Abstract
Based on the calciuric effect of sodium (Na), it has been speculated, although not proven, that higher Na intake might have a detrimental effect on bone health. The objective was to determine the relationship between Na intake (expressed as urinary Na) and bone mineral density/content (BMD/BMC) during a 3-year study. Participants were healthy, postmenopausal, Caucasian women (n = 136 at baseline) with no medications affecting bone. After baseline screening, half were instructed to reduce sodium intake to ~1,500 mg/day (intervention). The other half remained on habitual intake of ~3,000 mg/day (control). All subjects were given calcium and vitamin D supplements to achieve recommended levels. Anthropometries, densitometry, blood and 24-h urine analyses, and dietary and activity records were assessed every 6 months. Data were analyzed as a continuum, irrespective of the initial assignment to a control or intervention group, using random effects regressions with repeated measures analysis of variance to examine changes over time. Results showed that subjects with higher Na intake had higher BMD in the forearm and spine at baseline and all subsequent time-points (p < 0.01). In the forearm, time and higher urinary calcium modified results, producing a curvilinear decrease in BMD (p < 0.01). In the spine, more active individuals had higher BMD at all time-points. We conclude that higher sodium intake, within the range consumed, had a positive effect on some skeletal sites and no adverse effect on bone in women who had adequate calcium and vitamin D intake.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Possible effects of sodium (Na) on bone health have been a point of research in both humans and animals for more than two decades. A positive relationship between urinary Na, reflecting Na intake, and urinary calcium (Ca) excretion in humans and animals has been confirmed in numerous studies (Goulding and Campbell 1983, 1984; Matkovic et al. 1995; Nordin et al. 1993; Saric et al. 2005). Based on this relationship, it was speculated that excess Na intake might decrease bone mineral density (BMD) with possible detrimental effect on bone health. However, there are only two studies that reported negative effects of Na directly on BMD in humans. Nordin and Polley (1987) reported that forearm BMD was negatively correlated with 24-h urinary Na excretion in a cross-sectional study of 440 healthy postmenopausal women. Devine et al. (1995) showed that higher urinary Na resulted in a more rapid bone loss of hip and ankle in postmenopausal women. The latter study, however, was designed to monitor the effect of Ca supplementation and exercise on bone mass. In contrast, Greendale et al. (1994) found a positive relationship between sodium intake and BMD of the ultradistal radius and hip in male and female participants of the Rancho Bernardo study (an on-going Californian study started in 1972 examining life style and nutritional parameters in relation to various health outcomes in several thousand adults), although, after adjusting for confounders, the statistical significance disappeared in women, but remained in men at the ultradistal radius. The results from numerous other studies did not show any direct relationship between Na intake/urinary excretion and BMD as an outcome, but did show higher urinary Ca excretion with higher urinary Na (Carbone et al. 2005; Dawson-Hughes et al. 1996; Matkovic et al. 1995).
Based on the literature reviews conducted throughout the past decade and by several authors, the relationship still remains unclear and the overall conclusion is that the current knowledge about the role of Na in bone health is meager and conflicting (Burger et al. 1998; Cashman and Flynn 2003; Cohen and Roe 2000; Teucher and Fairweather-Tait 2003). In his review, Heaney concluded that: “At calcium intakes at or above currently recommended levels, there appear to be no deleterious effects of prevailing salt intakes on bone or the calcium economy …” (Heaney 2006). Recently, some authors (Heer et al. 2009; Frings-Meuthem et al. 2008; Frassetto et al. 2008) revisited the issue and argued that a typical Western diet, high in sodium and low in potassium with its net acid production, causes chronic low-grade metabolic acidosis and as such may contribute to increased osteoclastic activity and bone loss. Those studies, however, were also of a short duration and therefore not able to examine any changes in BMD as an outcome measure.
Well-designed, prospective studies in humans examining the effect of Na intake on BMD or fracture risks to clarify the possible influence of Na on bone have not been conducted probably because of several difficulties: (a) an inability to obtain a wide enough range in Na intakes among subjects—it would not be feasible from an ethical or health perspective to supplement subjects with sodium; (b) the need for a relatively long duration of the study in order to observe changes in bone over time; (c) the need for the 24-h urine collections to assess Na intake, since dietary records and their analyses are unreliable; (d) the need for frequent and extensive evaluation of study subjects to control for other confounders, since the effect of Na could be easily masked by other more powerful factors (medications, diuretics).
In view of the above, a longitudinal study in Caucasian, postmenopausal women was conducted to determine whether those with higher habitual Na intake will lose more bone mass in different skeletal sites compared to those who were instructed to reduce their Na intake and maintain it at a lower level. Other factors potentially affecting bone mass (anthropometries, body compositions, blood and urine parameters, nutrition, life style, physical activity) were evaluated and accounted for in the analyses. To our knowledge, this is the only long-term study in postmenopausal women designed specifically to examine the effect of Na on BMD at various skeletal sites.
