Abstract
We examined the inhibitory effect of amiodarone, a class III anti-arrhythmic agent, on voltage-dependent K+ (Kv) currents in freshly isolated rabbit coronary arterial smooth muscle cells, using a whole-cell patch clamp technique. Amiodarone inhibited Kv currents in a concentration-dependent manner, with a half-maximal inhibitory concentration (IC50) value of 3.9 ± 1.44 μM and a Hill coefficient of 0.45 ± 0.14. Amiodarone did not have a significant effect on the steady-state activation of Kv channels, but shifted the inactivation current toward a more negative potential. Application of consecutive pulses progressively augmented the amiodarone-induced Kv channel inhibition. Another class III anti-arrhythmic agent, dofetilide, did not inhibit the Kv current or change the inhibitory effect of amiodarone on Kv channels. Therefore, these results strongly suggest that amiodarone inhibits Kv currents in a concentration- and state-dependent manner.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anti-arrhythmic agents are a group of pharmaceuticals that exert beneficial effects on cardiac arrhythmias. Amiodarone, a class III anti-arrhythmic agent, has remarkable clinical effects on atrial fibrillation, atrial flutter, ventricular tachycardia, and ventricular fibrillation (Carlsson et al. 2002; Kodama et al. 1999). Theoretically, prolonging the cardiac refractory period could effectively decrease cardiac arrhythmias (Hondeghem and Snyders 1990), and amiodarone has been known to prolong the cardiac action potential and thus the refractory period, by blocking rapidly activated delayed rectifier K+ currents (I Kr) (Kiehn et al. 1999). Although the clinical effects of amiodarone are beneficial, numerous side effects including vasodilation, pulmonary toxicity, and ocular and skin changes are alarming and cannot be ignored (Gessner et al. 2007). With regard to the actions of amiodarone on K+ channels, amiodarone inhibits the delayed rectifier K+ channel, the inward rectifier K+ channel, and the Na+-activated K+ channel in cardiac cells (Nishida et al. 2011). However, the effect of amiodarone on vascular Kv channels remains to be assessed.
Several K+ channels are expressed on vascular smooth muscle cell membranes, including ATP-sensitive K+ (KATP), inwardly rectifying K+ (Kir), big-conductance Ca2+-activated K+ (BKCa), and voltage-dependent K+ (Kv) channels (Clapp and Gurney 1992; Nelson and Quayle 1995; Okabe et al. 1987; Quayle et al. 1993). Most K+ channels are essential for the maintenance of membrane potential and vascular tone (Nelson and Quayle 1995) specifically, Kv channels, which are highly expressed in most vascular smooth muscle cells, are major determinants for the regulation of resting membrane potential and vascular tone in some arteries (Ko et al. 2008; Nelson and Quayle 1995; Yuan 1995). In fact, application of the Kv channel inhibitor 4-aminopyridine (4-AP) effectively induces membrane depolarization in many arteries (Hara et al. 1980; Ko et al. 2008; Nelson and Quayle 1995). Furthermore, alterations in Kv channel activity and/or expression are closely associated with circulatory and metabolic diseases such as hypertension, hypoxia, and diabetes (Archer et al. 2001; Cox et al. 2001; Liu et al. 2001). For this reason, the modulation of Kv channel expression and function is regarded as a potential therapeutic target to overcome these diseases.
Considering that amiodarone is widely used to treat cardiac arrhythmias and that vascular Kv channels are of physiological importance, the side effects of amiodarone on native vascular Kv channels should be clearly established to avoid potential vascular toxic effects.
In the present study, we investigated the effect of amiodarone on vascular Kv channels using freshly isolated rabbit coronary arterial smooth muscle cells. We clearly demonstrate that amiodarone inhibits Kv channels in a dose- and state-dependent manner.
Materials and methods
Single cell isolation
Male New Zealand White rabbits were anesthetized by simultaneous injection of sodium pentobarbital (50 mg/kg) and heparin (100 U/kg) into the ear vein. The left descending coronary arteries were isolated from the heart and cleaned of connective tissue using normal Tyrode’s solution under a stereomicroscope. The endothelium was removed by passing an air bubble through the arteries. The arteries were transferred into 1 ml of Ca2+-free normal Tyrode’s solution containing papain (1.0 mg/ml), bovine serum albumin (BSA, 1.0 mg/ml), and dithiothreitol (DTT, 1.0 mg/ml) and incubated for 25 min at 37 °C. After the first incubation, arteries were transferred into 1 ml of Ca2+-free normal Tyrode’s solution containing collagenase (2.8 mg/ml), BSA (1.0 mg/ml), and DTT (1.0 mg/ml) for 21–22 min at 37 °C. After enzymatic treatment, single cells were separated by gentle agitation in Kraft-Brühe (KB) solution with a fire-polished glass pipette. Cells were stored at 4 °C for 10 h. All animal experiments were approved by the Committee for Animal Experiments of Kangwon National University.
