Abstract
Summary
Many previous studies have reported excellent clinical results with percutaneous kyphoplasty (PKP). In contrast, numerous complications and problems have also been reported, such as puncture difficulty, cement leakage, and adjacent vertebral fracture.
Introduction
This study is to evaluate the application and clinical outcomes of unilateral transverse process-pedicle and bilateral PKP in the treatment of osteoporotic vertebral compression fractures (OVCF).
Methods
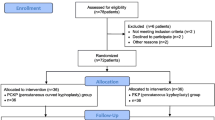
A total of 56 cases with two levels thoracolumbar OVCF were randomly assigned for treatment with unilateral transverse process-pedicle and bilateral PKP. The patients were followed up postoperatively and were assessed mainly with regard to clinical and radiologic outcomes. Clinical outcomes were evaluated with mainly the use of a visual analogue scale (VAS) for pain. Radiologic outcomes were assessed mainly on the basis of radiation dose and bone cement distribution.
Results
The operation was completed successfully in 56 cases. In the unilateral level, the operation time, the volume of the injected cement, and radiation dose were significantly less than bilateral level. All patients had significantly improvement on VAS score after the procedures, compared with their preoperative period. In the bilateral level, 7 patients had obvious pain in the puncture sites at 1 month postoperatively caused by facet joint violation. With local block treatment, the pain disappeared in all patients at the last follow-up.
Conclusion
Both bilateral and unilateral PKP are relatively safe and effective treatments for patients with painful OVCF. But unilateral PKP received less radiation dose and operation time, offered a higher degree of deformity correction, and resulted in less complication than bilateral.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Vertebral fractures complicating osteoporosis are the most common forms of osteoporotic fracture [1]. Osteoporotic vertebral compression fractures (OVCF) are frequent in women older than 60 years and may result in debilitating pain and spinal deformity. Because of increasing of population’s age and severe morbidity due to these fractures, painful vertebral fractures are a growing serious public health problem with important socio-economic effects. Although two third of them gradually improves with conservative treatment, intractable pain, decreased self-esteem, senile kyphosis, early satiety, mood disorder, and even increased mortality have been frequently reported [2–4]. Today, percutaneous kyphoplasty (PKP) is a widely used vertebral augmentation procedure for treating painful vertebral compression fractures. A percutaneous bilateral approach is typically used to access the vertebral body. Low viscosity cement is required to overcome injection resistance and achieve interdigitation with the bone, providing biomechanical stabilization. Many previous studies have reported excellent clinical results with PKP. In contrast, numerous complications and problems have also been reported, such as puncture difficulty, cement leakage, and adjacent vertebral fracture [5–8].
The present study used a prospective, self-controlled study to compare clinical results and changes in the injected cement as well as the radiographic results between unilateral transverse process-pedicle approach and bilateral traditional approach in application of PKP.
Methods
The study protocol was approved by the Institutional Review Boards and the Ethics Committees of Hong Hui Hospital, Xi’an Jiaotong University. Before surgery, informed consent was obtained from all patients after a full explanation of the therapeutic procedure.
Patient population
In this prospective case series, 56 patients with two-level thoracolumbar OVCF were treated with PKP between May 2009 and February 2013. There were 41 (73.2 %) females and 15 (26.8 %) males with a mean age of 68.8 years (range 55–74 years). The inclusion criteria were as follows: (1) collapse ≥15 % of the vertebral height; (2) severe back pain related to a two-level OVCF refractory to analgesic medication for at least 2 weeks; (3) pain with a visual analogue scale (VAS) ≥5, tapping pain at the spinal process of the fractures vertebral body; and (4) on magnetic resonance imaging (MRI), the affected vertebral body showed a hypointense signal on T1-weighted images and hyperintense signal on T2-weighted images; (5) bone attenuation (T-score less than −2.5) on bone densitometry. The exclusion criteria were as follows: (1) secondary osteoporosis (corticosteroids, endocrine disorders, and an inflammatory process); (2) inability to give informed consent; (3) uncorrected coagulopathy; (4) general poor physical state; (5) painless OVCF; (6) spinal metastatic cancer; and (7) neurologic symptoms.
