Abstract
Summary
Many current guidelines for the assessment of osteoporosis, including those in Kuwait, initiate fracture risk assessment in men and women using BMD T-score thresholds. We compared the Kuwaiti guidelines with FRAX-based age-dependent intervention thresholds equivalent to that in women with a prior fragility fracture. FRAX-based intervention thresholds identified women at higher fracture probability than fixed T-score thresholds, particularly in the elderly.
Purpose
A FRAX® model been recently calibrated for Kuwait, but guidance is needed on how to utilise fracture probabilities in the assessment and treatment of patients.
Methods
We compared age-specific fracture probabilities, equivalent to women with no clinical risk factors and a prior fragility fracture (without BMD), with the age-specific fracture probabilities associated with femoral neck T-scores of −2.5 and −1.5 SD, in line with current guidelines in Kuwait. Upper and lower assessment thresholds for BMD testing were additionally explored using FRAX.
Results
When a BMD T-score of −2.5 SD was used as an intervention threshold, FRAX probabilities of a major osteoporotic fracture in women aged 50 years were approximately twofold higher than those in women of the same age but with an average BMD. The increase in risk associated with the BMD threshold decreased progressively with age such that, at the age of 83 years or more, a T-score of −2.5 SD was associated with a lower probability of fracture than that of the age-matched general population with no clinical risk factors. The same phenomenon was observed from the age of 66 years at a T-score of −1.5 SD. A FRAX-based intervention threshold, defined as the 10-year probability of a major osteoporotic fracture in a woman of average BMI with a previous fracture, rose with age from 4.3% at the age of 50 years to 23%, at the age of 90 years, and identified women at increased risk at all ages. Qualitatively comparable findings were observed in the case of hip fracture probability and in men.
Conclusion
Intervention thresholds based on BMD alone do not optimally target women at higher fracture risk than those on age-matched individuals without clinical risk factors, particularly in the elderly. In contrast, intervention thresholds based on fracture probabilities equivalent to a ‘fracture threshold’ consistently target women at higher fracture risk, irrespective of age.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is operationally defined based on the measurement of bone mineral density (BMD) assessment [1], with recent refinements of the description that focus on measurements at the femoral neck as a reference standard [2]. The WHO-defined T-score of ≤−2.5 SD, originally designed as an epidemiological tool, has been widely adopted as both a diagnostic and intervention threshold. The principal difficulty for fracture risk assessment is that this threshold has high specificity but low sensitivity, so that the majority of fragility fractures occur in individuals with BMD values above the osteoporosis threshold [3]. Over the last two decades, many risk factors have been identified that contribute to fracture risk, at least partly if not wholly independent of BMD: these include age, sex, a prior fracture [4], a family history of fracture [5] and lifestyle risk factors such as physical inactivity [6] and smoking [7]. These and other factors have been combined in analyses of individual cohort studies to develop algorithms and scores to characterise future risk in an individual.
The most widely validated and utilised fracture-risk assessment tool is FRAX® which was developed by the former WHO collaborating centre at the University of Sheffield. The FRAX tool integrates the risks of fracture together with the risk of death to provide the 10-year probability of hip fracture and major osteoporotic fracture (clinical spine, distal forearm, proximal humerus and hip fracture) [8, 9].
The 10-year probabilities of fracture [10] and death vary markedly in different regions of the world, so that the FRAX models are calibrated to the known epidemiology of fracture and death. This assumes that the relative importance of the risk factors and their interactions are the same as in the original material. At present, 63 country models are available, and the tool currently provides coverage for over 80% of the global population [11].
Historically, treatment has been targeted to patients with a prior fragility fracture, a WHO-defined T-score or both. Since its release, FRAX has been incorporated into more than 100 guidelines worldwide [12]. The setting of universal intervention thresholds is problematic from an international perspective since the risk of fracture, the costs of fracture and treatment, reimbursement policy and willingness to pay, vary in different countries. In Kuwait, assessment guidelines are predominantly based on BMD and the presence of osteoporosis. A FRAX model for Kuwait, calibrated to the total Kuwaiti population, was released in March 2016 [13]. The aim of the present analysis was to explore FRAX-based intervention thresholds that might be used to identify men age 50 years or more and postmenopausal women from Kuwait at high fracture risk and to compare this strategy with the selection of individuals based on BMD.
