Abstract
Summary
We studied factors affecting osteoporotic hip fracture mortality in Hawaiʻi, a region with unique geography and racial composition. Men, older adults, higher ASA score, lower BMI, and NHPI race were associated with higher mortality. This is the first study demonstrating increased mortality risk after hip fracture in NHPI patients.
Purpose
To estimate mortality rates and identify specific risk factors associated with 1-year mortality after osteoporotic hip fracture in Hawaiʻi.
Methods
A retrospective review of adults (≥ 50 years) hospitalized with an osteoporotic hip fracture at a large multicenter healthcare system in Hawaiʻi from 2011 to 2019. The Kaplan–Meier curves and log-rank tests examined survival probability by sex, age group, race/ethnicity, primary insurance, body mass index (BMI), and American Society of Anesthesiologists (ASA) physical status classification. After accounting for potential confounders, adjusted hazard ratios (aHR) and 95% confidence intervals (CI) were obtained from Cox proportional hazards regression models.
Results
We identified 1755 cases of osteoporotic hip fracture. The cumulative mortality rate 1 year after fracture was 14.4%. Older age (aHR 3.50; 95% CI 2.13–5.76 for ≥ 90 vs 50–69), higher ASA score (aHR 5.21; 95% CI 3.09–8.77 for ASA 4–5 vs 1–2), and Native Hawaiian/Pacific Islander (NHPI) race (aHR 1.84; 95% CI 1.10–3.07 vs. White) were independently associated with higher mortality risk. Female sex (aHR 0.64; 95% CI 0.49–0.84 vs male sex) and higher BMI (aHR 0.35; 95% CI 0.18–0.68 for obese vs underweight) were associated with lower mortality risk.
Conclusion
In our study, men, older adults, higher ASA score, lower BMI, and NHPI race were associated with significantly higher mortality risk after osteoporotic hip fracture. NHPIs are an especially vulnerable group and comprise a significant portion of Hawaiʻi’s population. Further research is needed to address the causes of higher mortality and interventions to reduce hip fractures and associated mortality.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Osteoporotic hip fractures represent a serious health concern in older adults and are associated with significant morbidity and mortality. Osteoporosis is a skeletal disorder characterized by decreased bone mineral density and strength, which is associated with an increased risk for hip fracture, especially in older post-menopausal women [1, 2]. Overall mortality within 1 year after hip fracture has been estimated to be as high as 33%, with several studies reporting mortality rates greater than 20% [3,4,5,6,7]. In addition, mortality rates have been found to increase over time, with one long-term study finding that 1-year mortality increased by 2% each year over 17 years [3]. As elderly populations continue to grow in many countries worldwide, it is estimated that the number of hip fractures could increase to 4.5 million by the year 2050, more than three times the 1.26 million estimated in 1990 [8].
Specific patient groups have been found to have higher rates of mortality following hip fracture. Men have higher excess mortality and risk of death after hip fracture despite women sustaining more hip fractures overall [9,10,11]. In addition, differences in mortality, survival, and function after hip fracture have also been reported by race and ethnicity [12,13,14]. Hawaiʻi is home to an ethnically diverse population, especially compared to the contiguous USA. According to 2020 census data, 37.2% of individuals living in Hawaiʻi identified as Asian, 10.8% identified as Native Hawaiian and other Pacific Islander, and 25.3% identified as two or more races [15]. Hawaiʻi’s elderly population has also been steadily increasing with each decade. It is now estimated that individuals 65 and older will make up 23.7% of the state’s population by 2040 [16].
Studies investigating mortality after osteoporotic hip fracture in Hawaiʻi are limited. Additional long-term studies in Hawaiʻi are needed to better understand the current state of hip fracture mortality, identify populations at high risk for mortality after hip fracture, and facilitate targeted interventions in those high-risk populations. The diversity of the population in Hawaiʻi presents a unique opportunity to study hip fracture mortality in understudied populations, such as NHPI. Therefore, this study aimed to determine mortality rates and identify specific risk factors associated with 1-year mortality after osteoporotic hip fracture in Hawaiʻi.
