Abstract
Fungal infections are incurring high risks in a range from superficial mucosal discomforts (such as oropharyngeal candidiasis and vulvovaginal candidiasis) to disseminated life-threatening diseases (such as invasive pulmonary aspergillosis and cryptococcal meningitis) and becoming a global health problem in especially immunodeficient population. The major obstacle to conquer fungal harassment lies in the presence of increasing resistance to conventional antifungal agents used in newly clinically isolated strains. Although recombinant cytokines and mono-/poly-clonal antibodies are added into antifungal armamentarium, more effective antimycotic drugs are exceedingly demanded. It is comforting that the development of fungal vaccines and adjuvants opens up a window to brighten the prospective way in the diagnosis, prevention and treatment of fungal assaults. In this review, we focus on the progression of several major fungal vaccines devised for the control of Candida spp., Aspergillus spp., Cryptococcus spp., Coccidioides spp., Paracoccidioides spp., Blastomyces spp., Histoplasma spp., Pneumocystis spp. as well as the adjuvants adopted. We then expound the interaction between fungal vaccines/adjuvants and host innate (macrophages, dendritic cells, neutrophils), humoral (IgG, IgM and IgA) and cellular (Th1, Th2, Th17 and Tc17) immune responses which generally experience immune recognition of pattern recognition receptors, activation of immune cells, and clearance of invaded fungi. Furthermore, we anticipate an in-depth understanding of immunomodulatory properties of univalent and multivalent vaccines against diverse opportunistic fungi, providing helpful information in the design of novel fungal vaccines and adjuvants.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Fungal infections and antifungal therapy
Fungi are the third largest eukaryotic species next to animals and plants and have a globally profound impact on human health. Owning to rising immune dysfunctions caused by such as long-term antibiotic medication, frequent use of immunosuppressants, chemo-/radio-therapy in cancer population and emergence of multidrug resistant fungal strains, the risks induced by fungal infections are tremendously attracting scientific and clinical attentions in recent decades (Fisher et al. 2020). The latest data show that the annual superficial fungal infections involving, for example, skin, hair, nails and eyes, affect about 1 billion people worldwide, the yearly oral and vaginal mucosal fungal infections influence approximate 135 million people around the world, and allergic fungal infections endanger nearly 23.3 million population (Bongomin et al. 2017). At present, the most common opportunistic fungi are Candida (~ 23%) followed by Aspergillus (~ 8.3%) and Cryptococcus (~ 7.7%) which are heavily detrimental to human being in the case of internal colonization, propagation and systemic invasive infections (Bongomin et al. 2017; Suleyman and Alangaden 2021).
At present, the major antifungal drugs consist of polyenes (such as amphotericin B and nystatin), triazoles and imidazole derivatives (such as fluconazole, itraconazole, posaconazole, voriconazole and esaconazole), and semi-synthetic echinocandins (such as caspofungin, anidulafungin and micafungin) (Dubey and Singla 2019). However, it is known that these traditional antifungal agents are naturally futile to inhibit several fungi. For example, C. krusei and some C. glabrata have intrinsic resistance to fluconazole (Hassan et al. 2021). As a result, increasing incidence of antifungal resistance is becoming an obstacle to restrict clinical application of antifungals available due to up-regulation of efflux pumps, metabolic plasticity, impediment of cell wall and extracellular matrix, overexpressed target-encoding genes, presence of persister cells, and biofilm formation (Martinez and Casadevall 2006; Mowat et al. 2008; Johnson et al. 2016; Wu et al. 2017). The side effects caused by traditional antifungal drugs including nephrotoxicity by amphotericin B and hepatotoxicity by azoles are also unhelpful for their clinical application for some patients with severely damaged immunity. Meanwhile, the economic expense is another heavy burden for patients with long-term use of antifungal agents. Besides antifungal agents, there are several biological preparations including recombinant cytokines (e.g. recombinant human IFNα-2b and GM-CSF) and mono-/poly-clonal antibodies (anti-IL-17) that are effective for antifungal purpose in the treatment of, for example, vulvovaginal candidiasis, refractory oropharyngeal candidiasis and candidiasis (Vazquez et al. 1998; Li et al. 2019; Yamanaka-Takaichi et al. 2022). There are also growing evidence to support the connection of fungal dysbiosis with the aggravation of inflammatory bowel diseases, systemic lupus erythematosus, Alzheimer’s disease, colorectal cancer, and psoriasis with obscure mechanisms (Ling et al. 2020; Bruno et al. 2022; Li et al. 2022; Zhang et al. 2022; Yang et al. 2023). In the face of increased fungal or fungus-related infections, existing antifungal approaches are still limited and new antifungal approaches are desperately required. Due to specialized target recognition and relatively low toxicity, vaccines aim to protect host from invaded fungi by stimulating antibody-mediated humoral immune response and acquire growing interest.
Fungal vaccines and adjuvants
Fungal vaccines are considered an effective way to prevent acute and recurrent invasive infections caused by aggressive fungi, and usually composed of either killed/weakened fungal cells or purified fungal components. During the past decades, the development of fungal vaccines is being emphasized due to increasing challenges posed by, for example, Candida spp., Aspergillus spp., Cryptococcus spp., and Coccidioides spp.. To gain strong immune response, adjuvants are concomitantly administered with vaccines.
Fungal vaccines
Candida spp. are a group of well-studied dimorphic opportunistic fungi that can cause from superficial skin/mucosal disturbs to systemic invasive/deep-seated infections with high morbidity and mortality. The cell wall components (e.g. glucans and adhesins) and live/attenuated strains can be proper candidates in the design of Candida vaccines, some of which have been tested in pre-clinical trials (Table 1). Aspergillus spp. can cause systemic invasive aspergillosis through spores and usually involves bronchus, lung, gastrointestinal tract, eye, nose, mucosa, and skin. Aspergillus spp. were previously known to affect only severely immunocompromised patients, making vaccination difficult. However, extra studies have shown that immunocompetent subjects can also be affected by Aspergillus, some of them can gain positive effects after vaccination (Table 1). Cryptococcosis is a type of disseminated infectious diseases caused by Cryptococcus spp. which frequently induces pneumonia and meningitis, and occasionally involves skin, bone and visceral organ. Patients with cryptococcosis are usually asymptomatic when initially infected with this genus, but the immune-deficient or suppressed patients may suffer from burrowing abscess and granuloma after Cryptococcus spp. change from a latent state to an active state (Brunet et al. 2018). Similarly, Cryptococcus vaccines also need to work in patients with severe T-cell deficiency, e.g. HIV/AIDS patients (Caballero Van Dyke and Wormley 2018). A number of Cryptococcus vaccines have been designed, and their mechanisms of action are elucidated in Table 1. Besides, there are also several reported vaccines against other endemic fungi including Coccidioides spp., Paraccidioides spp., Blastomyces spp., Histoplasma spp., Pneumocystis spp. which are also reviewed in Table 1.
Adjuvants for fungal vaccines
Adjuvants are non-specific immune enhancers that can prime the immune response to an antigen or alter the type of immune response when injected with or pre-injected with a vaccine. Adjuvants can enlarge or lengthen the response and improve the memory response, thus reducing vaccine dosage required (Di Pasquale et al. 2015).
Conventional adjuvants
Conventional adjuvants consists of Freund's adjuvant and toxin adjuvant. The former consists of complete and incomplete Freund's adjuvants. The complete Freund's adjuvant can bind to the recombinant N terminal of Als1p and Als3p of C. albicans. The incomplete Freund's adjuvant can bind to the antigen protein Eno1p (Spellberg et al. 2005; Shibasaki et al. 2013). Toxin adjuvants mainly contains cholera toxin (CT), tetanus toxoid (TT) and diphtheria toxin (CRM197). These adjuvants can present β-mannan and some Sap antigen proteins to adaptive cells, effectively promoting antigen-specific immune responses (Wu et al. 2007; Bromuro et al. 2010; Sandini et al. 2011; De Bernardis et al. 2012). MF59 is the commonly used milk adjuvant and composed of squalene, span 85 and tween 80 which are dissolved in citrate buffer. MF59 can induce significantly higher humoral immunity than aluminum salt adjuvant and certain cellular immune responses (Pietrella et al. 2010).
Delivery adjuvants
Delivery adjuvants is primarily comprised of nanoparticle adjuvants and glucan particles. The advantages of nanoparticle adjuvants involve their interactions with antigen-presenting cells (APC) to promote cross-presentation and cross-protection against fungal antigens. Biocompatible materials possess good absorption and low degradation, making nanoparticle adjuvants safer than conventional adjuvants (Ahmed et al. 2018). Nanoparticle adjuvants can deliver traditional antifungal drugs, e.g. amphotericin B, fluconazole, itraconazole, to the designated locus, displaying potent anti-mycotic effects (Grego et al. 2021). Glucan particles, derived from Saccharomyces cerevisiae cell wall, own spherical complex internal cavities to load diverse antifungal drugs. Since Dectin-1 are widely distributed in myeloid cells, most innate cells like macrophages and dendritic cells (DC) can recognize the major fungal cell wall component β-glucan through Dectin-1, thereby activating innate immune response to invaded fungi. As a result, glucan particles can not only deliver antifungal cargos to inflammatory foci, but also trigger intrinsic immune-stimulatory property of innate immunity (Mirza et al. 2017).
Toll-like receptor (TLR) adjuvants
TLR adjuvants for fungal vaccines mainly contain alum and combined adjuvant. Alum can help C. albicans Als and Hyr1 antigens induce antibody response and CD4+T helper cell response (Baquir et al. 2010; Luo et al. 2011; De Bernardis et al. 2012). Alum can also rapidly recruit neutrophils and other immune cells, and enhance adaptive immunity by inducing tissue damages and activating inflammatory DCs (Oleszycka and Lavelle 2014). Combined adjuvants are prepared by formulating the fungal recombinant protein Bl-Eng2 (Blastomyces endoglucanase 2) which contains an immunodominant antigen and Dectin-2 agonist/adjuvant with δ inulin (Advax) containing TLR agonists. Several of these combined adjuvants, i.e. Bl-Eng4 formulated with Advax3 containing TLR2 agonists or Advax8 containing TLR9 agonists, could provide better protection against pulmonary infection with Blastomyces dermatitidis than Freund's adjuvant (Wüthrich et al. 2021).
Chinese herbal polysaccharide adjuvant
Since polysaccharides are potent activators of immune response, a variety of polysaccharides are extracted from Chinese herbal medicines and purified as adjuvants for fungal vaccines. These polysaccharide preparations include Rehmannia glutinosa polysaccharide (RGP), Radix isatidis polysaccharide (RIPS), Ganoderma lucidum polysaccharide (GLP) and Astragalus polysaccharide (APS) and their derivatives (Hagan et al. 2015). It was found that RGP liposome controlled release preparation was effective to improve the immune response and increase the number of central memory cells and efficient memory cells through enhancing the phagocytosis activity of macrophages and the production of IL-6, IL-12, IL-1β and TNF-α (Wang et al. 2018). Similarly, nano self-assembled lipid RGP adjuvant could also significantly promote macrophage proliferation, pro-inflammatory cytokine production, and cellular uptake through macroendocytosis-dependent and radioimmunotherapy-mediated endocytosis (Huang et al. 2019). RIPS has been demonstrated to enhance spleen cell antigen-specific cellular immune responses, T cell activation, and cytokine production (Wang et al. 2021). GLP-2, a novel β-glucan extracted from Ganoderma lucidum, is a potent TLR4 agonist for adaptive immune response. Studies have shown that GLP-carrying liposome drug delivery system could significantly improve the activity of GLP in promoting splenocyte proliferation and peritoneal macrophage activation (Liu et al. 2015). In another study, GLP and ovalbumin (OVA) were encapsulated into liposome as a vaccine and inoculated into mice. The results showed that GLP-OVA-loaded liposomes (GLPL/OVA) could induce more powerful antigen-specific immune responses, higher antigen-specific IgG antibodies, better splenocyte proliferation, stronger cytokine secretion by splenocytes and activation of CD3+CD4+ and CD3+CD8+ T cells than each single-component formulation (Liu et al. 2016). Polysaccharides extracted from the fruits of Physalis alkekengi L. are used as an adjuvant of a DNA vaccine (pD-HSP90C) which is composed of the recombinant plasmid of epitope C (LKVIRK) from heat shock protein 90 (HSP90) of C. albicans (Yang et al. 2014). The low molecular weight polysaccharides (LMW-ASP) isolated from the root of Astragalus membranaceus (Fisch) Bge. could enhance immune response of a recombinant protein (rP-HSP90C) vaccine containing epitope C (LKVIRK) of Hsp90. Studies have further shown that LMW-ASP promoted the levels of antibodies IgG, IgG1 and IgG2b and cytokines IL-2, IL-4, IL-10 and IL-12 in mice immunized with rP-HSP90C (Yang et al. 2016).
