Abstract
Painful diabetic neuropathy (PDN) is known to adversely affect psychosocial functioning by enhancing levels of anxiety and depression. This study was designed to verify the antihypernociceptive, anxiolytic, and antidepressant-like effects of Combretin A and Combretin B (two triterpenes cycloartane-type isolated from the leaves of Combretum fragrans) in streptozotocin-induced diabetic neuropathy in mice. PDN was induced in mice by the administration of streptozotocin (STZ, 200 mg/kg, i.p.). The effect of oral administration of Combretin A (25 and 50 mg/kg) and Combretin B (25 and 50 mg/kg) on nociception (mechanical allodynia, thermal hyperalgesia, cold allodynia, and chemical hyperalgesia), anxiety (elevated plus maze, light-dark box test, social interaction), and depressant (open field test, forced swimming test, tail suspension test) was evaluated. Combretin A (25 and 50 mg/kg) and Combretin B (25 and 50 mg/kg) caused antihypernociceptive, anxiolytic, and antidepressant-like effects in in STZ-induced diabetic neuropathy in mice. Both compounds also caused a decrease in blood glucose and improved body weight in treated animals. They also significantly (p < 0.001) reduced tumor necrosis factor alpha (TNF-α), interleukin-1 beta (IL-1β), malondialdehyde (MDA), and nitric oxide (NO) production in serum and sciatic nerves, and, significantly (p < 0.001) increased superoxide dismutase (SOD) and catalase (CAT) activity in serum, sciatic nerves, and brain. Combretin A and Combretin B also showed a great systemic effect, conserving values of evaluated parameters close to normal in treated mice. The results of this study confirm the antihypernociceptive, antianxiety, and antidepressant activities of Combretin A and Combretin B.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pain is a subjective process, which aims to protect a living organism against all unpleasant stimulations. Acute pain with its unpleasant perception as well as chronic pain with its emotional experience have turned the painful process into an entire disease that requires immediate relief nowadays (Nguelefack et al. 2015). Because chronic inflammatory pain seriously affects people’s daily activities while deeply reducing the quality of life, it remains the toughest challenge to solve in medicine (Orrù et al. 2014). In addition, unresolved persistent pain results in the development of a state of anxiety, depression, loss of independence, and decreased activity in patients while creating a prolonged vicious circle that worsens its state. Chronic pain has a negative emotional component and is strictly correlated to anxiety and depression (Nguelefack et al. 2015; Dworkin and Gitlin 1991).
Serious lesion and/or disease that may affect the peripheral nervous system may cause development of peripheral neuropathic pain. This is the case of approximately 25 to 30% of people suffering from diabetes mellitus (Treede et al. 2008; Daousi et al. 2004; Davies et al. 2006). Complex and multidimensional damage, painful diabetic neuropathy (PDN) considered as the most problematic type of chronic pain to treat, frequent and affecting up to 50% of patients, which predisposes to severe functional limitations both physically and mentally, is characterized by hyperalgesia and allodynia (Barrett et al. 2007; Boulton et al. 2000; Vileikyte et al. 2005; Baron et al. 2010; Leung and Cahill 2010). Experimentally in animals, PDN is a good model of neuropathic pain with rapid and prolonged development of mechanical and thermal hypersensitivity (Decosterd and Woolf 2000). Many patients with PDN are known to have a state of anxiety and depression, in addition to 60 to 90% of depressed patients report pain, it can be said that chronic pain is accompanied by a state of depression and anxiety (Vileikyte et al. 2005; Leo 2005).
In diabetic patients, multiple behaviors (smoking, alcoholism, drug abuse, poorer eating, and appetite dysregulation) are related to the development of a state of anxiety and depression with consequent onset of diabetic retinopathy, macrovascular complications, neuropathy, nephropathy, and sexual dysfunction (Gonder-Frederick et al. 2002; De Groot et al. 2001). Thus, anxiety and depression represent important comorbidity of PDN whose severity depends on the intensity of the pain (Lloyd et al. 1991; Dyck et al. 1997; Chan et al. 1990). Thereby, the evaluation of pain as well as the symptoms of anxiety and depression should be performed simultaneously in an animal model (Hache et al. 2012).
Combretin A and Combretin B isolated from the MeOH extract of the leaves of Combretum fragrans (Combretaceae) are two cycloartane-type triterpenes (Dawe et al. 2016), who have already shown antiinflammatory, antinociceptive, and anticancer potential linked with inhibitory properties on reactive oxygen species (ROS), NO, and TNFα production (Mbiantcha et al. 2017). Triterpenoids are a very large class of compounds that are widely distributed in the plant kingdom (Hanson 2003) and that possess several pharmacological properties among which analgesic, antiinflammatory, antianxiety, and antidepressant properties (Calixto et al. 2000; Moroney et al. 1988; Bortalanza et al. 2002; Subarnas et al. 1993; Durst et al. 2002; Herrera-Ruiza et al. 2006; Morris et al. 2006). Given the fact that Combretin A and Combretin B are two newly identified triterpenes (Dawe et al. 2016), no scientific work has yet shown their antihyperalgesic and neuropharmacological properties. Hence, the current study was aimed to investigate the antihyperalgesic, antidepressant, and antianxiety enhanced effects of these two compounds.
Materials and methods
Plant material
The fresh leaves of Combretum fragrans were collected from the Far-North Region (Maroua, Cameroon). After the harvest, the plant was identified by Mr. Victor Nana, a botanist at the Cameroonian National Herbarium in Yaounde where a specimen is kept under the number 30309/H.N.C. (Dawe et al. 2016).
Extraction and isolation
After drying (in the shade) of 1.2 kg of the leaves of Combretum fragrans, these leaves were crushed and macerated (at room temperature) in 10 l of methanol (MeOH). One hundred twenty-six grams of residue obtained after concentration (solvent removal) was suspended in water (H2O) and extracted successively with hexane, AcOEt, and BuOH. From conventional separation procedures (CC, HPLC, Preparative TLC, etc), six (6) compounds among which 126 mg of Combretin A and 114 mg of Combretin B (Fig. 1) were isolated from the AcOEt-soluble fraction (48 g). The usual spectroscopic techniques (UV, IR, MS, 1D, and 2D NMR) followed by comparison with certain physical and spectral data described in the literature have made it possible to elucidate the structures of the different compounds (Dawe et al. 2016).
Drugs and reagents
The following chemicals were obtained from Sigma: Streptozoticin (STZ), pregabalin (PGB), fluoxetine, and diazepam. All other elements were of analytical grade and were obtained from the local supplier. Pregabalin, fluoxetine, and diazepam were prepared in normal saline (0.9%). The mixture of 2.5% DMSO and 2.5% tween 80 was used to dissolve Combretin A and Combretin B.
Experimental animals
To demonstrate the coherent effects of our different compounds, the minimum possible of animals as the intensity of nociceptive stimuli was used. All tests were achieved using mature male and female mice (3 months old; 25–35 g), bred in the animal house facility (controlled temperature (22 ± 1 °C); 12 h light/12 h dark cycle with standard lab chow and water ad libitum) of the National Institute of Health (NIH), Islamabad, Pakistan. The treatment of animals was in agreement with the Institutional Animal Care, Use and Standards Committee (IACUC) of National Institute of Health, and the study protocols accepted by the Ethics Committee of the National Institute of Health, Islamabad, Pakistan.