Methods
Guidelines in Kuwait
The Kuwait Osteoporosis Society, adopted BMD-based criteria as intervention thresholds in 2014 [14]. The strategy was based on case finding where men and women with one or more major risk factor (including fragility fracture after age 40 years, parental hip fracture, systemic glucocorticoid therapy, malabsorption, primary hyperparathyroidism, hypogonadism and osteopenia apparent on X-ray) or two or more minor risk factors are referred for densitometry. The currently published criterion for treatment of osteoporosis in Kuwait is a BMD T-score ≤−2.5 SD, though provision is made for treatment in patients with osteopenia using fixed FRAX probability thresholds of 20% for a major fracture and 3% for hip fracture. The guideline takes some elements from the guidelines of the National Osteoporosis Foundation in the US and those of the Scottish Intercollegiate Network in Scotland [15, 16].
FRAX-based intervention threshold
The UK guidance for the identification of individuals at high fracture risk, first developed by the National Osteoporosis Guideline Group (NOGG), recommends that postmenopausal women with a prior fragility fracture may be considered for intervention without the necessity for a BMD test [17, 18]. In postmenopausal women without a fragility fracture but a FRAX risk factor, the intervention threshold set by NOGG is at the age-specific fracture probability equivalent to women with a prior fragility fracture. In this context, fragility fracture is defined as a previous fracture in adult life occurring spontaneously or a fracture arising from trauma which, in a healthy individual, would not have resulted in a fracture (http://www.shef.ac.uk/FRAX/). For example, using the NOGG guidance, a woman at age 65 years (BMI 24 kg/m2) with a prior fragility fracture has a 10-year probability of a major osteoporotic fracture of 17% and this forms the intervention threshold for that age. A woman of the same age with no prior fracture but on glucocorticoids for rheumatoid arthritis has a fracture probability of 19%. Thus, the latter would be eligible for treatment despite the absence of a prior fracture. The same intervention threshold (17%) is applied to men of the same age, since the effectiveness and cost-effectiveness of intervention in men are broadly similar to that in women for equivalent risk. This approach was used to compare with the Kuwaiti guidance.
Comparison
Using the FRAX model for Kuwait, we computed the 10-year probability of a major osteoporotic fracture and a hip fracture in men and women with a BMD T-score of −2.5 SD at 5-year intervals from the age of 50 years. We similarly computed the 10-year probability of a major osteoporotic fracture and a hip fracture with a BMD T-score of −1.5 SD. The T-score of −1.5 SD was chosen to represent the mid-range of osteopenia. For comparison, fracture probabilities were computed (without the inclusion of BMD) in women by age who had sustained a prior fragility fracture. Fracture probabilities by age were compared to age-specific probabilities in men and women with no clinical risk factors (without the inclusion of BMD). Body mass index was set at 30 kg/m2 (the average value of Kuwaiti women [19]) for all scenarios, and individuals were assumed to have no other FRAX risk variables.
In line with NOGG, we explored the setting of assessment thresholds for BMD. The inclusion of BMD in the calculation of probability improves the accuracy of the assessment [20] but its added value is greatest where fracture probabilities lie close to an intervention threshold [21,22,23]. In other words, testing is confined to those in whom there is a reasonable likelihood that individuals at high (or low) risk would be reclassified at low (or high) risk based on the BMD test. On this basis, we calculated two assessment thresholds which were applied to the FRAX-based thresholds described above:
-
The threshold probability below which neither treatment nor a BMD test should be considered (lower assessment threshold).
-
The threshold probability above which treatment may be recommended without the need for BMD (upper assessment threshold).
The lower assessment threshold was based on the 10-year probability (without BMD) of a major osteoporosis fracture equivalent to women without clinical risk factors (and a body mass index of 30 kg/m2). This is consistent with a view in most practice guidelines that individuals without clinical risk factors should not be considered eligible for assessment [12].