Surgical techniques
After the patient had given consent, all operations were performed by two senior orthopedists (BR. H. and DJ. H.) specialized in spine surgery. All PKP procedures were performed in the operating room with availability of probable immediate decompressive surgery (KMC; KINETIC MEDICAL Co., LTD, Shanghai, China). The patient was positioned prone on two transverse bolsters under the chest and pelvis. Then, we applied a gentle three-point reduction force on the fractured vertebra to relatively reduction. In all procedures, local anesthesia was used to detect the patient neurological status. The surgical techniques for PKP were carried out as previously described [3], which alway requires a bilateral transpedicular approach procedure. In this study, we also adopted a unilateral transverse process-pedicle approach. The selection of two different puncture techniques for the fractured vertebra was random. The C-arm is adjusted so that there is no bilateral shadow on the affected vertebral body, and the shapes of the pedicles are symmetrical with the same distance to spinous process. In the bilateral puncture, the trocars were inserted through the lateral margin of the pedicle at 3 o’ clock on the right side and 9 o’ clock on the left. In the unilateral puncture, the puncture point was located at 5 mm from the lateral margin of the pedicle where it intersects the midportion of the transverse process, and the extraversion angle was range from 10 to 30 ° (Fig. 1). In both techniques, lateral fluoroscopy was used to advance the needle through the pedicle and into the anterior one third of the vertebral body. The position of the tip of each needle, its communication with the vertebral vein, was then checked. Thermoluminescent dosimeters (TLD) (Becquerel and Sievert, Taipei, Taiwan) were placed on the right flank of each patient (proximal to the iliac crest) and the upper sternum (juxta-thyroid) of the operator. The TLDs remained in place during the entire procedure including the first projection (which checked the index level for PKP) and the last projection (following removal of the injection needle), and both dosimeters were subsequently removed for dose measurements. The data of operation time, bone cement injection, radiation dose, and bone cement leakage were recorded and compared.
a Skin incision design for percutaneous kyphoplasty. Black arrow represents bilateral puncture point; white arrow represents unilateral puncture point. b In the frontal view, the puncture needle locates at 5 mm from the lateral margin of the pedicle where it intersects the midportion of the transverse process. c The extraversion angle was range from 10 to 30 °
All patients were discharged after 24 h and were advised to avoid extreme physical strain for 2 months. Follow-up consultation was at 1, 3, 6, 9, and 12 months after the procedure. These follow-ups included clinical and radiographical assessments, as performed prior to surgery. After the surgery, all patients were evaluated by an osteoporosis specialist who monitored their pharmacologic anti-osteoporosis treatment.
Outcome measures
Overall pain was evaluated by using a VAS from 0 (no pain at the base) to 10 (maximal imaginable pain at the summit). We assessed the patient health status with Short Form 36 (SF36) questionnaire. Translation and validation study of the Chinese version of the form has already been performed. The questionnaires were completed preoperatively, 1, 6, and 12 months after surgery.
Anteroposterior and lateral standing radiographs were obtained to measure the kyphotic angle of the vertebral body in all patients preoperatively, at the time of discharge, and at 6 and 12 months after surgery. The kyphotic angle measurement was taken from the superior and inferior endplates of the fractured vertebra. After the PKP procedure, computed tomography (CT) scans of the treat level was performed to assess the bone cement distribution and to identify possible extra bone cement leakage. The axial vertebral body view can be divided into nine areas, from A to I (Fig. 2).
Statistical analysis
All statistical analyses were performed with the use of SPSS software, version 12 (SPSS Inc., Chicago, IL, USA). Categorical variables were compared by the chi-squared and Fisher’s exact tests and are presented as number and percent. Baseline continuous variables were compared by independent two-sample t tests and are present as mean and SD. Paired t tests were used to compare assessments before and after surgery in each group. P < 0.05 was considered to indicate statistical significance.
Results
Clinical results
Puncture of the trocars into the fractured vertebral body was accurately performed under C-arm guidance in all cases, and there were no intraoperative deaths in this study (Fig. 3). After 12 months, a total of 2 patient deaths from causes unrelated to the procedures were lost to follow-up and were excluded. Finally, 54 patients were included in this study, and the follow-up rate was 96.4 % (54/56). The characteristic data of patients were showed in Table 1.
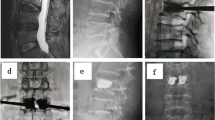
A 67-year-old female with lumbar 1,2 OVCF treated by PKP. a, b Preoperative anteroposterior and lateral radiographs showed a L1 and L2 fractures. c MR image showed hyperintense signal on T2-weighted images. d Preoperative sagittal CT scans showed integrity of posterior margin of vertebral body. e C-arm image showed L1 OVCF treated by bilateral PKP. f C-arm image showed L2 OVCF treated by unilateral PKP. g, h Postoperative anteroposterior and lateral radiographs showed satisfied bone cement distribution and vertebral height restoration. OVCF osteoporotic vertebral compression fractures, PKP percutaneous kyphoplasty, CT computed tomography, MRI magnetic resonance imaging
Overall, 55 vertebral bodies were treated with unilateral method, and 53 were treated with bilateral method. One patient with two-level thoracolumbar OVCF was treated with unilateral PKP because of right pedicle deformity. The mean volume of the injected cement in the unilateral level and bilateral level was 6.2 ± 0.6 and 8.5 ± 0.8 mL, respectively (P < 0.01). The operation time was significantly different between two levels with a shorter operation time observed using the unilateral puncture technique (15.6 ± 4.2 min) compared to the bilateral technique (38.6 ± 7.9 min) (P < 0.01). The mean radiation dose to each vertebra of patient using the unilateral technique was 0.88 ± 0.28 mSv, compared with 1.89 ± 1.05 mSv, and the difference between two levels was significant (P < 0.01). The mean radiation dose to the operator was not significantly different between two levels, although a less dose in the unilateral technique (0.21 ± 0.12 mSv) than the bilateral technique (0.24 ± 0.12 mSv) was noted (Table 2).
