Abstract
Effects of treatment of middle-aged male rats with 3, 5, 7, 3′, 4′-pentamethoxyflavone (PMF) on vascular and perivascular adipose tissue (PVAT) functions and blood chemistry were investigated. Rats received PMF (22 mg/kg), orally or vehicle, twice a day for 6 weeks. The PMF-treated rats had lower serum glucose, higher HDL-C levels, but no change in other parameters. Thoracic aortic and mesenteric rings of PMF treated rats produced lower maximal contraction to phenylephrine that was normalized by NG-nitro-L-arginine (L-NA) or endothelial removal. The aortic- and mesenteric rings of the PMF treated rats showed improved relaxation to acetylcholine, but not to glyceryl trinitrate, and had higher eNOS protein. DL-propargylglycine (PAG) caused greater increase in the baseline tension of the PMF-treated aortic ring and higher contraction to low concentrations of phenylephrine. PVAT lowered the contractile response of the L-NA pretreated aortic rings to phenylephrine for both groups, but PAG had no effect. The cystathionine-γ-lyase (CSE) protein of the thoracic rings, but not of the PVAT, shows increased expression after PMF treatment. Overall, PMF treatment of middle aged rats appeared to increase production of NO and H2S from the blood vessels by upregulating the expression of eNOS and CSE. PMF also decreased fasting serum glucose and increased HDL-C levels, with no toxicity to liver and kidney functions. Thus, PMF is a novel compound for possible use as a health product to prevent and/or to reduce the development of diabetes type II and/or cardiovascular disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular disease is one of the leading causes of global death and disability, and it imposes a huge burden on healthcare costs (Yazdanyar and Newman 2009). Although the etiology for cardiovascular diseases is multifactorial, age is one of the main risk factors (Herrera et al. 2010; Lakatta 2002, 2015). Age impairs vascular endothelial functions, and this becomes detectable during the middle age of normal humans and animals (El Assar et al. 2012; Hongo et al. 1988; Koga et al. 1989; Redheuil et al. 2010; Rodriguez-Manas et al. 2009).
It is now well established that the perivascular adipose tissue (PVAT), the adipose tissue surrounding blood vessels, exerts anti-contractile effects on various vascular beds including those of the thoracic aorta (Sun et al. 2013) by releasing adiponectin, angiotensin-(1-7), nitric oxide, H2S, and other unknown relaxing factors called PVAT-derived relaxing factors (PVRF) (Beltowski et al. 2010; Chang et al. 2013; Dubrovska et al. 2004; Fang et al. 2009; Gil-Ortega et al. 2010; Lohn et al. 2002). The anti-contractile effect of PVAT is impaired in conditions of metabolic syndrome, hypertension, and aging (Galvez-Prieto et al. 2012; Gil-Ortega et al. 2010; Lu et al. 2011; Ma et al. 2010; Melrose et al. 2013; Szasz et al. 2012). The impaired anti-vasocontractile response of PVAT to norepinephrine in the thoracic aorta of an obese rat with a high free fatty acid level can be restored by reducing the free fatty acid levels (Sun et al. 2013) and partially reversed by diet-induced weight loss (Bussey et al. 2014).
Kaempferia parviflora (KP) Wall Ex. Baker, black ginger, Kra-chai-dum, or Thai ginseng belongs to the family Zingiberaceae. In Thai traditional medicine, rhizomes of this plant have been used for many purposes (see more details in Yorsin et al. 2014), but especially for the treatment of hypertension and as a male aphrodisiac (Wutythamawech 1997; Yenjai et al. 2004). In Laosfolk medicine, it has been used to lower blood sugar levels and facilitate blood flow and vitality (Akase et al. 2011). In Japan, KP extract is used as a food supplement for the treatment of metabolic syndrome (Nakao et al. 2011). A number of scientific investigations have been reported on the activities of ethanol extracts from the KP rhizome that include promoting male sexual desire (Chaturapanich et al. 2011; Sudwan et al. 2006), preventing gastric ulcers (Rujjanawate et al. 2005), anti-inflammation (Sae-wong et al. 2009; Tewtrakul and Subhadhirasakul 2008; Horigome et al. 2014), and increased blood flow (Chaturapanich et al. 2008; Malakul et al. 2011; Murata et al. 2013). An ethyl acetate extract of KP rhizome reduced obesity in spontaneously obese type II diabetic mice by suppressing accumulation of visceral and subcutaneous fat and plasma triglyceride levels (Akase et al. 2011; Shimada et al. 2011). This might be due to a stimulation of the β3-adrenergic receptors in brown adipose tissue that enhanced the utilization of triglycerides for heat production via uncoupling protein-1 in the mitochondria (Kobayashi et al. 2015; Matsushita et al. 2015; Yoshino et al. 2014). Recently, Yorsin et al. (2014) also found that a dichloromethane extract of the KP rhizomes (KPD) caused a lowering in the accumulation of body and liver lipid, as well as on plasma levels of triglycerides and glucose in middle-aged male rats after receiving an oral dose of KPD for 6 weeks. In addition, the KPD treatment caused an increase in expression of eNOS in blood vessels that sequentially enhanced the nitric oxide production to oppose vasocontraction to phenylephrine and to facilitate vasodilation to acetylcholine of the blood vessel of the middle-aged male rat. These parameters were beneficial for preventing or prolonging the development of cardiovascular diseases. However, KPD is a mixture of several polyphenolic compounds with the major constituents being 5,7-dimethoxyflavone (DMF), 3,5,7-trimethoxyflavone (TMF), and 3,5,7,3′,4′-pentamethoxyflavone (PMF). Among these three, PMF has been reported to possess an aphrodisiac activity as it caused relaxation of isolated human cavernosal strips by acting partly via the NO-cGMP pathway and inhibition of intracellular Ca2+ mobilization (Jansakul et al. 2012). Recently, Yorsin et al. (2015) also found that PMF caused relaxation of isolated thoracic aortic rings both in an endothelium-independent and endothelium-dependent fashion, partly by stimulating the release of NO and H2S. In addition, PMF also increased adipogenesis in 3T3-L1-adipocytes in cell culture experiments (Horikawa et al. 2012). Thus, in the present study, PMF, isolated from KP rhizomes, was chosen for further study to obtain more information on the action of this compound from KPD on lowering the sugar and lipid levels as well as on the improvement of vascular functions in middle-aged male rats by using the same protocol as was previously used for the KPD extracts but with additional experiments on the role of PVAT and H2S on the vascular functions. It was expected that if the PMF led to an improvement of vascular functions, as a result of its lowering of sugar and/or lipid levels in middle-aged rats with no signs of toxicity, then PMF would be a good choice for further development for use as a health product for preventing or delaying the development of cardiovascular diseases.