Materials and methods
The study was advertised through local newspapers and community and senior centers. The interested participants were screened for eligibility over the phone and evaluated for general health, physical functioning and cognitive abilities. Several hundred (n = 428) women were contacted to select 136 who met all criteria and were willing to participate in the study. The selected subjects were 5 years or more postmenopausal, able to live independently, current non-smokers, free of any chronic disease (kidney stones, hypertension, diabetes, severe osteoporosis, cancer) and not taking diuretics and medications known to affect bone metabolism, including but not limited to estrogen, bisphosphonates, and corticosteroids, as described previously (Ilich and Brownbill 2008). The enrollment was staggered through 2 years, but each participant was followed-up for 3 years. The protocol was approved by the University of Connecticut Institutional Review Board and each participant signed the informed consent. Figure 1 presents the flow chart of the design and variables measured.
Anthropometry and bone densitometry
Weight and standing stature were recorded in kg and cm, respectively, with subjects in normal indoor clothing without shoes, and body mass index (BMI) (kg/m2) was calculated. Each participant had her total body, non-dominant forearm (ultradistal and proximal sites of ulna and radius), spine (antero-posterior) and non-dominant femur (neck, trochanter, Ward’s triangle, shaft, and total) measured by dual energy X-ray absorptiometry (DXA) with a Lunar DPX-MD densitometer (GE Medical Systems, Madison, WI) using specialized software for each skeletal site. The total body scan also yielded an analysis of soft tissue (fat and lean), used as a confounder in analyses. The bone densitometer was calibrated daily. Long-term stability was monitored by measuring an aluminum spine phantom on a weekly basis, with a resulting average coefficient of variation (CV) of 0.45% for the entire study period. The measurements did not show drift during the study period, with an average BMD of 1.256 ± 0.01 g/cm2, ranging from 1.244 to 1.274 g/cm2. The %CV of BMD for different skeletal sites in vivo was calculated from the repeated measurements (5 times each) on five normal women, comparable to the study subjects. The %CV for the BMD of various skeletal sites was as follows: forearm (radius and ulna pooled together at 1/3 distance from styloid process), 0.7%: lumbar spine (L2–L4), 1.0%; femoral neck, 1.5%; Ward’s triangle, 1.5%; femoral shaft, 0.7%; trochanter, 0.9%; and total hip, 0.6%. The %CVs were comparable with the manufacturer’s values, indicating acceptable precision of the instrument (Ilich et al. 2000).
Dietary and physical activity assessment
The subjects completed a 3-day dietary record (2 weekdays and 1 weekend day), upon entering the study, and then every 3–6 months. Each subject was thoroughly and individually instructed how to complete the records by a registered dietitian (Ilich et al. 2003). Nutrient intake from the record was analyzed with Food Processor® (ESHA Research, Salem, OR), by the same dietitian, and the mean daily intake was calculated for energy and all other macro and micro-nutrients, as well as caffeine and alcohol consumption. The supplemental intake of vitamins and minerals was carefully recorded as well, and included in the total nutrient analysis, as described previously (Ilich et al. 2003). All subjects were given Ca (~630 mg/day) and vitamin D (~400 IU/day) supplements throughout the study (Citracal®, Mission Pharmacal, San Antonio, TX). If a subject was taking Ca and vitamin D supplements before entering the study, she was asked to replace them with Citracal®.
Physical activity was assessed using interview format with a modified version of the Allied Dunbar National Fitness Survey (Fenton et al. 1994; Ilich and Brownbill 2008). Subjects were asked about participation in recreational and sport activities of at least 4 kcal/min (intensity likely to produce health benefit) as well as about performing heavy housework, home improvement, gardening and walking (distances of at least 1 mile). Each activity was assessed for frequency and duration and expressed in hours/week based on the average of the previous 4 weeks. Total activity score was calculated as well (Ilich and Brownbill 2008; Ilich-Ernst et al. 2002).
Intervention for reduction of sodium intake and subjects’ compliance
After the initial screening, half of the randomly assigned subjects were instructed to reduce Na intake to approximately 1,500 mg/day (3.8 g salt). The randomization was performed by systematically arranging intervention and control codes, assigning to each code a random number and then sorting by the random number column. The subjects in the control group remained on their usual Na intake (~3,000 mg/day). The instructions on how to reduce sodium, along with the educational material, brochures, diet plans, food lists, recipes, and tips were delivered to participants on an individual basis (by a registered dietitian) at the first visit and then reinforced at each subsequent visit. In-between the visits, subjects were followed-up by frequent telephone calls and mailings of new recipes and information. All instructions were aimed to facilitate reduction in Na without altering intake of other nutrients. Records of intake and interviews about the adherence to the protocol were conducted every 3 months in the first year and then every 6 months thereafter. A similar schedule was followed for the biological check, alternating between spot and 24-h urine sample analyses of Na. The compliance in the control group was assessed in the same way/intervals. With time, some of the participants in the control group reduced their Na intake and those in the intervention group did not comply well in reducing their Na intake. Therefore, the final analyses were conducted on the continuum of intake, regardless of which group each subject was initially assigned to. However, additional calculation based on the intention-to-treat was performed as well. Compliance with Ca supplementation in all subjects was calculated from the returned pills.