Induction of experimental diabetes by streptozotocin
To produce experimental diabetes, streptozotocin (200 mg/kg) were intraperitoneally injected in mice (Kamei et al. 1991; Sánchez-Ramírez et al. 2006), while 0.9% of saline solution was injected into control animals. Three (3) days after streptozotocin injection, diabetes was confirmed by measuring blood glucose from a drop of blood obtained from the tail vein of each animal using the Glucometer Accu-Chek Performa (Roche Diabetes Care, Inc., Indianapolis, USA) as a measuring device. After selecting only mice with a glycemic level ≥ 300 mg/dL for our study, treatment started 2 weeks after streptozotocin injection and lasted 4 weeks during this time; mechanical allodynia (Von Frey filament), thermal hyperalgesia (hotplate), and cold allodynia (acetone) were performed every week.
Antinociceptive activity
For this study, 36 diabetic and 6 non-diabetic mice were selected, divided into 7 groups including six animals each. Group 1 (non-diabetic mice) received no treatment; group 2 (diabetic mice) received mixture of 2.5% DMSO and 2.5% Tween 80 (per os); group 3 (diabetic mice) received pregabalin (30 mg/kg, per os); groups 4 and 5 (diabetic mice) received Combretin A (25 and 50 mg/kg, per os); and groups 6 and 7 (diabetic mice) received Combretin B (25 and 50 mg/kg, per os).
Assessment of mechanical allodynia
A metal grid served as support for this test. Indeed, after 25 min period of acclimatization in their environment, mechanical allodynia was tested by stimulation of the plantar surface of animals.
A series of eight calibrated von Frey nylon hairs (0.04, 0.07, 0.16, 0.4, 0.6, 1, 1.4, and 2 g) was used to evaluate mechanical allodynia. The filaments were applied in ascending or descending order sequentially on the plantar surface. A positive response made by rapid withdrawal or flinching made it possible to switch to the lightest filament, while a negative answer allowed using the next heaviest filament. The up-down method previously described by Chaplan et al. (1994) and Li et al. (2000) was used to determine the 50% withdrawal threshold.
Assessment of thermal hyperalgesia
Stable temperature (54 ± 1 °C) hot-plate apparatus (Ugo-Basile, Varese, Italy), with a cutoff time approximately 12 s, was used to evaluate the susceptibility of mice to heat. After placing each mouse on the hot plate, the reaction time was recorded from the moment the animal licked its paw and made a jump (Biella et al. 2003).
Assessment of cold allodynia
To evaluate the reaction of diabetic mice to cold stimulus, acetone was applied five times at 5 min intervals on the plantar surface. Cold allodynia was considered when the animal reacted by rapid withdrawal to two out of five applications representing 40% (Li et al. 2000).
Sample collections
On the 30th day, the animals were sacrificed under deep chloroform vapor anesthesia, then by cardiac puncture the blood was taken from a syringe, allowed to coagulate and submitted to 15 min centrifugation at 3000 rpm, then the serum was taken with a pipette and placed in a dry tube for analysis. Whole spinal cord and brain were immediately removed and crushed in phosphate buffer saline (PBS) due to 0.1 g of organ per 1 ml of buffer, centrifuged at 3000 rpm during 15 min (4 °C) using an Eppendorf 5804 R, Hamburg centrifuge and the supernatants were collected for analysis (Fatani et al. 2015).
Serum and tissue parameters
TNF-α (tumor necrosis factor-α) and IL-1β concentrations have been evaluated in serum and spinal cord supernatant by using enzyme-linked immunosorbent assay kit provided by Elabscience Biotechnology Inc. (China) (Fatani et al. 2015).
The MDA and NO levels, as the SOD and catalase (CAT) activities, were measured in serum, brain supernatant, and spinal cord supernatant by an assay kit (Elabscience Biotechnology Inc., China), ALT, AST, and ALP activities and protein level were measured in the serum and the liver supernatant, while the creatinine level was measured in the serum by an assay kit (MDT DIAGNOSTICS Srl. Maddaloni (CE), Italy).
Neuropharmacological investigation of Combretin A and Combretin B
In order to determine the neuropharmacological properties of the compounds, the diabetic mice were subjected to various tests to evaluate the anxiolytic and antidepressant activities.
Assessment for antianxiety activity
For this study, 36 diabetic and 6 non-diabetic mice were selected and divided into seven (7) groups of six animals each. Group I, normal control (non-diabetic group); group II, diabetic control (mixture of 2.5% DMSO and 2.5% Tween 80); group III (diabetic group), diazepam (1 mg/kg, i.p.); groups IV and V (diabetic group), Combretin A (25 and 50 mg/kg, p.o.); groups VI and VII (diabetic group), Combretin B (25 and 50 mg/kg, p.o.). In 28 days, the animals were milked daily and the parameters were evaluated weekly. The mice were used only once in each behavioral test.
Elevated plus maze test
The plus maze apparatus is a labyrinth with a height of 25 cm, consists of two open arms (16 × 5 cm) and two firm arms (16 × 5 × 12 cm) connected by a central platform of 5 × 5 cm. To carry out this test, each mouse is placed in the center of the labyrinth (head turned towards an open arm), then the animal was observed for a period of 5 min during which time is noted in the arms open and close (Bhattamisra et al. 2007). The percentage of time spent in each arm is determined by the formula below:
where SS = seconds spent and TS = total seconds (300 s equal to 5 min).
Light-dark box test
A box of rectangular shape (45 × 27 × 27 cm) possessing two compartments (illuminated and unlit) separated by a wall leaving an aperture of 7.5 × 7.5 cm was used for this test. After placing each mouse in the center of the illuminated compartment, the animal was observed for 5 min during which the time spent in this compartment was noted (Crawley and Goodwin 1980; File 1996). The formula below has been used to determine the:
where SSLC = seconds spent in light compartment and TS = total seconds (300 s equal to 5 min).
Social interaction test
A completely open box (22 × 15 × 12 cm) was used to carry out this test. Each animal receiving the treatment was isolated for 1 h, then introduced into the box with another mouse that has not received any treatment. Then the two animals were observed for genital investigation, following, sniffing a partner, grooming, biting, kicking, wrestling, neck licking and boxing, and climbing over and under during a period of 5 min (File 1996).
Assessment of antidepressant activity
For this study, 36 diabetic and 6 non-diabetic mice were selected and divided into seven (7) groups of six animals each. The animals were treated as in the previous test with the only difference that the positive control in this test received fluoxetine (5 mg/kg) as a treatment. The forced swimming test (FST), tail suspension test (TST), and open field test (OFT) were conducted every week during 4 weeks. The mice were used only once in each behavioral test.
Open field test
A rectangular box (40 × 60 × 50 cm) with a surface divided into 12 equal rectangles was used to perform this test allowing the effects of the compounds on the exploratory and locomotor activities of mice. During this test for each animal, one crossing (considered locomotor activity) was counted when a side of a rectangle was crossed by the four legs of the animal while one rearing (considered as exploratory activity) was counted when the animal was standing on both hind legs during 5 min (Felipe et al. 2007). Any olfactory sign of an animal was eliminated by cleaning the open field with ethanol 10%.
