Abstract
Summary
Systematic review and meta-analysis of the effect of moderate- to high-dose vitamin D supplementation in pregnancy on offspring bone mineralisation found a positive effect of vitamin D supplementation on offspring bone mineral density (BMD) at age 4–6 years, with a smaller effect on bone mineral content.
Purpose
A systematic review and meta-analysis was performed to assess the effect of pregnancy vitamin D supplementation on offspring bone mineral density (BMD) in childhood.
Methods
A literature search was conducted for published RCTs of antenatal vitamin D supplementation with assessment of offspring BMD or bone mineral content (BMC) by dual-energy X-ray absorptiometry (DXA) using MEDLINE and EMBASE up to 13th July 2022. Risk of bias was assessed using the Cochrane Risk of Bias 2 tool. Study findings were grouped in two age groups of offspring assessment: neonatal period and early childhood (3–6 years). Random-effects meta-analysis of the effect on BMC/BMD at 3–6 years was performed using RevMan 5.4.1, yielding standardised mean difference (SMD) (95% CI).
Results
Five RCTs were identified with offspring assessment of BMD or BMC; 3250 women were randomised within these studies. Risk of bias was low in 2 studies and “of concern” in 3. Supplementation regimes and the control used (3 studies used placebo and 2 used 400 IU/day cholecalciferol) varied, but in all studies the intervention increased maternal 25-hydroxvitamin D status compared to the control group. Two trials assessing BMD in the neonatal period (total n = 690) found no difference between groups, but meta-analysis was not performed as one trial represented 96.4% of those studied at this age. Three trials assessed offspring whole-body-less-head BMD at age 4–6 years. BMD was higher in children born to mothers supplemented with vitamin D [0.16 SD (95% confidence interval 0.05, 0.27), n = 1358] with a smaller effect on BMC [0.07 SD (95% CI − 0.04, 0.19), n = 1351].
Conclusions
There are few RCTs published to address this question, and these are inconsistent in methodology and findings. However, meta-analysis of three trials suggests moderate- to high-dose vitamin D supplementation in pregnancy might increase offspring BMD in early childhood, but further trials are required to confirm this finding. (Prospero CRD42021288682; no funding received).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vitamin D supplementation in pregnancy has been shown to reduce the risk of symptomatic neonatal hypocalcaemia, but there is also much interest in other potential benefits of this gestational intervention for obstetric and offspring health [1]. Given the importance of vitamin D repletion for skeletal health, a role for in utero vitamin D exposure in offspring skeletal development has been suggested. Some observational mother–offspring cohort studies have shown positive associations between maternal serum 25-hydroxyvitamin D [25(OH)D] status in pregnancy and offspring bone mineral density (BMD) in the neonatal period [2, 3], childhood [4,5,6] and through to peak bone mass [7]; however, these findings are not consistent across all cohorts [8, 9]. Several randomised controlled trials (RCT) assessing the effect of antenatal vitamin D supplementation on offspring BMD have been undertaken. We therefore performed a systematic review and meta-analysis to describe the current available literature and facilitate the best estimate of the association between antenatal vitamin D supplementation and offspring BMD.
Methods
The study protocol was registered in PROSPERO (www.crd.york.ac.uk/PROSPERO) on 2nd November 2021 (CRD42021288682), and the review and meta-analysis were undertaken in accordance with guidelines from PRISMA [10]. A literature search was undertaken to identify RCTs of vitamin D supplementation in pregnant women with offspring assessment of BMD or bone mineral content (BMC). The intervention studied was vitamin D during pregnancy either as cholecalciferol (vitamin D3) or ergocalciferol (vitamin D2). All vitamin D supplementation regimes were included, including daily, weekly and single high-dose supplementation. Trials of vitamin D and calcium co-supplementation were excluded unless all treatment groups received the same calcium supplementation. Food fortification studies were also excluded. Studies in which the vitamin D supplementation continued according to maternal randomisation group in the offspring postnatally or in which there was secondary postnatal randomisation of the infant to vitamin D supplementation were also excluded as pre- and post-natal supplementation could have differing effects. We included studies with control groups using placebo, no treatment and low-dose (≤ 400 IU/day) vitamin D. Low-dose vitamin D was included as a potential control group as this is currently standard care for pregnancy in many developed countries [11]. The study outcomes considered were dual-energy x-ray absorptiometry (DXA) assessment of BMD or BMC in the offspring. Assessment of BMD by other methods including single photon absorptiometry (SPA), radiographic density and quantitative ultrasonography (QUS) was not included, as these techniques are not reliable for assessment of bone mineralisation in this age group [12].
