Abstract
Chronic kidney disease (CKD) is a global healthcare problem; however until now, there is no effective treatment that can stop its progression. In this study, we aimed to investigate the effect of empagliflozin, a sodium-glucose linked transporter-2 inhibitor (SGLT2I) in a model of unilateral ureteric obstruction (UUO) in rats, as a model of progressive renal interstitial fibrosis in vivo and the possibility of inclusion of klotho protein. Rats were randomly divided into five groups: group 1: control group, group 2: UUO untreated group, group 3: prophylactic SGLT2I treatment before UUO, group 4: immediate SGLT2I treatment after UUO, and group 5: delayed SGLT2I treatment (this group received distilled water 1 week after UUO then empagliflozin for 2 weeks). At the end of the experiment period, animals were sacrificed, and kidney fibrotic and inflammatory parameters were measured. Also kidney sections were examined histopathologically for CTGF expression. UUO resulted in renal dysfunction and fibrosis through upregulating inflammatory cascade (NF-κB-TLR4) as well as many fibrotic pathways (as TGF-β1, αSMA, Wnt, CTGF, and fibronectin) with significant reduction in the klotho protein expression. We hypothesized that both prophylactic and immediate treatment with empagliflozin after UUO in rats exert more renoprotective effect in comparison with delayed treatment via enhancement of renal klotho expression and activity, for further investigations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic kidney disease (CKD) is a global healthcare problem, and its prevalence in adult over 20 years of age was around 12% in female and 10% in male in the recent analysis (Mills et al. 2015).
CKD progression is characterized by increased inflammatory and profibrotic cytokines with progressive loss of nephrons as a result of the accumulation of extracellular matrix (ECM) components, resulting in a decline in the renal function over years (Tucker et al. 2015).
CKD often occurs secondary to other disorders including hypertension, infection, aging nephropathy, and diabetes mellitus. Most cases with CKD are well diagnosed before they reach the end stage of renal failure; however until now, there is no effective treatment that can stop the progressive loss of nephrons or retard the progressive decline in renal functions (Lewis et al. 2001). Irrespective of the initial cause, accumulation of ECM and interstitial fibrosis are the common pathological alteration in CKD (Roberts et al. 1997).
Klotho is a membrane-bound protein expressed mainly in the kidney distal tubule as well as in the sinoatrial node, choroid plexus, and parathyroid gland (Takeshita et al. 2004). Recent data showed that klotho expression depressed with any damage to the kidney. Also it has been discovered that klotho protein plays an important anti-fibrotic effect on several organs (Barker et al. 2015).
In diabetic nephropathy and some models of renal fibrosis, klotho expression is concurrently decreased and possibly exacerbating the development of fibrosis (Deng et al. 2015). Indeed, klotho expression is associated with inhibition of TGFB1 and fibronectin induced upregulation of fibrosis and collagen expression which makes klotho as a potential target for prevention of renal fibrosis (Satoh et al. 2012).
Sodium-glucose linked transporter-2 inhibitors (SGLT2I) are a novel approach for treatment of diabetes mellitus type 2. At present, only few studies evaluated the effect of SGLT2 inhibition on renoprotection in CKD.
Several studies suggested that elevation of interstitial glucose concentration contributes to tubular ECM synthesis and consequently development of renal fibrosis in diabetic nephropathy, and according to these findings, SGLT2 inhibition is associated with reduction of fibrotic markers (Panchapakesan et al. 2013).
Indeed, some studies demonstrated the renoprotective effect of empagliflozin, one of the SGLT2I, in diabetic kidney disease (Wanner et al. 2016).
Based on the above, we evaluated the effect of empagliflozin in a model of unilateral ureteric obstruction (UUO) in rats, as a model of progressive renal interstitial fibrosis in vivo and the possibility of inclusion of klotho protein.
Materials and methods
Materials
The following materials were used: empagliflozin (Behringer, Ingelheim, Germany); urethane: urethane (Sigma Chemical Co., St. Louis, MO); Quantichrom urea assay kit, Quantichrom creatinine assay kit (Bio Assay systems, Hayward, USA); TGF-β1 rat ELISA kit (KAMIYA BIOMEDICAL COMPANY, KT-30309, Seattle, USA); fibronectin rat ELISA kit (My BioSource, USA); NF-κB rat ELISA kit (CUSABIO-Biotech, Co., China); TLR4 rat ELISA kit (CUSABIO-Biotech, Co., China); α-SMA rat ELISA kit (CUSBIO-Biotech, Co., China); Wnt-1 rat ELISA kit (CUSABIO-Biotech, Co., China); PCR Master Mix for klotho (Applied Bio-systems).
Animal welfare and ethical statements
Forty adult male Wistar rats weighing 200–220 g were obtained from animal house unit, Faculty of Veterinary Medicine, Zagazig University, Egypt. Animals were allowed to be accustomed for a period of time (1 week) at the animal facility of Faculty of Medicine, Zagazig University. Rats were housed at constant temperature (22 ± 2 °C) and light-controlled room on alternating 12:12 h and constant humidity (60 ± 10%). Free access to standard rat food and water ad libitum. The study was in accordance with protocol approved by the local Animal Ethical Committee of Zagazig University, Egypt. Experimental design and animal handling were carried out in accordance with the guidelines of the US national institutions of health on laboratory animals use and care.
Unilateral ureteric obstruction operation
UUO is one of the established models for chronic renal interstitial fibrosis (Chevalier et al. 2009). It was performed according to Schinner et al. (2013). The animals were anesthetized with ketamine and chlorpromazine, 100 and 0.75 mg/kg/i.p., respectively, and each rat’s abdominal wall was shaved first; a midline abdominal incision was made. The left kidney was brought to the surface and the ureter was located and tied with surgical silk at transition of proximal to distal ureter. Sham-operated animals were subjected to the same incision and manipulation of the ureter without ligation (Radovic et al. 2014).