Methods
Research setting and design
This was a retrospective chart review of patients admitted for hip fractures at three medical centers within the Hawaiʻi Pacific Health healthcare system from 2011 to 2019. Hawaiʻi Pacific Health is a not-for-profit healthcare network of hospitals, clinics, physicians, and other healthcare providers that covers the state of Hawaiʻi. It is one of Hawaiʻi’s largest healthcare providers [17]. This study was reviewed by the Hawaiʻi Pacific Health Research Institute (HPHRI) and determined to be exempt from Institutional Review Board review and patient consent (HPHRI Study Number: 2020–059).
Study participants
This study included patients aged 50 years or older hospitalized with a primary diagnosis of hip fracture from January 1, 2011, to December 31, 2019. Hip fracture cases were identified by searching for patients with a primary discharge diagnosis ICD-9 code (corresponding ICD-10 code) of 820.0 (S72019A, S72023A, S72026A, S72033A, S72036A, S72043A, S72046A, S72099A), 820.2 (S72109A, S721143A, S72146A, S7223XA, and S7226XA), and 820.8 (S72009A). Osteoporotic hip fractures were defined as those resulting from a fall from standing height or less. Cases with a diagnostic ICD-9 code of 733.14 were not included because this code is frequently associated with femur fractures related to malignancy. More than one fracture per person was only allowed if the subsequent fracture occurred more than 180 days from the previous one. More recent admissions likely represented readmissions from medical or surgical complications (363 cases excluded). Open fractures with ICD-9 codes of 820.1, 820.3, 820.9 (5 cases), subtrochanteric, pathological, and non-specific fractures were also excluded, resulting in 2208 total cases. Non-specific fractures included acetabular fractures or pelvic fractures.
Variables for analysis
Data collected included the age of the patient at the time of admission, sex, weight, height, race/ethnicity (White, Chinese, Filipino, Japanese, NHPI, and others), primary insurance (private, Medicare, Medicaid, and others), admission year, treatment facility (A, B, and C), fracture type (femoral neck and intertrochanteric), osteoporosis treatment before admission (yes and no), ASA score, and surgical procedure during the hospitalization (yes and no). Treatment facilities A, B, and C are all medical centers within the Hawai’i Pacific Health healthcare system. Treatment facility A is located in the state capital of Honolulu on the island of O’ahu. Treatment facility B is located in central O’ahu. Treatment facility C is located on the island of Kaua’i.
Ages at admission were classified into three groups (50–69 years, 70–89 years, ≥90 years). Using BMI calculated from weight and height, patients were categorized into four BMI groups (underweight (< 18.5), healthy (18.5–24.9), overweight (25–29.9), and obese (≥30)). Osteoporosis treatment before admission included treatment with bisphosphonates (ibandronate, zoledronic acid, risedronate, and alendronate), denosumab, calcitonin, raloxifene, teriparatide, abaloparatide, or romosozumab.
Anesthesiologists use the ASA physical status classification to assess patients' general health before surgery and anesthesia. The score uses a scale from 1 to 6 to assess a patient’s overall physical status with six classes ((1) the patient is a completely healthy fit patient, (2) the patient has mild systemic disease, (3) the patient has severe systemic disease that is not incapacitating, (4) the patient has incapacitating disease that is a constant threat to life, (5) a moribund patient who is not expected to live 24 h with or without surgery, (6) identifies deceased organ donors) [18]. This study categorized patients into three groups (ASA score: 1–2, 3, and 4–5). The ASA score is a standardized way for anesthesiologists to communicate a patient's general status to other healthcare providers [19]. While not primarily used to predict surgical mortality risks, it may represent the global physiological impact of pre-existing diseases on the patient and is predictive of mortality and postoperative complications in hip fracture patients [20, 21]. A patient’s 1-year mortality status was defined by discharge disposition and their later electronic medical records. The admission date was defined as the index date for each hip fracture case.
