Abstract
Coronary artery diseases are principal sources of mortality and disability in global human population. Progressively, rivaroxaban is being evaluated for the prevention of atherosclerotic thrombi, particularly with anti-platelet agents. Hence, the current report aimed to investigate the cardioprotective effect of rivaroxaban on isoproterenol (ISO)-induced cardiac injury model in rats and the possible synergistic effect when combined with aspirin. Male Wistar rats were randomly assigned into five different groups. Cardiac injury was induced by subcutaneous injection of ISO (85 mg/kg) for 2 consecutive days. Rat tail bleeding time was performed prior to sacrifice. Cardiac enzymes, platelet activity, inflammatory, and oxidative stress biomarkers levels were measured using enzyme-linked immunoassay (ELISA). Pre-administration of rivaroxaban alone and on combination with aspirin prevented ISO-induced increase in cardiac thiobarbituric acid reactive substances (TBARS), interleukin 6 (IL-6), and thromboxane B2 (TXB2) levels. Moreover, a significant prolongation of bleeding time was demonstrated among aspirin, rivaroxaban, and aspirin plus rivaroxaban treated groups. On the other hand, the combination treatment of aspirin plus rivaroxaban showed no marked difference in these biomarkers and bleeding time relative to either drug administered separately. However, a prominent decrease of cardiac 6-keto prostaglandin F1α (6-Keto-PGF1α) level was displayed in the combination treatment when compared with ISO and rivaroxaban-treated groups, whereas no significant improvement was seen in cardiac glycoprotein V (GPV) levels except in aspirin-treated group. The study results demonstrated that rivaroxaban decreases cardiac oxidative stress, inflammation, and platelets reactivity. However, the addition of rivaroxaban to aspirin did not seem to show synergistic antioxidant, anti-inflammatory, or antiplatelet effect.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite the ongoing movement in the prevention and treatment of cardiovascular diseases (CVDs), CVDs are still considered the foremost prevalent sources of mortality and disability for most racial and ethnic groups (Roth et al. 2018; Kyu et al. 2018). In 2017, CVDs have accounted for 17.8 million deaths (Jagannathan et al. 2019) and still expanding to extend more than 23.6 million deaths by the year 2030 (Benjamin et al. 2018). Atherosclerosis is considered the pathological foundation of CVDs, most importantly coronary artery disease (Soehnlein and Libby 2021). As a part of entangled chronic inflammatory process, early atherosclerotic plaque is shaped by the buildup of circulating low density lipoproteins (LDL) and inflammatory components in the tunica intima of the coronary arteries walls (Kobiyama and Ley 2018). The deposited LDL is oxidized under the influence of oxidative stress which is generated by various pathological risk factors, resulting in the expression of multiple adhesion molecules (Badimon et al. 2012). Undoubtedly, an interplay of oxidative stress, inflammation, and immune response are all joined for the growth of atherosclerotic lesion (Wolf and Ley 2019; Bakogiannis et al. 2019; Fuentes et al. 2019). Gradually, smooth muscle cells proliferate and migrate to tunica intima, contributing in the formation of a fibrous cap coating the atherosclerotic plaque (Milutinović et al. 2020). Over time, a progressive thinning of the fibrous cap is mediated by releasing photolytic proteins such as matrix metalloproteinases (MMPs) and plasminogen activators (Bentzon et al. 2014). Once the mature atherosclerotic lesion ruptures, subendothelial collagen fibrils leach and disclose to the circulating platelets mediating their adherence to the injured endothelium through platelet membrane receptors glycoprotein (GP)IIb/IIIa and GPIb-V-IX (Lordan et al. 2021). Platelet activation fosters the emission of platelet-derived vasoactive substances, including thromboxane A2 (TXA2) and adenosine diphosphate (ADP), to potentiate ambient platelets activation and vasoconstriction (Alyavi et al. 2021). Concurrently, coagulation pathway is activated, and thrombin burst is generated attributing in the forming of fibrin-stabilized clot occluding the coronary artery and depriving the cardiac tissues from oxygen (Badimon and Vilahur 2014). During ischemic/reperfusion injury in myocardial infarction, cardiac oxygen starvation triggers a dynamic orchestrated process, which involves the recruitment of innate and adaptive inflammatory response (Abbate et al. 2020), generation of reactive oxygen species, and suppression of scavenging system (Carretero et al. 2020; Shahzad et al. 2018).
Isoproterenol (ISO) is a synthetic catecholamine that belongs to the pharmacological family of nonselective β-adrenergic receptor agonist (Allawadhi et al. 2018; Barisione et al. 2010). ISO has been considered a widely utilized compound in experimental animal models inducing a spectrum of cardiac abnormalities (Zhang et al. 2008; Grant et al. 2020). Studies showed that over-activation of β-adrenergic receptors mediates cardiac oxidative stress generation, pro-inflammatory cytokine release, signaling cascades alterations, and thrombi formation (Garlie et al. 2011; Corbi et al. 2013; Xiao et al. 2018). Clearly, the experimental approach of applying the ISO model mimics the same array of structural and functional pathological composites in myocardial infarction (MI), making it a successful approach for the embodiment of MI in rats (Dhalla et al. 2010). Indeed, employing ISO at supramaximal doses has been associated with mitochondrial dysfunction, producing cytotoxic free radicals, suppressing levels of antioxidant enzymes, promoting lipid peroxidation, and triggering inflammation (Rathore et al. 1998; Mukherjee et al. 2015; Forte et al. 2021).
Up to the present time, prevention and treatment of atherosclerotic thrombosis have been concentrating on targeting platelets as being the prevailing element in arterial thrombi (Montalescot et al. 2013). Aspirin has been used as a primary and secondary prevention of atherosclerotic diseases by halting the conversion of arachidonic acid to eicosanoids (prostaglandin E2, TXA2, and prostacyclin), thus promoting long-term antiplatelet effect (Tarantino et al. 2016). However, aspirin therapy is circumscribed by its side effects such gastrointestinal bleeding (Barbarawi et al. 2019) and the conflicting data regarding efficacy and safety, more specifically in elderly cohorts (Ujjawal et al. 2021). In addition, recent research is emphasizing poor response to aspirin, especially among diabetes mellitus patients (Santilli et al. 2015). However, recent evidence suggests more cumulative role of coagulation proteins early in atherosclerotic events (Rocha et al. 2021). Studies showed an evidence of coagulation component in early stable atherosclerotic lesions compared to advanced ones, suggesting an underlying process for exerting plaque thrombogenicity (Borissoff et al. 2010, 2009; Spronk et al. 2004). Moreover, factor Xa has been shown to be incorporated in inflammation, tissue fibrosis, vascular remodeling, and atherosclerotic plaque progression (Busch et al. 2005; Spronk et al. 2014; Tantry et al. 2020). Therefore, the rational of using anticoagulant; that targets factor Xa, as a preventive component in atherosclerotic events, is sensible.
Rivaroxaban is the first developed member of the novel direct factor Xa inhibitors with immense potency and selectivity (Perzborn et al. 2011). The drug discovery has been revolutionary in the area of oral anticoagulation after decades of vitamin K antagonists (VKAs) occupying the foreground (Sindet-Pedersen et al. 2017). Unlike VKAs, rivaroxaban shows comparable efficacy and superior safety with predictable pharmacokinetic and pharmacodynamic profile, hence allowing fixed daily dosing with halting the need for periodic monitoring (Sindet-Pedersen et al. 2017; Tellor et al. 2015). Interestingly, rivaroxaban has been described for possessing a pleiotropic effect that is very similar to that of statins (Posma and Sluimer 2021). Recently, studies showed that rivaroxaban’s activity is not only confined in coagulation pathway, but also in inflammation, oxidative stress, and platelet activation (Liu et al. 2019; Graff et al. 2007; Özbudak et al. 2019). As with inflammation, an animal study showed that rivaroxaban succeeded in reversing the antioxidant activity of cardiac glutathione and glutathione reductase in sunitinib-induced cardiotoxicity model (Imam et al. 2020). On the other hand, an in vitro study conducted in 2016 showed that rivaroxaban displayed an inhibitory effect on TF derived platelet activation (Wan et al. 2016). Importantly, recent evidence showed that rivaroxaban could have a possible synergistic effect when combined with antiplatelet agents (Coppens et al. 2019). Indeed, an in vitro study that investigated rivaroxaban effect on platelet activation alone or with ticagrelor demonstrated that the combination therapy resulted in a synergistic increase in the inhibitory effect on platelet aggregation (Perzborn et al. 2015). The COMPASS trial, which is a large multicenter randomized clinical trial, showed that the addition of innovative reduced dose or rivaroxaban (2.5 mg twice daily) to aspirin (100 mg once daily) as a dual pathway therapy in patients with chronic vascular disease has been associated with lower cardiovascular events and a lower mortality when compared with either drugs alone (rivaroxaban 5 mg twice daily; aspirin 100 mg once daily) (Eikelboom et al. 2017). However, the underlying mechanisms of the latter benefit have not been clearly demonstrated in the literature. Hence, the present study aimed to evaluate the protective effect of rivaroxaban in ISO-induced cardiac injury and to investigate its possible synergistic effect when co-administered with aspirin.