Solutions and chemicals
The normal Tyrode’s solution contained (mM) NaCl 135, KCl 5.4, NaH2PO4 0.33, HEPES 5, and glucose 16.6 and was adjusted to pH 7.4 with NaOH. The KB solution contained (mM) KOH 70, L-glutamate 50, KH2PO4 20, KCl 55, taurine 20, MgCl2 3, glucose 20, HEPES 10, and EGTA 0.5 and was adjusted to pH 7.3 with KOH. The pipette-filling solution contained (mM) K-aspartate, 110; KCl, 25; NaCl, 5; MgCl2, 1; Mg-ATP, 4; EGTA, 10; and HEPES, 10 and was adjusted to pH 7.2 with KOH. Amiodarone, DPO-1, and dofetilide were purchased from Tocris Cookson (Ellisville, MO) and dissolved in dimethyl sulfoxide (DMSO) or ethanol.
Electrophysiology and data analysis
A digital interface (NI-DAQ-7; National Instruments, Union, CA, USA) and an amplifier (EPC-8; Medical system Corp, Darmstadt, Germany) were used to record whole-cell currents. PatchPro software was applied to generate the pulse protocol and for data acquisition. The patch pipettes were pulled with PP-830 vertical puller (Narishige Scientific Instrument Laboratory, Tokyo, Japan) using borosilicate capillaries (Clark Electromedical Instruments, Pangbourne, UK). The patch pipette had a resistance of 3–4 MΩ when filled with the internal solution. The average cell capacitance was 13.96 pF (n = 26). All electrophysiological experiments were performed at room temperature.
Origin 7.5 software (Microcal Software, Inc., Northampton, MA, USA) was used for all data analyses. The kinetics of drug-channel interactions was described by a first-order blocking scheme (Snyders and Yeola 1995). The half-maximal inhibitory (IC50) value and the Hill coefficient (n) were obtained using concentration-dependent data fitting the following Hill equation:
where ƒ is the fractional current inhibition (ƒ = 1 − I drug / I control) at the test potential and [D] is the drug concentration.
Steady-state activation curves were obtained from tail currents elicited by returning the potential to −40 mV after depolarizing voltages of −80 to +60 mV, in 10-mV increments. The evoked tail currents at each potential were normalized using the maximal tail current. The activation curves were fitted to the Boltzmann equation as follows:
where V is the test potential, V 1/2 represents the midpoint of activation, and k is the slope factor.
A two-pulse voltage protocol was applied to obtain the steady-state inactivation curve. Currents were recorded with a 600-ms test potential to +40 mV after 7-s pre-conditioning pulses (from −80 to +30 mV in 10-mV increments) in the absence and presence of the drug. Another Boltzmann equation was used to fit the steady-state inactivation curves as follows:
where V is the test potential, V 1/2 is the potential of the half-maximal inactivation point, and k represents the slope value.
Results are presented as the means ± standard error of the mean (SEM). Statistical significance was calculated using Student’s t test, and a value of P < 0.05 was regarded as statistically significant.
Results
Amiodarone-induced inhibition of Kv currents
The effect of amiodarone on Kv currents was recorded in freshly isolated rabbit coronary arterial smooth muscle cells. To effectively exclude the interference of other K+ channels, we included the EGTA (10 mM) and ATP (4 mM) in the pipette solution to block the BKCa and KATP channels, respectively. Step-depolarizing pulses ranging from −60 to +60 mV were applied for 600 ms in increments of 10 mV to elicit the Kv currents. Figure 1a shows representative Kv currents under the control condition. Kv currents were rapidly activated and then partially inactivated by an intrinsic inactivation process. Application of amiodarone (10 μM) decreased the Kv current within 2 min (Fig. 1b). The current-voltage (I-V) relationships of steady-state currents are summarized in Fig. 1c. Amiodarone decreased the Kv current amplitude but sustained the Kv current shape. At +10 mV, application of 10 μM amiodarone decreased the Kv current by 50.33 %.
