Abstract
As an aggressive malignancy, glioblastoma multiforme (GBM) is the most common type of brain tumor. The existing treatments have shown limited achievement in increasing the overall survival of patients. Therefore, identifying the key molecules involved in GBM will provide new potential therapeutic targets. Carmustine is an alkylating agent used as a supplementary therapeutic option for GBM. However, the extensive use of carmustine has been limited by uncertainty about its efficacy. MicroRNAs (miRNAs) are essential in post-transcriptional gene regulation. Many aberrantly expressed miRNAs have been detected in various types of human cancer, including GBM. In this study, we evaluated the potential therapeutic effect of miR-143 in combination with carmustine on GBM cells. A172 cells were transfected with miR-143 mimics and then treated with carmustine. To assess the cell viability, apoptosis induction, and cell cycle progression, the MTT assay, Annexin V/PI apoptosis assay, and flow cytometry were used, respectively. Furthermore, qRT‐PCR assay was applied to evaluate the expression level of genes related to apoptosis. The obtained results evidenced that miR-143 transfection could promote the sensitivity of A172 cells to carmustine and enhance carmustine-induced apoptosis via modulating the expression levels of Caspase-3, Caspase-9, Bax, and Bcl-2. Also, our results revealed that combination therapy could effectively diminish cell cycle progression in A172 cells. In conclusion, these results confirmed that miR-143 could enhance carmustine-mediated suppression of cell proliferation and improve the chemosensitivity of A172 cells to this chemotherapeutic agent. Therefore, miR-143 combination therapy may be a promising GBM treatment approach.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As an aggressive and lethal cancer, glioblastoma multiforme (GBM) accounts for about 60% of brain tumors in adults. The incidence of GBM is less than 10 per 100,000 persons, but its rate has grown over the last decade. The median survival from diagnosis in patients with GBM is about ten months (Taylor et al. 2019). Hallmarks of the aggressive GBM include extensive infiltration and vascular proliferation into the brain parenchyma. The standard treatment for GBM is surgery. This method includes consideration of maximum resection of tumor tissue. Even, when possible, surgical resection of GBM is limited via the aggressiveness of the GBM, which is characterized by extensive tumor vascularization and infiltration into the surrounding tissue. Hence, resection surgery is followed by a course of radiotherapy and chemotherapy (Ozdemir-Kaynak et al. 2018). Various chemotherapeutic agents have been used to improve GBM patients’ survival rate. Among these, alkylating antineoplastic agents, including temozolomide, lomustine, and carmustine, have displayed some advantages and have been employed clinically in treating GBM (Hanif et al. 2017). Carmustine, which is a nitrogen mustard compound, induces the formation of interstrand DNA crosslinks between the amino group of cytosine and guanine bases. Carmustine is used either in the initial diagnosis of GBM or tumor recurrence by wafer implantation or intravenous injection (Xiao et al. 2020; Wu et al. 2021). O6-alkylguanine-DNA transferase (AGT) is an enzyme participating in DNA repair, and studies have shown that it provides chemoresistance in brain tumors, especially against carmustine. Subsequently, carmustine is sometimes used in cooperation with inhibitors of AGT to achieve better therapeutic outcomes (Gajewski et al. 2005; Attenello et al. 2012). Carmustine is highly cytotoxic, and treatment with this drug leads to the development of resistance that further limits its advantage; moreover, it is associated with many side effects (Friedman et al. 2000). In patients with GBM, chemotherapy efficacy is limited due to high recurrence rates, devastating neurological deterioration, and overall resistance to therapy (Kim et al. 2015). MicroRNAs (miRNAs) are a class of short single-stranded non-coding RNA, having 21–25 nucleotides length. miRNAs play critical roles in protein translation inhibition and mRNA degradation by directly targeting mRNAs. Currently, over 700 miRNAs have been identified in human cells. By regulating the expression of oncogenes and tumor suppressors, they participate in processes correlated to the molecular pathology of cancer. Moreover, miRNAs are usually located in fragile genomic regions or cancer-related regions (Novakova et al. 2009; Ghasabi et al. 2019; Buruiană et al. 2020; Rezaei et al. 2020). miR-143, located in miR-143/miR-145 cluster on chromosome 5, is evolutionarily conserved across species. This cluster is located on chromosome 5 in human (5q33). miR-143 is imperative in cancer cells' growth, progression, and invasiveness (Das and Pillai 2015; Poli et al. 2020). miR-143 is highly expressed in human's normal tissues, including the colon, cervix, uterus, prostate, stomach, and small intestines. In contrast, a low level of miR-143 expression was described in the kidney, placenta, skeletal muscle, liver, testis, brain, and spleen (Iio et al. 2010). Studies have shown that miR-143 is remarkably downregulated in some cancer cell lines, including prostate (Ozen et al. 2008), colon (Akao et al. 2010; Hosseini et al. 2023), ovary (Iorio et al. 2007), bladder (Noguchi et al. 2013), breast (Iorio et al. 2011), neuroblastoma (Yamagata et al. 2010), renal cell carcinoma (Wach et al. 2013), osteosarcoma (Zhang et al. 2010), esophageal squamous cell carcinoma (Wada et al. 2020) and GBM (Zhao et al. 2013; Zaer et al. 2023). A growing body of studies has revealed that miR-143 overexpression could increase the sensitivity of malignant cells to chemotherapy agents, including temozolomide in GBM cells, oxaliplatin in colon cancer cells, and docetaxel in prostate cancer cells (Xu et al. 2011; Wang et al. 2014; Gomes et al. 2018).