Experimental design
Animals were divided into five groups (n = 8). Group I (control group) is the sham-operated group, and group II UUO untreated group (UUO). Both groups (I and II) received distilled water 1.5 ml/day p.o. for 1 week before operation and 2 weeks after operation. Group III (prophylactic SGLT2I treatment before UUO (PT)) received empagliflozin 10 mg/kg/day/p.o. (Zhou and Wu 2017) for 1 week before operation and 2 weeks after operation. Group IV is immediate SGLT2I treatment after UUO (IT). This group received empagliflozin 10 mg/kg/day/p.o. immediately after UUO for 2 weeks. Group V is delayed SGLT2I treatment (DT). This group received distilled water 1 week after UUO then empagliflozin 10 mg/kg/day/p.o. for 2 weeks.
Laboratory analysis
At the end of the experiment, fasting blood glucose (FBG) levels using an Accu-check active glucometer (Roche Diagnostics, Manheim, Germany) and body weight (BW) were estimated. Then, the animals were anesthetized with urethane (1.3 g/kg, i.p.) and samples of blood were collected from orbital sinus and serum was separated by centrifugation at 3000 rpm for 10 min. Serum was used for estimation of urea, creatinine, and sodium. The animals were euthanized by decapitation then kidneys were isolated.
Kidneys were dissected into two parts; a part was fixed in 10% neutral formalin to be used for histopathological examination. The second part was submerged in liquid nitrogen and stored at – 80 °C until analyzed.
Measurement of serum urea, creatinine, and sodium levels
Urea level was determined in serum using Quantichrom urea assay kit, and creatinine level was determined in serum using Quantichrom creatinine assay kit respectively (Bio Assay systems, Hayward, USA), according to manufacturer’s instructions. For urea, transfer 20 μl water, standard (50 mg/dl), and samples to appropriately labeled tubes. Add 1000 μl working reagent and tap lightly to mix. Incubate 20 min (50 min) and read OD520nm (OD430nm) (Ji and Bachmanov 2007). For creatinine, transfer 100 μl 2 mg/dl standard and serum samples to cuvettes. Add 1000 μl working reagent to each cuvette and pipet briefly to mix. Read OD immediately (OD0) and at 5 min (OD5) at 490–530 nm (Davalos-Misslitz et al. 2007). Serum sodium was estimated by using the colorimetric method Berry et al. (1988).
Determination of transforming growth factor beta level in kidney homogenates
The level of transforming growth factor beta (TGF-β1) was detected in the kidney homogenates using rat ELISA kits obtained from KAMIYA BIOMEDICAL COMPANY, KT-30309, Seattle, USA. Bring all reagents and samples to room temperature (18–25 °C). Add standard 50 μl to each standard well, add sample 50 μl to each sample well, and add sample diluent 50 μl to each blank/control well.
Add 100 μl of HRP-conjugate reagent to each well, cover with a closure plate membrane, and incubate for 60 min at 37 °C. Wash the plate four times. Add chromogen solution A 50 μl and chromogen solution B 50 μl to each well successively. Then protect from light to incubate for 15 min at 37 °C. Add 50 μl stop solution to each well. The color in the wells should change from blue to yellow. Read the optical density (OD) at 450 nm using an ELISA reader within 15 min after adding stop solution. Use the professional curve fitting software to make a standard curve and calculate the level.
Measurement of fibronectin level in kidney homogenates
Fibronectin was measured using ELISA (My BioSource, USA, according to the manufacturers’ instructions. This kit was based on sandwich enzyme-linked immune-sorbent assay technology. Add 100 μl standard or sample to each well for 90 min at 37 °C. Add 100 μl biotin-detection antibody working solution to each well for 60 min at 37 °C. Aspirate and wash three times. Add 100 μl SABC working solution to each well. Incubate for 30 min at 37 °C. Aspirate and wash five times. Add 90 μl TMB substrate. Incubate 15–30 min at 37 °C. Add 50 μl stop solution. Read at 450 nm immediately.
Determination of nuclear factor-kappa B concentrations in kidney homogenates
Nuclear factor-kappa B (NF-κB) levels were detected in the kidney homogenates using commercially available kits according to manufacturer’s instructions (CUSABIO-Biotech, Co., China). Bring all reagents and samples to room temperature before use. Centrifuge the sample again after thawing before the assay. Add 100 μl of standard and sample per well. Cover with the adhesive strip provided. Incubate for 2 h at 37 °C. Add 100 μl of biotin-antibody (1×) to each well. Incubate for 1 h at 37 °C. Aspirate each well and wash, repeating the process three times. Add 100 μl of HRP-avidin (1×) to each well. Cover the microtiter plate with a new adhesive strip. Incubate for 1 h at 37 °C. Repeat the aspiration/wash process for five times. Add 90 μl of TMB substrate to each well. Incubate for 15–30 min at 37 °C. Protect from light. Add 50 μl of stop solution to each well. Determine the optical density of each well within 5 min, using a microplate reader set to 450 nm.
Quantitative determination of toll-like receptor 4 level in kidney homogenates
The level of toll-like receptor 4 (TLR4) in kidney homogenates was measured using TLR4 ELISA kit (CUSABIO-Biotech, Co., China). Add 100 μl of standard and sample per well. Incubate for 2 h at 37 °C. Remove the liquid of each well, without washing. Add 100 μl of biotin-antibody (1×) to each well. Incubate for 1 h at 37 °C. Aspirate each well and wash, repeating the process two times for a total of three washes. Add 100 μl of HRP-avidin (1×) and incubate for 1 h at 37 °C. Repeat the aspiration/wash process for five times. Add 90 μl of TMB substrate to each well. Incubate for 15–30 min at 37 °C. Protect from light. Add 50 μl of stop solution to each well and gently tap the plate to ensure thorough mixing. Determine the optical density of each well within 5 min, using a microplate reader set to 450 nm.
Measurement of α-smooth muscle actin level in kidney homogenates
α-Smooth muscle actin (α-SMA) level was determined in kidney tissue homogenates using α-SMA ELISA kit of rat which was obtained from CUSBIO-Biotech, Co., China. This assay employs the quantitative sandwich enzyme immunoassay technique. Antibody specific for α-SMA has been pre-coated onto a microplate. Standards and samples are pipetted into the wells and any α-SMA present is bound by the immobilized antibody. After removing any unbound substances, a biotin-conjugated antibody specific for α-SMA is added to the wells. After washing, avidin-conjugated horseradish peroxidase (HRP) is added to the wells. Following a wash to remove any unbound avidin-enzyme reagent, a substrate solution is added to the wells and color develops in proportion to the amount of α-SMA bound in the initial step. The color development is stopped and the intensity of the color is measured. Determine the optical density of each well within 5 min, using a microplate reader set to 450 nm.