Search strategy and study selection
The literature search was initially conducted on 30th November 2021 and subsequently updated on 13th July 2022. MEDLINE and EMBASE was searched from conception via OvidSP using the search terms (“vitamin D” OR cholecalciferol OR colecalciferol OR ergocalciferol).af AND (Pregnan* OR Antenat* OR Gestation*).af AND (bone).af. Two authors (RJM and HDG) independently screened the titles and abstracts to identify full texts for review, and assessed these for inclusion. Disagreements were resolved through discussion. The reference lists of relevant reviews were additionally scanned for any additional applicable studies. We included only full reports that had been published in peer-reviewed journals. Conference abstracts without full publication of data were therefore excluded. Data for maternal 25(OH)D status and offspring BMD and BMC were extracted independently by two authors (RJM and HDG) and disagreements resolved by discussion. Results were tabulated into an excel spreadsheet for synthesis.
Risk of bias
Two authors (RJM and HDG) independently assessed risk of bias using the Risk of Bias 2.0 tool (www.riskofbias.info) [13].
Data analysis
All 25(OH)D data was converted to measurements in nanomoles/l using a conversion factor of 2.5 from nanograms/litre.
Data for bone outcomes were extracted from the papers as mean, standard deviation (SD) or standard error and number of participants (n) and entered into RevMan5.4. Where SD was not available, this was calculated using SE and n using the calculator within RevMan5.4. for further analysis. Forest plots were used as graphical representation of the results of the meta-analysis and showed standardised mean (SD) for neonatal whole-body BMD and BMC and childhood whole-body-less-head (WBLH) BMD and BMC. WBLH data were used as this is the recommended site for assessment of BMD in childhood due to the large contribution of the skull which responds to stimuli differently to the remainder of the skeleton [14, 15]. As the data were derived from randomised controlled trials, random allocation of potential confounders could be assumed, so only unadjusted data were included in the meta-analysis. One study included follow-up of the offspring at both 3 and 6 years of age [16], and therefore the meta-analysis was performed twice using each set of data. For studies that included multiple arms of vitamin D supplementation at different doses, the findings for all doses were combined into a single group to include in the meta-analysis [17, 18]. The heterogeneity of the studies included in the meta-analysis was assessed using the I2, chi-squared test and Tau2. Random-effects meta-analysis was used due to differences in study methodology and standardised mean difference is reported to account for the difference in age at follow-up.
Results
The literature search revealed 2338 records after deduplication. After title and abstract screening, nine reports were eligible for full review [16, 19,20,21,22,23,24,25,26]. Three reports were subsequently excluded: one study assessed offspring BMD by SPA and included supplementation with an unknown amount of calcium in addition to vitamin D [26], one assessed only bone turnover markers and not BMC/BMD [25] and the third re-analysed the data included in another publication with stratification by postnatal vitamin D status [21]. Finally, the search identified 5 RCTs; one reported bone outcomes at two ages in separate reports; thus, there were 6 published reports for data extraction [16, 19, 20, 22,23,24] (Fig. 1).
Study characteristics
The characteristics of the included studies are presented in Table 1. The protocols for 4 of the studies had been reviewed by an research ethics review board [16, 19, 20, 23, 24]; the study of Sahoo et al. did not report ethical review but had been registered in a clinical trials registry [22]. Two trials reported assessment of offspring BMD in the neonatal period [20, 23], one in infancy [22] and three in early childhood (ages 3–6 years) [16, 19, 24]. No trials assessed the effect of pregnancy vitamin D supplementation on offspring BMD after the age of 6 years. The number of offspring with BMD assessed by DXA in each trial varied between 25 and 665. The RCTs were conducted in both high- [16, 19, 20] and low-/middle-income countries [22,23,24]. All the RCTs were conducted in a double-blind manner and used oral cholecalciferol as the investigational medicinal product (IMP); daily supplementation (doses 1000–2400 IU/day) was assessed in three trials [19,20,21, 23], weekly supplementation in one study [24] and four- or eight-weekly supplementation in one study [22]. Overall, the doses used were equivalent to between 600 and 4000 IU/day. Three RCTs used placebo as the control group [19, 20, 23, 24] and two trials compared to a control group receiving 400 IU/day cholecalciferol [21, 22]. The MAVIDOS and COPSAC2010 studies allowed women to continue self-supplementation with up to 400 IU/day cholecalciferol, and Vaziri et al. allowed women to continue to take prescribed supplements; thus, the exact supplemental vitamin D intake of both the control and intervention groups in these studies is unknown. Nonetheless, in all the studies, maternal 25(OH)D status in late pregnancy or at delivery was higher in the cholecalciferol group(s) than the control group for the study (Table 1). The gestation at which the vitamin D supplementation was commenced varied markedly between 11- and 28-week gestation. All studies continued supplementation until delivery. O’Callaghan et al. additionally included a group randomised to both pre- and post-natal supplementation with 28,000 IU/week. This group was excluded from consideration in this systematic review and meta-analysis.
