Abstract
To investigate the topical anti-inflammatory activity of the crude extract of Cariniana domestica fruit peels (CdE), its dichloromethane, n-butanol, and ethyl acetate (EtAc) fractions, and steroids (β-sitosterol, lupeol, and stigmasterol) isolated from the EtAc fraction in models of irritant contact dermatitis (ICD) croton oil-induced in mice. We induced skin inflammation by single (acute; 1 mg/ear) and multiple (chronic; 0.4 mg/ear) croton oil application. We topically applied C. domestica (CdE, fractions, and gel formulations) and β-sitosterol, lupeol, and stigmasterol immediately after applying croton oil. HPLC-DAD chromatography of the EtAc fraction and stability of the gel formulations were verified. HPLC-DAD of the EtAc fraction revealed the stigmasterol, lupeol, and β-sitosterol presence. CdE and EtAc fraction gels showed no organoleptic or pH changes at room temperatures. CdE and dichloromethane, n-butanol, and EtAc (1 mg/ear) fractions decreased the acute ear edema with maximum inhibition (Imax) of 97 ± 2, 86 ± 1, 81 ± 4, and 95 ± 2%, respectively. CdE and EtAc fraction gel presented similar effects, with respective Imax of 85 ± 6% (3%;15 mg/ear) and 82 ± 2% (1%;15 mg/ear). β-sitosterol (7.5 μg/ear), lupeol (10 μg/ear), and stigmasterol (5.7 μg/ear) also reduced this parameter by 46 ± 8, 51 ± 7, and 62 ± 7%, respectively. All topical treatments reduced the inflammatory cells’ infiltration in the acute ICD model. CdE reduced the ear edema by 77 ± 4% (1 mg/ear) and the inflammatory cell infiltration in the chronic ICD model. CdE’s anti-inflammatory effect was accompanied by a minimum development of adverse effects. C. domestica demonstrates a promising potential for the development of a topical anti-inflammatory agent.

Cariniana domestica, popularly known as jequitibá-roxo, presented topical anti-inflammatory activity in an acute and chronic irritant contact dermatitis croton oil-induced in mice. The crude extract (solutions and gel formulations) and different fractions obtained from fruit peels of C. domestica showed topical antiinflammatory activity on skin inflammation models with minimum adverse effects in preliminary toxicological studies (behavior and biochemical parameters). Moreover, the HPLC analysis revealed the presence of β-sitosterol, stigmasterol and lupeol, which also presented topical anti-inflammatory effect in the acute irritant contact dermatitis croton oil-induced. Our findings support the use of this species as a promising topical antiinflammatory agent.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Skin acts as the first line of defense against several pathogens and other external noxious agents (Di Meglio et al. 2011; Saraiva et al. 2011). Its primary function is to provide an effective barrier which affords defensive immunological reactions against several insults from the environment (Bangert et al. 2011; Feingold et al. 2007; Pinto et al. 2015). However, a cutaneous barrier abnormality triggers an inappropriate immune activity leading to the development of cutaneous inflammatory diseases, such as irritant contact dermatitis (Chibli et al. 2014; Proksch et al. 2008; Saraiva et al. 2011).
Irritant contact dermatitis is a localized inflammatory reaction caused by direct contact with chemical substances such as detergents, acids, and alkalis, as well as physical agents such as temperature and climatic conditions (Eberting 2014; Lee et al. 2013; Seyfarth et al. 2011). In the skin’s inflammatory process, there occurs skin barrier disruption, keratinocyte activation, and pro-inflammatory cytokines release (Lee et al. 2013; Lisby and Baadsgaard 2010). Acute skin inflammation is clinically characterized by edema, erythema, cell infiltration, coalescing vesicles, pustules, ulceration, and even skin necrosis (Lisby and Baadsgaard 2010; Slodownik et al. 2008). In its chronic form, dryness, fissuring, and hyperkeratosis are more pronounced. Furthermore, some clinical cases may manifest stinging, burning, or itchy sensations (Eberting 2014; Lisby and Baadsgaard 2010).
Anti-inflammatory agents are quite effective in several forms of skin barrier disruption, with glucocorticoids being the most prescribed drugs for these inflammatory skin conditions (Eberting 2014; Siddiqui et al. 2016; Simpson et al. 2014). Nevertheless, steroid-based therapies cause adverse effects such as hypopigmentation, delayed wound healing, skin atrophy, and dryness, which limit long-term use (Lee et al. 2016; Simpson et al. 2014; Xiao et al. 2015).
The lack of safer and more effective therapies supports the search for therapeutic alternatives to treat inflammatory skin diseases (Horinouchi et al. 2013). An attractive option would be the use of medicinal plant extracts due to their significant sources of biologically active natural products and the promising possibility for drug discovery considering their easy access and relatively low cost (Ibrahim et al. 2012; Mendes et al. 2016). Several studies have proven the effectiveness of extracts or isolated compounds of plants for treating inflammatory skin disease treatment (Brum et al. 2016; Lee et al. 2016; Lim et al. 2015; Piana et al. 2016; Saraiva et al. 2011).
Cariniana domestica (Mart.) Miers. belongs to the Lecythidaceae family, is commonly known as “jequitibá-roxo,” and found in Brazil, Bolivia, and Peru. Previous studies have established the presence of triterpenoid, flavonoid, and phenolic compounds in the leaves and fruit peels of this species (Janovik et al. 2011; Janovik et al. 2012a). There are few studies concerning the ethnopharmacological uses of Cariniana spp., although the infusion with peels of this species has reportedly been used as an anti-inflammatory and antimicrobial agent (Janovik et al. 2012b). Corroborating these reports, studies have shown that the stem barks of Cariniana rubra are a reputed traditional remedy in decoction and infusion forms to treat inflammatory disorders, as confirmed by Santos et al. (2011). However, so far, no studies demonstrate C. domestica’s anti-inflammatory activity, although other biological activities have recently been found along with the identification of secondary metabolites (Janovik et al. 2011; Janovik et al. 2012a, b), including phytochemical compounds with anti-inflammatory activities proven in previous studies (Bellik et al. 2012; Chibli et al. 2014; Choi and Kim 2013; Khan et al. 2012; Phanse et al. 2012; Xu et al. 2014).
To contribute to the search for new medicinal plants with anti-inflammatory potential and for better understanding the ethnopharmacological relevance of C. domestica, we investigated the effectiveness and preliminary safety of this species as a topical anti-inflammatory agent in an irritant contact dermatitis model induced by croton oil.
Material and methods
Chemicals
All chemicals were of analytical grade. Hematoxylin-eosin and paraffin were purchased from Merck (Darmstadt, Germany). Croton oil, hexadecyltrimethylammonium bromide (HTAB), tetramethylbenzidine (TMB), dexamethasone, acetonitrile, ethylenediaminetetraacetic acid (EDTA), β-sitosterol, lupeol, and stigmasterol were acquired from Sigma Chemical Co. (St. Louis, Mo, USA). Isoflurane (Baxter, São Paulo, Brazil), sodium acetate, acetone, absolute ethanol, acetic acid, and formaldehyde (all from Vetec, Rio de Janeiro, Brazil) were used. Methylparaben (Nipagin®; Belga), hydroxyethylcellulose (Natrosol® QP400H; FarmaQuímica), and formylgermanium (Germal®; Delaware) were purchased from local suppliers. The colorimetric kits for alanine aminotransferase (ALT), aspartate aminotransferase (AST), glucose, or creatinine were purchased from Labtest (Minas Gerais, Brazil).
Plant material and extractions
The same crude extract (CdE) and fractions of C. domestica fruit peels used by Janovik et al. (2012a) were stored in hermetically sealed containers, with a temperature of 5 ± 2 °C to maintain the phytochemical quality of these samples. A dried voucher specimen is preserved in the herbarium of the Department of Biology at Federal University of Santa Maria by register number SMBD 11818.