Immune response to fungi
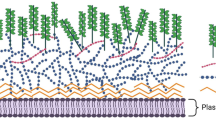
Most opportunistic fungi are symbiotic with and tolerated by host when immunocompetent (Cassone and Cauda 2012). Once the host immune defense is compromised or suppressed, these commensal fungi have great opportunity to transform into aggressive pathogens attacking host organs and tissues (Del Poeta and Casadevall 2012). In-depth understanding of potential mechanisms by which the immune response to fungal infections is performed contributes to the design and application of specific fungal vaccine, and vice versa. Multiple factors including the recognition of immune cells, the site of infected tissues or organs, the morphology of fungi (yeast/mycelial state), the generation of fungal virulence factors, and the structural changes of cell wall affect the initiation, duration and strength of host immune reaction to fungi (Gross et al. 2006; Brunke et al. 2016). Mostly, innate immunity has to work together with adaptive immunity to remove invaded or overgrown fungi (Fig. 1).
Immune defense to Fungi. Fungal cell walls contain several pathogen-associated molecular patterns (PAMPs) that can be recognized by a group of pattern recognition receptors (PRRs). Activation of PRR induces a series of downstream events that contribute to the formation of antigen-specific adaptive immune responses. After identifying the fungal component, TLR (TLR-2, TLR2/6, TLR-4) activates the TIR domain, leading to stimulation of MyD88 or TRIF and downstream complexes (IRAK, TRAF, IKK) followed by translocation of NF-κB, IRF-3, MAPK and other transcription factors. CLRs such as Dectin-1, 2, and Mincle stimulate T cell lineage-specific tyrosine kinases (Syk) and downstream complexes (CARD9-BCL10-MALT1), and initiate the NF-κB signaling. DC-specific intracellular adhesion molecules grab non-integrin (DC-SIGN) receptors modulate NF-κB translocations through RAS and Raf1 activation pathways. These transcription factors drive the expression of various cytokines and regulate T cell differentiations. TLR: Toll like receptor; MyD88: Myeloid differentiation factor 88; IRAK1: Interleukin 1 receptor associated kinase 1; TRAF: Tumor necrosis factor receptor-associated factor; CLR: C-lectin receptor; Mincle: macrophage inducible Ca2 + -dependent lectin receptor; SYK: Spleen tyrosine kinase; CARD9: caspase recruitment domain-containing protein 9; Malt1: mucosa-associated lymphoid tissue lymphoma translocation 1; NF-κB: nuclear factor kappa-light-chain-enhancer of activated B cells; MAPK: mitogen-activated protein kinase; ERK: Extracellular signal-regulated kinase; JNK: c-Jun N-terminal kinase; NLRP3: NLR family pyrin domain containing 3
Candida
The cell wall components of Candida spp., such as β-glucans, α-mannan, N-mannan, O-mannan, β-mannosides, can be recognized by a set of pattern recognition receptors (PRRs) including toll-like receptors (TLRs), C-type lectin receptors (CLRs), RIG I-like receptors (RLRs), NOD-like receptors (NLRs), complement receptors (CRs) and galectins (Zheng et al. 2015). One of the most well-studied CLRs Dectin-1 can recognize β-glucan which is a key constituent of Candida cell wall, followed by activation of multiple innate cells (macrophages, DCs, neutrophils) and clearance of fungi through oxidative stress, apoptosis, phagocytosis, extracellular traps, and antimicrobial peptides (Nikolakopoulou et al. 2020). During this process, Dectin-1 can cooperate with TLR2 and TLR4 to coordinate antifungal immune responses via spleen tyrosine kinase (Syk) dependent (Syk-CARD9/NLRP3) or independent (Raf-1) pathways and myeloid differentiation factor 88 (MyD88) associated NF-κB pathway (Jia et al. 2014; Luisa Gil et al. 2016). As the most powerful antigen presenting cell (APC), DC connects innate immunity with adaptive immunity, and efficiently presents the recognized antigen constituents of Candida to T cells. The stimulated IL-12 drives differentiation of naive T cells into CD4+Th1 subpopulation which further produce IFN-γ to upregulate the expression of IL-12Rβ2. The upregulated IL-12Rβ2 conversely increase IL-12 sensitivity to promote Th1 cell differentiation, facilitating Th1 protective response to Candida infections (Tong and Tang 2017). Th17 cell is another crucial adaptive cells in the protection from Candida infections. The differentiation of Th17 is influenced by cytokines IL-17, IL-21, and IL-22. Individuals with dysfunctional Th17 cells are inclined to increased susceptibility to chronic mucocutaneous candidiasis (Huppler et al. 2012).
Aspergillus
The first line of host immunity against Aspergillus is the airway epithelium of upper respiratory tract containing mucus secreting cells and ciliated cells. The former generate mucus to capture inhaled conidia. The latter drive trapped conidia to the oropharyngeal junction. The airway epithelium of upper respiratory tract can also produce chitinase to destroy the cell wall chitin of A. fumigatus (van de Veerdonk et al. 2017; Garth et al. 2018). Alveolar macrophages (AMs) and neutrophils are the primary phagocytes to clear Aspergillus. AMs can produce pentraxin 3 and surface protein-D which immediately combine with inhaled conidia of A. fumigatus to trigger phagocytosis (Smole et al. 2020). AMs can also recognize and swallow conidia via TLR2/4 and Dectin-1 to elicit inflammatory cytokines and chemokines through NF-κB (Anthoney et al. 2018). Captured conidia by AMs can also recruit neutrophils by TNF-α and CXCL2 to the site of infection, enabling the formation of neutrophils extracellular trap (NET) and the production of lactoferrin which can inactivate conidia and mycelium in germination state (Guo et al. 2020). Immature DCs can also recognize and engulf conidia and mycelia via PRRs and present processed antigens to T cells, ultimately activating adaptive immune response to Aspergillus (Wang et al. 2017a).
Cryptococcus
Cryptococcosis is the most common cause of meningitis in HIV positive patients. The innate immunity to Cryptococcus mainly depends on phagocytic cells including macrophages, DCs and neutrophils (Voigt et al. 2014; Wang et al. 2022b). When Cryptococcus spp. are inhaled into the lung, they encounter diverse phagocytic effector cells and are engulfed through the recognitions of complement receptors (CRs, e.g. CR1, CR3, and CR4) and Fc receptors (Guerra et al. 2014; Sun and Shi 2016). The adaptive immune response to Cryptococcus mainly relies on T and B lymphocytes. CD4+T cells play a dominant role in pulmonary Cryptococcus infections by releasing IL-17 (Guo et al. 2022). CD8+T cells can kill Cryptococcus by granulysin (Ma et al. 2002). γδT cells (mostly CD4−CD8−T) secrete anti-inflammatory Th2 cytokines to balance the exaggerated Th1 response, thereby regulating the Th1-Th2 response to Cryptococcus. However, depletion of γδT cells can boost IFN-γ synthesis and Cryptococcus clearance through Th1-mediated lung response (Uezu et al. 2004). Cryptococcal infections are lethal in mice deficient of B cells compared with those with normal B cells, which can be partly due to B-cell secreted IgM that can bind to Cryptococcus. Depletion of IgM secreted B cells ends up with declined AM phagocytosis and high-risk fungal transmission to brain (Rohatgi and Pirofski 2012). Moreover, B-cell defects are closely tied up with pulmonary immunopathology and inflammation in company with cryptococcal infections (Feldmesser et al. 2002).
Coccidioides
Coccidioidosis is characterized by primary respiratory infections. Occasional dissemination of Coccidioides spores can cause lesions in skin, lung, skeleton, liver, brain and lymph nodes. T-cell-mediated immunity is the most critical part of the immune response to Coccidioides (Cox and Magee 2004). It is reported that neutrophils are more effective in inhibiting arthroconidia than mature spherules, and pretreatment of macrophages with IFN-γ or TNF-α enhances the killing of arthroconidia in vitro (Castro-Lopez and Hung 2017). When the inhaled arthroconidia reach alveoli, they interact with DCs which migrate to local lymph nodes where the antigenic information is presented to and activate Naive T lymphocytes. Activated T cells migrate back to the lung infection loci, differentiate into antigen-specific CD4+Th or CD8+T cells and perform antifungal activity through secreting inflammatory cytokines and triggering granulomatous responses (Castro-Lopez and Hung 2017). It should be noted that Th1 and Th17 can synergistically enhance the recruitment of phagocytic cells to alveoli, ultimately promoting early reduction of Coccidioides load and inhibiting inflammatory pathology at the site of infection (Wüthrich et al. 2011b; Wang et al. 2014). It is believed that MyD88 and Card9 are the two pivotal intracellular immune adaptors for activating the protective Th17 response to Coccidioides infections (Hung et al. 2011, 2016).
Other fungi
There are several other opportunistic fungi that can cause diverse endemic fungal diseases. Paracocccidioidomycosis is a systemic fungal disease caused by the fungi Paracoccidioides brasiliensis and Paracoccidioides lutzii (Santos et al. 2020). Blastomycosis, an endemic fungal infection by Blastomyces, can cause chronic pneumonia as the primary clinical manifestation, and occasionally trigger extrapulmonary infections involving skins and subcutaneous tissues, bones and joints, prostates and central nervous system (Mazi et al. 2021). Histoplasmosis, another common endemic fungal disease induced by Histoplasma, can cause severe acute pulmonary infections in immunocompromised patients (Azar and Hage 2017). Th1 and Th17-mediated immune responses are regarded as major effectors to protect the host from infections caused by these fungal pathogens (Wu et al. 2013b; Ketelut-Carneiro et al. 2019). In non-immunized host, Th17/IL-17 axis confers protection to primary infections through recruiting and activating neutrophils and macrophages to the site of infection in the company of producing a group of chemokines and pro-inflammatory cytokines. During this process, a cluster of well-known PRRs including Dectin-1, Dectin-2, TLR, mannose receptor (MR) and galactin-3 are responsible to recognize the pathogen associated molecular patterns (PAMPs) on the fungal cell wall (Wüthrich et al. 2011a; Ketelut-Carneiro et al. 2019), thereby stimulating a series of downstream events. Other than T cells, multiple effects of neutrophils include phagocytosis, oxidative and non-oxidative cytotoxicity mechanisms that kill intracellular and extracellular pathogens, the production of pro-inflammatory cytokines and chemokines, as well as the elicited neutrophil extracellular traps (NET) are also involved in the combat against these endemic fungal infections (Puerta-Arias et al. 2020).
Fungal vaccine/adjuvant-host interaction
The antigen used for fungal vaccine preparation is usually univalent. Although multivalent fungal vaccines which contain more than one unrelated antigen are of better choice to prevent fungal infections, the immune responses elicited by fungal vaccines are largely different from those by whole fungal cells. In addition, adjuvants can also trigger intense and distinctive immune responses (Fig. 2).