Clinical chemistry
Blood and 24-h urine samples were obtained every 6 months. Serum was analyzed for total Ca, magnesium (Mg), phosphorus (P), proteins, creatinine (Cr), alkaline phosphatase and electrolytes (Na, potassium, chloride), all measured by automated procedures (Quest Diagnostics, Wallingford, CT). Remaining samples were stored at −80°C and later analyzed for markers of bone turnover, osteocalcin (OC) and undercarboxylated osteocalcin (UOC) by ELISA (Biomedical Technologies, Inc, Stoughton, MA) in the General Clinical Research Center at the University of Connecticut Health Center. Vitamin D (25 hydroxy) and parathyroid hormone (PTH) were analyzed by Allegro immunoassay, both by Nichols Institute (San Juan, Capistrano, CA) at baseline, 6 and 12 months only.
Special attention was paid to the 24-h urine collections, since urinary Na determined from the sample served as an estimate for dietary Na (in addition to the spot urine analysis in alternate visits). Each participant received written instructions and was individually taught how to collect the urine. Because the compliance was self-reported, urinary Cr was also used to screen for possible errors and incomplete collections. The samples were collected in the previously distributed containers without additives and subjects were instructed to keep containers in a refrigerator during collection. Upon return, the total volume was measured and the sample routinely analyzed by chemstrips for basic parameters (e.g. glucose, protein, pH etc.). Thereafter, the samples were divided in aliquots and analyzed for Ca, Na, Mg, potassium, P, and normalized by Cr (Quest Diagnostics). The remaining samples were stored at −20°C and later analyzed at GCRC for urinary cross-linked N-telopeptides of mature type I collagen (NTx), using ELISA (Ostex, Seattle, WA).
Data analysis
Analyses were performed with the SAS (Version 8.2, SAS Institute, Cary, NC) statistical software and Data-Desk® (Data Desk Description, Inc., Ithaca, NY). Overall, statistical significance was declared if p ≤ 0.05. After checking normality assumptions, preliminary analyses were conducted by developing multiple regression models with either BMD or BMC as dependent variable and urinary Na/Cr and Ca/Cr as explanatory variables. Potential confounders typically included age, BMI or lean/fat tissue, dietary Ca, energy and/or protein intake, urinary potassium or phosphorus, and various measures of physical activity. Additionally, all follow-up bone measurements were calculated as a percent change from baseline. The intention-to-treat approach was utilized first, to evaluate the effect of Na on BMD/BMC irrespective of compliance or drop-outs. In that regard, average cumulative values for all variables of interest were calculated by summing the available values from all time-points (baseline, 6, 12, 18, 24, 30, and 36 months). However, as it has already been established in clinical trials, when compliance declines (either due to drop-out or poor adherence to protocol), treatment effect decreases, regardless of its efficacy (Everitt and Pickles 1999). Therefore, a more comprehensive analysis for longitudinal studies (random effects regression models incorporating repeated measures and accounting for the missing data) was utilized to examine the change in BMD across time, and to determine the most significant predictors.
Analysis strategy overview
All models were fitted using four BMD (and/or BMC) outcomes: composite BMD of femur (neck, trochanter, Ward’s triangle, shaft), forearm (including radius and ulna at both ultradistal and 1/3 proximal site), L2–L4 lumbar spine and total body. In addition, separate analyses were conducted for the femoral neck BMD/BMC, due to its importance in the osteoporosis diagnosis and susceptibility to fracture. To examine the BMD change over time, several multilevel models were estimated (Lindenberger and Ghisletta 2004; Rogosa and Saner 1995): unconditional means models for each outcome; unconditional growth models; and time-variant and time-invariant predictors were added to the model. For each outcome variable, a separate model was estimated for each of the following time-variant predictors: BMI, fat and lean tissue, physical activity, urinary and dietary calcium, vitamin D, energy, protein, and potassium intakes, alcohol and caffeine consumed, and the time-invariant predictor, age. In each of these models, two time effects were estimated as random effects: time-linear and time-non-linear. Additionally, the following random effects were also estimated: the main effect of the covariate of interest, the interaction between the covariate and non-linear and linear time, the main effects of each time term, the main effect of urinary and dietary sodium, as well as the two-way interactions between each of the time terms and each sodium measure (resulting in 4 parameters). Subsequently, model trimming was performed by estimating a separate model that included only the significant covariate measures (the main effect of the covariate, the interaction with the covariate with time, or both) and the main effects of time, and sodium (both urinary and dietary). Lastly, a final trimmed model was estimated for each of the outcomes that only included the significant random effects from the previous model, along with the two fixed effects of time-linear and time-non-linear.
