Abstract
Summary
The present cross-sectional study performed using data from the Korea National Health and Nutrition Examination Survey in 9526 women older than 18 years of age demonstrates that high sodium intake is associated with lower bone mineral density and sodium intake ≥2000 mg/day is a risk factor for osteoporosis in postmenopausal women.
Introduction
Several studies have reported that large amount of dietary sodium intake is highly associated with elevated urinary calcium. However, the direct effect of excessive dietary sodium intake on bone mass, as a risk factor for osteoporosis, is still a controversial issue. The aim of the present study was to assess the relationship between high intake of sodium and lower bone mass and risk of osteoporosis in adult women.
Methods
This cross-sectional study was performed using data from the Korea National Health and Nutrition Examination Survey (KNHANES), 2008–2011. Participants (n = 9526 women older than 18 years) were divided into a premenopausal (n = 4793) and postmenopausal (n = 4733) group. Both groups were subdivided into five groups according to quintiles of energy-adjusted sodium intake. Multiple regression analysis was performed to assess relationships between sodium intake and lower bone mass.
Results
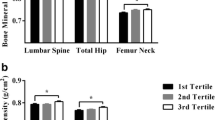
Multivariate linear regression analysis showed that high sodium intake was negatively associated with bone mineral content (BMC) and bone mineral density (BMD) in postmenopausal women. After adjusting confounding factors, high sodium intake was negatively associated with BMC and BMD of the lumbar spine in postmenopausal women. Postmenopausal women, whose sodium intake was ≥2000 mg/day (odds ratio 1.284, 95% CI 1.029–1.603, P = 0.027), were at risk of developing osteoporosis after adjustment of confounding variables.
Conclusions
The present study suggested that high sodium intake could be a potential risk factor for low bone mass after adjusting for confounding factors in postmenopausal women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a skeletal disorder, which has features of impaired bone strength leading to elevated risk of skeletal fractures and has become a major public health concern [1]. In Korea, osteoporosis prevalence has been reported to be 38.0% in postmenopausal women [2] and is thought to be steadily rising because of increased life expectancy and changing lifestyle including physical activity and nutrition.
It has been generally accepted that adequate nutrition, especially calcium and vitamin D intake, plays major roles in improving skeletal health and preventing osteoporosis [3, 4]. Based on the existence of linked or common reabsorptive pathways for sodium and calcium in the convoluted portion of the proximal tubule and in the thick ascending loop of Henle, excessive sodium intake is associated with urinary calcium excretion. Higher calcium excretion might be associated with lower bone mass [5, 6].
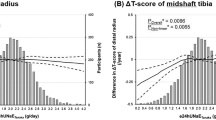
Previous reports have shown that large amount of dietary sodium is highly associated with elevated urinary calcium [6–13]. However, there are still controversial issues regarding the effects of dietary sodium on bone mineral content (BMC) or bone mineral density (BMD). An animal study showed that high intake of dietary sodium was negatively associated with BMC of the femur in rats [14], and a longitudinal study reported negative correlation between urinary sodium excretion and bone density changes of hip and intertrochanter in 124 postmenopausal women [15]. In contrast, two reported studies demonstrated positive association between sodium intake and BMD at an ultradistal radius in men but not in women [16] and BMD of forearm and spine in postmenopausal women [17]. However, a recent prospective observational study has reported that there was no association between calibrated sodium intake and changes in BMD at the hip or lumbar spine during 3 to 6 years of follow-up [18].
Therefore, the present study was designed as a cross-sectional study examining the direct effect of excessive dietary sodium intake on bone mass, which is a risk factor for osteoporosis in adult women, using data from nationwide representative survey. The aim of the present study was to test the hypothesis that high intake of sodium is negatively associated with bone mass and risk of developing osteoporosis using data from Korea National Health and Nutrition Examination Survey (KNHANES).
Methods
Subjects and exclusion criteria
We used data from the KNHANES 2008–2011 for this study. KNHANES, conducted by Korean Ministry of Health and Welfare, is a nationwide cross-sectional survey designed to evaluate health and nutritional status of non-institutionalized and civilian Korean population. KNHANES comprises of three component surveys: health interview, health examination, and nutrition survey. The health interview and health examination at Mobile Examination Centers (MEC) were conducted by trained staff members followed by in-person household interview by dietitians. The survey used multistage clustered probability design to select nationally representative sample. Institutional Review Board of Korea National Statistical Office, Centers for Disease Control and Prevention approved the KNHANES protocol. Informed consent was obtained from all participants [19, 20].