Interactions between fungal vaccines (adjuvants) and host immune system. Fungal vaccines and adjuvants orally and subcutaneously enter into host and encounter at first the innate immune cells including macrophages, dendritic cells (DCs) and neutrophils. Recognizing vaccine epitopes by pattern recognition receptors (PRRs), the innate cells can be widely primed with the help of adjuvants. The antigen processing cells (APCs) like DC gain antigenic information and present to naïve CD4+ and CD8+ T cells. Subsequently, naïve CD4+ T cells are activated and evolve into Th1, Th2 and Th17 cells, whereas CD8+ T cells are stimulated and differentiate into Tc1, Tc2 and Tc17 subtypes. These responsive T cells trigger a variety of inflammatory cytokine release. For example, IL-4 and IL-13 produced by Th1 and Th2 cells facilitate B cells to produce IgM, IgG and IgA subtypes in the serum and mucosa. Th17 cell-produced IL-17A/F and IL-22 recruit and activate neutrophils and macrophages to the site of infection, thereby promoting epithelial homeostasis, tissue repair and fungal eradication. Tc1, Tc2 and Tc17 cells produce IFN-γ TNF-α, IL-4, IL-5, IL-13, IL-17A and IL23 to promote phagocytosis of macrophages, maturation of B cells and antibody release, as well as apoptosis, thereby enhancing fungal clearance
Innate immune response to fungal vaccine and adjuvant
During vaccination, the innate immune cells including macrophages, DCs, neutrophils are extensively activated to elicit multiple downstream events. A recent study showed that chitosan hydrogel (CH-HG) can act as an adjuvant to enhance the protection of a recombinant protein vaccine containing epitope C from C. albicans HSP90 (rP-HSP90C) against systemic candidiasis. The study found that CH-HG was not only effective to cross-present and internalize rP-HSP90C in BMDCs, but also recruit considerable macrophages and DCs in vivo post vaccination for 15 and 5 days (Li et al. 2021). Another study revealed that immunization of a recombinant protein mannosyltransferase 4 (rPmt4p) of C. albicans could generate IgG antibodies to reduce the fungal burden, alleviate kidney inflammation, and prolong the survival rate in a murine model of systemic candidiasis. The protective mechanisms of rPmt4p vaccine could be ascribed to the activation of macrophage opsonization and neutrophil killing of C. albicans (Wang et al. 2022a). It was believed that tyrosine phosphatase SHP-2 renders macrophages and neutrophils contributory to the early control of C. albicans infection via regulating CLR-induced activation of Syk (Deng et al. 2015). The mice vaccinated by a recombinant Pb27 protein (rPb27) from P. brasiliensis with CPG oligodeoxynucleotide motif as an adjuvant were spared from Paracoccidioidomycosis through a mechanism dependent on TLR-9 associated phagocytosis and microbicidal activity of macrophages (Morais et al. 2016). An avirulent vaccine Coccidioides strain NR-166 (∆cts2/∆ard1/∆cts3) could influence the activation and polarization of macrophages and DCs in response to C. posadasii infection (Diep et al. 2021). Similar to immune memory established by adaptive immunity, the heat killed C. neoformans strain H99γ elicited an innate memory-like phenotype in macrophages that was maintained for at least 70 days, providing a pathogen-specific protection against secondary challenge of wild-type C. neoformans strain H99 in the absence of adaptive immune cells after immunization in mice. This study revealed that the secondary challenge triggered a rapid up-regulation of IFN-γ and STAT1 signaling pathways (Leopold Wager et al. 2018). Similarly, a sublingual vaccine V132 prepared from heat-inactivated C. albicans was able to induce innate trained immunity in combination with a polyvalent bacterial vaccine MV140 by promoting metabolic and epigenetic reprogramming in human DCs through activating mitogen-activated protein kinases (MAPK), nuclear factor-κB (NF-κB) and mammalian target of rapamycin (mTOR)-mediated signaling pathways in the prevention of recurrent urinary tract infections (RUTIs) (Martin-Cruz et al. 2020). As a main force in antifungal immunity, different DC subsets are considered to be target candidates in fungal vaccine design (Roy and Klein 2012). Intranasal immunization of a DC-vaccine (Ag2-DC) prepared by transfecting the primary BMDCs with a plasmid DNA encoding a protective epitope of Coccidioides called Antigen-2 or proline rich antigen (Ag2/PRA) contributes to significant retention of DCs and IFN-γ, IL-4 and IL-17 cytokine-secreting T cells in lungs (Awasthi et al. 2019).
Humoral immune response to fungal vaccine and adjuvant
When fungal vaccines in combination with adjuvants come into contact with antigen-reactive B cells, the humoral immune response will commence (Cyster and Allen 2019). Compared with complement system, collectins and antimicrobial peptides, B-mediated antibodies confer principal and indispensable protections to invasive candidiasis (Xin and Cutler 2011). The responses of antibody to diverse pathogenic fungi comprise neutralization of antigen, inhibition of pathogen adherence to host cells, opsonization, antibody-dependent cellular cytotoxicity (ADCC), complement activation, blockage of filament and biofilm formations, and immune regulation (Torosantucci et al. 2005; Shukla et al. 2021). Among the five antibody isotypes, IgG, IgM and IgA are the major protectors upon the stimulation of fungal vaccines. It is known that antibodies are useful in bloodstream infections, but fungal hematogenous dissemination seldom occurs in, for example, AIDS patients unless neutropenia is confronted. A recombinant DNA vaccine containing epitope C (LKVIRK) from HSP90 of C. albicans (pD-HSP90C) enhanced specific antibody titers IgG, IgG1, IgG2b assisted by a polysaccharide adjuvant isolated from the fruits of Physalis alkekengi L., significantly elongating the survival rate in a systemic candidiasis murine model (Yang et al. 2016). A study observed that vaccination with secreted aspartyl proteinase 2 protein (Sap2) from C. parapsilosis increased titers of Sap2-specific IgG and IgM antibodies, inhibited C. tropicalis biofilm formation, and enhanced neutrophil-mediated fungal killing in C. tropicalis-associated systemic candidiasis (Shukla and Rohatgi 2020). Recently, with a multi-kingdom antibody profiling (multiKAP) approach, a mechanism by which gut mycobiota modulates the human B cell expansion and CARD9-dependent induction of host-protective antifungal IgG was expounded (Doron et al. 2021). Although B cell-mediated antibody generation provides potent antifungal protection during vaccination, vaccine-induced antibodies are pivotal drivers to initiate and promote cellular response. For example, post immunization with Pneumocystis, the responses of IgG, IgM and IgA to Pneumocystis protein, β-glucan and chitosan/chitin are heavily dependent on CD4+T cells (Rapaka et al. 2019). Due to a challenging fact that most individuals with high-risk of fungal infections are usually immunocompromised, normal vaccination is unable to elicit effective and lasting humoral immune response. As a result, direct injection/gavage of antibody is becoming a well-recognized passive immunotherapy for antifungal purpose. Monoclonal antibodies (MAbs) C7 (against C. albicans cell wall mannoprotein), A9 (against A. fumigatus cell wall glycoprotein), 18B7 (against cryptococcal capsular polysaccharide) and Mycograb (against Candida Hsp90 protein) were exploited to prevent and treat fungal infections (Chaturvedi et al. 2005; Larsen et al. 2005; Sevilla et al. 2006; Bugli et al. 2013). Recently, an antibody-like Dectin1-Fc(IgG)(s) from distinct subclasses (IgG2a and IgG2b) was devised and demonstrated to have a dose-dependent protections against fungal infections by C. albicans SC5314, H. capsulatum G217B and C. neoformans H99 (Ruiz Mendoza et al. 2022).
Cellular immune response to fungal vaccine and adjuvant
Vaccine/adjuvant-mediated CD4+T responses
Of note, the pathogen-specific CD4+T cells primarily induce Th1, Th2 and Th17 immune responses which become the major cellular defense during vaccination (Becattini et al. 2015). The three T subtypes have disparate cytokine profiles. It is known that IFN-γ and TNF-α are the signature cytokines for Th1, while IL-4, IL-5 and IL13 are characteristic factors for Th2, IL-17A, IL-17F and IL-22 are classical Th17 associated cytokines (Annunziato et al. 2015). It is well-accepted that Th1 cells can help B lymphocytes produce IgG2a isotype in mice and IgM, IgG, and IgA, but not IgE, in human. Both IL-4 and IL-13 can facilitate B cells to produce IgG1 and IgE in mice and the five classes of immunoglobulin in human. IL-17A and IL-17F can target either immune or nonimmune cell types and play a key role in the recruitment, activation, and migration of neutrophils, while IL-22 can promote epithelial cell homeostasis, antimicrobial defense and tissue repair (Annunziato et al. 2015). Multiple types of fungal vaccines are competent to arouse Th1, Th2 and Th17 responses and alter Th1/Th2 and Th1/Th17 ratios in the treatment of systemic candidiasis (Spellberg et al. 2006; Li et al. 2021), invasive cryptococcosis (Masso-Silva et al. 2018), and aspergillosis (Clemons et al. 2014a). It is noteworthy that the cellular immune response to these vaccines is usually characterized by increased Th1 and Th17 responses together with diminished Th2 reaction (Masso-Silva et al. 2018). An immunoproteomic study further indicated that Th2-related antigens represent hopeful candidates for the design of immunotherapy regimens, whereas Th1-related antigens may serve as alterative option for vaccine device (Firacative et al. 2018). The vaccine-motivated Th1/Th2 differentiation might partly attribute to oxidized/reduced mannan derived from fungal cell walls which could activate DCs to stimulate the polarization of Th1 and Th2. It appeared that oxidized mannan could stimulate Th1 responses via phosphorylated p38 dependent IL-12p70 production, while reduced mannan instructed a Th2 bias via phosphorylated ERK dependent IL-10 and IL-4 (Tong et al. 2016). It is well-recognized that Th17 responses provide protection against cutaneous fungal infections, while Th1 responses offer protection against systemic fungal infections (Kashem et al. 2015; Shukla and Rohatgi 2020). The protective features of Th1 and Th17 are corroborated in vaccinations against diverse pathogenic fungi (Specht et al. 2015; Ueno et al. 2019; Li et al. 2021; Wang et al. 2023). Consistently, the fungal vaccines/adjuvants also skew Th1/Th2/Th17 polarization against diverse endemic fungi. For example, a subunit vaccine by encapsulating a recombinant coccidioidal antigen (rCpa1) in Rhodotorula mucilaginosa yeast-derived glucan-chitin particles (GCPs) could stimulate a robust Th17 immunity to confer protection against pulmonary coccidioidomycosis in mice caused by Coccidioides posadasii through a mechanism requiring activation of CARD9-associated Dectin-1 and Dectin-2 signal pathways (Campuzano et al. 2020). The mice vaccine made from Sporothrix schenckii cell wall proteins (ssCWP) and the adjuvant Montanide™ Pet Gel A (PGA) stimulated a preferential Th1/Th2 profile, promoting S. schenckii yeast to be phagocytosed (Portuondo et al. 2017). The combined use of a pan-fungal vaccine calnexin and the conjugates of glycoprotein Blastomyces Eng2 (Bl-Eng2) and Dectin-2 as the adjuvant could augment activation of immune effectors to kill fungi and safeguard mice from lethal fungal challenge by B. dermatitidis (Wang et al. 2017b).