Results
Descriptive characteristics with anthropometries and bone variables at baseline for all subjects (n = 136), those who stayed in the study for 36 months (n = 97), and those who dropped out at various time-points (n = 39) are presented in Table 1. Table 2 shows nutritional, serum, and 24-h urine variables presented in the same manner. At baseline, there was no statistical difference in any of the variables between initially assigned intervention (reduced Na) and control (maintenance of Na intake) groups. Measures of physical activity at baseline expressed as hours/week were heavy housework, gardening, walking, recreation/sports and total activity score: 2.1 ± 4.3, 1.0 ± 2.2, 1.4 ± 1.7, 1.0 ± 1.8, 5.6 ± 5.6 h/week (mean ± SD), respectively. In comparing the variables at baseline between subjects who stayed and those who dropped out, only age, total body BMC and urinary Ca/Cr were statistically different by two-sample t test. Additionally, dichotomous variables coding missing and non-missing cases were created for all variables used. The calculated correlations resulted in near-1 values and the cross-tabulations showed that the missing cases increased “uniformly” with the study progression, indicating no particular bias in the drop-out. The drop-out percent (number of subjects) was 8.8% (n = 12), 5.6% (n = 7), 8.5% (n = 10), 0.9% (n = 1), 7.5% (n = 8), and 1.0% (n = 1) at 6, 12, 18, 24, 30, and 36 months of evaluation, respectively, with the overall drop-out rate in 3 years of 28.7% (n = 39), with 97 subject finishing the study. The reasons for drop-out ranged from the lost interest (n = 27), changes in family situation and moving (n = 6), to developing chronic conditions (heart disease, n = 2), starting medication affecting bone metabolism (n = 3), or death (n = 1).
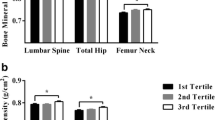
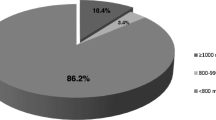
Average calcium intake was adequate throughout the study. Apart from food sources, Ca also originated from various multi-mineral/vitamin supplements as well as from Ca citrate administered in the study, except at the baseline when it originated from any other commercial Ca supplement (typically Ca carbonate). Dietary intake was between 800 and 900 mg/day at each assessment, but together with supplements it ranged from 1,300 to 1,500 mg/day. The average compliance with Ca supplements administered in the study was calculated by counting the returned pills every 6 months and it was: 93.7, 93.5, 93.7, 92.9, 93.7, and 94.1% for 6, 12, 18, 24, 30, and 36 months evaluations, respectively. Figure 2 presents tertiles of 24-h urinary Na/Cr excretion at each time-point, and Fig. 3 presents urinary Ca/Cr excretion according to the tertiles of urinary Na/Cr. It should be noticed that higher urinary Na/Cr was associated with higher urinary Ca/Cr at each time-point, but the statistical significance was reached only at baseline, 24 and 36 months.
Table 3 shows results from multiple regression models created with bone outcomes assessed at 36 months as dependent variables and cumulative averages over 36 months for urinary Na/Cr and Ca/Cr (as explanatory variables), and age, cumulative BMI and/or body fat or lean tissue, cumulative dietary Ca, energy or protein, and modes of cumulative physical activity as confounders. Urinary Ca/Cr was negatively and urinary Na/Cr was positively associated with BMD/BMC of various skeletal sites.
There was no statistical difference in mean BMD of the forearm (F = 0.661, p = 0.417), hip (F = 0.679, p = 0.411) or spine (F = 0.154, p = 0.695) between baseline and 36 months (univariate ANOVA) indicating that, on average, no appreciable amount of bone had been lost over 3 years. No appreciable loss of BMD of various skeletal sites was observed when %change between baseline and 36 months was calculated using the entire study population. The results from random effects regression, utilized to assess both linear and non-linear trends over time with covariates of interest and BMD at various skeletal sites, are described below (results with BMC showed similar trends, not presented).
Forearm analysis
A main effect of non-linear time indicated that individuals’ forearm BMD decreased non-linearly, t = −2.41, p = 0.0176. A main effect of urinary Na indicated that higher urinary Na was associated with higher forearm BMD at baseline and subsequent time-points, t = 2.63, p = 0.0089. As expected, a main effect of age indicated that across time, older individuals had less dense bones than younger individuals, t = −3.51, p = 0.0005. An interaction between non-linear time and urinary Ca indicated that radius BMD decreased non-linearly across time, t = −2.69, p = 0.0074, in a group with higher urinary Ca excretion (Fig. 4). Similar effects were obtained when the whole forearm was included (both ulna and radius at proximal and ultradistal sites, data not presented).
