Norberg MM, Krystal JH, Tolin DF (2008) A meta-analysis of D-cycloserine and the facilitation of fear extinction and exposure therapy. Biol Psychiatry 63:1118–1126
O’Brien CP, Childress AR, Ehrman R, Robbins SJ (1998) Conditioning factors in drug abuse: can they explain compulsion? J Psychopharmacol 12:15–22
Price KL, McRae-Clark AL, Saladin ME, Maria MM, DeSantis SM, Back SE, Brady KT (2009) D-cycloserine and cocaine cue reactivity: preliminary findings. Am J Drug Alcohol Abuse 35:434–438
Prisciandaro JJ, Myrick H, Henderson S, McRae-Clark AL, Santa Ana EJ, Saladin ME, Brady KT (2013) Impact of DCS-facilitated cue exposure therapy on brain activation to cocaine cues in cocaine dependence. Drug Alcohol Depend 132:195–201
Ressler KJ, Rothbaum BO, Tannenbaum L, Anderson P, Graap K, Zimand E, Hodges L, Davis M (2004) Cognitive enhancers as adjuncts to psychotherapy: use of D-cycloserine in phobic individuals to facilitate extinction of fear. Arch Gen Psychiatry 61:1136–1144
Santa Ana EJ, Rounsaville BJ, Frankforter TL, Nich C, Babuscio T, Poling J, Gonsai K, Hill KP, Carroll KM (2009) D-Cycloserine attenuates reactivity to smoking cues in nicotine dependent smokers: a pilot investigation. Drug Alcohol Depend 104:220–227
Schacht JP, Anton RF, Myrick H (2013) Functional neuroimaging studies of alcohol cue reactivity: a quantitative meta-analysis and systematic review. Addict Biol 18:121–133
Scheurich A, Loerch B, Szegedi A, Hautzinger M, Schmidt LG (2004) Cue exposure: differential effects on cue reactivity and drinking outcome measures. Alcohol Clin Exp Res 28:65A
Sobell LC, Brown J, Leo GI, Sobell MB (1996) The reliability of the Alcohol Timeline Followback when administered by telephone and by computer. Drug Alcohol Depend 42:49–54
Sullivan EV, Pfefferbaum A (2005) Neurocircuitry in alcoholism: a substrate of disruption and repair. Psychopharmacology (Berlin) 180:583–594
Vollstädt-Klein S, Wichert S, Rabinstein J, Buhler M, Klein O, Ende G, Hermann D, Mann K (2010) Initial, habitual and compulsive alcohol use is characterized by a shift of cue processing from ventral to dorsal striatum. Addiction 105:1741–1749
Vollstädt-Klein S, Loeber S, Kirsch M, Bach P, Richter A, Buhler M, von der Goltz C, Hermann D, Mann K, Kiefer F (2011) Effects of cue-exposure treatment on neural cue reactivity in alcohol dependence: a randomized trial. Biol Psychiatry 69:1060–1066
Vollstädt-Klein S, Loeber S, Richter A, Kirsch M, Bach P, von der Goltz C, Hermann D, Mann K, Kiefer F (2012) Validating incentive salience with functional magnetic resonance imaging: association between mesolimbic cue reactivity and attentional bias in alcohol-dependent patients. Addict Biol 17:807–816
Watson BJ, Wilson S, Griffin L, Kalk NJ, Taylor LG, Munafo MR, Lingford-Hughes AR, Nutt DJ (2011) A pilot study of the effectiveness of D-cycloserine during cue-exposure therapy in abstinent alcohol-dependent subjects. Psychopharmacology (Berlin) 216:121–129
Yalachkov Y, Kaiser J, Naumer MJ (2012) Functional neuroimaging studies in addiction: multisensory drug stimuli and neural cue reactivity. Neurosci Biobehav Rev 36:825–835
Acknowledgments
This study was supported by a grant from the Deutsche Forschungsgemeinschaft (grant ID SFB 636, D6) and the Bundesministerium für Bildung und Forschung (NGFN+ grant ID 01 GS08152, SP 13). We would like to thank Daniela Hirsch and Carsten Kern for their assistance in data collection, and Jürgen Weber for his contribution in data preparation. The experiments comply with the current laws of Germany.
Conflict of interest
The authors report no biomedical financial interests or potential conflicts of interestClinicalTrials.gov ID: NCT00926900.
Author contributions
FK, MK, CG, SL, and SVK were responsible for the study concept and design. MK and AJ contributed to recruitment, the acquisition of fMRI, and MRI data. MK and AJ conducted the CET sessions. MK, SH, AJ, and SVK were involved in data administration. FK, MK, PB, SH, IR, and SVK provided the data analysis and interpretation of findings. FK and SVK drafted the manuscript. FK, MK, PB, SH, IR, AJ, CG, RS, KM, SL, and SVK provided critical revision of the manuscript for important intellectual content. All authors critically reviewed content and approved final version for publication.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 79 kb)
Rights and permissions
About this article
Cite this article
Kiefer, F., Kirsch, M., Bach, P. et al. Effects of d-cycloserine on extinction of mesolimbic cue reactivity in alcoholism: a randomized placebo-controlled trial. Psychopharmacology 232, 2353–2362 (2015). https://doi.org/10.1007/s00213-015-3882-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-015-3882-5