We compiled data of 37,753 participants from 2008 to 2011 KNHANES. Exclusion criteria were as follows: males (n = 17,195), age <19 years (n = 4479), missing data on dietary sodium intake (n = 1297), pregnancy or lactation (n = 430), renal failure (n = 23), missing data on BMC or BMD (n = 4391), Z-scores of sodium intake, BMD and BMC less than −3.29 or greater than +3.29 (n = 88), extreme energy intake (<500 kcal/d or >4000 kcal/day; n = 153), hormonal drug use such as estrogen or progesterone (n = 163), and missing data on postmenopausal status (n = 8). Thus, a total of 9526 female subjects were included for final analysis.
Information on medical conditions was collected by face-to-face interview, and cigarette smoking, alcohol use, and physical activity were obtained from self-administration of health interview questionnaire in MEC. Trained staffs measured height of the subjects with the use of a stadiometer (SECA 225, SECA, Germany) to the nearest 0.1 cm and weight with the use of an electronic scale (GL-6000-20, G-tech, Korea) to the nearest 0.1 kg.
For biochemical analysis, fasting blood and urine samples were taken, refrigerated, and then analyzed within 24 h at the Central Testing Center in Seoul, Korea. Serum 25-hydroxyvitamin D (25(OH)D) concentration (ng/mL) was measured using the radioimmunoassay method (1470 WIZARD Gamma-Counter, PerkinElmer, Finland). Serum alkaline phosphatase (ALP) levels were measured using the enzymatic method (Hitachi Automatic Analyzer 7600, Hitachi, Japan). Parathyroid hormone level was measured by the chemiluminescence immunoassay method (LIAISON, Diasorin, USA). Urinary sodium concentration was measured employing the ISE method (Hitachi Automatic Analyzer 7600, Hitachi, Japan).
Dietary intake data was collected by 1-day 24-h recall method during the household interview. Daily intake of energy, protein, sodium, calcium, potassium, and phosphorous was calculated based on Korean Food Composition Table [21]. High sodium intake is defined as ≥2000 mg/day based on the WHO guideline and recommendation [22].
Postmenopausal status was defined based on a self-reported questionnaire survey containing question for the determination of whether 1 year had passed since the time of last menstruation including hysterectomy. Regular exercise was defined as vigorous physical activity (e.g., running, mountaineering, fast bicycling, fast swimming, soccer, basketball, and singles tennis) for at least 20 min per day, 3 days per week or moderate physical activity (e.g., slow swimming, volleyball, doubles tennis, badminton, and walking) for at least 30 min per day, 5 days per week [23]. BMC and BMD at the total femur, femoral neck, and lumbar spine (L1–L4) sites were measured by trained technicians using dual-energy X-ray absorptiometry (DISCOVERY-W fan-beam densitometer, HOLOGIC, MA, USA) with CVs of 1.8, 2.5, and 1.9%, respectively. Osteopenia or osteoporosis was diagnosed with supplying by the DXA manufacturer (from Japanese population) [24] using T-score criteria of the World Health Organization: Normal, T-score of the total femur, femoral neck, and lumbar spine at either site ≥ −1; osteopenia, −2.5 < the lowest T-score < −1; and osteoporosis, the lowest T-score ≤ −2.5 [25].