Materials and methods
Chemicals and reagents
Rivaroxaban was purchased from Megafine Pharma (P) Ltd. Company® (Lot No. RB1907004) (Maharashi Karve Road, Marine Lines, Mumbai-400002, Maharashtra, India). Isoproterenol hydrochloride (N-isopropyl-L-noradrenaline hydrochloride) was purchased from Sigma-Aldrich Company® (Lot No. BCBW7995) (St. Louis, MO, USA). Aspirin was obtained from the River Jordan Pharmaceutical company quality control department (ID NO.WS/21/019/01). The cell culture reagent, dimethyl sulfoxide (DMSO) ChemCruz®, was purchased from Santa Cruz Biotechnology® (Lot No. A2418) (Santa Cruz, CA, USA). Deionized water was obtained from Jordan University of Science and Technology (JUST, Irbid, Jordan) laboratories.
All treatment agents were weighted, freshly prepared, and administered instantly based on body weight. Aspirin and rivaroxaban treatment solutions were prepared by dissolving each in DMSO to produce solutions with a concentration of 13 mg/ml and 6.7 mg/ml, respectively (Maity et al. 2015; Gosselin et al. 2016). ISO treatment solution was prepared by dissolving ISO powder in deionized water to yield a solution with a concentration of 30 mg/ml ready for use (Rababa’h and Alzoubi 2021).
Experimental animals
Adult male Wistar rats (215–285 g), aged 10–12 weeks, were maintained in steel cages (10 rats/cage) under controlled room temperature (24 ± 1 °C) with 50 ± 5% relative humidity and 12:12 h light–dark cycle. Rats were allowed free access for standard rodent chow diet and tap water available ad libitum. All animals were kept for 10 days acclimation before manipulation, which took a place in the animal house at Jordan University of Science and Technology (JUST). Body weights for all rats were obtained initially, prior to treatment phase and prior to cardiac injury induction phase. All experimental procedures were performed in congruency with the regulations of the Animal Care and Use Committee (ACUC; ACUC approval No. 412–2021) at JUST and in accordance with the concepts of laboratory animal care and use as involved in the European Community guidelines.
Animal groups, treatment, and induction phases
Following acclimation (day 11), rats were randomly assigned into 5 different groups (n = 15 rats per group) based on the received treatment as follows: groups 1 and 2 received no treatment (only DMSO), whereas groups 3–5 received treatment with either aspirin alone (10 mg/kg/day; group 3), rivaroxaban alone (5 mg/kg/day; group 4), or as a combination (group 5) via oral gavage daily for 7 days. Both doses and duration of treatments were based on previous literature (Jia et al. 2018; Jiang et al. 2020; Daci et al. 2020; Kono et al. 2014). Table 1 summarizes different treatment groups.
Following treatment phase (on day 18), groups 2–5 were induced with cardiac injury by subcutaneously injecting rats with ISO preparation every 24 h for 2 subsequent days (days 18 and 19). ISO was administered at a dose of 85 mg/kg/day via subcutaneous injection (Rababa’h and Alzoubi 2021; Verma et al. 2019). Treatment preparations pertaining for each group were also administered during cardiac injury induction phase 1.5 h prior to ISO administration. Fig. 1 represents an illustration of the experiment timeframe.
Illustration of the experiment timeline. Following 10 days acclimation, administration of rivaroxaban alone and in combination with aspirin was initiated daily for 7 days via oral gavage. Starting from day 18, animals were subcutaneously injected with ISO daily for 2 days along with treatment administration to induce cardiac injury. Animals were decapitated on day 19. Group 2, isoproterenol-treated group; group 3, aspirin-treated group; group 4, rivaroxaban-treated group; group 5, rivaroxaban-aspirin-treated group; ISO, isoproterenol
Bleeding time procedure
Bleeding time was conducted using tail transection model with minor modifications (Dejana et al. 1979; Ambler et al. 1985; Song et al. 2012). Bleeding time procedure was performed on the second day of ISO induction prior to rat sacrifice. The non-anesthetized rats were trapped using restraints and placed horizontally over disposable incontinence surgical under-pad. Subsequently, a distal 2-mm segment of the tail tip was totally transected using a disposable surgical blade. The tail was immediately immersed in a 15-ml plastic tube containing a pre-warmed isotonic saline (37 °C). The tail tip was positioned vertically 2 mm below the body horizon. Using a stopwatch, bleeding time was tracked for each animal for a maximum cut-off time of 20 min. The time needed to reach a 30-s period of bleeding cessation is then defined. When bleeding time extended for more than the intended cut-off time, tracking was stopped, and bleeding time was documented as 20 min for statistical analysis. Bleeding time prolongation for 50 percent or more compared to the control group was considered significant.
Blood collection, heart dissection, and tissue homogenization
Once treatment and induction phases terminated, animals were sacrificed by cervical decapitation using rodent’s guillotine. Fresh blood for each animal was promptly withdrawn into micronized silica coated yellow topped clot activator tubes. All blood samples were centrifuged at 4500 rpm for 15 min. Serum samples were eluted and collected into pre-labeled Eppendorf tubes. Serum was subsequently stored at − 80 °C to be utilized in the biochemical analysis. Hearts were promptly excised, rinsed with ice-cold Dulbecco’s phosphate-buffered saline (PBS), dried, and weighted. Then, hearts were cut into equal halves, tightly wrapped with aluminum foil, and cryopreserved in liquid nitrogen before transferring for storage at − 80 °C until tissue homogenization.
For heart tissue homogenization, protease inhibitor cocktail solution was prepared by completely dissolving one tablet of SIGMAFAST™ protease inhibitor (Sigma Aldrich Corp, MI, USA) in 100 ml cold iced PBS (− 8 °C). In a 10-ml tube, two milliliters of the cocktail preparation were added to each halved rat heart and homogenized until completely soluble using handheld tissue homogenizer. Immediately, homogenates were incubated in ice for 15 min, followed by cold centrifugation (− 4 °C) at 16,000 rpm for another 15 min. The resultant homogenates were divided into several aliquots and were subsequently stored at − 80 °C.
Biochemical analysis
Serum levels of aspartate aminotransferase (AST) and alanine aminotransferase (ALT) were quantitatively determined with kinetic ultraviolet (UV) test using the DXC 700 Beckman Coulter AU analyzer. Heart homogenates levels of creatine kinase (CK) and serum levels of lactate dehydrogenase (LDH) were quantitatively determined with UV test using the Roche/Hitachi Cobas® c303 analyzer.
Enzyme-linked immunoassays were utilized to quantitatively measure heart tissue homogenates levels of inflammatory biomarkers including tumor necrosis alpha (TNF-α; cat No. ab236712, Abcam Company, Cambridge, UK) and interleukin-6 (IL-6; cat No. BMS625, Thermo Fisher Scientific, MA, USA), oxidative stress biomarkers including nitric oxide (NO; cat No. ab272517, Abcam Company, Cambridge, UK), superoxide dismutase (SOD; cat No. MBS2707324, MyBioSource Inc., San Diego, USA), and thiobarbituric acid-reactive substances (TBARS; cat No. MBS1600368, MyBioSource Inc., San Diego, USA) and platelet reactivity biomarkers including thromboxane B2 (TXB2; cat No. MBS2601763, MyBioSource Inc., San Diego, USA), 6-Keto-prostaglandin F1 alpha (6-Keto-PGF1α; cat No. MBS705437, MyBioSource Inc., San Diego, USA), and glycoprotein V (GPV; cat No. MBS2505264, MyBioSource Inc., San Diego, USA).
Statistical analysis
All data were analyzed using GraphPad Prism (7.0) “GraphPad Software, La Jolla California USA, www.graphpad.com.” Results were expressed as mean ± SD. Data analysis was performed using one way ANOVA test. Tukey’s multiple comparisons test was used as a post hoc analysis for all the comparisons. For all statistical analysis, P value of < 0.05 was considered to test statistical significance.
Results
Heart weight to body weight and bleeding time
Figure 2A represents heart weight to body weight (Hwt/Bwt) ratios of all experimental groups. Relative to control group, Hwt/Bwt ratio in ISO-treated group was significantly elevated (P value < 0.0001). However, pre-administration of rivaroxaban and the combination of rivaroxaban and aspirin were associated with non-significant increment in Hwt/Bwt ratios compared to control. Moreover, Fig. 2B demonstrates bleeding time for each studied group. Relative to control and ISO groups, bleeding time of aspirin, rivaroxaban, and aspirin + rivaroxaban groups were significantly prolonged (P value < 0.0001).
Heart weight to body weight ratio (A) and bleeding time (B) among different study groups. ISO, isoproterenol; ASA, aspirin; Riva, rivaroxaban; Hwt/Bwt, heart weight to body weight ratio. Each point represents the mean ± SD. One-way ANOVA followed by Tukey’s multiple comparisons test was used. *Significant difference from the control group. Level of significance was detected when P < 0.05
Cardiac enzymes, aspartate transaminase, and alanine transaminase levels
Administration of ISO was associated with significant increase in AST, LDH, and CK levels compared to the control group (P value < 0.05; Table 2). Interestingly, groups treated with aspirin, rivaroxaban and their combination were associated with significant increase in the levels of AST and ALT enzymes compared to the control group. Contradictorily, pre-administration of aspirin was associated with significant reduction in LDH enzymes compared with ISO-treated group (aspirin 4606 ± 526.9 U/L vs. ISO 6534 ± 1398 U/L; P value < 0.0001), Moreover, a pre-administration of aspirin or rivaroxaban was associated with marked protective effect against ISO-induced elevation of CK enzyme levels (Table 2).