The race/ethnicity variable was created from categories consistently available across all hospitals in Hawaiʻi, as per Hawaiʻi Health Information Corporation. Hawaiʻi Health Information Corporation data are used nationally by the Agency for Healthcare Research and Quality in the Healthcare Cost and Utilization Project [22]. Race and ethnicity data were provided by patient self-report at intake and included one primary race. Multiethnic individuals were represented by self-reports of their primary race [23,24,25,26]. Specific Asian/Asian American race categories were used due to the large Asian/Asian American population in Hawaiʻi in contrast with the combined category used by the US Census [26].
Statistical analysis
Patient characteristics by 1-year mortality status were described with frequencies and percentages for categorical variables and mean and standard deviations for continuous variables. Differences in patient characteristics between mortality status groups were examined by bivariate analysis with Pearson’s chi-squared test or Fisher’s exact test for categorical variables and t-test for continuous variables. The probability of surviving over 1 year from admission was examined with the Kaplan–Meier estimate and visualized in the Kaplan–Meier survival curve. The log-rank test was used to examine differences in survival probability by age group, sex, race/ethnicity, primary insurance, BMI group, ASA score, fracture type, and if the patient received surgical intervention. Cox proportional hazard regression models were constructed to examine the association between ASA scores and 1-year mortality. The first model included the ASA score (unadjusted model). The second model included variables with a p-value less than 0.10 in the bivariate analysis (adjusted model 1). The final model included variables with a p-value less than 0.05 in the second model (adjusted model 2). An unadjusted hazard ratio (uHR) and adjusted hazard ratios (aHRs) and their 95% confidence intervals (CIs) were obtained from model results. The proportional hazards assumption for the final model fit was tested using the Schoenfeld residuals against the transformed time. A p-value < 0.05 was considered statistically significant. All analyses were performed using R version 4.2.2 [27].
Results
Characteristics of the study population
There were 2208 total hospitalizations for osteoporotic hip fracture from 2011 to 2019. Within that population, 453 patients were missing ASA scores or BMI values. Those patients were excluded from the study, resulting in 1755 remaining cases for statistical analysis. Table 1 shows the baseline characteristics of patients with osteoporotic hip fractures (n = 1755). The overall mean age at admission was 80.7 years, and more than half of patients were within the 70–89 age group (58.6%). A total of 81.8% of osteoporotic hip fracture patients were 70 years or older. Many patients were female (71.7%), 36.2% of patients were White, and 63.8% were non-White. Those of non-White race primarily consisted of Japanese (36.2%), Filipino (10.1%), Chinese (4.7%), and NHPI (5.6%). Most patients had public insurance as their primary payer (Medicare: 65.2%; Medicaid: 23.8%). Before admission for hip fracture, only 6.6% of patients received osteoporosis treatment. Most patients (54.1%) had a healthy BMI (18.5–-24.9), while 28.5% were considered overweight or obese and 17.4% were considered underweight. Patients with an ASA score of 3 or greater comprised 76.1% of the study population. The majority of fractures were femoral neck fractures (55.4%).
Cumulative mortality and factors affecting 1-year mortality after hip fracture admission
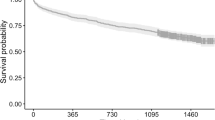
The cumulative mortality rate 1 year after admission for osteoporotic hip fracture was 14.4%. Table 1 summarizes patient characteristics concerning 1-year mortality. Within the group of those who expired before one year, there was a higher proportion of 90 + -year-old patients (p < 0.001), males (p = 0.027), non-White individuals (p = 0.004), those with Medicaid (p < 0.001), underweight individuals (p < 0.001), and those with an ASA score of 3, 4, or 5 (p < 0.001) compared to the group of those who survived after one year from admission. Figure 1 shows the Kaplan–Meier survival curves and log-rank test results for the 1-year survival rates after hip fracture admission, comparing patients by age group, sex, race/ethnicity, primary insurance, BMI group, and ASA score. Survival rates appear lower amongst older age groups (χ2 = 78.6, df = 2, p < 0.001), men (χ2 = 5.1, df = 1, p = 0.02), NHPI and Chinese race (χ2 = 17.2, df = 5, p = 0.004), patients who had Medicare and Medicaid insurance (χ2 = 19.5, df = 3, p < 0.001), patients with underweight BMI (χ2 = 40.9, df = 3, p < 0.001), and higher ASA score groups (χ2 = 71.5, df = 2, p < 0.001), compared to their respective corresponding groups.
