Abstract
Sepsis is a life-threatening condition caused by the body’s response to an infection. Dapsone is a sulfone with antibiotic properties, and experimental evidence suggests it has significant anti-inflammatory and anti-oxidative stress effects. The objective of this study was to investigate the efficacy of dapsone in mice after CLP (cecal ligation and puncture) surgery, which is a model for inducing sepsis. The study divided animals into five groups: CLP, sham, and three groups receiving different doses of dapsone (0.5, 1, 2 mg/kg). Sepsis was induced through CLP surgery, followed by dapsone administration. In each group, half of the mice were used to evaluate levels of various markers and pathological changes at 24 h post-CLP, while the other half was used to record the mortality rates within 96 h. The results showed that single-dose administration of dapsone at (0.5, 1, 2 mg/kg) after CLP surgery improved survival compared to the CLP group. Dapsone was also associated with a significant reduction in pro-inflammatory cytokines TNF-α, IL-1β, IL-6, NO, and MPO, as well as lactate and creatinine serum levels. However, dapsone did not have a significant effect on urea serum levels. In conclusion, the data suggest that dapsone treatment leads to increased survival in septic mice after CLP, and due to its ability to reduce TNF-α, IL-1β, IL-6, MPO, and lactate levels, it has anti-inflammatory effects in sepsis. The sepsis treatment with dapsone in mice protects against inflammation and oxidative stress.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sepsis is a severe and dangerous incidence caused by the immune response to a blood infection, ultimately leading to death (Wang et al. 2024). It is one of the most common causes of hospitalized patients’ death. Annually, approximately 18 million individuals are diagnosed with sepsis, and its mortality rate ranges from 28 to 40% (Jiang et al. 2024). While broad-spectrum antibiotics, corticosteroids, and fluid therapy are used to manage sepsis, lack of a specific treatment, the increasing prevalence of bacterial resistance, and the side effects of existing drugs have made it challenging to effectively treat this disease. Elderlies, pregnant women, hospitalized patients, and patients with cancer, cirrhosis, chronic kidney disease, and immune suppression are at a higher risk (Evans et al. 2021). The prevention of infection at first then the prevention of the spread of infection in the body are the two best strategies to prevent sepsis (Luangasanatip et al. 2015). Sepsis can be caused by a direct infection, such as appendicitis, urinary tract infections, or pneumonia, or indirectly through surgical procedures, trauma, or burns (Ludwig and Hummon 2017). It is characterized by a high level of acute infection in any part of the body, surpassing the threshold of resistance and compromising optimal immune function, resulting in systemic disease spread and associated inflammation throughout the body’s circulation, Eventually, the septic shock will occur with increased lactate, severe hypotension, followed by vascular collapse if this process continues (Hotchkiss et al. 2016). Inadequate oxygen supply to the cells and hypotension exacerbates this condition, leading to septic shock and low cardiac output (Marques et al. 2023; Morris et al. 2023).
Bacteria, fungi, and viruses can trigger sepsis and release critical inflammatory mediators and complex interactions with the onset of inflammatory cascade events (Poll et al. 2021). Important inflammatory mediators of immediate release from the innate immune system include interleukin-1β (IL-1β), IL-6, tumor necrosis factor-α (TNF-α), interferon-ɣ (IFN-ɣ), and essential secondary mediators such as nitric oxide (NO) and reactive oxygen species (Joffre et al. 2020). Nitric oxide is made by active macrophages, neutrophils, lymphocytes, and other cells that plays a crucial role in cellular signaling and regulating vascular tone and modulation of the inflammatory process. The increase of nitric oxide causes vasodilation and the reduction of the vascular response to vasoconstrictors (Oliveira et al. 2022). Reactive oxygen species (ROS) produced under these conditions impair cellular respiration and damage the cell; ROS decreases cell energy by reducing the mitochondrial DNA and impairing oxidation. Excess production of ROS causes oxidative stress and disturbs the balance between oxidants and antioxidants, which leads to vascular dysfunction, decreased cardiac function, and impairment in cellular mitochondria (Lu et al. 2022). While there is no specific biomarker for the diagnosis of sepsis, various parameters, such as white blood cell count, procalcitonin, TNF-α, IL-6, CRP, BUN, creatinine, and serum lactate level, are evaluated for diagnosis (Lippi 2019). Although medical treatments have made significant progress, clinical sepsis treatment still primarily involves antibiotics and supportive therapies, and there is no specific treatment available (Lu et al. 2023). Several studies used several compounds to ameliorate inflammation and oxidative stress, but in the end the desired result for the treatment of this disease in humans was not achieved (Dolin et al. 2019). Recently, using Toll-like receptor antagonists have been investigated, but they were not successful (Opal et al. 2013).