The fruits peel were dried and powdered in a knife mill, it was macerated at room temperature with 70% ethanol for 10 days with a daily shake-up, and this solvent was renewed twice. After filtration, the hydroalcoholic extract was evaporated under reduced pressure to remove the ethanol and was taken to complete dryness, yielding the C. domestica crude extract. Another part of the extract was successively partitioned with dichloromethane, ethyl acetate, and n-butanol, which also were dried to produce each corresponding fraction. We evaluated the topical anti-inflammatory activity of CdE and its fractions. The later was chosen due to a higher amount of phenolic compounds as described by previous studies (Janovik et al. 2012a).
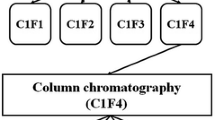
Quantification of steroids in the ethyl acetate fraction by HPLC-DAD
Chromatographic analyses were performed under isocratic conditions using C8 column (4.6 mm × 150 mm) packed with 5-μm-diameter particles. The mobile phase consisted of acetonitrile and water (95:5 v/v), filtered through a 0.45-μm membrane filter and degassed in an ultrasonic bath prior to use. Quantification of stigmasterol, lupeol, and β-sitosterol was performed by injecting 40 μL volume, flow rate of 1.0 mL/min, with HPLC separation followed by UV detection at 210 nm (Boligon et al. 2015). EtAc fraction was analyzed at a concentration of 10 mg/mL. Stock solutions of standards references were diluted in acetonitrile/water (1:1 v/v) at a concentration range of 0.025–0.500 mg/mL. Calibration curve for β-sitosterol is Y = 12,473x + 1186.7 (r = 0.9998), stigmasterol Y = 13,045x + 1261.4 (r = 0.9995), and lupeol Y = 11,985x + 1362.7 (r = 0.9999), where Y is the peak area of steroids obtained by HPLC and x is the concentration in milligrams per gram. All chromatography operations were performed at ambient temperature and in triplicate.
C. domestica gels
The CdE or EtAc fraction gels were prepared with hydroxyethylcellulose (Natrosols®; 2.8%), EDTA Proquimios (0.10%), methylparaben (Nipagin®; 0.25%), formylgermanium (Germals®; 0.25%), and distilled water (q.s.p) in the concentrations of 0.3, 1, and 3%. Briefly, EDTA, Nipagin, and distilled water were placed in a mortar to heat to 65 °C on a hot plate. After that, Natrosol was incorporated and then cooled down to 40 °C and the Germal and CdE or EtAc fraction was added previously dissolved in distilled water. The homogenization was performed with a pistil during the whole process (Piana et al. 2013). Base gel (without crude extract or fraction) was used in the vehicle group. Dexamethasone gel (0.5%) was used as a positive control.
Stability study of C. domestica gels
The gel concentration which showed the best results in the topical anti-inflammatory assays were used in the stability study. The evaluations were conducted following the Guide of Stability to Cosmetic Products (National Health Surveillance Agency-Anvisa 2004) with modifications. Organoleptic characteristics and pH measurements of the CdE and EtAc fraction gels were evaluated on the zero time and on the 90th day at room temperature (25 ± 5 °C) after the preparation of the gels. The tests were performed in triplicate in three batches of each sample. We performed the organoleptic characteristics considering any change of color, smell, and appearance, evaluated at lighting and packaging conditions. The pH measurements of the samples were performed with a laboratory pH meter (Digimed-DM-22, Digicrom Analytical), previously calibrated with buffer solutions of pH 4.0 and 7.0.
Animals
Adult male Swiss mice (25–30 g) were kept at 22 ± 2 °C (60–80% humidity) under a 12-h light-dark cycle and with standard laboratory food and water ad libitum. Experiments were performed between 8:00 a.m. and 5:00 p.m. and were conducted in accordance with national and international legislation (guidelines of Brazilian Council of Animal Experimentation—CONCEA—and of U.S. Public Health Service’s Policy on Humane Care and Use of Laboratory Animals—PHS Policy), approved by Institutional Committee for Animal Care and Use of the Federal University of Santa Maria (Process number 9475221015/2015) and were reported in compliance with the ARRIVE guidelines (Mcgrath and Lilley 2015). Animals were randomly assigned to different treatment groups and all experimental protocols were performed blindly with respect to drug administration. The number of animals and the intensity of irritant agent topically applied were the minimum necessary to demonstrate the consistent effects of treatments.
Treatments
CdE and its dichloromethane, n-butanol, and ethyl acetate fractions, β-sitosterol, lupeol, stigmasterol, gel formulations of CdE and of EtAc fraction, dexamethasone (solution and incorporated in gel), and croton oil were topically applied to the right ear of each mouse. Dexamethasone was used as a positive control. We chose doses of 7.5, 10, and 5.7 μg/ear for β-sitosterol, lupeol, and stigmasterol, respectively, to evaluate its anti-inflammatory effects because these doses are equivalent to its concentrations present in 1 g of C. domestica EtAc fraction. The animals were divided in experimental groups. In the acute irritant contact dermatitis model, the groups were naive, vehicle (acetone; 20 μL/ear), croton oil (1 mg/ear), croton oil plus CdE (0.01; 0.1; 0.3, or 1 mg/ear), croton oil plus dichloromethane fraction (0.001, 0.01, 0.1, or 1 mg/ear), croton oil plus n-butanol fraction (0.001, 0.01, 0.1, or 1 mg/ear), croton oil plus ethyl acetate fraction (0.001, 0.01, 0.1, or 1 mg/ear), croton oil plus β-sitosterol (7.5 μg/ear), croton oil plus lupeol (10 μg/ear), croton oil plus stigmasterol (5.7 μg/ear), croton oil plus dexamethasone (0.1 mg/ear), croton oil plus CdE gel (0.03, 0.1, 0.3, 1, and 3%), croton oil plus ethyl acetate gel (0.03, 0.1, 0.3, and 1%), and croton oil plus dexamethasone gel (0.5%). In the chronic irritant contact dermatitis model, the groups were naive, vehicle (acetone; 20 μL/ear), croton oil (0.4 mg/ear), croton oil plus CdE (1 mg/ear), and croton oil plus dexamethasone (0.1 mg/ear).
Ear edema measurement
The irritant contact dermatitis was induced by topical application of croton oil in the right ear of mice. Ear thickness was evaluated before and at 6 h after croton oil application using a digital micrometer (Digimess) in animals anesthetized with isoflurane (Adami et al. 2012; Piana et al. 2016). An increase in the ear thickness after the croton oil application compared to baseline measure was characterized as ear edema. The micrometer was applied near the tip of the ear just distal to the cartilaginous ridges. The ear edema was expressed in micrometer.
Croton oil-induced acute ear edema
Acute inflammation was induced by a single topical application of croton oil (1 mg/ear, 20 μL in acetone) on the right ear of mice. We evaluated the anti-inflammatory effect of the CdE (0.01–1 mg/ear), its fractions (ethyl acetate, n-butanol, and dichloromethane) (0.001–1 mg/ear), β-sitosterol (7.5 μg/ear), lupeol (10 μg/ear), and stigmasterol (5.7 μg/ear) or dexamethasone (0.1 mg/ear) which were dissolved in acetone. Moreover, CdE (0.03–3%), its EtAc fraction (0.03–1%), or dexamethasone (0.5%) was also incorporated in a gel formulation (15 mg/ear). Ear thickness was measured prior to and at 6 h after croton oil application. Treatments were performed immediately after croton oil administration. Six hours after croton oil application, the animals were euthanized and the ears were collected for further analyses (Piana et al. 2016).
Croton oil-induced chronic ear edema
Chronic inflammation was induced by multiple topical applications of croton oil (0.4 mg/ear in acetone) to the right ear for nine alternated days. CdE (1 mg/ear) or dexamethasone (0.1 mg/ear) was applied topically to each right ear (20 μL/ear) twice daily, from the fifth up to the ninth day after the topical application first of croton oil. Ear thickness was measured daily. On the last day of the experiment, the animals were euthanized and skin biopsies were taken for further analyses (Adami et al. 2012; Piana et al. 2016).