Material and methods
Cell culture
A172, U87 and U373 human GBM cell lines were received from the Pasture Institute of Iran, and cells were grown in Gibco RPMI‐1640 medium (USA) containing 10% fetal bovine serum (Gibco, USA), 100 μg/mL streptomycin and 100 U/mL penicillin at 37°C in a moist atmosphere providing 95% humidity and 5% carbon dioxide. The subculture was performed when the cells reached confluency (70–80%). The cell detachment was done using trypsin EDTA (0.25%, Gibco, USA).
RNA extraction, cDNA synthesis and quantitative real-timePCR (qRT‐PCR)
According to the protocol, the cell's total RNA was isolated utilizing TRIzol reagent (South Korea). The NanoDrop spectrophotometer (Thermo Scientific, USA) was employed to assess RNA quantity and quality. cDNA synthesis for miRNA was performed by using the miRCURY Lna Universal cDNA Synthesis Kit, and the BioFact cDNA synthesis kit was employed for target mRNAs. The expression levels of miR-143, Bax, Bcl-2, Caspase-3 and Caspase-9, were assessed via qRT‐PCR reaction utilizing SYBR Green PCR Master Mix (BioFact, South Korea). GAPDH and U6 genes were used as endogenous controls for normalizing the expression levels of target genes and miR-143, respectively. The Livak method (2−ΔΔCt) was used for relative gene expression analysis. The sequences of primers are illustrated in Table 1.
miRNA transfection
First, 1 × 106 A172 cells were placed in an electroporation buffer and put into a 500 mL cuvette, and 20 pmol of miR-143 mimics were added. Transient transfection of miRNA was carried out according to the recommended protocol and utilizing the Gene Pulser Xcell electroporation system (BioRad). Transfected cells (2 × 105 cells/well) were seeded into 6-well plates and kept in the incubator for 48 h. Eventually, the expression of miR-143 was evaluated using the qRT-PCR method.
MTT assay
MTT assay was carried out to assess whether miRNA-143 sensitizes A172 cells to carmustine treatment. The cells were split into two groups; one group was transfected with miR-143, and another was left untransfected. The cells were seeded into 96-well plates and incubated for 24 h. Afterward, the cells were treated with carmustine in different concentrations from 1 μg/mL to 100 μg/mL. After 24 h of exposure to carmustine, the media of wells was removed, and 50 μl MTT reagent (2 mg/ml) was added. Then, incubation was performed for a further 4 h. The MTT solution was substituted by 200 μl of DMSO, and the cells were incubated for 45 min. Finally, the optical density of wells at 570–630 nm was assessed using an ELISA reader system (Sunrise, Tecan, Switzerland). All experiments were conducted in triplicate.
Annexin V/ Propidium Iodide (PI) apoptosis assay
Apoptosis assay was performed utilizing Annexin V/PI Kit. The cells were arranged into four groups: the first group was transfected with miR-143, the second group was treated with carmustine, the third group was treated with miR-143 and carmustine combination, and the fourth group was control cells. 2 × 105 cells per well were cultured in a 6-well plate, and after treatment and incubation, the cells were collected, then binding buffer (100 μL), Annexin‐V/PI (5 μL), and PI (5 μL) were added to each sample, and incubation was performed for 20 min in a dark place. Eventually, the apoptosis rates of groups were assessed using the MACS Quant Flow Cytometry instrument, and the obtained data were analyzed with FlowJo software.