Cecal ligation and puncture (CLP) is one of the best models for sepsis induction; it is repeatable and immediate. Also, it resembles poly-microbial sepsis which made this model a gold standard for induction sepsis in animal models (Su et al. 2023).
Dapsone, 4,4′diaminodiphenyl sulphone, was used to treat leprosy (Calderón-Estrella et al. 2023). It is also used to treat malaria, herpes dermatitis, and acne, and is available topically and orally; it has fast absorption and can pass the blood–brain barrier (Molinelli et al. 2019). The primary mechanism of dapsone is like sulfonamides inhibits the synthesis of dihydrofolic acid and competes with para-aminobenzoic acid to occupy the dihydropteroate’s active site and has bacteriostatic effects (Ghaoui et al. 2020). Additionally, dapsone has been found to reduce the release and signaling of IL-8 by inhibiting phosphorylation NF-κB P65 (Kanoh et al. 2011; Kast et al. 2012). This drug inhibits myeloperoxidase enzyme (MPO), preventing the production of the antioxidant HOCl3 by neutrophils (Yousefi-Manesh et al. 2022). Additionally, dapsone can reduce the production of superoxide anions. Several studies showed the antioxidant effects of dapsone on ROS produced by neutrophils (Suda et al. 2005). Dapsone downregulates or inhibits the production of TNF-α (Kwon and Joo 2018). Dapsone also reduces prostaglandin production by inhibiting the cyclooxygenase enzyme, contributing to its anti-inflammatory effect (Ruzicka et al. 1983). It is involved in inhibiting neutrophil adhesion to IgE. Several studies found that dapsone is an inhibitor of lipid peroxidation, NO production, and apoptosis (Diaz-Ruiz et al. 2008; Zhou et al. 2014). Recent studies showed the dapsone effect on suppressing the production of inflammatory cytokines, IL-6 and IL-1β, in vitro (Geyfman et al. 2019).
As dapsone showed anti-inflammatory, anti-bacterial, immunomodulatory, and antioxidant effects, the aim of this research was to assess the effectiveness of dapsone in the treatment of sepsis induced by CLP surgery in male mice.
Material and methods
Studied animals
One-hundred NMRI mice weighing 25–30 g were used in this study. Animals were obtained and kept in the Pharmacology Department’s animal house at Tehran University of Medical Sciences (Tehran, Iran). Before and after surgery, they were kept in a plastic cage with a 12/12-h-light/dark cycle, at 23 ± 2 °C (room temperature). Clean water and food were provided for the mice. Animals were generally anesthetized before performing surgery, and proper anesthesia procedures were ensured during the experimentally procedures; a lamp over the field was used to keep them warm during procedures; the artificial tear drops were used to cover their eyes. Each procedure and injection were performed far from the others’ sight to protect them against the stressful situation. The Ethics in Medical Research Committee of Tehran University of Medical Sciences approved this study with an ethical code (IR.TUMS.MEDICINE.REC.1399.106).
Chemicals and reagents
In this study, dapsone was purchased from Gilaranco Co. (Rasht, Iran). Dimethyl sulfoxide, and ketamine 10% were purchased from Merck Company (Darmstadt, Germany). Xylazine was purchased from Alfasan Co. (Woerden, the Netherlands). Dimethyl sulfoxide was used to dissolve dapsone in normal saline (0.9% NaCl) (with a total concentration of 3% [v/v]).
Sepsis induction
A cecal ligation and puncture (CLP) model was performed in this study for sepsis induction (Rittirsch et al. 2009). Animals were anesthetized by xylazine (15 mg/kg) and ketamine (75 mg/kg) intraperitoneal (i.p) injection. Then animals’ reflexes were checked for anesthesia assurance. After anesthesia and shaving the mice’s abdominal hair, the marked location was sterilized; a 1-cm gentle incision was made in the midline of the animal’s abdomen that cut skin first, then the peritoneum. Sutures entirely blocked the last 20% part of the cecum (nearly 1 cm). In the middle of the cecum’s blocked part, a 20 G needle was inserted through one side and exited from the other side without damaging the blood vessels. A mild pressure squeezed the perforation’s top to ensure that the feces came out; these feces induced a polymicrobial infection that led to sepsis. The incision was sutured using simple stitches with 4/0 reverse-cutting silk surgical sutures, and 0.5 cc normal saline was injected subcutaneously to prevent hypotension.