Kaplan–Meier curves in 1755 inpatients up to 1 year following hip fracture according to age group, sex, race/ethnicity, primary insurance, BMI group, and ASA score. BMI, body mass index; NHPI, Native Hawaiian/Pacific Islander; ASA, American Society of Anesthesiologists. P-values were obtained from log-rank tests
Hazard ratios of 1-year mortality
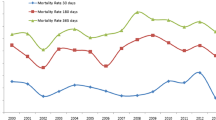
Table 2 summarizes the results of the Cox regression unadjusted and adjusted model 1. The unadjusted model suggests that the risk for 1-year mortality after hip fracture in those with an ASA score of 4 or 5 was 7.29 times higher than those with an ASA score of 1 or 2 [uHR (95% CI) = 7.29 (4.36, 12.2)]. After adjusting for potential confounders (adjusted model 1), their risk decreased; however, it was still 5.03 times higher [aHR (95% CI) = 5.03 (2.98, 8.49)]. After excluding the covariates with a p-value of 0.05 or greater (adjusted model 2), the 1-year mortality risk among those with an ASA score of 4 or 5 increased: it was 5.21 times higher than that of those with an ASA score of 1 or 2 [aHR (95% CI) = 5.21 (3.09, 8.77)] (Fig. 2). Older age (70–89 vs. 50–69: aHR (95% CI) = 1.62 (1.01, 2,62); ≥90 vs 50–69: aHR (95% CI) = 3.50 (2.13, 5.76)) and NHPI race (vs White: aHR (95% CI) = 1.84 (1.10, 3.07)) were also independently associated with higher mortality risk. Female sex (vs male: aHR (95% CI) = 0.64 (0.49, 0.84)) and higher BMI (healthy vs. underweight: aHR (95% CI) = 0.55 (0.41, 0.74); overweight vs. underweight: aHR (95% CI) = 0.40 (0.26, 0.61); obese vs underweight: aHR (95% CI) = 0.35 (0.18, 0.68)) were associated with lower mortality risk.
Adjusted hazard ratios of 1 year survival among inpatients with hip fractures: Cox proportional hazards regression modela (n = 1755). BMI, body mass index; NHPI, Native Hawaiian/Pacific Islander; ASA, American Society of Anesthesiologists. P-values were obtained from log-rank tests. aHazard ratios were obtained from the final model (model 2), including the variables with a p-value less than 0.05 in model 1 (Table 2). The chi-square test for the proportional hazards assumption found no violation (p > 0.05 for all variables)
Discussion
Despite rapid population aging in Hawaiʻi leading to an excess burden on the healthcare system, few studies have studied hip fractures in Hawaiʻi [2, 28]. Hawaiʻi is unique and differs from the contiguous USA, particularly regarding racial composition. Furthermore, to our knowledge, no recent studies have investigated hip fractures in minority groups such as NHPI. This long-term study from 2011 to 2019 identified independent risk factors associated with 1-year mortality after osteoporotic hip fracture in a large sample population in Hawaiʻi. This study showed higher 1-year mortality after hip fracture among NHPI patients and provides valuable data on hip fracture mortality in Hawaiʻi. While 1-year mortality after hip fracture is variable ranging from 14 to 58% [29], our study showed that 1-year mortality after hip fracture in Hawai’i is on the relatively lower end of the spectrum when compared to the contiguous USA and other parts of the world. However, future studies are needed to better understand the state of hip fractures in Hawaiʻi and to implement comprehensive and targeted interventions to reduce mortality [30].
