Abstract
Berberine, a chemical found in plants, is used as a supplement for diabetes. This study aimed to investigate the effects and the underlying molecular regulations of berberine in diabetic neuropathic pain in a rat model of diabetes. Rats were injected with streptozotocin (STZ) to induce diabetes and then were treated with berberine. Blood glucose levels and body weight were measured. Thermal and mechanical nociception were assessed by paw pressure test and hot tail immersion test. Oxidative stress was assessed by lipid peroxidation, production of reactive oxygen species (ROS) and catalase activity. Neuroinflammation was assessed by tumor necrosis factor-α (TNF-α) and interleukin-6 (IL-6) protein levels. Finally, μ-opioid receptor (MOR) protein and mRNA levels were measured. We found that berberine treatment partially suppressed blood glucose levels and restored body weight in diabetic rats. Berberine also suppressed STZ-induced oversensitivity of mechanical and thermal nociception. Additionally, berberine partially suppressed oxidative stress and inflammation of diabetic rats. Finally, berberine significantly enhanced protein and mRNA expression levels of μ-opioid receptor (MOR). Our findings suggest that berberine is a potential therapeutic alleviating diabetes and diabetic neuropathic pain, probably through suppression of oxidative stress and neuroinflammation that may be mediated by MOR.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus is prevalent chronic metabolic disorder, affecting approximately 400 million people worldwide (Nathan 2015). While several ways have been shown to effectively manage blood glucose levels, including medications such as use of insulin, diet, and physical activity, it is relatively more difficult to control the many common complications associated with diabetes including retinopathy, nephropathy, neuropathy, cardiovascular diseases, foot damage, and neurodegeneration (Toth 2014; Wong et al. 2016; Maffi and Secchi 2017).
Diabetic neuropathic pain is common among patients with diabetes. With approximately half of adult diabetic patients being affects, diabetic neuropathic pain has caused serious problems (Paisley and Serpell 2017). Due to damages of nerves resulted from high blood glucose levels, organs throughout the body are being affected, including heart, blood vessels, the digestive system, and painful feet and legs. Leaving improperly treated, diabetic neuropathy can be costly and devastating. While therapeutic strategies have been explored to treat this disabling diabetes complication, no effective treatment is available and there is an urgent need to develop drugs with high efficacy and safety (Javed et al. 2015).
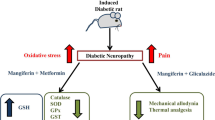
Several pathophysiological processes have been shown to be implicated in diabetic neuropathy, mainly including abnormal oxidative stress and neuroinflammation (Albers and Pop-Busui 2014). Suppressing oxidative stress and inflammatory status is associated with alleviation of neuropathic pain in a mouse mode of diabetes (Valsecchi et al. 2011). Additionally, μ-opioid receptors have been implicated in the pathogenesis of obesity, a risk factor for type 2 diabetes, and diabetic neuropathic pain. Reduced levels of μ-opioid receptors have been observed both the in the brains of diabetic individuals as well as the spinal cord of diabetic rats induced by STZ administration (Karlsson et al. 2015; Kou et al. 2016). Agonist-mediated activation of μ-opioid receptors alleviates mechanical hyperalgesia that is associated with diabetic neuropathy in rats (Schiene et al. 2015).
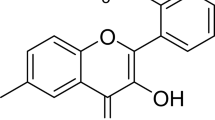
Berberine is a naturally occurring chemical extracted from several plants such as tree turmeric and goldenseal. Berberine possesses multiple biological and pharmacological activities including anti-tumor, anti-inflammatory and anti-oxidative stress effects (Caliceti et al. 2016). Recently, berberine has also been shown to have an anti-diabetic effect and has been used in clinical studies for the treatment of type 2 diabetes (Chang et al. 2015). Berberine has been shown to alleviate diabetic nephropathy through suppression of inflammatory responses and podocyte apoptosis by modulating TLR4/NF-κB activity (Zhu et al. 2018). Several recent studies have also shown that berberine is beneficial for suppressing diabetic neuropathy (Zhou et al. 2016; Zan et al. 2017). Additionally, berberine has been shown to suppress visceral pain and improves intestinal motility in mouse models of irritable bowel syndrome that involved MOR (Chen et al. 2015).
We therefore hypothesized that berberine might alleviate neuropathy in diabetic animal models through suppression of neuroinflammation and oxidative stress and this regulation might involve MOR. In this study, we further explored the effects of berberine in STZ-induced diabetes in rats and investigated its role in neuroinflammation, oxidative stress, and regulation of MOR.