Materials and methods
Plant material and isolation of PMF
Fresh Rhizomes of Kaempferia parviflora were collected in Ampur Phurua, Loei Province, Thailand in April 2009. Authentication was achieved by comparison with the herbarium specimens in the Department of Biology Herbarium, Faculty of Science, Prince of Songkla University, Thailand, where a voucher specimen (Collecting No. 2548-03) of the plant material used has been deposited. The PMF was isolated from the dichloromethane extract by column chromatography and was confirmed its chemical characteristic by spectroscopic data, 1H and 13C NMR spectra as previously described (Jansakul et al. 2012). The purity of the PMF was checked by a Symmetry® C18 column (5μm, 3.9x150 mm i.d.; Waters) on an analytical HPLC that was carried out on a HP1100 system equipped with a photodiode array detector (Agilent Technologies). The column was eluted with a gradient of CH3OH: H2O + 0.05 % of trifluoroacetic acid (10:90→100: 0). The flow rate was 1 mL/min; the UV traces of the eluants were measured at 210 and 254 nm and the UV spectra (DAD) were recorded between 200 and 500 nm. The HPLC chromatograms of the PMF together with their retention times and corresponding UV spectra at 210 and 254 nm are shown in Fig. 1, which showed that purity was about 99.9 %.
For oral administration, the PMF was suspended in a mixture of tween 80, 0.2 (g): carboxy-methylcellulose sodium salt, 0.2 (g): distilled water, 10 (mL), at a concentration of 22 mg/mL. The control rat was orally gavaged with this vehicle using the same volume as that for the PMF treated rat.
Pharmacological studies
Middle-aged (12–14 month old) Wistar male rats were obtained from the Southern Laboratory Animal Facility, Faculty of Science, Prince of Songkla University. The animals were housed in controlled environmental conditions at 25 °C on a 12 h dark and 12 h light cycle and allowed access to standard food and tap water ad libitum. The animal methods employed in this study were approved by the Prince of Songkla University Animal Care and Use Committee. The investigation conformed to the Guide for the Care and Use of Laboratory Animals (Ethic No. 03/58). The rats were randomly selected into two groups, six animals for each group. The experimental group was treated by oral administration of 22 mg/kg PMF twice (9.00 a.m. and 6.00 p.m.) a day for 6 weeks. The vehicle control groups received the vehicle twice a day using the same volume as that for the PMF (1 mL/kg animal body weight) in the same period of 6 weeks. Each rat had its body weight recorded and its 24-h food intake at day 0 (1 day before receiving oral gavage of the vehicle or PMF suspension) and then every consecutive 7 days over the 6-week period.
Effects of the PMF treatment on the basal blood pressure and on the hematology and clinical biochemical analysis
The same methods as previously described (Yorsin et al. 2014) were used. At the end of the 6 weeks PMF or vehicle treatment, each rat (13–15-h fasting) was anesthetized with Nembutal (60 mg/kg). A tracheal tube was inserted into the trachea, and a small polyethylene tube was cannulated into the right common carotid artery that had been connected to a pressure transducer and a Polygraph (P7D model, Grass Company) for blood pressure and heart rate recording. The data was collected after a 40-min equilibration period, by which time the basal blood pressure and heart rate of the animal became stable.
After measuring the basal blood pressure and heart rate, the rat was killed by decapitation with a guillotine, and 5 and 2 mL of blood samples were collected from the decapitated rat and placed into a glass test tube and a plastic test tube containing EDTA, respectively. The glass container with 5 mL of blood was left at room temperature for 30 min and then centrifuged at 1200 rpm for 10 min. The serum was then collected and kept at −70 °C until measurements were made for the kidney and liver enzymes and for glucose and lipid levels. These measurements were made by enzymatic methods using the Automatic Chemistry Analyzer (Hitachi Modular P800, Germany) that was routinely operated at the Prince of Songkla University Hospital. They were carried out within 1 month of sample collection. The 2 mL of blood with EDTA was sent to the hematology laboratory for a total blood count procedure measured by the Automated Hematology Analyzer (Celltac E, Model MEK-7222K, Japan).
Effects of PMF treatment on internal organs and lipid accumulation
The decapitated rat (after removing the thoracic aorta and mesenteric artery) was dissected as previously described (Yorsin et al. 2014). Heart, lung, liver, adrenal gland, kidney, testes; visceral fats from the epididymis, testis and retroperitoneal, and subcutaneous fats were removed and weighed using the MettlerPL2001-L balance (Mettler Toledo International Inc., Switzerland).
Two pieces of liver (middle lobe) were cut, embedded into a cryostat gel, the sections (20 μm thick), were stained with oil red O (0.5% in absolute propylene glycol), and mounted with glycerine jelly for observation by light microscopy. The oil red O of each slide was extracted with 1 mL of 100% dimethyl sulfoxide (DMSO), and its absorbance was measured at 520 nm using a Thermo Fisher Scientific spectrophotometer (Model G10s UV-VIS, USA). The concentration of the oil red O was obtained from the standard curve of known concentrations of the oil red O in 100 % DMSO (μg/mL). The area of a whole liver thin section was measured using the Auto CAD 2005 program. The amount of the accumulated liver lipid was expressed in terms of μg/mL/cm2 of the liver tissue thin section area.
Preparation of the thoracic aortic rings and mesenteric artery
The thoracic aorta with adhering perivascular adipose tissue (PVAT) was removed from the decapitated rat and placed in oxygenated 37 °C Krebs-Henseleit solution. Six adjacent rings of 4–5 mm in length were cut, two rings were left with an intact PVAT, and the other four rings had their PVAT removed together with adhering connective tissue and for one ring, the endothelium layer was removed by a small cotton bud. Each aortic ring was mounted with two stainless steel hooks in a 20-mL organ bath containing Krebs-Henseleit solution of the following composition (mM): NaCl 118.3, KCl 4.7, CaCl2 1.9, MgSO4·7H2O 0.45, KH2PO4 1.18, NaHCO3 25.0, glucose 11.66, Na2EDTA 0.024, and ascorbic acid 0.09, maintained at 37 °C and bubbled with a carbogen (95 % O2 and 5 % CO2 gas mixture). One of the hooks was fixed at the bottom and the other was connected to a transducer for recording the isometric tension by a polygraph. The tissues were equilibrated for 60 min under a resting tension of 1 g, and the bath solution was replaced with pre-warmed oxygenated Krebs-Henseleit solution every 15 min.