Risk of bias
Two trials (MAVIDOS and COPSAC2010) were graded as having low risk of bias [16, 19, 20] (Table 2). The studies by O’Callaghan et al., Sahoo et al. and Vaziri et al. were all deemed “of concern” which reflected the lack of a pre-specified analysis plan [22,23,24].
The findings of the study by Sahoo et al. were however considered uninterpretable due to a significant difference in age of follow-up of the children in the three randomisation groups (detailed in Table 2), and therefore these data were not included in subsequent review and meta-analysis.
Effect of maternal vitamin D supplementation on offspring whole body BMD or BMC in the neonatal period
Two studies assessed offspring whole body BMD in the neonatal period. The UK-based MAVIDOS trial of 1000 IU/day cholecalciferol vs placebo assessed whole-body DXA in 338 neonates born to mothers randomised to cholecalciferol and 327 born to placebo-group mothers [20]. There was no difference in whole-body BMD or BMC between the two groups, although, in a pre-planned secondary analysis, there was evidence of a positive effect of the intervention amongst winter deliveries. Vaziri et al. conducted a trial of 2000 IU/day cholecalciferol vs. placebo in India. This study was deemed “of concern” for risk of bias and had only a small number of participants with DXA assessment (n = 25) and very low rates of DXA follow-up (16.3%). No difference in offspring whole-body BMD in the late neonatal period [23] was identified. As the data from MAVIDOS represented 96.4% of the total number of neonates studied, meta-analysis of data from these two studies was not performed.
Effect of maternal vitamin D supplementation on offspring whole body BMD in early childhood
Three studies assessed offspring WBLH BMD at ages 3–6 years [16, 19, 24]. In the COPSAC2010 study performed in Denmark, offspring DXA assessment was undertaken at both 3 and 6 years of age [16]; in MAVIDOS and the BONUSKids study in Bangladesh, offspring DXA was at 4 years of age [19, 24], although the exact age at DXA and comparison of age between randomisation groups in BONUSKids is not reported. In both the MAVIDOS trial (placebo vs 1000 IU/day vitamin D) and COPSAC2010 (400 IU/day vs 2400 IU/day), vitamin D supplementation resulted in higher offspring WBLH BMD at ages 4 and 6 years, respectively [16, 19]. This effect was not observed in COPSAC2010 at age 3 years in a smaller subset of children (n = 94 vit D/105 control compared with n = 187 vit D/196 control at 6 years of age). In contrast in the BonusKIDS trial in Bangladesh, which used weekly cholecalciferol supplementation with either 4200 IU, 16,800 IU or 28,000 IU compared with placebo, no effect of cholecalciferol on offspring WBLH BMD or BMC at age 4 years was identified [24].
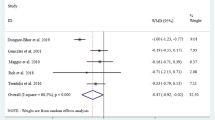
Meta-analysis of these data, including 802 children born to mothers randomised to vitamin D and 556 children born to the control-groups, showed a significant effect of maternal vitamin D supplementation on offspring BMD when the data from COPSAC2010 at age 6 years were included (SMD 0.16, 95% CI 0.05, 0.27, Fig. 2A). This was consistent but attenuated when the smaller data set at age 3 years was substituted for the 6-year data, including 720 vitamin D group children and 454 control-group children (SMD 0.11, 95% CI − 0.02, 0.23, Fig. 2B). There was a similar direction of effect for WBLH BMC, but the 95% confidence interval just bounded zero (Fig. 3A and 3B).
Data for whole body BMD and BMC and head BMD and BMC were also reported in COPSAC2010 and BONUSKids, but not in MAVIDOS. Similarly to the findings for WBLH, positive effects of supplementation were observed in COPSAC2010 at age 6 years (whole body BMD mean difference 0.009 g/cm2 (95% CI 0.001–0.017), BMC mean difference 13.9 g (95% CI 3.2–24.7); head BMD mean difference 0.033 g/cm2 (95% CI 0.010–0.057), BMC mean difference 6.1 g (95% CI 0.4–11.7)), but no effect for any of the cholecalciferol doses used compared to placebo in BONUSKids.