The effect of amiodarone on Kv current. Superimposed current traces were elicited with 600-ms depolarizing pulses from −60 to +60 mV at a −60-mV holding potential, in 10-mV increments under control conditions (a) and in the presence of 10 μM amiodarone (b). The current-voltage (I-V) relationship at a steady-state Kv current under control conditions (white circles) and in the presence (black circles) of 10 μM amiodarone (c). n = 6. *P < 0.05
Amiodarone inhibits Kv current in a concentration-dependent manner
Figure 2 shows the inhibitory effect of amiodarone on Kv current at various concentrations. Kv currents were elicited by applying +60 mV one-step depolarizing pulses from a holding potential of −60 mV. Amiodarone-induced Kv channel inhibition was amplified with increasing concentrations of amiodarone (0, 0.1, 0.3, 1, 3, 10, 30, 100, and 300 μM; Fig. 2a). Steady-state currents were normalized to control data and fitted to the Hill equation (Fig. 2b). The results of nonlinear least-square fitting yielded an IC50 value of 3.90 ± 1.41 μM and a Hill coefficient (n) of 0.44 ± 0.14. These results demonstrate that amiodarone inhibits Kv current in a concentration-dependent manner.
Concentration-dependent inhibition of Kv channels by amiodarone. a Representative current traces were recorded with a 600-ms one-step +40-mV depolarizing pulse from a holding potential of −60 mV in the presence of 0, 0.1, 0.3, 1, 3, 10, 30, 100, and 300 μM amiodarone. b Amiodarone-induced inhibition of the Kv current was measured at steady-state and normalized to the current amplitude observed in the absence of amiodarone. Normalized currents were fitted to the Hill equation. All n = 5
Effect of amiodarone on the steady-state activation and inactivation of Kv current
To determine whether amiodarone affected the gating properties by shifting the activation or inactivation curves, we examined the effect of amiodarone on steady-state Kv channel activation and inactivation curves. The activation curve was yielded using a tail current evoked by a typical two-pulse protocol, and the data were fitted to a Boltzmann function (see “Materials and methods”). As shown in Fig. 3b, 10 μM amiodarone did not shift the steady-state activation curve. The half-maximal potential for activation (V 1/2) and the slope value (k) were −8.16 ± 1.08 mV and 6.4 ± 0.60, respectively, under control conditions and −8.98 ± 0.85 mV and 5.96 ± 0.36, respectively, in the presence of 10 μM amiodarone.
Influence of amiodarone on Kv channel activation and inactivation curves. a Representative current traces, pulse protocol, and activation curve in the absence (white circles) and presence (black circles) of 10 μM amiodarone. Activation curves were obtained using the two-pulse protocol. The first pulse consisted of short 30–50 ms depolarizing step pulses between −80 and +60 mV in 10-mV increments at a holding potential of −80 mV. Subsequent pulses returned the membrane potential to −40 mV to elicit a tail current. n = 5. a Representative current traces, pulse protocol, and steady-state inactivation curve in the absence (white circles) and presence (black circles) of 10 μM amiodarone. The currents were obtained using a test step to +40 mV after 7-s pre-conditioning pulses of different voltages (from −80 to +30 mV in increments of 10 mV). The steady-state currents of the test pulse were normalized using the peak amplitude of the pre-pulses (left). n = 5. *P < 0.05. Absolute current amplitudes plotted against the 7-s pre-pulse potentials in the absence (white circles) and presence (black circles) of 10 μM amiodarone (right). n = 5. *P < 0.05
We obtained the steady-state inactivation curve using a conventional double-pulse protocol as described in the Materials and methods section. To fit the inactivation curve, the second pulses were normalized to the maximal currents and plotted with another Boltzmann equation. As shown in Fig. 3b (left), 10 μM amiodarone shifted the inactivation curve toward more negative potentials. The half-maximal potential for inactivation (V 1/2) and the slope value (k) were −34.52 ± 0.65 mV and 7.52 ± 0.46, respectively, under control condition and −39.62 ± 0.94 mV and 7.41 ± 0.56, respectively, in the presence of 10 μM amiodarone. These data suggest that amiodarone interacts with the channel in the inactivated state. In addition, the Kv current amplitudes at the first pulse (from −80 to +40 mV) of a double-pulse protocol were 28.15 ± 0.50 and 22.16 ± 1.04 pA/pF under control conditions and in the presence of amiodarone, respectively (Fig. 3b, right). Although the difference of the two values was statistically significant, it was much smaller than the inhibitory effect of 10 μM amiodarone on Kv currents elicited from a holding potential of −60 mV (∼50 %, see Figs. 1 and 2). These results indicate that amiodarone decreased the Kv currents by interacting with the Kv channels in their closed states as well as their inactivated states.