Assessment inflammatory parameters
Measurement of myeloperoxidase activity
Myeloperoxidase (MPO) is an enzyme which is a biochemical marker of polymorphonuclear leukocyte infiltration, more specifically neutrophil. MPO activity was determined as previously described (Oliveira et al. 2014; Piana et al. 2016). MPO enzyme activity was measured after 6 h of croton oil application (acute irritant contact dermatitis) or after 9 days (chronic irritant contact dermatitis). Ear tissue samples were homogenized with a motor-driven homogenizer in acetate buffer (8 mM, pH 5.4) containing HTAB and centrifuged at 11,000×g for 20 min and the supernatant was collected. The supernatant was incubated with acetate buffer (8 mM, pH 5.4) and TMB (18.4 mM) at 37 °C for 3 min. The reaction was stopped with acetic acid in a cold bath, and the enzyme activity value was assessed colorimetrically at 630 nm using a microplate reader. The results were expressed as optical density (OD)/mL of sample.
Histology
Separate groups of mice were used to assess histological changes in animal ears at 6 h (acute irritant contact dermatitis) or after 9 days (chronic irritant contact dermatitis) after croton oil alone or croton oil plus treatments. Mice were euthanized and the right ear was removed and fixed in alfac solution (16:2:1 mixture of ethanol 80%, formaldehyde 40%, and acetic acid). Each sample was embedded in paraffin, sectioned at 5 μm, and stained with hematoxylin-eosin. A representative area was selected for qualitative light microscopic analysis of the inflammatory cellular response with ×20 and ×40 objectives (Oliveira et al. 2014; Piana et al. 2016). To minimize a source of bias, the investigator was blinded to the analyzing group.
Assessment of possible adverse effects caused by C. domestica
We also preliminarily assessed a possible toxicity caused by repeated topical treatment with C. domestica. Animals were topically treated once a day with the CdE (1 mg/ear), dexamethasone (0.1 mg/ear), or vehicle (acetone, 20 μL/ear) during 14 days. Changes in the appearance of hair, behavior (irritability, salivation, and tremors), hair appearance, organs, and body weight were monitored (Cunha et al. 2009).
Biochemical markers of toxicity
After the 14th day of observation, the animals were deeply euthanized and the blood was collected by cardiac puncture. Hepatic and renal alterations were evaluated through alanine aminotransferase (ALT) and aspartate aminotransferase (AST) enzyme activities and through creatinine levels in the serum, respectively. Glucose levels were also evaluated using Labtest® kits (Labtest Diagnostica, Brazil).
Open-field and rotarod test
On the 14th day of the experiment, the possible effect of CdE (1 mg/ear), vehicle (20 μL/ear), and dexamethasone (0.1 mg/ear) on the forced and spontaneous locomotor activity of animals was evaluated using the rotarod and open-field tests, respectively. Morphine (100 mg/kg; s.c.) was used as a positive control (Trevisan et al. 2013). For the open-field test, the apparatus consisted of a box, measuring (28 × 18 × 12 cm) with a floor that was divided into 15 identical areas. The animals were transferred to the apparatus and observed for 5 min. The number of areas crossed with all paws (crossings) and the number of rearing responses were recorded. For the rotarod test, the animals were placed in an apparatus (3.7 cm in diameter, 8 rpm) and were subjected to the test. The number of falls from the apparatus was recorded during 240 s.
Statistical analysis
We present the results in the mean ± mean standard error (SEM) and mean ± standard deviation (SD) formats. We calculated the maximum inhibitory effect based on each treatment’s capability to reduce the evaluated inflammatory parameters with regard to the control group’s (croton oil) response, which we considered as 100% of the inflammatory effect. We assessed the statistical significance among the groups employing one or two-way (repeated measures) analysis of variance (ANOVA), followed by a post hoc Newman-Keuls or Bonferroni test. P values lower than 0.05 denote significant differences among groups. All tests were carried out using software GraphPad 5.0 (San Diego, CA, USA). We did not employ any statistical methods to determine the sample sizes, but they are similar to those reported in previous studies in the field (Brum et al. 2016; Piana et al. 2016).
Results
Ethyl acetate fraction steroids HPLC-DAD analysis
The HPLC-DAD analysis of the EtAc fraction revealed the presence of the lupeol (11.09 ± 0.10 mg/g), stigmasterol (5.68 ± 0.31 mg/g), and β-sitosterol (7.45 ± 0.20 mg/g) (Fig. 1).
Representative high-performance liquid chromatography profile of the EtAc fraction. Lupeol (peak 1; tR = 12.75 min), stigmasterol (peak 2; tR = 14.19 min), and β-sitosterol (peak 3; tR = 17.83 min). The relative amounts of the phytochemical compounds per gram of the EtAc fraction are expressed in the mean ± standard deviation (SD) format considering three determinations
Stability study
We did not detect any relevant changes in color, smell, or appearance in the CdE and EtAc fraction gels. The pH values ranged from 5.89 to 5.54 for the CdE gel and from 5.5 to 5.02 for the EtAc fraction gel, having been evaluated at time 0 and after 90 days of the preparation of the gels, respectively.
Effect of C. domestica CdE and fractions on croton oil-induced acute ear edema
To evaluate the topical anti-inflammatory effect of C. domestica, we topically treated the mice ears with the CdE or C. domestica fractions (dichloromethane, n-butanol, and ethyl acetate) dissolved in acetone, in a skin inflammation model induced by croton oil. The single topical application of croton oil increased ear thickness with a maximum inflammatory effect of 144 ± 7 μm 6 h after its application (Figs. 2 and 3). In turn, the topical application of the vehicle (acetone) did not change the thickness of the ears of the mice (9 ± 1 μm).
Effect of topically administered CdE on acute ear edema (a) and myeloperoxidase (MPO) activity (OD/mL sample) (b) in the ears of mice that received an application of croton oil. We evaluated ear edema and MPO activity 6 h after the croton oil application. We applied the CdE (0.01–1 mg/ear) immediately after the croton oil. Each bar represents the mean + SEM for six animals. ###p < 0.001 when compared to the vehicle (acetone) and naive groups; *p < 0.05 and ***p < 0.001 when compared to the control (croton oil) group. Statistical analysis was performed using two-way ANOVA followed by a post hoc Bonferroni test
Effect of dichloromethane, n-butanol, and CdE-isolated EtAc fractions topically administered on acute ear edemas (a–c) and myeloperoxidase (MPO) activity (OD/mL sample) (d–f) in mice ears that received croton oil applications. We evaluated ear edemas and MPO activities 6 h after the croton oil applications. We applied the fractions (0.001–1 mg/ear) immediately after the croton oil. Each bar represents the mean ± SEM for six animals. ###p < 0.001 when compared to the vehicle (acetone) and naive groups; **p < 0.01, ***p < 0.001 when compared to the control (croton oil) group. Statistical analysis was performed using two-way ANOVA followed by a post hoc Bonferroni test
The CdE (0.01–1 mg/ear) and fractions (0.001–1 mg/ear) reduced the croton oil-induced ear edema, with ID50 values of 0.07 (0.05–0.1), 0.01 (0.008–0.003), 0.02 (0.005–0.06), and 0.05 (0.04–0.07) mg/ear and maximum inhibition (Imax) values of 97 ± 2, 86 ± 1, 81 ± 4, and 95 ± 2% (at 1 mg/ear) for the CdE and the dichloromethane, n-butanol, and EtAc fractions, respectively, when compared to the vehicle group (Figs. 2a and 3a–c). Dexamethasone (dissolved in acetone), which we used as a positive control, inhibited the croton oil-induced ear edema by 96 ± 2%.
We also evaluated the MPO enzyme’s activity after 6 h of the single topical application of croton oil. Croton oil caused an increase of neutrophil infiltration in the ear tissue when compared to the naive group. The CdE and the dichloromethane, n-butanol, and EtAc fractions decreased the MPO’s activity with Imax values of 69 ± 1, 54 ± 3, 43 ± 3, and 76 ± 5% (at 1 mg/ear), respectively (Figs. 2b and 3d–f). Dexamethasone reduced the neutrophil infiltration in the ear tissue by 86 ± 9%.