Cardiac oxidative stress biomarkers
Oxidative stress biomarkers including SOD, TBARS, and NO were measured and evaluated at the end of the study in rat’s heart homogenates (Fig. 3). A significant decrease in the SOD enzyme levels was induced by ISO administration. Among experimental groups, aspirin-treated group was the sole treatment group that showed a marked increase in the SOD enzyme levels compared with ISO-treated group (0.3169 ± 0.063 and 0.2158 ± 0.042 ng/ml/mg protein, respectively; P value = 0.0159).
Levels of oxidative stress biomarkers among the study groups. A Superoxide dismutase, B thiobarbituric acid reactive substances, and C nitric oxide levels at the end of the study. Each point is the mean ± SD. SOD, superoxide dismutase; TBARS, thiobarbituric acid-reactive substances. One-way ANOVA followed by Tukey’s multiple comparisons test. Level of significance was detected when P value < 0.05
ISO-treated group demonstrated a significant elevation in the TBARS levels compared to control group (0.1429 ± 0.092 and 0.071 ± 0.017 nmole/ml/mg protein, respectively; P value = 0.02). Interestingly, TBARS levels were significantly decreased in all treatment groups when compared with ISO-treated group. Remarkably, only aspirin administration caused significant elevation of NO compared with the ISO-treated group (0.089 ± 0.036 and 0.052 ± 0.012 µml/mg protein, respectively; P value = 0.0165) and rivaroxaban-treated group (0.050 ± 0.013 µml/mg protein; P value = 0.016). Notably, NO levels were comparable between ISO-treated group and the combination therapy of aspirin and rivaroxaban,and were unremarkably blunted in the combination therapy when compared with aspirin-treated group.
Cardiac inflammatory biomarkers
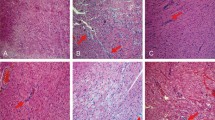
Heart tissue homogenates were used to evaluate the inflammatory biomarkers including TNF-α and IL-6 (Fig. 4). Compared with control group, ISO-treated group was associated with significant increase in the serum TNF-α and non-significant increase in IL-6 levels. However, a remarkable decrease in the IL-6 was associated with the administration of aspirin alone (P value = 0.009), rivaroxaban alone (P value < 0.0001), and their combination (P value < 0.0001) when compared with ISO-treated group. In addition, both rivaroxaban-treated and rivaroxaban-aspirin-treated groups were able to normalize IL-6 levels significantly when compared with the control group. However, all three treatment groups did not significantly prevent the elevation of TNF-α levels induced by ISO administration.
Inflammatory biomarkers among the study groups. A Interleukin-6 and B tumor necrosis factor alpha levels at the end of the study. Each point is the mean ± SD. IL-6, interleukin 6; TNF-α, tumor necrosis factor alpha. One-way ANOVA followed by Tukey’s multiple comparisons test. Level of significance was detected when P value < 0.05
Platelet and coagulation biomarker levels
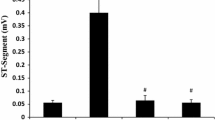
No marked increase in the 6-Keto-PGF1α levels was associated with ISO induction when compared with the control group. A significant decrease in 6-Keto-PGF1α levels was found in aspirin-rivaroxaban group when compared with rivaroxaban-only treated group (P = 0.00165), ISO-treated group (P value < 0.0001), and control group (P = 0.0102). ISO-treated group demonstrated a significant decrease in GPV levels compared to the control group (P = 0.0001). Interestingly, only aspirin group was associated with marked increase in the GPV levels when compared with ISO group (P = 0.0035) and rivaroxaban group (P = 0.0035). Additionally, a significant decrease in GPV levels was shown in rivaroxaban (P < 0.0001) and rivaroxaban-aspirin treated groups (P = 0.0063) when compared with control. Rebelliously, no marked effect was seen for rivaroxaban and the combination therapy groups when compared with ISO group. Instead, ISO induction produced insignificant elevation in TXB2 when compared to the control. On the other hand, a significant decrease in TXB2 levels was witnessed in all treatment groups: aspirin (P = 0.002), rivaroxaban (P = 0.043), and rivaroxaban plus aspirin (P = 0.006). Interestingly, D2D levels showed non-significant difference among all experimental groups (Fig. 5).
Platelets and coagulation biomarkers among the study groups. A 6-Keto-prostaglandin F1 alpha, B glycoprotein V, C thromboxane B2, and D D-dimer levels at the end of the study. Each point is the mean ± SD. 6-Keto, 6-Keto-prostaglandin F1 alpha; GPV, glycoprotein V; ISO, isoproterenol; ASA, aspirin; Riva, rivaroxaban. One-way ANOVA followed by Tukey’s multiple comparisons test. Level of significance was detected when P < 0.05
Discussion
In the current study, we aimed to investigate the impact of rivaroxaban solely and as a dual therapy with aspirin in ISO-induced cardiac injury animal model. ISO has been frequently utilized for the embodiment of cardiac injuries in rats (Song et al. 2020). The synthetic compound produces infarct-like detriments in the most vulnerable regions of the heart (Sagor et al. 2015). ISO induces cardiac injury by commencing a spectrum of complex biochemical alterations including triggering oxidative stress, platelet aggregation, and infiltration of inflammatory cells, as well as a spectrum of structural damage including changes in membrane permeability and cardiac hypertrophy (Raish et al. 2019; Wong et al. 2017). In the current study, subcutaneous injections of ISO, at a supratherapeutic dose, had successfully induced structural alterations by the significant increase of Hwt/Bwt ratio in ISO-treated group relative to control group. This goes in line with many experimental studies which demonstrated increase in the heart weight in ISO-treated model which is considered a landmark for ISO-induced cardiotoxicity (Jain et al. 2018; Lim et al. 2013). For the most part, this is attributed to the increment in the intravascular edematous space and the elevation of water and protein constitute (Hussain Shaik et al. 2012). However, pre-administration of rivaroxaban, solely or as a dual therapy with aspirin, did not manage to maintain heart weights at normal levels. Moreover, current observation showed significant prolongation of bleeding time in rivaroxaban-treated group compared with ISO-treated group. In addition, the present study showed significant prolongation in bleeding time for the combination therapy of aspirin with rivaroxaban when compared to ISO-treated group, but with no synergism when compared with the latter treatments solely.
Alterations in cytosolic cardiac enzymes such as LDH and total CK and elevation in AST levels are contemplated as an index to appraise the severity of necrotic injury to the myocardium (Bodor 2016). Elevated cardiac enzymes in the present study are consistent with previous experimental evidence, in which rats administered with ISO experienced a pronounced elevation in cardiac enzymes levels (Lalitha et al. 2013; Liu et al. 2018). Surprisingly, pretreatment of animals with rivaroxaban alone or in combination with aspirin have failed to normalize AST level and even produced higher levels than in the ISO-treated group. On the other hand, a decrease in total CK and LDH levels were evident after pre-treatment of rivaroxaban. This can be related to the non-cardiac nature of these enzymes (Bodor 2016), in addition to the fact that both aspirin and rivaroxaban are liver metabolized and can provoke liver enzymes alterations (Licata et al. 2018; Rafeeq et al. 2016). Thereby, conducting future experimental studies investigating more selective cardiac biomarkers is beneficial.
An oxidative stress-based pathway is considered one of the shared mechanisms in MI pathogenesis (Kurian et al. 2016). As a result of oxidative stress, distorted lipid metabolism is considered a leading inducer of a range of pathological alterations relevant to atherogenesis (Swapna et al. 2019). Lipid peroxides with their highly reactive and cytotoxic characteristics are involved in endothelial activation, platelet aggregation, and disruption of cell membrane permeability causing cardiac insult (Swapna et al. 2019; Park et al. 2015). Previous research pointed out that ISO administration was associated with impaired lipid metabolism (Sangeethadevi et al. 2021). In the current study, this was demonstrated as pretreatment with ISO was associated with significant elevation in TBARS. TBARS is considered a reliable estimator of lipid peroxidation, and its elevated level is extrapolated to indicate severe oxidative stress (Dayana and Manasa 2019). Among the suggestive mechanisms for ISO is the involvement in free radicals-mediated process. Clearly, ISO exhibits auto-oxidation which yields highly reactive quinines free radicals (Pullaiah et al. 2021). The resultant free radicals are involved in the peroxidation of membrane phospholipids, thus threatening the integrity of myocardial membranes, altering their permeability and eventually causing permanent damage (Sagor et al. 2015). It is generally perceived that a scavenging system involving endogenous antioxidant enzymes such as SOD, catalase, and glutathione peroxidase are incorporated in neutralizing free radicals formation and mitigating several pathologies (Rababa’h et al. 2018). However, overproduction of free radicals at the site of injury attenuates the activity of antioxidant enzymes (Hussein 2015). The data obtained from the current study was consistent with previous evidence as it shows marked reduced levels of SOD after treatment with ISO (Shackebaei et al. 2022; Xie et al. 2020). In the current data, rivaroxaban displayed antioxidant effect by improving SOD activity and significantly reducing TBARS levels. An animal study of experimental colitis was consistent with the current study findings as rivaroxaban managed to decrease accumulation of lipid peroxidation and restored SOD activity (Utku et al. 2015). However, one study showed that rivaroxaban antioxidant effect could be dose-dependent and was only seen at high doses (Samiei et al. 2019).