Study design
The animals were divided into five groups:
-
CLP group (sepsis): CLP surgery + normal saline i.p.
-
Sham group: surgical procedure without induction of sepsis, received DMSO, and normal saline i.p.
-
Treatment group 1: CLP + dapsone (0.5 mg/kg BW) i.p.
-
Treatment group 2: CLP + dapsone (1 mg/kg BW) i.p.
-
Treatment group 3: CLP + dapsone (2 mg/kg BW) i.p.
Based on previous studies and customized during the pre-test period, 0.5, 1, and 2 mg/kg of dapsone were injected intraperitoneally into animals in three different groups simultaneously with the completion of the surgery. After 24 h, half of mice in each group were anesthetized, and a blood sample was taken from the heart. Kidney tissue was then placed in 10% (w/v) formalin for pathological evaluation. Additionally, the remaining mice were observed for 96 h to evaluate the survival rate.
Sample collection and blood sampling
Twenty-four hours after performing surgery, a blood sample was taken after the animals were anesthetized by ketamine (75 mg/kg) and xylazine (15 mg/kg). The blood samples were centrifuged at 3000 rpm and serum was kept in a − 80 °C freezer for further assessments. For tissue sampling, animals’ kidneys were excised and washed with normal saline and stored in 10% formalin to be prepared for histopathological studies. In order to investigate the effects of dapsone on the survival of animals after 96 h, survival was observed and recorded in all groups. At the end of the study, for the animals in the survival group where blood sampling was not required, euthanasia was performed using carbon dioxide (CO2). After the administration of the anesthetic drugs mentioned above, the animals were placed in a CO2 chamber for 3 min.
Biomarker measurements
Mice-specific ELISA kits (DuoSet ELISA development system) were purchased from R&D Systems to assess the quantity of interleukin (IL) 1β, 6 and 10, tumor necrosis factor-α (TNF-α), as provided protocol. The optical density was set at 450 nm; the final concentration was adjusted and reported as pg/ml protein. The laboratory evaluated BUN, creatinine, nitric oxide (NO), myeloperoxidase enzyme (MPO), and lactate serum.
Histopathological studies
The fixation, dehydration, and clarification process for renal tissue samples is a standard procedure in histological analysis. The samples are placed in a 10% formalin solution for 24 h for fixation, followed by dehydration using increasing concentrations of ethanol and clarification with xylene. The tissue is dehydrated by gradually replacing the water content with a series of increasing concentrations of ethanol; tissue is clarified by infiltrating it with a clearing agent, xylene, which replaces the ethanol and renders the tissue transparent. After processing and embedding in paraffin, 5-µm-wide samples are stained with hematoxylin and eosin (H & E) for evaluation under × 400 magnification by a histologist. This method is well-established in histopathology and is essential for preserving, preparing, and evaluating tissue samples.
Statistical analysis
One-way ANOVA analysis followed by a Tukey post hoc test was used on GraphPad Prism (v6) to analyze the data and the differences between them. In this study, the significance level was p ≤ 0.05. After observing and recording the survival percentage, the graph was drawn, and the results were analyzed using the same software and method (Kaplan–Meier method and log-rank test).
Results
Assay for BUN, creatinine, and lactate
The mean BUN, creatinine, and lactate were 40.24 ± 0.95 mg/dl, 0.78 ± 0.16 mg/dl, and 5.37 ± 0.25 µg/ml in the CLP group, respectively. BUN serum levels had no significant difference between groups (p > 0.05). Creatinine and lactate levels were significantly lower in the 0.5 mg/kg dapsone group compared to CLP group (p < 0.05 and p < 0.001, respectively). other treatment groups did not show any significant decrease in BUN, creatinine, and lactate serum levels (Fig. 1).
Creatinine (A), lactate (B), and BUN (C) serum levels alterations. The CLP group received only normal saline + CLP; the sham group received dmso and normal saline; tree treatment group received CLP and dapsone at doses of 0.5, 1, and 2 mg/kg BW. *p-value < 0.05 compared with CLP group. **p-value < 0.01 compared with CLP group. ***p-value < 0.001 compared with CLP group
Elisa assay for IL-1β, IL-6, IL-10, and IL-6/IL-10 ratio
IL-1 β and IL-6, inflammatory cytokines, were significantly higher in the CLP group compared to sham (p < 0.01). Serum levels of IL-1β decreased significantly in 0.5 mg/kg and 2 mg/kg dapsone groups (p < 0.01 and p < 0.05, respectively). Serum levels of IL-10 were significantly decreased in CLP group, and 0.5 mg/kg of dapsone group increase IL-10 (p < 0.05). No significant differences were observed between the other groups.