Cell cycle analysis
The cell cycle status was assessed utilizing DAPI dye and flow cytometry. In the first step, 2 × 105 A172 cells transfected with miR-143 and then were seeded into a six-well plate. After 24 h, the cells were treated with carmustine and incubated for a further 24 h. Afterward, the cells were harvested, rinsed with cold PBS, and fixed in 1 ml of ice-cold ethanol (80%) for 24 h at -20 °C. The cells were rewashed and suspended with a solution containing RNase A (1%) and kept for 30 min. Next, the cells were rinsed, stained with DAPI solution (Triton X100 and DAPI), and maintained for 30 min in a dark place. Eventually, the accumulation of cells in the G1, S, and G2 phases of cell cycle was determined by flow cytometry. Data analysis was performed by using FlowJo software.
Statistical analysis
All experiments were done in triplicate, and collected data were analyzed utilizing GraphPad Prism 8.0 Software. The means ± standard deviation (SD) were used to express the obtained results. The student's t-test was performed to evaluate statistical differences between the two groups, and one-way variance (ANOVA) analysis was performed to compare multiple groups. P values that were lower than 0.05 were indicated as statistically significant.
Results
Cell line selection
Figure 1 displays our evaluation of miR‐143 expression across three cell lines (A172, U87, and U373). The findings indicate a notable decrease in miR‐143 expression in both A172 and U87 cell lines compared to U373 (*P < 0.05). Moreover, the expression level of miR‐143 was equivalent in A172 and U87 cell lines (non-significant), leading us to choose the A172 cell line for deeper exploration in this study (Fig. 1).
The overexpression of miR-143 reduced A172 cell proliferation
A qRT-PCR assay was used to validate the transfection efficiency. As shown in Fig. 2A, the qRT-PCR results illustrated that miR-143 expression levels significantly increased in A172 cells after transfection compared to negative control (NC) and untransfected cells (control). The cells were transfected with different doses of miR-143 (10, 20, and 40 pmol), and the results showed that the doses of 20 and 40 pmol significantly increased the expression of miR-143, so the dose of 20 pmol was chosen as the transfection dose. Then, the qRT-PCR method was used to determine the optimum incubation time (Fig. 2B). Cells were transfected with 20 pmol of miR-143 and incubated for different times (24, 48, and 72 h). The results showed that the highest expression levels of miR-143 were at 24 and 48 h after transfection (expression levels were the same), but after 72 h, the expression level decreased significantly. Based on the results, the dose of 20 pmol and 24 h were selected for the transfection dose of miR-143 and the incubation time of the cells.
A Various doses of miR-143 (10, 20, and 40 pmol) were transfected, and the expression level was evaluated using the qRT-PCR. B After transfection with a dose of 20 pmol miR-143, the cells were incubated for different times (24, 48, and 72 h), and the expression of miR-143 was evaluated. C The suppressive effect of miR-143 overexpression on cell proliferation was determined using the MTT method; (****P < 0.0001, ***P < 0.001, **P < 0.01, and ns = non-significant)
Afterward, the effect of miR-143 overexpression on cell proliferation was evaluated using MTT assay. The results evidenced that miR-143 upregulation in A175 cells led to a significant decrease in cell proliferation rate compared to control and NC groups. There was no significant difference in the cell proliferation levels between control and NC cells (Fig. 2C).
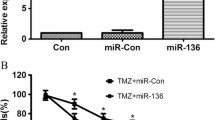
miR-143 cooperatively enhanced carmustine-induced cytotoxicity
An MTT assay was conducted to explore whether treatment with miR-143 could raise the sensitivity of the A172 cells to carmustine. According to Fig. 3, the viability rate reduces dose-dependently with carmustine treatment alone. Also, the combination of miR-143/carmustine remarkably decreased the viability of cells compared to individual groups. Our results exhibited that miR-143 transfection improved the sensitivity of A172 cells to carmustine. As reflected in Fig. 3, the IC50 of carmustine in the combination group was significantly decreased (from 260 µg/ml to 127.5 µg/ml).
miR-143 and carmustine combination effect on cell apoptosis
Using Annexin V/PI staining, the combination effect of miR-143 and carmustine on apoptosis induction was evaluated. Results displayed that miR-143 overexpression and carmustine significantly promote the apoptosis rate from 7.06% in control cells to 12.62% and 39.78%, respectively. Furthermore, in the combination group, the apoptosis rate increased to 69.81% (Fig. 4). These results evidenced that miR-143 overexpression slightly induces apoptosis, and in the combination group, it significantly improves carmustine-mediated apoptosis compared to other groups.