Moreover, in the present study, we investigated the level of cardiac NO. Our data shows that induction with ISO treatment was associated with insignificantly reduced levels of NO. Previously, Zhou and colleagues reported a decreased level of NO after the induction with ISO treatment (Zhou et al. 2017). Another experimental study of ISO-induced heart failure showed that ISO was associated with significant decrease in cardiac NO (Moursi et al. 2019). Data from the present study showed similar values of NO levels in animal groups treated with rivaroxaban solely or as a combination. This goes in line with an animal study of ischemia–reperfusion model, in which pre-treatment with rivaroxaban or clopidogrel was found to be associated with significant decrease in NO levels (Özbudak et al. 2019), but contradictory to another experimental study that proposed a NO-mediated vasorelaxant effect of direct oral anticoagulants (Mabley et al. 2019). In particular, the current data demonstrates a repressing effect of rivaroxaban on the NO-mediated action of aspirin when utilized in combination showed by lower NO levels in the combination therapy compared to aspirin therapy. Interestingly, rivaroxaban decreased levels of NO was speculated in a previous study as being an underlying mechanism of action for rivaroxaban to exert its antioxidant effect by increased usage of antioxidants including NO (Özbudak et al. 2019). However, conducting more research is in need to investigate the effect of rivaroxaban in NO signaling pathway as a dual therapy with aspirin.
Another mechanism involved in ISO-induced cardiac injury is the exacerbation of cardiac inflammatory process. Previous evidence addressed the crosstalk between cardiac injury induced by ISO in relation to the expression of inflammatory cytokines and MMPs (Viswanadha et al. 2020). One experimental study showed that isoproterenol-induced β-adrenergic receptors overstimulation contributes in MMP-13 mediated transactivation of PAR-1 in both cardiomyocytes and cardiac fibroblasts, which suggests a non-ischemic pathway for the activation of PAR-1, yielding in cardiac remodeling and inflammation as a pathological consequence (Jaffré et al. 2012). The current findings were consistent with previous results as ISO administration resulted in the elevation of TNF-α levels. Undoubtedly, the relationship between inflammation and coagulation has been well described in the literature. Indeed, previous evidence suggests the incorporation of both factor Xa and thrombin in inflammatory processes (Katoh et al. 2017). Interestingly, thrombin has been described as an inducer of platelet aggregation and thromboxane synthesis by multiple thrombin-platelet interactions. Previous evidence showed that thrombin activates platelets by cleaving PAR-1 and PAR-4 (Jennings 2009). TXB2 is considered a stable inactive predominant arachidonic acid derivative of human platelet cyclooxygenase (COX) 1 pathway. Assessment of TXB2 is considered an index of platelet COX-1 activity (Patrono and Rocca 2019). Furthermore, thromboxane plays a substantial role in MI, in which it elicits platelet aggregation, inflammation, blood vessel constriction, and coronary spasticity (Szczuko et al. 2021). On the other hand, 6-Keto-PGF1α is a stable metabolite of prostacyclin, which is another arachidonic acid derivative that is involved in preventing platelet aggregation and pertaining vasodilatory effect (Harding and Murray 2011). In the current study, a significant decrease in TXB2 was shown upon the administration of aspirin alone, rivaroxaban alone, and in combination. However, no superiority of rivaroxaban alone or as in combination with aspirin was evidenced when compared with aspirin only-treated group. Thus, findings in current study may suggest a comparable decrease in the platelet COX enzymes activity and platelet reactivity between aspirin and rivaroxaban with no additive influence of the combination therapy on COX enzyme activity. Moreover, the current study showed significant decrease in TXB2 in rivaroxaban-treated group when compared to ISO-treated group. This was inconsistent with a report suggesting in vivo increase in platelet reactivity by elevated production and release of TXA2 in patients receiving rivaroxaban and extrapolated a justification for the superiority of rivaroxaban in combination with aspirin based on the findings (Murphy et al. 2019). However, the latter study involved a very small sample size; thus, further research is warranted. In addition, the present data manifest a significant decrease of 6-Keto-PGF1α level by the combination of aspirin and rivaroxaban when compared with ISO-treated and rivaroxaban-treated groups. This may suggest that the reduction in the prostacyclin metabolite level is more likely influenced by aspirin inhibition of prostacyclin synthesis. Many studies supported the hypothesis of rivaroxaban working synergistically with antiplatelet therapy (Capodanno et al. 2018; Cammisotto et al. 2019), and others stood against it (Eller et al. 2014). Future studies investigating a potential antiplatelet effect of rivaroxaban synergistically with aspirin are warranted to explore the underlying mechanism.
Importantly, this is the first study to quantitatively report GPV levels using ISO-induced cardiotoxicity model. Previous studies showed that GPIb-V-IX complex has binding sites for both thrombin and von Willebrand factor and functions in establishing platelet adhesion to the vascular endothelium (Nieswandt and Watson 2003). While GPIb-IX acts as a receptor for thrombin, GPV acts as a safety lock cleaved by thrombin into soluble entities, thus allowing its access to the receptor (Nieswandt and Watson 2003; Candia 2012). Current data showed a significant decrease in GPV level after ISO induction. Low levels of GPV could be justified by the ISO-induced hypercoagulable state, which allows thrombin activation and cleavage of GPV. Moreover, aspirin showed significant increase in GPV levels, whereas a slight non-significant improvement in the combination group suggesting aspirin-mediated action.
Undoubtedly, the emerging concept of utilizing a vascular low dose of rivaroxaban portrays a promising era in atherothrombotic CVDs with growing evidence suggesting a pleiotropic-sparing action of rivaroxaban via PAR signaling pathway (Barrios et al. 2018). PARs belong to the family of G protein-coupled receptors comprising four different isoforms (PAR 1–4), which are expressed in numerous cell types including myocytes, platelets, endothelial cells, and neurons (Soh et al. 2010). Specifically, only PAR-1 (expressed in vascular cells and platelets) and PAR-2 (expressed in vascular cells only) are activated by FXa (Ramachandran et al. 2012). Independent of thrombin, FXa represents a potent platelet agonist, emitting platelet activation through PAR-1 which is prohibited in the presence of rivaroxaban (Hara et al. 2015). Multiple studies disclosed an involvement of both PAR-1 and PAR-2 in cardiac remodeling and hypertrophy, inflammatory signaling, and platelet activation (Petzold et al. 2020). A one experimental study showed that overexpression of PAR-1 participates in cardiac remodeling and structural hypertrophy (Ma and Dorling 2012). In a cardiac ischemic/reperfusion mice model, PAR-2 deficiency was associated with reduced infarct size and suppression of inflammatory process (Pawlinski et al. 2007). In addition, previous evidence showed that activation of PAR-1 and 2 is involved in inducing pro-atherogenic action on arterial vessel walls and subsequently propagating oxidative stress, inflammatory process, endothelial dysfunction, and apoptosis (Antoniak et al. 2010). Clearly, rivaroxaban employs its pleiotropic effect through suppressing the FXa-mediated activation of PAR (Spronk et al. 2014). Indeed, previous in vivo and in vitro study showed that rivaroxaban attenuated platelets activation through prohibiting FXa-dependent PAR-1 activation (Hara et al. 2015). In an animal model of hypertensive mice overexpressing renin, treatment with rivaroxaban managed to inhibit angiotensin II-induced expression of PAR-2 and inflammatory genes, thus inhibiting PAR-2 mediated inflammatory process (Ichikawa et al. 2019). Additionally, an experimental study showed that rivaroxaban reduced oxidative stress and prevented cardiac remodeling by down-regulating PAR-1, PAR-2, and NF-κB expression in a model of intermittent hypoxia (Mitsuishi et al. 2017). Definitely, rivaroxaban pleiotropic nature justifies its atheroprotective effect as displayed in previous evidence (Sanmartín et al. 2019).
Among the limitations of the present report, both dose-dependent and class-specific therapeutic effects of rivaroxaban were not investigated. Therefore, future studies utilizing variable doses of rivaroxaban and compared with other factor Xa inhibitors are recommended for the aforementioned purposes. Interestingly, further analysis comprising other antiplatelet therapies in addressing rivaroxaban therapeutic effect in the setting of myocardial injury could be beneficial. In our experiment, bleeding time was performed to evaluate platelet function and bleeding risk, albeit insensitive. Moreover, histopathologic examination was not performed and is beneficial to be conducted in future research.
