Abstract
Summary
The leading causes of mortality in our study were pneumonia, diseases of the circulatory system, and dementias. In patients with hip fractures, the emphasis should be placed not only on measures to prevent falls and osteoporosis, but also on preventing functional decline and pneumonia.
Purpose
To describe the specific causes of death in patients who died up to 2 years after sustaining a hip fracture, how many of those deaths were directly related to the hip fracture, and the risk factors for mortality.
Methods
A retrospective review of the clinical data of all patients admitted with hip fractures between December 2009 and September 2015. Cause of death was classified according to the International Statistical Classification of Diseases and Related Health Problems (ICD10)
Results
In the first 2 years after hip fracture, 911 patients (32.7%) died. The leading causes of mortality were pneumonia 177 (19.4%), diseases of the circulatory system 146 (16%), and dementias 126 (13.9%). Thirty patients (3.2%) died from causes directly related to hip fracture or surgery. Mortality risk factors with a higher relative risk were advanced age, male sex, higher comorbidity, delirium, and medical complications during admission.
Conclusions
Pneumonia and circulatory system diseases were the commonest causes of death in our study. In patients with hip fractures, emphasis should be placed on preventing functional decline and pneumonia. In a few patients, death was directly related to the hip fracture, although decompensation of chronic illness as a result of hip fracture and fracture-related functional decline may have been indirect causes. Patients with worse conditions at admission had the highest risk of mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hip fracture is a serious complication of falls and osteoporosis, both of which are common in older adults. It is well-known that mortality after a hip fracture is very high compared with the general population. In patients over 65 years, it is around 20% in the first year post-discharge [1] and many authors believe that excess mortality remains high for a very long time [2, 3]. Nevertheless, there is little information in the literature about the causes of late death during and after discharge from hospital. Since the number of hip fractures is expected to increase in the coming years, it is important to find out more about specific causes of death and whether some can be prevented. Some studies have found that the most common causes of death following a hip fracture are infections, especially pneumonia, and cardiovascular diseases [2, 4,5,6].
Many authors worldwide have found that advanced age, male sex, high comorbidity, living in a nursing home, and complications during admission are predisposing factors for mortality [7, 8]. The aims of our study were firstly to describe the specific causes of death of patients who died within 2 years of sustaining a hip fracture in our environment and how many deaths could have been directly related to hip fracture or surgery, and then to check whether they were the same causes found in studies carried out in other countries. Secondly, in all patients admitted for hip fractures, to analyze the differences between survivors and non-survivors and identify the risk factors for mortality. In both analyses, causes of mortality and mortality risk factors that could have been prevented were specifically looked for.
Patients and methods
Setting
The study was conducted in the Orthopaedic Surgery department in a tertiary university hospital serving a population of about 425,000 people in Barcelona, Spain.
Subjects
The clinical data of all patients admitted to the Orthopaedic Surgery Unit with hip fractures between December 2009 and September 2015 were retrospectively reviewed. Patients with hip fractures due to accidents or neoplasm were excluded. The search included the cause of death of patients who died during the first 2 years after a hip fracture. The study was approved by the institutional ethics committee.
Data collection
The following data were collected: age, sex, comorbidity measured by the Charlson index [9], the Barthel Index of Activities of Daily Living (ADL) [10], place of residence, number of drugs before admission, length of hospital stay, delay to surgery, and type of fracture. Hemoglobin and albumin levels at admission were recorded. Medical complications, final discharge destination (home, nursing home or inpatient rehabilitation facility), and cause of in-hospital mortality were also recorded. Mortality at 30 days, 1 year, 2 years, and specific causes of death were collected. Patient data not included in the electronic medical record was considered as non-localized. If the date of the patient’s death was found but not the cause, cause of death was considered as not recorded.
Cause of death was considered to be the disease leading to death, based on a complete review of medical history data and information on the patient’s clinical course and death. We considered only the primary cause of death, and whenever there was any doubt, it was resolved by discussion between the manuscript authors. Cause of death was classified according to the International Statistical Classification of Diseases and Related Health Problems (ICD10 version 2016) [11], which is published by the World Health Organization (WHO) and used to codify and classify causes of death.