Forced swimming test
A cylindrical container 10 cm in diameter and 25 cm in height containing 19 cm of water maintained at 25 ± 1 °C was used for this test. Each mouse was placed individually in the container for 5 min and the total duration of immobility (when the animal floats stops struggling and only moves to keep the head out of the water) was recorded for each animal during this period (Porsolt et al. 1977).
Tail suspension test
The method described by Steru et al. (1985) for evaluating the immobility time of a mouse suspended by the tail at a gallows was used for this test. Indeed at 50 cm above the ground and with the help of a fixed adhesive tape about 1 cm from the end of the tail, each mouse was suspended by the tail, then the total duration of immobility of each animal was noted during a period of 5 min.
Statistical analysis
Mean ± standard error of mean (SEM) have been used to present the data. Differences between groups were evaluated by analyses of variance (one-way and two ways ANOVA) followed by the Bonferroni post-test. One-way and two ways ANOVA followed by the Bonferroni post-test have been used to evaluate differences between groups. At p < 0.05, the differences were significant and were materialized by a, b, and c against the normal control and α, β, and λ against negative control.
Results
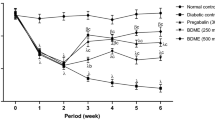
Effect of Combretin A and Combretin B mechanical allodynia, thermal hyperalgesia, and cold allodynia in STZ-induced diabetic pain
In normal animals that received no treatment, the mean value of maximal mechanical stimulation was approximately 13.50 g to cause a positive reaction of the animal. After injection of STZ, this mean value significantly decreased (p < 0.001) and in a time-dependent manner (Fig. 2a). Treatment with Combretin A and Combretin B (25 and 50 mg/kg) reduced STZ-induced mechanical allodynia significantly (p < 0.05, p < 0.01, p < 0.001) during the testing period (up to 4 weeks). Combretin A (50 mg/kg) reduced this pain to 64.06% at the fourth week, while Combretin B at the same dose reduced the pain to 78.26% at the sixth week. Pregabalin (30 mg/kg) reduces the pain to 65.59% at the fourth week.
Antihyperalgesic effect of Combretin A and Combretin B on mechanical allodynia (a), thermal hyperalgesia (b), and cold allodynia (c) induced by von frey filament, hot plate (54 ± 1 °C), and acetone, respectively. Data are expressed as the mean ± SEM of six animals per experimental group. ap < 0.05, bp < 0.01, cp < 0.001 significantly different from the normal control group (no diabetic) and αp < 0.05, βp < 0.01, λp < 0.001 significantly different from the diabetic control group, as determined by analysis of variance followed by Bonferroni’s test
Concerning the noxious thermal stimuli induced by the hot-plate (54 ± 1 °C) in STZ-treated mice, the paw withdrawal latency was significantly reduced (p < 0.001) from 2 to 4 weeks after administration. Treatment with Combretin A (25 and 50 mg/kg), Combretin B (25 and 50 mg/kg), and pregabalin (30 mg/kg) significantly (p < 0.05, p < 0.01, p < 0.001) affects STZ-induced noxious thermal hyperalgesia (Fig. 2b). Maximal inhibitions were observed at week 4 with 76.05%, 46.98%, and 45.68% respectively for Combretin A (50 mg/kg), Combretin B (50 mg/kg), and pregabalin (30 mg/kg).
Cold allodynia developed in mice 1 week after STZ injection and remained stable until the fourth week. The withdrawal response to cold stimuli was significantly (p < 0.05, p < 0.01, p < 0.001) increased in the STZ-treated mice (Fig. 2c). At the dose of 50 mg/kg, Combretin A and Combretin B inhibited the pain to 78.57% and 92.86% respectively at the fifth week, while pregabalin (30 mg/kg) at the same time induced an inhibition of 71.43%.
Effects of Combretin A and Combretin B of blood glucose and body weight in STZ-induced diabetic pain
After streptozotocin injection, blood glucose increased significantly (p < 0.001) and body weight decreased significantly (p < 0.001) in all animals compared to the normal control (Tables 1 and 2). In diabetic mice treated with different doses of Combretin A and Combretin B, glycemia level was significantly (p < 0.001) reduced compared with animals in the diabetic control group. However, likewise after treatment of animals with Combretin A and Combretin B, the body weight of the animals increased significantly (p < 0.001) compared to the mice of the diabetic control group.
Effects of Combretin A and Combretin B on levels of proinflammatory cytokines in diabetic mice
Compared to animals in the normal control group, TNF-α, and IL-1β levels significantly (p < 0.001) increased in the serum and sciatic nerve of untreated diabetic mice, while in animals receiving treatment these pro-inflammatory mediators decreased significantly compared to untreated diabetic mice. Combretin A and Combretin B (25 and 50 mg/kg) exhibited significant (p < 0.05, p < 0.01, p < 0.001) attenuated elevated levels of IL-1β and TNF-α in the serum and sciatic nerve when compared with the untreated diabetic mice (Figs. 3 and 4).
Effects of Combretin A and Combretin B on the levels of TNF-α (a) and IL-1β (b) in the serum of diabetic mice. Data are expressed as the mean ± standard error of the mean (n = 6) and were analyzed using one-way analysis of variance followed by the Bonferroni’s post hoc test. cp < 0.001 significantly different from the normal control group and αp < 0.05, βp < 0.01, λp < 0.001 significantly different from the diabetic control group. NC normal control, DC diabetic control, PGB30 mice received 30 mg/kg/day pregabalin, CA25 mice received 25 mg/kg/day Combretin A, CA50 mice received 50 mg/kg/day Combretin A, CB25 mice received 25 mg/kg/day Combretin B, CB50 mice received 50 mg/kg/day Combretin B, TNF tumor necrosis factor, IL interleukin
Effects of Combretin A and Combretin B on the levels of TNF-α (a) and IL-1β (b) in the sciatic nerves of diabetic mice. Data are expressed as the mean ± standard error of the mean (n = 6) and were analyzed using one-way analysis of variance followed by the Bonferroni post hoc test. cp < 0.001 significantly different from the normal control group and αp < 0.05, βp < 0.01, λp < 0.001 significantly different from the diabetic control group. NC normal control, DC diabetic control, PGB30 mice received 30 mg/kg/day pregabalin, CA25 mice received 25 mg/kg/day Combretin A, CA50 mice received 50 mg/kg/day Combretin A, CB25 mice received 25 mg/kg/day Combretin B, CB50 mice received 50 mg/kg/day Combretin B, TNF tumor necrosis factor, IL interleukin
Effects of Combretin A and Combretin B on oxidative stress bio-markers in diabetic mice
MDA and NO levels significantly (p < 0.001) increased in serum sciatic nerve and brain tissue in animals after diabetes induction. Furthermore, the diabetic mice exhibited lower enzymatic activity levels of SOD (p < 0.001) and CAT (p < 0.001) when compared with the normal control group. Combretin A (25 and 50 mg/kg), Combretin B (25 and 50 mg/kg), and pregabalin (30 mg/kg) group mice exhibited significant (p < 0.05, p < 0.01, and p < 0.001) inhibition of the diabetes-induced elevation of MDA and NO in the serum, sciatic nerve, and brain tissue. Additionally, the inhibited antioxidant enzymatic activity levels of SOD and CAT were markedly improved (p < 0.05, p < 0.01, and p < 0.001) in the treated group of mice (Figs. 5, 6, and 7).