Conclusions
The current study is the first experimental study to investigate the therapeutic effect of rivaroxaban with or without aspirin in ISO-induced cardiac injury model. The present data demonstrated antioxidant and anti-inflammatory effect of rivaroxaban against cardiac injury, in addition to platelet reactivity suppression effect. However, the addition of rivaroxaban to aspirin did not show synergistic effect on inflammation, oxidative stress, and platelet reactivity.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- CVD:
-
Cardiovascular disease
- LDL:
-
Low density lipoproteins
- MMPs:
-
Matrix metalloproteinases
- GP:
-
Glycoprotein
- TXA2:
-
Thromboxane A2
- ADP:
-
Adenosine diphosphate
- ISO:
-
Isoproterenol
- MI:
-
Myocardial infarction
- VKAs:
-
Vitamin K antagonists
- TF:
-
Tissue factor
- JUST:
-
Jordan University of Science and Technology
- ACUC:
-
Animal Care and Use Committee
- PBS:
-
Phosphate-buffered saline
- AST:
-
Aspartate aminotransferase
- ALT:
-
Alanine aminotransferase
- CK:
-
Creatine kinase
- LDH:
-
Lactate dehydrogenase
- TNF-α:
-
Tumor necrosis alpha
- IL-6:
-
Interleukin-6
- NO:
-
Nitric oxide
- SOD:
-
Superoxide dismutase
- TBARS:
-
Thiobarbituric acid-reactive substances
- TXB2:
-
Thromboxane B2
- 6-Keto-PGF1α:
-
6-Keto-prostaglandin F1 alpha
- GPV:
-
Glycoprotein V
- Hwt/Bwt:
-
Heart weight to body weight
- PAR:
-
Protease-activated receptors
- COX:
-
Cyclooxygenase
- ELISA:
-
Enzyme-linked immunoassay
References
Abbate A, Trankle CR, Buckley LF, Lipinski MJ, Appleton D, Kadariya D, Canada JM, Carbone S, Roberts CS, Abouzaki N, Melchior R, Christopher S, Turlington J, Mueller G, Garnett J, Thomas C, Markley R, Wohlford GF, Puckett L, Van Tassell BW (2020) Interleukin-1 blockade inhibits the acute inflammatory response in patients with ST-segment-elevation myocardial infarction. J Am Heart Assoc 9(5):1–9. https://doi.org/10.1161/JAHA.119.014941
Allawadhi P, Khurana A, Sayed N, Kumari P, Godugu C (2018) Isoproterenol-induced cardiac ischemia and fibrosis: Plant-based approaches for intervention. Phytother Res 32(10):1908–1932. https://doi.org/10.1002/ptr.6152
Alyavi BA, Uzokov JK, Mukhitdinova O (2021) Antiplatelet therapy in coronary artery disease. Indian J Forensic Med Toxicol 15(3):2111–2115. https://doi.org/10.37506/ijfmt.v15i3.15628
Ambler J, Butler KD, Ku EC, Maguire ED, Smith JR, Wallis RB (1985) CGS 12970: a novel, long acting thromboxane synthetase inhibitor. Br J Pharmacol 86(2):497–504. https://doi.org/10.1111/j.1476-5381.1985.tb08920.x
Antoniak S, Rojas M, Spring D, Bullard TA, Verrier ED, Blaxall BC, Mackman N, Pawlinski R (2010) Protease-activated receptor 2 deficiency reduces cardiac ischemia/reperfusion injury. Arterioscler Thromb Vasc Biol 30(11):2136–2142. https://doi.org/10.1161/ATVBAHA.110.213280
Badimon L, Vilahur G (2014) Thrombosis formation on atherosclerotic lesions and plaque rupture. J Intern Med 276(6):618–632. https://doi.org/10.1111/joim.12296
Badimon L, Padró T, Vilahur G (2012) Atherosclerosis, platelets and thrombosis in acute ischaemic heart disease. Eur Heart J Acute Cardiovasc Care 1(1):60–74. https://doi.org/10.1177/2048872612441582
Bakogiannis C, Sachse M, Stamatelopoulos K, Stellos K (2019) Platelet-derived chemokines in inflammation and atherosclerosis. Cytokine 122:1–10. https://doi.org/10.1016/j.cyto.2017.09.013
Barbarawi M, Kheiri B, Zayed Y, Gakhal I, Al-Abdouh A, Barbarawi O, Rashdan L, Rizk F, Bachuwa G, Alkotob ML (2019) Aspirin efficacy in primary prevention: a meta-analysis of randomized controlled trials. High Blood Press Cardiovasc Prev 26(4):283–291. https://doi.org/10.1007/s40292-019-00325-5
Barisione G, Baroffio M, Crimi E, Brusasco V (2010) Beta-Adrenergic Agonists. Pharmaceuticals 3(4):1016–1044. https://doi.org/10.3390/ph3041016
Barrios V, Almendro-Delia M, Facila L, Garcia-Moll X, Mazon P, Camafort M, María Cepeda J, Mediavilla Garcia JD, Pose Reino A, Suarez Fernandez C (2018) Rivaroxaban: searching the integral vascular protection. Expert Rev Clin Pharmacol 11(7):719–728. https://doi.org/10.1080/17512433.2018.1495559
Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, Chiuve SE, Cushman M, Delling FN, Deo R, De Ferranti SD, Ferguson JF, Fornage M, Gillespie C, Isasi CR, Jiménez MC, Jordan LC, Judd SE, Lackland D, Muntner P (2018) Heart disease and stroke statistics - 2018 update: a report from the American Heart Association. Circulation 137(12):67–492. https://doi.org/10.1161/CIR.0000000000000558
Bentzon JF, Otsuka F, Virmani R, Falk E (2014) Mechanisms of plaque formation and rupture. Circ Res 114(12):1852–1866. https://doi.org/10.1161/CIRCRESAHA.114.302721
Bodor GS (2016) Biochemical markers of myocardial damage. J Int Fed Clin Chem Lab Med 27(2):95–111
Borissoff JI, Spronk HM, Heeneman S, Ten Cate H (2009) Is thrombin a key player in the “coagulation-atherogenesis” maze? Cardiovasc Res 82(3):392–403. https://doi.org/10.1093/cvr/cvp066
Borissoff JI, Heeneman S, Kilinç E, Kaššák P, Van Oerle R, Winckers K, Govers-Riemslag JW, Hamulyák K, Hackeng TM, Daemen MJ, Ten Cate H, Spronk HM (2010) Early atherosclerosis exhibits an enhanced procoagulant state. Circulation 122(8):821–830. https://doi.org/10.1161/CIRCULATIONAHA.109.907121
Busch G, Seitz I, Steppich B, Hess S, Eckl R, Schömig A, Ott I (2005) Coagulation factor Xa stimulates interleukin-8 release in endothelial cells and mononuclear leukocytes implications in acute myocardial infarction. Atheroscler Thromb Vasc Biol 25(2):461–466. https://doi.org/10.1161/01.ATV.0000151279.35780.2d
Cammisotto V, Carnevale R, Nocella C, Stefanini L, Bartimoccia S, Coluccia A, Silvestri R, Pignatelli P, Pastori D, Violi F (2019) Nox2-mediated platelet activation by glycoprotein (GP) VI: effect of rivaroxaban alone and in combination with aspirin. Biochem Pharmacol 163:111–118. https://doi.org/10.1016/j.bcp.2019.02.016
Capodanno D, Mehran R, Valgimigli M, Baber U, Windecker S, Vranckx P, Dangas G, Rollini F, Kimura T, Collet JP, Gibson CM, Steg PG, Lopes RD, Gwon HC, Storey RF, Franchi F, Bhatt DL, Serruys PW, Angiolillo DJ (2018) Aspirin-free strategies in cardiovascular disease and cardioembolic stroke prevention. Nat Rev Cardiol 15(8):480–496
Carretero A, Gomez-Cabrera MC, Rios-Navarro C, Salvador-Pascual A, Bodi V, Viña J (2020) Early reductive stress and late onset overexpression of antioxidant enzymes in experimental myocardial infarction. Free Radical Res 54(2–3):173–184. https://doi.org/10.1080/10715762.2020.1735632
Coppens M, Weitz JI, Eikelboom JW (2019) Synergy of dual pathway inhibition in chronic cardiovascular disease: lessons from the COMPASS trial. Circ Res 124(3):416–425. https://doi.org/10.1161/CIRCRESAHA.118.313141
Corbi G, Conti V, Russomanno G, Longobardi G, Furgi G, Filippelli A, Ferrara N (2013) Adrenergic signaling and oxidative stress: a role for sirtuins? Front Physiol 4:1–14. https://doi.org/10.3389/fphys.2013.00324
Daci A, Da Dalt L, Alaj R, Shurdhiqi S, Neziri B, Ferizi R, Norata GD, Krasniqi S (2020) Rivaroxaban improves vascular response in LPS-induced acute inflammation in experimental models. PLoS One 15(12):1–16. https://doi.org/10.1371/journal.pone.0240669
Dayana K, Manasa MR (2019) Evaluation of the effect of ceftriaxone on lipid peroxidation and antioxidant levels in mice. Biomed Pharmacol J 12(1):245–250. https://doi.org/10.13005/bpj/1634
De Candia E (2012) Mechanisms of platelet activation by thrombin: a short history. Thromb Res 129(3):250–256. https://doi.org/10.1016/j.thromres.2011.11.001
Dejana E, Callioni A, Quintana A (1979) Bleeding time in laboratory animals. II - a comparison of different assay conditions in rats. Thromb Res 15(1–2):191–197
Dhalla NS, Adameova A, Kaur M (2010) Role of catecholamine oxidation in sudden cardiac death. Fundam Clin Pharmacol 24(5):539–546. https://doi.org/10.1111/j.1472-8206.2010.00836.x