Protein Wnt-1 assay
Protein Wnt-4 level was determined by using Wnt-1 ELISA kit (an enzyme-linked immunosorbent assay for quantitative determination of Wnt-4 level in tissue homogenates). The kits were purchased from CUSABIO-Biotech, Co., China. Bring all reagents and samples to room temperature before use. Centrifuge the sample again after thawing before the assay. Antibody specific for Wnt-4 has been pre-coated onto a microplate. Standards and samples are pipetted into the wells and any Wnt-4 present is bound by the immobilized antibody. After removing any unbound substances, a biotin-conjugated antibody specific for Wnt-4 is added to the wells. After washing, avidin-conjugated HRP is added to the wells. Following a wash to remove any unbound avidin-enzyme reagent, a substrate solution is added to the wells and color develops in proportion to the amount of Wnt-4 bound in the initial step. The color development is stopped and the intensity of the color is measured. Determine the optical density of each well within 5 min, using a microplate reader set to 450 nm.
Real-time PCR analysis for measurement of klotho
Total RNA was extracted from tissue homogenate using SV (spin or vacuum) total RNA isolation system (Promega, Madison, WI, USA) according to manufacturer’s instruction. Complementary DNA (cDNA) was synthesized using superscript III first-stand synthesis system as described in the manufacturer’s protocol (#K1621, Fermentas, Waltham, MA, USA). PCR reaction were done using SYBR Green Master Mix (Applied Bio-systems) gene-specific primers which are shown in Table 1 and were designed with gene Runner Software (Hasting Software, Inc., Hasting, NY) from RNA sequences from the gene bank.
Quantitative RT-PCR was performed in a 25-μl reaction volume consisting of 2X SYBR Green PCR Master Mix (Applied Bio-systems), 900 nM of each primer, and 2 μl of cDNA in which all values were normalized to beta actin which was used as the control housekeeping gene and reported as fold change over background levels detected in the diseased groups.
Histology
Kidney samples were fixed in 10% buffered formalin then embedded in paraffin. Five-micrometer-thick paraffin sections were stained with hematoxylin and eosin stain (Bancroft and Gamble 2002).
Immunohistochemical staining of connective tissue growth factor
Immunohistochemical staining was carried out using the En Vision (USA) method. Tissue sections (3–5 μm) were deparaffinized in xylene and rehydrated in graded alcohol. Slides were incubated for 10 min in 3% hydrogen peroxide in order to block endogenous peroxidase activity. Dako target retrieval solution (pH 6.0) was used for 20 min. Antibody binding was detected by Dako’s HRP envision kit (Dako Cytomation, Denmark). Tissue samples were incubated with goat anti-mouse CTFG antibody (Santa Cruz Biotechnology, USA), then incubated for 1 h at room temperature (Song et al. 2004). Connective tissue growth factor (CTGF) is expressed in the cytoplasmic compartment with membranous accentuation. Based on the intensity of immunoreactivity and according to the extent of cortical interstitial fibrosis, a semi-quantitative scale of 1–4 was used to score the reactivity of the samples (scale 1, normal, all cells are negative; scale 2, weak positive cells, involvement up to 25%; scale 3, moderate, involvement of 26 to 50%; 4, strong diffuse positive staining more than 50%) (Solez et al. 1993).
Statistical analysis
Data were given as mean ± SD. One-way analysis of variance (ANOVA test) was used for analysis of data, followed by Tukey’s post hoc multiple comparison tests using SPSS software Version 19 (IBM, Armonk, NY, USA). The difference in the severity of renal fibrosis score among the treatment groups was performed by using the Kruskal-Wallis rank test. Statistically, significant difference was considered when P < 0.05.
Results
Body weight changes and fasting blood glucose levels
Regarding body weight, it was examined at the beginning of the experiment, at the end of the experiment, and also weekly but there was no significant difference detected between all groups (Table 2). Also blood glucose levels at the beginning of the experiment and at the end of the experiment were measured and there was no significant difference detected between all groups (Table 2).
The effect of empagliflozin treatment on kidney function tests and serum sodium
UUO in rats significantly (P < 0.05) increased the serum level of urea and creatinine from 28.75 ± 0.96 and 0.67 ± 0.096 mg/dl in the control group to 68.25 ± 2.75 and 2.025 ± 0.22 mg/dl respectively. Protective treatment (PT), immediate treatment (IT), and delayed treatment (DT) with empagliflozin significantly (P < 0.05) reduced serum levels of urea to 30.5 ± 2.38, 30 ± 2.94, and 35.25 ± 3.3 mg/dl respectively when compared to UUO group II. Also protective, immediate, and delayed treatment with empagliflozin significantly (P < 0.05) decreased serum levels of creatinine to 0.925 ± 0.15, 0.925 ± 0.19, and 1.375 ± 0.21 mg/dl respectively compared with UUO group II (Table 3). Our results showed significant reduction of the serum urea and creatinine levels in both group III (PT) and group IV (IT) compared to group V(DT). Table 3 shows that there was no significant difference in the serum sodium levels between all groups.
The effect of empagliflozin treatment on TGF-β1 in renal homogenates
UUO induced significant increase of TGF-β1 level in renal homogenate to 74.93 ± 1.99 ng/ml compared to the control group. Treatment with empagliflozin (PT, IT, and DT) significantly (P < 0.05) reduced TGF-β1 level to 29.08 ± 3.47, 30.4 ± 4.24, and 45.35 ± 0.82 ng/ml respectively in relation to UUO group II (Figs. 4 and 5).
The effect of empagliflozin treatment on NF-κB in renal homogenates
UUO significantly (P < 0.05) increased the level of NF-κB in renal homogenate from 1.81 ± 0.084 ng/ml in the control group to 6.305 ± 0.87 ng/ml. Treatment with empagliflozin significantly reduced NF-κB level (in the three treated groups) to 2.87 ± 0.12, 2.70 ± 0.62, and 3.84 ± 0.27 ng/ml (respectively) compared to UUO group II (Figs. 4 and 5).