The upper assessment threshold was set to optimise the requirement for BMD testing [17]. As noted above, the risk of changing category from high risk to low risk or vice versa when adding BMD to the estimation of fracture probability is highest close to the threshold. When patients have a fracture probability that is 20% or more than the intervention threshold, almost no individuals are reclassified when probabilities are recomputed with the addition of BMD to FRAX [17]. For this reason, the upper assessment threshold was set at 1.2 times the intervention threshold. In some countries, assessment thresholds are based on hip fracture probabilities in addition to probabilities of a major osteoporotic fracture. The methodology used in the present report for hip fracture was identical to that used for a major osteoporotic fracture.
Results
In women with no clinical risk factors and an average BMD for age, probability of a major osteoporotic fracture rose with age from 1.0% at the age of 40 years to 14% at the age of 90 years (Table 1). Equivalent hip fracture probabilities are given in supplementary information (Table A1).
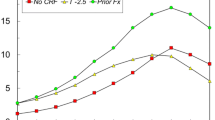
Intervention thresholds based on BMD
In women age 50 years at the threshold of osteoporosis (a BMD T-score of −2.5 SD), fracture probability was more than twofold higher than that in women of the same age without any risk factors. The 10-year fracture probability rose progressively with age from 2.6% at the age of 40 years to 13% at the age of 90 years. With advancing years, the difference in probability between women with a T-score of −2.5 SD and women of the same age without any risk factors decreased. Above the age of 83 years, the fracture probability was lower than in women of the same age but with no risk factors (Fig. 1). Thus, the BMD criterion for intervention using a fixed T-score became less and less appropriate with advancing age. At a T-score of −1.5 SD, the fracture probability was lower than that in women of the same age but with no risk factors from the age of 66 years.
The fracture probabilities equivalent to women with a previous fragility fracture are shown in Table 1. The probability of a major osteoporotic fracture rose with age, from 2.3% at the age of 40 years to 23% at the age of 90 years. Fracture probabilities were consistently higher than those in women with no clinical risk factors.
When hip fracture probability was used, the risk of hip fracture was ninefold increased at the age of 50 years for women with T-score −2.5 compared to women with no clinical risk factors and average BMD (albeit with low absolute probabilities in either scenario) and, as in the case of major osteoporotic fracture, decreased progressively with age. The fracture probability was lower than that in women of the same age but with no risk factors from the age of 87 years (Fig. 2). For a T-score of −1.5 SD, the same phenomenon was observed for hip fracture from the age of 65 years (data not shown).
In the case of men, the findings were similar. For a major osteoporotic fracture, a T-score of −2.5 SD was associated with a fracture probability that was lower than that in men of the same age but with no risk factors from the age of 90 years and for a T-score of −1.5 SD, at or above the age of 80 years. When hip fracture probability was used, the same phenomena at a T-score of −2.5 SD in men noted at or above the age of 88 years (see Fig. 2) and, with a T-score of −1.5 SD, above the age of 78 years.
Probability-based intervention thresholds and BMD assessment thresholds
The intervention threshold was set at the age-dependent 10-year probability of a major osteoporotic fracture that was equivalent to a woman with a prior fragility fracture (see Fig. 1). As used in the NOGG guidance, the lower assessment threshold, below which BMD tests are of limited value, was set at the age-specific probabilities in women with no clinical risk factors. The upper assessment was set at 1.2 times the intervention threshold. The three thresholds are shown in Table 2. Intervention thresholds, based on hip fracture probability are shown in the supplementary appendix (Table A2). The practical applications of these thresholds for Kuwait are provided in the discussion below.
Discussion
Bone mineral density (BMD) measured by dual X-ray absorptiometry (DXA) is the current reference standard for the diagnosis of osteoporosis. Since BMD is one of the strongest predictors of fracture risk [24, 25], many agencies worldwide have adopted BMD-based criteria as intervention thresholds. The present study demonstrates weaknesses in the use of fixed BMD thresholds as intervention thresholds. Whereas a T-score threshold of −2.5 SD was a strong risk factor for fracture at younger ages, with advancing age, the association with high risk decreased progressively with age. The effect was even more marked at a less stringent T-score threshold. For example, a T-score of −1.5 SD was a ‘protective factor’ for hip fracture from the age of 65 years in that fracture probabilities were lower than in women in the ‘general’ population (i.e. women with no clinical risk factors and average BMD for age). The reason relates to the decreasing BMD in the general population with age. The phenomenon has been noted in the case of major osteoporotic fractures in women from the Romania, UK and US [26, 27]. The present analysis identifies that the same phenomenon holds true for hip fracture prediction and in men.