At the end of the equilibration period, each aortic ring was tested for the viability of the endothelium by precontraction with phenylephrine (3 μM) until the response reached a plateau (5–8 min) and then addition of acetylcholine (30 μM). Endothelial viability was judged by a >65 % vasorelaxation back to the tension generated by the ring before adding the phenylephrine. Denudation was confirmed by the absence of vasorelaxation following the response to the addition of acetylcholine. The preparations were then washed several times with Krebs-Henseleit solution and allowed to fully relax for 45 min before the experimental protocol began.
The mesenteric ring was prepared as previously described (Yorsin et al. 2014). Briefly, the mesentery was removed from the decapitated rat and placed in a Petri dish with warm oxygenated Krebs-Henseleit solution. A third order branch of the mesenteric artery (diameter 200–250 μm) was cleaned of adhering fat and a section of about 2 mm long was mounted on two 40-μm stainless wires in the jaws of a10-mL-Dual-Wire Myograph chamber (model 400A, Danish Myo Technology A/S, Denmark) in 37 °C oxygenated Krebs-Henseleit solution (pH 7.4). The mesenteric artery was equilibrated for 1 h, and then normalization of the blood vessel was performed using a Lab Chart together with a DMT Normalization Module in order to determine the internal circumference as previously described (Mulvany and Halpern 1977). The vessel rings were re-equilibrated for 30 min, then the contractile response of each vessel rings was tested with 10 μM norepinephrine for 10–15 min, followed by washing several times with Krebs-Henseleit solution and equilibration for another 20 min. This procedure was repeated three times. The function of the intact endothelium was performed by precontracting the mesenteric ring with 10 μM norepinephrine for 10–15 min to reach a plateau, and then acetylcholine (30 μM) was added for relaxation.
Effects of the PMF treatment on the pharmacological vascular functions
Role of nitric oxide
At the end of 45-min re-equilibration after the functional endothelium testing, the basal tension of the thoracic aortic rings with intact endothelium and the rings without endothelium was adjusted to the optimal tension of 2 g (our preliminary experiments found that for middle-aged male rats, weight ca. 500 g, a basal tension of 2 g applied to the thoracic aortic ring gives optimal tension development in response to phenylephrine, unpublished data) and equilibration for another 10 min, and then a contractile response to a cumulative concentration-response (C-R) curve of phenylephrine was performed. This was followed by several washings, and the vessel was allowed to fully relax for 50 min. Then, the endothelium-intact aortic rings were preincubated with L-NA for 40 min, and then the second C-R curve to phenylephrine was performed.
Using two other sets of endothelium-intact thoracic aortic rings, one set was equilibrated under a basal tension of 2 g for 10 min and was then precontracted with phenylephrine (3 μM) for 10–15 min (plateau) followed by cumulative dilator C-R curves to acetylcholine. The other set was first preincubated with L-NA (3 mM) for 40 min before performing the cumulative dilator C-R curves to glyceryl trinitrate on the phenylephrine-precontracted aortic rings. The L-NA was included to prevent any activation of NOS by GTN as has been reported previously (Bonini et al. 2008; Moncada et al. 1991).
For the mesenteric artery, a cumulative C-R curve to phenylephrine and to acetylcholine (precontracted with 3 μM phenylephrine) was performed before and after incubating the blood vessels with L-NA. In the case of glyceryl trinitrate, its cumulative C-R curve was performed in the mesenteric ring (precontracted with 3 μM phenylephrine) that had been preincubated with L-NA as for the aortic preparations.
Role of PVAT and H2S
After equilibration, the endothelium-intact thoracic aortic rings with and without PVAT were incubated with L-NA for 40 min under a basal tension of 2 g. Then, a cumulative C-R curve to phenylephrine was performed in the presence of L-NA, followed by several washings and re-equilibration for 60 min in the presence of L-NA to allow full relaxation of the blood vessels to their original baseline of 2 g. After that, 10-mM DL-propargylglycine (PAG, a H2S inhibitor) was added into the incubation and left for 10–15 min until the aortic contraction reached a plateau, and the cumulative C-R curve to phenylephrine was performed in the presence of L-NA and PAG.
eNOS and CSE Western blot analysis
To analyze the expression of the eNOS and CSE enzyme, the thoracic aortae, mesenteric arteries, and PVAT of the PMF treated and vehicle control groups (n = 4) were harvested and kept at −70 °C until used. Protein extraction from the tissues and Western blot analysis were carried out as previously described (Yorsin et al. 2014). Briefly, each tissue from each animal was chopped on ice and homogenized in lysis buffer with 25 mM Tris-HCl, pH 7.6, 150 mM NaCl, 1 % NP-40, 1 % sodium deoxycholate, 0.1 % SDS, 0.5 mM EDTA and the protease inhibitor cocktail (GE Healthcare), centrifuged, and the total protein measured in the supernatants by the Biorad protein assay method. Fifty micrograms of protein was electrophoretically separated on 12 % polyacrylamide-SDS gels, and the proteins were transferred onto a nitrocellulose membrane. Nonspecific-binding sites were blocked with 5 % low fat dry milk in TBS-T (Tris buffer saline 0.1 % Tween 20) and then incubated with primary antibodies against eNOS (1:250), CSE (1:1,000), and β-actin (1:1,000) antibodies dissolved in 1 % low fat dry milk in TBS-T overnight at 4 °C [rabbit eNOS and rabbit β-actin antibodies were from Cell Signaling (USA); mouse CSE antibody was from Abnova (USA)]. Membranes were incubated with horseradish peroxidase anti-rabbit IgG antibody diluted to 1:5,000 (eNOS and β-actin) and horseradish peroxidase anti-mouse IgG antibody diluted to 1:5,000 (CSE) in 1 % low fat dry milk in TBS-T for 1 h. After being washed with TBS-T three times, the proteins were detected by an ECL chemiluminescent detection kit (Pierce) and the reaction was visualized by a chemiluminescence imaging instrument (Vilber Lourmat, France). The intensity of the bands was analyzed using the Fusion Capt Advance quantitation analysis program. To ensure equal protein loading, results were normalized to the β-actin protein expression and expressed as units relative to the β-actin densitometry.