Statistical analyses
All analyses were conducted with SPSS for Windows (Version 21.0, SPSS Inc., Chicago, IL, USA) using KNHANES sample weights to attain unbiased estimates of means and frequencies that were nationally representative of Korean population [26]. Complex sample analysis was used in this study to correct the distributions of the cluster sample regarding the primary sampling unit, covariance, and significance to correspond with those of the general Korean population. Values for sodium intake, BMD, or BMC at the total femur, femoral neck, and lumbar spine were standardized to identify univariate outliers. Cases with Z-scores less than −3.29 or greater than +3.29 were considered outliers and excluded from analysis. Daily intakes of nutrients were adjusted for energy intake using the residual method. Then, natural logarithmic transformation was undertaken for nutrient intake variables, including protein, sodium, calcium, potassium, and phosphorous, to achieve a normal distribution [27]. Continuous variables with normal distribution are presented as mean ± standard error of the mean (SEM). Categorical variables were expressed as frequencies and percentages. All analyses were performed by separating the female subjects into two groups: premenopausal women and postmenopausal women. The characteristics and risk factors for osteoporosis in study groups were compared using Student’s t test for continuous variables and chi square tests for categorical variables.
Multiple regression models were used to assess relationships between sodium intake and BMC or BMD. To screen out unsuitable potential covariates and to assess relationships between the potential covariates and BMC or BMD, we used multivariable regression analyses. In the multivariate models, the covariates showing P value under 0.20 were included in the final model [28]. All groups were subdivided into five groups according to quintiles of energy-adjusted sodium intake [27]. Analysis of covariance (ANCOVA) test with Bonferroni correction was performed to assess mean differences of BMC or BMD among intake quintile groups following the adjustment of confounding variables. We used multivariable logistic regression models to examine the associations between energy-adjusted sodium intake and osteoporosis. P value for trend was calculated by employing multivariate logistic regression analyses by handling the median value of each category of energy-adjusted sodium intake quintile as a continuous value. Analysis with and without the energy adjustment of sodium intake was done using a residual regression approach [27]. Two-sided P values <0.05 were considered statistically significant.
Results
Baseline characteristics and risk factors for osteoporosis of the study population are presented in Table 1. Premenopausal women were taller, consumed higher amount of energy, protein, calcium, phosphorous, potassium, and sodium, more likely to be alcohol drinker, and had higher BMC and BMD at the total femur, femoral neck, and lumbar spine, but lower body mass index (BMI), 25(OH)D, and ALP level than postmenopausal women.
There was a significant (P = 0.011) linear correlation between the amount of energy-adjusted sodium intake and urinary sodium excretion. After adjusting for potential confounders, logistic regression analysis showed that energy-adjusted sodium intake was negatively associated with the risk of osteoporosis in postmenopausal women, but not in premenopausal women (Table 2).
Consistently, Table 3 shows the negative association between energy-adjusted sodium intake and BMC/BMD, after adjustment for confounding variables, in postmenopausal women, but not in premenopausal women. Postmenopausal women consuming <2000 mg/day of sodium had lower odds ratios for osteoporosis than those with sodium intake ≥2000 mg/day, after adjustment for confounding variables (Table 4).
Discussion
This study is designed based on nationwide representative population and demonstrates that dietary sodium intake is negatively associated with BMC and BMD at lumbar spine sites in Korean postmenopausal woman, and postmenopausal women with high sodium intake increases the risk of osteoporosis after adjusting for potential confounders.
Devine et al. [15] performed a 2-year longitudinal study in postmenopausal women and reported that high sodium intakes were associated with increased bone loss at the hip area. However, these findings are inconsistent with other studies. Recently, Carbone et al. [18] performed a prospective observational cohort study including 69,735 postmenopausal women during a mean of 11.4-year follow-up and reported that there was no association of calibrated sodium intake with changes in BMD at the hip or lumbar spine. The mean sodium intake from Food Frequency Questionnaire (FFQ) was 2489.8 mg/day, and the biomarker-calibrated sodium was 2891.6 mg/day, lower than the 3728 mg/day level found in the present study. Illich et al. [17] reported positive association between dietary sodium intake and BMD at forearm and spine sites in 136 postmenopausal women, although all women in the study received calcium supplements. In addition, a prospective cohort study carried out involving 258 women and 169 men from dietary records showed that dietary sodium intake has a protective effect on the ultradistal radius site in men, but not in women in the multivariable models [16]. However, average sodium intake in the subjects was 3450 mg/day in men and 2576 mg/day in women, which was much lower when compared to population from Asian regions [29]. In this study, mean sodium intake was 3728 mg/day in postmenopausal women. A previous study consistently reported average intake of sodium intake was 3465 mg/day in 537 Korean postmenopausal women, suggesting that Korean consumed very high salt. [11]. Therefore, these discrepancies might be related with ethnic differences, age, gender, and different amount of calcium and sodium intake.