Vaccine/adjuvant-mediated CD8+T responses
CD8+T cells are mostly referred to cytotoxic T or Tc cells which mainly consist of three subtypes, i.e. Tc1, Tc2 and Tc17 (Annunziato et al. 2015). The representative cytokines produced by Tc1 cells are IFN-γ and TNF-α, while those by Tc2 include IL-4, IL-5, IL-13 without IFN-γ (Annunziato et al. 2015). Although CD8+T cells target intracellular pathogens and provide protections in diverse inflammations and autoimmune diseases (allergy and asthma), several fungal vaccines/adjuvants can evoke a skewed CD8+T responses. A previous study showed that co-immunization with rP-HSP90C and CH-HG provoked a stronger CD8+T responses than rP-HSP90C alone in a systemic candidiasis (Li et al. 2021). Although depletion of CD8+T or CD4+T cells did not affect the protection from a C. neoformans mutant (Δsgl1) vaccine, the immune protection was completely lost once both CD8+T and CD4+T cells were exhausted (Normile et al. 2021). It appears that CD4+T cells can help elicit CD8+T-cell responses upon viral and bacterial infections. However, there may have distinct intracellular pathways for the priming of CD4+ and CD8+T responses to A. fumigatus (De Luca et al. 2012). It was assumed that TLR3 was an essential receptor to sense fungal RNA by cross-presenting DCs, promoting antifungal memory CD8+T responses to aspergillosis in high-risk patients (Carvalho et al. 2012). Tc17 cells, a unique subgroup of IL-17-producing CD8+T cells, are found to be an essential player in systemic autoimmune pathology, such as experimental autoimmune encephalomyelitis (EAE), due to its in vivo plasticity (Liang et al. 2015). Several documents demonstrated the protective role of Tc17 cells elicited by HBV DNA vaccination (pcD-S2) and Mycobacterium vaccine therapy (Wu et al. 2013a; Kannan et al. 2020). Recently, a study revealed that vaccine-induced Tc17 cells could persist and confer resistance against B. dermatitidis and H. capsulatum, and are indispensable in vaccine immunity against lethal fungal pneumonia in CD4+T cell-deficient hosts (Nanjappa et al. 2012). In contrast to largely normal IFN-γ+ CD8+T cell (Tc1) responses, sustaining the proliferation of Tc17 cells requires the activation of intrinsic MyD88-Akt1-mTOR signaling during vaccine immunity against fungal pneumonia caused by B. dermatitidis (Nanjappa et al. 2015). Due to high levels of basal homeostatic proliferation and low levels of anti-apoptotic molecules Bcl-2 and Bcl-xL, vaccine-induced antifungal Tc17 cells are durable and stable with long-lasting memory without plasticity towards IFNγ-producing Tc1 cells (Nanjappa et al. 2017). Intriguingly, vaccine-induced GM-CSF+ Tc17 cells, a lineage more like Tc17 cells than IFN-γ-producing Tc1 cells, are instrumental to prevent pulmonary fungal infection caused by B. dermatitidis without inflamed pathology. During the vaccination, IL-23 is dispensable for memory GM-CSF+ Tc17 cell maintenance and recall responses (Mudalagiriyappa et al. 2022). Given that evidence available focuses on the functionality of CD8+T responses to a limited fungal vaccines mainly from Aspergillus and Blastomyces, extra efforts are warranted to decipher the underlying mechanisms of CD8+T responses to other commonly encountered fungal vaccines.
Perspective
Over the past few decades, we have achieved a great progression toward understanding of host immune responses to opportunistic fungi in multiple context of fungal infections, providing useful thoughts for design of novel fungal vaccines and associated adjuvants. Yet, there is no successful fungal vaccines approved for clinically purposes. Considering extremely low immune-competence of at-risk patients with fungal infections, it is a challenging task for fungal vaccines and adjuvants available to induce safe and sufficient immune reactions to eradicate overgrown fungi at no expense of immune system breakdown by such as cytokine release syndrome (CRS). It is important to notice that most antibody vaccines may be useful in mouse intravenous infection models. However, in patients with AIDS there may be a lot of fungi attached to the mucosal surface, but if the patient is not neutropenic, it is difficult for antibody vaccines to encounter the spread fungus via bloodstream. Although a promising approach to combining the vaccine with a cytokine or cytokines known to enhance the immune system can enhance the safety and efficacy of fungal vaccines, a thorough understanding of the interaction between fungi and host immune defense is a prerequisite which still require more efforts in animal and even pre-clinical tests. Nevertheless, it is still worth looking forward to several emerging potential technologies and platforms for designing fungal vaccines and adjuvants. These promising candidates include adoptive T-cell therapy, chimeric antigen receptor (CAR) T-cell therapy, fungal extracellular vesicles-mediated vaccines, as well as mRNA vaccines (Tso et al. 2018; Rivera et al. 2022; Loh and Lam 2023). Of note, consistent with long-lasting protective memory responses by adaptive immune cells, innate immune memory known as “trained immunity” can also be strongly elicited by non-fungal components, such as Bacillus Calmette-Guerin (BCG), offering a possibility to be used for the design of fungal vaccines and adjuvants to generate cross-species protection (Yang et al. 2016). As a result, in-depth exploration of the interaction between fungal vaccines (adjuvants) and host immune system will benefit for understanding the host immune response to opportunistic fungi, which in reverse, accelerates the development of universal and effective fungal vaccines and adjuvants with trans-species protections.
References
Ahmed AA, Hamzah H, Maaroof M (2018) Analyzing formation of silver nanoparticles from the filamentous fungus Fusarium oxysporum and their antimicrobial activity. Turk J Biol 42:54–62
Annunziato F, Romagnani C, Romagnani S (2015) The 3 major types of innate and adaptive cell-mediated effector immunity. J Allergy Clin Immunol 135:626–635
Anthoney N, Foldi I, Hidalgo A (2018) Toll and Toll-like receptor signalling in development. Development 145(9):dev156018
Assis-Marques MA, Oliveira AF, Ruas LP, dos Reis TF, Roque-Barreira MC, Coelho PS (2015) Saccharomyces cerevisiae expressing Gp43 protects mice against Paracoccidioides brasiliensis infection. PLoS ONE 10:e0120201
Awasthi S, Vilekar P, Conkleton A, Rahman N (2019) Dendritic cell-based immunization induces Coccidioides Ag2/PRA-specific immune response. Vaccine 37:1685–1691
Azar MM, Hage CA (2017) Clinical perspectives in the diagnosis and management of histoplasmosis. Clin Chest Med 38:403–415
Baquir B, Lin L, Ibrahim AS, Fu Y, Avanesian V, Tu A, Edwards J Jr, Spellberg B (2010) Immunological reactivity of blood from healthy humans to the rAls3p-N vaccine protein. J Infect Dis 201:473–477
Bastos Ascenço Soares R, Gomez FJ, Almeida Soares CM, Deepe GS (2008) Vaccination with heat shock protein 60 induces a protective immune response against experimental Paracoccidioides brasiliensis pulmonary infection. Infect Immun 76:4214–4221
Becattini S, Latorre D, Mele F, Foglierini M, De Gregorio C, Cassotta A, Fernandez B, Kelderman S, Schumacher TN, Corti D, Lanzavecchia A, Sallusto F (2015) T cell immunity. Functional heterogeneity of human memory CD4+ T cell clones primed by pathogens or vaccines. Science 347:400–406
Beenhouwer DO, May RJ, Valadon P, Scharff MD (2002) High affinity mimotope of the polysaccharide capsule of Cryptococcus neoformans identified from an evolutionary phage peptide library. J Immunol 169:6992–6999
Benito-Villalvilla C, Cirauqui C, Diez-Rivero CM, Casanovas M, Subiza JL, Palomares O (2017) MV140, a sublingual polyvalent bacterial preparation to treat recurrent urinary tract infections, licenses human dendritic cells for generating Th1, Th17, and IL-10 responses via Syk and MyD88. Mucosal Immunol 10:924–935
Bongomin F, Gago S, Oladele RO, Denning DW (2017) Global and multi-national prevalence of fungal diseases estimate precision. J Fungi (Basel) 3(4):57
Bozza S, Gaziano R, Lipford GB, Montagnoli C, Bacci A, Di Francesco P, Kurup VP, Wagner H, Romani L (2002) Vaccination of mice against invasive aspergillosis with recombinant Aspergillus proteins and CpG oligodeoxynucleotides as adjuvants. Microbes Infect 4:1281–1290
Braga CJ, Rittner GM, Muñoz Henao JE, Teixeira AF, Massis LM, Sbrogio-Almeida ME, Taborda CP, Travassos LR, Ferreira LC (2009) Paracoccidioides brasiliensis vaccine formulations based on the gp43-derived P10 sequence and the Salmonella enterica FliC flagellin. Infect Immun 77:1700–1707
Bromuro C, Torosantucci A, Chiani P, Conti S, Polonelli L, Cassone A (2002) Interplay between protective and inhibitory antibodies dictates the outcome of experimentally disseminated Candidiasis in recipients of a Candida albicans vaccine. Infect Immun 70:5462–5470
Bromuro C, Romano M, Chiani P, Berti F, Tontini M, Proietti D, Mori E, Torosantucci A, Costantino P, Rappuoli R, Cassone A (2010) Beta-glucan-CRM197 conjugates as candidates antifungal vaccines. Vaccine 28:2615–2623
Brunet K, Alanio A, Lortholary O, Rammaert B (2018) Reactivation of dormant/latent fungal infection. J Infect 77:463–468
Brunke S, Mogavero S, Kasper L, Hube B (2016) Virulence factors in fungal pathogens of man. Curr Opin Microbiol 32:89–95
Bruno M, Davidson L, Koenen H, van den Reek J, van Cranenbroek B, de Jong E, van de Veerdonk FL, Kullberg BJ, Netea MG (2022) Immunological effects of anti-IL-17/12/23 therapy in patients with psoriasis complicated by Candida infections. J Invest Dermatol 142:2929-2939.e2928
Bugli F, Cacaci M, Martini C, Torelli R, Posteraro B, Sanguinetti M, Paroni Sterbini F (2013) Human monoclonal antibody-based therapy in the treatment of invasive candidiasis. Clin Dev Immunol 2013:403121
Caballero Van Dyke MC, Wormley FL Jr (2018) A call to arms: quest for a cryptococcal vaccine. Trends Microbiol 26:436–446
Campuzano A, Zhang H, Ostroff GR, Dos Santos DL, Wüthrich M, Klein BS, Yu JJ, Lara HH, Lopez-Ribot JL, Hung CY (2020) CARD9-associated dectin-1 and dectin-2 are required for protective immunity of a multivalent vaccine against coccidioides posadasii infection. J Immunol 204:3296–3306