Besides, the qRT-PCR was utilized to evaluate the gene expression associated with apoptosis. According to the results, overexpression of miR-143 and carmustine treatment led to significant upregulation of Bax, Caspase-3, and Caspase-9 expression compared to the control. However, this increase was remarkably higher in the combination group than in others. Also, miR-143 overexpression and carmustine treatment led to the downregulation of Bcl-2 expression. Bcl-2 expression levels decreased more effectively in the combination group than in separate treatments (Fig. 5). These results demonstrated that combination therapy could strongly induce apoptosis in A172 cells through modulating Caspase-3, Caspase-9 Bax, and Bcl-2 expression.
The combination of carmustine and miR‐143 arrested A172 cell cycle at S and G2 phases
Cell cycle assay was conducted utilizing DAPI staining and flow cytometry. As shown in Fig. 5, miR-143 could significantly increase cell population in the S phase from 18.8% to 21%. In cells treated with carmustine, the population of the G2 cells increased from 15.8% to 29.3%. In addition, the combination treatment enhanced cell cycle arrest in S (28.5%) phase (Fig. 6).
Discussion
GBM remains the top deadly cancer of the brain. Current knowledge of the heterogeneity of GBM tumors changed the WHO classification method and shaped the demand for developing new and personalized therapies. Currently, approved treatments, including chemotherapies, show a poor survival rate for GBM. This is due mainly to the fact that the majority of patients gain resistance to these therapeutic agents (Da Ros et al. 2018). Therefore, novel therapeutic approaches are required to overcome this issue. Recent advances in basic GBM science have been translated into innovative clinical trials that take advantage of improved genetic and epigenetic features of GBM, as well as the microenvironment of the brain and interactions with immune system cells (Esemen et al. 2022; Rong et al. 2022). As mentioned, miRNAs, as an important group of epigenetic factors, play a significant role in GBM tumorigenesis (Jiménez-Morales et al. 2022). In particular, the role of miR-143 dysregulation in GBM development and progression has been proven in many studies. In addition, several studies have evidenced that miR-143 overexpression could reduce temozolomide chemoresistance in GBM cells (Zhao et al. 2013; Liu et al. 2015). However, its role in sensitizing GMB cells to other commonly used chemotherapeutic agents, namely carmustine, has not yet been determined. Subsequently, this study investigated the effect of miR-143 restoration on the antitumor activity of carmustine in A172 cell line.
The results from MTT assay demonstrated that miR-143 overexpression could diminish A172 cell proliferation significantly. Besides, the results evidenced that pre-treatment of A172 cells by miR-143 remarkably improved A172 cell chemosensitivity to carmustine treatment. It means that miR-143 combined with carmustine reduced the viability and proliferation rate more effectively than separate treatments. In addition, Annexin V/PI staining assay evidenced that miR-143 could promote carmustine-induced apoptosis in A172 cells. These results were consistent with the findings of Wang et al. showing that miR‑143 overexpression reduced cell proliferation and increased the gemcitabine chemosensitivity of bladder cancer cells (Wang et al. 2017). Borralho et al. showed that elevated expression of miR-143 resulted in a significant reduction in colorectal cancer cell viability. Furthermore, overexpression of miR-143 was associated with decreased viability after exposure to 5-fluorouracil (Borralho et al. 2009). Another study has proven that miR-143 overexpression remarkably increased the chemosensitivity of glioblastoma stem cells to Shikonin. In addition, overexpression of miR-143 significantly enhanced the apoptotic fraction and caused apoptosis to occur earlier (Liu et al. 2015).