Effects of Combretin A and Combretin B on the enzymatic activity levels of SOD (a), CAT (b), and MDA (c), and on the levels of NO (d) in the serum of diabetic mice. Data are expressed as the mean ± standard error of the mean (n = 6) and were analyzed using one-way analysis of variance followed by the Bonferroni post hoc test. bp < 0.01, cp < 0.001 significantly different from the normal control group and αp < 0.05, βp < 0.01, λp < 0.001 significantly different from the diabetic control group. NC normal control, DC diabetic control, PGB30 mice received 30 mg/kg/day pregabalin, CA25 mice received 25 mg/kg/day Combretin A, CA50 mice received 50 mg/kg/day Combretin A, CB25 mice received 25 mg/kg/day Combretin B, CB50 mice received 50 mg/kg/day Combretin B, SOD superoxide dismutase, CAT catalase, MDA malondialdehyde, NO nitric oxide
Effects of Combretin A and Combretin B on the enzymatic activity levels of SOD (a), CAT (b), and MDA (c), and on the levels of NO (d) in the sciatic nerve of diabetic mice. Data are expressed as the mean ± standard error of the mean (n = 6) and were analyzed using one-way analysis of variance followed by the Bonferroni post hoc test. ap < 0.05, cp < 0.001 significantly different from the normal control group and βp < 0.01, λp < 0.001 significantly different from the diabetic control group. NC normal control, DC diabetic control, PGB30 mice received 30 mg/kg/day pregabalin, CA25 mice received 25 mg/kg/day Combretin A, CA50 mice received 50 mg/kg/day Combretin A, CB25 mice received 25 mg/kg/day Combretin B, CB50 mice received 50 mg/kg/day Combretin B, SOD superoxide dismutase, CAT catalase, MDA malondialdehyde, NO nitric oxide
Effects of Combretin A and Combretin B on the enzymatic activity levels of SOD (a), CAT (b), and MDA (c), and on the levels of NO (d) in the brain of diabetic mice. Data are expressed as the mean ± standard error of the mean (n = 6) and were analyzed using one-way analysis of variance followed by the Bonferroni’s post hoc test.ap < 0.05, bp < 0.01, cp < 0.001 significantly different from the normal control group and αp < 0.05, βp < 0.01, λp < 0.001 significantly different from the diabetic control group. NC normal control, DC diabetic control, PGB30 mice received 30 mg/kg/day pregabalin, CA25 mice received 25 mg/kg/day Combretin A, CA50 mice received 50 mg/kg/day Combretin A, CB25 mice received 25 mg/kg/day Combretin B, CB50 mice received 50 mg/kg/day Combretin B, SOD superoxide dismutase, CAT catalase, MDA malondialdehyde, NO nitric oxide
Effects of Combretin A and Combretin B on biochemical parameters in diabetic mice
Table 3 shows the effects of Combretin A and Combretin B on some parameters of liver and kidney functions. It appears that, there was a significant increase (p < 0.001) in ALT, AST, and ALP activities and creatinine concentration, and significant (p < 0.01) decrease of total proteins in diabetic mice (untreated) as compared to normal control. In all animals treated at different doses of Combretin A and Combretin B, the results show a significant improvement in all the parameters evaluated, a decrease of the creatinine level and the activity of the enzymes (ALT, AST, and ALP) followed by an increase in total protein level.
Neuropharmacological investigation
Antianxiety activities
As shown in Fig. 8, treatment with Combretin A and Combretin B at doses of 25 or 50 mg/kg, p.o., induced a relaxing effect in mice when assessed by the elevated plus maze test (EPMT). The results showed the important (p < 0.05, p < 0.001) increase of the time the animals remained in the open arms and the significant (p < 0.01, p < 0.001) decrease of the time spent in the closed arms when compared with the controls (Fig. 8a and b). This activity was observed throughout the course of treatment. Diazepam (1 mg/kg, i.p.), used as a positive control, produced a statistically significant (p < 0.05, p < 0.01) increase of the time spent in the open arms starting from the second week of treatment, and significantly (p < 0.05, p < 0.01) decreasing the time spent in the closed arms from the third week of treatment.
Effects of Combretin A and Combretin B in the absolute time spent in the open arms (a) and closed arms (b) during 6 min of exposure to the elevated plus maze. Data are expressed as the mean ± SEM of six animals per experimental group. ap < 0.05, bp < 0.01, cp < 0.001 significantly different from the normal control group (no diabetic) and λp < 0.001 significantly different from the diabetic control group, as determined by analysis of variance followed by Bonferroni’s test
The light-dark box test results shown in Fig. 9 show that untreated diabetic mice have spent very little time in the illuminated area and this time is significantly (p < 0.001) reduced compared to non-diabetic mice. The treatment of diabetic mice by the different doses of Combretin A (25 or 50 mg/kg), Combretin B (25 or 50 mg/kg), and diazepam (1 mg/kg) increased significantly (p < 0.05, p < 0.01, and p < 0.001) the time passed in the illuminated area compared to treated non-diabetic mice.
Effects of Combretin A and Combretin B in the absolute time spent in the open (white/light) compartment during 5 min of exposure to the light-dark box test. Data are expressed as the mean ± SEM of six animals per experimental group. ap < 0.05, bp < 0.01, cp < 0.001 significantly different from the normal control group (no diabetic) and λp < 0.001 significantly different from the diabetic control group, as determined by analysis of variance followed by Bonferroni’s test
Regarding social interaction, the results show that all diabetic animals show a significant (p < 0.001) decrease in this parameter compared to non-diabetic animals. The treatment of mice at the tested doses of Combretin A and Combretin B significantly (p < 0.01, p < 0.001) improved the social interaction in a dose-dependent manner from the first week to the fourth week. Diazepam at the dose of 1 mg/kg produced an improvement significantly (p < 0.01) improvement only at the second and third weeks of treatment (Fig. 10).
Effects of Combretin A and Combretin B in the absolute time for social interaction during 5 min. Data are expressed as the mean ± SEM of six animals per experimental group. ap < 0.05, bp < 0.01, cp < 0.001 significantly different from the normal control group (no diabetic) and λp < 0.001 significantly different from the diabetic control group, as determined by analysis of variance followed by Bonferroni’s test
Antidepressant activities
In the open-field test, all diabetic animals presented an important decrease of the number of crossing and rearings (Fig. 11a and b). All treatments with Combretin A (25 or 50 mg/kg), Combretin B (25 mg/kg), and fluoxetine (5 mg/kg) did not alter significantly the number of rearings comparatively to control group. Moreover, mice treated with Combretin B (50 mg/kg) exhibited significant (p < 0.05, p < 0.01) alterations in the number of crossings during 4 weeks of treatment when compared with the control group.
Effects of Combretin A and Combretin B on the locomotor activity of mice in the OFT during 5 min. Data are expressed as the mean ± SEM of six animals per experimental group. ap < 0.05, bp < 0.01, cp < 0.001 significantly different from the normal control group (no diabetic) and αp < 0.05, βp < 0.01, λp < 0.001 significantly different from the diabetic control group, as determined by analysis of variance followed by Bonferroni’s test
The effects of Combretin A, Combretin B, and fluoxetine on the immobility time of mice in FST are shown in Fig. 12. During the 4-week treatment, Combretin A (25 and 50 mg/kg) and Combretin B (25 and 50 mg/kg) produced a significant (p < 0.001) decrease in the duration of immobility during the 4 weeks. In addition, fluoxetine (5 mg/kg) significantly (p < 0.05, p < 0.01) decreased the immobility time only for the last 3 weeks.