Carvalho A, De Luca A, Bozza S, Cunha C, D’Angelo C, Moretti S, Perruccio K, Iannitti RG, Fallarino F, Pierini A, Latgé JP, Velardi A, Aversa F, Romani L (2012) TLR3 essentially promotes protective class I-restricted memory CD8+ T-cell responses to Aspergillus fumigatus in hematopoietic transplanted patients. Blood 119:967–977
Cassone A, Cauda R (2012) Candida and candidiasis in HIV-infected patients: where commensalism, opportunistic behavior and frank pathogenicity lose their borders. AIDS 26:1457–1472
Cassone A, Bromuro C, Chiani P, Torosantucci A (2010) Hyr1 protein and β-glucan conjugates as anti-Candida vaccines. J Infect Dis 202:1930
Castro-Lopez N, Hung CY (2017) Immune response to coccidioidomycosis and the development of a vaccine. Microorganisms 5(1):13
Cenci E, Mencacci A, Bacci A, Bistoni F, Kurup VP, Romani L (2000) T cell vaccination in mice with invasive pulmonary aspergillosis. J Immunol 165:381–388
Chaturvedi AK, Kavishwar A, Shiva Keshava GB, Shukla PK (2005) Monoclonal immunoglobulin G1 directed against Aspergillus fumigatus cell wall glycoprotein protects against experimental murine aspergillosis. Clin Diagn Lab Immunol 12:1063–1068
Chong KT, Woo PC, Lau SK, Huang Y, Yuen KY (2004) AFMP2 encodes a novel immunogenic protein of the antigenic mannoprotein superfamily in Aspergillus fumigatus. J Clin Microbiol 42:2287–2291
Chow SK, Casadevall A (2011) Evaluation of Cryptococcus neoformans galactoxylomannan-protein conjugate as vaccine candidate against murine cryptococcosis. Vaccine 29:1891–1898
Clemons KV, Danielson ME, Michel KS, Liu M, Ottoson NC, Leonardo SM, Martinez M, Chen V, Antonysamy MA, Stevens DA (2014a) Whole glucan particles as a vaccine against murine aspergillosis. J Med Microbiol 63:1750–1759
Clemons KV, Martinez M, Chen V, Liu M, Yoon HJ, Stevens DA (2014b) Protection against experimental aspergillosis by heat-killed yeast is not antibody dependent. Med Mycol 52:422–426
Cox RA, Magee DM (2004) Coccidioidomycosis: host response and vaccine development. Clin Microbiol Rev 17:804–839
Cyster JG, Allen CDC (2019) B Cell Responses: Cell Interaction Dynamics and Decisions. Cell 177:524–540
Datta K, Lees A, Pirofski LA (2008) Therapeutic efficacy of a conjugate vaccine containing a peptide mimotope of cryptococcal capsular polysaccharide glucuronoxylomannan. Clin Vaccine Immunol 15:1176–1187
De Bernardis F, Boccanera M, Adriani D, Girolamo A, Cassone A (2002) Intravaginal and intranasal immunizations are equally effective in inducing vaginal antibodies and conferring protection against vaginal candidiasis. Infect Immun 70:2725–2729
De Bernardis F, Amacker M, Arancia S, Sandini S, Gremion C, Zurbriggen R, Moser C, Cassone A (2012) A virosomal vaccine against candidal vaginitis: immunogenicity, efficacy and safety profile in animal models. Vaccine 30:4490–4498
De Luca A, Iannitti RG, Bozza S, Beau R, Casagrande A, D’Angelo C, Moretti S, Cunha C, Giovannini G, Massi-Benedetti C, Carvalho A, Boon L, Latgé JP, Romani L (2012) CD4(+) T cell vaccination overcomes defective cross-presentation of fungal antigens in a mouse model of chronic granulomatous disease. J Clin Invest 122:1816–1831
Del Poeta M, Casadevall A (2012) Ten challenges on Cryptococcus and cryptococcosis. Mycopathologia 173:303–310
Delgado N, Xue J, Yu JJ, Hung CY, Cole GT (2003) A recombinant beta-1,3-glucanosyltransferase homolog of Coccidioides posadasii protects mice against coccidioidomycosis. Infect Immun 71:3010–3019
Deng Z, Ma S, Zhou H, Zang A, Fang Y, Li T, Shi H, Liu M, Du M, Taylor PR, Zhu HH, Chen J, Meng G, Li F, Chen C, Zhang Y, Jia XM, Lin X, Zhang X, Pearlman E, Li X, Feng GS, Xiao H (2015) Tyrosine phosphatase SHP-2 mediates C-type lectin receptor-induced activation of the kinase Syk and anti-fungal TH17 responses. Nat Immunol 16:642–652
Di Pasquale A, Preiss S, Tavares Da Silva F, Garçon N (2015) Vaccine Adjuvants: from 1920 to 2015 and Beyond. Vaccines (basel) 3:320–343
Diaz-Arevalo D, Bagramyan K, Hong TB, Ito JI, Kalkum M (2011) CD4+ T cells mediate the protective effect of the recombinant Asp f3-based anti-aspergillosis vaccine. Infect Immun 79:2257–2266
Diep AL, Tejeda-Garibay S, Miranda N, Hoyer KK (2021) Macrophage and dendritic cell activation and polarization in response to coccidioidesposadasii infection. J Fungi (Basel) 7(8):630
Doron I, Leonardi I, Li XV, Fiers WD, Semon A, Bialt-DeCelie M, Migaud M, Gao IH, Lin WY, Kusakabe T, Puel A, Iliev ID (2021) Human gut mycobiota tune immunity via CARD9-dependent induction of anti-fungal IgG antibodies. Cell 184:1017-1031.e1014
Dubey AK, Singla RK (2019) Current trends in anti-candida drug development. Curr Top Med Chem 19:2525–2526
Fan H, Guo JY, Ma SL, Zhang N, An CL (2016) Synthetic p55 tandem DNA vaccine against Pneumocystis carinii in rats. Microbiol Immunol 60(6):397–406
Feldmesser M, Mednick A, Casadevall A (2002) Antibody-mediated protection in murine Cryptococcus neoformans infection is associated with pleotrophic effects on cytokine and leukocyte responses. Infect Immun 70:1571–1580
Fernandes CM, Normile TG, Fabri J, Brauer VS, Sagr DE, Frases S, Nimrichter L, Malavazi I, Del Poeta M (2022) Vaccination with live or heat-killed aspergillus fumigatus ΔsglA conidia fully protects immunocompromised mice from invasive aspergillosis. Mbio 13:e0232822
Fernandes Costa A, Evangelista Araujo D, Santos Cabral M, Teles Brito I, de Menezes B, Leite L, Pereira M, Correa Amaral A (2019) Development, characterization, and in vitro-in vivo evaluation of polymeric nanoparticles containing miconazole and farnesol for treatment of vulvovaginal candidiasis. Med Mycol 57:52–62
Fernández-Arenas E, Molero G, Nombela C, Diez-Orejas R, Gil C (2004) Low virulent strains of Candida albicans: unravelling the antigens for a future vaccine. Proteomics 4:3007–3020
Firacative C, Gressler AE, Schubert K, Schulze B, Müller U, Brombacher F, von Bergen M, Alber G (2018) Identification of T helper (Th)1- and Th2-associated antigens of Cryptococcus neoformans in a murine model of pulmonary infection. Sci Rep 8:2681
Fisher MC, Gurr SJ, Cuomo CA, Blehert DS, Jin H, Stukenbrock EH, Stajich JE, Kahmann R, Boone C, Denning DW, Gow NAR, Klein BS, Kronstad JW, Sheppard DC, Taylor JW, Wright GD, Heitman J, Casadevall A, Cowen LE (2020) Threats posed by the fungal kingdom to humans, wildlife, and agriculture. mBio 11(3):e00449-20
Garth JM, Mackel JJ, Reeder KM, Blackburn JP, Dunaway CW, Yu Z, Matalon S, Fitz L, Steele C (2018) Acidic mammalian chitinase negatively affects immune responses during acute and chronic aspergillus fumigatus exposure. Infect Immun 86(7):e00944-17
Grego EA, Siddoway AC, Uz M, Liu L, Christiansen JC, Ross KA, Kelly SM, Mallapragada SK, Wannemuehler MJ, Narasimhan B (2021) Polymeric nanoparticle-based vaccine adjuvants and delivery vehicles. Curr Top Microbiol Immunol 433:29–76
Gross O, Gewies A, Finger K, Schäfer M, Sparwasser T, Peschel C, Förster I, Ruland J (2006) Card9 controls a non-TLR signalling pathway for innate anti-fungal immunity. Nature 442:651–656
Gu X, Hua YH, Zhang YD, Bao DI, Lv J, Hu HF (2021) The pathogenesis of aspergillus fumigatus, host defense mechanisms, and the development of AFMP4 antigen as a vaccine. Pol J Microbiol 70:3–11
Guerra CR, Seabra SH, de Souza W, Rozental S (2014) Cryptococcus neoformans is internalized by receptor-mediated or “triggered” phagocytosis, dependent on actin recruitment. PLoS ONE 9:e89250
Guo Y, Kasahara S, Jhingran A, Tosini NL, Zhai B, Aufiero MA, Mills KAM, Gjonbalaj M, Espinosa V, Rivera A, Luster AD, Hohl TM (2020) During aspergillus infection, monocyte-derived DCs, neutrophils, and plasmacytoid DCs enhance innate immune defense through CXCR3-dependent crosstalk. Cell Host Microbe 28:104-116.e104
Guo X, Mao X, Tian D, Liao Y, Su B, Ye C, Shi D, Liu TF, Ling Y, Hao Y (2022) Cryptococcus neoformans infection induces IL-17 production by promoting STAT3 phosphorylation in CD4(+) T cells. Front Immunol 13:872286
Hagan T, Nakaya HI, Subramaniam S, Pulendran B (2015) Systems vaccinology: enabling rational vaccine design with systems biological approaches. Vaccine 33:5294–5301
Hassan Y, Chew SY, Than LTL (2021) Candida glabrata: pathogenicity and resistance mechanisms for adaptation and survival. J Fungi (basel) 7(8):667
Huang Y, Nan L, Xiao C, Ji Q, Li K, Wei Q, Liu Y, Bao G (2019) Optimum preparation method for self-assembled PEGylation nano-adjuvant based on rehmannia glutinosa polysaccharide and its immunological effect on macrophages. Int J Nanomedicine 14:9361–9375
Hung CY, Gonzalez A, Wüthrich M, Klein BS, Cole GT (2011) Vaccine immunity to coccidioidomycosis occurs by early activation of three signal pathways of T helper cell response (Th1, Th2, and Th17). Infect Immun 79:4511–4522
Hung CY, Hurtgen BJ, Bellecourt M, Sanderson SD, Morgan EL, Cole GT (2012) An agonist of human complement fragment C5a enhances vaccine immunity against Coccidioides infection. Vaccine 30:4681–4690
Hung CY, Castro-Lopez N, Cole GT (2016) Card9- and MyD88-mediated gamma interferon and nitric oxide production is essential for resistance to subcutaneous coccidioides posadasii infection. Infect Immun 84:1166–1175
Huppler AR, Bishu S, Gaffen SL (2012) Mucocutaneous candidiasis: the IL-17 pathway and implications for targeted immunotherapy. Arthritis Res Ther 14:217
Hurtgen BJ, Hung CY, Ostroff GR, Levitz SM, Cole GT (2012) Construction and evaluation of a novel recombinant T cell epitope-based vaccine against Coccidioidomycosis. Infect Immun 80:3960–3974
Ibrahim AS, Spellberg BJ, Avanesian V, Fu Y, Edwards JE Jr (2006) The anti-Candida vaccine based on the recombinant N-terminal domain of Als1p is broadly active against disseminated candidiasis. Infect Immun 74:3039–3041
Ito JI, Lyons JM (2002) Vaccination of corticosteroid immunosuppressed mice against invasive pulmonary aspergillosis. J Infect Dis 186:869–871
Ito JI, Lyons JM, Hong TB, Tamae D, Liu YK, Wilczynski SP, Kalkum M (2006) Vaccinations with recombinant variants of Aspergillus fumigatus allergen Asp f 3 protect mice against invasive aspergillosis. Infect Immun 74:5075–5084