To confirm apoptosis and flow cytometry results, mRNA expression of apoptosis-related genes was measured by qRT-PCR. The results demonstrated that miR-143 and carmustine could significantly increase Caspase-3/9 and Bax levels and inhibit Bcl-2 expression compared to control cells. Also, a combination of miR-143 and carmustine could increase the expression of Bax and Caspase-3/9 and decrease Bcl-2 expression more than individual groups. The BCL-2 protein family in the intrinsic apoptosis pathway is crucial in the programmed cell death process. This family comprises pro-survival or anti-apoptotic factors, such as BCL-2 and A1/BFL-1, and pro-apoptotic members, including Bax and Bak proteins. The Bax/Bcl-2 ratio plays an essential role in controlling cell apoptosis. Bax, which normally exists in the cytoplasm, binds with anti-apoptotic proteins such as Bcl-2, playing an important role in mitochondria integrity. When cells are exposed to an apoptotic stimulus, Bax is translocated to the mitochondria and induces pore formation and cytochrome C release, leading to apoptosis activation. Increased Bax expression mediates early apoptosis. Dysregulation of the Bcl-2 family is associated with many cancers (Ola et al. 2011; Ramesh and Medema 2020; Alam et al. 2022). Caspases are a family of proteases that play a key role in apoptosis. This family has two distinct groups: the initiator caspases consisting of Caspase-2, -8, -9, -10, and executioner caspases, including Caspase-3, -6, -7. Diverse commonly used cancer treatments stimulate cell apoptosis to eliminate malignant cells by indirectly engaging these caspases (Boice and Bouchier-Hayes 2020). Li et al. investigated the significance of miR-143 overexpression in regulating the ability of osteosarcoma cells to survive, invade, and migrate. Their findings indicated that miR-143 overexpression was able to constrain the migration and invasion abilities in osteosarcoma cells significantly. Moreover, they demonstrated that miR-143 suppresses Bcl-2 expression and activates Caspase-3, thereby promoting apoptosis induction in osteosarcoma cells (Li et al. 2016). Cao et al. investigated the effects of Zhoushi Qiling Decoction (ZQD), a Traditional Chinese medicine, on human prostate cancer cells. Their findings exhibited that ZQD could stimulate cell apoptosis by miR-143-mediated regulation of Bcl-2 expression. Treatment of prostate cancer cells with ZQD was able to promote apoptosis induction dose-dependently. This effect was reversed by suppressing miR-143 expression in prostate cancer cells using anti-miR-143 treatment. These findings indicate the significance of ZQD-induced miR-143 in preventing prostate cancer by targeting Bcl-2 expression and increasing the activity of Bax and caspase-3 pro-apoptotic factors (Cao et al. 2021). Another study has also established that one of the mechanisms by which carmustine induces apoptosis in malignant cells is to modulate the Bax/Bcl-2 ratio (Zhang et al. 2015).
In the present study, we also investigated the effect of miR-143 and carmustine on GBM cell growth and proliferation by analyzing cell cycle progression. The results obtained from flow cytometry indicated that restoration of miR-143 could induce considerable cell arrest in the S phase. Also, cell treatment with carmustine could induce significant cell arrest in the G2 phase. The combination group exhibited cell arrest in both S and G2 phases, indicating its suppressive effect on cell division and proliferation. Previous studies have also demonstrated the role of miR-143 as a regulator of cell cycle progression in different cancers (Chang et al. 2017; Hossian et al. 2018). In particular, miR-143 overexpression has been shown to induce S-phase cell cycle arrest in A549 and H1299 lung cancer cells (Sanada et al. 2019). Besides, carmustine has been reported to induce cell cycle arrest at the G2/M phase in melanoma cells by regulating p21 and p27 protein expression (Lin et al. 2018). These findings indicated the cooperative function of miR-143 and carmustine in preventing cell cycle progression in GBM.
Conclusion
This research has shown that combining miR-143 and carmustine in A172 cell lines illustrates cooperative anti-tumor effects. Exogenous overexpression of miR-143 was able to increase A172 cell chemosensitivity to carmustine. miR-143 combined with carmustine prevented GMB cell proliferation and promoted apoptosis by controlling the expression of apoptosis-related genes. Also, miR-143 and carmustine showed a cooperative effect on suppressing cell cycle progression. Therefore, treating A172 cells with carmustine and restoring miR-143 could be a new therapeutic approach to improve GBM chemosensitivity and suppress its growth and development.
Data availability
No datasets were generated or analysed during the current study.
Code availability
Not applicable.