Drugs
The following drugs were used. Acetylcholine chloride, NG-nitro-L-arginine (L-NA), norepinephrine, phenylephrine hydrochloride, DL-propargylglycine (PAG), pentobarbital, and dimethyl sulfoxide (DMSO) and oil red O were from Sigma, USA. Glyceryl trinitrate was from Mycomed, Denmark. 3, 5, 7, 3′, 4′-Pentamethoxyflavone (PMF) was isolated at the Prince of Songkla University, Thailand (Jansakul et al. 2012). Acetylcholine chloride, norepinephrine, and phenylephrine were dissolved in a solution containing NaCl 9 g/L, NaH2P04 0.19 g/L, and ascorbic acid 0.03 g/L, and the glyceryl trinitrate was dissolved in distilled water. Glyceryl trinitrate was from Mycomed, Denmark; here, sublingual tablets were dissolved in distilled water, but calculated concentrations were not confirmed and may thus have been overestimated.
Statistical analysis
Results are expressed as a mean value ± S.E.M. (n = 6 for vascular function study and N = 4 for protein expression by Western blotting). “n” is the number of animals. Statistical differences were determined by the Student’s paired or unpaired t test or by one-way ANOVA. A P value <0.05 was considered to identify a significant difference between values.
Results
Effects of 6 weeks PMF treatment on the body weight, food intake, animal blood pressure, internal organs and adipose tissue, and blood chemistry
No changes in body weight and food intake were found during the 6 week period of treatment with PMF or vehicle on the rats (Fig. 1 suppl.). Basal systolic and diastolic pressure as well as the basal heart rate of anesthetized rats were similar between the PMF- and the vehicle-treated rats (Table 1 suppl.). None of the internal organs, visceral and subcutaneous adipose tissue weight, nor of liver lipid accumulation were found to be altered after PMF treatment compared to the vehicle control group (Fig. 2 suppl. and Tables 2 and 3 suppl.). The fasting serum levels for HDL-C were higher, but not the triglycerides, cholesterol, and LDL-C of the PMF-treated rats, whereas the glucose levels were lower than for the vehicle control rats (Table 1). Serum levels of the alkaline phosphatase, serum glutamic oxaloacetic transaminase (SGOT), serum glutamic pyruvic transaminase (SGPT), blood urea nitrogen (BUN) and creatinine, and the determined hematological values of the PMF-treated rats were in the normal ranges and not different from that of the vehicle control group (Tables 4 and 5 suppl.).
Effects of PMF treatment on pharmacological vascular functions
Effect on the thoracic aorta
PMF treatment caused a lowering of the maximal contractile response of the thoracic aortic ring with an intact endothelium to phenylephrine compared to that of the vehicle control group. Pretreatment of the aortic rings with L-NA or by denudation of the vascular endothelium caused a similar significant increase in the maximal contraction with a 5-fold decrease in the EC50 values for the aortic rings to the phenylephrine of both the ones obtained from the PMF- and the vehicle-treated rats (Fig. 2a–c and Table 2).
Effect of 6 weeks oral gavage of PMF or vehicle (Veh, control) on contractile response to phenylephrine of endothelium-intact (endo, a), endothelium-intact with L-NA (b), or without endothelium (no endo, c) thoracic aorta. Values represent a mean ± S.E.M. of six animals each group. *Significantly lower than that of the vehicle control group, P < 0.05
Even though the precontraction caused by phenylephrine was less in the endothelium-intact aortae from the PMF-treated animals, the relative vasodilatation due to acetylcholine was greater in these vessels (Fig. 3a). However, dilatation to glyceryl trinitrate of the L-NA pretreated endothelium-intact aortic rings of the PMF-treated rats was similar, with no changes in their EC50 values, to that of the vehicle-treated rats (Fig. 3b and Table 3).
Effect of 6 weeks oral gavage of PMF or vehicle (Veh, control) on relaxation of the endothelium-intact thoracic aortic ring precontracted with phenylephrine to acetylcholine (a) or glyceryl trinitrate in the presence of L-NA (b). Values represent a mean ± S.E.M. of six animals. *Significantly lower than that of the vehicle control group, P < 0.05
A similar result was found for the contractile response of the mesenteric rings to phenylephrine: there was a lower maximal contraction in the PMF-treated group, with no changes in the EC50 values, compared to that of the vehicle control group. L-NA also caused a significant shift to the left of the phenylephrine C-R curve; a 2-fold decrease in the EC50 values, with a similar increase in the maximal response by both groups but now these were no longer different (Fig. 4 and Table 4).
Effect of 6 weeks oral gavage of PMF or vehicle (Veh, control) on the contractile response of the mesenteric ring to phenylephrine before and after pre-incubation with L-NA. Values represent a mean ± S.E.M. of six animals. *Significantly lower than the other groups; †significantly lower than the one with L-NA, P < 0.05
Relaxation of the mesenteric rings from the PMF-treated animals (precontracted with phenylephrine) was significantly higher in its sensitivity with no change in the EC50, but not in its maximal relaxation, in comparison with the vehicle control groups (Fig. 5a, Table 3). And this effect was eliminated in the presence of L-NA. No differences were observed in the vasorelaxation to glyceryl trinitrate on the L-NA pretreated mesenteric rings precontracted with phenylephrine, between that of the PMF- and the vehicle-treated rats (Fig. 5b, Table 3).