Aspiration pneumonia was considered when it was noted on the medical record. When aspiration pneumonia occurred in a patient with dysphagia due to a severe degenerative neurological disease, cause of death was considered to be the latter. Patients who died after a period of progressive general physical deterioration were classified in the group of symptoms, signs, and abnormal clinical and laboratory findings not classified elsewhere whose general symptoms and signs are functional decline (code R50-R69).
As causes of death directly related to hip fracture, we considered those arising from the surgery itself: complications (hemorrhagic and infections) as well as pulmonary embolism, which has long been known to be a fracture-related cause of death [12]. Causes considered to be directly related to the fracture were: “haemorrhage and haematoma complicating surgery” (code T81.0), “infection following surgery” (code T81.4), and “pulmonary embolism” (code I 26) within the first 30 days after surgery.
Hip fracture pathway
Our hospital has an established hip fracture pathway. During admission, all patients received low molecular weight heparin prophylaxis, which was maintained for at least 30 days after surgery. Prior to surgery, antibiotic prophylaxis was given in accordance with hospital protocols. No patient underwent surgery in the 3 days after discontinuing clopidogrel or other platelet antiaggregants, and received only acetylsalicylic acid at a daily dose of 100 mg. Platelets were transfused prior to surgery if the platelet count was below 80,000. Blood was transfused when the haemoglobin level was below 80 g/L or there was haemodynamic instability. Management of anticoagulant treatments before and after surgery was as established in hospital protocols. At discharge, all patients were advised to take a vitamin D supplement and specific anti-osteoporosis treatment, except those who were not required to receive it due to their illnesses. During admission, patients were visited at least once by a doctor from the Geriatric Unit for geriatric assessment, in accordance with the framework of co-operation developed between the two departments with respect to hip fractures.
Statistical analysis
Continuous variables were analyzed by calculating means and ranges, then compared using the Student’s t test with Welch’s correction. For categorical variables, absolute numbers, relative frequencies, or proportions were calculated and compared using the Fisher’s exact test. Multivariate Cox regression analysis (proportional hazards model) was performed to establish independent variables for mortality in the first two years after sustaining a hip fracture. Categorical variables were dichotomous. Statistical analysis was performed using the IBM SPSS Statistical Package (version 22) (SPSS Inc., Chicago, IL, USA). Statistical significance was p ≤ 0.05 in all cases.
Results
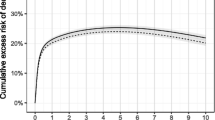
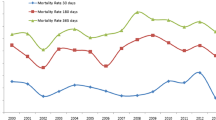
Between December 2009 and September 2015, 2909 patients were admitted to hospital with a hip fracture. Complete data was obtained for 2788 (95.8%) patients 2 years after the hip fracture. Data was not available from all patients, since some were tourists and others lacked data in the outpatient electronic medical record (Fig. 1). Cumulative mortality was 115 (4%) patients during admission, 207 (7.3%) at 30 days, 656 (23.2%) at 1 year, and 911 (32.7%) at 2 years. Median time to death was 175 days (interquartile range 39–419). Specific causes of death occurring within 2 years of a hip fracture are grouped and listed in descending order of frequency in Tables 1, 2, 3, and 4. Thirty patients (3.2%) died from causes directly related to hip fractures or surgery (Table 5).
The characteristics of surviving and non-surviving patients at 2 years were also compared. Their baseline characteristics at admission and in-hospital outcomes are shown in Table 6. All statistically significant variables included in the multivariate Cox regression analysis were the same as those that were statistically significant in the comparison of survivors and non-survivors: age, sex, place of residence, Barthel and Charlson indexes, number of drugs, length of hospital stay, delay to surgery, hemoglobin and albumin at admission, blood transfusion, delirium, medical and traumatological complications, and inpatient rehabilitation facility (Table 7). Reference group for categorical variables is male sex, presence of delirium, and presence of complications. The hip fracture pathway was followed in all patients.
Discussion
In our study, the most common causes of death in the first 2 years after a hip fracture were: diseases of the respiratory system, diseases of the circulatory system and dementias, which are very similar to those mentioned in studies conducted in other countries. In a study by Panula et al. [4] conducted in Finland, with a mean follow-up of 3.7 years after hip fracture, the most common causes of mortality were the same, with the leading one being circulatory diseases. In another study with a 2-year follow-up, Wehren et al. [6] found that the increase in mortality in patients with hip fractures relative to the general population was mainly due to septicaemia and pneumonia.