References
Akao Y, Nakagawa Y, Hirata I, Iio A, Itoh T, Kojima K, Nakashima R, Kitade Y, Naoe T (2010) Role of anti-oncomirs miR-143 and-145 in human colorectal tumors. Cancer Gene Ther 17:398–408
Alam M, Alam S, Shamsi A, Adnan M, Elasbali AM, Al-Soud WA, Alreshidi M, Hawsawi YM, Tippana A, Pasupuleti VR (2022) Bax/Bcl-2 cascade is regulated by the EGFR pathway: Therapeutic targeting of non-small cell lung cancer. Front Oncol 12:933
Attenello F, Raza SM, Dimeco F, Olivi A (2012) Chemotherapy for brain tumors with polymer drug delivery. Handb Clin Neurol 104:339–353
Boice A, Bouchier-Hayes L (2020) Targeting apoptotic caspases in cancer. Biochim Biophys Acta Mol Cell Res 1867:118688
Borralho PM, Kren BT, Castro RE, Moreira da Silva IB, Steer CJ, Rodrigues CM (2009) MicroRNA-143 reduces viability and increases sensitivity to 5-fluorouracil in HCT116 human colorectal cancer cells. FEBS J 276:6689–6700
Buruiană A, Florian ȘI, Florian AI, Timiș T-L, Mihu CM, Miclăuș M, Oșan S, Hrapșa I, Cataniciu RC, Farcaș M (2020) The roles of miRNA in glioblastoma tumor cell communication: Diplomatic and aggressive negotiations. Int J Mol Sci 21:1950
Cao H, Wang D, Gao R, Chen L, Feng Y, Gao D (2021) Zhoushi Qiling decoction induces apoptosis of human prostate cancer cells via miR-143/Bcl-2 axis. Aging (Albany NY) 13:17202
Chang L, Zhang D, Shi H, Bian Y, Guo R (2017) MiR-143 inhibits endometrial cancer cell proliferation and metastasis by targeting MAPK1. Oncotarget 8:84384–84395
Da Ros M, De Gregorio V, Iorio AL, Giunti L, Guidi M, De Martino M, Genitori L, Sardi I (2018) Glioblastoma chemoresistance: the double play by microenvironment and blood-brain barrier. Int J Mol Sci 19:2879
Das AV, Pillai RM (2015) Implications of miR cluster 143/145 as universal anti-oncomiRs and their dysregulation during tumorigenesis. Cancer Cell Int 15:1–12
Esemen Y, Awan M, Parwez R, Baig A, Rahman S, Masala I, Franchini S, Giakoumettis D (2022) Molecular pathogenesis of glioblastoma in adults and future perspectives: a systematic review. Int J Mol Sci 23:2607
Friedman HS, Kerby T, Calvert H (2000) Temozolomide and treatment of malignant glioma. Clin Cancer Res 6:2585–2597
Gajewski TF, Sosman J, Gerson SL, Liu L, Dolan E, Lin S, Vokes EE (2005) Phase II trial of the O6-alkylguanine DNA alkyltransferase inhibitor O6-benzylguanine and 1, 3-bis (2-chloroethyl)-1-nitrosourea in advanced melanoma. Clin Cancer Res 11:7861–7865
Ghasabi M, Mansoori B, Mohammadi A, Duijf PH, Shomali N, Shirafkan N, Mokhtarzadeh A, Baradaran B (2019) MicroRNAs in cancer drug resistance: Basic evidence and clinical applications. J Cell Physiol 234:2152–2168
Gomes SE, Pereira DM, Roma-Rodrigues C, Fernandes AR, Borralho PM, Rodrigues CM (2018) Convergence of miR-143 overexpression, oxidative stress and cell death in HCT116 human colon cancer cells. PLoS ONE 13:e0191607
Hanif F, Muzaffar K, Perveen K, Malhi SM, Simjee SU (2017) Glioblastoma multiforme: a review of its epidemiology and pathogenesis through clinical presentation and treatment. Asian Pac J Cancer Prev 18:3
Hosseini SS, Nazifi P, Amini M, Zargari F, Yari AH, Baradaran B, Mahboob S, Mokhtarzadeh A (2023) Crocin Suppresses Colorectal Cancer Cell Proliferation by Regulating miR-143/145 and KRAS/RREB1 Pathways. Anticancer Agents Med Chem (Formerly Current Medicinal Chemistry-Anti-Cancer Agents) 23:1916–1923
Hossian A, Sajib M, Tullar PE, Mikelis CM, Mattheolabakis G (2018) Multipronged activity of combinatorial miR-143 and miR-506 inhibits lung cancer cell cycle progression and angiogenesis in vitro. Sci Rep 8:1–14
Iio A, Nakagawa Y, Hirata I, Naoe T, Akao Y (2010) Identification of non-coding RNAs embracing microRNA-143/145 cluster. Mol Cancer 9:1–7