The effects of age, urinary sodium (Na), as a measure of Na intake, and urinary calcium (Ca) on forearm (1/3 proximal radius) bone mineral density (BMD) across time in younger (grand mean centered to 60 years, top) and older (grand mean centered to 80 years, bottom) subjects. Graphing strategy: For each figure, a set of equations was created by writing out the full regression equation for the final models, and using all combinations of high and low values of variables for the significant effects. Specifically, separate equations were computed by multiplying high and low (1SD above and below the mean) values of each variable of interest (e.g., urinary Na, Ca) by the effect estimate for that particular effect (e.g., main effect of Na on BMD). Separate equations were computed to examine the full spectrum of relationships between variables that the data predict. The generic form of these equations is: BMD = intercept + effect estimate [high or low value (±1SD)] + effect 2 [high or low value (±1SD)] + effect 3 [high or low value (±1SD)]
Spine (L2–L4) analysis
Consistent with the forearm results, a main effect was found for urinary Na, t = 3.02, p = 0.0027. At any given time-point, individuals with higher urinary Na had higher spine BMD. In addition, a main effect for total activity score indicated that at any given time-point, more active individuals had higher spine BMD, t = 2.10, p = 0.0366 (Fig. 5).
The effect of urinary sodium (Na), as a measure of Na intake, and total physical activity on lumbar spine (L2–L4) bone mineral density (BMD) across time. Visually, it appears that BMD increases with time; however, the time effect here is “washed out” by the dominant effect of urinary Na and physical activity. The regression slope in subjects with higher urinary Na and physical activity is less negative
Femur (neck, Ward’s triangle, shaft, trochanter) analysis
A main effect of non-linear time indicated that femoral BMD decreased non-linearly, t = −2.73, p = 0.0073. Consistent with results for the forearm (and not surprisingly), a main effect of age indicated that across time, older individuals had less dense bones than younger individuals, t = −3.08, p = 0.0022. A main effect of BMI indicated that the higher the BMI at any given time-point, the higher the BMD, t = 5.33, p < 0.0001. BMI also interacted with linear time indicating that the BMD of individuals with higher BMI decreased at a slower rate than those with lower BMI, t = 2.32, p = 0.0208. A main effect for lean tissue indicated that higher values of lean tissue were associated with higher BMD at any given time-point, t = 3.31, p = 0.0010, in a similar manner as BMI. There was no effect of sodium on femoral BMD. Separate analyses for femoral neck only showed similar trends but with the lower statistical significance. There was also no relationship with sodium (data not presented).
Total body analysis
The unconditional growth model for total body BMD did not converge, indicating that there was no between-person variability; therefore, this model was not pursued further.
All three markers of bone turnover were significantly and positively related to each other at baseline and in subsequent evaluations. Both OC and UOC were significant negative predictors of BMD at total body, hip and forearm sites at some time-points, while at 24-month, OC was significantly higher in subjects with higher urinary Na (Ilich et al. 2004, Abstr). However, each of those analyses was done on a cross-sectional basis and the noted results were sporadic throughout the time-points rather than consistent. When multiple regressions were created at 36 months for BMD of the noted skeletal sites as dependent variables and cumulative average values of bone markers and other confounders, none of the markers showed any significant relationship with BMD. Similarly, in the random effects regression analysis, bone markers did not show any effect on BMD nor did an interaction with Na exist. Serum vitamin D(25 hydroxy) and PTH, measured only in the first year, were not related with urinary Na/Cr and did not have any relationship with BMD/BMC, as reported earlier (Ilich et al. 2002, Abstr).
Discussion
To the best of our knowledge, this is the first and only long-term study that was specifically designed to monitor the effect of dietary Na (expressed as urinary Na) on BMD/BMC in healthy postmenopausal women. By utilizing repeated measures mixed models, it was shown that subjects with higher Na intake had higher BMD in forearm and spine, starting already at baseline and at any subsequent evaluation time-point. There was no effect of Na on total body or femoral BMD. These results are surprising in view of the evidence that higher sodium intake promotes higher urinary Ca excretion and speculations that it might compromise bone status, particularly in elderly. These results also do not support the initial hypothesis that higher sodium intake will lead to higher bone loss.
Average sodium intake in the entire population (and when distributed according to the initial group assignment) was above the current recommendations of 1,500 mg/day for this population (Institute of Medicine 2004), with the baseline average urinary Na/Cr of 2,465 ± 903 mg/gCr, ranging from 560 to 5,308 mg/gCr (Table 2) and cumulative average throughout the study of 2,448 ± 680 mg/gCr, ranging from 1,138 to 4,896 mg/gCr. After baseline, subjects typically achieved a difference in urinary Na/Cr between 1,500 and 3,000 mg/gCr at various time-points (Fig. 2). There was also a weak positive correlation between urinary Na and urinary Ca throughout the study, indicating that higher Na exerted higher urinary Ca excretion, although a statistically significant difference was not achieved at all of the time-points. Therefore, the difference in Na intake/urinary excretion among subjects was large enough to cause the difference in urinary Ca, and subsequently any possible effect on BMD based on the “urinary Ca excretion hypothesis”, but this hypothesis was not supported. It is important to note that all subjects had adequate Ca intake. Therefore, it cannot be speculated whether the same results would have been obtained in subjects with inadequate Ca intake and/or higher Na intake.