The histological analysis showed that croton oil caused edema and inflammatory cell infiltration compared to the naïve and vehicle groups. The CdE and different fractions (1 mg/ear) reduced both events compared to the croton oil group, and these effects were comparable to that of dexamethasone (Fig. 4). Quantitatively, the naïve, acetone, and croton oil groups presented 38 ± 2, 48 ± 2, and 180 ± 15 polymorphonuclear cells per field, while the topical treatments showed 89 ± 2 polymorphonuclear cells per field for the CdE, 135 ± 1 for the dichloromethane fraction, 136 ± 1 for the n-butanol fraction, 106 ± 1 for the EtAc fraction, and 73 ± 1 for dexamethasone (Fig. 4).
Effect of topically administered CdE (CE), dichloromethane (DI), n-butanol (BU), and EtAc (EA) on histological changes (hematoxylin-eosin ×20 and ×40) and on the number of polymorphonuclear cells per field in the ears of mice that received croton oil applications. We observed histological changes of topical treatments at 1 mg/ear and evaluated 6 h after the croton oil applications. Each bar represents the mean ± SEM for six animals. The arrows indicate the presence of polymorphonuclear cells in the ear tissue. ###p < 0.001 when compared to the vehicle (acetone) and naive groups; ***p < 0.001 when compared to the control (croton oil) group. Statistical analysis was performed using two-way ANOVA followed by a post hoc Bonferroni test
Effect of steroids quantified in the EtAc fraction of C. domestica on the croton oil-induced acute ear edema
We evaluated the topical anti-inflammatory effect of steroids (β-sitosterol, lupeol, or stigmasterol) identified and quantified in the EtAc fraction of C. domestica in a skin inflammation model induced by croton oil. The single topical application of croton oil caused ear edema with a maximum edematogenic effect of 126 ± 10 μm after 6 h of its application, when compared to the vehicle and naïve groups (Fig. 5). In turn, the topical application of the vehicle (acetone) did not significantly change the thickness of the mice ears (8 ± 1 μm).
Effect of topically administered β-sitosterol (7.5 μg/ear), lupeol (10 μg/ear), and stigmasterol (5.7 μg/ear) on the acute ear edema (a), myeloperoxidase (MPO) activity (OD/mL sample) (b), histological changes (hematoxylin-eosin ×200 and ×400) (c), and on the number of polymorphonuclear cells per field (d) in the skin of mice ears topically administered with croton oil. We applied the topical treatments immediately after the croton oil. Each bar represents the mean ± SEM for six animals. The arrows indicate the presence of polymorphonuclear cells in the ear tissue. ###p < 0.001 when compared to the vehicle (acetone) and naive groups; *p < 0.05, **p < 0.01, and ***p < 0.001 when compared to the control (croton oil) group. Statistical analysis was performed using two-way repeated measures ANOVA followed by post hoc Bonferroni (ear edema and number of polymorphonuclear cells per field) and Student Newman-Keuls (MPO activity) tests
β-sitosterol (7.5 μg/ear), lupeol (10 μg/ear), and stigmasterol (5.7 μg/ear) (all dissolved in acetone) reduced the croton oil-induced ear edema, with Imax values of 46 ± 8, 51 ± 7, and 62 ± 7%, respectively, when compared to the vehicle group (Fig. 5a). We also evaluated the activity of the MPO enzyme 6 h after the single topical application of croton oil. Croton oil increased the MPO activity in the ear tissue when compared to the naive group. β-sitosterol, lupeol, and stigmasterol decreased the MPO activity with respective Imax values of 65 ± 11, 60 ± 9, and 35 ± 11% (Fig. 5b).
Histologically, the croton oil increased the dermis thickness and the infiltration of inflammatory cells (177 ± 16 polymorphonuclear cells per field), when compared to the naïve (36 ± 2 cells) and vehicle (50 ± 3 cells) groups. β-sitosterol, lupeol, and stigmasterol reduced the ear edema and inflammatory cell infiltration (99 ± 12, 95 ± 6, and 80 ± 8 polymorphonuclear cells per field, respectively) when compared to the croton oil group (Fig. 5c, d).
Effect of C. domestica CdE and EtAc fraction gels on croton oil-induced acute ear edema
We also evaluated the topical anti-inflammatory effect of C. domestica by incorporating the CdE and EtAc fraction into gel formulations after single topical applications of croton oil.
The C. domestica CdE gel (0.03–3%; 15 mg/ear), EtAc fraction gel (0.03–1%; 15 mg/ear), and base gel (15 mg/ear) decreased the acute ear edema induced by croton oil with Imax values of 85 ± 6% (at 3%; 15 mg/ear), 82 ± 2% (at 1%; 15 mg/ear), and 42 ± 7%, respectively, when compared to the vehicle group (Fig. 6a, b). Likewise, the dexamethasone gel reduced the ear edema by 100%.
Effects of the CdE (0.03–3%; 15 mg/ear), EtAc (0.03–1%; 15 mg/ear), and base (15 mg/ear) gel formulations topically administered on the acute ear edema (a and b) and on myeloperoxidase (MPO) activity (OD/mL sample) (c and d) in mice ears that received croton oil applications. We evaluated ear edema and MPO activity 6 h after the croton oil application. We applied the topical treatments immediately after the croton oil. Each bar represents the mean ± SEM for six animals. ###p < 0.001 when compared to the vehicle (acetone) and naive groups; ***p < 0.001 when compared to the control (croton oil) group. Statistical analysis was performed using two-way ANOVA followed by a post hoc Bonferroni test
Moreover, the gel formulations of C. domestica CdE and EtAc fraction decreased the MPO enzyme’s activity, a marker of inflammatory cell infiltration, by 77 ± 3 and 67 ± 7%, respectively (Fig. 6c, d), while the dexamethasone gel inhibited the MPO activity by 96 ± 2%. A histological analysis confirmed this effect of the C. domestica gel formulations (at 1 and 3%; 15 mg/ear) (Fig. 7). Quantitatively, the naïve and croton oil groups presented 38 ± 2 and 180 ± 15 polymorphonuclear cells per field, while the topical treatments showed a number of polymorphonuclear cells per field of 113 ± 2 for the CdE gel, 96 ± 2 for the EtAc fraction gel, 133 ± 1 for the base gel, and 83 ± 1 for the dexamethasone gel (Fig. 7).
Effects of the CdE (3%; 15 mg/ear), EtAc (1%; 15 mg/ear), and base (15 mg/ear) gel formulations topically administered on histological changes (hematoxylin-eosin ×20 and ×40) and on the number of polymorphonuclear cells per field in mice ears that received croton oil applications. We evaluated the histological changes of the topical treatments 6 h after the croton oil application. Each bar represents the mean ± SEM for six animals. The arrows indicate the presence of polymorphonuclear cells in the ear tissue. ###p < 0.001 when compared to the vehicle (acetone) and naive groups; ***p < 0.001 when compared to the control (croton oil) group. Statistical analysis was performed using two-way ANOVA followed by a post hoc Bonferroni test
Effect of C. domestica CdE on chronic ear edema induced by croton oil
We induced a chronic ear edema through the repeated topical application of croton oil. The multiple applications of croton oil caused an ear edema which stabilized from the third day of the application until the last day of the experiment (day nine). Furthermore, there was an increase in MPO activity (assessed on the ninth day), when compared to the vehicle group.
After 6 days of topical treatment with C. domestica CdE or dexamethasone, ear edema was reduced as well as the infiltration of inflammatory cells (observed at the ninth day), with Imax of 77 ± 4% on the last day of the experiment (Fig. 8a). The treatment also decreased the MPO activity by 77 ± 7% (Fig. 8b). Dexamethasone inhibited the ear edema from the sixth day and the MPO activity evaluated on the ninth day with Imax values of 94 ± 2 and 83 ± 4%, respectively.