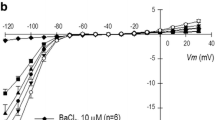
Use-dependent inhibition of Kv channels by amiodarone
To examine whether amiodarone inhibited Kv channel currents in a use-dependent manner, we applied consecutive pulses to the Kv current at frequencies of 1 and 2 Hz in the absence and presence of amiodarone. Such pulses are frequently used to test the state dependency of ion channel blockage. Under control conditions, the peak amplitude of the Kv currents reduced by 10 and 28 % at 1 and 2 Hz, respectively. However, application of 10 μM amiodarone reduced the Kv currents by 40 % (Fig. 4a) and 57 % (Fig. 4b) at 1 and 2 Hz, respectively. This data suggests that amiodarone inhibits the Kv channels in a state-dependent manner.
Frequency-dependent inhibition of the Kv current by amiodarone. Superimposed current traces elicited by 20 repeated 150-ms depolarizing pulses to +60 mV from a holding potential of −60 mV at frequencies of 1 Hz (a) and 2 Hz (b) in the absence (white circles) and presence (black circles) of 10 μM amiodarone. Each peak current was normalized by the peak current at the first pulse and plotted against the pulse number. n = 5. *P < 0.05
To further confirm that amiodarone inhibited Kv channel in a state-dependent manner, we tested its effects on Kv channels with a holding potential of −100 mV. The holding potential −100 mV was chosen over −60 mV due to the chance of a small portion of Kv channels being active or inactive at a holding potential of −60 mV. Amiodarone was applied without the depolarizing pulse for 5 min. As shown in Fig. 5a, the currents elicited by the first depolarizing pulse (first) and subsequent depolarizing pulses (second and third) did not differ at the holding potential of −60 mV. However, compared with the current elicited by the first depolarizing pulse, subsequent depolarizing pulses produced further inhibition at the holding potential of −100 mV (Fig. 5b). Taken together with the results in Figs. 3 and 4, these data also support a state-dependent inhibition of Kv channels by amiodarone.
Effect of a hyperpolarized holding potential (−100 mV) on Kv current inhibition by amiodarone. Representative current traces (upper panels) were elicited by 600-ms one-step depolarizing pulses to +60 mV at a holding potential of −60 mV (a) and −100 mV (b). Amiodarone was pre-treated for 5 min before application of depolarizing pulses. The current densities elicited by the first, second, and third at a holding potential of −60 mV (a) and −100 mV (b) in the absence (white circles) and presence (black circles) of 10 μM amiodarone were shown in the lower panels. n = 4
Effect of another class III anti-arrhythmic drug on Kv channels
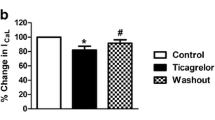
To determine whether another class III anti-arrhythmic drug inhibited Kv channels in vascular smooth muscle, we recorded the Kv current in the presence of another class III anti-arrhythmic agent, dofetilide. As shown in Fig. 4a, dofetilide (1 μM) did not inhibit Kv channel currents nor did it change the inhibitory effect of amiodarone on Kv channels (44.73 ± 0.59 pA/pF under control conditions, 44.25 ± 0.49 pA/pF in the presence of dofetilide, and 19.85 ± 1.72 pA/pF in the presence of 10 μM amiodarone + dofetilide). This reduction in Kv current amplitude by amiodarone + dofetilide did not differ from the inhibition of Kv current by amiodarone alone (Fig. 6). These results suggest that amiodarone-induced inhibition of Kv currents is completely independent of class III anti-arrhythmic function.