Materials and methods
Diabetic rat model and drug treatment
All animal procedures were approved by Guangxi Medical University’s ethics committee. Male adult Wistar rats were housed in an environmentally controlled animal facility at a 12-h light-dark cycle with free access to a regular diet and drinking water. Rats weighed 180–220 g at the beginning to the study and were singly housed. Rats were randomly divided into five groups: sham (vehicle treatment, n = 10), diabetes (STZ+ vehicle treatment, n = 10), diabetes+ Ber 5 (STZ+ 5 mg/kg berberine), diabetes+ Ber 20 (STZ+ 20 mg/kg berberine), and diabetes+ Ber 40 (STZ+ 40 mg/kg berberine).
After 1 week of acclimation to the animal facility, diabetes was induced with a single dose of streptozotocin (STZ, 60 mg/kg body weight) by intraperitoneal (i.p.) injection. Fasting blood glucose levels were assessed 2 weeks following STZ administration and rats with a glucose level of over 16.7 mM were included in this study as diabetic (Zhou et al. 2016). Berberine was prepared according to a previous study by first dissolving with dimethyl sulfoxide (DMSO) and then diluted with 0.9% normal saline (Yang et al. 2018). At 2 weeks after STZ administration, diabetic rats were treated with berberine at indicated dose by i.p. injection daily for 10 weeks or insulin at 5 IU/kg by subcutaneous injection. Blood glucose levels and body weight were measured every 4 weeks. Mechanical and thermal nociception were assessed every 2 weeks. Rats were euthanized under anesthesia and tissues were harvested for biochemical analysis at 12 weeks following STZ injection.
Mechanical and thermal nociceptive tests
Mechanical nociception was assessed by paw pressure test as described previously with a rodent pincher analgesia meter (Kiasalari et al. 2017). Briefly, mechanical pressure was applied to the left hind paw of the rat being tested with increasing force. The threshold at which rat withdrew its paw was recorded. A maximum force of 500 g was applied and the threshold hold was recorded as 500 g even if rats did not withdraw at this force level. Each rat was subjected to three trials with a 10-min interval between two trials. The average threshold was calculated.
Hot tail immersion test was performed to assess the thermal nociception as described previously (Kiasalari et al. 2017). Briefly, the tail of the rat being test was immersed into 51 °C water for a maximum of 30 s and the latency when the rat withdrew the tail was recorded. Each rat was subjected to four trials with a 5-min interval between two trials. The average latency was calculated.
Assessment of oxidative stress
Oxidative stress was assessed by lipid peroxidation, reactive oxygen species (ROS) production, and catalase activity as described previously (Zhao et al. 2015).
Malondialdehyde (MDA) levels were measured in the serum from different rat groups to determine lipid peroxidation. Briefly, blood sample was collected from each rat using cardiac puncture, homogenized in 1.15% KCl solution supplemented with 1 mM phenyl methyl sulphonyl fluoride, and 10% trichloroacetic acid was added to the supernatant after centrifuging for 20 min at 1500×g. The samples were extracted after centrifuging for a second time for 5 min at 1000×g, added with 0.67% thiobabituric acid and incubated for 20 min in boiling water. The absorbance at the wavelength of 535 nm was measured and converted to MDA concentration.
Hydrogen peroxide (H2O2) levels were measured to determine ROS production. Briefly, rat blood was homogenized in phosphate buffer (500 mM) supplemented with 10 mM sodium azide. After centrifuging at 4 °C for 10 min at a speed of 15, 000 g, 100 μl reaction solution was added to 50 μl of supernatant and incubated for 20 min at room temperature. The optic density was measured at the wavelength of 560 nm and the H2O2 concentration was calculated.
Catalase activity was determined by homogenizing blood in 0.25 M sucrose, which was first centrifuged for 10 min at 1000 g. The supernatant of the homogenate was further centrifuged 4 °C for 20 min at a speed of 10, 000 g. The supernatant (50 μl) from the second centrifuge was mixed with 1.7 M hydrogen peroxide and 0.05 M phosphate until 3 ml. The absorption was measured at the wavelength of 240 nm. Catalase activity was calculated.