Effect of 6 weeks oral gavage PMF or vehicle (Veh, control) on relaxation of the mesenteric ring precontracted with phenylephrine to acetylcholine in the absence or presence of L-NA (a) or to glyceryl trinitrate in the presence of L-NA (b). Values represent a mean ± S.E.M. of six animals. *Significantly lower than that of the vehicle control group; †significantly higher than that of the corresponding control group, P < 0.05
Role of PVAT and H2S
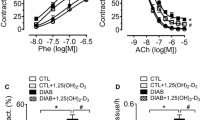
The C-R curves to phenylephrine of endothelium-intact aortic rings from the PMF-treated rats were similar to that of the vehicle control rat in the presence of PVAT and after blocking of the nitric oxide synthase by L-NA. However, the maximal contraction to phenylephrine was about 2-fold lower with a 2-fold greater increase in the EC50 compared to the one without PVAT (Fig. 6 and Table 2). Addition of PAG into the incubation medium caused a spontaneous contraction of the thoracic aortic rings that was significantly greater for the aortic rings without the PVAT of the PMF-treated rats than that for the vehicle control groups (Endo + L-NA + PAG; Veh 0.55 ± 0.30; PMF 2.2 ± 0.51). Subsequently, there was a greater contraction for low concentrations of the phenylephrine C-R curve of the PMF-treated rats than that of the vehicle control group (Fig. 6a). A small spontaneous contraction of the aortic ring with intact PVAT sometimes seen after adding the PAG for the PMF-treated rats was not statistically significant (PVAT + Endo + L-NA + PAG; Veh 0.4 ± 0.23; PMF 0.7 ± 0.40, Fig. 6b).
Effect of 6 weeks oral administration of PMF or vehicle (Veh, control) on the contractile response to phenylephrine of L-NA pretreated endothelium-intact (endo) thoracic aortic rings in the presence (right) or absence (left) of perivascular adipose tissue (PVAT) before and after incubation with PAG. Values represent a mean ± S.E.M. of six animals. *Significantly higher than the other groups, P < 0.05. Note: Miniature bar graphs in Fig. 6a, b showed the increased basal tension after addition of the PAG
eNOS and CSE Western blot analysis
The quantitative expression of the eNOS protein as determined by Western blotting from the isolated thoracic aorta and the mesenteric artery was significantly higher for those obtained from the PMF-treated rat compared to that of the vehicle control groups (Fig. 7a, b). In addition, the expression of the CSE protein in the thoracic aorta, but not in the PVAT, of the PMF-treated rats was also greater than that of the vehicle control group (Fig. 8a, b).
The effect of 6 weeks oral administration of PMF or vehicle on eNOS protein expression of the thoracic aorta and mesenteric artery compared to a vehicle control group (Veh). For each blot, β-actin expression is shown as a loading control. Each point represents a mean ± S.E.M. of four animals. *Significantly higher than the vehicle control group, P < 0.05
The effect of 6 weeks oral administration of PMF or vehicle on CSE protein expression of the thoracic aorta and PVAT compared to a vehicle control group (Veh). For each blot, β-actin expression is shown as a loading control. Each point represents a mean ± S.E.M. of four animals. *Significantly higher than the vehicle control group, P < 0.05
Discussion
We have previously shown that the oral administration of KPD to middle-aged male rats caused a lowering in the accumulation of body fat, plasma glucose, and triglycerides levels and an increase in NO production by up-regulation of the vascular eNOS protein expression in middle-aged male rats (Yorsin et al. 2014). However, KPD is a mixture of many substances with the three major compounds of DMF, TMF, and PMF that accounted for about 22 % of the dried KPD (Yorsin et al. 2014). Thus, in the present study, PMF at a dosage of 22 mg/kg was used to treat the rats, twice a day, in the same manner as was previously obtained for the KPD. As shown in the result section, PMF had no effect on body weight, body fat, or accumulation of liver lipid. This indicated that the anti-obesity effects of the KPD are unlikely to be caused by PMF. However, PMF treatment did cause a lowering in the plasma glucose levels with an increase in the HDL-C level, both of which are beneficial parameters for preventing the development of Type II-diabetes and cardiovascular disease. Matsuda et al. (2014) reported that PMF significantly increased the mRNA levels of the glucose transporter 4 (GLUT-4) of 3T3-L1 in a cell culture experiment. Thus, it was possible that the lowering of plasma glucose activity by PMF shown in the present study might be due to the enhancement of glucose uptake via the GLUT-4 of the adipose tissue and other GLUT-4-dependent cells. However, further studies on the effect of the PMF treatment on glucose transporter proteins of the adipose tissue and/or the skeletal muscle cells will be needed to confirm this possibility. The finding that the serum liver and kidney enzyme levels (ALP, SGOT, SGPT, BUN, and creatinine) together with the hematological parameters were in the normal range and were not different from the vehicle control, as well as there being no signs of gross toxicity observed. This confirmed that the PMF treatment in the present study had no effect on the liver and kidney functions and had no gross toxicities.
Although PMF treatment did not alter the basal systolic pressure, diastolic pressure, or basal heart rate in anesthetized rats, it did cause changes in vascular functions of the middle-aged rat; the animal model which was found an impairment of the endothelial functions (Chongsa et al. 2015;Yorsin et al. 2014). Thus, it was found that the thoracic aortic- and mesenteric ring of the PMF treated group had a lower contractile response to phenylephrine with an increase in the dilatation to acetylcholine (precontracted with phenylephrine) than that of the vehicle control group. The underlying mechanism for this could be due to PMF, a very poor antioxidant compound (Jakhar et al. 2014), that caused an increase in NO production from the vascular endothelial cell that opposed the vasocontraction to phenylephrine and enhanced vasodilation to acetylcholine. To support this, other experiments were performed in the presence of L-NA or by denudation of the vascular endothelium and it was established that the effects disappeared. In addition, the up-regulation of the expression of eNOS protein by the PMF-treated thoracic and mesenteric artery in comparison to the vehicle control group also supported this conclusion. However, in the present study, the rats had been treated with the PMF for 6 weeks and it could not be certain whether it was PMF itself, its metabolites and/or indirect contribution by other physiological changes that caused the endothelial cell to increase the eNOS protein expression. Thus, further experiments to explore the effect of the PMF on aortic endothelial cells eNOS protein expression would be useful.
It is unlikely that PMF treatment caused a change in the vascular smooth muscle function, as the endothelium-denuded aortic ring showed a similar contractile response to phenylephrine by the thoracic and mesenteric rings obtained from the PMF-treated and the vehicle control rats. This was supported by the finding that there was no difference in the vasodilatation to glyceryl trinitrate of the endothelium-intact aortic and mesenteric rings that had been pretreated with L-NA, to eliminate the glyceryl trinitrate-induced NO production (Bonini et al. 2008; Moncada et al. 1991) between the PMF-treated and the vehicle control groups. The lack of effect on glyceryl trinitrate induced relaxation was to some extent unexpected, since in old animals and individuals, the nitroglycerin-dependent relaxation is impaired (Oelze et al. 2014; Wenzel et al. 2008). It may be noted that the comparatively high EC50 for glyceryl trinitrate relaxation (ca. 10 nM) compared to that observed by Moncada (ca. 3 nM) may be due to the overestimation of glyceryl trinitrate concentrations as mentioned in the “Methods” section.