The effect of empagliflozin treatment on TLR4 in renal homogenates
UUO induced significant increase of TLR4 levels in renal homogenate from 6.55 ± 0.81 ng/ml in control group to 14.75 ± 0.74 ng/ml. Treatment with empagliflozin in the three groups significantly (P < 0.05) reduced TLR4 levels to 7.68 ± 0.67, 8.33 ± 0.32, and 11.375 ± 0.82 ng/ml (respectively) in relation to UUO group II (Figs. 4 and 5).
The effect of empagliflozin treatment on α-SMA level in renal homogenates
UUO significantly (P < 0.05) increased α-SMA level in renal homogenate from 3.4 ± 0.497 ng/ml in control group to 16.88 ± 0.82 ng/ml. Treatment with empagliflozin (PT, IT, and DT) showed significant reduction of α-SMA level to 6.53 ± 0.97, 6.85 ± 0.79, and 10.15 ± 0.82 ng/ml respectively in relation to UUO group II (Figs. 4 and 5).
The effect of empagliflozin treatment on Wnt-1 level in renal homogenates
UUO significantly (P < 0.05) increased Wnt-1 level in renal homogenate from 29.18 ± 0.91 pg/ml in the control group to 70.33 ± 1.18 pm/ml. Treatment with empagliflozin in the three groups significantly decreased Wnt-1 in comparison with UUO group II to 36.73 ± 1.27, 39.23 ± 2.92, and 51.15 ± 0.82 pm/ml respectively (Figs. 4 and 5).
The effect of empagliflozin treatment on fibronectin level in renal homogenates
UUO significantly (P < 0.05) increased the level of fibronectin in renal homogenate to 13.5 ± 0.82 ng/ml compared to the control group 2.01 ± 0.82 ng/ml. Treatment with empagliflozin in the three groups significantly (P < 0.05) reduced fibronectin level in comparison with UUO group II to 5.75 ± 0.68, 6.75 ± 0.54, and 8.69 ± 0.51 ng/ml (Figs. 4 and 5).
The effect of empagliflozin treatment on klotho expression in renal homogenates
UUO significantly (P < 0.05) reduced klotho expression in the renal homogenate to 0.23 ± 0.008 compared to the control group. Empagliflozin administration (PT, IT, and DT) significantly increased klotho expression to 0.88 ± 0.017, 0.7 ± 0.045, and 0.55±0.029 respectively in relation to the UUO group II (Figs. 4 and 5). Our results showed that prophylactic treatment with empagliflozin in group III significantly increased klotho expression compared to both immediate and delayed treatment groups.
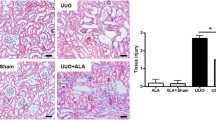
Kidney histology
The alterations in kidney tissue structure were examined under light microscopy. As presented in Figs. 1 and 2, normal group showed normal architecture of renal capsules, glomerulus, and tubules. No apparent degeneration, inflammation, or necrosis. The UUO group showed interstitial fibrosis, cystic dilatation, and inflammation. Group III (PT) showed normal kidney tissues with only features of minimal cell injury such as cystic dilatation. In group IV (IT), kidney tissues showed minimal cystic dilatation, minimal tubular necrosis, and minimal inflammation with absence of fibrosis. In group V (DT), renal tissue showed moderate tubular necrosis, cysts, tubular casts, moderate fibrosis, and inflammation.
Histopathological examination of the kidney tissues stained with H&E × 100). a Control group I—normal tubules and glomeruli. b Group II exposed to UUO—showed interstitial fibrosis, cystic dilatation, and inflammation (arrows). c Group III (PT)—normal kidney tissues showed only features of minimal cell injury such as cystic dilatation. d Group IV (IT)—kidney tissues with minimal cystic dilatation, tubular necrosis, and inflammation with absence of fibrosis. e Group V (DT)—renal tissue with moderate tubular necrosis, cysts, tubular casts, fibrosis, and inflammation
The expression level of CTGF in kidney tissue
CTGF expression levels in the kidney following UUO were evaluated by immunohistochemical analysis as represented in Fig. 2. In the UUO group, there is marked expression of the CTGF protein (staining score 4). By contrast, there are weak expressions of CTGF in the empagliflozin pretreated and treated groups compared with the UUO group (Fig. 3; Table 4).
Representative CTGF immunohistochemistry in different groups (magnification × 400). a Control group I no staining was present. b Group II exposed to UUO showed diffuse CTGF staining score 4. c Group III (PT) renal tissues stained positive for CTGF score 2. d Group IV (IT)—kidney tissues stained positive for CTGF score 2. e Group V (DT)—renal tissue stained positive for CTGF score 3
Histopathological examination of the kidney tissues stained with H&E × 100. a Group II exposed to UUO showed marked necropsy, cysts, tubular casts, fibrosis, and inflammation (H&E × 100) (arrows). b Group III (PT) showed section of improved nearly normal renal tissues (H&E × 400). c Group IV (IT) showed renal section of improved tissue with mild tubular necrosis and inflammation (H&E × 100). d Group V (DT) showed renal tissue section with mild necropsy and tubular necrosis (H&E × 100)
Discussion
Chronic kidney disease (CKD) has become a major health problem as it usually progresses to end-stage renal disease (Mills et al. 2015).
CKD is characterized by functional and/or structural abnormalities of the kidney, and the development of gradual loss of the kidney function with fibrosis in the glomeruli and interstitial space is a common pathological alteration (Hodgkins and Schnaper 2012). Despite the prevalence of this problem, the current therapeutic agents for CKD are mostly ineffective (Figs. 4 and 5).