Discussion
Summary of main findings
There are few randomised controlled trials that have assessed the effect of pregnancy vitamin D supplementation on offspring bone mineral density, and the existing trials vary markedly in terms of the population studied and supplementation protocols used. There were only two published RCTs of the effect of pregnancy vitamin D supplementation on offspring whole body bone outcomes in the neonatal period of which one trial included only a very small number of participants. Neither study reported an effect of the intervention on offspring BMD, but meta-analysis was not undertaken due to the majority of the data being from one of the two studies. In contrast, meta-analysis of RCTs reporting offspring BMD in early childhood (ages 4–6 years) suggests that moderate- to high-dose vitamin D supplementation during pregnancy might increase offspring WBLH BMD, with a similar direction of effect for WBLH BMC. However, caution should be taken in the interpretation of this due to the differences in study population and trial design, although the two studies most similar in population (MAVIDOS and COPSAC2010) reported similar outcomes in childhood.
The differing findings for the neonatal period and early childhood may reflect statistical power, with fewer data available in the neonatal period than at age 3–4 years and 4–6 years. Similarly, this is likely to reflect the difference in the findings of the meta-analysis in early childhood when the two follow-up ages of COPSAC2010 was used. It is however possible that an evolving effect is responsible for this difference, as seen in the MAVIDOS trial, in which no significant effect on neonatal BMD was observed [20], yet at 4 years, a difference in BMD between the two randomisation groups was present [19]. Prenatal vitamin D supplementation increases breast milk vitamin D content [27], and is one potential mechanism for a stronger effect size beyond the neonatal period. Changing associations between maternal 25(OH)D status in late pregnancy and offspring adiposity have also been documented in a birth cohort study, with a positive association with fat mass at birth, no association at age 4 years and a negative association at age 6 years [28]. Associations of pregnancy 25(OH)D status with epigenetic markers [29] and differences in DNA methylation in response to supplementation [30] have been reported. Maternal 25(OH)D status in pregnancy has also been associated with metabolomic profiles in the offspring [31] in an observational study but has not yet been explored in an RCT. These may represent mechanisms by which in utero vitamin D exposure has a long-lasting and evolving effect on postnatal health outcomes.
Quality of evidence
Currently, there are only five reported RCTs of vitamin D supplementation in pregnancy to assess offspring BMD as an outcome, despite there being many trials that have assessed other outcomes, such as birth anthropometry, neonatal calcium status [32] and maternal health in pregnancy [33]. Due to the limited number of studies, we are unable to assess publication bias. Assessment of BMD was the primary trial outcome in only the MAVIDOS study [20, 34]. Risk of bias was considered “of concern” in three studies due to a lack of a pre-specified analysis plan, but this may reflect BMD being a secondary outcome. Overall, these studies all had high attrition, with follow-up between 16.3 and 61.5% (although typically higher in the studies considered low risk of concern for bias), often leading to differences in participants and non-participants where these data are reported. This high attrition is in part due to the technical challenges of obtaining DXA scans without movement artefact in the age groups studied, with substantially more children attending follow-up visits than DXA data available. For example, only 199 technically acceptable DXA scans were obtained from 517 children attending the follow-up visit at age 3 in COPSAC2010. Information on factors that may additionally affect BMD in the offspring for example current vitamin D status, physical activity and vitamin D supplement use was typically lacking. Unless allocation to pregnancy vitamin D supplementation is also influencing these outcomes (which would not be expected) and thus could represent a mechanistic pathway between pregnancy vitamin D supplementation and offspring bone mineralisation, random distribution of these factors between study arms would be expected. It is, however, not possible to completely rule out an imbalance in relevant covariates during follow-up as a result of chance. Application of the GRADE rating for evidence quality would rate the evidence for the effect of maternal vitamin D supplementation on offspring BMD as low due to the inconsistency between the reported studies and inability to assess publication bias, but currently the best possible estimate of the effect based on the available evidence is as shown in Fig. 2.
Potential bias in the review process
The authors of this systematic review and meta-analysis also authored the MAVIDOS study. However, this review was performed using pre-specified inclusion criteria. Additionally, given the authors’ familiarity with the literature on this topic and completion of a previous comprehensive systematic review of antenatal vitamin D supplementation [35], there is high certainty that all RCTs of maternal vitamin D supplementation in pregnancy assessing this outcome have been identified.