Eikelboom JW, Connolly SJ, Bosch J, Dagenais GR, Hart RG, Shestakovska O, Diaz R, Alings M, Lonn EM, Anand SS, Widimsky P, Hori M, Avezum A, Piegas LS, Branch KRH, Probstfield J, Bhatt DL, Zhu J, Liang Y, Yusuf S (2017) Rivaroxaban with or without aspirin in stable cardiovascular disease. N Engl J Med 377(14):1319–1330. https://doi.org/10.1056/nejmoa1709118
Eller T, Busse J, Dittrich M, Flieder T, Alban S, Knabbe C, Birschmann I (2014) Dabigatran, rivaroxaban, apixaban, argatroban and fondaparinux and their effects on coagulation POC and platelet function tests. Clin Chem Lab Med 52(6):835–844. https://doi.org/10.1515/cclm-2013-0936
Forte E, Panahi M, Baxan N, Ng FS, Boyle JJ, Branca J, Bedard O, Muneer Hasham MG, Benson L, Harding SE, Rosenthal N, Sattler S (2021) Type 2 MI induced by a single high dose of isoproterenol in C57BL/6 J mice triggers a persistent adaptive immune response against the heart. J Cell Mol Med 25(1):229–243. https://doi.org/10.1111/jcmm.15937
Fuentes E, Moore-Carrasco R, de Andrade Paes AM, Trostchansky A (2019) Role of platelet activation and oxidative stress in the evolution of myocardial infarction. J Cardiovasc Pharmacol Ther 24(6):509–520. https://doi.org/10.1177/1074248419861437
Garlie JB, Hamid T, Gu Y, Ismahil MA, Chandrasekar B, Prabhu SD (2011) Tumor necrosis factor receptor 2 signaling limits β-adrenergic receptor-mediated cardiac hypertrophy in vivo. Basic Res Cardiol 106(6):1193–1205. https://doi.org/10.1007/s00395-011-0196-6
Gosselin R, Grant RP, Adcock DM (2016) Comparison of the effect of the anti-Xa direct oral anticoagulants apixaban, edoxaban, and rivaroxaban on coagulation assays. Int J Lab Hematol 38(5):505–513. https://doi.org/10.1111/ijlh.12528
Graff J, Von Hentig N, Misselwitz F, Kubitza D, Becka M, Breddin HK, Harder S (2007) Effects of the oral, direct factor Xa inhibitor rivaroxaban on platelet-induced thrombin generation and prothrombinase activity. J Clin Pharmacol 47(11):1398–1407. https://doi.org/10.1177/0091270007302952
Grant MK, Abdelgawad IY, Lewis CA, Seelig D, Zordoky BN (2020) Lack of sexual dimorphism in a mouse model of isoproterenol-induced cardiac dysfunction. PLoS One 15(7):1–19. https://doi.org/10.1371/journal.pone.0232507
Hara T, Fukuda D, Tanaka K, Higashikuni Y, Hirata Y, Nishimoto S, Yagi S, Yamada H, Soeki T, Wakatsuki T, Shimabukuro M, Sata M (2015) Rivaroxaban, a novel oral anticoagulant, attenuates atherosclerotic plaque progression and destabilization in ApoE-deficient mice. Atherosclerosis 242(2):639–646. https://doi.org/10.1016/j.atherosclerosis.2015.03.023
Harding P, Murray DB (2011) The contribution of prostaglandins versus prostacyclin in ventricular remodeling during heart failure. Life Sci 89(19–20):671–676. https://doi.org/10.1016/j.lfs.2011.07.025
Hussain Shaik A, Rasool SN, Kareem MA, Krushna GS, Akhtar PM, Devi KL (2012) Maslinic acid protects against isoproterenol-induced cardiotoxicity in albino Wistar rats. J Med Food 15(8):741–746. https://doi.org/10.1089/jmf.2012.2191
Hussein MA (2015) Cardioprotective effects of astaxanthin against isoproterenol-induced cardiotoxicity in rats. J Nutr Food Sci 5(1):1–6. https://doi.org/10.4172/2155-9600.1000335
Ichikawa H, Shimada M, Narita M, Narita I, Kimura Y, Tanaka M, Osanai T, Okumura K, Tomita H (2019) Rivaroxaban, a direct factor Xa inhibitor, ameliorates hypertensive renal damage through inhibition of the inflammatory response mediated by protease-activated receptor pathway. J Am Heart Assoc 8(8):1–14. https://doi.org/10.1161/JAHA.119.012195
Imam F, Al-Harbi NO, Khan MR, Qamar W, Alharbi M, Alshamrani AA, Alhamami HN, Alsaleh NB, Alharbi KS (2020) Protective effect of RIVA against sunitinib-induced cardiotoxicity by inhibiting oxidative stress-mediated inflammation: probable role of TGF-β and Smad signaling. Cardiovasc Toxicol 20(3):281–290. https://doi.org/10.1007/s12012-019-09551-8
Jaffré F, Friedman AE, Hu Z, Mackman N, Blaxall BC (2012) β-adrenergic receptor stimulation transactivates protease-activated receptor 1 via matrix metalloproteinase 13 in cardiac cells. Circulation 125(24):2993–3003. https://doi.org/10.1161/CIRCULATIONAHA.111.066787
Jagannathan R, Patel SA, Ali MK, Narayan KM (2019) Global updates on cardiovascular disease mortality trends and attribution of traditional risk factors. Curr Diab Rep 19(7):1–12. https://doi.org/10.1007/s11892-019-1161-2
Jain PG, Mahajan UB, Shinde SD, Surana SJ (2018) Cardioprotective role of FA against isoproterenol induced cardiac toxicity. Mol Biol Rep 45(5):1357–1365. https://doi.org/10.1007/s11033-018-4297-2
Jennings LK (2009) Role of platelets in atherothrombosis. Am J Cardiol 103(3):4–10. https://doi.org/10.1016/j.amjcard.2008.11.017
Jia YM, Gu TT, Ji JZ, Tai T, Zhang MR (2018) Aspirin attenuates the bioactivation of and platelet response to Vicagrel in mice. J Cardiovasc Pharmacol 72(5):252–258
Jiang X, Liu X, Liu X, Wu X, Jose PA, Liu M, Yang Z (2020) Low-dose aspirin treatment attenuates male rat salt-sensitive hypertension via platelet cyclooxygenase 1 and complement cascade pathway. J Am Heart Assoc 9(1):1–19. https://doi.org/10.1161/JAHA.119.013470
Katoh H, Nozue T, Michishita I (2017) Anti-inflammatory effect of factor-Xa inhibitors in Japanese patients with atrial fibrillation. Heart Vessels 32(9):1130–1136. https://doi.org/10.1007/s00380-017-0962-y
Kobiyama K, Ley K (2018) Atherosclerosis: a chronic inflammatory disease with an autoimmune component. Circ Res 123(10):1118–1120. https://doi.org/10.1056/NEJMoa0807646
Kono S, Yamashita T, Deguchi K, Omote Y, Yunoki T, Sato K, Kurata T, Hishikawa N, Abe K (2014) Rivaroxaban and apixaban reduce hemorrhagic transformation after thrombolysis by protection of neurovascular unit in rat. Stroke 45(8):2404–2410. https://doi.org/10.1161/STROKEAHA
Kurian GA, Rajagopal R, Vedantham S, Rajesh M (2016) The role of oxidative stress in myocardial ischemia and reperfusion injury and remodeling: revisited. Oxid Med Cell Longev 2016:1–14. https://doi.org/10.1155/2016/1656450
Kyu HH, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, Abbastabar H, Abd-Allah F, Abdela J, Abdelalim A, Abdollahpour I, Abdulkader RS, Abebe M, Abebe Z, Abil OZ, Aboyans V, Abrham AR, Abu-Raddad LJ, Abu-Rmeileh NM, Murray CJL (2018) Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392(10159):1859–1922. https://doi.org/10.1016/S0140-6736(18)32335-3
Lalitha G, Poornima P, Archanah A, Padma VV (2013) Protective effect of neferine against isoproterenol-induced cardiac toxicity. Cardiovasc Toxicol 13(2):168–179. https://doi.org/10.1007/s12012-012-9196-5
Licata A, Puccia F, Lombardo V, Serruto A, Minissale MG, Morreale I, Giannitrapani L, Soresi M, Montalto G, Almasio PL (2018) Rivaroxaban-induced hepatotoxicity: review of the literature and report of new cases. Eur J Gastroenterol Hepatol 30(2):226–232. https://doi.org/10.1097/MEG.0000000000001030
Lim KH, Ko D, Kim JH (2013) Cardioprotective potential of Korean red ginseng extract on isoproterenol-induced cardiac injury in rats. J Ginseng Res 37(3):273–282. https://doi.org/10.5142/jgr.2013.37.273
Liu J, Chen L, Lu H (2018) Cardioprotective effect of salvianolic acid B against isoproterenol-induced inflammation and histological changes in a cardiotoxicity rat model. Trop J Pharm Res 17(11):2189–2197. https://doi.org/10.4314/tjpr.v17i11.12
Liu J, Nishida M, Inui H, Chang J, Zhu Y, Kanno K, Matsuda H, Sairyo M, Okada T, Nakaoka H, Ohama T, Masuda D, Koseki M, Yamashita S, Sakata Y (2019) Rivaroxaban suppresses the progression of ischemic cardiomyopathy in a murine model of diet-induced myocardial infarction. J Atheroscler Thromb 26(10):915–930. https://doi.org/10.5551/jat.48405
Lordan R, Tsoupras A, Zabetakis I (2021) Platelet activation and prothrombotic mediators at the nexus of inflammation and atherosclerosis: potential role of antiplatelet agents. Blood Rev 45(1):1–18. https://doi.org/10.1016/j.blre.2020.100694