The effect of empagliflozin treatment on a NF-κB, b TLR4, c α-SMA, d TGF-β1, e Wnt-1, f klotho (mRNA), and g fibronectin levels in renal homogenates of rats subjected to UUO. Data represent mean ± SD; n = 8; (P < 0.05). UUO unilateral ureteric obstruction. (a) means significant with the control group. (b) means significant with the UUO group. (c) means significant with prophylactic SGLT2I treated group. (d) means significant with immediate SGLT2I treated group
The effect of empagliflozin treatment on a NF-κB, b TLR4, c α-SMA, d TGF-β1, e Wnt-1, f klotho (mRNA), and g fibronectin levels in renal homogenates of rats subjected to UUO. Data represent mean ± SD; n = 8; P < 0.05. (a) means significant with the control group. (b) means significant with the UUO group. (c) means significant with prophylactic SGLT2I treated group. (d) means significant with immediate SGLT2I treated group
Among the recent developed antidiabetic drugs, sodium-glucose co-transporter-2 inhibitors (SGLT2I) were found to elicit renoprotective properties in diabetic kidney diseases of some animal models (Gembardt et al. 2014; Gallo et al. 2016). Experimental studies focused on SGLT2I renoprotective role in the nondiabetic kidney disorders are limited. Accordingly, this study was designed to examine the possible renoprotective effects of empagliflozin (one of the SGLT2I) as a novel pharmacological target against unilateral ureteric obstruction (UUO)-induced kidney fibrosis in rats.
In the current study, we found that empagliflozin treatment significantly decreased serum urea and creatinine levels compared to UUO group whether prophylactic or curative treatment. Furthermore, we observed that NF-κB expression in the renal tissues significantly decreased with empagliflozin treatment whether (prophylactic or curative). The NF-κB is an important transcription factor minimally expressed in the cell cytoplasm. However, when cells were stimulated by oxidative stress or cytokines, NF-κB was activated and translocated to the nucleus to regulate gene transcription (Qi et al. 2016). NF-κB activation plays an important role in inflammatory signals and fibrosis; therefore, its activation can directly contribute to fibroblast activation and renal fibrosis (Huang et al. 2017).
Panchapakesan et al. 2013 demonstrated that diabetic nephropathy resulted in increased NF-κB levels which in turn resulted in increased expression of toll-like receptor-4 (TLR4) and enhanced interleukin-6 secretion in human proximal tubule cell line.
TLR4 is an important regulatory factor for immunological and inflammatory response. In addition, Zhou et al. 2015 found that TLR4/NF-κB-dependent pathway can promote renal fibrosis by facilitating the macrophage shift to M1 phenotype responsible for renal fibrosis. Results of the current study showed elevation in renal TLR4 expression after UUO. In addition, our work revealed that oral administration of empagliflozin either prophylactic or curative can downregulate the TLR4/NF-κB signaling pathway indicating that empagliflozin can indirectly suppress renal fibrosis. Consistent with our results, Compbell et al. (2011) have suggested that TLR4 expressed in macrophage and renal epithelial cells can dramatically increase in UUO, therefore promoting renal fibrosis. Also, in parallel to our results, Panchapakesan et al. (2013) showed that empagliflozin can attenuate TLR/4-NF-κB pathway in human proximal tubule cell line exposed to high glucose level. In addition, Lei et al. (2017) showed that relaxin can suppress renal interstitial fibrosis in mice by downregulating the TLR4-NF-κB signaling pathway.
Our results revealed marked increase in renal TGF-β1 content associated with activation of extracellular matrix (ECM) and development of renal fibrosis as indicated also by elevated renal α-SMA and fibronectin expression in rats subjected to UUO. Notably, after kidney injury, kidney tissues undergo a series of events including cellular activation with production and secretion of pro-inflammatory cytokines. These cytokines provide signaling for guiding infiltration of inflammatory cells to the injured sites. These inflammatory cells produce ROS as well as more inflammatory and fibrogenic cytokines (Eddy 2000). These effects, in turn, stimulate tubular epithelial cells, mesangial cells, and fibroblasts to produce large amount of ECM.
The hallmarks of fibroblasts and mesangial cellular activation increase the expression of α-smooth muscle actin (α-SMA) and fibronectin. α-SMA level closely correlates with the degree of fibrosis in the kidney and predicts the severity of the decline in the kidney function (Hewitson 2009).
Transforming growth factor β1 (TGF-β1) and connective tissue growth factor (CTGF) play a critical role in ECM accumulation and renal fibrosis. Upregulation of TGF-β1 and CTGF can also stimulate mesangial cells and fibroblast differentiation to myofibroblasts expressing more ECM (Schnaper et al. 2003).
Deposition of large amount of ECM led to tubular atrophy, microvascular retraction, destruction of renal parenchyma, and finally loss of kidney function (Zeisberg and Nelison 2010).
In this work, renal TGF-β1 content and renal expression of α-SMA and fibronectin were reduced in the three empagliflozin treated groups. These results are in accordance with the previous study of Wetzl et al. (2017) who reported that zaprinast and serelaxin have beneficial effects on kidney fibrosis by modulating α-SMA and fibronectin in UUO in mice. In addition, Zhang et al. (2010) demonstrated that low-dose paclitaxel can lessen the interstitial fibrosis in the kidney of rat UUO model by reduction of TGF-β1 expression.
The present immunohistochemical findings showed that the fibrogenic factor CTGF protein expression was significantly elevated by the UUO in relation to the control group. On the other hand, empagliflozin (treatment and pretreatment) significantly decreased the expression of CTGF compared to the UUO group. Similar findings were observed by Ojima et al. (2015) who reported that empagliflozin treatment for 4 weeks significantly blocked the increased CTGF expression in diabetic rats. In the same context, Libin et al. (2018) reported that emodin (a natural active component from Chinese herbs) prevented surgery-induced renal fibrosis in rats through downregulating the expression of TGF-β1 and CTGF.
Wnt protein plays an important role in the formation of renal fibrosis (Mesar et al. 2012), and disturbance of Wnt signaling is linked to some human diseases including tissue fibrosis and tumorigenesis (Zhou and Liu 2015).
Zhou et al. (2017) demonstrated that Wnt ligands were upregulated in kidney fibrosis associated with UUO; in the same study, they also showed that blockade of Wnt secretion from renal tubules ameliorated kidney fibrosis and downregulated fibroblast activation. Wang et al. (2011) also showed that activation of Wnt/β catenin pathway resulted in podocyte dysfunction and injury with development and progression nephropathy.
In the same context, MacDonald et al. (2009) demonstrated that Wnt signaling pathway has been activated by diabetic nephropathy leading to increased expression of downstream signaling β-catenin factor and contributed to cell proliferation, migration, apoptosis, and other dysfunctions.
This work revealed that oral administration of prophylactic and curative empagliflozin showed significant reduction in renal Wnt expression compared with UUO group.