Effects of dofetilide, another class III anti-arrhythmic agent, on the amiodarone-induced inhibition of Kv currents. a Superimposed current traces under control conditions, in the presence of dofetilide and in the presence of dofetilide + amiodarone. b Summarized data from traces in a. n = 5, *P < 0.05. NS not significant
Inhibitory effect of amiodarone on Kv channels in the presence of Kv 1.5 inhibitor
To assess the contribution of the Kv1.5 current to amiodarone, we recorded the Kv currents in presence of Kv 1.5 inhibitor, DPO-1. As shown in Fig. 7a, the application of DPO-1 (1 μM) rapidly reduced the Kv current amplitude. Additional application of amiodarone induced the further inhibition of Kv current (45.88 ± 0.39 pA/pF under control conditions, 15.25 ± 0.48 pA/pF in the presence of 1 μM DPO-1, and 10.84 ± 0.96 pA/pF in the presence of DPO-1 + amiodarone, Fig. 7b). However, the degree of inhibition was small compared to amiodarone alone. Due to limitations in the tools available for analyzing independent Kv channel subunits, we were unable to address the detailed Kv subtypes involved in further inhibition; however, we speculate that one of the main targets of amiodarone should be the Kv1.5 subtype.
Discussion
In this study, we demonstrated the inhibitory effect of the anti-arrhythmic agent, amiodarone, on Kv channel currents in freshly isolated rabbit coronary arterial smooth muscle cells. Our results demonstrated that amiodarone inhibited the vascular Kv channel in a dose-dependent manner, regardless of cardiac I Kr inhibition. Amiodarone did not shift the steady-state activation curves of Kv channels; however, it shifted the inactivation current curves toward a more negative potential. Furthermore, amiodarone inhibited Kv channel currents in a use-dependent manner. Together, these results suggest that amiodarone inhibited the Kv channel in a dose- and state-dependent manner.
Based on our present findings, amiodarone, which is known to inhibit cardiac I Kr channels, inhibits vascular Kv channels independent of its function as a class III anti-arrhythmic agent. First, another class III anti-arrhythmic agent, dofetilide, did not affect the Kv channels or the inhibitory effect of amiodarone. Second, amiodarone-targeting I Kr channels encoded by the human ether-a-go-go-related gene (hERG, Kv11.1) have been identified mainly in the heart and in the brain, but not in vascular smooth muscle (Park et al. 2010a, 2010b). Therefore, the inhibitory effect of amiodarone on vascular Kv channels was completely independent of the inhibition of I Kr channels. Furthermore, amiodarone inhibited the Kv channels within 2 min of treatment. This fast inhibition could suggest that the inhibitory effect of amiodarone is not mediated by complicated intracellular signaling mechanisms, but it may be due to direct action by interacting with the Kv channels.
Although we were unable to address the detailed binding mechanism between amiodarone and vascular Kv channels, our data suggested that amiodarone might inhibit Kv channels in a state-dependent manner. First, amiodarone inhibited Kv channels in a use-dependent manner, which suggests that the inhibition of Kv channels by amiodarone is state-dependent (Fig. 4). In addition, compared with Kv current elicited by the first depolarizing pulse, subsequent depolarizing pulses produced further inhibition at a holding potential of −100 mV. This holding voltage should prevent any spontaneous channel activation and inactivation. This result also supports a state-dependent mechanism of action of amiodarone on Kv channels (Fig. 5). Finally, amiodarone shifted the steady-state inactivation curve to a more negative potential, which indicates that amiodarone could inhibit Kv channels in a state-dependent manner (Fig. 3).
Amiodarone has been widely used since the 1980s for the clinical treatment of arrhythmias. It is categorized as a class III anti-arrhythmic agent, which has been proven to prolong the cardiac action potential and thereby the refractory period, by blocking I Kr (Kiehn et al. 1999). Therefore, many studies have focused on investigating the effects of amiodarone on cardiac K+ channels. For example, amiodarone inhibited hERG potassium channels in Xenopus oocytes (Kauthale et al. 2015; Kiehn et al. 1999) and cardiac ATP-sensitive potassium channels in rat ventricular myocytes (Holmes et al. 2000). In addition, hKv 1.5 and apamin-sensitive potassium channels, stably expressed in human embryonic kidney 293 (HEK-293) cells, have been reported to be inhibited by amiodarone (Kobayashi et al. 2001; Turker et al. 2013). However, these studies have been restricted to the cardiac K+ channels and cultured cell lines; limited studies exist investigating the effects of amiodarone on Kv channels of native arterial smooth muscle cells.