Ivey FD, Magee DM, Woitaske MD, Johnston SA, Cox RA (2003) Identification of a protective antigen of Coccidioides immitis by expression library immunization. Vaccine 21:4359–4367
Jansook P, Pichayakorn W, Ritthidej GC (2018) Amphotericin B-loaded solid lipid nanoparticles (SLNs) and nanostructured lipid carrier (NLCs): effect of drug loading and biopharmaceutical characterizations. Drug Dev Ind Pharm 44:1693–1700
Jia XM, Tang B, Zhu LL, Liu YH, Zhao XQ, Gorjestani S, Hsu YM, Yang L, Guan JH, Xu GT, Lin X (2014) CARD9 mediates Dectin-1-induced ERK activation by linking Ras-GRF1 to H-Ras for antifungal immunity. J Exp Med 211:2307–2321
Jin Z, Dong YT, Liu S, Liu J, Qiu XR, Zhang Y, Zong H, Hou WT, Guo SY, Sun YF, Chen SM, Dong HQ, Li YY, An MM, Shen H (2022) Potential of polyethyleneimine as an adjuvant to prepare long-term and potent antifungal nanovaccine. Front Immunol 13:843684
Johannesson H, Vidal P, Guarro J, Herr RA, Cole GT, Taylor JW (2004) Positive directional selection in the proline-rich antigen (PRA) gene among the human pathogenic fungi Coccidioides immitis, C. posadasii and their closest relatives. Mol Biol Evol 21:1134–1145
Johnson CJ, Cabezas-Olcoz J, Kernien JF, Wang SX, Beebe DJ, Huttenlocher A, Ansari H, Nett JE (2016) The extracellular matrix of Candida Albicans biofilms impairs formation of neutrophil extracellular traps. PLoS Pathog 12:e1005884
Kannan N, Haug M, Steigedal M, Flo TH (2020) Mycobacterium smegmatis vaccine vector elicits CD4+ Th17 and CD8+ Tc17 T cells with therapeutic potential to infections with mycobacterium avium. Front Immunol 11:1116
Kashem SW, Igyarto BZ, Gerami-Nejad M, Kumamoto Y, Mohammed JA, Jarrett E, Drummond RA, Zurawski SM, Zurawski G, Berman J, Iwasaki A, Brown GD, Kaplan DH (2015) Candida albicans morphology and dendritic cell subsets determine T helper cell differentiation. Immunity 42:356–366
Ketelut-Carneiro N, Souza COS, Benevides L, Gardinassi LG, Silva MC, Tavares LA, Zamboni DS, Silva JS (2019) Caspase-11-dependent IL-1α release boosts Th17 immunity against Paracoccidioides brasiliensis. PLoS Pathog 15:e1007990
Khan S, Alam F, Azam A, Khan AU (2012) Gold nanoparticles enhance methylene blue-induced photodynamic therapy: a novel therapeutic approach to inhibit Candida albicans biofilm. Int J Nanomedicine 7:3245–3257
Kischkel B, Castilho PF, de Oliveira KM, Rezende PS, Bruschi ML, Svidzinski TI, Negri M (2020) Silver nanoparticles stabilized with propolis show reduced toxicity and potential activity against fungal infections. Future Microbiol 15:521–539
Kleinnijenhuis J, Quintin J, Preijers F, Joosten LA, Ifrim DC, Saeed S, Jacobs C, van Loenhout J, de Jong D, Stunnenberg HG, Xavier RJ, van der Meer JW, van Crevel R, Netea MG (2012) Bacille Calmette-Guerin induces NOD2-dependent nonspecific protection from reinfection via epigenetic reprogramming of monocytes. Proc Natl Acad Sci USA 109:17537–17542
Kuttel MM, Casadevall A, Oscarson S (2020) Cryptococcus neoformans capsular GXM conformation and epitope presentation: a molecular modelling study. Molecules 25(11):2651
Lara HH, Romero-Urbina DG, Pierce C, Lopez-Ribot JL, Arellano-Jiménez MJ, Jose-Yacaman M (2015) Effect of silver nanoparticles on Candida albicans biofilms: an ultrastructural study. J Nanobiotechnology 13:91
Larsen RA, Pappas PG, Perfect J, Aberg JA, Casadevall A, Cloud GA, James R, Filler S, Dismukes WE (2005) Phase I evaluation of the safety and pharmacokinetics of murine-derived anticryptococcal antibody 18B7 in subjects with treated cryptococcal meningitis. Antimicrob Agents Chemother 49:952–958
Leopold Wager CM, Hole CR, Campuzano A, Castro-Lopez N, Cai H, Caballero Van Dyke MC, Wozniak KL, Wang Y, Wormley FL Jr (2018) IFN-γ immune priming of macrophages in vivo induces prolonged STAT1 binding and protection against Cryptococcus neoformans. PLoS Pathog 14:e1007358
Li K, Yu JJ, Hung CY, Lehmann PF, Cole GT (2001) Recombinant urease and urease DNA of Coccidioides immitis elicit an immunoprotective response against coccidioidomycosis in mice. Infect Immun 69:2878–2887
Li T, Liu Z, Zhang X, Chen X, Wang S (2019) Therapeutic effectiveness of type I interferon in vulvovaginal candidiasis. Microb Pathog 134:103562
Li X, Yang Y, Yang F, Wang F, Li H, Tian H, Wang G (2021) Chitosan hydrogel loaded with recombinant protein containing epitope C from HSP90 of Candida albicans induces protective immune responses against systemic candidiasis. Int J Biol Macromol 173:327–340
Li XV, Leonardi I, Putzel GG, Semon A, Fiers WD, Kusakabe T, Lin WY, Gao IH, Doron I, Gutierrez-Guerrero A, DeCelie MB, Carriche GM, Mesko M, Yang C, Naglik JR, Hube B, Scherl EJ, Iliev ID (2022) Immune regulation by fungal strain diversity in inflammatory bowel disease. Nature 603:672–678
Liang Y, Pan HF, Ye DQ (2015) Tc17 cells in immunity and systemic autoimmunity. Int Rev Immunol 34:318–331
Liao G, Zhou Z, Burgula S, Liao J, Yuan C, Wu Q, Guo Z (2015) Synthesis and immunological studies of linear oligosaccharides of β-glucan as antigens for antifungal vaccine development. Bioconjug Chem 26:466–476
Lin L, Ibrahim AS, Xu X, Farber JM, Avanesian V, Baquir B, Fu Y, French SW, Edwards JE Jr, Spellberg B (2009) Th1-Th17 cells mediate protective adaptive immunity against Staphylococcus aureus and Candida albicans infection in mice. PLoS Pathog 5:e1000703
Ling Z, Zhu M, Liu X, Shao L, Cheng Y, Yan X, Jiang R, Wu S (2020) Fecal fungal dysbiosis in Chinese patients with Alzheimer’s disease. Front Cell Dev Biol 8:631460
Lipinski T, Fitieh A, St Pierre J, Ostergaard HL, Bundle DR, Touret N (2013) Enhanced immunogenicity of a tricomponent mannan tetanus toxoid conjugate vaccine targeted to dendritic cells via Dectin-1 by incorporating β-glucan. J Immunol 190:4116–4128
Liu Z, Ma X, Deng B, Huang Y, Bo R, Gao Z, Yu Y, Hu Y, Liu J, Wu Y, Wang D (2015) Development of liposomal Ganoderma lucidum polysaccharide: formulation optimization and evaluation of its immunological activity. Carbohydr Polym 117:510–517
Liu Z, Xing J, Zheng S, Bo R, Luo L, Huang Y, Niu Y, Li Z, Wang D, Hu Y, Liu J, Wu Y (2016) Ganoderma lucidum polysaccharides encapsulated in liposome as an adjuvant to promote Th1-bias immune response. Carbohydr Polym 142:141–148
Loh JT, Lam KP (2023) Fungal infections: Immune defense, immunotherapies and vaccines. Adv Drug Deliv Rev 196:114775
Ludwig DB, de Camargo LEA, Khalil NM, Auler ME, Mainardes RM (2018) Antifungal activity of chitosan-coated poly(lactic-co-glycolic) acid nanoparticles containing amphotericin B. Mycopathologia 183:659–668
Luisa Gil M, Murciano C, Yáñez A, Gozalbo D (2016) Role of Toll-like receptors in systemic Candida albicans infections. Front Biosci (landmark Ed) 21:278–302
Luo G, Ibrahim AS, Spellberg B, Nobile CJ, Mitchell AP, Fu Y (2010) Candida albicans Hyr1p confers resistance to neutrophil killing and is a potential vaccine target. J Infect Dis 201:1718–1728
Luo G, Ibrahim AS, French SW, Edwards JE Jr, Fu Y (2011) Active and passive immunization with rHyr1p-N protects mice against hematogenously disseminated candidiasis. PLoS ONE 6:e25909
Ma LL, Spurrell JC, Wang JF, Neely GG, Epelman S, Krensky AM, Mody CH (2002) CD8 T cell-mediated killing of Cryptococcus neoformans requires granulysin and is dependent on CD4 T cells and IL-15. J Immunol 169:5787–5795
Maitta RW, Datta K, Lees A, Belouski SS, Pirofski LA (2004) Immunogenicity and efficacy of Cryptococcus neoformans capsular polysaccharide glucuronoxylomannan peptide mimotope-protein conjugates in human immunoglobulin transgenic mice. Infect Immun 72:196–208
Maliszewska I, Lisiak B, Popko K, Matczyszyn K (2017) Enhancement of the efficacy of photodynamic inactivation of Candida Albicans with the use of biogenic gold nanoparticles. Photochem Photobiol 93:1081–1090
Martin-Cruz L, Sevilla-Ortega C, Benito-Villalvilla C, Diez-Rivero CM, Sanchez-Ramón S, Subiza JL, Palomares O (2020) A combination of polybacterial MV140 and candida albicans V132 as a potential novel trained immunity-based vaccine for genitourinary tract infections. Front Immunol 11:612269
Martín-Cruz L, Angelina A, Baydemir I, Bulut Ö, Subiza JL, Netea MG, Domínguez-Andrés J, Palomares O (2022) Candida albicans V132 induces trained immunity and enhances the responses triggered by the polybacterial vaccine MV140 for genitourinary tract infections. Front Immunol 13:1066383
Martinez LR, Casadevall A (2006) Cryptococcus neoformans cells in biofilms are less susceptible than planktonic cells to antimicrobial molecules produced by the innate immune system. Infect Immun 74:6118–6123
Martínez-López R, Nombela C, Diez-Orejas R, Monteoliva L, Gil C (2008) Immunoproteomic analysis of the protective response obtained from vaccination with Candida albicans ecm33 cell wall mutant in mice. Proteomics 8:2651–2664
Mašek J, Bartheldyová E, Turánek-Knotigová P, Skrabalová M, Korvasová Z, Plocková J, Koudelka S, Skodová P, Kulich P, Křupka M, Zachová K, Czerneková L, Horynová M, Kratochvílová I, Miller AD, Zýka D, Michálek J, Vrbková J, Sebela M, Ledvina M, Raška M, Turánek J (2011) Metallochelating liposomes with associated lipophilised norAbuMDP as biocompatible platform for construction of vaccines with recombinant His-tagged antigens: preparation, structural study and immune response towards rHsp90. J Control Release 151:193–201
Masso-Silva J, Espinosa V, Liu TB, Wang Y, Xue C, Rivera A (2018) The F-Box protein Fbp1 shapes the immunogenic potential of Cryptococcus neoformans. mBio 9(1):e01828-17
Mazi PB, Rauseo AM, Spec A (2021) Blastomycosis. Infect Dis Clin North Am 35:515–530
Mead HL, Roe CC, Higgins Keppler EA, Van Dyke MCC, Laux KL, Funke AL, Miller KJ, Bean HD, Sahl JW, Barker BM (2020) Defining critical genes during spherule remodeling and endospore development in the fungal pathogen. Coccidioides Posadasii Front Genet 11:483
Mirza Z, Soto ER, Dikengil F, Levitz SM, Ostroff GR (2017) Beta-glucan particles as vaccine adjuvant carriers. Methods Mol Biol 1625:143–157
Moazeni M, Kelidari HR, Saeedi M, Morteza-Semnani K, Nabili M, Gohar AA, Akbari J, Lotfali E, Nokhodchi A (2016) Time to overcome fluconazole resistant Candida isolates: solid lipid nanoparticles as a novel antifungal drug delivery system. Colloids Surf B Biointerfaces 142:400–407