IL-6/IL-10 ratio was assessed as an anti-inflammatory index. There was a significant increase in CLP group compared to sham; on the other hand, 0.5 mg/kg and 2 mg/kg dapsone groups had a significant decrease compared to the CLP group (p < 0.001, and p < 0.01, respectively) (Fig. 2).
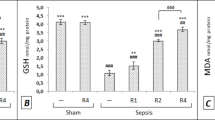
TNF-α, MPO, and NO serum levels alterations
MPO levels were significantly decreased in the 0.5 mg/kg group (p < 0.01). However, MPO levels had no significant differences in higher doses of dapsone, and TNF-α levels in all dapsone groups were significantly decreased (p < 0.01, p < 0.01, and p < 0.001, respectively). No alterations in nitric oxide serum levels resulted except in the 2 mg/kg dapsone group; significantly lower levels of NO were observed (p < 0.05) (Fig. 3).
The protective effect of dapsone on sepsis survival
The survival of all the treatment groups (with different doses of dapsone) was significantly higher than the CLP group in 96 h (p < 0.05). The 1 mg/kg dapsone group had significantly lower deaths of mice at the end of 4 days (p < 0.05) (Fig. 4).
Histopathological study
The cortex of glomeruli and base membrane of the glomerular cells were deprived in the CLP group, 0.5 mg/kg and 2 mg/kg dapsone groups. The bowman capsules were expanded because of the accumulation of the capsular and glomerular cells; some parts of the macula densa were not observed in those three mentioned groups. The afferent and efferent arterioles were dilated due to hemorrhage. The cells in proximal and distal tubules were in different stages of apoptosis. Also, a hemorrhage and cell apoptosis were observed in the medulla. These alterations were not observed in the 1 mg/kg dapsone group (Fig. 5).
Photomicrographs showed the effect of dapsone on the histological alternation of kidney: A CLP group received only normal saline after CLP surgery; B sham group received DMSO and normal saline; C received 0.5 mg/kg dapsone + CLP; D received 1 mg/kg dapsone + CLP; E received 2 mg/kg dapsone + CLP. Images are stained with H&E staining at a (mag: 400 ×)
Discussion
Sepsis and septic shock are caused by systemic symptoms caused by microbes entering the bloodstream, resulting in organ dysfunction; it is an important clinical disease with high mortality rates and substantial cost, which kills many people every year in the world (Ding et al. 2024). It imposes on the world’s health systems that, surprisingly, no definitive selective cure has been found for this disease so far, and an increase in statistics has accompanied it, and today many studies are trying to solve this problem (Xue et al. 2022). During this disease, we have destructive events include an increase in the production of inflammatory mediators such as interleukins, reactive oxygen species, nitric oxide, and oxidative stress (Gyawali et al. 2019).
Dapsone is a drug of sulfone groups that is structurally similar to sulfonamides, was first synthesized in 1908, and used in leprosy treatment in 1945. It has also been studied to show a wide range of anti-inflammatory, anti-oxidative stress, and anti-apoptotic effects (Molinelli et al. 2019). In the present study, the effects of dapsone on the inflammatory response and mortality of male mice in the animal model of sepsis (CLP) were investigated to determine whether dapsone can have a positive effect on survival rate, inflammatory response, antioxidant, and kidney organ protection and reduce the adverse effects of sepsis or not.
This study is the first to examine the effects of dapsone on sepsis animal model by CLP in mice. The incidence of sepsis was associated with increased levels of cytokines IL-1β, IL-6, TNF-α, lactate, nitric oxide, and myeloperoxidase in animals.
However, creatinine and lactate levels were lower in the 0.5 mg/kg dapsone group. Serum levels of IL-1β decreased in the 0.5 mg/kg and 2 mg/kg dapsone groups, and levels of IL-10 were higher in the 0.5 mg/kg dapsone group. TNF-α levels in the 0.5 mg/kg, 1 mg/kg, and 2 mg/kg dapsone groups were lower than in the CLP group. MPO levels were decreased in the 0.5 mg/kg group, NO levels were lower in the 2 mg/kg dapsone, and the survival time of the treated groups was higher than the CLP group.