NHPI patients are an especially vulnerable group in Hawaiʻi that has experienced significant health, economic, and social disparities. Native Hawaiians have been found to have higher mortality rates than the general population due to conditions like heart disease and diabetes [31]. Our study adds to the body of literature concerning disparities of care amongst NHPI patients by highlighting disparities in the care of hip fractures, a finding that has not been previously reported [32]. The poor clinical outcomes in NHPI patients have been attributed to a disproportionate disease burden, worsened by barriers to healthcare access and utilization in NHPI patients [33]. Additional research on hip fractures in the NHPI population is needed to determine whether there are ethnic differences in bone strength measurements, the incidence of osteoporosis, or risk factors for fracture in NHPI patients [32]. Our study reinforces the need to promote healthcare equity in NHPI patients.
Consistent with prior studies, male sex and older age were independent predictors of increased risk for mortality one year after hip fracture. Age is a non-modifiable risk factor for hip fracture and likely makes recovery after fracture more difficult, which is illustrated by the higher mortality risk that was determined in this study [34]. The higher rates of mortality among males compared to females have been previously reported [9, 28, 35, 36]. Further studies are needed to clarify this finding, with some studies attributing increased mortality in men to increased risk of infections (pneumonia, influenza, and septicemia) post-hip fracture [37]. However, the increased risk of mortality in men persists even after adjusting for comorbid conditions [35], as seen in our study. Additionally, differences in the quality of in-hospital care have not been found to explain the higher mortality in men with hip fractures [38].
Higher BMI values were associated with lower mortality risk and may be a protective factor following hip fracture. The “obesity paradox” is a finding where the risk of outcome (e.g., mortality) is significantly reduced for higher BMI, where increased risk is expected [39]. The “obesity paradox” has been noted in cancer and cardiovascular disease, and there seems to be evidence that it is seen in mortality post-hip fracture. Obesity may be protective against frailty, which contributes to mortality post-fracture. Obese individuals may have a higher reservoir of triglyceride that can provide vital calories to help the body heal in the post-hip fracture state [40]. Other authors have suggested methodical and non-causal explanations, including reverse causation [28, 41, 42]. Further research is needed to delineate the relationship between BMI and one-year mortality post-fracture.
This study provides insight into the state of hip fractures in Hawaiʻi by identifying patients who are at high risk for mortality after hip fracture. Specific interventions targeting these high-risk groups are critical. Osteoporosis treatment, appropriate rehabilitation, and fall prevention assessments are crucial interventions that should be implemented following a hip fracture, as those with a prior hip fracture are at an increased risk for future fracture [34]. Implementing a fracture liaison service is another intervention that has been shown to improve appropriate osteoporosis evaluation and offer treatment for patients after discharge [43]. The results of this study highlight a gap in osteoporosis care in Hawai’i and may be an initiative in implementing fracture liaison services or fracture prevention programs in hospitals in Hawai’i. Focusing on NHPI patients, efforts are needed to establish culturally sensitive healthcare systems, increase NHPI representation in the healthcare workforce, allocate sufficient financial resources via NHPI-administered programs, and implement better screening and education programs in predominantly NHPI communities [31].
Our study has several limitations to acknowledge. First, because our study was retrospective, there may be errors and inconsistencies within medical records. Due to the study design, we were not able to determine the causes of death of hip fracture patients. Death was identified through medical records and not registry data. Therefore, there may be cases of mortality after hip fracture that may be missed, underestimating hip fracture mortality rates.
Furthermore, there may be inaccuracies in recording of comorbidities at the time of hip fracture. We did not calculate more specific comorbidity scores (Charlson Comorbidity Index) and did not adjust for specific comorbidity scores in our model. In our study, we used the ASA physical status instead, which is a measure of a patient's general health at the time of surgery. ASA was readily available from anesthesiologist notes within electronic medical records. ASA and Charlson Comorbidity Index have shown similarly strong stepwise association with 1-year mortality in hip fractures [44], and ASA has been found to be correlated to more objective comorbidity measures such as the Charlson Comorbidity Index and Elixhauser comorbidity index [45, 46]. Second, our study was conducted within a single healthcare organization in Hawaiʻi. Therefore, our findings may not generalize to other regions or healthcare systems. Third, while we adjusted for confounding in the determination of factors that affect hip fracture mortality, there is a possibility of unmeasured confounding factors leading to bias.