Monteiro DR, Gorup LF, Silva S, Negri M, de Camargo ER, Oliveira R, Barbosa DB, Henriques M (2011) Silver colloidal nanoparticles: antifungal effect against adhered cells and biofilms of Candida albicans and Candida glabrata. Biofouling 27:711–719
Morais EA, Chame DF, Melo EM, de Carvalho Oliveira JA, de Paula AC, Peixoto AC, da Silva SL, Gomes DA, Russo RC, de Goes AM (2016) TLR 9 involvement in early protection induced by immunization with rPb27 against Paracoccidioidomycosis. Microbes Infect 18:137–147
Mowat E, Lang S, Williams C, McCulloch E, Jones B, Ramage G (2008) Phase-dependent antifungal activity against Aspergillus fumigatus developing multicellular filamentous biofilms. J Antimicrob Chemother 62:1281–1284
Mudalagiriyappa S, Sharma J, Vieson MD, Nanjappa SG (2022) GM-CSF(+) Tc17 cells are required to bolster vaccine immunity against lethal fungal pneumonia without causing overt pathology. Cell Rep 41:111543
Nanjappa SG, Heninger E, Wüthrich M, Gasper DJ, Klein BS (2012) Tc17 cells mediate vaccine immunity against lethal fungal pneumonia in immune deficient hosts lacking CD4+ T cells. PLoS Pathog 8:e1002771
Nanjappa SG, Hernández-Santos N, Galles K, Wüthrich M, Suresh M, Klein BS (2015) Intrinsic MyD88-Akt1-mTOR signaling coordinates disparate Tc17 and Tc1 responses during vaccine immunity against fungal pneumonia. PLoS Pathog 11:e1005161
Nanjappa SG, McDermott AJ, Fites JS, Galles K, Wüthrich M, Deepe GS Jr, Klein BS (2017) Antifungal Tc17 cells are durable and stable, persisting as long-lasting vaccine memory without plasticity towards IFNγ cells. PLoS Pathog 13:e1006356
Narra HP, Shubitz LF, Mandel MA, Trinh HT, Griffin K, Buntzman AS, Frelinger JA, Galgiani JN, Orbach MJ (2016) A Coccidioides posadasii CPS1 deletion mutant is avirulent and protects mice from lethal infection. Infect Immun 84:3007–3016
Niemirowicz K, Durnaś B, Tokajuk G, Głuszek K, Wilczewska AZ, Misztalewska I, Mystkowska J, Michalak G, Sodo A, Wątek M, Kiziewicz B, Góźdź S, Głuszek S, Bucki R (2016) Magnetic nanoparticles as a drug delivery system that enhance fungicidal activity of polyene antibiotics. Nanomedicine 12:2395–2404
Niemirowicz K, Durnaś B, Tokajuk G, Piktel E, Michalak G, Gu X, Kułakowska A, Savage PB, Bucki R (2017) Formulation and candidacidal activity of magnetic nanoparticles coated with cathelicidin LL-37 and ceragenin CSA-13. Sci Rep 7:4610
Nikolakopoulou C, Willment JA, Brown GD (2020) C-type lectin receptors in antifungal immunity. Adv Exp Med Biol 1204:1–30
Normile TG, Rella A, Del Poeta M (2021) Cryptococcus neoformans Δsgl1 vaccination requires either CD4(+) or CD8(+) T cells for complete host protection. Front Cell Infect Microbiol 11:739027
Oleszycka E, Lavelle EC (2014) Immunomodulatory properties of the vaccine adjuvant alum. Curr Opin Immunol 28:1–5
Orsborn KI, Shubitz LF, Peng T, Kellner EM, Orbach MJ, Haynes PA, Galgiani JN (2006) Protein expression profiling of Coccidioides posadasii by two-dimensional differential in-gel electrophoresis and evaluation of a newly recognized peroxisomal matrix protein as a recombinant vaccine candidate. Infect Immun 74(3):1865–1872
Oscarson S, Alpe M, Svahnberg P, Nakouzi A, Casadevall A (2005) Synthesis and immunological studies of glycoconjugates of Cryptococcus neoformans capsular glucuronoxylomannan oligosaccharide structures. Vaccine 23:3961–3972
Pappagianis D (1993) Evaluation of the protective efficacy of the killed Coccidioides immitis spherule vaccine in humans. the valley fever vaccine study group. Am Rev Respir Dis 148:656–660
Paulovičová L, Paulovičová E, Karelin AA, Tsvetkov YE, Nifantiev NE, Bystrický S (2012) Humoral and cell-mediated immunity following vaccination with synthetic Candida cell wall mannan derived heptamannoside-protein conjugate: immunomodulatory properties of heptamannoside-BSA conjugate. Int Immunopharmacol 14:179–187
Pietrella D, Rachini A, Torosantucci A, Chiani P, Brown AJ, Bistoni F, Costantino P, Mosci P, d’Enfert C, Rappuoli R, Cassone A, Vecchiarelli A (2010) A beta-glucan-conjugate vaccine and anti-beta-glucan antibodies are effective against murine vaginal candidiasis as assessed by a novel in vivo imaging technique. Vaccine 28:1717–1725
Portuondo DL, Batista-Duharte A, Ferreira LS, de Andrade CR, Quinello C, Téllez-Martínez D, de Aguiar Loesch ML, Carlos IZ (2017) Comparative efficacy and toxicity of two vaccine candidates against Sporothrix schenckii using either Montanide™ Pet Gel A or aluminum hydroxide adjuvants in mice. Vaccine 35:4430–4436
Puerta-Arias JD, Mejía SP, González Á (2020) The role of the interleukin-17 axis and neutrophils in the pathogenesis of endemic and systemic mycoses. Front Cell Infect Microbiol 10:595301
Rachini A, Pietrella D, Lupo P, Torosantucci A, Chiani P, Bromuro C, Proietti C, Bistoni F, Cassone A, Vecchiarelli A (2007) An anti-beta-glucan monoclonal antibody inhibits growth and capsule formation of Cryptococcus neoformans in vitro and exerts therapeutic, anticryptococcal activity in vivo. Infect Immun 75:5085–5094
Radwan MA, AlQuadeib BT, Šiller L, Wright MC, Horrocks B (2017) Oral administration of amphotericin B nanoparticles: antifungal activity, bioavailability and toxicity in rats. Drug Deliv 24:40–50
Rapaka RR, Dai G, Zheng M, Kolls JK (2019) CD4(+) T cell regulation of antibodies cross-reactive with fungal cell wall-associated carbohydrates after pneumocystis murina infection. Infect Immun 87(7):e00158-19
Rella A, Mor V, Farnoud AM, Singh A, Shamseddine AA, Ivanova E, Carpino N, Montagna MT, Luberto C, Del Poeta M (2015) Role of Sterylglucosidase 1 (Sgl1) on the pathogenicity of Cryptococcus neoformans: potential applications for vaccine development. Front Microbiol 6:836
Ribeiro AM, Bocca AL, Amaral AC, Faccioli LH, Galetti FC, Zárate-Bladés CR, Figueiredo F, Silva CL, Felipe MS (2009) DNAhsp65 vaccination induces protection in mice against Paracoccidioides brasiliensis infection. Vaccine 27:606–613
Rittner GM, Muñoz JE, Marques AF, Nosanchuk JD, Taborda CP, Travassos LR (2012) Therapeutic DNA vaccine encoding peptide P10 against experimental paracoccidioidomycosis. PLoS Negl Trop Dis 6:e1519
Rivera A, Lodge J, Xue C (2022) Harnessing the immune response to fungal pathogens for vaccine development. Annu Rev Microbiol 76:703–726
Rohatgi S, Pirofski LA (2012) Molecular characterization of the early B cell response to pulmonary Cryptococcus neoformans infection. J Immunol 189:5820–5830
Roy RM, Klein BS (2012) Dendritic cells in antifungal immunity and vaccine design. Cell Host Microbe 11:436–446
Ruiz Mendoza S, Liedke SC, Rodriguez de La Noval C, Ferreira MDS, Gomes KX, Honorato L, Nimrichter L, Peralta JM, Guimarães AJ (2022) In vitro and in vivo efficacies of Dectin-1-Fc(IgG)(s) fusion proteins against invasive fungal infections. Med Mycol 60(8):myac050
Sandini S, La Valle R, Deaglio S, Malavasi F, Cassone A, De Bernardis F (2011) A highly immunogenic recombinant and truncated protein of the secreted aspartic proteases family (rSap2t) of Candida albicans as a mucosal anticandidal vaccine. FEMS Immunol Med Microbiol 62:215–224
Santos LA, Grisolia JC, Burger E, de Araujo Paula FB, Dias ALT, Malaquias LCC (2020) Virulence factors of Paracoccidioides brasiliensis as therapeutic targets: a review. Antonie Van Leeuwenhoek 113:593–604
Saville SP, Lazzell AL, Chaturvedi AK, Monteagudo C, Lopez-Ribot JL (2009) Efficacy of a genetically engineered Candida albicans tet-NRG1 strain as an experimental live attenuated vaccine against hematogenously disseminated candidiasis. Clin Vaccine Immunol 16:430–432
Scheckelhoff MR, Deepe GS Jr (2006) Pulmonary V beta 4+ T cells from Histoplasma capsulatum-infected mice respond to a homologue of Sec31 that confers a protective response. J Infect Dis 193:888–897
Sevilla MJ, Robledo B, Rementeria A, Moragues MD, Pontón J (2006) A fungicidal monoclonal antibody protects against murine invasive candidiasis. Infect Immun 74:3042–3045
Sherwani MA, Tufail S, Khan AA, Owais M (2015) Gold nanoparticle-photosensitizer conjugate based photodynamic inactivation of biofilm producing cells: potential for treatment of C. albicans infection in BALB/c mice. PLoS ONE 10:e0131684
Shi H, Dong S, Zhang X, Chen X, Gao X, Wang L (2018) Phage vaccines displaying YGKDVKDLFDYAQE epitope induce protection against systemic candidiasis in mouse model. Vaccine 36:5717–5724
Shibasaki S, Aoki W, Nomura T, Miyoshi A, Tafuku S, Sewaki T, Ueda M (2013) An oral vaccine against candidiasis generated by a yeast molecular display system. Pathog Dis 69:262–268
Shubitz LF, Yu JJ, Hung CY, Kirkland TN, Peng T, Perrill R, Simons J, Xue J, Herr RA, Cole GT, Galgiani JN (2006) Improved protection of mice against lethal respiratory infection with Coccidioides posadasii using two recombinant antigens expressed as a single protein. Vaccine 24:5904–5911
Shukla M, Rohatgi S (2020) Vaccination with secreted aspartyl proteinase 2 protein from Candida parapsilosis can enhance survival of mice during C. tropicalis-mediated systemic candidiasis. Infect Immun 88(10):e00312-20
Shukla M, Chandley P, Rohatgi S (2021) The role of B-cells and antibodies against candida vaccine antigens in invasive candidiasis. Vaccines (Basel) 9(10):1159
Smole U, Kratzer B, Pickl WF (2020) Soluble pattern recognition molecules: Guardians and regulators of homeostasis at airway mucosal surfaces. Eur J Immunol 50:624–642
Specht CA, Lee CK, Huang H, Tipper DJ, Shen ZT, Lodge JK, Leszyk J, Ostroff GR, Levitz SM (2015) Protection against experimental cryptococcosis following vaccination with glucan particles containing cryptococcus alkaline extracts. Bio 6:e01905-01915
Specht CA, Lee CK, Huang H, Hester MM, Liu J, Luckie BA, Torres Santana MA, Mirza Z, Khoshkenar P, Abraham A, Shen ZT, Lodge JK, Akalin A, Homan J, Ostroff GR, Levitz SM (2017) Vaccination with recombinant cryptococcus proteins in glucan particles protects mice against cryptococcosis in a manner dependent upon mouse strain and cryptococcal species. mBio 8(6):e01872-17
Spellberg BJ, Ibrahim AS, Avenissian V, Filler SG, Myers CL, Fu Y, Edwards JE Jr (2005) The anti-Candida albicans vaccine composed of the recombinant N terminus of Als1p reduces fungal burden and improves survival in both immunocompetent and immunocompromised mice. Infect Immun 73:6191–6193