Results from some animal studies (usually in rats) showed negative effects of Na on bone (Goulding and Campbell 1983, 1984), mostly in the conditions of low Ca intake and high Na loads. However, regarding Na–bone relationships, studies in rats are not an adequate comparison to studies in humans since animals are typically given much higher loads of Na (up to 12 times more than recommended). Also, rats excrete only about 1% of ingested Ca while humans excrete ~16%. Rats also have limited capacity for bone modeling and have different responses to other dietary factors (e.g. protein, phosphorus) (Shortt and Flynn 1990).
Other, indirect evidence of the Na–bone relationship comes from short-term interventional studies and measurements of markers of bone turnover after Na loading or restriction. Some older studies showed an increase in hydroxyproline with sodium loading (Need et al. 1991), while others were inconclusive (Cirillo et al. 1997). Evans et al. (1997) reported that postmenopausal, but not premenopausal women, responded to 1 week of high Na intake (6,900 mg/day) after 1 week of low-Na intake (1,150 mg/day), with an increase in deoxypyridinoline, while Ca absorption did not change. The results from studies by Ginty et al. (1998) in young and by Lietz et al. (1997) in older women examining the effects of low/high Na on bone markers were inconclusive. A 7-week reduction in salt in young men and women with adequate Ca intake did not affect any of the bone metabolism markers (Natri et al. 2005). The above studies might have been too acute or too short to simulate free-living conditions or to allow for normal physiological adaptation.
Carbone et al. (2005) reported the results from a 6-month intervention with low-Na diet (2 g/day) in 40 postmenopausal Caucasian and African-American women. They found decreased activity of a bone formation marker, aminoterminal propeptide of type I collagen, in subjects who followed a low-Na diet (after baseline Na intake of ≥3.4 g/day). Bone markers in the present study did not provide any appreciable insight into the relationship between Na and bone turnover.
The connection between urinary Ca and Na excretion stems from their competition for reabsorption in the proximal tubule and ascending loop-of-Henle (Nordin et al. 1993). Theoretically, hypercalciuria induced by Na might cause a slight decrease in serum ionized Ca which triggers a PTH–vitamin D (calcitriol) response leading to possible increased intestinal Ca absorption to compensate for the urinary Ca loss. This was shown to occur in young subjects (Breslau et al. 1982), but not in older osteoporotic women (Breslau et al. 1985) and not in healthy men and women age 18–65 years (Cirillo et al. 1997). Elevated PTH might also decrease fecal Ca loss by preserving endogenous Ca and increase renal Ca reabsorption (Shortt and Flynn 1990).
As reviewed by Cashman and Flynn (2003), serum PTH was significantly increased in relation to Na-induced calciuria in studies where the level of Na intake was within the physiological range (2,300–6,900 mg/day). However, the increment in PTH change varied between the studies even with the same increment in Na load. This is reasonable to expect due to difficulties in measuring various PTH fragments in serum. On a cellular level, intermittent administration of PTH promotes recruitment of preosteoblasts and maturation of lining osteoblasts, both of which promote collagen synthesis and bone formation, see review (Rubin and Bilezikian 2003). Consequently, the low-dose-intermittent administration of PTH (teriparatide) is used as the newest treatment of osteoporosis.
In view of the above, it could be postulated that with higher Na intake in part of the population (and adequate Ca intake), the Na-induced calciuric effect is such as to cause a mild elevation of PTH on an intermittent basis in response to the particular ingestion of salt. As a result, the effect produced is similar to that created by low-dose-intermittent administration of PTH (as via teriparatide). Obviously, the effect with Na is very subtle and not easily recognizable and could be masked by other more dominant biological and dietary influences. This might explain why subjects with habitually higher urinary Na had higher BMD/BMC, even at baseline, than those with habitually lower Na intake. Supplementation with Ca prevented bone loss in both groups.
It could be argued that the manipulation with Na intake might lead to changes in other nutrients, particularly energy. Some researchers showed that sodium restriction could be achieved without altering the intake of other nutrients (Korhonen et al. 2000), particularly in situations where subjects are under close monitoring and counseled by a registered dietitian, as in the present study. Among the subjects, only the intake of potassium increased slightly (Ilich and Brownbill 2004, Abstr), but potassium intake/urinary excretion was accounted for in the analyses. The subjects were supplemented with Ca and vitamin D and, on average, had adequate intakes of both. It is possible that this supplementation suppressed bone turnover leading to bone remodeling transient (Heaney 1994) and caused a slight increase in measurable BMD. It could be speculated that this effect might have masked and/or overridden the calciuric effect of Na, although it is unlikely to persist over 3 years. Moreover, the same effect would have been expected in subjects with lower Na intake, yet, they presented with lower BMD/BMC.