In the context of the current guidelines in Kuwait, several additional factors make the use of the T-score problematic as the major gateway to targeting individuals at high fracture risk. Whereas a prior fragility fracture confers a risk that is significant at all ages and independent of BMD, this increase in risk is ignored in that treatment is recommended only where the BMD T-score ≤−2.5 SD. The same is true for all major risk factors. Thus, the guideline does not use the information provided by the presence of strong risk factors. Bizarre but not improbable scenarios arise. For example, consider a 65-year-old woman (BMI set at 30 kg/m2) whose mother had sustained a hip fracture (Table 3). Under existing guidelines, her risk factor earns her a BMD test and the decision to treat rests solely on her T-score. At a T-score of −2.5 SD, the threshold of osteoporosis, she can be offered treatment (equivalent to a 10-year probability of a major osteoporotic fracture of 11%) but is denied treatment with a T-score of −2.0 SD, even though her fracture probability is higher than that in the BMD-based threshold (9.1 vs. 6.5%).
A final consideration concerns the availability of densitometers in many countries. The policy assumes that all prospective patients should have a BMD test, and the availability of BMD equipment is limited. In a recent survey, there were 7.5 DXA machines per million of the general Kuwaiti population (JA Kanis 2014 personal communication), whereas 11 or more is considered appropriate to service the needs of a case-finding strategy [28].
The advent of FRAX has provided an opportunity to base intervention thresholds based on fracture probability, which increases the sensitivity of fracture prediction compared to the use of BMD alone [20]. FRAX has been incorporated into more than 100 guidelines worldwide, but the way FRAX is used to identify cases for treatment varies. An increasing number of guidance documents have recommended the use of intervention thresholds that are based on age-specific fracture probabilities equivalent to a woman with a prior fragility fracture [29, 30], first espoused by the National Osteoporosis Guideline group (NOGG) in the UK [18]. In the present paper, we have compared the performance of the NOGG approach applied to the Kuwaiti population using the Kuwait-specific FRAX model. The intervention threshold using this approach varied from 4.3% at the age of 50 years to 23% at the age of 90 years. Thus, men and women who have a fracture probability that is equal or exceeds that of a woman with a prior fracture would be eligible for treatment even in the absence of a fracture history. These intervention thresholds are developed without the use of BMD in the FRAX model. Notwithstanding, the categorisation of patients at high or low risk is improved using BMD. For this reason, the present study provided assessment thresholds for the use of BMD tests in a manner similar to that of NOGG. The approach capitalises on the improved risk assessment provided by BMD tests but decreases the number of tests required when BMD is used as the principal gateway for assessment [31].
Practical application
The concept of assessment thresholds can be illustrated in terms of the management pathway. The management process begins with the assessment of fracture probability and the categorisation of fracture risk on the basis of age, sex, BMI and the clinical risk factors. On this information alone, some patients at high risk may be offered treatment without recourse to BMD testing. For example, as noted above, most guidelines in Europe and North America recommend treatment in the absence of BMD in women with a previous fragility fracture. Many would perform a BMD test, but frequently this is for reasons other than to decide on intervention (e.g. as a baseline for monitoring treatment). There will be other instances where the probability will be so low that a decision not to treat can be made without BMD. An example might be the well woman at menopause with no clinical risk factors. Thus, not all individuals require a BMD test.
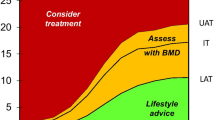
The use of assessment thresholds is illustrated in the management algorithm given in Fig. 3 and outlined below [29].
-
1.
Women with a prior fragility fracture should be considered for treatment.
-
2.
Postmenopausal women and men with a clinical risk factor should have fracture probability assessed using the FRAX tool without measurement of BMD.
-
3.
Individuals with probabilities of a major osteoporotic fracture below the lower assessment threshold given in Fig. 3 can be reassured. A further assessment may be recommended in 5 years or less depending on the clinical context.
-
4.
Men and women with probabilities of a major osteoporotic fracture above the upper assessment threshold (or with probabilities of a hip fracture above the upper limit) can be considered for treatment without BMD testing.