Effect of CdE topically administered on chronic ear edema (a), myeloperoxidase (MPO) activity (OD/mL sample) (b), histological changes (hematoxylin-eosin ×200 and ×400) (c), and the number of polymorphonuclear cells per field (d) in the skin of mice ears topically administered with croton oil. We applied the CdE (1 mg/ear) after administering the croton oil. We observed histological changes of the CdE at the 1-mg/ear dose. Each bar represents the mean ± SEM for six animals. The arrows indicate the presence of polymorphonuclear cells in the ear tissue. ###p < 0.001 when compared to the vehicle (acetone) and naive groups; *p < 0.05, **p < 0.01, and ***p < 0.001 when compared to the control (croton oil) group. Statistical analysis was performed using two-way repeated measures ANOVA followed by a post hoc Bonferroni test
We also assessed histological changes to the ear tissue after the chronic application of croton oil. The repeated topical application of croton oil generated severe ear edema and inflammatory cell migration when compared to the vehicle group. The CdE and dexamethasone reduced these inflammatory parameters when compared to the croton oil plus vehicle group (Fig. 8c). Quantitatively, the naïve and croton oil groups presented 38 ± 3 and 264 ± 4 polymorphonuclear cells per field, while the topical treatments with CdE and dexamethasone reduced the inflammatory cell infiltration to 110 ± 1 and 87 ± 2 cells, respectively (Fig. 8d).
Effect of C. domestica CdE on possible adverse effects
We also assessed the possible adverse effects caused by the repeated topical application of C. domestica CdE once a day for 14 days. The repeated topical treatment with C. domestica CdE caused neither body weight loss nor behavioral alterations. However, the topical application of dexamethasone decreased the animals’ body weights by 12 ± 4% (P < 0.05) when compared to the vehicle group. Moreover, the CdE significantly reduced the relative weight of kidneys by 19 ± 4% (P < 0.05), whereas the dexamethasone reduced the relative weights of kidneys and spleens by 23 ± 4% (P < 0.01) and 59 ± 9% (P < 0.001), respectively, when compared to the vehicle group.
To investigate if the C. domestica CdE alters the animals’ spontaneous and forced locomotor activity, we performed the open-field and rotarod tests. The topical treatments with CdE and dexamethasone neither altered the number of falls in the rotarod test nor the number of crossing and rearing responses in the open-field test (Table 1) when compared to the vehicle group. However, morphine (100 mg/kg; s.c.) changed the forced and spontaneous locomotion of mice when compared to the vehicle group (Table 1). Besides, we analyzed biochemical markers of toxicity through the evaluation of AST and ALT activity as well as glucose and creatinine levels. The topical administration of C. domestica CdE and dexamethasone did not alter any biochemical parameters when compared to the vehicle group (Table 2).
Discussion
Skin inflammation plays an important role in the development and progress of skin diseases, including irritant contact dermatitis. This type of contact dermatitis is triggered by skin exposure to irritant agents which alter the homeostasis of the cutaneous permeability barrier and activate the innate immunity (Lim et al. 2015; Yeom et al. 2012). Ear edema and inflammation models induced by irritant agents in mice are an interesting way to investigate new therapeutic alternatives with topical anti-inflammatory effects. The increase of skin thickness, indicative of the formation of edema, is the first step for the development of skin irritation and local inflammation, being an effective parameter to define the process that occurs during skin inflammation (Kumar et al. 2011; Saraiva et al. 2011).
We demonstrated for the first time that C. domestica fruit peels presented topical anti-inflammatory activity in acute and chronic animal models of irritant contact dermatitis induced by croton oil, thus confirming the information reported by Janovik et al. (2012b), who described the use of peel infusions of the Cariniana spp. species as a traditional remedy to treat inflammatory disorders. Thus, C. domestica fruit peels become a promising therapeutic strategy for treating skin diseases without causing adverse effects in preliminary tests.
Firstly, we evaluated the efficacy of the C. domestica CdE and its different fractions (dichloromethane, n-butanol, and ethyl acetate) (all dissolved in acetone) in an acute skin inflammation model induced by croton oil. All treatments presented topical anti-inflammatory activity against a single application of croton oil. Among the fractions, the EtAc presented surprising anti-inflammatory activity with the same efficacy of dexamethasone.
Ear edema induced by croton oil is a widely used model to investigate substances with topical anti-inflammatory effects (Cai et al. 2014; Trivellatograssi et al. 2013). Croton oil is an irritant agent which contains phorbol esters, mainly the 12-O-tetradecanoyl phorbol-13-acetate, a potent activator of protein kinase C and several other signaling pathways, which, in turn, are essential for the activation of pro-inflammatory enzymes and the release of inflammatory mediators (Cabrini et al. 2011; Pinto et al. 2015; Tian et al. 2013).
A single application of croton oil promotes an acute inflammatory process characterized by vasodilatation, edema, and the infiltration of polymorphonuclear leucocytes. Furthermore, skin neutrophil accumulation plays a critical role in cutaneous inflammation disorders, such as irritant contact dermatitis since it releases pro-inflammatory mediators that amplify the inflammatory process (Adami et al. 2012; Piana et al. 2016). Two hours after the application of croton oil, one may observe vasodilatation and ear edema, while an increase in polymorphonuclear leukocyte infiltration occurs after 6 h (Boller et al. 2010).
We demonstrated that a single topical application of croton oil caused ear edema and increased the MPO activity in the skin of mice ears. The C. domestica CdE and all its fractions reduced both inflammatory parameters induced by croton oil, indicating its possible application as a herbal medicine to treat skin inflammatory diseases.
The pharmacological action of herbal medicines possibly occurs due to a conjunct action of its constituents present in plant extracts. Therefore, the identification of these compounds is important to explain and justify its biological effects and comprise its action mechanism (Bellik et al. 2012). Since the EtAc fraction of C. domestica presented higher effectiveness against the skin inflammation induced by croton oil, we investigated its phytochemical constituents by HPLC-DAD. Among the compounds detected and quantified in the EtAc fraction, we found steroids lupeol, β-sitosterol, and stigmasterol. Thus, we evaluated the possible topical anti-inflammatory effect of these constituents on the same irritant contact dermatitis model. As expected, β-sitosterol, lupeol, and stigmasterol reduced all inflammatory parameters (ear edema and inflammatory cell infiltration) induced by the topical application of croton oil.
Our results are supported by previous studies which demonstrated the efficacy of these phytochemical compounds in the treatment of inflammatory disorders (Cabrini et al. 2011; Horinouchi et al. 2013; Medeiros et al. 2007; Pinto et al. 2015; Shah and Alagawadi 2011; Vassallo et al. 2013). These anti-inflammatory effects may occur by inhibition of transcriptional factors and/or arachidonic acid metabolism (Chibli et al. 2014; Phanse et al. 2012; Xu et al. 2014).
Besides the mechanism mentioned above, other pathways may be involved in the anti-inflammatory action of these constituents, which should be investigated in subsequent studies. Regarding the results obtained, we believe that the EtAc fraction’s anti-inflammatory effect may be due to the combined action of different phytochemical compounds since all constituents tested in this study effectively reduced the inflammatory parameters evaluated. However, we cannot exclude the fact that other phytochemical compounds compose the EtAc fraction and could also contribute to its anti-inflammatory effect.
Previous studies identified the phytochemical constituents of C. domestica fruit peels extract (CdE) and its fractions using HPLC. The chromatography profile indicated the presence of constituents with established anti-inflammatory activity such as triterpenoids (lupeol and β-amyrin), sterols (stigmasterol and β-sitosterol), flavonoids (rutin, quercetin, and kaempferol), and phenolic acids (gallic, caffeic, and chlorogenic) (Hwang et al. 2014; Janovik et al. 2012; Pandey and Negi 2016; Tsang et al. 2016). Janovik et al. (2012a) showed that especially the EtAc fraction presented all phenolic acids analyzed. These phytochemical compounds, such as phenolic acids, triterpenoids, sterols, and flavonoids, also exhibit anti-inflammatory actions in inflammation models (Chibli et al. 2014; Brum et al. 2016; Hernández-Valle et al. 2014; Passos et al. 2013; Siddiqui et al. 2016; Tsang et al. 2016).