Previous studies reported that high urinary sodium excretion is significantly associated with low BMD and high prevalence of osteoporosis in the lumbar spine in a Korean nationwide population cohort [30, 31]. These two studies did not investigate the relationship between high sodium intake and the risk of osteoporosis in postmenopausal women, but the present study found a negative relationship between high sodium intake and BMD in the lumbar spine in postmenopausal women. In this study, the effect of high dietary sodium intake was not related to BMC and BMD in the hip, but was related to them in the lumbar spine in postmenopausal women. These findings might be related to the proportion of the trabecular bone as it is an important area for calcium metabolism. The percentage of the trabecular bone at the lumbar spine ranges from 72 to 80% and at the femur neck ranges from 23.5 to 25% [32, 33]. Therefore, a higher proportion of the trabecular in the lumbar is a more prominent decreasing rate of BMC and BMD than hip in postmenopausal women with high dietary sodium intake.
The present study has shown that risk of osteoporosis is higher in the excessive sodium consumption group (≥2000 mg/day) than in the low dietary sodium intake group (<2000 mg/day) among postmenopausal women. According to dietary reference intake for Koreans (KDRI), the daily recommended intake for sodium is <2000 mg/day [34]. However, in this study, the mean value of daily sodium intake was 4003 mg/day for women, which was 201.2% of KDRI. In addition, average calcium intake reported in the present study is 437.5 mg/day in women, which is lower than KDRI (KDRI recommends 650–700 mg/day of calcium intake for female adults). Previous studies investigated that sodium-induced calciuria is greater when there is insufficient calcium intake, which could exert an adverse effect on bone health [35, 36]. Thus, because of excessive sodium intake and inadequate calcium intake, the bone health of the study population could be vulnerable to sodium intake.
Excessive dietary sodium intake has a calciuric effect and increases bone remodeling mediated by an increase in parathyroid hormone in consequence of temporarily reduced serum calcium concentration, which might subsequently lead to lower BMC and BMD and higher risk of osteoporosis [6]. Heaney [37] reported that average loss of calcium was 20–60 mg for every 2300 mg of dietary sodium, suggesting that sodium intake might contribute to the pathogenesis of osteoporosis. In addition, Evans et al. [13] observed that high sodium intake was associated with an increase in bone resorption as measured by urinary deoxypyridinoline excretion in postmenopausal women, but not in premenopausal women. These findings were consistent with the present study that sodium intake was negatively associated with bone loss in postmenopausal but not in premenopausal women. It seems that sodium-induced calciuria is compensated for by a PTH-mediated increase in calcium absorption in premenopausal women, although the adaptive mechanism is unlikely to function properly in postmenopausal women and a compensatory mechanism might be insufficient to counterbalance the increased urinary calcium loss [6].
The major strength of this study lies in the fact that the data were gathered from a nationally representative survey throughout Korea, and thus, the findings could be generalized to the adult Korean population. However, the present study is also associated with several limitations. First, due to the cross-sectional study design, we were unable to identify the exact cause-and-effect relationship between dietary sodium intake and risk of osteoporosis. Second, sodium intake was calculated using a single 24-h recall method, which might be less accurate in comparison with FFQ. However, a 24-h recall is one of the few practically available methods for assessing dietary intakes in a large population, which was used in previous population-based studies [38]. In addition, urinary sodium was measured in the present study and significantly correlated with sodium intake. Third, although we adjusted for various possible confounding factors, there may be certain left-out residual confounders. Fourth, given that the sodium intake of Korean population is much higher as compared with many other regions including North America, Western Europe, and Australia/New Zealand [29], the generalizability of the findings is limited. Finally, it is possible that the Japanese reference database provided by the DXA manufacturer might be different from the mean bone mass in Koreans. Lee et al. [24] performed a retrospective cross-sectional study using KNHANES 2008–2010 to investigate the Korean reference values for BMD in 25,043 Korean adults aged 20 and older. They reported that prevalence of osteoporosis in women was lower when using new diagnostic reference data compared with the existing Japanese reference data provided by the manufacturer of the DXA device [24]. Despite this discrepancy, the Japanese reference database for deciding T-score in KNHANES 2008–2010 is used as a formal reference.