Effects of Combretin A and Combretin B on the immobility time of mice in the FST during 5 min. Data are expressed as the mean ± SEM of six animals per experimental group. ap < 0.05, bp < 0.01, cp < 0.001 significantly different from the normal control group (no diabetic) and λp < 0.001 significantly different from the diabetic control group, as determined by analysis of variance followed by Bonferroni’s test
Concerning the effects of Combretin A, Combretin B, and fluoxetine on the immobility time of mice in tail suspension test, Fig. 13 indicated a significant (p < 0.05, p < 0.01, p < 0.001) treatment effect observed on all weeks for Combretin A (p < 0.001) and Combretin B (p < 0.001), and last 3 weeks for fluoxetine (p < 0.05, p < 0.01).
Effects of Combretin A and Combretin B on the immobility time of mice in the TST during 5 min. Data are expressed as the mean ± SEM of six animals per experimental group. ap < 0.05, bp < 0.01, cp < 0.001 significantly different from the normal control group (no diabetic) and αp < 0.05, βp < 0.01, λp < 0.001 significantly different from the diabetic control group, as determined by analysis of variance followed by Bonferroni’s test
Discussion
The therapeutic potential of Combretin A and Combretin B, two new cycloartane-type triterpenes isolated from Combretum fragrans (combretaceae), were evaluated in the treatment of streptozotocin-induced painful peripheral neuropathy in rodent associated with antidepressant and anxiolytic-like effects. In our previous studies, these two compounds showed in vitro inhibitory activities on human cancer cell lines (MCF-7 cells), TNFα, ROS, and NO production, as well as an analgesic and acute antiinflammatory activity in vivo (Mbiantcha et al. 2017).
Diabetes mellitus is an evolutive pathology with the most common consequence being the appearance of neuropathic pain that occurs in more than half of diabetic patients and is manifested by spontaneous hyperalgesia and allodynia (Apfel et al. 2001). Symptoms such as hyperalgesia and allodynia materializing chronic neuropathic pain observed in patients with diabetes mellitus also are observed in the STZ-induced diabetic animal model (Gul et al. 2000; Kamei et al. 2001). In the present study, in diabetic mice, mechanical allodynia, thermal hyperalgesia, cold allodynia, and chemical hyperalgesia was significantly modified than that observed in normal control animals, showing development of neuropathic pain. This was accompanied by the development of depressant and anxiety symptoms as assessed by performance on EPMT, light-dark box test (LDBT), social interaction test (SIT), OFT, FST, and TST.
To evaluate the effects of potential analgesic substances, STZ-induced diabetic mice are frequently used as a prototype of painful diabetic neuropathy since these animals exhibit hyperalgesic behavior in response to harmful stimuli (Hasanein and Soltani 2009; Hasanein et al. 2009). Furthermore, according to a recent paper, Combretin A and Combretin B at the same doses used in this study induced antinociceptive affect in acetic acid and formalin-induced pain in normal mice (Mbiantcha et al. 2017). The results of this work clearly show, for the first time that long-term Combretin A and Combretin B administration by the oral route produced an important antihyperalgesic and antiallodynic properties in a mice classic of diabetic neuropathy. In addition, the antineuropathic effect of these compounds was equieffective to pregabalin, known for its use in the treatment of neuropathic pain (Dworkin et al. 2010; Vranken 2012).
Diabetic neuropathy presents a very complex physiopathology with the development of oxidative stress, hyperglycemia, and inflammatory damage (Calcutt 2004). In this study, injection of STZ into healthy mice causes a significant increase in blood glucose in all animals and this hyperglycemia was maintained during the experimental period of several weeks. Interestingly, the antihyperalgesic and antiallodynic effects of Combretin A and Combretin B in diabetic animals are accompanied by significant decrease in serum glucose level, as compared with the untreated diabetic mice. Therefore, the interesting antihyperalgesic effect of these compounds in diabetic mice may be related to the decrease of this factor.
The hyperglycemia that develops during DN induces the installation of oxidative stress by release of superoxide and hydroxyl radicals following autoxidation of proteins and monosaccharides (Bolajoko et al. 2008; Julius et al. 2009), leading to the production of hydroxyl radicals and superoxide. In diabetic animals induced by STZ, the development of hyperglycemia causes a non-enzymatic glycosylation responsible for the decrease of the activity of antioxidative enzymes; this decrease in enzymatic activity would be more pronounced in the sciatic nerve, which justifies the fact that the nerve cells of the sciatic nerve are more sensitive and very vulnerable to the changes resulting from the oxidative stress caused by the installation of hyperglycemia (Halliwell 1991; Fatani et al. 2015). In protecting the body against oxidative stress, several enzymes are involved among which SOD which converts superoxide anions (O2.-) in H2O2 and CAT which degrades H2O2 to give O2 and H2O. Moreover, it is known that in diabetic animals, the development of hyperglycemia causes a decrease in the activity of SOD and CAT in the sciatic nerve (Halliwell 1991; Al-Enazi 2013). Thus, in the oxidative stress induced by hyperglycemia, decreased activity of SOD and CAT enzymes would be responsible for decreased protection against free radicals and the vulnerability of sciatic nerve cells (Al-Enazi 2013). In this study, the results show that Combretin A and Combretin B restore the activity of SOD and CAT in the sciatic nerve and in the serum of diabetic animals, which suggests that these two compounds are capable of protecting the body against the oxidative damage caused by hyperglycemia. Furthermore, Combretin A and Combretin B exhibited antioxidative properties, since the activity of the antioxidant enzymes as well as the levels of the endogenous antioxidant molecules have been significantly improved in the sciatic nerve and in the serum of diabetic mice after injection of STZ. The antioxidant properties of Combretin A and Combretin B observed in vivo in this study and in vitro in our previous studies (Mbiantcha et al. 2017) could justify the antidiabetic properties of these two compounds. Given that during the evolution of diabetic neuropathy, we observe development of the inflammatory process, the installation of oxidative stress and hypersensitivity in animals, this leads us to suggest that the antihyperalgesic and antiallodynic effects of Combretin A and Combretin B obtained in this study could be associated with their antiinflammatory and antioxidant activity.