-
5.
Individuals with probabilities of a major osteoporotic fracture within the limits of the assessment thresholds given in Fig. 3 should have a BMD test and probabilities recomputed. If probabilities exceed the treatment threshold, intervention should be considered.
Intervention thresholds for Kuwait as set by FRAX-based 10-year probabilities (%) of a major osteoporotic fracture. The red area is where treatment could be recommended, the green area is where treatment would not be recommended and the orange area is where BMD could be measured (where available) to enhance the estimation of fracture risk. UAT upper assessment threshold, IT intervention threshold, LAT lower assessment threshold
The intervention thresholds proposed above are not without limitations. The consequences of assessment and intervention thresholds on the requirements for BMD testing have not been explored. It will also be important to explore the cost-effectiveness of intervention and the budget impact of any changes in reimbursement policy. Despite these gaps, intervention strategies based on fracture probabilities are more effective than strategies reliant on the use of BMD alone in identifying high-risk individuals for treatment and avoiding intervention in those at low risk [32]. An added advantage is that BMD testing is not a prerequisite for assessment or treatment. This feature would be particularly useful in areas of Kuwait with limited access to DXA. It should be noted that the algorithms proposed are specific for Kuwait but the same principles can be applied to any country where a FRAX model is available. More generally, the mean BMI in Kuwaiti women is 30 kg/m2 which will have an impact in lowering the treatment threshold compared with many countries. More importantly, the thresholds derived depend critically on the hazards of fracture and death in Kuwait. Thus, each FRAX model is country specific. Notwithstanding, these factors do not nullify the general conclusion that age-dependent FRAX-based intervention thresholds identify women at higher fracture probability than fixed T-score thresholds.
We conclude that FRAX-based intervention thresholds identify men and women at higher fracture probability than fixed T-score thresholds, particularly in the elderly.
References
Kanis JA, Melton LJ, Christiansen C, Johnston C, Khaltaev N (1994) The diagnosis of osteoporosis. J Bone Miner Res 9:1137–1141
Kanis JA, McCloskey EV, Johansson H, Oden A, Melton LJ 3rd, Khaltaev N (2008) A reference standard for the description of osteoporosis. Bone 42:467–475
World Health Organisation (1994) assessment of fracture risk and its application to screening for postmenopausal osteoporosis. WHO Technical Report Series 843. 1994. WHO, Geneva
Kanis JA, Johnell O, De Laet C et al (2004a) A meta-analysis of previous fracture and subsequent fracture risk. Bone 35:375–382
Kanis JA, Johansson H, Oden A et al (2004) A family history of fracture and fracture risk: a meta-analysis. Bone 35:1029–1037
Feskanich D, Willett W, Colditz G (2002) Walking and leisure-time activity and risk of hip fracture in postmenopausal women. JAMA 288:2300–2306
Kanis JA, Johnell O, Oden A et al (2005) Smoking and fracture risk: a meta-analysis. Osteoporos Int 16:155–162
Kanis JA on behalf of the World Health Organization Scientific Group (2008a) Assessment of osteoporosis at the primary health-care level. Technical Report. WHO Collaborating Centre, University of Sheffield, UK
Kanis JA, Johnell O, Oden A, Johansson H, McCloskey E (2008b) FRAX™ and the assessment of fracture probability in men and women from the UK. Osteoporos Int 19:385–397
Kanis JA, Odén A, McCloskey EV, Johansson H, Wahl D, Cyrus Cooper C on behalf of the IOF Working Group on Epidemiology and Quality of Life (2012) A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int 23:2239–2256
Oden A, McCloskey EV, Kanis JA, Harvey NC, Johansson H (2015) Burden of high fracture probability worldwide: secular increases 2010-2040. Osteoporos Int 26:2243–2248
Kanis JA, Harvey NC, Cooper C, Johansson H, Odén A, McCloskey EV, the Advisory Board of the National Osteoporosis Guideline Group (2016) A systematic review of intervention thresholds based on FRAX. Arch Osteoporos 11(1):25