Numerous studies on sepsis suggest that TNF-α plays an important role in promoting a destructive inflammatory response such as activation of the NF-κb pathway, MAPK, stimulation of the acute phase response in the liver, an increase in CRP levels, and apoptosis in sepsis patients (Hu et al. 2023; Lin et al. 2024; Wang et al. 2023). It seems that the control of sepsis in the future will mainly rely on modulating the immune system and reducing the harmful effects of cytokines, especially TNF-α. Geyfman et al. in 2019 demonstrated that dapsone reduced the production of inflammatory cytokines IL-1β, IL-6, and TNF-α (Geyfman et al. 2019) In this study, dapsone was able to reduce the mentioned factors. In another study in South Korea, Kwon et al. investigated the effects of this drug on bone marrow cells exposed to lipopolysaccharide. After testing, they found dapsone at a low concentration of 25 μg/ml significantly decreased TNF-α levels, like our study (Kwon and Joo 2018). Abe et al. studied the pharmacological mechanism of dapsone in lupus erythematosus, in which dapsone administration suppressed TNF-α expression and significantly reduced its production (Abe et al. 2008).
Several studies showed that the transcription factor, nuclear factor kappa B (NF-κb), can be induced and activated by various factors such as LPS, ROS, TNF-α, and even IL-1β. This led to an increase in inflammatory mediators’ transcription, production, and release (Mohammadi et al. 2024). Dapsone appears to have the mechanism of affecting and blocking the NF-κb pathway resulting from TNF-α reduction by dose-dependent reduction or suppression of its production at the mRNA level or reduction of ROS by reducing the intracellular and extracellular production of superoxide anion (Jafari et al. 2021). Furthermore, the ROS produced by neutrophils has been able to increase other inflammatory cytokines. On the other hand, laboratory observations indicate an increase in the biosynthesis of IL-1β and IL-6 as secondary mediators by TNF-α. This result is consistent with Geyfman et al. that when the anti-TNF-α antibody is injected into mice, the TNF-α and IL-1β cytokines have increased the IL-6, which in turn stimulates CRP production. CRP may act directly as a proinflammatory cytokine and stimulate phagocytic cells, which dapsone can prevent these factors’ development. (Cho et al. 2011; Suda et al. 2005).
Rashidian et al. investigated the dapsone effect on acetic acid-induced colitis; they observed that dapsone, similar to our study, reduced TNF-α and MPO enzyme levels in the mice (Rashidian et al. 2019).
In this study, dapsone reduced the level of proinflammatory cytokines and modulated and increased the level of cytokine IL-10, an anti-inflammatory cytokine.
Another study conducted to investigate the anti-inflammatory potential effect of dapsone in COVID-19 revealed that hypochlorous acid produced by this enzyme, a potent oxidant produced by neutrophils, plays a role in inflammatory conditions; it results from the reaction of chlorine and hydrogen peroxide by the enzyme myeloperoxidase, which is reduced by reversible inhibition of this enzyme by dapsone. This decrease might cause by the decrease in neutrophil migration and their adhesion to immunoglobulins, which was consistent with the results of new studies and this study (Al-Kuraishy et al. 2024).
In sepsis, oxidant molecules’ production increased more than active oxygen, nitric oxide, and hydrogen peroxide species. This production led to a hypometabolic state with a decrease and disruption of cellular respiration. The cells start the glycolysis pathway by breaking down glucose after mitochondrial dysfunction and cell hypoxia. At the end of this pathway, pyruvate produced by the enzyme lactate dehydrogenase is converted to lactate. The cell can use lactate until there is not enough oxygen because hypoxia induces the HIF-1α gene. This gene is a regulatory key to glycolysis and increases the expression of lactate dehydrogenase (Mantzarlis et al. 2017; Andaluz-Ojeda et al. 2012). Dapsone was able to significantly reduce serum lactate levels and reduce the destructive effects of this pathway in our study. A study of the effects of dapsone on pyruvate in the blood of patients with leprosy found that pyruvic acid levels were generally high in the disease, and it was significantly increased after administration of dapsone (Sinha et al. 1982).
Nevertheless, it is not clear whether this increase is due to a disruption of its natural breakdown path or increased production. In this study, it was observed that serum lactate levels decreased significantly after the administration of dapsone. This decrease could be due to the decrease of ROS and NO, according to previously published articles on the anti-inflammatory and antioxidant effects of dapsone, which can increase pyruvate production due to impairment of the pathway (Diaz-Ruiz et al. 2008; Zhou et al. 2014).
During sepsis, systemic inflammation causes nitric oxide production by the endothelial nitric oxide synthase (eNOS) and induced nitric oxide synthase (iNOS). The increase of NO production can cause vascular dysfunction and tissue damage. Several studies showed that LPS of microorganisms induces iNOS expression and increases NO production (Titheradge 1999). So, using NOS inhibitors improves hemodynamic variables and increases survival in different models. Nitric oxide appears to play an essential protective role through cellular immune function. Th1 cells produce NO in response to foreign antigens (Gallo et al. 2012). The study showed that dapsone significantly reduced this factor in the treatment group (the 2 mg/kg group).