The development of diabetic neuropathy is accompanied by a rise in the level of inflammatory mediators such as pro-inflammatory cytokines (TNF-α and IL-1β) in the serum and in the sciatic nerve of diabetic animals, consequence of the installation of hyperglycemia and insulin-resistance (Fatani et al. 2015; Brownlee 2005; Navarro-González and Mora-Fernández 2008). In addition, dysfunction observed at the level of neuronal cells just as the death of patients with diabetes can be caused by overexpression of these inflammatory biomarkers (Li et al. 2013; Djordjevic et al. 2015). Previous studies have indicated that Combretin A and Combretin B may exert in vivo protective effect against carrageenan-induced inflammation and in vitro cytotoxic effects against human cancer cell lines (MCF-7 cells) and significant inhibitory property on NO and TNF-α production (Mbiantcha et al. 2017). In the present study, serum, sciatic, and brain tissues pro-inflammatory markers among which NO, TNF-α, and IL-1β were significantly increased in STZ-induced diabetic animal. Combretin A and Combretin B treatment in diabetic mice significantly reduced such markers in the present study. Many physiological processes, namely, inflammation, immunity, pain, proliferation, and growth can be influenced by activation of nuclear factor κB (NF-κB) which is a protein transcription factor (Bonizzi and Karin 2004; Shishodia and Aggarwal 2004). After activating NF-κB by release of the complex IκB/NF-κB, nuclear factor NF-κB enters nucleus and triggers transcription of cytokines (TNF-α, IL-1β, interferon), enzymes (COX-2, iNOS), stress proteins, and immunoreceptors (Li and Karin 1999; Christman et al. 2000; Celec 2004). Moreover, the activity of the nuclear factor NF-κB, also considered as a sensor of oxidative stress, may be regulated by the levels of intracellular oxygen reactive metabolites. Similarly, it is known that overexpression of antioxidant enzymes and many antioxidant substances are capable of inhibiting the activation of nuclear factor NF-κB (Li and Karin 1999). In view of the foregoing, it is clear to suggest that the effects of Combretin A and Combretin B obtained in this study are related to a modulatory effect on nuclear factor NF-κB activity.
The neuropathic pain associated with the nerve damage that results from it causes many consequences among which anxiety, depression, and anhedonia that can be reproduced in animal models (Santos et al. 2017). In different animal models, pain is evaluated by sensory hypersensitivity, whereas anxiety and depression can be evaluated by EPMT, LDBT, SIT and TST, FST, OFT, respectively (Wang et al. 2011; Chang et al. 2015). Otherwise, it has been shown that in the animal model of diabetic neuropathy, in addition to the increased sensitivity to pain, animals develop a state of anxiety and depression. The similar results were observed by Santos et al. (2017) and Hache et al. (2012), specifying that chronic pain is closely related to the development of depressive and anxious behavior. In the present study, the administration of Combretin A and Combretin B (25 and 50 mg/kg) significantly ameliorated the symptom of depression and anxiety in all the animals treated; suggesting that these two compounds has antidepressant and anxiolytic-like effects.
Hyperglycemia induced autoxidation of glucose which in turn generates reactive oxygen species, attacks cells, and compromised membrane function (Lery et al. 1999). After administration of STZ in animals, we observe the increase of many serum parameters such as creatinine which materializes the kidney involvement; otherwise, the increase of enzymes such as alkaline phosphatase and transaminases which indicate hepatic damage is also observed in the serum (Sallie et al. 1991). Likewise, in the case of STZ-induced diabetes, there is severe pancreatic cell necrosis, which results in an increase in the serum level of AST (Recknagel 1987). Rajesh and Latha (2004) have also shown that the complete loss of cell membrane integrity and function would be closely related to an increase in the activity of these enzymes in the blood. In the current study, diabetic hyperglycemia induced by STZ caused the increasing of the serum level of AST, ALT, and ALP (hepatic enzymes), serum levels of creatinine and decreased serum level of total protein which were considered as significant signs of liver and renal dysfunction (Almdal and Vilstrup 1988). After the treatment of STZ-diabetic mice with Combretin A and Combretin B, the level of creatinine was significantly decreased in treated animals compared to the untreated diabetic control group. Similarly, the elevation of serum level of hepatic enzymes (AST, ALT and ALP) caused by administration of STZ was declined after the treatment with Combretin A and Combretin B, compared with the diabetic control group. It becomes evident from our results that both compounds improve the functional state of the liver and kidneys by maintaining the normal values of renal and hepatic parameters. The improvement of protein production, enzyme activity (AST, ALT, and ALP), and creatinine by Combretin A and Combretin B could be attributed to the antioxidant activities.
Conclusion
This study reveals that Combretin A and Combretin B have antiallodynic effect in the model of thermal and cold allodynia and antihyperalgesic effect in the thermal hyperalgesia in streptozotocin-induced neuropathic pain model, in a neuropathic pain via its antihyperglycemic, antioxidative, and antiinflammatory properties. These properties are associated with antidepressive and anxiolytic-like effects. The compounds improved liver and kidney functions by increasing total protein synthesis and decreasing enzymes activities (ALAT and ASAT) and creatinine levels of diabetic mice. Therefore, Combretin A and Combretin B may be useful as a new solution for the management of neuropathy in people with chronic diabetes.
Data availability
All data supporting our findings are adequately contained within the manuscript.
References
Al-Enazi MM (2013) Ameliorative potential of rutin on streptozotocin induced neuropathic pain in rat. Afr J Pharm Pharmacol 7(41):2743–2754
Almdal TP, Vilstrup H (1988) Strict insulin treatment normalizes the organic nitrogen contents and the capacity of urea–N synthesis in experimental diabetes in rats. Diabetes 31:114–118
Apfel SC, Asbury AK, Bril V, Burns TM, Campbell JN, Chalk CH, Dyck PJ, Dyck PJ, Feldman EL, Fields HL, Grant IA, Griffin JW, Klein CJ, Lindblom U, Litchy WJ, Low PA, Melanson M, Mendell JR, Merren MD, O'Brien PC, Rendell M, Rizza RA, Service FJ, Thomas PK, Walk D, Wang AK, Wessel K, Windebank AJ, Ziegler D, Zochodne DW (2001) Positive neuropathic sensory symptoms as endpoints in diabetic neuropathy trials. J Neurol Sci 189:3–5
Baron R, Binder A, Wasner G (2010) Neuropathic pain: diagnosis, pathophysiological mechanisms, and treatment. Lancet Neurol 9(8):807–819