The anti-inflammatory treatment for skin diseases preferentially occurs through the topical route, which often provides higher effectiveness than other administration routes due to the avoidance of the first-pass hepatic metabolism, besides exerting a local effect that minimizes the possible adverse effects (Chibli et al. 2014; Sigmundsdottir, 2010). We also demonstrate the topical anti-inflammatory effect of the CdE and EtAc fraction of C. domestica incorporated into gel formulations on the acute irritant contact dermatitis model induced by croton oil, given that the topical route is the most used to treat skin inflammatory diseases. We chose the CdE and EtAc to be tested in gel formulations due to previous studies published by Janovik et al. (2012a), who demonstrated that the crude extract and ethyl acetate fraction of C. domestica presented higher amounts of polyphenols with well-established anti-inflammatory action (Khan et al. 2012). Besides, our results showed that the CdE and EtAc fraction (dissolved in acetone) reduced more effectively the ear edema and MPO activity, with respective maximum inhibition values of 97 ± 2 and 95 ± 2% for ear edema and 69% ± 1 and 76 ± 5% for MPO activity compared to the other fractions evaluated. The C. domestica gel formulations also reduced both ear edema and neutrophil infiltration (measured by MPO activity and confirmed by the histological procedure), thus demonstrating that the C. domestica CdE and EtAc fraction gels are both also effective when incorporated into a gel formulation.
The pH measurements of the topical formulations (C. domestica CdE and EtAc fraction gels), kept at room temperature (25 ± 5 °C), were stable and compatible with the skin’s physiological pH value (4.6–5.8) (Silva et al. 2013). Moreover, the organoleptic characteristics remained unchanged.
We also verified the topical anti-inflammatory effect of the C. domestica CdE on a chronic irritant contact dermatitis model induced by croton oil. Repeated applications of croton oil are important to assess the response of compounds with anti-inflammatory and anti-proliferative activity, seeing that it induces epidermal hyperplasia and cutaneous inflammation, increases ear thickness, and causes polymorphonuclear leucocyte infiltration. Moreover, repeated cutaneous barrier perturbations cause a decrease in stratum corneum hydration, causing epidermal hyperplasia and skin inflammation signs. These events are similar to those observed in the chronic subtype of irritant contact dermatitis (Eberting 2014; Saraiva et al. 2011; Yeom et al. 2012). Therefore, in this model, the C. domestica CdE reduced all chronic inflammatory parameters evaluated, showing to also be useful in the suppression of already installed skin inflammation.
There is a growing search for new topical anti-inflammatory agents which are more effective and safe than the topical anti-inflammatory drugs currently used. Plant-related compounds and extracts represent a promising alternative for the treatment of inflammatory skin diseases (Sung et al. 2016). Although their effectivity has been proven, their safety must also be established so that the risk/benefit ratio is known and to provide appropriate information to patients regarding individual protection from possible health hazards (Akindele et al. 2015).
The topical anti-inflammatory treatment with the C. domestica CdE proved to be relatively safe in preliminary toxicological tests. We verified that the daily topical application of C. domestica CdE during 14 days did not change the body weight of animals but slightly reduced the kidney weight. However, dexamethasone treatment reduced the animals’ spleen and body weights. These alterations caused by dexamethasone may indicate toxicity signs after exposure to toxic substances (Akindele et al. 2015).
Moreover, the topical application of C. domestica CdE and dexamethasone did not alter the locomotor or biochemical parameters evaluated. As expected, morphine (positive control) demonstrated forced and spontaneous motor activity changes in mice, which is consistent with previous studies (Fialho et al. 2017). Unfortunately, there are few reports about the possible toxicity caused by the use of C. domestica. Although the topical application may induce fewer adverse effects than when administered systematically, we preliminarily evaluated the development of possible adverse effects caused by the crude extract of C. domestica after its repeated topical application. However, our preliminary results are the first pieces of evidence regarding the toxicological profile of C. domestica, and they do not confirm that it is fully safe. To ensure the safety profile of C. domestica, it would be interesting to evaluate, in subsequent studies, the toxicity caused by its acute and chronic systemic administration in preclinical assays. Therefore, it is crucial to thoroughly evaluate the notion that therapies with natural products do not present adverse effects, so to avoid the indiscriminate use of natural products with proven pharmacological activity (Akindele et al. 2015).
Conclusion
Although C. domestica did not show superior efficacy to dexamethasone, our results suggest that formulations containing its extract can be an interesting anti-inflammatory prototype for the treatment of inflammatory skin diseases, given that C. domestica reduced the inflammatory parameters in acute and chronic irritant contact dermatitis models induced by croton oil.
Abbreviations
- CdE:
-
Crude extract of C. domestica
- MPO:
-
Myeloperoxidase
- NF-κB:
-
Factor nuclear kappa B
- ICD:
-
Irritant contact dermatitis
- ID50 :
-
Inhibitory dose 50%
- I max :
-
Maximal inhibition
- HTAB:
-
Hexadecyltrimethylammoniumbromide
- TMB:
-
Tetramethylbenzidine
- EDTA:
-
Diaminoethanetetraacetic
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- s.c.:
-
Subcutaneous
- SEM:
-
Standard error of the mean
- TPA:
-
12-O-Tetradecanoylphorbol-13-acetate
- PKC:
-
Protein kinase C
- PLA2 :
-
Phospholipase A2
- AP-1:
-
Activating protein-1
References
Adami M, Prudente A d S, Mendes DAGB, Horinouchi CD d S, Cabrini DA, Otuki MF (2012) Simvastatin ointment, a new treatment for skin inflammatory conditions. J Dermatol Sci 66:127–135
Akindele AJ, Unachukwu EG, Osiagwu DD (2015) 90 days toxicological assessment of hydroethanolic leaf extract of Ipomoea asarifolia (Desr.) Roem. and Schult. (Convolvulaceae) in rats. J Ethnopharmacol 174:582–594
Bangert C, Brunner PM, Stingl G (2011) Immune functions of the skin. Clin Dermatol 29:360–376
Bellik Y, Boukraâ L, Alzahrani HA, Bakhotmah BA, Abdellah F, Hammoudi SM, Iguer-Ouada M (2012) Molecular mechanism underlying anti-inflammatory and anti-allergic activities of phytochemicals: an update. Molecules 18:322–353
Boligon AA, Piana M, Kubiça TF, Mario DN, Dalmolin TV, Bonez PC, Weiblen R, Lovato L, Alves SH, Campos MMA, Athayde ML (2015) HPLC analysis and antimicrobial, antimycobacterial and antiviral activities of Tabernaemontana catharinensis A. DC. J Appl Biomed 13:7–18
Boller S, Soldi C, Marques MCA, Santos EP, Cabrini DA, Pizzolatti MG, Zampronio AR, Otuki MF (2010) Anti-inflammatory effect of crude extract and isolated compounds from Baccharis illinita DC in acute skin inflammation. J Ethnopharmacol 130:262–266
Brum TF, Camponogara C, da Silva Jesus R, Belke BV, Piana M, Boligon AA, Pires FB, Oliveira SM, da Rosa MB, de Freitas Bauermann L (2016) Ethnopharmacological study and topical anti-inflammatory activity of crude extract from Poikilacanthus glandulosus (Nees) Ariza leaves. J Ethnopharmacol 193:60–67
Cabrini DA, Moresco HH, Imazu P, Pietrovski EF, Gasparin DA, Mendes B, Prudente S, Pizzolatti MG, Brighente MC, Otuki MF (2011) Analysis of the potential topical anti-inflammatory activity of Averrhoa carambola L. in mice. Evid Based Complement Alternat Med 2011:1–7
Cai C, Chen Y, Zhong S, Ji B, Wang J, Bai X, Shi G (2014) Anti-inflammatory activity of N-butanol extract from Ipomoea stolonifera in vivo and in vitro. PLoS One 9:1–9
Chibli LA, Rodrigues KCM, Gasparetto CM, Pinto NCC, Fabri RL, Scio E, Alves MS, Del-Vechio-Vieira G, Sousa OV (2014) Anti-inflammatory effects of Bryophyllum pinnatum (lam.) Oken ethanol extract in acute and chronic cutaneous inflammation. J Ethnopharmacol 154:330–338
Choi J, Kim S (2013) Rutin suppresses atopic dermatitis and allergic contact dermatitis. Exp Biol Med 238:410–417
Cunha LC, Azeredo FS, Mendonça ACV, Vieira MS, Pucci LL, Valadares MC, Freitas HOG, Sena ÂAS, Lino RDS (2009) Avaliação da toxicidade aguda e subaguda, em ratos, do extrato etanólico das folhas e do látex de Synadenium umbellatum Pax. Rev Bras Farmacogn 19:403–411.