Western blot
DRGs and spinal cord were isolated from rats of each indicated group, homogenized in lysis buffer and proteins were subjected to standard preparation and separation by electrophoresis as described previously (Mao et al. 2017). Proteins were transferred to a polyvinylidene membrane, incubated in primary antibodies at 4 °C for overnight and in secondary antibodies at room temperature and detected using a LI-COR imaging system. Protein expression was quantified and presented as relatively to control group. The following antibodies were used in this study: anti-MOR (ab10275) and anti-GAPDH (ab8245). All antibodies were purchased from Abcam.
Quantitative real-time polymerase chain reaction
qRT-PCR was performed to assess the mRNA levels as described previously (Yang et al. 2018). Briefly, following isolation from rats of each indicated group, DRGs and spinal cord were subjected for total RNA extraction by the Trizon reagent (Invitrogen, Waltham, MA USA). The SYBR Green master (Invitrogen) was used for qRT-PCR. GAPDH was used as an internal control.
ELISA
Serum levels of TNF-α and IL-6 were assessed by ELISA using respective kits (R&D Biosystem, Minneapolis, MN) according to manufacturer’s instruction.
Immunofluorescent staining
Immunofluorescent staining was performed according to a previous study (Wan et al. 2016). Briefly, rats were anesthetized, perfused with PBS followed by 4% paraformaldehyde and post-fixed. The spinal cord and DRG were dissected and incubated in 30% sucrose for overnight. Sagittal sections of the spinal cord and horizontal sections of the DRG were stained with anti-MOR antibody (ab10275, Abcam). After staining, sections were observed under fluorescent microscope and images were taken. The optical intensity was measured to represent the expression level of MOR.
Statistical analysis
The statistical difference between two groups was determined by one- or two-way ANOVA analysis following a Tukey’s post hoc test. Mean ± SD was used for data presentation. Significant difference was reached with P < 0.05.
Results
Berberine suppressed STZ-induced blood glucose and body weight changes in a dose-dependent manner
To confirm the establishment and persistence of diabetic symptoms, we measured blood glucose levels and body weight of all rats. Consistent with previous studies on induction of diabetes by STZ injection, we found that STZ administration significantly increased blood glucose levels (Fig. 1a) and decreased body weight (Fig. 1b) at 4, 8, and 12 weeks compared to that of control rats at the same time points. Treatment of diabetic rats with a low-dose berberine (5 mg/kg) did not affect STZ-induced changes in blood glucose levels and body weight. Importantly, we found that higher doses of berberine (20 mg/kg and 40 mg/kg) partially and significantly suppressed both blood glucose levels and body weight in diabetic rats. Similarly, insulin treatment also reduced blood glucose levels and body weight in diabetic rats.
Berberine restored mechanical and thermal nociception in diabetic rats in a dose-dependent manner
We then investigated mechanical and thermal nociception which is impair in diabetic animal models. Paw pressure test showed that STZ administration significantly reduced mechanical threshold starting at 2 weeks post injection that persisted until the end of the study (12 weeks) (Fig. 2a). We found that a low dose of berberine (5 mg/kg) did not improve mechanical threshold in diabetic rats. However, higher doses of berberine (20 mg/kg and 40 mg/kg) gradually improved mechanical nociception. Although lower that control group, higher doses of berberine significantly increased mechanical threshold in diabetic rats.
Effects of berberine treatment to diabetic rats, starting 2 weeks since STZ injection, on mechanical nociceptive test a and thermal nociceptive test b. Data are presented as mean ± SD. *p < 0.05, **p < 0.01 compared to sham group in the same week. #p < 0.05, ##p < 0.01 compared to diabetes group in the same week
In the hot tail immersion test, we found that STZ administration significantly reduced tail withdraw latency (Fig. 2b). Consistent with the above results, we found that higher doses of berberine (20 mg/kg and 40 mg/kg) gradually improved thermal nociception and significantly increased paw withdraw latency.
Interestingly, we did not observe any rescuing effect of insulin treatment on both mechanical and thermos nociception in diabetic rats, suggesting the effects of berberine are not due to reduced blood glucose levels.
Berberine suppressed oxidative stress in diabetic rats
We found that STZ administration increased oxidative stress as indicated by increased MDA (Fig. 3a) and ROS (Fig. 3b) production and decreased catalase activity in the serum (Fig. 3c) starting from 4 weeks after treatment. Importantly, we found that berberine treatment at the dose of 40 mg/kg significantly suppressed MDA and ROS production and increased catalase activity, although they were still significantly different from the control group. These results suggest that berberine treatment partially suppressed STZ-induced oxidative stress. Additionally, we found that insulin treatment did not suppress STZ-induced oxidative stress, suggesting that berberine treatment-mediated suppression of oxidative stress is not due to reduced glucose levels.