Ma L, Dorling A (2012) The roles of thrombin and protease-activated receptors in inflammation. Semin Immunopathol 34(1):63–72. https://doi.org/10.1007/s00281-011-0281-9
Mabley J, Patel JP, Sayed A, Arya R, Scutt G (2019) Direct oral anticoagulant (DOAC)-mediated vasodilation: role of nitric oxide. Thromb Res 176(1):36–38. https://doi.org/10.1016/j.thromres.2019.02.014
Maity G, De A, Das A, Banerjee S, Sarkar S, Banerjee SK (2015) Aspirin blocks growth of breast tumor cells and tumor-initiating cells and induces reprogramming factors of mesenchymal to epithelial transition. Lab Invest 95(7):702–717. https://doi.org/10.1038/labinvest.2015.49
Milutinović A, Šuput D, Zorc-Pleskovič R (2020) Pathogenesis of atherosclerosis in the tunica intima, media, and adventitia of coronary arteries: an updated review. Bosnian J Basic Med Sci 20(1):21–30. https://doi.org/10.17305/BJBMS.2019.4320
Mitsuishi R, Imano H, Kato R, Ijiri Y, Yamaguchi T, Yoshiyama M, Hayashi T (2017) Rivaroxaban attenuates cardiac remodeling due to intermittent hypoxia by suppressing the synergistic effects of PAR-1 and PAR-2. J Am Coll Cardiol 69(11):2033. https://doi.org/10.1016/S0735-1097(17)35422-0
Montalescot G, Sechtem U, Achenbach S, Andreotti F, Arden C, Budaj A, Bugiardini R, Crea F, Cuisset T, Di Mario C, Ferreira JR, Gersh BJ, Gitt AK, Hulot JS, Marx N, Opie LH, Pfisterer M, Prescott E, Ruschitzka F, Yildirir A (2013) 2013 ESC guidelines on the management of stable coronary artery disease. Eur Heart J 34(38):2949–3003. https://doi.org/10.1093/eurheartj/eht296
Moursi SM, Ashour WM, Elbelbesy RM (2019) Vaspin improves experimental isoproterenol-induced heart failure in rats. Am J Biomed Sci 11(3):141–151. https://doi.org/10.5099/aj190300141
Mukherjee D, Ghosh AK, Dutta M, Mitra E, Mallick S, Saha B, Reiter RJ, Bandyopadhyay D (2015) Mechanisms of isoproterenol-induced cardiac mitochondrial damage: protective actions of melatonin. J Pineal Res 58(3):275–290. https://doi.org/10.1111/jpi.12213
Murphy PT, Grace S, Glavey S, Quinn J (2019) Rivaroxaban may increase platelet activation in vivo via thromboxane A2. Circ Res 125(2):e9. https://doi.org/10.1161/CIRCRESAHA.119.315453
Nieswandt B, Watson SP (2003) Platelet-collagen interaction: is GPVI the central receptor? Blood 102(2):449–461. https://doi.org/10.1182/blood-2002-12-3882
Özbudak E, Ceyla Eraldemir FC, Arıkan AA, Şahin D, Kır HM, Kurt T, Faruk Gülaştı ÖF, Yavuz Ş (2019) An evaluation of rivaroxaban and clopidogrel in a rat lower extremity ischemia-reperfusion model: an experimental study. Turk J Thorac Cardiovasc Surg 27(4):513–520. https://doi.org/10.5606/tgkdc.dergisi.2019.18061
Park JY, Lee S-H, Shin M-J, Hwang GS (2015) Alteration in metabolic signature and lipid metabolism in patients with angina pectoris and myocardial infarction. PLoS One 10(8):1–15. https://doi.org/10.1371/journal.pone.0135228
Patrono C, Rocca B (2019) Measurement of thromboxane biosynthesis in health and disease. Front Pharmacol 10:1–11. https://doi.org/10.3389/fphar.2019.01244
Pawlinski R, Tencati M, Hampton CR, Shishido T, Bullard TA, Casey LM, Andrade-Gordon P, Kotzsch M, Spring D, Luther T, Abe J, Pohlman TH, Verrier ED, Blaxall BC, Mackman N (2007) Protease-activated receptor-1 contributes to cardiac remodeling and hypertrophy. Circulation 116(20):2298–2306. https://doi.org/10.1161/CIRCULATIONAHA.107.692764
Perzborn E, Roehrig S, Straub A, Kubitza D, Misselwitz F (2011) The discovery and development of rivaroxaban, an oral, direct factor Xa inhibitor. Nat Rev Drug Discovery 10(1):61–75. https://doi.org/10.1038/nrd3185
Perzborn E, Heitmeier S, Laux V (2015) Effects of rivaroxaban on platelet activation and platelet-coagulation pathway interaction: in vitro and in vivo studies. J Cardiovasc Pharmacol Ther 20(6):554–562. https://doi.org/10.1177/1074248415578172
Petzold T, Thienel M, Dannenberg L, Mourikis P, Helten C, Ayhan A, M’Pembele R, Achilles A, Trojavky K, Konsek D, Zhang Z, Regenauer R, Pircher J, Ehrlich A, Lüsebrink E, Nicolai L, Stocker TJ, Brandl R, Röschenthaler F, Polzin A (2020) Rivaroxaban reduces arterial thrombosis by inhibition of FXa-driven platelet activation via protease activated receptor-1. Circ Res 126(4):486–500. https://doi.org/10.1161/CIRCRESAHA.119.315099
Posma JJ, Sluimer JC (2021) Pleiotropic, cellular effects of rivaroxaban on autophagy explain atheroprotective effects. J Am Coll Cardiol 6(12):981–983. https://doi.org/10.1016/j.jacbts.2021.10.015
Pullaiah CP, Nelson VK, Rayapu S, GV NK, Kedam T (2021) Exploring cardioprotective potential of esculetin against isoproterenol induced myocardial toxicity in rats: in vivo and in vitro evidence. BMC Pharmacol Toxicol 22(1):1–11. https://doi.org/10.1186/s40360-021-00510-0
Rababa’h AM, Alzoubi MA (2021) Origanum majorana L. extract protects against isoproterenol-induced cardiotoxicity in rats. Cardiovasc Toxicol 21(7):543–552. https://doi.org/10.1007/s12012-021-09645-2
Rababa’h AM, Guillory AN, Mustafa R, Hijjawi T (2018) Oxidative stress and cardiac remodeling: an updated edge. Curr Cardiol Rev 14(1):53–59. https://doi.org/10.2174/1573403X14666180111145207
Rafeeq A, Najam R, Hussain SJ (2016) Aspirin associated liver toxicity – the optimal dose of aspirin in liver insufficiency. Int J Sci Res Knowl 4(2):28–32. https://doi.org/10.12983/ijsrk-2016-p0028-0032
Raish M, Ahmad A, Ansari MA, Alkharfy KM, Ahad A, Khan A, Ali N, Ganaie MA, Hamidaddin MA (2019) Beetroot juice alleviates isoproterenol-induced myocardial damage by reducing oxidative stress, inflammation, and apoptosis in rats. 3 Biotech 9(4):1–11
Ramachandran R, Noorbakhsh F, DeFea K, Hollenberg MD (2012) Targeting proteinase-activated receptors: therapeutic potential and challenges. Nat Rev Drug Discovery 11(1):69–86. https://doi.org/10.1038/nrd3615
Rathore N, John S, Kale M, Bhatnagar D (1998) Lipid peroxidation and antioxidant enzymes in isoproterenol induced oxidative stress in rat tissues. Indian J Physiol Pharmacol 38(4):297–303
Rocha BM, da Cunha GJ, Aguiar CM (2021) A narrative review of low-dose rivaroxaban in patients with atherothrombotic cardiovascular disease: vascular protection beyond anticoagulation. Cardiovasc Diagn Ther 11(1):130–141. https://doi.org/10.21037/cdt-20-859
Roth GA, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, Abbastabar H, Abd-Allah F, Abdela J, Abdelalim A, Abdollahpour I, Abdulkader RS, Abebe HT, Abebe M, Abebe Z, Abejie AN, Abera SF, Abil OZ, Abraha HN, Murray CJL (2018) Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392(10159):1736–1788. https://doi.org/10.1016/S0140-6736(18)32203-7
Sagor M, Taher A, Tabassum N, Potol M, Alam M (2015) Xanthine oxidase inhibitor, allopurinol, prevented oxidative stress, fibrosis, and myocardial damage in isoproterenol induced aged rats. Oxid Med Cell Longev 2015:1–9. https://doi.org/10.1155/2015/478039
Samiei F, Sajjadi H, Jamshidzadeh A, Seydi E, Pourahmad J (2019) Contrasting role of concentration in rivaroxaban induced toxicity and oxidative stress in isolated kidney mitochondria. Drug Res 69(10):523–527. https://doi.org/10.1055/a-1001-2154
Sangeethadevi G, Jansy Isabella RAR, Saravanan G, Ponmurugan P, Chandrasekaran P, Sengottuvelu S, Vadivukkarasi S (2021) Attenuation of lipid metabolic abnormalities, proinflammatory cytokines, and matrix metalloproteinase expression by biochanin-A in isoproterenol-induced myocardial infarction in rats. Drug Chem Toxicol 44(2):1–12. https://doi.org/10.1080/01480545.2021.1894707
Sanmartín M, Bellmunt S, Cosín-Sales J, García-Moll X, Riera-Mestre A, Almendro-Delia M, Luis Hernández J, Lozano F, Mazón P, Suarez Fernández C (2019) Role of rivaroxaban in the prevention of atherosclerotic events. Expert Rev Clin Pharmacol 12(8):771–780. https://doi.org/10.1080/17512433.2019.1637732
Santilli F, Lapenna D, La Barba S, Davì G (2015) Oxidative stress-related mechanisms affecting response to aspirin in diabetes mellitus. Free Radical Biol Med 80:101–110. https://doi.org/10.1016/j.freeradbiomed.2014.12.010