Kv channels are one of the major channels to determine resting membrane potential in vascular smooth muscles and mediating the physiological changes of agonist-induced vascular tone (Nelson and Quayle 1995). Therefore, an alteration in Kv channel expression and/or function is closely related to cardiovascular and metabolic diseases such as hypertension, hypertrophy, hypoxia, and diabetes (Archer et al. 2001; Cox et al. 2001; Liu et al. 2001). For this reason, the unexpected effects of various drugs on Kv channels should be elucidated to avoid misinterpretation of experimental results. Several drugs are reported to inhibit Kv channels regardless of their primary function. For example, the Ca2+ channel inhibitors efonidipine, verapamil, NNC 55–0396, and mibefradil directly inhibit vascular Kv channels (Hong et al. 2012; Ko et al. 2010; Park et al. 2013; Son et al. 2014). Several kinase inhibitors, such as bisindolylmaleimide (I) (a protein kinase C inhibitor), LY 294002 (a PI3 kinase inhibitor), genistein (a tyrosine kinase inhibitor), staurosporine (a protein kinase C inhibitor), H-89 (a protein kinase A inhibitor), and YC-1 (a guanylyl cyclase inhibitor) also directly inhibit vascular Kv channels independent of their primary functions (Hong et al. 2013; Ko et al. 2009; Park et al. 2010a, 2010b; Park et al. 2005a; Park et al. 2005b; Son et al. 2006). Recently, our group reported that the calmodulin inhibitors, trifluoperazine, W-7, and CGS 9343B, inhibited Kv current independent of calmodulin inhibition (Hong et al. 2014; Li et al. 2015a; Li et al. 2015b). Considering the physiological relevance of vascular Kv channels and the clinical efficacy of amiodarone, the effect of amiodarone on vascular Kv channels should be clearly considered for safety purposes.
Over recent decades, numerous studies have successfully addressed the physiological and pharmacological properties of vascular Kv channels; however, the molecular identities of these channels remain controversial. Furthermore, most studies investigating the molecular subtype of native Kv channels were performed in rats and mice, not rabbits. For this reason, it is difficult to determine exactly which Kv subtypes are expressed in rabbit coronary arterial smooth muscle and which Kv subtypes interact with amiodarone. However, based on previous studies, the Kv1.1, Kv1.2, Kv1.4, Kv1.5, Kv2.1, and Kv9.3 subtypes are expressed in vascular smooth muscle (Standen and Quayle 1998; Xu et al. 1999; Yuan et al. 1998). In the present study, we could not establish which Kv subtype mainly interacted with amiodarone. However, the data described in Fig. 7 suggests that amiodarone predominantly inhibits the Kv1.5 subtype. Furthermore, considering that Kv1.5 is the main subtype expressed in most arterial smooth muscle and amiodarone inhibits hKv1.5 in HEK-293 cells (Kobayashi et al. 2001), one of the main targets of amiodarone should be the Kv 1.5 subtype.
Although, amiodarone effectively controls the cardiac arrhythmias in patients with myocardial disease, it also acts as a powerful vasodilator in vessels (Grossman et al. 1998). In fact, amiodarone stimulated endothelial cells by increasing endothelial Ca2+ concentration, which resulted in the release of nitric oxide and prostaglandins causing vasodilation (Förstermann et al. 1991; Grossman et al. 1998; Heijman and Dobrev 2013). Application of amiodarone is therefore beneficial in both the heart and the vessel. However, in this study, we demonstrated that amiodarone inhibited the Kv channel in vascular smooth muscle. Considering that the inhibition of K+ channel in vascular smooth muscle could induce the vasoconstriction, the inhibitory effect of amiodarone on Kv channel is possibly harmful in aspect of smooth muscle. Although amiodarone has a beneficial effect on heart and vessel, our results should also be taken into consideration in functional studies of vascular smooth muscle by amiodarone.
Conclusions
Overall, to our knowledge, we are the first to demonstrate that amiodarone inhibits the vascular Kv channels in a dose- and state-dependent manner, independent of I Kr inhibition. Therefore, our results should be considered when using amiodarone in studies of vascular function.