PMF treatment appeared to cause an increase in the basal release of H2S from the thoracic aortic ring, as it was found that PAG, the inhibitor H2S production (Hosoki et al. 1997), caused an increase in the baseline tension of the L-NA-pretreated thoracic aortic ring that was higher than that of the vehicle control group. Thus, higher vasoconstrictor responses of blood vessels from the PMF-treated animals to lower concentrations of phenylephrine were observed, although the responses to the higher phenylephrine concentrations were unaffected. These findings are consistent with the finding that the amount of the CSE protein expression by the thoracic aorta was higher for the PMF treated- than for the vehicle-treated control group. However, further study would need to clarify the mechanism that would be responsible for the increase in CSE protein by the PMF treatment.
It is unlikely that PMF affected the PVAT functions of the middle-aged male rat, as PVAT attenuated the contractile response of the thoracic aortic ring with L-NA to phenylephrine that was similar to that of the PMF treated- and the vehicle control. Furthermore, there was no change in the PVAT-H2S production after PMF treatment, although PAG did cause a rise of the baseline tension of the L-NA pretreated PVAT-intact thoracic aortic of some PMF treated rats compared to that of the vehicle control group, but the difference did not reach statistical significance. This was also supported by the finding that the amount of PVAT-CSE protein expression was similar for the PMF-treated and the vehicle control group. This would be consistent with the anti-contractile effect of PVAT being impaired in hypertension and aging (Galvez-Prieto et al. 2012; Lu et al. 2011; Szasz et al. 2012).
In conclusion, oral administration of the PMF to middle-aged male rats did not appear to cause change in vascular smooth muscle function in aorta or mesentery. However, the treatment caused an up-regulation of the expression of blood vessel eNOS and CSE proteins that resulted in an increase of NO and H2S productions to modulate the blood vessel function by opposing contraction to phenylephrine and enhancing vasodilatation to acetylcholine. PMF treatment also caused a decrease in plasma glucose and an increase in plasma HDL cholesterol levels of the rats. These finding are consistent with PMF treatment being beneficial for preventing and/or delaying the development of Type II diabetes and cardiovascular disorders. Thus, these animal data suggest that PMF is a novel compound that might be developed as a food supplement for preventing or delaying the development of diabetes and/or cardiovascular diseases in aging human beings. However, eNOS and CSE are constitutive proteins and therefore changes in their basal levels may be affecting their gene function and expression. Therefore, in future studies, levels of the mRNA of these two enzymes as well as the functional activities of the enzymes should be quantified to extend the knowledge of the present findings.
References
Akase T, Shimada T, Terabayashi S, Ikeya Y, Sanada H, Aburada M (2011) Antiobesity effects of Kaempferia parviflora in spontaneously obese type II diabetic mice. J Nat Med 65:73–80. doi:10.1007/s11418-010-0461-2
Beltowski J, Jamroz-Wisniewska A, Tokarzewska D (2010) Hydrogen sulfide and its modulation in arterial hypertension and atherosclerosis. Cardiovasc Hematol Agents Med Chem 8:173–186. doi:10.2174/187152510792481207
Bonini MG, Stadler K, Silva SO, Corbett J, Dore M, Petranka J, Fernandes DC, Tanaka LY, Duma D, Laurindo R, Mason RP (2008) Constitutive nitric oxide synthase activation is a significant route for nitroglycerin-mediated vasodilation. Proc Natl Acad Sci U S A 105:8569–8574. doi:10.1073/pnas.0708615105
Bussey C, Withers S, Edwards G, Heagerty A (2014) Obesity-related perivascular adipose tissue damage is not completely reversed following diet-induced weight loss. Heart 100(Suppl 3):A1–A138. doi:10.1136/heartjnl-2014-306118.202
Chang L, Milton H, Eitzman DT, Chen YE (2013) Paradoxical roles of perivascular adipose tissue in atherosclerosis and hypertension. Circ J 77:11–18
Chaturapanich G, Chaiyakul S, Verawatnapakul V, Pholpramool C (2008) Effects of Kaempferia parviflora extracts on reproductive parameters and spermatic blood flow in male rats. Reproduction 136:515–522. doi:10.1530/REP-08-0069
Chaturapanich G, Chaiyakul S, Verawatnapakul V, Yimlamai T, Pholpramool C (2011) Enhancement of aphrodisiac activity in male rats by ethanol extract of Kaempferia parviflora and exercise training. Andrologia 44(Suppl.1):323–328. doi:10.1111/j.1439-0272.2011.01184.x
Chongsa W, Kanokwiroon K, Jansakul C (2015) Effects of 6 weeks oral administration of Phyllanthus acidus leaf water extract on the vascular functions of middle-aged male rats. J Ethnopharmacol 156:162–174. doi:10.1016/j.jep.2015.10.10.030
Dubrovska G, Verlohren S, Luft FC, Gollasch M (2004) Mechanisms of ADRF release from rat aortic adventitial adipose tissue. Am J Physiol Heart Circ Physiol 286:H1107–H1113