Iorio MV, Visone R, Di Leva G, Donati V, Petrocca F, Casalini P, Taccioli C, Volinia S, Liu C-G, Alder H (2007) MicroRNA signatures in human ovarian cancer. Can Res 67:8699–8707
Iorio MV, Casalini P, Piovan C, Braccioli L, Tagliabue E (2011) Breast cancer and microRNAs: therapeutic impact. Breast 20:S63–S70
Jiménez-Morales JM, Hernández-Cuenca YE, Reyes-Abrahantes A, Ruiz-García H, Barajas-Olmos F, García-Ortiz H, Orozco L, Quiñones-Hinojosa A, Reyes-González J, del Carmen A-Pérez M (2022) MicroRNA delivery systems in glioma therapy and perspectives: A systematic review. J Control Release 349:712–730
Kim S-S, Harford JB, Pirollo KF, Chang EH (2015) Effective treatment of glioblastoma requires crossing the blood–brain barrier and targeting tumors including cancer stem cells: the promise of nanomedicine. Biochem Biophys Res Commun 468:485–489
Li W-h, Wu H-j, Li Y-x, Pan H-g, Meng T, Wang X (2016) MicroRNA-143 promotes apoptosis of osteosarcoma cells by caspase-3 activation via targeting Bcl-2. Biomed Pharmacother 80:8–15
Lin K-I, Lin C-C, Kuo S-M, Lai J-C, Wang Y-Q, You H-L, Hsu M-L, Chen C-H, Shiu L-Y (2018) Carnosic acid impedes cell growth and enhances anticancer effects of carmustine and lomustine in melanoma. Biosci Rep 38:BSR20180005
Liu J, Qu C-B, Xue Y-X, Li Z, Wang P, Liu Y-h (2015) MiR-143 enhances the antitumor activity of shikonin by targeting BAG3 expression in human glioblastoma stem cells. Biochem Biophys Res Commun 468:105–112
Noguchi S, Yasui Y, Iwasaki J, Kumazaki M, Yamada N, Naito S, Akao Y (2013) Replacement treatment with microRNA-143 and-145 induces synergistic inhibition of the growth of human bladder cancer cells by regulating PI3K/Akt and MAPK signaling pathways. Cancer Lett 328:353–361
Novakova J, Slaby O, Vyzula R, Michalek J (2009) MicroRNA involvement in glioblastoma pathogenesis. Biochem Biophys Res Commun 386:1–5
Ola MS, Nawaz M, Ahsan H (2011) Role of Bcl-2 family proteins and caspases in the regulation of apoptosis. Mol Cell Biochem 351:41–58
Ozdemir-Kaynak E, Qutub AA, Yesil-Celiktas O (2018) Advances in glioblastoma multiforme treatment: new models for nanoparticle therapy. Front Physiol 9:170
Ozen M, Creighton C, Ozdemir M, Ittmann M (2008) Widespread deregulation of microRNA expression in human prostate cancer. Oncogene 27:1788–1793
Poli V, Seclì L, Avalle L (2020) The microRNA-143/145 cluster in tumors: a matter of where and when. Cancers 12:708
Ramesh P, Medema JP (2020) BCL-2 family deregulation in colorectal cancer: potential for BH3 mimetics in therapy. Apoptosis 25:305–320
Rezaei T, Amini M, Hashemi ZS, Mansoori B, Rezaei S, Karami H, Mosafer J, Mokhtarzadeh A, Baradaran B (2020) microRNA-181 serves as a dual-role regulator in the development of human cancers. Free Radical Biol Med 152:432–454
Rong L, Li N, Zhang Z (2022) Emerging therapies for glioblastoma: Current state and future directions. J Exp Clin Cancer Res 41:1–18
Sanada H, Seki N, Mizuno K, Misono S, Uchida A, Yamada Y, Moriya S, Kikkawa N, Machida K, Kumamoto T, Suetsugu T, Inoue H (2019) Involvement of dual strands of miR-143 (miR-143–5p and miR-143–3p) and their target oncogenes in the molecular pathogenesis of lung adenocarcinoma. Int J Mol Sci 20:4482
Taylor OG, Brzozowski JS, Skelding KA (2019) Glioblastoma multiforme: an overview of emerging therapeutic targets. Front Oncol 9:963
Wach S, Nolte E, Theil A, Stöhr C, Rau TT, Hartmann A, Ekici A, Keck B, Taubert H, Wullich B (2013) MicroRNA profiles classify papillary renal cell carcinoma subtypes. Br J Cancer 109:714–722