Comparison to other reviews
A previous systematic review from the current research group conducted in 2013 identified only one intervention study assessing offspring BMD as an outcome of antenatal vitamin D supplementation [35, 36], but that study has not been included in this systematic review as offspring bone mineralisation was assessed by SPA and the women randomised to vitamin D also received an unknown quantity of calcium supplementation (which was not received by the control group) [36]. All the RCTs identified in this updated systematic review were published since 2016.
O’Callaghan and the BONUSKids research team also performed meta-analysis of the MAVIDOS, COPSAC2010 and BONUSKids study findings although this was not done as part of a formal systematic review. No effect of pregnancy vitamin D supplementation on offspring WBLH BMD or BMC at ages 3–4 years was found in that meta-analysis [24]. However, only the data from the mother–offspring pairs randomised to 28,000 IU/week combined with the group randomised to 28,000 IU/week pre- and post-natal supplementation in the BONUSKids study was included. Care should be taken in using data from this pre-/post-natal supplementation arm, as differing effects of in utero and post-natal vitamin D exposure may occur [1]. Furthermore, although all the RCTs included in our meta-analysis used different doses of cholecalciferol, an increase in maternal 25(OH)D for each dose used was observed in all 5 studies in this systematic review; as a result, inclusion of the data from both the 4000 IU/week and 16,000 IU/week supplementation groups in BONUSKids in the meta-analysis is appropriate.
Implications for clinical practice and ongoing research
An overall effect of pregnancy vitamin D supplementation on offspring early childhood BMD is suggested by this meta-analysis and supports the use of higher dose vitamin D supplementation during pregnancy than is currently recommended in many developed countries [37,38,39,40]. However, the studies included differed markedly in terms of the population studied, baseline and achieved 25(OH)D status, the timing of vitamin D commencement and supplementation regimes used and therefore extrapolation of these findings should be undertaken with care. Offspring assessment of BMD should be considered in other existing RCTs of antenatal vitamin D supplementation. Increasing the available data for meta-analysis would enable stratification by population factors and cholecalciferol doses and dosing regimens and enable further understanding on whether achieved 25(OH)D, change in 25(OH)D or dose of supplementation used are important. For example, the positive effects of antenatal vitamin D supplementation on childhood BMD were observed in the two studies conducted in high-income countries on women predominantly of White ethnicity using daily supplementation [16, 19], whereas this effect was not found in the study conducted in Bangladesh using weekly supplementation [24]. This could be a chance finding in only a small number of studies, but differing response to vitamin D supplementation by ethnicity and other lifestyle factors has been reported [41]. This may in part reflect genetic clustering and distribution of single nucleotide polymorphisms in the vitamin D pathway [42], which have been associated with the response to vitamin D supplementation in pregnancy [43,44,45]. Thus, care should be taken in the translation of clinical trial findings to differing populations, and further studies in diverse populations and using multiple dosing arms to establish optimal dosing regimens would enable greater understanding. Furthermore, ongoing follow-up of the children included in these RCTs is important to demonstrate a sustained effect of this intervention through to peak bone mass and a longer-term benefit on skeletal health.
Conclusions
Although the currently available data is limited, vitamin D supplementation during pregnancy using doses higher than currently recommended in many guidelines may have a beneficial effect of offspring bone mineral density in early childhood. Further data are required in diverse population groups either through BMD assessment in offspring born into existing RCTs or in newly established trials to confirm that this effect is consistent across all populations. Long-term follow-up of these offspring to confirm persistence of this effect should also be undertaken.