El Assar M, Angulo J, Vallejo S, Peiro C, Sanchez-Ferrer CF, Rodriguez-Manas L (2012) Mechanisms involved in the aging-induced vascular dysfunction. Front Physiol 3:132. doi:10.3389/fphys.2012.00132
Fang L, Zhao J, Chen Y, Ma T, Xu G, Tang C, Liu X, Geng B (2009) Hydrogen sulfide derived from periadventitial adipose tissue is a vasodilator. J Hypertens 27:2174–2185. doi:10.1097/HJH.0b013e328330a900
Galvez-Prieto B, Somoza B, Gil-Ortega M, Garcia-Prieto CF, de Las Heras AI, Gonzalez MC, Arribas S, Aranguez I, Bolbrinker J, Kreutz R, Ruiz-Gayo M, Fernandez-Alfonso MS (2012) Anticontractile effect of perivascular adipose tissue and leptin are reduced in hypertension. Front Pharmacol 3:103. doi:10.3389/fphar.2012.00103
Gil-Ortega M, Stucchi P, Guzman-Ruiz R, Cano V, Arribas S, Gonzalez MC, Ruiz-Gayo M, Fernandez-Alfonso MS, Somoza B (2010) Adaptative nitric oxide over production in perivascular adipose tissue during early diet-induced obesity. J Endocrinol 151:3299–3306. doi:10.1210/en.2009-1464
Herrera MD, Mingorance C, Rodriguez-Rodriguez R, Alvarez de Sotomayor M (2010) Endothelial dysfunction and aging: an update. Ageing Res Rev 9:142–152. doi:10.1016/j.arr.2009.07.002
Hongo K, Nakagomi T, Kassell NF, Sasaki T, Lehman M, Vollmer DG, Tsukahara T, Ogawa H, Torner J (1988) Effects of aging and hypertension on endothelium-dependent vascular relaxation in rat carotid artery. Stroke 19:892–897. doi:10.1161/01.STR.19.7. 892
Horigome S, Yoshida I, Tsuda A, Harada T, Yamaguchi A, Yamazaki K, Inohana S, Isagawa S, Kibune N, Satoyama T, Katsuda S, Suzuki S, Watai M, Hirose N, Mitsue T, Shirakawa H, Komai M (2014) Identification and evaluation of anti-inflammatory compounds from Kaempferia parviflora. Biosci Biotechnol Biochem 78:851–860. doi:10.1080/09168451.2014.905177
Horikawa T, Shimada T, Okabe Y, Kinoshita K, Koyama K, Miyamoto K, Ichinose K, Takahashi K, Aburada M (2012) Polymethoxyflavonoids from Kaempferia parviflora induce adipogenesis on 3T3-L1 preadipocytes by regulating transcription factors at an early stage of differentiation. Biol Pharm Bull 35:686–692. doi:10.1248/bpb.35.686
Hosoki R, Matsuk N, Kimura H (1997) The possible role of hydrogen sulfide as an endogenous smooth muscle relaxant in synergy with nitric oxide. Biochem Biophys Res Commun 237:527–531. doi:10.1006/bbrc.1997.6878
Jakhar R, Paul S, Park YR, Han J, Kang SC (2014) 3,5,7,3',4'-pentamethoxyflavone, a quercetin derivative protects DNA from oxidative challenges: potential mechanism of action. J Photochem Photobiol B131:96–103. doi:10.1016/j.jphotobiol.2014.01.003
Jansakul C, Tachanaparuksa K, Mulvany MJ, Sukpondma Y (2012) Relaxant mechanisms of 3, 5, 7, 3', 4'-pentamethoxyflavone on isolated human cavernosum. Eur J Pharmacol 691:235–244. doi:10.1016/j.ejphar.2012.07.019
Kobayashi H, Horiguchi-Babamoto E, Suzuki M, Makihara H, Tomozawa H, Tsubata M, Shimada T, Sugiyama K, Aburada M (2015) Effects of ethyl acetate extract of Kaempferia parviflora on brown adipose tissue. J Nat Med. doi:10.1007/s11418-015-0936-2
Koga T, Takata Y, Kobayashi K, Takishita S, Yamashita Y, Fujishima M (1989) Age and hypertension promote endothelium-dependent contractions to acetylcholine in the aorta of the rat. Hypertension 14:542–548. doi:10.1161/01.HYP.14.5.542
Lakatta EG (2002) Cardiovascular ageing in health sets the stage for cardiovascular disease. Heart Lung Circ 11(2):76–91. doi:10.1046/j.1444-2892.2002.00126.x
Lakatta EG (2015) So! What's aging? Is cardiovascular aging a disease? J Mol Cell Cardiol 83:1–13. doi:10.1016/j.yjmcc.2015.04.005
Lohn M, Dubrovska G, Lauterbach B, Luft FC, Gollasch M, Sharma AM (2002) Periadventitial fat releases a vascular relaxing factor. FASEB J 16:1057–1063. doi:10.1096/fj.02-0024com
Lu C, Su LY, Lee RM, Gao YJ (2011) Alterations in perivascular adipose tissue structure and function in hypertension. Eur J Pharmacol 656:68–73. doi:10.1016/j.ejphar.2011.01. 023
Ma L, Ma S, He H, Yang D, Chen X, Luo Z, Liu D, Zhu Z (2010) Perivascular fat-mediated vascular dysfunction and remodeling through the AMPK/mTOR pathway in high-fat diet-induced obese rats. Hypertens Res 33:446–453. doi:10.1038/hr.2010.11
Malakul W, Ingkaninan K, Sawasdee P, Woodman OL (2011) The ethanolic extract of Kaempferia parviflora reduces ischaemic injury in rat isolated hearts. J Ethnopharmacol 137:184–191. doi:10.1016/j.jep.2011.05.004
Matsuda H, Nakamura S, Yoshikawa M (2014) Search for new type of PPARγ agonist like anti-diabetic compounds from medicinal plants. Biol Pharm Bull 37:884–891. doi:10.1248/bpb.b14-00037
Matsushita M, Yoneshiro T, Aita S, Kamiya T, Kusaba N, Yamaguchi K, Takagaki K, Kameya T, Sugie H, Saito M (2015) Kaempferia parviflora extract increases whole-body energy expenditure in humans: roles of brown adipose tissue. J Nutr Sci Vitaminol (Tokyo) 61:79–83. doi:10.3177/jnsv.61.79
Melrose HM, Heagerty A, Edwards G, Austin C (2013) Aging modulates the anti-contractile effects of perivascular adipose tissue; the role of nitric oxide. Proceedings of the Physiological Society, Proc 37th IUPS, PCC407.