The findings of our study suggest that the causes of death after a hip fracture can be divided into two broad types: those that might have had aspects that were preventable and those that did not. Similarly, some risk factors for mortality may also have had preventable aspects. Diseases such as advanced or terminal stage cancer and neurodegenerative diseases do not, at this stage, seem to offer preventable aspects, and the hip fracture in question was probably the result of a weakened condition and sarcopenia due to the underlying disease.
With respect to causes of death considered to be directly related to hip fracture, the total number was small and would appear to be difficult to prevent, since all measures to minimize the risk of infection and bleeding were carried out correctly. We considered pulmonary thromboembolism to be a fracture-related cause in the first 30 days after surgery, following a study by McNamara et al. [13]. Eighty-five percent of events occurred within 5 weeks of the fracture, and the duration of low molecular weight heparin prophylaxis recommended by clinical practice guidelines varied between 28 and 35 days [14].
In the group of patients with organ failure such as chronic heart failure, COPD, or cirrhosis, decompensated primary disease because of the hip fracture should be ruled out in the patient, either during admission or after discharge, before deciding whether any of these offsets are preventable. Admission also provides an opportunity to check whether the pharmacological and non-pharmacological treatment is correct and whether compliance is appropriate.
We found two major causes of death with possible preventable aspects: pneumonia and functional decline.
Pneumonia was the leading cause of death in our study. We divided pneumonia into those with bacterial causes and those caused by aspiration, since the measures to prevent them differ in some respects. Pneumonia was the fourth most common reason for hospitalization and the sixth leading cause of death in older adults in our environment. In bacterial pneumonia, measures that have been shown to be effective for prevention include proper oral hygiene, stopping smoking, an annual flu vaccination and pneumococcal vaccination [15]. In 2018, a trial demonstrated that the incidence of pneumonia was lower in elderly patients with hip fractures who followed the postoperative pulmonary rehabilitation program after surgery [16]. Aspiration pneumonia is defined as pneumonia with previous aspiration factors and suspected or proven aspiration [17]. Here we highlight the fact that a significant proportion of the pneumonias that we found was probably caused by aspiration, and these alone accounted for almost 7% of total mortality. Two papers in Japan also found that a high number of pneumonias occurring during admission with hip fractures were due to aspiration [18, 19]. Some of the main risks for aspiration pneumonia are oral dysphagia and a vulnerable status with frailty and comorbidity, conditions that apply to most patients with fractured hips. Based on these data, recommendations that could be made to prevent aspiration pneumonia include correction of posture for swallowing, prevention of gastroesophageal reflux, and actively looking for dysphagia in hospitalized and discharged patients, since this condition continues to be underdiagnosed and untreated [20].
We think that the group of patients that we classified as “General symptoms and signs,” in which death is not well defined and occurs after a period of functional decline, may already have been in the end-of-life phase of functional decline and the hip fracture was a possible complication related either to the trajectory of dying or to the beginning of functional decline. Whatever the case, an effort should be made to identify patients who do not recover in the first few weeks or are afraid of falling in order to intensify physiotherapy to prevent immobility syndrome and its consequences.
In our study, patients who died in the first 2 years after a hip fracture were older, male, had higher comorbidity scores, and more medical complications throughout hospitalization, including delirium. It seems reasonable to consider that patients with hip fractures and worse conditions are those at highest risk of mortality. A higher Barthel index and haemoglobin and albumin at admission appear to be statistically significant protective factors, although the association is small. Most risk factors are not modifiable, although some aspects could be addressed: Hypoalbuminemia on admission may be an indicator of malnutrition, which is very prevalent in hip fracture. Nutritional intervention is cost effective in functional recovery and nutritional status [21]. In a retrospective study, Sheikh et al. also found that haemoglobin below 10 g/dL was a predictor of mortality [22]; it would be necessary therefore to find out whether anaemia is caused by the fracture or reflects the presence of other chronic diseases. The need for blood transfusion is associated with factors other than haemoglobin at admission: female sex, fracture type, and fixation method [23].
Marcantonio et al. have already reported that delirium on admission is associated with poor functional recovery and increased mortality, [24] and other authors such Martocchia et al. [25] and Shields et al. [26] demonstrated that delirium can be reduced in patients admitted for hip fractures by carrying out a comprehensive geriatric assessment and ensuring close collaboration between the orthopaedic and geriatric teams.