Shackebaei D, Hesari M, Ramezani-Aliakbari S, Hoseinkhani Z, Ramezani-Aliakbari F (2022) Gallic acid protects against isoproterenol-induced cardiotoxicity in rats. Hum Exp Toxicol 41:1–10. https://doi.org/10.1177/09603271211064532
Shahzad S, Hasan A, Faizy AF, Mateen S, Fatima N, Moin S (2018) Elevated DNA damage, oxidative stress, and impaired response defense system inflicted in patients with myocardial infarction. Clin Appl Thromb Hemost 24(5):780–789. https://doi.org/10.1177/1076029617725602
Sindet-Pedersen C, Pallisgaard JL, Staerk L, Gerds TA, Fosbøl EL, Torp-Pedersen C, Gislason G, Olesen JB (2017) Comparative safety and effectiveness of rivaroxaban versus VKAs in patients with venous thromboembolism: a Danish nationwide registry-based study. Thromb Haemost 117(6):1182–1191. https://doi.org/10.1160/TH16-10-0745
Soehnlein O, Libby P (2021) Targeting inflammation in atherosclerosis — from experimental insights to the clinic. Nat Rev Drug Discovery 20(8):589–610. https://doi.org/10.1038/s41573-021-00198-1
Soh UJ, Dores MR, Chen B, Trejo J (2010) Signal transduction by protease-activated receptors. Br J Pharmacol 160(2):191–203. https://doi.org/10.1111/j.1476-5381.2010.00705.x
Song Q, Wang S, Zhao W (2012) Total steroidal alkaloids from Veratrum patulum L. Inhibit platelet aggregation, thrombi formation and decrease bleeding time in rats. J Ethnopharmacol 141(1):183–186. https://doi.org/10.1016/j.jep.2012.02.017
Song L, Srilakshmi M, Wu Y, Saleem TS (2020) Sulforaphane attenuates isoproterenol-induced myocardial injury in mice. Biomed Res Int 2020:1–7. https://doi.org/10.1155/2020/3610285
Spronk HM, Van Der Voort D, Ten Cate H (2004) Blood coagulation and the risk of atherothrombosis: a complex relationship. Thromb J 2(1):1–10. https://doi.org/10.1186/1477-9560-2-12
Spronk HM, De Jong AM, Crijns HJ, Schotten U, Van Gelder IC, Ten Cate H (2014) Pleiotropic effects of factor Xa and thrombin: what to expect from novel anticoagulants. Cardiovasc Res 101(3):344–351. https://doi.org/10.1093/cvr/cvt343
Swapna K, Sathibabu Uddandrao VV, Parim B, Ravindarnaik R, Suresh P, Ponnusamy P, Balakrishnan S, Vadivukkarasi S, Harishankar N, Reddy KP, Nivedha PR, Saravanan G (2019) Effects of asiatic acid, an active constituent in Centella asiatica (L.): restorative perspectives of streptozotocin-nicotinamide induced changes on lipid profile and lipid metabolic enzymes in diabetic rats. Comp Clin Pathol 28(5):1321–1329. https://doi.org/10.1007/s00580-019-02955-6
Szczuko M, Kozioł I, Kotlega D, Brodowski J, Drozd A (2021) The role of thromboxane in the course and treatment of ischemic stroke: review. Int J Mol Sci 22(21):1–15. https://doi.org/10.3390/ijms222111644
Tantry U, Cummings C, MacKrell P, Gonze M, Ulloa K, Bafford R, Rout A, Sukhi A, Gurbel P (2020) Synergistic influence of rivaroxaban on inflammation and coagulation biomarkers in patients with coronary artery disease and peripheral artery disease on aspirin therapy. Future Cardiol 16(2):69–75. https://doi.org/10.2217/fca-2019-0091
Tarantino E, Amadio P, Squellerio I, Porro B, Sandrini L, Turnu L, Cavalca V, Tremoli E, Barbieri SS (2016) Role of thromboxane-dependent platelet activation in venous thrombosis: aspirin effects in mouse model. Pharmacol Res 107:415–425. https://doi.org/10.1016/j.phrs.2016.04.001
Tellor KB, Patel S, Armbruster AL, Daly MW (2015) Evaluation of the appropriateness of dosing, indication and safety of rivaroxaban in a community hospital. J Clin Pharm Ther 40(4):447–451. https://doi.org/10.1111/jcpt.12288
Ujjawal A, Gupta M, Ghosh RK, Jain V, Bandyopadhyay D, Qamar A, Aronow WS, Deedwania P, Kapadia S, Lavie CJ (2021) Aspirin for primary prevention of coronary artery disease. Curr Probl Cardiol 46(3):1–18. https://doi.org/10.1016/j.cpcardiol.2020.100553
Utku OG, Karatay EA, Erdal H, Arhan M, Onal IK, Ibis M, Ekinci O, Yilmaz Demirtas C, Unal S (2015) Rivaroxaban induces mucosal healing in a rat model of trinitrobenzene sulfonic acid-induced colitis. Med Princ Pract 24(5):470–476. https://doi.org/10.1159/000431361
Verma VK, Malik S, Narayanan SP, Mutneja E, Sahu AK, Bhatia J, Arya DS (2019) Role of MAPK/NF-κB pathway in cardioprotective effect of Morin in isoproterenol induced myocardial injury in rats. Mol Biol Rep 46(1):1139–1148. https://doi.org/10.1007/s11033-018-04575-9
Viswanadha VP, Dhivya V, Beeraka NM, Huang CY, Gavryushova LV, Minyaeva NN, Chubarev VN, Mikhaleva LM, Tarasov VV, Aliev G (2020) The protective effect of piperine against isoproterenol-induced inflammation in experimental models of myocardial toxicity. Eur J Pharmacol 885:1–11. https://doi.org/10.1016/j.ejphar.2020.173524
Wan H, Yang Y, Zhu J, Wu S, Zhou Z, Huang B, Wang J, Shao X, Zhang H (2016) An in-vitro evaluation of direct thrombin inhibitor and factor Xa inhibitor on tissue factor-induced thrombin generation and platelet aggregation: a comparison of dabigatran and rivaroxaban. Blood Coag Fibrinol 27(8):882–885. https://doi.org/10.1097/MBC.0000000000000509
Wolf D, Ley K (2019) Immunity and inflammation in atherosclerosis. Circ Res 124(2):315–327. https://doi.org/10.1161/CIRCRESAHA.118.313591
Wong ZW, Thanikachalam PV, Ramamurthy S (2017) Molecular understanding of the protective role of natural products on isoproterenol-induced myocardial infarction: a review. Biomed Pharmacother 94:1145–1166. https://doi.org/10.1016/j.biopha.2017.08.009
Xiao H, Li H, Wang JJ, Zhang JS, Shen J, An XB, Zhang CC, Wu JM, Song Y, Wang XY, Yu HY, Deng XN, Li ZJ, Xu M, Lu ZZ, Du J, Gao W, Zhang AH, Feng Y, Zhang YY (2018) IL-18 cleavage triggers cardiac inflammation and fibrosis upon β-Adrenergic insult. Eur Heart J 39(1):60–69. https://doi.org/10.1093/eurheartj/ehx261
Xie Q, Li S, Gao Y, Jin L, Dai C, Song J (2020) Ergosterol attenuates isoproterenol-induced myocardial cardiotoxicity. Cardiovasc Toxicol 20(5):500–506. https://doi.org/10.1007/s12012-020-09574-6
Zhang J, Knapton A, Lipshultz SE, Weaver JL, Herman EH (2008) Isoproterenol-induced cardiotoxicity in Sprague-Dawley rats: correlation of reversible and irreversible myocardial injury with release of cardiac troponin T and roles of iNOS in myocardial injury. Toxicol Pathol 36(2):277–288. https://doi.org/10.1177/0192623307313010
Zhou R, Ma P, Xiong A, Xu Y, Wang Y, Xu Q (2017) Protective effects of low-dose rosuvastatin on isoproterenol-induced chronic heart failure in rats by regulation of DDAH-ADMA-NO pathway. Cardiovasc Ther 35(2):1–8. https://doi.org/10.1111/1755-5922.12241
Funding
This work was supported by the Deanship of Research at Jordan University of Science and Technology [Grant No. 369–2021 to AR].
Author information
Authors and Affiliations
Contributions
AR, NA, and MA designed the study. AR and NA conducted the experimental work. AR, NA, and MA drafted the manuscript; AR and NA conducted the field research; AR contributed new reagents or analytic tools; AR, NA, and MA performed data analysis and interpreted the results; AR and NA contributed to the discussion. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
The experimental procedures were performed in congruency with the regulations of the Animal Care and Use Committee (ACUC; ACUC approval No. 412–2021) at Jordan University of Science and Technology and in accordance with the concepts of laboratory animal care and use as involved in the European Community Guidelines.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Abedalqader, N.N., Rababa’h, A.M. & Ababneh, M. The protective effect of rivaroxaban with or without aspirin on inflammation, oxidative stress, and platelet reactivity in isoproterenol-induced cardiac injury in rats. Naunyn-Schmiedeberg's Arch Pharmacol 396, 337–351 (2023). https://doi.org/10.1007/s00210-022-02319-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-022-02319-y