In conclusion, the results from this longitudinal study designed to evaluate the Na–bone relationship show that higher Na intake (within the reported range) was positively associated with forearm and spine BMD in this population of otherwise healthy and well-nourished Caucasian elderly women. No adverse effect of higher sodium intake was noted in any of the other skeletal sites. These results are in contrast to previous findings and the not proven speculation that Na, due to its calciuric effect, might adversely impact bone health. Considering the length and complexity of this study, specific design and inclusion of numerous confounders, it is reasonable to expect that these findings will move the long-standing debate about sodium intake and bones in postmenopausal women to the point suggesting that moderately high sodium and adequate Ca intake does not result in decreased BMD/BMC.
References
Breslau NA, McGuire JL, Zerwekh JE, Pak CY (1982) The role of dietary sodium on renal excretion and intestinal absorption of calcium and on vitamin D metabolism. J Clin Endocrinol Metab 55:369–373
Breslau NA, Sakhaee K, Pak CYC (1985) Impaired adaptation to salt-induced urinary calcium losses in postmenopausal osteoporosis. Trans Assoc Am Phys 98:107–115
Burger H, de Laet CE, van Daele PL et al (1998) Risk factors for increased bone loss in an elderly population: the Rotterdam Study. Am J Epidemiol 147:871–879
Carbone LD, Barrow KD, Bush AJ et al (2005) Effects of low sodium diet on bone metabolism. J Bone Miner Metab 23:506–513
Cashman KD, Flynn A (2003) Sodium effects on bone and calcium metabolism. In: New SA, Bonjour JP (eds) Nutritional aspects of bone health. Royal Society of Chemistry, Cambridge (CB), pp 267–289
Cirillo M, Ciacci C, Laurenzi M, Mellone M, Mozzacca G, De Santo NG (1997) Salt intake, urinary sodium and hypercalciuria. Miner Electrolyte Metab 23:265–268
Cohen AJ, Roe FJC (2000) Review of risk factors for osteoporosis with particular reference to a possible etiological role of dietary salt. Food Chem Toxicol 38:237–253
Dawson-Hughes B, Fowler SE, Dalsky G, Gallagher C (1996) Sodium excretion influences calcium homeostasis in elderly men and women. J Nutr 126:2107–2112
Devine A, Criddle RA, Dick IM, Kerr DA, Prince RL (1995) A longitudinal study of the effect of sodium and calcium intakes on regional bone density in postmenopausal women. Am J Clin Nutr 62:740–745
Evans CEL, Chughtai AY, Blumsohn A, Giles M, Eastell R (1997) The effect of dietary sodium on calcium metabolism in premenopausal and postmenopausal women. Eur J Clin Nutr 51:394–399
Everitt BS, Pickles A (1999) Statistical aspect of the design and analysis of clinical trials. Imperial College Press, London
Fenton PH, Collins MF, Tuxworth W et al (1994) Health education authority of London Sports Council. The Allied Dunbar National Fitness Survey Technical Report. Sports Council and Health Education Authority, London
Frassetto LA, Morris CR Jr, Sellmeyer DE, Sebastian A (2008) Adverse effects of sodium chloride on bone in the aging human population resulting from habitual consumption of typical American Diets. J Nutr 138:419S–422S
Frings-Meuthem P, Baecker N, Heer M (2008) Low grade metabolic acidosis may be the cause of sodium chloride-induced exaggerated bone resorption. J Bone Miner Res 23:517–524
Ginty F, Flynn A, Cashman KD (1998) The effect of dietary sodium intake on biochemical markers of bone metabolism in young women. Br J Nutr 79:343–347
Goulding A, Campbell DR (1983) Dietary NaCl loads promote calciuria and bone loss in adult oophorectomized rats consuming a low calcium diet. J Nutr 113:1409–1414
Goulding A, Campbell DR (1984) Effects of oral loads of sodium chloride on bone composition in growing rats consuming ample dietary calcium. Miner Electrolyte Metab 10:58–62
Greendale GA, Barret-Connor EL, Edelstein S, Ingles S, Haile R (1994) Dietary sodium and bone mineral density: results of a 16-year follow-up study. J Am Geriatr Soc 42:1050–1055
Heaney RP (1994) The bone-remodeling transient: implications for the interpretation of clinical studies of bone mass change. J Bone Miner Res 9:1515–1523
Heaney RP (2006) Role of dietary sodium in osteoporosis. J Am Coll Nutr 25:271S–276S
Heer M, Frings-Meuthem P, Titze J, Boschmann M, Frish S, Baecker N, Beck L (2009) Increasing sodium intake from a previous low or high intake affects water, electrolyte and acid-base balance differently. Br J Nutr 101:1286–1294