Barrett AM, Lucero MA, Le T, Robinson RL, Dworkin RH, Chappell AS (2007) Epidemiology, public health burden, and treatment of diabetic peripheral neuropathic pain: a review. Pain Med 8(Suppl. 2):S50–S62
Bhattamisra SK, Singh PN, Singh SK, Kumar V (2007) Anxiolytic activity of Marsilea minuta Linn. Journal of Herbal Medicine and Toxicology 1:15–20
Biella GE, Groppetti A, Novelli A, Fernández-Sánchez MT, Manfredi B, Sotgiu ML (2003) Neuronal sensitization and its behavioral correlates in a rat model of neuropathy are prevented by a cyclic analog of orphenadrine. J Neurotrauma 20:593–601
Bolajoko EB, Mossanda KS, Adeniyi F, Akinosun O, Fasanmade A, Moropane M (2008) Antioxidant and oxidative stress status in type 2 diabetes and diabetic foot ulcer. S Afr Med J 98:614–617
Bonizzi G, Karin M (2004) The two NF-κB activation pathways and their role in innate and adaptive immunity. Trends Immunol 25:280–288
Bortalanza LB, Ferreira J, Hess SC, Monache FD, Yunes RA, Calixto JB (2002) Anti-allodynic action of the tormentic acid, a triterpene isolated from plant, against neuropathic and inflammatory persistent pain in mice. Eur J Pharmacol 453:203–208
Boulton AJM, Malik RA, Arezzo J, Sosenko JM (2000) Diabetic neuropathy: technical review. Diabetes Care 27:1458–1487
Brownlee M (2005) The pathobiology of diabetic complications: a unifying mechanism. Diabetes 54:1615–1625
Calcutt NA (2004) Experimental models of painful diabetic neuropathy. J Neurol Sci 220:137–139
Calixto JB, Beirith A, Ferreira J, Santos AR, Cechinel FV, Yunes RA (2000) Naturally occurring antinociceptive substances from plants. Phytother Res 14:401–418
Celec P (2004) Nuclear factor Kappa B-molecular biomedicine: the next generation. Biomed Pharmacother 58:365–371
Chan AW, MacFarlane IA, Bowsher DR (1990) Chronic pain in patients with diabetes mellitus: comparison with non-diabetic population. Pain Clin 3:147–159
Chang CY, Guo HR, Tsai WC, Yang KL, Lin LC, Cheng TJ, Chuu JJ (2015) Subchronic arsenic exposure induces anxiety-like behaviors in normal mice and enhances depression-like behaviors in the chemically induced mouse model of depression. Biomed Res Int 2015:159015
Chaplan SR, Bach FW, Pogrel JW, Chung JM, Yaksh TL (1994) Quantitative assessment of tactile allodynia in the rat paw. J Neurosci Methods 53:55–63
Christman JW, Blackwell TS, Juurlink BHJ (2000) Redox regulation of nuclear factor Kappa B: therapeutic potential for attenuating inflammatory responses. Brain Pathol 10:153–162
Crawley J, Goodwin FK (1980) Preliminary report of a simple animal behavior model for the anxiolytic effects of benzodiazepines. Pharmacol Biochem Behav 13:167–170
Daousi C, MacFarlane IA, Woodward A, Nurmikko TJ, Bundred PE, Benbow SJ (2004) Chronic painful peripheral neuropathy in an urban community: a controlled comparison of people with and without diabetes. Diabet Med 21:976–982
Davies M, Brophy S, Williams R, Taylor A (2006) The prevalence, severity, and impact of painful diabetic peripheral neuropathy in type 2 diabetes. Diabetes Care 29:1518–1522
Dawe A, Wabo Fotso KGD, Bankeu Kezetas JJ, Fawaia Y, Alid Shaiq M, Ngadjuie Tchaleu B (2016) Combretins A and B, new cycloartane-type triterpenes from Combretum fragrans. Helv Chim Acta 99:617–620
De Groot M, Anderson R, Freedland KE, Clouse RE, Lustman PJ (2001) Association of depression and diabetes complications: a meta-analysis. Psychosom Med 63:619–630
Decosterd I, Woolf CJ (2000) Spared nerve injury: an animal model of persistent peripheral neuropathic pain. Pain 87(2):149–158
Djordjevic A, Bursać B, Veličković N, Vasiljević A, Matić G (2015) The impact of different fructose loads on insulin sensitivity, inflammation, and PSA-NCAM-mediated plasticity in the hippocampus of fructose-fed male rats. Nutr Neurosci 18:66–75
Durst T, Merali Z, Arnason JT, Sanchez-Vindas EP, Poveda AL (2002) Anxiolytic Marcgraviaceae compositions containing betulinic acid, betulinic acid derivates, and methods. WO/2002/091858
Dworkin RH, Gitlin MJ (1991) Clinical aspects of depression in chronic pain patients. Clin J Pain 7:79–94
Dworkin RH, O’Connor AB, Audette J, Baron R, Gourlay GK, Haanpää ML, Kent JL, Krane EJ, LeBel AA, Levy RM, Mackey SC, Mayer J, Miaskowski CD, Raja SN, ASC R, Schmader KE, Stacey B, Stanos S, Treede RD, Turk DC, Walco GA, Wells CD (2010) Recommendations for the pharmacological management of neuropathic pain: an overview and literature update. Mayo Clin Proc 85(3):S3–S14
Dyck PJ, Davies JL, Litchy WJ (1997) Longitudinal assessment of diabetic polyneuropathy using a composite score in the Rochester diabetic neuropathy study cohort. Neurology 49:229–239
Fatani AJ, Al-Rejaie SS, Abuohashish HM, Al-Assaf A, Parmar MY, Ola MS, Ahmed MM (2015) Neuroprotective effects of Gymnema sylvestre on streptozotocin-induced diabetic neuropathy in rats. Exp Ther Med 9:1670–1678
Felipe FCB, Filho JTS, Souza LO, Silveira JA, Uchoa DEA, Silveira ER, Deusdênia LPO, De Barros Viana GS (2007) Piplartine, an amide alkaloid from Piper tuberculatum, presents anxiolytic and antidepressant effects in mice. Phytomedicine 14:605–612
File SE (1996) The use of social interaction as a method for detecting anxiolytic activity of chlordiazepoxide like drugs. J Neurosci Methods 2:219–238
Gonder-Frederick LA, Cox DJ, Ritterband LM (2002) Diabetes and behavioral medicine: the second decade. J Consult Clin Psychol 70:611–625
Gul H, Yildiz O, Dogrul A, Yesilyurt O, Isimer A (2000) The interaction between IL-1beta and morphine: possible mechanism of the deficiency of morphine-induced analgesia in diabetic mice. Pain 89:39–45
Hache G, Guiard BP, Le Dantec Y, Orvoën S, David DJ, Gardier AM, Coudore F (2012) Antinociceptive effects of fluoxetine in a mouse model of anxiety/depression. Neuro Report 23(9):525–529
Halliwell B (1991) Drug antioxidant effects. A basis for drug selection. Drugs 42:569–605
Hanson JR (2003) Natural products: the secondary metabolites. The Royal Society of Chemistry, Cambridge, pp 112–121
Hasanein P, Soltani N (2009) Effects of the endocannabinoid transport inhibitors AM404 and UCM707 on diabetic neuropathy in rats. Clin Exp Pharmacol Physiol 36:1127–1131
Hasanein P, Parviz M, Keshavarz M, Roohbakhsh A (2009) URB597, an inhibitor of fatty acid amide hydrolase, reduces hyperalgesia in diabetic rats. Can J Physiol Pharmacol 87:432–439
Herrera-Ruiza M, Jime’nez-Ferrera JE, De Limab TCM, Avile’s-Montesc D, Pe’rez-Garcı D, Gonzalez-Cortazara D, Tortorielloa J (2006) Anxiolytic and antidepressant-like activity of a standardized extract from Galphimia glauca. Phytomedicine 13:23–28
Julius U, Drel VR, Grässler J, Obrosova IG (2009) Nitrosylated proteins in monocytes as a new marker of oxidative-nitrosative stress in diabetic subjects with macroangiopathy. Exp Clin Endocrinol Diabetes 117:72–77