The main strengths of our study are as follows: [1] we not only looked at the patients’ cause of death, but emphasized preventable aspects; 2) the study was conducted in our environment and is, to our knowledge, the only one to consider specific causes of death following hip fracture in our country; [3] most studies of causes of death are based on death certificates [4,5,6, 27]. In this study, we chose to collect data from medical records, and cause of death was established after a complete review, which provided more information. The main limitation of our study is that it is a retrospective, unicentric study. Another limitation is that we were unable to track down all patients after discharge, and in almost 10% of patients, cause of death was not recorded. Furthermore, it was not always easy to clarify the ultimate cause of a patient’s death using the data in the medical history, since some patients had more than one comorbidity, which other authors have also mentioned [4].
Conclusions
Diseases of the respiratory system, especially pneumonia, and circulatory system diseases, were the most common causes of death in our study. In patients with hip fractures, the emphasis should be placed not only on measures that prevent falls and osteoporosis, but also on prevention of functional decline and pneumonia. Dysphagia should be actively looked for in hospitalized patients and after discharge to avoid aspiration pneumonia. We found few patients whose cause of death was directly related to the hip fracture, although decompensation of chronic illnesses occurring after hip fractures and fracture-related functional decline may be indirect causes. Risk factors for mortality with a higher relative risk were advanced age, male sex, higher comorbidity, delirium, and medical complications during admission.
Change history
04 March 2021
A Correction to this paper has been published: https://doi.org/10.1007/s11657-021-00912-x
References
Schnell S, Friedman SM, Mendelson DA, Bingham KW, Kates SL (2010) The 1-year mortality of patients treated in a hip fracture program for elders. Geriatr Orthop Surg Rehabil 1(1):6–14. https://doi.org/10.1177/2151458510378105
Von Friesendorff M, Mc Guigan FE, Wizert A et al (2016) Hip fracture, mortality risk, and cause of death over two decades. Osteop Int 27(10):2945–2953. https://doi.org/10.1007/s00198-016-3616-5
Haentjens P, Magaziner J, Colón-Emeric CS et al (2010) Metaanalysis: excess mortality after hip fracture among older women and men. Ann Intern Med 152(6):380–390. https://doi.org/10.7326/0003-4819-152-6-201003160-00008
Panula J, Pihlajamäki H, Mattila V et al (2011) Mortality and cause of death in hip fracture patients aged 65 or older – a population-based study. BMC Muskuloskelet Disord 12:105. https://doi.org/10.1186/1471-2474-12-105
Gonzalez-Montalvo JI, Alarcon T, Hormigo Sanchez AI (2011) ¿Por qué fallecen los pacientes con fractura de cadera? Med Clin (Barc) 137(8):355–360. https://doi.org/10.1016/j.medcli.2010.07.005
Wehren LE, Hawkes WG, Orwig DL, Hebel R, Zimmerman SI, Magaziner J (2003) Gender differences in mortality after hip fracture: the role of infection. J Bone Miner Res 18(12):2231–2237. https://doi.org/10.1359/jbmr.2003.18.12.2231
Chatterton BD, Moores TS, Ahmad S, Cattell A, Roberts PJ (2015) Cause of death and factors associated with early in-hospital mortality after hip fracture. Bone Joint J 97-B(2):246–251. https://doi.org/10.1302/0301-620X.97B2.35248
Muraki S, Yamamoto S, Ishibashi H, Nakamura K (2006) Factors associated with mortality following hip fracture in Japan. J Bone Miner Metab 24(2):100–104. https://doi.org/10.1007/s00774-005-0654-z
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 40(5):373–383
Mahoney F, Barthel D (1965) Functional evaluation: the Barthel Index. Md Med J. 14:61–65
Wordl Health Organisation (1992) The International Statistical Classification of Diseases and Related Health Problems, Tenth Revision. WHO, Geneva
Perez J, Warwick DJ, Case CP, Bannister GC (1995) Death after proximal femoral fracture—an autopsy study. Injury. 26(4):237–240. https://doi.org/10.1016/0020-1383(95)90008-I