References
Moon RJ, Davies JH, Cooper C, Harvey NC (2020) Vitamin D, and maternal and child health. Calcif Tissue Int 106(1):30–46
Viljakainen HT, Saarnio E, Hytinantti T, Miettinen M, Surcel H, Makitie O et al (2010) Maternal vitamin D status determines bone variables in the newborn. J Clin Endocrinol Metab 95(4):1749–1757
Weiler H, Fitzpatrick-Wong S, Veitch R, Kovacs H, Schellenberg J, McCloy U et al (2005) Vitamin D deficiency and whole-body and femur bone mass relative to weight in healthy newborns. CMAJ 172(6):757–761
Javaid MK, Crozier SR, Harvey NC, Gale CR, Dennison EM, Boucher BJ et al (2006) Maternal vitamin D status during pregnancy and childhood bone mass at age 9 years: a longitudinal study. Lancet 367(9504):36–43
Moon RJ, Harvey NC, Davies JH, Cooper C (2015) Vitamin D and bone development. Osteoporos Int 26(4):1449–1451
Viljakainen HT, Korhonen T, Hytinantti T, Laitinen EK, Andersson S, Makitie O et al (2011) Maternal vitamin D status affects bone growth in early childhood–a prospective cohort study. Osteoporos Int 22(3):883–891
Zhu K, Whitehouse AJ, Hart P, Kusel M, Mountain J, Lye S et al (2014) Maternal vitamin D status during pregnancy and bone mass in offspring at 20 years of age: a prospective cohort study. J Bone Miner Res 29(5):1088–1095
Garcia AH, Erler NS, Jaddoe VWV, Tiemeier H, van den Hooven EH, Franco OH et al (2017) 25-hydroxyvitamin D concentrations during fetal life and bone health in children aged 6 years: a population-based prospective cohort study. Lancet Diabetes Endocrinol 5(5):367–376
Lawlor DA, Wills AK, Fraser A, Sayers A, Fraser WD, Tobias JH (2013) Association of maternal vitamin D status during pregnancy with bone-mineral content in offspring: a prospective cohort study. Lancet 381(9884):2176–2183
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
National Institute for Health and Clinical Excellence. Antenatal care (NICE Clinical Guideline 62). www.guidance.nice.org.uk/cg622008.
Kalkwarf HJ, Abrams SA, DiMeglio LA, Koo WWK, Specker BL, Weiler H (2014) Bone densitometry in infants and young children: the 2013 ISCD Pediatric Official Positions. J Clin Densitom 17(2):243–257
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:l4898
Shuhart CR, Yeap SS, Anderson PA, Jankowski LG, Lewiecki EM, Morse LR et al (2019) Executive summary of the 2019 ISCD Position Development Conference on monitoring treatment, DXA cross-calibration and least significant change, spinal cord injury, peri-prosthetic and orthopedic bone health, transgender medicine, and pediatrics. J Clin Densitometry 22(4):453–71
Moon RJ, D’Angelo S, Crozier SR, Godfrey KM, Davies JH, Cooper C et al (2022) Is the skull responsive to bone mineralisation stimuli in children? Bone 160:116415
Brustad N, Garland J, Thorsen J, Sevelsted A, Krakauer M, Vinding RK et al (2020) Effect of high-dose vs standard-dose vitamin D supplementation in pregnancy on bone mineralization in offspring until age 6 years: a prespecified secondary analysis of a double-blinded, randomized clinical trial. JAMA Pediatr 174(5):419–427
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (2022) Cochrane handbook for systematic reviews of interventions version 6.3 (updated February 2022): Cochrane
Rücker G, Cates CJ, Schwarzer G (2017) Methods for including information from multi-arm trials in pairwise meta-analysis. Res Synth Methods 8(4):392–403
Curtis EM, Moon RJ, D’Angelo S, Crozier SR, Bishop NJ, Gopal-Kothandapani JS, et al (2022) Pregnancy vitamin D supplementation and childhood bone mass at age 4 years: findings from the maternal vitamin D osteoporosis study (MAVIDOS) randomized controlled trial. JBMR Plus 2022;n/a(n/a):e10651
Cooper C, Harvey NC, Bishop NJ, Kennedy S, Papageorghiou AT, Schoenmakers I et al (2016) Maternal gestational vitamin D supplementation and offspring bone health (MAVIDOS): a multicentre, double-blind, randomised placebo-controlled trial. Lancet Diabetes Endocrinol 4(5):393–402
Brustad N, Chawes BL, Thorsen J, Krakauer M, Lasky-Su J, Weiss ST et al (2022) High-dose vitamin D supplementation in pregnancy and 25(OH)D sufficiency in childhood reduce the risk of fractures and improve bone mineralization in childhood: follow-up of a randomized clinical trial. EClinicalMedicine 43:101254