Berberine reduced neuroinflammation in diabetic rats
We then examined the effects of berberine on STZ-induced neuroinflammation. First, we confirmed overproduction of proinflammatory cytokines TNF-α (Fig. 4a) and IL-6 (Fig. 4b) in the serum by ELISA. Quantification results showed that STZ significantly upregulated TNF-α and IL-6 levels. We found that while 40 mg/kg berberine treatment did not completely restore TNF-α and IL-6 levels to that of control group, it significantly suppressed STZ-induced TNF-α and IL-6 production, indicating that berberine suppresses STZ-induced neuroinflammation in rats. Additionally, we found that insulin treatment at 5 IU/kg did not alter the serum levels of TNF-α and IL-6 in diabetic rats.
Berberine restored MOR expression in diabetic rats
Finally, we investigated the effects of berberine on MOR expression. Consistent with previous studies, we found that STZ treatment slightly suppressed MOR protein expression in both spinal cord and DRGs of the rats (Fig. 5a and b). Strikingly, we found that berberine significantly restored both MOR protein and mRNA expression in STZ treated rat spinal cord and DRG and these levels were significantly higher than that of the control rats (Fig. 5c and d). On the other hand, we found that insulin treatment did not affect MOR levels.
Effects of berberine treatment (40 mg/kg for 12 weeks) on MOR expression in the spinal cord and DRG of diabetic rats. Western blot was used to detect MOR protein expression in spinal cord a and DRG b. Relative MOR protein expression c from Western blot and relative MOR mRNA expression d from qRT-PCR were analyzed. Data are presented as mean ± SD. * p < 0.05 compared to sham group. # p < 0.05 compared to diabetes group
To further confirm the effect of berberine on MOR expression, we performed immunohistochemistry on spinal cord and DRG sections using MOR antibody (Fig. 6a) and found that, berberine treatment significantly increased the optical density of MOR (Fig. 6b) consistent with an increase in MOR expression. Similarly, insulin treatment had no effect on MOR expression.
Discussion
In this study, we investigated the effects of berberine in diabetic neuropathy in the STZ-induced diabetic rat model and the potential underlying molecular mechanism mediating these effects. Our study showed that berberine not only restored body weight and blood glucose levels but also suppressed hypersensitive thermal and mechanical nociception in diabetic rats. Additionally, our results revealed that berberine substantially suppresses neuroinflammation and oxidative stress in the DRGs and spinal of STZ-treated rats. Finally, we showed that MOR expression was suppressed by STZ administration and importantly, berberine significantly enhanced MOR protein and mRNA levels.
Diabetic neuropathy is a disabling severe complication of diabetes affecting approximately half of diabetic patients. There have been urgent needs for the development of therapeutics that are effective for diabetic neuropathy. Several animal models of diabetes have been established and phenotypes of diabetic neuropathy have been carefully characterized for the screening of effective therapeutic strategies (Biessels et al. 2014). In the STZ-induced diabetic model, not only the increased blood glucose levels and body weight loss are recapitulated, but the animals are also affected by neuropathic pain, making it an ideal model to study diabetic neuropathy. In this study, we confirmed STZ-induced diabetic neuropathy in rats by tests of mechanical and thermal nociception and also explored the optimal dosage of berberine in the alleviation of diabetic neuropathy in STZ-administered rats. Our study showed that while a low dose (5 mg/kg) of berberine did not affect diabetic neuropathy, higher doses (20 mg/kg and 40 mg/kg) substantially reduced the sensitivity of nociception, indicating an alleviation of neuropathic pain. Our study is consistent with the previous study showing a neuroprotective effect of berberine during the Morris water maze test in a rat model of diabetic neuropathy (Zhou et al. 2016) and our study further extended the neuroprotective effects on thermal and mechanical nociception in diabetic rats. Similar protective effects of berberine against neuropathic pain were also observed in a rat model of peripheral nerve injury (Yang et al. 2018). These studies, including ours, suggest that berberine may be beneficial for neuroprotection in general.