Di Meglio P, Perera GK, Nestle FO (2011) The multitasking organ: recent insights into skin immune function. Immunity 35:857–869
Eberting CL (2014) Irritant contact dermatitis: mechanisms to repair. J Clin Exp Dermatol Res 5:4–11
Feingold KR, Schmuth M, Elias PM (2007) The regulation of permeability barrier homeostasis. J Invest Dermatol 127:1574–1576
Fialho MFP, Brusco I, Brum S, Piana M, Boligon AA, Trevisan G, Oliveira SM (2017) Buddleja thyrsoides Lam. crude extract presents antinociceptive effect on an arthritic pain model in mice. 474, 2993–3010
Hernández-Valle E, Herrera-Ruiz M, Salgado GR, Zamilpa A, Ocampo MLA, Aparicio AJ, Tortoriello J, Jiménez-Ferrer E (2014) Anti-inflammatory effect of 3-O-[(6'-O-palmitoyl)-β-D-glucopyranosyl sitosterol] from Agave angustifolia on ear edema in mice. Molecules 19:15624–15637
Horinouchi CDDS, Mendes DAGB, Soley BDS, Pietrovski EF, Facundo VA, Santos ARS, Cabrini DA, Otuki MF (2013) Combretum leprosum Mart. (Combretaceae): potential as an antiproliferative and anti-inflammatory agent. J Ethnopharmacol 145:311–319
Hwang SJ, Kim YW, Park Y, Lee HJ, Kim KW (2014) Anti-inflammatory effects of chlorogenic acid in lipopolysaccharide-stimulated RAW 264.7 cells. Inflamm Res 63:81–90
Ibrahim B, Sowemimo A, Van Rooyen A, Van De Venter M (2012) Antiinflammatory, analgesic and antioxidant activities of Cyathula prostrata (Linn.) Blume (Amaranthaceae). J Ethnopharmacol 141:282–289
Janovik V, Boligon A, Bandeira R, Athayde M (2011) HPLC/DAD analysis, determination of total phenolic and flavonoid contents and antioxidant activity from the leaves of Cariniana domestica (Mart) Miers. Res J Phytochem 5:209–215
Janovik V, Boligon A, Athayde M (2012a) Antioxidant activities and HPLC/DAD analysis of phenolic and carotenoids from the barks of Cariniana domestica (Mart.) Miers. Res J Phytochem 6:105–112
Janovik V, Boligon AA, Frohlich JK, Schwanz TG, Pozzebon TV, Alves SH, Athayde ML (2012b) Isolation and chromatographic analysis of bioactive triterpenoids from the bark extract of Cariniana domestica (Mart) Miers. Nat Prod Res 26:66–71
Khan AQ, Khan R, Qamar W, Lateef A, Ali F, Tahir M, Rehman MU, Sultana S (2012) Caffeic acid attenuates 12-O-tetradecanoyl-phorbol-13-acetate (TPA)-induced NF-κB and COX-2 expression in mouse skin: abrogation of oxidative stress, inflammatory responses and proinflammatory cytokine production. Food Chem Toxicol 50:175–183
Kumar KG, Dhamotharan R, Kulkarni NM, Mahat MYA, Gunasekaran J, Ashfaque M (2011) Embelin reduces cutaneous TNF-α level and ameliorates skin edema in acute and chronic model of skin inflammation in mice. Eur J Pharmacol 662:63–69
Lee HY, Stieger M, Yawalkar N, Kakeda M (2013) Cytokines and chemokines in irritant contact dermatitis. Mediat Inflamm 2013:1–7
Lee J, Choi YY, Kim MH, Han JM, Lee JE, Kim EH, Hong J, Kim J, Yang WM (2016) Topical application of Angelica sinensis improves pruritus and skin inflammation in mice with atopic dermatitis-like symptoms. J Med Food 19:98–105
Lim KM, Bae SJ, Koo JE, Kim ES, Bae ON, Lee JY (2015) Suppression of skin inflammation in keratinocytes and acute/chronic disease models by caffeic acid phenethyl ester. Arch Dermatol Res 307:219–227
Lisby S, Baadsgaard O (2010) Mechanisms of irritant contact dermatitis, in: Duus, J.J., Frosch, P.J., Leppoittevin, J.P. (Eds.), Contact dermatitis pp. 69–82
Mcgrath JC, Lilley E (2015) Implementing guidelines on reporting research using animals (ARRIVE etc.): new requirements for publication in BJP. Br J Pharmacol 172:3189–3193
Medeiros R, Otuki MF, Avellar MCW, Calixto JB (2007) Mechanisms underlying the inhibitory actions of the pentacyclic triterpene α-amyrin in the mouse skin inflammation induced by phorbol ester 12-O-tetradecanoylphorbol-13-acetate. Eur J Pharmacol 559:227–235
Mendes DAGB, Soley BDS, Prudente ADS, Sponchiado G, Ferreira BGA, dos Santos MC, de Andrade ASM, Amorim CDM, Bresolin TMB, Meyre-Silva C, Zuffellato-Ribas KC, Assreuy J, Otuki MF, Cabrini DDA (2016) Hydroalcoholic extract of Sapium glandulatum (Vell.) Pax displays potent anti-inflammatory activities through a glucocorticoid receptor-dependent pathway. Phytomedicine 23:1610–1620
National Health Surveillance Agency (Anvisa) (2004) Guide of stability to cosmetic products, Brazil
Oliveira SM, Silva CR, Wentz AP, Paim GR, Correa MS, Bonacorso HG, Prudente AS, Otuki MF, Ferreira J (2014) Antinociceptive effect of 3-(4-fluorophenyl)-5-trifluoromethyl-1H-1-tosylpyrazole. A Celecoxib structural analog in models of pathological pain. Pharmacol Biochem Behav 124:396–404
Pandey A, Negi PS (2016) Traditional uses, phytochemistry and pharmacological properties of Neolamarckia cadamba: a review. J Ethnopharmacol 181:118–135
Passos GF, Medeiros R, Marcon R, Nascimento AFZ, Calixto JB, Pianowski LF (2013) The role of PKC/ERK1/2 signaling in the anti-inflammatory effect of tetracyclic triterpene euphol on TPA-induced skin inflammation in mice. Eur J Pharmacol 698:413–420
Phanse MA, Patil MJ, Abbulu K, Chaudhari PD, Patel B (2012) In-vivo and in-vitro screening of medicinal plants for their anti-inflammatory activity: an overview. J Appl Pharm Sci 2:19–33
Piana M, Silva MA, Trevisan G, De Brum TF, Silva CR, Boligon AA, Oliveira SM, Zadra M, Hoffmeister C, Rossato MF, Tonello R, Laporta LV, De Freitas RB, Belke BV, Da Silva Jesus R, Ferreira J, Athayde ML (2013) Antiinflammatory effects of Viola tricolor gel in a model of sunburn in rats and the gel stability study. J Ethnopharmacol 150:458–465
Piana M, Camponogara C, Boligon AA, Machado MM, De Brum TF, Oliveira SM, De Freitas Bauermann L (2016) Topical anti-inflammatory activity of Solanum corymbiflorum leaves. J Ethnopharmacol 179:16–21
Pinto NDCC, Machado DC, Da Silva JM, Conegundes JLM, Gualberto ACM, Gameiro J, Moreira Chedier L, Castañon MCMN, Scio E (2015) Pereskia aculeata miller leaves present in vivo topical anti-inflammatory activity in models of acute and chronic dermatitis. J Ethnopharmacol 173:330–337
Proksch E, Brandner JM, Jensen JM (2008) The skin: an indispensable barrier. Exp Dermatol 17:1063–1072