References
Archer SL, London B, Hampl V, et al. (2001) Impairment of hypoxic pulmonary vasoconstriction in mice lacking the voltage-gated potassium channel Kv1.5. FASEB J 15:1801–1803
Carlsson B, Singh BN, Temciuc M, et al. (2002) Synthesis and preliminary characterization of a novel antiarrhythmic compound (KB130015) with an improved toxicity profile compared with amiodarone. J Med Chem 45:623–630
Clapp LH, Gurney AM (1992) ATP-sensitive K+ channels regulate resting potential of pulmonary arterial smooth muscle cells. Am J Phys 262:916–920
Cox RH, Folander K, Swanson R (2001) Differential expression of voltage-gated K+ channel genes in arteries from spontaneously hypertensive and Wistar-Kyoto rats. Hypertension 37:1315–1322
Förstermann U, Pollock JS, Schmidt HH, et al. (1991) Calmodulin-dependent endothelium-derived relaxing factor/nitric oxide synthase activity is present in the particulate and cytosolic fractions of bovine aortic endothelial cells. Proc Natl Acad Sci U S A 88:1788–1792
Gessner G, Heller R, Hoshi T, et al. (2007) The amiodarone derivative 2-methyl-3-(3,5-diiodo-4-carboxymethoxybenzyl) benzofuran (KB130015) opens large- conductance Ca2+-activated K+ channels and relaxes vascular smooth muscle. Eur J Pharmacol 555:185–193
Grossman M, Dobrev D, Kirch W (1998) Amiodarone causes endothelium-dependent vasodilation in human hand vein in vivo. Clin Pharmacol Ther 64:302–311
Hara Y, Kitamura K, Kuriyama H (1980) Actions of 4-aminopyridine on vascular smooth muscle tissues of the guinea-pig. Br J Pharmacol 68:99–106
Heijman J, Dobrev D (2013) Pleiotropic actions of amiodarone: still puzzling after half a century. Naunyn Schmiedeberg’s Arch Pharmacol 386:571–574
Holmes DS, Sun ZQ, Porter LM, et al. (2000) Amiodarone inhibits cardiac ATP-sensitive potassium channels. J Cardiovasc Electrophysiol 11:1152–1158
Hondeghem LM, Snyders DJ (1990) Class III antiarrhythmic agents have a lot of potential but a long way to go. Reduced effectiveness and dangers of reverse use dependence. Circulation 81:686–690
Hong DH, Yang D, Choi IW, et al. (2012) The T-type Ca2+ channel inhibitor mibefradil inhibits voltage-dependent K+ channels in rabbit coronary arterial smooth muscle cells. J Pharmacol Sci 120:196–205
Hong DH, Choi IW, Son YK, et al. (2013) The effect of P13 kinase inhibitor LY294002 on voltage-dependent K+ channels in rabbit coronary arterial smooth muscle cells. Life Sci 92:916–922
Hong DH, Son YK, Li H, et al. (2014) The calmodulin inhibitor and antipsychotic drug trifluoperazine inhibits voltage-dependent K+ channels in rabbit coronary arterial smooth muscle cells. Biochem Biophys Res Commun 443:321–425
Kauthale RR, Dadarkar SS, Husain R, et al. (2015) Assessment of temperature-induced hERG channel blockade variation by drugs. J Appl Toxicol 35:799–805
Kiehn J, Thomas D, Karle CA, et al. (1999) Inhibitory effects of the class III antiarrhythmic drug amiodarone on cloned HERG potassium channels. Naunyn Schmiedeber’s Arch Pharmacol 359:212–219
Ko EA, Han J, Jung ID, et al. (2008) Physiological roles of K+ channels in vascular smooth muscle cells. J Smooth Muscle Res 44:65–81
Ko EA, Park WS, Son YK, et al. (2009) The effect of tyrosine kinase inhibitor genistein on voltage-dependent K+ channels in rabbit coronary arterial smooth muscle cells. Vasc Pharmacol 50:51–56
Ko EA, Park WS, Son YK, et al. (2010) Calcium channel inhibitor, verapamil, inhibits the voltage-dependent K+ channels in rabbit coronary smooth muscle cells. Biol Pharm Bull 33:47–52
Kobayashi S, Reien Y, Ogura T, et al. (2001) Inhibitory effect of bepridil on hKv1.5 channel current: comparison with amiodarone and E-4031. Eur J Pharmacol 430:149–157
Kodama I, Kamiya K, Toyama J (1999) Amiodarone: ionic and cellular mechanisms of action of the most promising class III agent. Am J Cardiol 84:20–28
Li H, Choi IW, Hong DH, et al. (2015a) W-7 inhibits voltage-dependent K+ channels independent of calmodulin activity in rabbit coronary arterial smooth muscle cells. Eur J Pharmacol 750:14–19
Li H, Hong DH, Kim HS, et al. (2015b) The calmodulin inhibitor CGS 9343B inhibits voltage-dependent K+ channels in rabbit coronary arterial smooth muscle cells. Toxicol Appl Pharmacol 285:207–213