Klotho is an important membrane-bound protein expressed primarily in the kidney tubules. It represents one of the most promising anti-fibrotic strategies in renal fibrosis (Asai et al. 2012).
In 2015, Barker et al. demonstrated that any damage or injury to the kidney resulted in depression of klotho expression. Deficiency of klotho in mice results in many disorders including osteoporosis, gonadal atrophy, pulmonary emphysema, and vascular calcification (Kuro et al. 1997). On the other aspect, normalization of klotho expression protects against cardiac diseases (Yang et al. 2015), pulmonary damage (Ravikumar et al. 2014), renal disease (Hu et al. 2017), neurodegenerative disease (Brobey et al. 2015), and diabetes (Lin and Sun 2015). Many effects of klotho protein are mediated through modulation of several signaling pathways including TGF-β1 (Doi et al. 2011), IGF-1 (Wolf et al. 2008), and Wnt (Zhou et al. 2013).
Klotho protein exerts marked anti-fibrotic effects through these pathways. Sugiura et al. (2012) found that klotho-deficient mice have been shown increased ECM deposition by mesangial cells. They also found that klotho-deficient mice exhibited marked renal fibrosis and higher expression of α-SMA, fibronectin, and TGF-β1. In addition, Deng et al. (2015) found that in diabetic nephropathy, klotho expression is markedly decreased with exacerbated renal fibrosis.
In the same context, Wu et al. (2017) and Doi et al. (2011) found that when UUO was performed in mice and they treated with different concentrations of recombinant klotho protein, klotho resulted in a dose-dependent reduction of renal fibrosis as well as decreased α-SMA and collagen I expression. Another line of evidence demonstrated klotho expression as a treatment of renal fibrosis was introduced by Hu et al. (2010) and Shi et al. (2015) who found that bilateral ischemia reperfusion injury (IRI) in mice with over expression of klotho resulted in less fibrosis and less expression of pro-fibrotic markers like α-SMA, collagen I, and CTGF compared to klotho-deficient mice. Taken together, it is well established that development and exacerbation of renal fibrosis in many different models are mainly associated with klotho deficiency.
The results of the present work demonstrated that prophylactic and curative treatment with empagliflozin resulted in a significant upregulation of renal klotho expression when compared to UUO group.
Conclusion
Considering all previous findings, we can hypothesize that UUO resulted in renal dysfunction and fibrosis through many mechanisms including upregulating inflammatory cascade (NF-κB-TLR4) as well as many fibrotic pathways (as TGF-β1, αSMA, Wnt, CTGF, and fibronectin) with significant reduction in klotho expression.
We also hypothesized that treatment (prophylactic and curative) with empagliflozin could protect against UUO-induced renal dysfunction and fibrosis in rats via reduction of inflammatory and fibrotic cascades as well as via enhancement of renal klotho expression and activity. These results also demonstrated that prophylactic and immediate treatment with empagliflozin after UUO in rats exerted more renoprotective effect in comparison with delayed treatment with the same drug, for further investigations.
To our knowledge, this study gives us novel insights into the renal protective effect of empagliflozin as SGLT2I drug via upregulating klotho expression in UUO in rats.
Abbreviations
- SGLT2I:
-
Sodium-glucose linked transponter-2 inhibitors
- UUO:
-
Unilateral ureteric obstruction
- TNF-α:
-
Tumor necrosis factor-α
- TGF-β1 :
-
Transforming growth factor beta
- NF-κB:
-
Nuclear factor κB
- TLR4:
-
Toll-like receptor-4
- α-SMA:
-
Alpha-smooth muscle actin
- CTGF:
-
Connective tissue growth factor
References
Asai O, Nakatani K, Tanaka T, Sakan H, Imura A, Yoshimoto S, Samejima KI, Yamaguchi Y, Matsui M, Akai Y, Konishi N, Iwano M, Nabeshima Y, Saito Y (2012) Decreased renal α-Klotho expression in early diabetic nephropathy in humans and mice and its possible role in urinary calcium excretion. Kidney Int 81(6):539–547
Bancroft JD, Gamble M (2002) Theory and practice of histological techniques. 5th.Ed. Churchill Livingstone Pub, Edinburgh, pp 175–175
Barker SL, Pastor J, Carranza D, Quinones H, Griffith C, Goetz R, Mohammadi M, Ye J, Zhang J et al (2015) The demonstration of alpha klotho deficiency in human chronic kidney disease with a novel synthetic antibody. Nephrol Dial Transplant 3:228–233
Berry MN, Mazzachi RD, Pejakovic M, Peake MJ (1988) Enzymatic determination of sodium in serum. Clin Chem 34:2295–2298
Brobey RK, German D, Sonsalla PK, Gurnani P, Pastor J, Hsieh CC, Papaconstantinou J, Foster PP, Kuro-o M, Rosenblatt KP (2015) Klotho protects dopaminergic neuron oxidant-induced degeneration by modulating ASK1 and P38 MAPK signaling pathways. PLoS One 10:e0139914
Chevalier RL, Forbes MS, Thornhill BA (2009) Ureteral obstruction as a model of renal interstitial fibrosis and obstructive nephropathy. Kidney Int 75:1145–1152. https://doi.org/10.1038/ki.2009.86
Compbell MT, Hile KL, Zhang H, Asanuma H, Vanderbrink BA, Rink RR, Meldrum KK (2011) Toll-like receptor 4: a novel signaling pathway during renal fibrogenesis. J Surg Res 168:e61–e69
Davalos-Misslitz ACM, Rieckenberg J, Willenzon S, Worbs T, Kremmer E, Bernhardt G, Förster R (2007) Generalized multi-organ autoimmunity in CCR7-deficient mice. Eur J Immunol 37:613–622