Santos EN, Lima JC, Noldin VF, Cechinel-Filho V, Rao VS, Lima EF, Schmeda-Hirschmann G, Sousa PT Jr, Martins DT (2011) Anti-inflammatory, antinociceptive and antipyretic effects of methanol extract of Cariniana rubra stem bark in animal models. An Acad Bras Cienc 83:557–566
Saraiva RA, Araruna MKA, Oliveira RC, Menezes KDP, Leite GO, Kerntopf MR, Costa JGM, Rocha JBT, Tomé AR, Campos AR, Menezes IRA (2011) Topical anti-inflammatory effect of Caryocar coriaceum Wittm. (Caryocaraceae) fruit pulp fixed oil on mice ear edema induced by different irritant agents. J Ethnopharmacol 136:504–510
Seyfarth F, Schliemann S, Antonov D, Elsner P (2011) Dry skin, barrier function, and irritant contact dermatitis in the elderly. Clin Dermatol 29:31–36
Shah AS, Alagawadi KR (2011) Anti-inflammatory, analgesic and antipyretic properties of Thespesia populnea Soland ex. Correa seed extracts and its fractions in animal models. J Ethnopharmacol 137:1504–1509
Siddiqui F, Naqvi S, Abidi L, Faizi S, Avesi L (2016) Opuntia dillenii cladode: opuntiol and opuntioside attenuated cytokines and eicosanoids mediated inflammation 182, 221–234
Silva MA, Trevisan G, Klafke JZ, Rossato MF, Walker CIB, Oliveira SM, Silva CR, Boligon AA, Flores FC, Silva CDB, Athayde ML, Ferreira J (2013) Antinociceptive and anti-inflammatory effects of Aloe saponaria haw on thermal injury in rats. J Ethnopharmacol 146:393–401
Simpson BS, Luo X, Costabile M, Caughey GE, Wang J, Claudie DJ, McKinnon RA, Semple SJ (2014) Polyandric acid A, a clerodane diterpenoid from the Australian medicinal plant Dodonaea polyandra, attenuates pro-inflammatory cytokine secretion in vitro and in vivo. J Nat Prod 77:85–91
Slodownik D, Lee A, Nixon R (2008) Irritant contact dermatitis: a review. Australas J Dermatol 49:1–11
Sung YY, Lee AY, Kim HK (2016) Forsythia suspensa fruit extracts and the constituent matairesinol confer anti-allergic effects in an allergic dermatitis mouse model. J Ethnopharmacol 187:49–56
Tian H, Matsuo Y, Fukunaga A, Ono R, Nishigori C, Yodoi J (2013) Thioredoxin ameliorates cutaneous inflammation by regulating the epithelial production and release of pro-inflammatory cytokines. Front Immunol 4:1–12
Trevisan G, Rossato MF, Walker CIB, Oliveira SM, Rosa F, Tonello R, Silva CR, Machado P, Boligon AA, Martins MAP, Zanatta N, Bonacorso HG, Athayde ML, Rubin MA, Calixto JB, Ferreira J (2013) A novel, potent, oral active and safe antinociceptive pyrazole targeting kappa opioid receptors. Neuropharmacology 73:261–273
Trivellatograssi L, Malheiros A, Meyre-Silva C, Da Silva Buss Z, Monguilhott ED, Fröde TS, Da Silva KABS, De Souza MM (2013) From popular use to pharmacological validation: a study of the anti-inflammatory, anti-nociceptive and healing effects of Chenopodium ambrosioides extract. J Ethnopharmacol 145:127–138
Tsang, M.S.M., Jiao, D., Chan, B.C.L., Hon, K.L., Leung, P.C., Lau, C.B.S., Wong, E.C.W., Cheng, L., Chan, C.K.M., Lam, C.W.K., Wong, C.K., 2016. Anti-inflammatory activities of pentaherbs formula, berberine, gallic acid and chlorogenic acid in atopic dermatitis-like skin inflammation. Molecules 21
Vassallo A, De Tommasi N, Merfort I, Sanogo R, Severino L, Pelin M, Della Loggia R, Tubaro A, Sosa S (2013) Steroids with anti-inflammatory activity from Vernonia nigritiana Oliv. & Hiern. Phytochemistry 96:288–298
Xiao X, Xie H, Jian D, Deng Y, Chen X, Li J (2015) Rebounding triad (severe itching, dryness and burning) after facial corticosteroid discontinuation defines a specific class of corticosteroid-dependent dermatitis. J Dermatol 42:697–702
Xu Q, Wang Y, Guo S, Shen Z, Wang Y, Yang L (2014) Anti-inflammatory and analgesic activity of aqueous extract of Flos populi. J Ethnopharmacol 152:540–545
Yeom M, Kim SH, Lee B, Han JJ, Chung GH, Choi HD, Lee H, Hahm DH (2012) Oral administration of glucosylceramide ameliorates inflammatory dry-skin condition in chronic oxazolone- induced irritant contact dermatitis in the mouse ear. J Dermatol Sci 67:101–110
Acknowledgments
We thank Professor Margareth Linde Athayde for donating the extract of C. domestica. We also thank the professor of the Program in Biological Sciences: Toxicological Biochemistry (Federal University of Santa Maria), Vera Morsh, for loaning equipment.
Funding
This study was supported by the Conselho Nacional de Desenvolvimento Científico e Tecnológico-CNPq, Coordenação de Aperfeiçoamento de Pessoal de Ensino Superior - CAPES/PROEX (process no. 23038.005848/2018-31; grant no. 0737/2018) (Brazil), and the Fundação de Amparo à Pesquisa do Estado do Rio Grande do Sul - FAPERGS and the Conselho Nacional de Desenvolvimento Científico e Tecnológico - CNPq (grant no. 16/2551-0000281-9) and FAPERGS (Grant no. 17/2551-0001082-5). CC is recipient of fellowship from CAPES/PROEX (process no. 88882.182152/2018-01) and SMO is recipient of fellowship from CNPq (Grant no. 307220/2017-6). We also acknowledge fellowships from CNPq and CAPES.
Author information
Authors and Affiliations
Contributions
Participated in research design: G.B.M, C.C., C.R.S., S.M.O.
Conducted experiments: G.B.M, C.C., C.R.S., S.M.O.
Plant material and extractions, gel preparation, accelerated stability study, data analysis, writing, and discussion of these: M.P.
Performed data analysis: C.C., C.R.S., S.M.O.
Wrote or contributed to the writing of the manuscript: G.B.M, C.C., C.R.S., S.M.O.
All the authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare.
Ethical approval
All procedures performed in studies involving animals were in accordance with the ethical standards of the institution (approved by Institutional Committee for Animal Care and Use of the Federal University of Santa Maria, number process 9475221015/2015) and guidelines of Brazilian Council of Animal Experimentation—CONCEA—and of U.S. Public Health Service’s Policy on Humane Care and Use of Laboratory Animals—PHS Policy) were also followed.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Milani, G.B., Camponogara, C., Piana, M. et al. Cariniana domestica fruit peels present topical anti-inflammatory efficacy in a mouse model of skin inflammation. Naunyn-Schmiedeberg's Arch Pharmacol 392, 513–528 (2019). https://doi.org/10.1007/s00210-018-1594-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-018-1594-1