Conclusion
The purpose of this study was to estimate mortality rates and identify specific risk factors associated with 1-year mortality after osteoporotic hip fracture in Hawaiʻi. Understanding which populations are at the highest risk for mortality after hip fracture is important because targeted interventions are needed in those high-risk populations. Specific patient populations like men and older adults were found to be at higher risk for mortality after hip fracture. In contrast, certain factors like higher BMI were found to be potentially protective. In particular, NHPI patients were found to be at increased risk for mortality after hip fracture. Our study highlights the need for further efforts to achieve healthcare equity in hip fracture care.
Data availability
The data that support the findings of this study are available on request from the corresponding author, SYL. The data are not publicly available due to patient level data that could compromise the privacy of research participants.
References
Aspray TJ, Hill TR (2019) Osteoporosis and the ageing skeleton. Subcell Biochem 91:453–476
Lim SY, Bolster MB (2015) Current approaches to osteoporosis treatment. Curr Opin Rheumatol 27:216–224
Guzon-Illescas O, Perez Fernandez E, Crespi Villarias N, Quiros Donate FJ, Pena M, Alonso-Blas C, Garcia-Vadillo A, Mazzucchelli R (2019) Mortality after osteoporotic hip fracture: incidence, trends, and associated factors. J Orthop Surg Res 14:203
Barcelo M, Torres OH, Mascaro J, Casademont J (2021) Hip fracture and mortality: study of specific causes of death and risk factors. Arch Osteoporos 16:15
Karres J, Zwiers R, Eerenberg JP, Vrouenraets BC, Kerkhoffs G (2022) Mortality prediction in hip fracture patients: physician assessment versus prognostic models. J Orthop Trauma 36:585–592
Cummings SR, Melton LJ (2002) Epidemiology and outcomes of osteoporotic fractures. Lancet 359:1761–1767
Johnell O, Kanis J (2005) Epidemiology of osteoporotic fractures. Osteoporos Int 16(Suppl 2):S3-7
Gullberg B, Johnell O, Kanis JA (1997) World-wide projections for hip fracture. Osteoporos Int 7:407–413
Haentjens P, Magaziner J, Colon-Emeric CS, Vanderschueren D, Milisen K, Velkeniers B, Boonen S (2010) Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med 152:380–390
von Friesendorff M, McGuigan FE, Wizert A, Rogmark C, Holmberg AH, Woolf AD, Akesson K (2016) Hip fracture, mortality risk, and cause of death over two decades. Osteoporos Int 27:2945–2953
Katsoulis M, Benetou V, Karapetyan T et al (2017) Excess mortality after hip fracture in elderly persons from Europe and the USA: the CHANCES project. J Intern Med 281:300–310
Penrod JD, Litke A, Hawkes WG, Magaziner J, Doucette JT, Koval KJ, Silberzweig SB, Egol KA, Siu AL (2008) The association of race, gender, and comorbidity with mortality and function after hip fracture. J Gerontol A Biol Sci Med Sci 63:867–872
Lo JC, Srinivasan S, Chandra M, Patton M, Budayr A, Liu LH, Lau G, Grimsrud CD (2015) Trends in mortality following hip fracture in older women. Am J Manag Care 21:e206-214
Sullivan KJ, Husak LE, Altebarmakian M, Brox WT (2016) Demographic factors in hip fracture incidence and mortality rates in California, 2000–2011. J Orthop Surg Res 11:4
United States Census Bureau QuickFacts Hawaii. www.census.gov/quickfacts/HI Accessed 12/10 2023