Deng M, Lou Y, Li Y, Yang Q, Deng X, Wu P, Ma H (2015) Klotho gene delivery ameliorates renal hypertrophy and fibrosis in streptozotocin-induced diabetic rats by suppressing the rho associated called-coil kinase. Signal Pathway Mol Med Rep 12:45–54
Doi S, Zou Y, Togao O, Pastor JV, John GB, Wang L, Shiizaki K, Gotschall R, Schiavi S, Yorioka N, Takahashi M, Boothman DA, Kuro-o M (2011) Klotho inhibits transforming growth factor-beta 1 (TGF-beta 1) signaling and suppresses renal fibrosis and cancer metastasis in mice. J Biol Chem 286:8655–8665
Eddy AA (2000) Molecular basis of renal fibrosis. Pediatr Nephrol 15:290–301
Gallo LA, Ward MS, Fotherngham AK, Zhuang A, Borg DJ, Flemming NB et al (2016) Once daily administration of the SGLT2 inhibitor, empagliflozin, attenuates markers of renal fibrosis without improving albuminuria in diabetic db/db mice. Sci Res 6:26428
Gembardt F, Bartaun C, Jarzebaska N, Mayoux E, Todorov VT, Hohenstein B et al (2014) The SGLT2 inhibitor empagliflozin ameliorates early features of diabetic nephropathy in BTBR ob/ob type 2 diabetic mice with and without hypertension. Am J Physiol Renal Physiol 307:F317–F325
Hewitson TD (2009) Renal tubulointerstitial fibrosis: common but never simple. Am J Physiol Renal Physiol 296:F1239–F1244
Hodgkins KS, Schnaper HW (2012) Tubulointerstitial injury and the progression of chronic kidney disease. Pediatr Nephrol 27(6):901–902
Hu MC, Shi M, Zhang J, Quinones H, Juro-O M, MOE OW (2010) Klotho deficiency is an early biomarker of renal ischemia-reperfusion injury and its replacement is protective. Kidney Int 78:1240–1251
Hu MC, Shi M, Gillings N, Flores B, TYakashi M et al (2017) Recombinant alpha klotho may be prophylactic and therapeutic for acute to chronic kidney disease progression and uremic cardiomyopathy. Kidney Int 91:1104–1114
Huang J, Chen Z, Li J, Chen Q, Li J, Gong W, Huang J, Liu P, Huang H (2017) Protein kinase GK2a catalytic subunit ameliorates diabetic renal inflammatory fibrosis via NF-kappa B signaling pathway. Biochempharmacol 132:102–117
Ji H, Bachmanov AA (2007) Differences in postingestive metabolism of glutamate and glycine between C57BL/6ByJ and 129P3/J mice. Physiol Genomics 31(3):475–482
Kuro-O M, Matsumura Y, Aizawa H, Kawaguchi H, Suga T, Utsugi T et al (1997) Mutation of the mouse klotho gene leads to a syndrome resembling ageing. Nature 390:45–51
Lei C, Ming LS, Deng L, Yi-Ping Z, Xing JW et al (2017) Relaxin abrogates renal interstitial fibrosis by regulating macrophage polarization via inhibition of toll-like receptor 4 signaling. Oncotarget 8(13):21044–21053
Lewis EJ, Hunsicker LG, Clarke WR, Berl T, Phohl MA, Lewis JB, Ritz E, Atkins RC, Rohde R, Raz I (2001) Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med 345:851–860
Libin M, Hua L, Shuchao Z, Xiaoling X, ·Kean C et al. (2018) Emodin ameliorates renal fibrosis in rats via TGF-β1/Smad signaling pathway and function study of Smurf 2. Int Urol Nephrol 50:373–382. https://doi.org/10.1007/s11255-017-1757-x
Lin Y, Sun Z (2015) In vivo pancreatic beta cell-specific expression of antiaging gene klotho, a novel approach for preserving beta-cells in type 2 diabetes. Diabetes 64:1444–1458
MacDonald BT, Tamai K, He X (2009) Wnt/B-catenin signaling: components mechanisms and diseases. Dev Cell 17(1):9–26
Mesar I, Kes P, Jukie NB (2012) A role of WNT in kidney development and function. Acta Media Croatica 66(Suppl. 2):56–58
Mills KT, Xu Y, Zhang W, Bundy JD, Chen CS, Kelly TN, Chen J, He J (2015) A systematic analysis of worldwide population-based data on the global burden of chronic kidney disease in 2010. Kidney Int 88(5):950–957
Ojima A, Matsui T, Nishino Y, Nakamura N, Yamagishi S (2015) Empagliflozin, an inhibitor of sodium-glucose cotransporter 2 exerts anti-inflammatory and anti-fibrotic effects on experimental diabetic nephropathy partly by suppressing AGEs-receptor axis. Horm Metab Res 2 47(09):686–692. https://doi.org/10.1055/s-0034-1395609
Panchapakesan V, Pegg K, Gross S, Komala MG, Mudaliar H, Forrbes J, Pollock C, Mather A (2013) Effects of SGLT2 inhibition in human kidney proximal tubular cells-renoprotection in diabetic nephropathy? PLoS One 8(2): e544423-2
Qi M, Yin L, Xu L, Tao X, Qi Y, Han X, Wang C, Xu Y, Sun H, Liu K, Peng J (2016) Dioscin alleviates lipopolysaccharide-induced inflammatory kidney injury via the microRNA let-71/TLR4/MayD88 signaling pathway. Pharmacol Res 111:509–522
Radovic N, Aralica G, Liubanovic DG, Jelecv U, Kontek M (2014) Effect of unilateral ureteral obstruction and anti-angiotensin II treatment on renal tubule cell apoptosis and intestinal fibrosis in rats. Coll Antropol, Jun 38(2):583–588
Ravikumar P, Ye J, Zhang J, Pinch SN, Hu MC, Kuro-O M et al (2014) Alpha-klotho protects against oxidative damage in pulmonary epithelia. Am J Physiol Lung Cell Mol Physiol 307:L566–L575
Roberts IS, Burrows C, Shanks JH, Venning M, McWilliam LJ (1997) Interstitial myofibroblasts: predictors of progression in membranous nephropathy. J Clin Pathol 50:123–127
Satoh M, Nagasu H, Morita Y, Yamaguchi TP, Kanwar YS, Kashihara N (2012) Klotho protects against mouse renal fibrosis by inhibiting Wnt signaling. Am J Physiol Renal Physiol 303:F1641–F1651
Schinner E, Schramm A, Kees F, Hofmann F, Schlossmann J (2013) The cyclic GMP-dependent protein kinase Ialpha suppresses kidney fibrosis. Kidney Int 84:1198–1206