Wada M, Goto Y, Tanaka T, Okada R, Moriya S, Idichi T, Noda M, Sasaki K, Kita Y, Kurahara H (2020) RNA sequencing-based microRNA expression signature in esophageal squamous cell carcinoma: Oncogenic targets by antitumor miR-143-5p and miR-143-3p regulation. J Hum Genet 65:1019–1034
Wang L, Shi Z-m, Jiang C-f, Liu X, Chen Q-d, Qian X, Li D-m, Ge X, Wang X-f, Liu L-Z (2014) MiR-143 acts as a tumor suppressor by targeting N-RAS and enhances temozolomide-induced apoptosis in glioma. Oncotarget 5:5416
Wang H, Li Q, Niu X, Wang G, Zheng S, Fu G, Wang Z (2017) miR-143 inhibits bladder cancer cell proliferation and enhances their sensitivity to gemcitabine by repressing IGF-1R signaling. Oncol Lett 13:435–440
Wu W, Klockow JL, Zhang M, Lafortune F, Chang E, Jin L, Wu Y, Daldrup-Link HE (2021) Glioblastoma multiforme (GBM): An overview of current therapies and mechanisms of resistance. Pharmacol Res 171:105780
Xiao Z-Z, Wang Z-F, Lan T, Huang W-H, Zhao Y-H, Ma C, Li Z-Q (2020) Carmustine as a supplementary therapeutic option for glioblastoma: a systematic review and meta-analysis. Front Neurol 11:1036
Xu B, Niu X, Zhang X, Tao J, Wu D, Wang Z, Li P, Zhang W, Wu H, Feng N (2011) miR-143 decreases prostate cancer cells proliferation and migration and enhances their sensitivity to docetaxel through suppression of KRAS. Mol Cell Biochem 350:207–213
Yamagata T, Yoshizawa J, Ohashi S, Yanaga K, Ohki T (2010) Expression patterns of microRNAs are altered in hypoxic human neuroblastoma cells. Pediatr Surg Int 26:1179–1184
Zaer SJ, Aghamaali M, Amini M, Doustvandi MA, Hosseini SS, Baradaran B, Najafi S, Esfandyari YB, Mokhtarzadeh A (2023) Cooperatively inhibition effect of miR-143-5p and miR-145-5p in tumorigenesis of glioblastoma cells through modulating AKT signaling pathway. BioImpacts 14:29913–29913
Zhang H, Cai X, Wang Y, Tang H, Tong D, Ji F (2010) microRNA-143, down-regulated in osteosarcoma, promotes apoptosis and suppresses tumorigenicity by targeting Bcl-2. Oncol Rep 24:1363–1369
Zhang J, Chen M, Zhang Y, Zhao L, Yan R, Dai K (2015) Carmustine induces platelet apoptosis. Platelets 26:437–442
Zhao S, Liu H, Liu Y, Wu J, Wang C, Hou X, Chen X, Yang G, Zhao L, Che H (2013) miR-143 inhibits glycolysis and depletes stemness of glioblastoma stem-like cells. Cancer Lett 333:253–260
Acknowledgements
The authors are grateful for the supports from Immunology Research Center, Tabriz University of Medical Sciences, Tabriz, Iran, and also Department of Biology, University of Guilan, Rasht, Iran.
Funding
The authors appreciate the supports from the Immunology Research Center, Tabriz University of Medical Sciences, Tabriz, Iran (grant number: 62578).
Author information
Authors and Affiliations
Contributions
Conceptualization: Amir Ali Mokhtarzadeh, Mahmoudreza Aghamaali, Behzad Baradaran, Sheyda Jodeiry Zaer;
Methodology: Amir Ali Mokhtarzadeh, Mohammad Amin Doustvandi;
Supervision: Amir Ali Mokhtarzadeh, Mahmoudreza Aghamaali;
Investigation: Sheyda Jodeiry Zaer, Souzan Najafi, Seyed Samad Hosseini, Mohammad Amini, Mohammad Amin Doustvandi, Nazila Mozammel; data analysis: Sheyda Jodeiry Zaer, Mohammad Amini, Mohammad Amin Doustvandi;
Writing original draft: Sheyda Jodeiry Zaer, Seyed Samad Hosseini;
Writing—review & editing: Sheyda Jodeiry Zaer, Seyed Samad Hosseini, Amir Ali Mokhtarzadeh;
The authors declare that all data were generated in-house and that no paper mill was used.
Corresponding authors
Ethics declarations
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zaer, S.J., Aghamaali, M., Najafi, S. et al. MicroRNA-143 overexpression enhances the chemosensitivity of A172 glioblastoma cells to carmustine. Naunyn-Schmiedeberg's Arch Pharmacol (2024). https://doi.org/10.1007/s00210-024-03287-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00210-024-03287-1