McNamara I, Sharma A, Prevost T, Parker M (2009) Symptomatic venous thromboembolism following a hip fracture. Acta Orthop 80(6):687–692. https://doi.org/10.3109/17453670903448273
Shin WC, Lee SM, Suh KT (2017) Recent updates of the diagnosis and prevention of venous thromboembolism in patients with a hip fracture. Hip pelvis 29(3):159–167. https://doi.org/10.5371/hp.2017.29.3.159
Torres OH, Gil E, Pacho C, Ruiz D (2013) Actualización de la neumonía en el anciano. Rev Esp Geriatr Gerontol. 48(2):72–78. https://doi.org/10.1016/j.regg.2012.06.001
Chang SC, Lai JI, Lu MC, Lin KH, Wang WS, Lo SS, Lai YC (2018) Reduction in the incidence of pneumonia in elderly patients after hip fracture surgery: An inpatient pulmonary rehabilitation program. Medicine. 97(33):e11845. https://doi.org/10.1097/MD.0000000000011845
Shariatzadeh MR, Huang JQ, Marrie TJ (2006) Differences in the features of aspiration pneumonia according to site of acquisition: community or continuing care facility. J Am Geriatr Soc. 54:296–302. https://doi.org/10.1111/j.1532-5415.2005.00608.x
Metani H, Tsubahara A, Hiraoka T, Seki S, Hasegawa T (2015) Risk factor for patients who develop pneumonia either before or after hip fracture surgery. Jpn J Compr Rehabil Sci 6:43–49. https://doi.org/10.11336/jjcrs.6.43
Teramoto S, Fukuchi Y, Sasaki H, Sato K, Sekizawa K, Matsuse T (2008) High incidence of aspiration pneumonia in community-and hospital-acquired pneumonia in hospitalized patients: a multicenter, prospective study in Japan. J Am Geriatr Soc. 56(3):577–579. https://doi.org/10.1111/j.1532-5415.2008.01597.x
Baijens LWJ, Clave P, Cras P et al (2016) European Society for Swallowing Disorders- European Union Geriatric Medicine Society white paper: oropharyngeal dysphagia as a geriàtric syndrome. Clin Interv Aging 11:1403–1428. https://doi.org/10.2147/CIA.S107750
Malafarina V, Reginster JY, Cabrerizo S et al (2018) Nutritional Status and Nutritional Treatment Are Related to Outcomes and Mortality in Older Adults with Hip Fracture. Nutrients 10(5):555. Published 2018 Apr 30. https://doi.org/10.3390/nu10050555
Sheik HQ, Hossain FS, Aqil A, Akinbamijo B, Mushtaq V, Kapoor H (2017) A comprehensive analysis of the causes and predictors of 30-day mortality following hip fracture surgery. Clin Orthop Surg 9(1):10–18. https://doi.org/10.4055/cios.2017.9.1.10
Desai SJ, Wood KS, Marsh J, Bryant D, Abdo H, Lawendy AR, Sanders DW. (2014) Factors affecting transfusion requirement after hip fracture: can we reduce the need for blood? Can J Surg 2014, 57(5): 342–348. https://doi.org/10.1503/cjs.030413
Marcantonio ER, Flacker JM, Michaels M, Resnick NM (2000) Delirium is independently associated with poor functional recovery alter hip fracture. J Am Geriatr Soc. 48(6):618–624. https://doi.org/10.1111/j.1532-5415.2000.tb04718.x
Martocchia A, Curto M, Comite F et al (2015) Orthogeriatric Group. Recent Pat CNS Drug Discov. 10(1):55–64. https://doi.org/10.2174/1574889810666150216152624.
Shields L, Henderson V, Caslake R (2017) Comprehensive geriatric assessment for prevention of delirium after hip fracture: a systematic review of randomized controlled trials. J Am Geriatr Soc 65(7):1559–1565. https://doi.org/10.1111/jgs.14846
Cameron ID, Chen JS, March LM et al (2010) Hip fracture causes excess mortality owing to cardiovascular and infectious disease in institutionalized older people: a prospective 5-year study. J Bone Miner Res 4:866–872. https://doi.org/10.1359/jbmr.091029
Acknowledgments
We would like to thank Janet Gaynor Dawson for her help with the English in this paper and Ignasi Gich for his statistical assessment.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Ethical approval
The study was approved by the institutional ethics committee (IIBSP-FEM-2018-18). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent is not required
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Barceló, M., Torres, O.H., Mascaró, J. et al. Hip fracture and mortality: study of specific causes of death and risk factors. Arch Osteoporos 16, 15 (2021). https://doi.org/10.1007/s11657-020-00873-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-020-00873-7