Azizieh FY (2015) Incidence of hip fracture in Kuwait: a national registry-based study Arch Osteoporos 10: 40
Kuwait Osteoporosis Society (2014) 2014 Kuwait osteoporosis society guidelines for the screening and treatment of osteoporosis Accessed 28 Sept 2016, www.kops-kw.org/GuideLines.aspx
Cosman F, de Beur SJ, LeBoff MS et al (2014) Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 25:2359–2381
Scottish Intercollegiate Guidelines Network (SIGN) (2015) Management of osteoporosis and the prevention of fragility fractures. Edinburgh: SIGN; 2015. (SIGN publication no. 142). http://www.sign.ac.uk. Accessed May 11 2015
Kanis JA, McCloskey, EV, Johansson H, Strom O, Borgstrom F, Oden A and the National Osteoporosis Guideline Group (2008c) Case finding for the management of osteoporosis with FRAX®—assessment and intervention thresholds for the UK. Osteoporos Int 19: 1395-1408 erratum 2009. Osteoporos Int 20: 499–502
Compston J, Cooper A, Cooper C, On behalf of the National Osteoporosis Guideline Group (NOGG) et al (2009) Guidelines for the diagnosis and management of osteoporosis in postmenopausal women and men from the age of 50 years in the UK. Maturitas 62:105–108
Newkuwat. The public authority for civil information. https://www.paci.gov.kw/ accessed 30 june 2106
Kanis JA, Oden A, Johnell O et al (2007) The use of clinical risk factors enhances the performance of BMD in the prediction of hip and osteoporotic fractures in men and women. Osteoporos Int 18:1033–1046
Johansson H, Oden A, Johnell O et al (2004) Optimization of BMD measurements to identify high risk groups for treatment—a test analysis. J Bone Miner Res 19:906–913
Leslie WD, Majumdar SR, Lix LM et al (2012) High fracture probability with FRAX usually indicates densitometric osteoporosis: implications for clinical practice. Osteoporos Int 23:391–397
Kanis JA, McCloskey E, Johansson H, Oden A, Leslie WD (2012) FRAX(®) with and without bone mineral density. Calcif Tissue Int 90:1–13
Marshall D, Johnell O, Wedel H (1996) Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. Br Med J 312(7041):1254–1259
Johnell O, Kanis JA, Oden A, Johansson H, De Laet C, Delmas P et al (2005) Predictive value of BMD for hip and other fractures. J Bone Miner Res 20:1185–1194
Grigorie D, Sucaliuc A, Johansson H, Kanis JA, McCloskey E (2013) FRAX-based intervention and assessment thresholds for osteoporosis in Romania. Arch Osteoporos 8:164
Kanis JA, Compston J, Cooper C, Harvey NC, Johansson H, Odén A, McCloskey EV (2016) SIGN guidelines for Scotland: BMD versus FRAX versus QFracture. Calcif Tissue Int 98:417–425
Kanis JA, Johnell O (2005) Requirements for DXA for the management of osteoporosis in Europe. Osteoporos Int 16:229–238
Lekamwasam S, Adachi JD, Agnusdei D et al (2012) A framework for the development of guidelines for the management of glucocorticoid-induced osteoporosis. Osteoporos Int 23:2257–2276
Kanis JA, McCloskey EV, Johansson H, Cooper C, Rizzoli R, Reginster JY (2013) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 24:23–57
Johansson H, Kanis JA, Oden A, Compston J, McCloskey E (2012) A comparison of case-finding strategies in the UK for the management of hip fractures. Osteoporos Int 23:907–915
Kanis JA, McCloskey EV, Harvey NC, Johansson H, Leslie WD (2015) Intervention thresholds and the diagnosis of osteoporosis. J Bone Miner Res 30:1747–1753
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Professor Kanis led the team that developed FRAX as director of the then WHO collaborating centre for metabolic bone diseases; he has no financial interest in FRAX. Professors McCloskey, Oden, Harvey and Dr. Johansson are members of the FRAX team. Professors Harvey, Kanis and McCloskey are members of the Expert Advisory Group of the National Osteoporosis Guideline Group, UK.
Rights and permissions
About this article
Cite this article
Johansson, H., Azizieh, F., al Ali, N. et al. FRAX- vs. T-score-based intervention thresholds for osteoporosis. Osteoporos Int 28, 3099–3105 (2017). https://doi.org/10.1007/s00198-017-4160-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-017-4160-7