In conclusion, dietary sodium intake was negatively associated with the lumbar spine BMC/BMD and increased the risk of osteoporosis in postmenopausal women, indicating that excessive sodium intake might be detrimental to bones in elderly, especially in postmenopausal women. Additional long-term clinical trials are desirable to confirm the effect of high-sodium diet on bone health over time.
References
Klibanski A, Adams-Campbell L, Bassford T et al (2001) Osteoporosis prevention, diagnosis, and therapy. JAMA 285:785–795
Park EJ, Joo IW, Jang MJ, Kim YT, Oh K, Oh HJ (2014) Prevalence of osteoporosis in the Korean population based on Korea National Health and Nutrition Examination Survey (KNHANES), 2008-2011. Yonsei Med J 55:1049–1057
Bonjour JP, Gueguen L, Palacios C, Shearer MJ, Weaver CM (2009) Minerals and vitamins in bone health: the potential value of dietary enhancement. Brit J Nutr 101:1581–1596
Heaney RP (2007) Bone health. Am J Clin Nutr 85:300s–303s
Teucher B, Fairweather-Tait S (2003) Dietary sodium as a risk factor for osteoporosis: where is the evidence? Proc Nutr Soc 62:859–866
Shortt C, Flynn A (1990) Sodium-calcium inter-relationships with specific reference to osteoporosis. Nutr Res Rev 3:101–115
Breslau NA, McGuire JL, Zerwekh JE, Pak CY (1982) The role of dietary sodium on renal excretion and intestinal absorption of calcium and on vitamin D metabolism. J Clin Endocrinol Metab 55:369–373
Zarkadas M, Gougeon-Reyburn R, Marliss EB, Block E, Alton-Mackey M (1989) Sodium chloride supplementation and urinary calcium excretion in postmenopausal women. Am J Clin Nutr 50:1088–1094
Ross PD, Knowlton W (1998) Rapid bone loss is associated with increased levels of biochemical markers. J Bone Miner Res 13:297–302
Garnero P, Sornay-Rendu E, Claustrat B, Delmas PD (2000) Biochemical markers of bone turnover, endogenous hormones and the risk of fractures in postmenopausal women: the OFELY study. J Bone Miner Res 15:1526–1536
Park SM, Joung JY, Cho YY, Sohn SY, Hur KY, Kim JH, Kim SW, Chung JH, Lee MK, Min YK (2015) Effect of high dietary sodium on bone turnover markers and urinary calcium excretion in Korean postmenopausal women with low bone mass. Eur J Clin Nutr 69:361–366
Lin PH, Ginty F, Appel LJ, Aickin M, Bohannon A, Garnero P, Barclay D, Svetkey LP (2003) The DASH diet and sodium reduction improve markers of bone turnover and calcium metabolism in adults. J Nutr 133:3130–3136
Evans CE, Chughtai AY, Blumsohn A, Giles M, Eastell R (1997) The effect of dietary sodium on calcium metabolism in premenopausal and postmenopausal women. Eur J Clin Nutr 51:394–399
Chan AYS, Poon P, Chan ELP, Fung SLM, Swaminathan R (1993) The effect of high sodium-intake on bone-mineral content in rats fed a normal calcium or a low-calcium diet. Osteoporosis Int 3:341–344
Devine A, Criddle RA, Dick IM, Kerr DA, Prince RL (1995) A longitudinal-study of the effect of sodium and calcium intakes on regional bone-density in postmenopausal women. Am J Clin Nutr 62:740–745
Greendale GA, Barrettconnor E, Edelstein S, Ingles S, Haile R (1994) Dietary-sodium and bone-mineral density—results of a 16-year follow-up-study. J Am Geriatr Soc 42:1050–1055
Ilich JZ, Brownbill RA, Coster DC (2010) Higher habitual sodium intake is not detrimental for bones in older women with adequate calcium intake. Eur J Appl Physiol 109:745–755
Carbone L, Johnson KC, Huang Y et al (2016) Sodium intake and osteoporosis. Findings From the Women's Health Initiative J Clin Endocrinol Metab 101:1414–1421
The Division of Chronic Disease Surveillance, Korea Centers for Disease Control and Prevention (2008–2011) The fourth and fifth Korea National Health and Nutrition Examination Survey (KNHANES IV & V)
Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, Chun C, Khang YH, Oh K (2014) Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol 43:69–77
Rural Resource Development Institute (2006) Food composition table, 7th edn. Suwon, Korea
World Health Organization (2012) WHO guideline: sodium intake for adults and children. World Health Organization, Geneva
Kim JE, Lee YH, Huh JH, Kang DR, Rhee Y, Lim SK (2014) Early-stage chronic kidney disease, insulin resistance, and osteoporosis as risk factors of sarcopenia in aged population: the fourth Korea National Health and Nutrition Examination Survey (KNHANES IV), 2008-2009. Osteoporosis Int 25:2189–2198
Lee KS, Bae SH, Lee SH, Lee J, Lee DR (2014) New reference data on bone mineral density and the prevalence of osteoporosis in Korean adults aged 50 years or older: the Korea National Health and Nutrition Examination Survey 2008-2010. J Korean Med Sci 29:1514–1522
Genant HK, Cooper C, Poor G et al (1999) Interim report and recommendations of the World Health Organization task-force for osteoporosis. Osteoporos Int 10:259–264
Saylor J, Friedmann E, Lee HJ (2012) Navigating complex sample analysis using national survey data. Nurs Res 61:231–237
Willett WC, Howe GR, Kushi LH (1997) Adjustment for total energy intake in epidemiologic studies. Am J Clin Nutr 65:1220S–1228S
Greenland S, Pearce N (2015) Statistical foundations for model-based adjustments. Annu Rev Publ Health 36:89–108
Powles J, Fahimi S, Micha R, Khatibzadeh S, Shi P, Ezzati M, Engell RE, Lim SS, Danaei G, Mozaffarian D (2013) Global, regional and national sodium intakes in 1990 and 2010: a systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ 3(12):e003733
Kim SW, Jeon JH, Choi YK, Lee WK, Hwang IR, Kim JG, Lee IK, Park KG (2015) Association of urinary sodium/creatinine ratio with bone mineral density in postmenopausal women: KNHANES 2008-2011. Endocrine 49:791–799
Park Y, Kwon SJ, Ha YC (2016) Association between urinary sodium excretion and bone health in male and female adults. Ann Nutr Metab 68:189–196
Eastell R, Mosekilde L, Hodgson SF, Riggs BL (1990) Proportion of human vertebral body bone that is cancellous. J Bone Miner Res 5:1237–1241
Werner C, Iversen BF, Therkildsen MH (1988) Contribution of the trabecular component to mechanical strength and bone mineral content of the femoral neck. An experimental study on cadaver bones. Scand J Clin Lab Invest 48:457–460
The Korean Nutrition Society (2010) Dietary reference intakes for Koreans. Hanareum, Seoul, pp 337–401
Bedford JL, Barr SI (2011) Higher urinary sodium, a proxy for intake, is associated with increased calcium excretion and lower hip bone density in healthy young women with lower calcium intakes. Nutrients 3:951–961
Carbone LD, Bush AJ, Barrow KD, Kang AH (2003) The relationship of sodium intake to calcium and sodium excretion and bone mineral density of the hip in postmenopausal African-American and Caucasian women. J Bone Miner Metab 21:415–420
Heaney RP (2006) Role of dietary sodium in osteoporosis. J Am Coll Nutr 25:271–276
Shin D, Joh HK, Kim KH, Park SM (2013) Benefits of potassium intake on metabolic syndrome: the fourth Korean National Health and Nutrition Examination Survey (KNHANES IV). Atherosclerosis 230:80–85
Acknowledgements
This work was supported by the Korea Research Foundation (2015R1D1A1A09060823) funded by the Korean Government.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Kwon, SJ., Ha, YC. & Park, Y. High dietary sodium intake is associated with low bone mass in postmenopausal women: Korea National Health and Nutrition Examination Survey, 2008–2011. Osteoporos Int 28, 1445–1452 (2017). https://doi.org/10.1007/s00198-017-3904-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-017-3904-8