State of Hawaii, Department of Business, Economic Development and Tourism The Elderly Population in Hawaii: Current Living Circumstances and Housing Options. https://files.hawaii.gov/dbedt/economic/reports/Elderly_Population_in_Hawaii-Housing_Dec2021.pdf
Health HP Hawaii Pacific Health-About Us. https://www.hawaiipacifichealth.org/media/16017/hawaii-pacific-health-at-a-glance.pdf Accessed 1/21 2023
Doyle DJ, Hendrix JM, Garmon EH (2024) American Society of Anesthesiologists Classification. StatPearls. Treasure Island (FL). https://www.ncbi.nlm.nih.gov/books/NBK441940/
Kilinc G, Karakus O, Gurer B (2023) The role of ASA score and Charlson comorbidity index in predicting in-hospital mortality in geriatric hip fracture patients. Eur Rev Med Pharmacol Sci 27:7065–7072
Ringdal KG, Skaga NO, Steen PA, Hestnes M, Laake P, Jones JM, Lossius HM (2013) Classification of comorbidity in trauma: the reliability of pre-injury ASA physical status classification. Injury 44:29–35
Meyer A, Prasad KG, Antisdel J (2014) Mycobacterium chelonae dacryocystitis after endoscopic dacryocystorhinostomy. Allergy Rhinol (Providence) 5:87–90
Andrews RM (2015) Statewide hospital discharge data: collection, use, limitations, and improvements. Health Serv Res 50(Suppl 1):1273–1299
Sentell T, Unick GJ, Ahn HJ, Braun KL, Miyamura J, Shumway M (2013) Illness severity and psychiatric hospitalization rates among Asian Americans and Pacific Islanders. Psychiatr Serv 64:1095–1102
Sentell TL, Valcour N, Ahn HJ, Miyamura J, Nakamoto B, Chow D, Masaki K, Seto TB, Chen JJ, Shikuma C (2015) High rates of Native Hawaiian and older Japanese adults hospitalized with dementia in Hawai’i. J Am Geriatr Soc 63:158–164
Tokunaga DS, Siu AM, Lim SY (2022) Nontuberculous mycobacterial skin and soft tissue infection in Hawai’i. BMC Infect Dis 22:360
Chang C, Siu A, Kimata C, Sawada H, Mak VP, Lim SY (2024) Gout in Native Hawaiian patients in Hawai’i: clinical characteristics and disparities. Arthritis Care Res (Hoboken) 76(5):712–719. https://pubmed.ncbi.nlm.nih.gov/38163751/#:~:text=Native%20Hawaiians%20patients%20with%20gout,rates%20of%20rheumatology%20specialty%20care
R Core Team (2022) A language and environment for statistical computing. R Foundation for Statistical Computing. https://www.R-project.org/
Hori K, Siu AM, Nguyen ET, Andrews SN, Choi SY, Ahn HJ, Nakasone CK, Lim SY (2020) Osteoporotic hip fracture mortality and associated factors in Hawai’i. Arch Osteoporos 15:183
Schnell S, Friedman SM, Mendelson DA, Bingham KW, Kates SL (2010) The 1-year mortality of patients treated in a hip fracture program for elders. Geriatr Orthop Surg Rehabil 1:6–14
Lisk R, Yeong K (2014) Reducing mortality from hip fractures: a systematic quality improvement programme. BMJ Qual Improv Rep 3(1):u205006.w2103. https://doi.org/10.1136/bmjquality.u205006.w2103, https://pubmed.ncbi.nlm.nih.gov/27493729/
Mokuau; N, Deleon; PH, Kaholokula; JK, Soares; S, Tsark; JU, Haia C (2016) Challenges and promise of health equity for Native Hawaiians. https://nam.edu/challenges-and-promise-of-health-equity-for-native-hawaiians/
Cauley JA, Nelson DA (2013) Chapter 26 - race, ethnicity, and osteoporosis. In: Marcus R, Feldman D, Dempster DW, Luckey M, Cauley JA (eds) Osteoporosis, 4th edn. Academic Press, San Diego, pp 605–622
Morisako AK, Tauali’i M, Ambrose AJH, Withy K (2017) Beyond the ability to pay: the health status of Native Hawaiians and other Pacific Islanders in Relationship to health insurance. Hawaii J Med Public Health 76:36–41