Sahoo SK, Katam KK, Das V, Agarwal A, Bhatia V (2016) Maternal vitamin D supplementation in pregnancy and offspring outcomes: a double-blind randomized placebo-controlled trial. J Bone Miner Metab. https://doi.org/10.1007/s00774-016-0777-4
Vaziri F, Dabbaghmanesh MH, Samsami A, Nasiri S, Shirazi PT (2016) Vitamin D supplementation during pregnancy on infant anthropometric measurements and bone mass of mother-infant pairs: a randomized placebo clinical trial. Early Hum Dev 103:61–68
O’Callaghan KM, Shanta SS, Fariha F, Harrington J, Mahmud AA, Emdin AL et al (2022) Effect of maternal prenatal and postpartum vitamin D supplementation on offspring bone mass and muscle strength in early childhood: follow-up of a randomized controlled trial. Am J Clin Nutr 115(3):770–780
Gopal-Kothandapani JS, Rigby AS, Harrison R, Eastell R, Moon RJ, Curtis EM et al (2020) Maternal pregnancy vitamin D supplementation increases offspring bone formation in response to mechanical loading: findings from a MAVIDOS Trial sub-study. J Musculoskelet Neuronal Interact 20(1):4–11
Congdon P, Horsman A, Kirby PA, Dibble J, Bashir T (1983) Mineral content of the forearms of babies born to Asian and white mothers. BMJ (Clin Res Ed) 286(6373):1233–1235
Wall CR, Stewart AW, Camargo CA Jr, Scragg R, Mitchell EA, Ekeroma A et al (2016) Vitamin D activity of breast milk in women randomly assigned to vitamin D3 supplementation during pregnancy. Am J Clin Nutr 103(2):382–388
Crozier SR, Harvey NC, Inskip HM, Godfrey KM, Cooper C, Robinson SM (2012) Maternal vitamin D status in pregnancy is associated with adiposity in the offspring: findings from the Southampton Women’s Survey. Am J Clin Nutr 96(1):57–63
Harvey NC, Sheppard A, Godfrey KM, McLean C, Garratt E, Ntani G et al (2014) Childhood bone mineral content is associated with methylation status of the RXRA promoter at birth. J Bone Miner Res 29(3):600–607
Curtis E, Cook E, Kristic N, D’Angelo S, Crozier SR, Moon RJ et al (2017) DNA methylation at the RXRA promotor at birth is associated with gestational vitamin D supplementation: results from the MAVIDOS trial. Osteoporos Int 28(Suppl 1):OC36
Blighe K, Chawes BL, Kelly RS, Mirzakhani H, McGeachie M, Litonjua AA et al (2017) Vitamin D prenatal programming of childhood metabolomics profiles at age 3 y. Am J Clin Nutr 106(4):1092–1099
Green HD, D’Angelo S, Cooper C, Harvey NC, Moon RJ (2022) editors. P300: vitamin D supplementation during pregnancy increases offspring birth weight and calcium status: a systematic review and meta-analysis WCO-IOF-ESCEO 2022 World Congress on Osteoporosis, Osteoarthritis and Musculoskeletal Diseases; 2022 2022
Gallo S, McDermid JM, Al-Nimr RI, Hakeem R, Moreschi JM, Pari-Keener M et al (2020) Vitamin D supplementation during pregnancy: an evidence analysis center systematic review and meta-analysis. J Acad Nutr Diet 120(5):898-924.e4
Harvey NC, Javaid K, Bishop N, Kennedy S, Papageorghiou AT, Fraser R et al (2012) MAVIDOS Maternal Vitamin D Osteoporosis Study: study protocol for a randomized controlled trial. The MAVIDOS Study Group Trials 13:13
Harvey N, Holroyd C, Ntani G, Javaid M, Cooper P, Moon R, et al (2014) Vitamin D supplementation in pregnancy: a systematic review. Health Technol Assess 18(45)
Cockburn F, Belton NR, Purvis RJ, Giles MM, Brown JK, Turner TL et al (1980) Maternal vitamin D intake and mineral metabolism in mothers and their newborn infants. BMJ 281(6232):11–14
National Institute for Health and Care Excellence (2014) Vitamin D: increasing supplement use in at-risk groups [PHC56]. https://www.nice.org.uk/guidance/ph56; 2014
Ross AC, Taylor CL, Yaktine AL, Del Valle HB (2011) Dietary reference intakes for calcium and vitamin D 2011
Paxton GA, Teale GR, Nowson CA, Mason RS, McGrath JJ, Thompson MJ et al (2013) Vitamin D and health in pregnancy, infants, children and adolescents in Australia and New Zealand: a position statement. Med J Aust 198(3):142–143
Munns CF, Shaw N, Kiely M, Specker BL, Thacher TD, Ozono K et al (2016) Global consensus recommendations on prevention and management of nutritional rickets. J Clin Endocrinol Metab 101(2):394–415