Oxidative stress is implicated in the pathogenesis of diabetes and lipid peroxidation has been shown to induce diabetic neuropathy (Low et al. 1997). Increased oxidative stress markers are found in various tissues of diabetic mice and rats induced by STZ including suppression of the activities of an antioxidant enzyme, induction of MDA in pancreatic tissue and increased levels of serum NO and treatment of diabetic rats with an antioxidant quercetin suppressed oxidative stress in the pancreas (Coskun et al. 2005). Similarly, increased oxidative stress is also detected in diabetic rat brain, suppression of which improved neurotrophic support (Ola et al. 2014). Consistent with roles of oxidative stress in diabetic neuropathy and the antioxidant effects of berberine, in this study we showed that accompanying alleviation in diabetic neuropathic pain, berberine treatment also reduced oxidative stress levels in the DRGs and spinal cord of diabetic rats.
Similar to oxidative stress, increased inflammation is also implicated in the pathogenesis of diabetes and is frequently studied together with oxidative stress. In the brain of diabetic rats induced by STZ, proinflammatory cytokine levels including IL-6, IL-1β, and TNF-α, which were suppressed by an anti-oxidative and anti-inflammatory flavonoid, morin leading to ameliorated diabetic encephalopathy (Ola et al. 2014). Similarly, increased levels of IL-1β and TNF-α were also detected in the DRG and sciatic nerve lysates of diabetic rats and suppression of these proinflammatory cytokine levels was associated with alleviation of neuropathic pain (Kiasalari et al. 2017). In this study, we confirmed STZ-induced inflammatory responses by examining TNF-α and IL-6 protein levels in the DRGs and spinal cord of diabetic rats and our results showed that these proinflammatory cytokines were upregulated in response to STZ administration. Importantly, our study showed that STZ-induced TNF-α and IL-6 protein expression in both DRGs and spinal cord was significantly suppressed by berberine treatment, indicating a role of berberine in the suppression of neuroinflammation in STZ-induced diabetic rats. Our findings are indeed consistent with known roles of berberine in the inhibition of oxidative stress and inflammation. While most previous studies examined the effects of berberine in the serum, liver, kidney, pancreas, heart, cortex, and hippocampus of diabetic animals (Li et al. 2014), we further explored the anti-oxidative stress and anti-neuroinflammation roles of berberine in the DRGs and spinal cord which are involved in the regulation of neuropathic pain.
Finally, in this study, we investigated the potential molecular mechanism underlying berberine mediated alleviation of diabetic neuropathic pain. Previously, it has been shown that decreased spinal cord MOR expression was associated with diabetic neuropathic pain (Kou et al. 2016). Consistent with this previous study, our study also showed a reduction in the protein and mRNA levels of MOR in both the DRGs and spinal cord of diabetic rats. Importantly, we detected a drastic increase of MOR expression in diabetic samples treated with berberine, consistent with a previous study showing berberine increased MOR expression in the cortical neurons rat embryos as well as the bowel of a mouse model of visceral pain (Chen et al. 2015). Our findings, together with the previous reports, suggest that berberine alleviates diabetic neuropathic pain through regulation of MOR expression. Although beyond the scope of our study, one future direction will be to further explore the connection between berberine and MOR in the management of diabetic neuropathy. Berberine has been shown to be able to cross the blood brain barrier after systemic administration and may thus directly play a role through MOR in the nervous system (Chen et al. 2015). Our study with the DRG and spinal cord confirms this possibility. Additionally, the reduction of pro-inflammatory cytokines including TNF-α and IL-6 in response to MOR activation observed in our model of diabetic neuropathy is consistent with a previous study showing an inhibitory effect of MOR agonists on cytokine production in a model of colitis and an increased expression of cytokine in animals with genetic deletion of the MOR gene (Anselmi et al. 2015). However, further studies are required to determine the exact molecular mechanism underlying berberine mediated effects on diabetic neuropathic pain.
One limitation of this study is that we only used one animal model to investigate the effects of berberine on diabetic neuropathic pain. Although beyond the scope of our current study, it will be important to confirm our finding in other diabetes models such as the db/db mice which carry mutations in leptin receptor and develop robust neuropathy including hyperalgesia and allodynia within 12 weeks prior to any clinical studies (O’Brien et al. 2014).
Conclusion
In summary, the results of our study indicate that berberine not only suppresses diabetic symptoms, but is also effective in alleviating diabetic neuropathy, making it an ideal therapeutic adjuvant for the treatment of this devastating complication of diabetes. Our study also indicates that these effects of berberine may involve the suppression of oxidative stress and inflammation and that restoration of MOR expression levels may be important for suppression of neuropathic pain. Although beyond the scope of this study, these important findings warrant further investigation on the berberine-MOR link for development treatments of diabetic neuropathy (van Beek et al. 2018).