Schnaper HW, Hayashida T, Hubchak SC, Poncelet AC (2003) TGF-beta signal transduction and mesangial cell fibrogenesis. Am J Physiol Renal Physiol 284:F243–F252
Shi M, Flores B, Gillings N, Bian A, Cho HJ, Yan S et al (2015) Alpha klotho mitigates progression of AK1 to CKD through activation of autophagy. J Am Soc Nephrol 27:2331–2345
Solez K, Axelsen RA, Benediktsson H, Burdick JF, Cohen AH, Colvin RB, Croker BP, Droz D, Dunnill MS, Halloran PF, Häyry P, Jennette JC, Keown PA, Marcussen N, Mihatsch MJ, Morozumi K, Myers BD, Nast CC, Olsen S, Racusen LC, Ramos EL, Rosen S, Sachs DH, Salomon DR, Sanfilippo F, Verani R, von Willebrand E, Yamaguchi Y (1993) International standardization of criteria for the histologic diagnosis of renal allograft rejection: the Banff working classification of kidney transplant pathology. Kidney Int 44:411–422
Song Y, Li C, Cai L (2004) Fluvastatin prevents nephropathy likely through suppression of connective tissue growth factor-mediated extracellular matrix accumulation. Exp Mol Pathol 76:66–75
Sugiura H, Yoshida S, Shiohira S, Kohei J, Mitobe M, Kurosu H et al (2012) Reduced klotho expression level in kidney aggravates renal interstitial fibrosis. Am J Physiol Renal Physiol 302:F1252–F1264
Takeshita K, Fujimori T, Kurotaki Y, Honjo H, Tsujikawa H, Yasui K, Lee JK, Kamiya K, Kitaichi K, Yamamoto K, Ito M, Kondo T, Iino S, Inden Y, Hirai M, Murohara T, Kodama I, Nabeshima Y (2004) Sino arterial node dysfunction and early unexpected death of mice with a defect of klotho gene expression. Circulation 109:1776–1782
Tucker PS, Scanlan AT, Dalbo VJ (2015) Chronic kidney disease influences multiple systems: describing the relationship between oxidative stress, inflammation, kidney damage, and concomitant disease. Oxidative Med Cell Long:806358, 8 pages
Wang D, Dai C, Li Y, Liu Y (2011) Canonical growth factor-β1-driven podocyte injury and proteinuria. Kidney Int 80(11):1159–1169
Wanner C, InZucchi SE, Lachin JM, Fitchelt D, von Eynatten M, Mattheus M et al (2016) Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med 375:1801–1802
Wetzl V, Schinner E, Kees F, Faerber L, Schlossmann J (2017) Differences in renal antifibrotic Cgmp/Cgki-dependent signaling of serelaxin, zaprinast and their combination. Naunyn-Schmiedeberg Arch Pharmacol 390:939-948
Wolf L, Levanon-Cohen S, Bose S, Ligumsky H, Sredni B, Kanely H et al (2008) A tumor suppressor and a modulator of the IGF-1 and FGF pathways in human breast cancer. Oncogene 27:7094–7105
Wu NL, Xie J, An SW, Oliver N, Barrezueta NX, Lin MH et al (2017) Inhibition of TRPC6 channels ameliorates renal fibrosis and contributes to renal protection by soluble klotho. Kidney Int 91:830–841
Yang K, Wang C, Nie L, Zho X, Gu J, Guan X, Wang S et al (2015) Klotho protects against indoxyl sulphate-induced myocardial hypertrophy. J Am Soc Nephrol 26:2434–2446
Zeisberg M, Nelison EG (2010) Mechanisms of tubulointerstitial fibrosis. J Am Soc Nephrol 21:1819–1834
Zhang D, Suin L, Xian W, Liu F, et al (2010) Low-dose paclitaxel ameliorates renal fibrosis in rat UUO model by inhibition of TGF-β/smad activity. Lab Investig 90: 436–447
Zhou L, Liu Y (2015) Wnt/B-catenin signaling and podocyte dysfunction ion proteinuria kidney disease. Nat Rev Nephrol 11:535–545
Zhou Y, Wu W (2017) The sodium-glucose-co-transporter 2 inhibitor empagliflozin, protects against diabetic cardiomyopathy by inhibition of endoplasmic reticulum stress pathway. Cell Physical Biochem 41(6):2503–2512
Zhou L, Li Y, Zhou D, Tan RJ, Liu Y (2013) Loss of klotho contributes to kidney injury by depression of wnt/β-catenin signaling. J Am Soc Nephrol 24:771–785
Zhou Y, Zhang T, Wang X, Wei X, Chen Y, Guo L, Zhang J, Wang C (2015) Curcumin modulates macrophage polarization through the inhibition of the toll-like receptor 4 expression and its signaling pathways cell physical. Biochem 36:631–641
Zhou D, Fu H, Zhang L, Zhang K, Min Y, et al (2017) Tubule-derived wnts are required for fibroblast activation and kidney fibrosis. J Am Soc Nephrol 28 https://doi.org/10.1681/ASN.2016080902
Acknowledgments
The authors thank the associate prof. Hayam Rashed, associate prof. of pathology, Zagazig University Egypt, for his kind help in histopathological examination.
Author information
Authors and Affiliations
Contributions
Noha A.T. Abbas, Mohammed M. Awad, and Amal El. Salem designed experiments. Noha A. T. Abbas and Amal El. Salem performed the experiments. Noha A. T. Abbas and Amal El. Salem wrote the paper. Mohammed M. Awad revised and finalized the manuscript.
Corresponding author
Ethics declarations
All experimental protocols were approved by the ethics committee of Zagazig University. The study was approved by the local Animal Ethical Committee of Zagazig University, Egypt. All experimental procedures were carried out in accordance with the guidelines set forth by the National Institutes of Health (USA).
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Abbas, N.A.T., El. Salem, A. & Awad, M.M. Empagliflozin, SGLT2 inhibitor, attenuates renal fibrosis in rats exposed to unilateral ureteric obstruction: potential role of klotho expression. Naunyn-Schmiedeberg's Arch Pharmacol 391, 1347–1360 (2018). https://doi.org/10.1007/s00210-018-1544-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-018-1544-y