Liu Y, Terata K, Rusch NJ, et al. (2001) High glucose impairs voltage-gated K+ channel current in rat small coronary arteries. Circ Res 89:146–152
Nelson MT, Quayle JM (1995) Physiological roles and properties of potassium channels in arterial smooth muscle. Am J Phys 268:799–822
Nishida A, Takizawa T, Matsumoto A, et al. (2011) Inhibition of ATP-sensitive K+ channels and L-type Ca2+ channels by amiodarone elicits contradictory effect on insulin secretion in MIN6 cells. J Pharmacol Sci 116:73–80
Okabe K, Kitamura K, Kuriyama H (1987) Features of 4-aminopyridine sensitive outward current observed in single smooth muscle cells from the rabbit pulmonary artery. Pflügers Arch 409:561–568
Park WS, Son YK, Han J, et al. (2005a) Stauroporine inhibits voltage-dependent K+ current through a PKC-independent mechanism in isolated coronary arterial smooth muscle cells. J Cardiovasc Pharmacol 45:260–269
Park WS, Son YK, Ko EA, et al. (2005b) The protein kinase C inhibitor, bisindolylmaleimide (I), inhibits voltage-dependent K+ channels in coronary arterial smooth muscle cells. Life Sci 77:512–527
Park WS, Son YK, Ko EA, et al. (2010a) A carbohydrate fraction, AIP1, from Artemisia iwayomogi reduces the action potential duration by activation of rapidly activating delayed rectifier K channels in rabbit ventricular myocytes. Korean J Physiol Pharmacol 14:119–125
Park WS, Ko JH, Ko EA, et al. (2010b) The guanylyl cyclase activator YC-1 directly inhibits the voltage-dependent K+ channels in rabbit coronary arterial smooth muscle cells. J Pharmacol Sci 112:64–72
Park MH, Son YK, Hong DH, et al. (2013) The Ca2+ channel inhibitor efonidipine decreases voltage-dependent K+ channel activity in rabbit coronary arterial smooth muscle cells. Vasc Pharmacol 59:90–95
Quayle JM, McCarron JG, Brayden JE, et al. (1993) Inward rectifier K+ currents in smooth muscle cells from rat resistance-sized cerebral arteries. Am J Phys 265:1363–1370
Snyders DJ, Yeola SW (1995) Determinants of antiarrhythmic drug action. Electrostatic and hydrophobic components of block of the human cardiac hKv 1.5 channel. Circ Res 77:575–583
Son YK, Park WS, Kim SJ, et al. (2006) Direct inhibition of a PKA inhibitor, H-89 on Kv channels in rabbit coronary arterial smooth muscle cells. Biochem Biophys Res Commun 341:931–937
Son YK, Hong DH, Li H, et al. (2014) The Ca2+ channel inhibitor NNC 55-0396 inhibits voltage-dependent K+ channels in rabbit coronary arterial smooth muscle cells. J Pharmacol Sci 19:312–319
Standen NB, Quayle JM (1998) K+ channel modulation in arterial smooth muscle. Acta Physiol Scand 164:549–557
Turker I, Yu CC, Chang PC, et al. (2013) Amiodarone inhibits apamin-sensitive potassium currents. PLoS One 8:e70450
Xu C, Lu Y, Tang G, et al. (1999) Expression of voltage-dependent K+ channel genes in mesenteric artery smooth muscle cells. Am J Phys 277:1055–1063
Yuan XJ (1995) Voltage-gated K+ currents regulate resting membrane potential and [Ca2+]i in pulmonary arterial myocytes. Circ Res 77:370–378
Yuan XJ, Wang J, Juhaszova M, et al. (1998) Molecular basis and function of voltage-gated K+ channels in pulmonary arterial smooth muscle cells. Am J Phys 274:621–635
Acknowledgments
This work was supported by the National Research Foundation (NRF) of Korea grant funded by the Korean government (Ministry of Education: 2014-R1A1A4A01003840) (Ministry of Science, ICT and Future Planning: 2012-M3A9C7050184, 2015-R1A4A1038666).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethical approval
All experimental procedures performed in studies involving animals were approved by the Committee for Animal Experiments of Kangwon National University.
Rights and permissions
About this article
Cite this article
Li, H., Kim, H.S., Kim, H.W. et al. The class III anti-arrhythmic agent, amiodarone, inhibits voltage-dependent K+ channels in rabbit coronary arterial smooth muscle cells. Naunyn-Schmiedeberg's Arch Pharmacol 389, 713–721 (2016). https://doi.org/10.1007/s00210-016-1232-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-016-1232-8