References
Albers JW, Pop-Busui R (2014) Diabetic neuropathy: mechanisms, emerging treatments, and subtypes. Curr Neurol Neurosci Rep 14:473
Anselmi L, Huynh J, Duraffourd C, Jaramillo I, Vegezzi G, Saccani F, Boschetti E, Brecha NC, De Giorgio R, Sternini C (2015) Activation of mu opioid receptors modulates inflammation in acute experimental colitis. Neurogastroenterol Motil 27:509–523
Biessels GJ, Bril V, Calcutt NA, Cameron NE, Cotter MA, Dobrowsky R, Feldman EL, Fernyhough P, Jakobsen J, Malik RA, Mizisin AP, Oates PJ, Obrosova IG, Pop-Busui R, Russell JW, Sima AA, Stevens MJ, Schmidt RE, Tesfaye S, Veves A, Vinik AI, Wright DE, Yagihashi S, Yorek MA, Ziegler D, Zochodne DW (2014) Phenotyping animal models of diabetic neuropathy: a consensus statement of the diabetic neuropathy study group of the EASD (Neurodiab). J Peripher Nerv Syst 19:77–87
Caliceti C, Franco P, Spinozzi S, Roda A, Cicero AF (2016) Berberine: new insights from pharmacological aspects to clinical evidences in the management of metabolic disorders. Curr Med Chem 23:1460–1476
Chang W, Chen L, Hatch GM (2015) Berberine as a therapy for type 2 diabetes and its complications: from mechanism of action to clinical studies. Biochem Cell Biol 93:479–486
Chen C, Lu M, Pan Q, Fichna J, Zheng L, Wang K, Yu Z, Li Y, Li K, Song A, Liu Z, Song Z, Kreis M (2015) Berberine improves intestinal motility and visceral pain in the mouse models mimicking diarrhea-predominant irritable bowel syndrome (IBS-D) symptoms in an opioid-receptor dependent manner. PLoS One 10:e0145556
Coskun O, Kanter M, Korkmaz A, Oter S (2005) Quercetin, a flavonoid antioxidant, prevents and protects streptozotocin-induced oxidative stress and beta-cell damage in rat pancreas. Pharmacol Res 51:117–123
Javed S, Alam U, Malik RA (2015) Burning through the pain: treatments for diabetic neuropathy. Diabetes Obes Metab 17:1115–1125
Karlsson HK, Tuominen L, Tuulari JJ, Hirvonen J, Parkkola R, Helin S, Salminen P, Nuutila P, Nummenmaa L (2015) Obesity is associated with decreased mu-opioid but unaltered dopamine D2 receptor availability in the brain. J Neurosci 35:3959–3965
Kiasalari Z, Rahmani T, Mahmoudi N, Baluchnejadmojarad T, Roghani M (2017) Diosgenin ameliorates development of neuropathic pain in diabetic rats: involvement of oxidative stress and inflammation. Biomed Pharmacother 86:654–661
Kou ZZ, Wan FP, Bai Y, Li CY, Hu JC, Zhang GT, Zhang T, Chen T, Wang YY, Li H, Li YQ (2016) Decreased endomorphin-2 and mu-opioid receptor in the spinal cord are associated with painful diabetic neuropathy. Front Mol Neurosci 9:80
Li Z, Geng YN, Jiang JD, Kong WJ (2014) Antioxidant and anti-inflammatory activities of berberine in the treatment of diabetes mellitus. Evid Based Complement Alternat Med 2014:289264
Low PA, Nickander KK, Tritschler HJ (1997) The roles of oxidative stress and antioxidant treatment in experimental diabetic neuropathy. Diabetes 46(Suppl 2):S38–S42
Maffi P, Secchi A (2017) The burden of diabetes: emerging data. Dev Ophthalmol 60:1–5
Mao Y, Li Z, Chen K, Yu H, Zhang S, Jiang M, Ma Y, Liang C, Liu H, Li H, Hua Q, Zhou H, Sun Y, Fan X (2017) Antinociceptive effect of ghrelin in a rat model of irritable bowel syndrome involves TRPV1/opioid systems. Cell Physiol Biochem 43:518–530
Nathan DM (2015) Diabetes: advances in diagnosis and treatment. JAMA 314:1052–1062
O’Brien PD, Sakowski SA, Feldman EL (2014) Mouse models of diabetic neuropathy. ILAR J 54:259–272