Spellberg BJ, Ibrahim AS, Avanesian V, Fu Y, Myers C, Phan QT, Filler SG, Yeaman MR, Edwards JE Jr (2006) Efficacy of the anti-Candida rAls3p-N or rAls1p-N vaccines against disseminated and mucosal candidiasis. J Infect Dis 194:256–260
Stuehler C, Khanna N, Bozza S, Zelante T, Moretti S, Kruhm M, Lurati S, Conrad B, Worschech E, Stevanović S, Krappmann S, Einsele H, Latgé JP, Loeffler J, Romani L, Topp MS (2011) Cross-protective TH1 immunity against Aspergillus fumigatus and Candida albicans. Blood 117:5881–5891
Suleyman G, Alangaden GJ (2021) Nosocomial fungal infections: epidemiology, infection control, and prevention. Infect Dis Clin North Am 35:1027–1053
Sun D, Shi M (2016) Neutrophil swarming toward Cryptococcus neoformans is mediated by complement and leukotriene B4. Biochem Biophys Res Commun 477:945–951
Tarcha EJ, Basrur V, Hung CY, Gardner MJ, Cole GT (2006) A recombinant aspartyl protease of Coccidioides posadasii induces protection against pulmonary coccidioidomycosis in mice. Infect Immun 74:516–527
Tong Y, Tang J (2017) Candida albicans infection and intestinal immunity. Microbiol Res 198:27–35
Tong C, Cui Z, Sun X, Lei L, Feng X, Sun C, Gu J, Han W (2016) Mannan derivatives instruct dendritic cells to induce Th1/Th2 cells polarization via differential mitogen-activated protein kinase activation. Scand J Immunol 83:10–17
Torosantucci A, Bromuro C, Chiani P, De Bernardis F, Berti F, Galli C, Norelli F, Bellucci C, Polonelli L, Costantino P, Rappuoli R, Cassone A (2005) A novel glyco-conjugate vaccine against fungal pathogens. J Exp Med 202:597–606
Tso GHW, Reales-Calderon JA, Pavelka N (2018) The elusive anti-candida vaccine: lessons from the past and opportunities for the future. Front Immunol 9:897
Ueno K, Urai M, Sadamoto S, Shinozaki M, Takatsuka S, Abe M, Otani Y, Yanagihara N, Shimizu K, Iwakura Y, Shibuya K, Miyazaki Y, Kinjo Y (2019) A dendritic cell-based systemic vaccine induces long-lived lung-resident memory Th17 cells and ameliorates pulmonary mycosis. Mucosal Immunol 12:265–276
Uezu K, Kawakami K, Miyagi K, Kinjo Y, Kinjo T, Ishikawa H, Saito A (2004) Accumulation of gammadelta T cells in the lungs and their regulatory roles in Th1 response and host defense against pulmonary infection with Cryptococcus neoformans. J Immunol 172:7629–7634
Upadhya R, Lam WC, Maybruck B, Specht CA, Levitz SM, Lodge JK (2016) Induction of protective immunity to cryptococcal infection in mice by a heat-killed, chitosan-deficient strain of Cryptococcus neoformans. mBio 7(3):e00547-16
van de Veerdonk FL, Gresnigt MS, Romani L, Netea MG, Latgé JP (2017) Aspergillus fumigatus morphology and dynamic host interactions. Nat Rev Microbiol 15:661–674
Vazquez JA, Gupta S, Villanueva A (1998) Potential utility of recombinant human GM-CSF as adjunctive treatment of refractory oropharyngeal candidiasis in AIDS patients. Eur J Clin Microbiol Infect Dis 17:781–783
Vecchiarelli A, Cenci E, Puliti M, Blasi E, Puccetti P, Cassone A, Bistoni F (1989) Protective immunity induced by low-virulence Candida albicans: cytokine production in the development of the anti-infectious state. Cell Immunol 124:334–344
Voigt J, Hünniger K, Bouzani M, Jacobsen ID, Barz D, Hube B, Löffler J, Kurzai O (2014) Human natural killer cells acting as phagocytes against Candida albicans and mounting an inflammatory response that modulates neutrophil antifungal activity. J Infect Dis 209:616–626
Wang H, LeBert V, Hung CY, Galles K, Saijo S, Lin X, Cole GT, Klein BS, Wüthrich M (2014) C-type lectin receptors differentially induce th17 cells and vaccine immunity to the endemic mycosis of North America. J Immunol 192:1107–1119
Wang H, Li M, Lerksuthirat T, Klein B, Wüthrich M (2015) The C-type lectin receptor MCL mediates vaccine-induced immunity against infection with blastomyces dermatitidis. Infect Immun 84:635–642
Wang F, Zhang C, Jiang Y, Kou C, Kong Q, Long N, Lu L, Sang H (2017a) Innate and adaptive immune response to chronic pulmonary infection of hyphae of Aspergillus fumigatus in a new murine model. J Med Microbiol 66:1400–1408
Wang H, Lee TJ, Fites SJ, Merkhofer R, Zarnowski R, Brandhorst T, Galles K, Klein B, Wüthrich M (2017b) Ligation of Dectin-2 with a novel microbial ligand promotes adjuvant activity for vaccination. PLoS Pathog 13:e1006568
Wang Y, Kwak M, Lee PC, Jin JO (2018) Rehmannia glutinosa polysaccharide promoted activation of human dendritic cells. Int J Biol Macromol 116:232–238
Wang YL, Shu XH, Zhang X, Liu YB, Zhang YJ, Lv T, Huang X, Song CL (2021) Effects of two polysaccharides from traditional Chinese medicines on rat immune function. Front Vet Sci 8:703956
Wang X, Liu P, Jiang Y, Han B, Yan L (2022a) The prophylactic effects of monoclonal antibodies targeting the cell wall Pmt4 protein epitopes of Candida albicans in a murine model of invasive candidiasis. Front Microbiol 13:992275
Wang Y, Pawar S, Dutta O, Wang K, Rivera A, Xue C (2022b) Macrophage mediated immunomodulation during cryptococcus pulmonary infection. Front Cell Infect Microbiol 12:859049
Wang R, Oliveira LVN, Lourenco D, Gomez CL, Lee CK, Hester MM, Mou Z, Ostroff GR, Specht CA, Levitz SM (2023) Immunological correlates of protection following vaccination with glucan particles containing Cryptococcus neoformans chitin deacetylases. NPJ Vaccines 8:6
Wang Y, Wang K, Masso-Silva JA, Rivera A, Xue C (2019) A heat-killed cryptococcus mutant strain induces host protection against multiple invasive mycoses in a murine vaccine model. mBio 10(6):e02145-19
Wozniak KL, Young ML, Wormley FL Jr (2011) Protective immunity against experimental pulmonary cryptococcosis in T cell-depleted mice. Clin Vaccine Immunol 18:717–723
Wu X, Lipinski T, Carrel FR, Bailey JJ, Bundle DR (2007) Synthesis and immunochemical studies on a Candida albicans cluster glycoconjugate vaccine. Org Biomol Chem 5:3477–3485
Wu B, Zou Q, Hu Y, Wang B (2013a) Interleukin-22 as a molecular adjuvant facilitates IL-17-producing CD8+ T cell responses against a HBV DNA vaccine in mice. Hum Vaccin Immunother 9:2133–2141
Wu SY, Yu JS, Liu FT, Miaw SC, Wu-Hsieh BA (2013b) Galectin-3 negatively regulates dendritic cell production of IL-23/IL-17-axis cytokines in infection by Histoplasma capsulatum. J Immunol 190:3427–3437
Wu S, Wang Y, Liu N, Dong G, Sheng C (2017) Tackling fungal resistance by biofilm inhibitors. J Med Chem 60:2193–2211
Wüthrich M, Gern B, Hung CY, Ersland K, Rocco N, Pick-Jacobs J, Galles K, Filutowicz H, Warner T, Evans M, Cole G, Klein B (2011a) Vaccine-induced protection against 3 systemic mycoses endemic to North America requires Th17 cells in mice. J Clin Invest 121:554–568
Wüthrich M, Hung CY, Gern BH, Pick-Jacobs JC, Galles KJ, Filutowicz HI, Cole GT, Klein BS (2011b) A TCR transgenic mouse reactive with multiple systemic dimorphic fungi. J Immunol 187:1421–1431
Wüthrich M, Dobson HE, Ledesma Taira C, Okaa UJ, Dos Santos DL, Isidoro-Ayza M, Petrovsky N, Klein BS (2021) Combination adjuvants enhance recombinant protein vaccine protection against fungal infection. Mbio 12:e0201821
Xin H, Cutler JE (2011) Vaccine and monoclonal antibody that enhance mouse resistance to candidiasis. Clin Vaccine Immunol 18:1656–1667
Xin H, Dziadek S, Bundle DR, Cutler JE (2008) Synthetic glycopeptide vaccines combining beta-mannan and peptide epitopes induce protection against candidiasis. Proc Natl Acad Sci U S A 105:13526–13531
Xin H, Cartmell J, Bailey JJ, Dziadek S, Bundle DR, Cutler JE (2012) Self-adjuvanting glycopeptide conjugate vaccine against disseminated candidiasis. PLoS ONE 7:e35106
Yamanaka-Takaichi M, Ghanian S, Katzka DA, Torgerson RR, Alavi A (2022) Candida infection associated with Anti-IL-17 medication: a systematic analysis and review of the literature. Am J Clin Dermatol 23:469–480
Yang YL, Wang CW, Chen CT, Wang MH, Hsiao CF, Lo HJ (2009) Non-lethal Candida albicans cph1/cph1 efg1/efg1 mutant partially protects mice from systemic infections by lethal wild-type cells. Mycol Res 113:388–390
Yang H, Han S, Zhao D, Wang G (2014) Adjuvant effect of polysaccharide from fruits of Physalis alkekengi L. in DNA vaccine against systemic candidiasis. Carbohydr Polym 109:77–84
Yang F, Xiao C, Qu J, Wang G (2016) Structural characterization of low molecular weight polysaccharide from Astragalus membranaceus and its immunologic enhancement in recombinant protein vaccine against systemic candidiasis. Carbohydr Polym 145:48–55
Yang P, Xu R, Chen F, Chen S, Khan A, Li L, Zhang X, Wang Y, Xu Z, Shen H (2023) Fungal gut microbiota dysbiosis in systemic lupus erythematosus. Front Microbiol 14:1149311
Zhai B, Wozniak KL, Masso-Silva J, Upadhyay S, Hole C, Rivera A, Wormley FL Jr, Lin X (2015) Development of protective inflammation and cell-mediated immunity against Cryptococcus neoformans after exposure to hyphal mutants. Mbio 6:e01433-e11415
Zhang Z, Chen Y, Yin Y, Chen Y, Chen Q, Bing Z, Zheng Y, Hou Y, Shen S, Chen Y, Wang T (2022) Candida tropicalis induces NLRP3 inflammasome activation via glycogen metabolism-dependent glycolysis and JAK-STAT1 signaling pathway in myeloid-derived suppressor cells to promote colorectal carcinogenesis. Int Immunopharmacol 113:109430
Zheng NX, Wang Y, Hu DD, Yan L, Jiang YY (2015) The role of pattern recognition receptors in the innate recognition of Candida albicans. Virulence 6:347–361
Funding
This work was supported by Natural Science Foundation for Distinguished Young Scholars of Anhui Province (2008085J40).
Author information
Authors and Affiliations
Contributions
Zixu Wang and Jing Shao wrote the main manuscript text, prepared figure 1 and 2, Table 1. Both authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interests
The authors declare no competing interests.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Additional information
Communicated by Yusuf Akhter.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, Z., Shao, J. Fungal vaccines and adjuvants: a tool to reveal the interaction between host and fungi. Arch Microbiol 206, 293 (2024). https://doi.org/10.1007/s00203-024-04010-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00203-024-04010-7