Moon RJ, Harvey NC, Cooper C, D’Angelo S, Crozier SR, Inskip HM et al (2016) Determinants of the maternal 25-hydroxyvitamin D response to vitamin D supplementation during pregnancy. J Clin Endocrinol Metab 101(12):5012–5020
Elkum N, Alkayal F, Noronha F, Ali MM, Melhem M, Al-Arouj M et al (2014) Vitamin D insufficiency in Arabs and South Asians positively associates with polymorphisms in GC and CYP2R1 genes. PLoS One 9(11):e113102
Moon RJ, Cooke LDF, D’Angelo S, Curtis EM, Titcombe P, Davies JH, et al (2022) Maternal and fetal genetic variation in vitamin D metabolism and umbilical cord blood 25-hydroxyvitamin D. J Clin Endocrinol Metab
Moon RJ, Harvey NC, Cooper C, D’Angelo S, Curtis EM, Crozier SR et al (2017) Response to antenatal cholecalciferol supplementation is associated with common vitamin D-related genetic variants. J Clin Endocrinol Metab 102(8):2941–2949
Batai K, Murphy AB, Shah E, Ruden M, Newsome J, Agate S et al (2014) Common vitamin D pathway gene variants reveal contrasting effects on serum vitamin D levels in African Americans and European Americans. Hum Genet 133(11):1395–1405
Funding
We are grateful for the following funding: UKRI Medical Research Council (MRC) [MC_PC_21022; MC_PC_21003; MC_PC_21001]; National Institute for Health and Care Research (NIHR) Southampton Biomedical Research Centre, University of Southampton, and University Hospital Southampton NHS Foundation Trust; NIHR Oxford Biomedical Research Centre, University of Oxford; and Versus Arthritis (17702 and 21231). The work leading to these results was supported by the European Union’s Seventh Framework Programme (FP7/2007–2013), projects EarlyNutrition, ODIN and LifeCycle under grant agreements numbers 289346, 613977 and 733206, and by the BBSRC (HDHL-Biomarkers, BB/P028179/1 and BB/P028187/1), as part of the ALPHABET project, supported by an award made through the ERA-Net on Biomarkers for Nutrition and Health (ERA HDHL), Horizon 2020 grant agreement number 696295. RJM is funded by Health Education England (HEE)/National Institute for Health Research (NIHR) for this research project. KMG is supported by the UK Medical Research Council (MC_UU_12011/4), the National Institute for Health Research (NIHR Senior Investigator (NF-SI-0515–10042) and NIHR Southampton Biomedical Research Centre (IS-BRC-1215–20004)), the European Union (Erasmus + Programme ImpENSA 598488-EPP-1–2018-1-DE-EPPKA2-CBHE-JP), British Heart Foundation (RG/15/17/3174, SP/F/21/150013) and the US National Institute On Aging of the National Institutes of Health (Award No. U24AG047867). For the purpose of Open Access, the author has applied a Creative Commons Attribution (CC BY) licence to any Author Accepted Manuscript version arising from this submission.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Consents and ethics approval
This systematic review and meta-analysis contains no original data and thus issues of ethics, informed consent and patient confidentiality do not apply.
Conflicts of interest
HDG and SD have no conflicts of interest. RJM has received travel bursaires from Kyowa Kirin. KMG has received reimbursement for speaking at conferences sponsored by companies selling nutritional products, and is part of an academic consortium that has received research funding from Abbott Nutrition, Nestec, BenevolentAI Bio Ltd. and Danone, outside the submitted work. JHD has received travel bursaries from Novo Nordisk, SANDOZ and Pfizer unrelated to this work. EMC reports honoraria/travel support from Eli Lilly, Pfizer and UCB outside the submitted work. CC reports personal fees from ABBH, Amgen, Eli Lilly, GSK, Medtronic, Merck, Novartis, Pfizer, Roche, Servier and Takeda, outside the submitted work. NCH reports personal fees, consultancy, lecture fees and honoraria from Alliance for Better Bone Health, AMGEN, MSD, Eli Lilly, Servier, Shire, Consilient Healthcare and Internis Pharma, outside the submitted work.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Moon, R.J., Green, H.D., D’Angelo, S. et al. The effect of pregnancy vitamin D supplementation on offspring bone mineral density in childhood: a systematic review and meta-analysis. Osteoporos Int 34, 1269–1279 (2023). https://doi.org/10.1007/s00198-023-06751-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-023-06751-5