BUN and creatinine are factors indicating the physiological role of the kidney. In this study, dapsone administration was not significantly reduced BUN levels. Because dapsone could significantly reduce lactate and creatinine, it seems that with a greater number of samples, BUN will have a significant decrease (Nezamoleslami et al. 2020).
Further evaluation of dapsone effects on other pathways such as NF-Kb and MAPK, and on the expression and pathway of TLR-4, also a further microscopic examination of other tissues such as the liver is suggested.
Conclusion
The present study results showed that administration of dapsone after inducing sepsis using the CLP method in male mice could increase survival and a significant reduction in destructive inflammatory factors. This suggests that dapsone can reduce the destructive effects of sepsis and help improve the body’s normal function and increase the chances of survival, which can be due to the antioxidant and anti-inflammatory activity of dapsone.
It is important to note that while this study provides promising results regarding the potential therapeutic effects of dapsone in sepsis animal models, further research is needed to fully understand its mechanisms of action and evaluate its safety and efficacy in clinical settings.
Data availability
No datasets were generated or analysed during the current study.
References
Abe M, Shimizu A, Yokoyama Y, Takeuchi Y, Ishikawa O (2008) A possible inhibitory action of diaminodiphenyl sulfone on tumour necrosis factor-α production from activated mononuclear cells on cutaneous lupus erythematosus. Clinical and Experimental Dermatology: Experimental Dermatology 33(6):759–763
Al-Kuraishy HM, Al-Gareeb AI, Elekhnawy E, Alexiou A, Batiha GES (2024) The potential effect of dapsone on the inflammatory reactions in COVID-19: staggering view. Comb Chem High Throughput Screen 27(5):674–678
Andaluz-Ojeda D, Bobillo F, Iglesias V, Almansa R, Rico L, Gandía F et al (2012) A combined score of pro-and anti-inflammatory interleukins improves mortality prediction in severe sepsis. Cytokine 57(3):332–336
Calderón-Estrella F, Franco-Bourland RE, Rios C, de Jesús-Nicolás D, Pineda B, Méndez-Armenta M et al (2023) Early treatment with dapsone after spinal cord injury in rats decreases the inflammatory response and promotes long-term functional recovery. Heliyon 9(4):e14687
Cho SC, Rhim JH, Choi HR, Son YH, Lee SJ, Song K-Y et al (2011) Protective effect of 4, 4′-diaminodiphenylsulfone against paraquat-induced mouse lung injury. Exp Mol Med 43(9):525–537
Diaz-Ruiz A, Zavala C, Montes S, Ortiz-Plata A, Salgado-Ceballos H, Orozco-Suarez S et al (2008) Antioxidant, antiinflammatory and antiapoptotic effects of dapsone in a model of brain ischemia/reperfusion in rats. J Neurosci Res 86(15):3410–3419
Ding X, Liang W, Xia H, Liu Y, Liu S, Xia X, Zhu X, Pei Y, Zhang D (2024) Analysis of immune and prognostic-related lncRNA PRKCQ-AS1 for predicting prognosis and regulating effect in sepsis. J Inflamm Res 17:279–299
Dolin HH, Papadimos TJ, Chen X, Pan ZK (2019) Characterization of pathogenic sepsis etiologies and patient profiles: a novel approach to triage and treatment. Microbiol Insights 12:1178636118825081
Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C et al (2021) Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Crit Care Med 49(11):e1063–e1143
Gallo E, Katzman S, Villarino AV (2012) IL-13-producing Th1 and Th17 cells characterize adaptive responses to both self and foreign antigens. Eur J Immunol 42(9):2322–2328
Geyfman M, Debabov D, Poloso N, Alvandi N (2019) Mechanistic insight into the activity of a sulfone compound dapsone on Propionibacterium (Newly Reclassified as Cutibacterium) Acnes-mediated cytokine production. Exp Dermatol 28(2):190–197