LeBlanc KE, Muncie HL Jr, LeBlanc LL (2014) Hip fracture: diagnosis, treatment, and secondary prevention. Am Fam Physician 89:945–951
Yong EL, Ganesan G, Kramer MS, Howe TS, Koh JSB, Thu WP, Logan S, Cauley JA, Tan KB (2020) Risk factors and trends associated with mortality among adults with hip fracture in Singapore. JAMA Netw Open 3:e1919706
Kannegaard PN, van der Mark S, Eiken P, Abrahamsen B (2010) Excess mortality in men compared with women following a hip fracture. National analysis of comedications, comorbidity and survival. Age Ageing 39:203–209
Wehren LE, Hawkes WG, Orwig DL, Hebel JR, Zimmerman SI, Magaziner J (2003) Gender differences in mortality after hip fracture: the role of infection. J Bone Mineral Res 18:2231–2237
Kristensen PK, Johnsen SP, Mor A, Thillemann TM, Pedersen AB (2017) Is the higher mortality among men with hip fracture explained by sex-related differences in quality of in-hospital care? A population-based cohort study. Age Ageing 46:193–199
Lennon H, Sperrin M, Badrick E, Renehan AG (2016) The obesity paradox in cancer: a review. Curr Oncol Rep 18:56
Li J, Li D, Wang X, Zhang L (2022) The impact of body mass index on mortality rates of hip fracture patients: a systematic review and meta-analysis. Osteoporos Int 33:1859–1869
Prieto-Alhambra D, Premaor MO, Aviles FF, Castro AS, Javaid MK, Nogues X, Arden NK, Cooper C, Compston JE, Diez-Perez A (2014) Relationship between mortality and BMI after fracture: a population-based study of men and women aged >/=40 years. J Bone Mineral Res 29:1737–1744
Sheehan KJ, O’Connell MD, Cunningham C, Crosby L, Kenny RA (2013) The relationship between increased body mass index and frailty on falls in community dwelling older adults. BMC Geriatr 13:132
Stephens JR, Caraccio D, Mabry DR, Stepanek KV, Jones MS, Hemsey DF (1995) Moore CR (2021) Implementation of a fracture liaison service for patients with hip fracture cared for on a hospital medicine service. Hosp Pract 49:41–46
Ek S, Meyer AC, Hedstrom M, Modig K (2022) Comorbidity and the association with 1-year mortality in hip fracture patients: can the ASA score and the Charlson Comorbidity Index be used interchangeably? Aging Clin Exp Res 34:129–136
Li G, Walco JP, Mueller DA, Wanderer JP, Freundlich RE (2021) Reliability of the ASA physical status classification system in predicting surgical morbidity: a retrospective analysis. J Med Syst 45:83
Whitmore RG, Stephen JH, Vernick C, Campbell PG, Yadla S, Ghobrial GM, Maltenfort MG, Ratliff JK (2014) ASA grade and Charlson comorbidity index of spinal surgery patients: correlation with complications and societal costs. Spine J 14:31–38
Acknowledgements
This project was supported by the Office of the Dean through the Barry & Virginia Weinman Endowment. MM and HJA are partially supported by Ola Hawaii (2U54MD007601-36) and the Center for Pacific Innovations, Knowledge, and Opportunities (PIKO; U54GM138062) funded by the National Institute of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Taylor, L., Matsunaga, M., Ahn, H.J. et al. Risk factors associated with 1-year mortality after osteoporotic hip fracture in Hawaiʻi: higher mortality risk among Native Hawaiians and other Pacific Islanders. Osteoporos Int (2024). https://doi.org/10.1007/s00198-024-07195-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00198-024-07195-1