Moncada S, Rees DD, Schulz R, Palmer RM (1991) Development and mechanism of a specific supersensitivity to nitrovasodilators after inhibition of vascular nitric oxide synthesis in vivo. Proc Nat Acad Sci USA 88:2166–2170. doi:10.1073/pnas.88.6.2166
Mulvany MJ, Halpern W (1977) Contractile properties of small arterial resistance vessels in spontaneously hypertensive and normotensive rats. Circ Res 41:19–26. doi:10.1161/01. RES.41.1.19
Murata K, Deguchi T, Fujita T, Matsuda H (2013) Improvement in blood fluidity by Kaempferia parviflora rhizome. J Nat Med 67:719–724. doi:10.1007/s11418-012-0729-9
Nakao K, Murata K, Deguchi T, Itoh K, Fujita T, Higashino M, Yoshioka Y, Matsumura S, Tanaka R, Shinada T, Ohfune Y, Matsuda H (2011) Xanthine oxidase inhibitory activities and crystal structures of methoxyflavones from Kaempferia parviflora rhizome. Biol Pharm Bull 34:1143–1146. doi:10.1248/bpb.34.1143
Oelze M, Kroller-Schon S, Steven S, Lubos E, Doppler C, Hausding M, Tobias S, Brochhausen C, Li H, Torzewski M, Wenzel P, Bachschmid M, Lackner KJ, Schulz E, Munzel T, Daiber A (2014) Glutathione peroxidase-1 deficiency potentiates dysregulatory modifications of endothelial nitric oxide synthase and vascular dysfunction in aging. Hypertension 63:390–396. doi:10.1161/HYPERTENSIONAHA. 113.01602
Redheuil A, Yu WC, Wu CO, Mousseaux E, de Cesare A, Yan R, Kachenoura N, Bluemke D, Lima JA (2010) Reduced ascending aortic strain and distensibility: earliest manifestations of vascular aging in humans. Hypertension 55:319–326. doi:10.1161/HYPERTENSIONAHA.109.141275
Rodriguez-Manas L, El-Assar M, Vallejo S, Lopez-Doriga P, Solis J, Petidier R, Montes M, Nevado J, Castro M, Gomez-Guerrero C, Peiro C, Sanchez-Ferrer CF (2009) Endothelial dysfunction in aged humans is related with oxidative stress and vascular inflammation. Aging Cell 8:226–238. doi:10.1111/j.1474-9726.2009.00466.x
Rujjanawate C, Kanjanapothi D, Amornlerdpison D, Pojanagaroon S (2005) Anti-gastric ulcer effect of Kaempferia parviflora. J Ethnopharmacol 102:120–122. doi:10.1016/j.jep.2005.03.035
Sae-wong C, Tansakul P, Tewtrakul S (2009) Anti-inflammatory mechanism of Kaempferia parviflora in murine macrophage cells (RAW 264.7) and in experimental animals. J Ethnopharmacol 124:576–580. doi:10.1016/j.jep.2009.04.059
Shimada T, Nagai E, Harasawa Y, Watanabe M, Negishi K, Akase T, Sai Y, Miyamoto K, Aburada M (2011) Salacia reticulata inhibits differentiation of 3T3-L1 adipocytes. J Ethnopharmacol 136:67–74. doi:10.1016/j.jep.2011.04.012
Sudwan P, Saenphet K, Saenphet S, Suwansirikul S (2006) Effect of Kaempferia parviflora Wall.ex. Baker on sexual activity of male rats and its toxicity. Southeast Asian J Trop Med Public Health 37(Suppl. 3):210–215
Sun X, Hou N, Han F, Guo Y, Hui Z, Du G, Zhang Y (2013) Effect of high free fatty acids on the anti-contractile response of perivascular adipose tissue in rat aorta. J Mol Cell Cardiol 63:169–174. doi:10.1016/j.yjmcc.2013.07.018
Szasz T, Carrillo-Sepuveda MA, Webb RC (2012) Aging decrease the anticontractile effect of perivascular adipose tissue in the mouse aorta. Hypertension 60:A260
Tewtrakul S, Subhadhirasakul S (2008) Effects of compounds from Kaempferia parviflora on nitric oxide, prostaglandin E2 and tumor necrosis factor-alpha productions in RAW264.7 macrophage cells. J Ethnopharmacol 120:81–84. doi:10.1016/j.jep.2008.07.033
Wenzel P, Schuhmacher S, Kienhofer J, Muller J, Hortmann M, Oelze M, Schulz E, Treiber N, Kawamoto T, Scharffetter-Kochanek K, Munzel T, Burkle A, Bachschmid MM, Daiber A (2008) Manganese superoxide dismutase and aldehyde dehydrogenase deficiency increase mitochondrial oxidative stress and aggravate age-dependent vascular dysfunction. Cardiovasc Res 80:280–289. doi:10.1093/cvr/cvn182
Wutythamawech W (1997) Encyclopedia of Thai Herbs I. 1st ed. Peth 69 printing, Bangkok, 288p.
Yazdanyar A, Newman AB (2009) The burden of cardiovascular disease in the elderly: morbidity, mortality, and costs. Clin Geriatr Med 25(563-577):vii. doi:10.1016/j.cger.2009.07.007
Yenjai C, Prasanphen K, Daodee S, Wongpanich V, Kittakoop P (2004) Bioactive flavonoids from Kaempferia parviflora. Fitoterapia 75:89–92. doi:10.1016/j.fitote.2003.08.017
Yorsin S, Kanokwiroon K, Radenahmad N, Jansakul C (2014) Effects of Kaempferia parviflora rhizomes dichloromethane extract on vascular functions in middle-aged male rat. J Ethnopharmacol 156:162–174. doi:10.1016/j.jep.2014.08.020
Yorsin S, Sukpondma Y, Jansakul C (2015) Vasorelaxant effects of 3,5,7,3',4'-pentamethoxyflavone isolated from Kaempferia parviflora: partly stimulating the release of NO and H2S by rat thoracic aorta. J Physiol Biomed Sci 28:5–14
Yoshino S, Kim M, Awa R, Kuwahara H, Kano Y, Kawada T (2014) Kaempferia parviflora extract increases energy consumption through activation of BAT in mice. Food Sci Nutr 2:634–637. doi:10.1002/fsn3.144
Acknowledgments
This work was supported by the Higher Education Research Promotion and National Research University Project of Thailand, Office of the Higher Education Commission. The authors thank Prof. Poungpen Sirirugsa, Department of Biology, Faculty of Science, for her kind help in identifying the plant; the Central Equipment Unit, Faculty of Science, for facilitating use of the HPLC equipment; Miss Srisurat Duangsai for technical assistance, Dr. Brian Hodgson for English assistance, and Prof. Michael J. Mulvany, Aarhus University, Denmark, for his valuable comments and editing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Yorsin, S., Kanokwiroon, K., Radenahmad, N. et al. Increased vascular eNOS and cystathionine-γ-lyase protein after 6 weeks oral administration of 3, 5, 7, 3′, 4′-pentamethoxyflavone to middle-aged male rats. Naunyn-Schmiedeberg's Arch Pharmacol 389, 1183–1194 (2016). https://doi.org/10.1007/s00210-016-1280-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-016-1280-0