Kamei J, Ohhashi Y, Aoki T, Kasuya Y (1991) Streptozotocin-induced diabetes in mice reduces the nociceptive threshold, as recognized after application of noxious mechanical stimuli but not of thermal stimuli. Pharmacol Biochem Behav 39(2):541–544
Kamei J, Zushida K, Morita K, Sasaki M, Tanaka S (2001) Role of vanilloid VR1 receptor in thermal allodynia and hyperalgesia in diabetic mice. Eur J Pharmacol 422:83–86
Leo RJ (2005) Chronic pain and comorbid depression. Curr Treat Options Neurol 7:403–412
Lery V, Zaltzber H, Ben-Amotz A, Kanter Y, Aviram M (1999) Carotene affects antioxidant status in non-insulin dependent diabetes mellitus. Pathophysiology 6:157–162
Leung L, Cahill CM (2010) TNF-α and neuropathic pain-a review. J Neuroinflammation 7:27
Li N, Karin M (1999) Is NF-κB the sensor of oxidative stress? FASEB J 13:1137–1143
Li Y, Dorsi MJ, Meyer RA, Belzberg AJ (2000) Mechanical hyperalgesia after an L5 spinal nerve lesion in the rat is not dependent on input from injured nerve fibers. Pain 85:493–502
Li J, Wei GH, Huang H, Lan YP, Liu B, Liu H, Zhang W, Zuo YX (2013) Nerve injury-related autoimmunity activation leads to chronic inflammation and chronic neuropathic pain. Anesthesiology 118:416–429
Lloyd CE, Matthews KA, Wing RR, Orchard TJ (1991) Psychosocial factors and complications of IDDM: the Pittsburgh epidemiology of diabetes complications study viii. Diabetes Care 15:166–172
Mbiantcha M, Almas J, Dawe A, Faheem A, Sidra Z (2017) Analgesic, anti-inflammatory and anticancer activities of Combretin A and Combretin B isolated from Combretum fragrans F. HOFFM (Combretaceae) leaves. Inflammopharmacology 1:12
Moroney MA, Alcaraz MJ, Forder RA, Carey F, Hoult JRS (1988) Activity of Lupane triterpenoids from Maytenus species. J Pharm Pharmacol 40:787
Morris HV, Dawson GR, Reynolds DS, Atack JR, Stephens DN (2006) Both alpha 2 and alpha 3 GABA-A receptor subtypes mediate the anxiolytic properties of benzodiazepine site ligands in the conditioned emotional response paradigm. Eur J Neurosci 23:2495–2504
Navarro-González JF, Mora-Fernández C (2008) The role of inflammatory cytokines in diabetic nephropathy. J Am Soc Nephrol 19:433–442
Nguelefack TB, Dutra RC, Paszcuk AF, De Andrade EL, Calixto JB (2015) TRPV1 channel inhibition contributes to the antinociceptive effects of Croton macrostachyus extract in mice. BMC Complement Altern Med 15:293
Orrù A, Marchese G, Casu G, Casu MA, Kasture S, Cottiglia F, Acquas E, Mascia MP, Anzani N, Ruiu S (2014) Withania somnifera root extract prolongs analgesia and suppresses hyperalgesia in mice treated with morphine. Phytomedicine 21:745–752
Porsolt RD, Bertin A, Jalfre M (1977) Behavioral despair in mice: a primary screening test for antidepressants. Arch Int Pharmacodyn Ther 229:327–336
Rajesh MG, Latha MS (2004) Preliminary evaluation of the antihepatotoxic effect of Kamilari, a polyherbal formulation. J Ethnopharmacol 91:99–104
Recknagel RO (1987) Carbon tetrachloride hepatotoxicity. Pharmacol Rev 19:145–195
Sallie R, Tredger JM, William R (1991) Drugs and the liver. Biopharm Drug Dispos 12:251–259
Sánchez-Ramírez GM, Caram-Salas NL, Rocha-González HI, Vidal-Cantú GC, Medina-Santillán R, Reyes-García G, Granados-Soto V (2006) Benfotiamine relieves inflammatory and neuropathic pain in rats. Eur J Pharmacol 530(1–2):48–53
Santos JA, Piccinelli AC, Formagio MD, Oliveira CS, Santos EPD, Alves Stefanello ME, Lanza Junior U, Oliveira RJ, Sugizaki MM, Kassuya CAL (2017) Antidepressive and antinociceptive effects of ethanolic extract and fruticuline A from Salvia lachnostachys Benth leaves on rodents. PLoS One 12(2):e0172151. https://doi.org/10.1371/journal.pone.0172151
Shishodia S, Aggarwal BB (2004) Nuclear factor-κB: a friend or a foe in cancer? Biochem Pharmacol 15:1071–1080
Steru L, Chermat R, Thierry B, Simon P (1985) The tail suspension test: a new method for screening antidepressants in mice. Psychopharmacology 85:367–370
Subarnas A, Tadano T, Kisara K, Ohizumi O (1993) An alpha-adrenoceptor-mediated mechanism of hypoactivity induced by beta-amyrin palmitate. J Pharm Pharmacol 45:1006–1008
Treede RD, Jensen TS, Campbell JN, Cruccu G, Dostrovsky JO, Griffin JW, Hansson P, Hughes R, Nurmikko T, Serra J (2008) Neuropathic pain: redefinition and a grading system for clinical and research purposes. Neurology 70:1630–1635
Vileikyte L, Leventhal H, Gonzalez JS, Peyrot M, Rubin RR, Ulbrecht JS, Garrow A, Waterman C, Cavanagh PR, Boulton AJM (2005) Diabetic peripheral neuropathy and depressive symptoms. Diabetes Care 28(10):2378–2383
Vranken JH (2012) Elucidation of pathophysiology and treatment of neuropathic pain. Cent Nerv Syst Agents Med Chem 12(4):304–314
Wang J, Goffer Y, Xu D, Tukey DS, Shamir DB, Eberle SE, Zou AH, Blanck TJ, Ziff EB (2011) A single sub-anesthetic dose of ketamine relieves depression-like behaviors induced by neuropathic pain in rats. Anesthesiology 115(4):812–821
Acknowledgements
The authors would like to thank the study participants; the staff of Department of Pharmaceutical Sciences, COMSATS Institute of Information Technology, Abbottabad- 22060, Pakistan. The authors wish to express their gratitude to TWAS (Academy of Science of Developing Countries) and COMSATS Institute of Information Technology staff member.
Funding
This manuscript research project was supported by the TWAS (Academy of Science of Developing Countries) and the COMSATS Institute of Information Technology, under the Post-doctoral Fellowship Award to Mbiantcha Marius (RF no. 3240287152).
Author information
Authors and Affiliations
Contributions
MM and KR designed the work. MM, KR, DA, MA, HD, NUR and IA conducted the work, collected and analyzed the data. MM, AAD, AG, NYW and BTDF drafted the manuscript and revised it critically. All authors agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
To demonstrate the coherent effects of our different compounds, the minimum possible of animals as the intensity of nociceptive stimuli was used. All tests were achieved using mature male and female mice (3 months old; 25–35 g), bred in the animal house facility (controlled temperature (22 ± 1 °C); 12 h light/12 h dark cycle with standard lab chow and water ad libitum) of the National Institute of Health (NIH), Islamabad, Pakistan. The treatment of animals was in agreement with the Institutional Animal Care and Use Committee (IACUC) of the National Institute of Health, and the study protocols accepted by the ethics committee of National Institute of Health, Islamabad, Pakistan.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
A statement regarding consent for publication is not applicable for this study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mbiantcha, M., Khalid, R., Dawe, A. et al. Antihypernociceptive and neuroprotective effects of Combretin A and Combretin B on streptozotocin-induced diabetic neuropathy in mice. Naunyn-Schmiedeberg's Arch Pharmacol 392, 697–713 (2019). https://doi.org/10.1007/s00210-019-01626-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-019-01626-1