Ghaoui N, Hanna E, Abbas O, Kibbi AG, Kurban M (2020) Update on the use of dapsone in dermatology. Int J Dermatol 59(7):787–795
Gyawali B, Ramakrishna K, Dhamoon AS (2019) Sepsis: the evolution in definition, pathophysiology, and management. SAGE Open Medicine 7:2050312119835043
Hotchkiss RS, Moldawer LL, Opal SM, Reinhart K, Turnbull IR, Vincent J-L (2016) Sepsis and septic shock. Nat Rev Dis Primers 2(1):1–21
Hu B, Chen Z, Liang L, Zheng M, Chen X, Zeng Q (2023) Melatonin promotes mitochondrial biogenesis and mitochondrial degradation in hepatocytes during sepsis. Altern Ther Health Med 29:284–289
Jafari RM, Shayesteh S, Ala M, Yousefi-Manesh H, Rashidian A, Hashemian SM et al (2021) Dapsone ameliorates colitis through TLR4/NF-kB pathway in TNBS induced colitis model in rat. Arch Med Res 52(6):595–602
Jiang W, Song L, Zhang Y, Ba J, Yuan J, Li X, Liao T, Zhang C, Shao J, Yu J, Zheng R (2024) The influence of gender on the epidemiology of and outcome from sepsis associated acute kidney injury in ICU: a retrospective propensity-matched cohort study. Eur J Med Res 29(1):56
Joffre J, Hellman J, Ince C, Ait-Oufella H (2020) Endothelial responses in sepsis. Am J Respir Crit Care Med 202(3):361–370
Kanoh S, Tanabe T, Rubin BK (2011) Dapsone inhibits IL-8 secretion from human bronchial epithelial cells stimulated with lipopolysaccharide and resolves airway inflammation in the ferret. Chest 140(4):980–990
Kast RE, Lefranc F, Karpel-Massler G, Halatsch M-E (2012) Why dapsone stops seizures and may stop neutrophils’ delivery of VEGF to glioblastoma. Br J Neurosurg 26(6):813–817
Kwon MJ, Joo HG (2018) Dapsone modulates lipopolysaccharide-activated bone marrow cells by inducing cell death and down-regulating tumor necrosis factor-α production. J Vet Sci 19(6):744–749
Lin SP, Xu XJ, Liao C, Zhao N, Chen YY, Song H, Xu WQ, Liang J, Shen DY, Zhang JY, Shen HP, Zhao FY, Tang YM (2024) The predictive utility of cytokines, procalcitonin and C-reactive protein among febrile pediatric hematology and oncology patients with severe sepsis or septic shock. Pediatr Hematol Oncol 41(1):1–14
Lippi G (2019) Sepsis biomarkers: past, present and future. Clin Chem Lab Med 57(9):1281–1283
Lu J, Liu J, Li A (2022) Roles of neutrophil reactive oxygen species (ROS) generation in organ function impairment in sepsis. J Zhejiang University-SCIENCE b 23(6):437–450
Lu Y, Shi Y, Wu Q, Sun X, Zhang W-Z, Xu X-L, et al. (2023) An overview of drug delivery nanosystems for sepsis-related liver injury treatment. Int J Nanomed 765–79
Luangasanatip N, Hongsuwan M, Limmathurotsakul D, Lubell Y, Lee AS, Harbarth S, Day NP, Graves N, Cooper BS (2015) Comparative efficacy of interventions to promote hand hygiene in hospital: systematic review and network meta-analysis. BMJ 351:h3728
Ludwig KR, Hummon AB (2017) Mass spectrometry for the discovery of biomarkers of sepsis. Mol BioSyst 13(4):648–664
Mantzarlis K, Tsolaki V, Zakynthinos E (2017) Role of oxidative stress and mitochondrial dysfunction in sepsis and potential therapies. Oxid Med Cell Longev 2017(1):5985209
Marques A, Torre C, Pinto R, Sepodes B, Rocha J (2023) Treatment advances in sepsis and septic shock: modulating pro-and anti-inflammatory mechanisms. J Clin Med 12(8):2892
Mohammadi F, Rahimi K, Ahmadi A, Hooshmandi Z, Amini S, Mohammadi A (2024) Anti-inflammatory effects of Mentha pulegium L. extract on human peripheral blood mononuclear cells are mediated by TLR-4 and NF-κB suppression. Heliyon 10(1):e24040
Molinelli E, Paolinelli M, Campanati A, Brisigotti V, Offidani A (2019) Metabolic, pharmacokinetic, and toxicological issues surrounding dapsone. Expert Opin Drug Metab Toxicol 15(5):367–379
Morris DC, Zhang ZG, Jaehne AK, Zhang J, Rivers EP (2023) Clinical, molecular, and exosomal mechanisms of cardiac and brain dysfunction in sepsiS. Shock 59(2):173–179