Ilich JZ, Brownbill RA (2004) Effects of sodium restriction on intake of other nutrients in older women: a 2-year follow-up. FASEB J 18:A883 (Abstr)
Ilich JZ, Brownbill RA (2008) Habitual and low-impact activities are associated with better bone outcomes and lower body fat in older women. Calc Tissue Int 83:260–271
Ilich JZ, Zito M, Brownbill RA, Joyce ME (2000) Change in bone mass after Colles’ fracture: a case report of unique data collection and long-term implications. J Clin Densitom 3:383–389
Ilich JZ, Brownbill RA, Mulrenan HE, Tamborini L (2002) Tracking serum 25 hydroxy vitamin D (25-OHD) and parathyroid hormone (PTH) in healthy elderly women over a 1-year period. Calc Tissue Int 70:276 (Abstr)
Ilich JZ, Brownbill RA, Tamborini L (2003) Bone and nutrition in elderly women: protein, energy, and calcium as main determinants of bone mineral density. Eur J Clin Nutr 57:554–565
Ilich JZ, Brownbill RA, Fall PM (2004) Osteocalcin in relation to bone mass and sodium intake in postmenopausal women. Calc Tissue Int 74:S68 (Abstr)
Ilich-Ernst JZ, Brownbill RA, Ludemann MA, Fu R (2002) Critical factors for bone health in women across the age span: How important is muscle mass? Medscape Women’s Health, eJournal 7(3). Available at: http://www.medscape.com/viewarticle/432910
Institute of Medicine (2004) Dietary reference intakes for water, potassium, sodium, chloride and sulfur. National Academy Press, Washington, DC
Korhonen MH, Jarvinen RMK, Sarkkinen ES, Uusitupa MIJ (2000) Effects of salt-restricted diet on the intake of other nutrients. Am J Clin Nutr 72:414–420
Lietz G, Avenell A, Robins SP (1997) Short-term effects of dietary sodium intake on bone metabolism in postmenopausal women measured using urinary deoxypyridinoline excretion. Br J Nutr 78:73–82
Lindenberger U, Ghisletta P (2004) Modeling longitudinal changes in old age: from co-variance structures to dynamic systems. In: Dixon R, Backman L, Nilsson L-G (eds) New frontiers in cognitive aging. Oxford University Press, Oxford, UK, pp 199–216
Matkovic V, Ilich JZ, Andon MB et al (1995) Urinary calcium, sodium, and bone mass of young females. Am J Clin Nutr 62:417–425
Natri A-M, Karkkainen MUM, Ruusunen M, Puolanne E, Lamberg-Allardt C (2005) A 7-week reduction in salt intake does not contribute to markers of bone metabolism in young healthy subjects. Eur J Clin Nutr 59:311–317
Need AG, Morris HA, Cleghorn DB, DeNichilo D, Horowitz M, Nordin BEC (1991) Effect of salt restriction on urine hydroxyproline excretion in postmenopausal women. Arch Intern Med 151:757–765
Nordin BEC, Polley KJ (1987) Metabolic consequences of the menopause. A cross-sectional, longitudinal and intervention study on 557 normal postmenopausal women. Calcif Tissue Int 41:S1–S59
Nordin BEC, Need A, Morris HA, Horowitz M (1993) The nature and significance of the relationship between urinary sodium and urinary calcium in women. J Nutr 123:1615–1622
Rogosa D, Saner H (1995) Longitudinal data analysis examples with random coefficient models. J Educ Behav Stat 20:149–170
Rubin MR, Bilezikian JP (2003) New anabolic therapies in osteoporosis. Endocrinol Metab Clin N Am 32:285–307
Saric M, Piasek M, Blanusa M, Kostial K, Ilich JZ (2005) Sodium and calcium intake and bone mass in rats revisited. Nutrition 21:609–614
Shortt C, Flynn A (1990) Sodium–calcium interrelationship with specific reference to osteoporosis. Nutr Res Rev 3:101–115
Teucher B, Fairweather-Tait (2003) Dietary sodium as a risk for osteoporosis: where is the evidence. Proc Nutr Soc 62:859–866
Acknowledgments
The authors are thankful to all women who participated in the study. The authors appreciate statistical consultations by Antonius H.N. Cillessen. Funded in part by the NRI/USDA 2001-00836, Donaghue Medical Research Foundation DF98-056, University of Connecticut Office for Sponsored Programs and Bayer HealthCare LLC, Morristown, NJ, USA. The experiments comply with the current laws of the US and were approved by the Institutional Review Board.
Conflict of interest statement
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Susan Ward.
Rights and permissions
About this article
Cite this article
Ilich, J.Z., Brownbill, R.A. & Coster, D.C. Higher habitual sodium intake is not detrimental for bones in older women with adequate calcium intake. Eur J Appl Physiol 109, 745–755 (2010). https://doi.org/10.1007/s00421-010-1412-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-010-1412-z