Ola MS, Aleisa AM, Al-Rejaie SS, Abuohashish HM, Parmar MY, Alhomida AS, Ahmed MM (2014) Flavonoid, morin inhibits oxidative stress, inflammation and enhances neurotrophic support in the brain of streptozotocin-induced diabetic rats. Neurol Sci 35:1003–1008
Paisley P, Serpell M (2017) Improving pain control in diabetic neuropathy. Practitioner 261:23–26
Schiene K, Tzschentke TM, Schroder W, Christoph T (2015) Mechanical hyperalgesia in rats with diabetic polyneuropathy is selectively inhibited by local peripheral nociceptin/orphanin FQ receptor and micro-opioid receptor agonism. Eur J Pharmacol 754:61–65
Toth C (2014) Diabetes and neurodegeneration in the brain. Handb Clin Neurol 126:489–511
Valsecchi AE, Franchi S, Panerai AE, Rossi A, Sacerdote P, Colleoni M (2011) The soy isoflavone genistein reverses oxidative and inflammatory state, neuropathic pain, neurotrophic and vasculature deficits in diabetes mouse model. Eur J Pharmacol 650:694–702
van Beek M, Geurts JW, Slangen R, Schaper NC, Faber CG, Joosten EA, Dirksen CD, van Dongen RT, van Kuijk SMJ, van Kleef M (2018) Severity of neuropathy is associated with long-term spinal cord stimulation outcome in painful diabetic peripheral neuropathy: five-year follow-up of a prospective two-center clinical trial. Diabetes Care 41:32–38
Wan FP, Bai Y, Kou ZZ, Zhang T, Li H, Wang YY, Li YQ (2016) Endomorphin-2 inhibition of substance P signaling within Lamina I of the spinal cord is impaired in diabetic neuropathic pain rats. Front Mol Neurosci 9:167
Wong TY, Cheung CM, Larsen M, Sharma S, Simo R (2016) Diabetic retinopathy. Nat Rev Dis Primers 2:16012
Yang S, Yu Z, Sun W, Jiang C, Ba X, Zhou Q, Xiong D, Xiao L, Deng Q, Hao Y (2018) The antiviral alkaloid berberine ameliorates neuropathic pain in rats with peripheral nerve injury. Acta Neurol Belg. https://doi.org/10.1007/s13760-018-1006-9
Zan Y, Kuai CX, Qiu ZX, Huang F (2017) Berberine ameliorates diabetic neuropathy: TRPV1 modulation by PKC pathway. Am J Chin Med 45:1709–1723
Zhao X, Li XL, Liu X, Wang C, Zhou DS, Ma Q, Zhou WH, Hu ZY (2015) Antinociceptive effects of fisetin against diabetic neuropathic pain in mice: engagement of antioxidant mechanisms and spinal GABAA receptors. Pharmacol Res 102:286–297
Zhou J, Du X, Long M, Zhang Z, Zhou S, Zhou J, Qian G (2016) Neuroprotective effect of berberine is mediated by MAPK signaling pathway in experimental diabetic neuropathy in rats. Eur J Pharmacol 774:87–94
Zhu L, Han J, Yuan R, Xue L, Pang W (2018) Berberine ameliorates diabetic nephropathy by inhibiting TLR4/NF-kappaB pathway. Biol Res 51:9
Author contribution statement
Jun Dong and Zhongfu Zuo contributed equally to this work. Jun Dong, Zhongfu Zuo, Wei Yan, and Wenqiang Liu conceived and designed research. Wenqiang Liu, and Qingyu Zheng analyzed data. Jun Dong and Xuezheng Liu wrote the manuscript. All authors read and approved the manuscript.
Funding
The study was supported by the National Natural Science Foundation of China (81571383); China Postdoctoral Science Foundation (2017 M612870); and Program for Liaoning Excellent Talents in University (LJQ2015069).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dong, J., Zuo, Z., Yan, W. et al. Berberine ameliorates diabetic neuropathic pain in a rat model: involvement of oxidative stress, inflammation, and μ-opioid receptors. Naunyn-Schmiedeberg's Arch Pharmacol 392, 1141–1149 (2019). https://doi.org/10.1007/s00210-019-01659-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-019-01659-6