Nezamoleslami S, Sheibani M, Jahanshahi F, Mumtaz F, Abbasi A, Dehpour AR (2020) Protective effect of dapsone against renal ischemia-reperfusion injury in rat. Immunopharmacol Immunotoxicol 42(3):272–279
Oliveira FRMB, Assreuy J, Sordi R (2022) The role of nitric oxide in sepsis-associated kidney injury. Bioscience reports 42(7):BSR20220093
Opal SM, Laterre P-F, Francois B, LaRosa SP, Angus DC, Mira J-P et al (2013) Effect of eritoran, an antagonist of MD2-TLR4, on mortality in patients with severe sepsis: the ACCESS randomized trial. JAMA 309(11):1154–1162
Rashidian A, Rashki A, Abdollahi A, Haddadi N-S, Chamanara M, Mumtaz F et al (2019) Dapsone reduced acetic acid-induced inflammatory response in rat colon tissue through inhibition of NF-kB signaling pathway. Immunopharmacol Immunotoxicol 41(6):607–613
Rittirsch D, Huber-Lang MS, Flierl MA, Ward PA (2009) Immunodesign of experimental sepsis by cecal ligation and puncture. Nat Protoc 4(1):31–36
Ruzicka T, Wasserman SI, Soter NA, Printz MP (1983) Inhibition of rat mast cell arachidonic acid cyclooxygenase by dapsone. J Allergy Clin Immunol 72(4):365–370
Sinha SN, Gupta SC, Bajaj AK, Srivastava NP, Mehrotra TN (1982) Effect of dapsone on blood lactic and pyruvic acids in leprosy. Int J Lepr Other Mycobact Dis 50(4):468–470
Su J, Chen S, Xiao J, Feng Z, Hu S, Su Q et al (2023) Aloe-emodin ameliorates cecal ligation and puncture-induced sepsis. Int J Mol Sci 24(15):11972
Suda T, Suzuki Y, Matsui T, Inoue T, Niide O, Yoshimaru T et al (2005) Dapsone suppresses human neutrophil superoxide production and elastase release in a calcium-dependent manner. Br J Dermatol 152(5):887–895
Titheradge MA (1999) Nitric oxide in septic shock. Biochimica et Biophysica Acta (BBA)-Bioenergetics 1411(2–3):437–55
van der Poll T, Shankar-Hari M, Wiersinga WJ (2021) The immunology of sepsis. Immunity 54(11):2450–2464
Wang Z, Guo Z, Wang X, Liao H, Chen F, Liu Y et al (2023) Reduning alleviates sepsis-induced acute lung injury by reducing apoptosis of pulmonary microvascular endothelial cells. Front Immunol 14:1196350
Wang R, Li Q, Wu P, Ren K, Li Y, Wang Y et al (2024) Fe-capsaicin nanozymes attenuate sepsis-induced acute lung injury via NF-κB signaling. Int J Nanomed 19:73
Xue W, Pang J, Liu J, Wang H, Guo H, Chen Y (2022) Septic cardiomyopathy: characteristics, evaluation, and mechanism. Emergency and Critical Care Medicine 2(3):135–147
Yousefi-Manesh H, Noori T, Asgardoon MH, Derakhshan MH, Tavangar SM, Sheibani M et al (2022) Protective effect of dapsone against bleomycin-induced lung fibrosis in rat. Exp Mol Pathol 124:104737
Zhou T, Zhao L, Zhan R, He Q, Tong Y, Tian X et al (2014) Blood-brain barrier dysfunction in mice induced by lipopolysaccharide is attenuated by dapsone. Biochem Biophys Res Commun 453(3):419–424
Author information
Authors and Affiliations
Contributions
Conceptualization, H.sh, Methodology, H.sh, A.d, M.sh.
Formal analysis and investigation: H.sh, A.d, M.sh, A.p, A.a.
Writing—original draft preparation: M.Sh and A.p. Writing—review and editing: M.sh, A.a, H.sh, A.p.
Funding acquisition and Supervision: [H.sh]. The published version of the manuscript has been read and approved by all authors. The authors declare that all data were generated in-house and that no paper mill was used.
Corresponding author
Ethics declarations
Ethics approval
The Ethics in Medical Research Committee of Tehran University of Medical Sciences approved this study with an ethical code (IR.TUMS.MEDICINE.REC.1399.106).
Consent to publish
It is not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sayyad, M.S., Dehpour, A., Poopak, A. et al. Investigating the efficacy of dapsone in treating sepsis induced by cecal ligation and puncture surgery in male mice. Naunyn-Schmiedeberg's Arch Pharmacol (2024). https://doi.org/10.1007/s00210-024-03251-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00210-024-03251-z