The VAS pain scores were shown in Table 3. All patients had significantly less pain after the procedures, compared with their preoperative period. The mean pain score decreased from 8.7 ± 1.6 before surgery to 2.7 ± 1.2 at 1 month postoperatively and to 2.6 ± 1.3 at 12 months after surgery (P < 0.01). According to the physical and mental health of SF-36, eight dimensionality concepts of physical functioning (PF), role limitations due to physical health (RP), bodily pain (BP), general health perceptions (GH), vitality (VT), social functioning (SF), role limitations due to emotional problems (RE), and general mental health (MH) were measured and listed in Table 4. There were statistically significant differences between the preoperation and postoperation at each assessment (P < 0.01).
Radiographic results
Preoperative and postoperative radiographic assessments of the two levels were measured (Fig. 3) and listed in Table 5. Both unilateral and bilateral PKP significantly reduced the kyphotic angle during follow-up. The kyphotic angle in the unilateral level improved significantly from 15.9 ± 6.4° before surgery to 9.3 ± 5.1° at the 12-month follow-up. The kyphotic angle in bilateral level improved significantly from 16.2 ± 7.1° before surgery to 11.5 ± 3.8° at the 12-month follow-up. Significantly greater reduction in kyphotic angle was noted in the unilateral level than in the bilateral level (P < 0.05).
All postoperative CT scans were evaluated by an experienced radiologist who independently assessed bone cement distribution using the same evaluation standard. In the unilateral level, bone cement mainly distributed in the anterior and middle of the vertebra body (A, B, C, D, E, F), and in the bilateral level, bone cement mainly distributed in the lateral and posterior of the vertebra body (A, D, G, C, F, I) (Fig. 4).
Complications
No procedure-related adverse events were observed in this study. Evaluation of intraoperative and postoperative radiographs revealed extravertebral cement leakages in 4 of 54 treated by unilateral technique (7.4 %) and in 10 of 54 treated using bilateral technique (18.5 %) (P < 0.01). The site of leakage was the adjacent intervertebral disc in 7 cases (2 cases in the unilateral level and 5 in the bilateral level), the paravertebral soft issue or vein in 6 cases (2 cases in the unilateral level and 4 in the bilateral level), and the spinal canal in 1 case in the bilateral level. During the follow-up period, a total of 4 patients (7.4 %) experienced a new fracture in 6 levels. In the bilateral level, 7 patients (12.9 %, 7/54) had obvious pain (VAS > 5) in the puncture sites at 1 month postoperatively caused by facet joint violation. With local block treatment, the pain disappeared in all patients at the last follow-up.
Discussion
An ideal therapy for vertebral body fractures should bring about a quick and lasting improvement of the symptoms as well as a durable correction of the kyphotic deformity caused by the fracture [1, 9–11]. Vertebroplasty and kyphoplasty are modern alternatives to the hitherto existing treatment concepts, percutaneous minimally invasive procedures for which, apart from a quick and lasting pain reduction, a quality of life improvement has been proven [4, 12–15]. In a survey study published by Garfin et al. [16], good to very good clinical results are presented for vertebroplasty and kyphoplasty, with significant pain reduction postoperatively as opposed to preoperatively. Mcliernan et al. [17] were able to demonstrate a significant quality-of-life improvement for vertebroplasty in the course of 12 months. In this study, our findings confirmed the results of previous studies, showing that a significant advantage of unilateral PKP compared to bilateral during the 12 months of follow-up although these two procedures are relatively safe and well able to reduce pain and improve patient’s quality of life.
In this study, postoperative pain symptoms improved significantly for all patients, with a significant difference in the VAS scores. However, in the bilateral puncture, 12.9 % patients had obvious pain in the puncture sites at 1 month postoperatively. With local block treatment, the pain disappeared in all patients at the last follow-up. These complications may be related with the puncture technique. Compared with unilateral technique, the puncture point of bilateral was more close to the facet joint, and the violation of facet joint was often.
In our study, the radiation doses to the patient are significantly different between using unilateral and bilateral techniques. However, the doses to the operator are not different statistically. The dosimeter on the operator is mainly exposed to the scatter radiation, while that on the patient is partly exposed to the primary radiation. Therefore, the dose amount on the operator is less than that on the patient (0.88, 1.89 mSv to patient vs. 0.21, 0.24 mSv to operator). Probably, for the small dose amount to the operator, we need a large sample size to prove the doses to operator different between the two techniques, if any.
In this study, the cement leakage in the unilateral level was significantly less than the bilateral level (7.4 vs. 18.5 %). These complications may be related with the puncture technique. Compared with the bilateral technique, the puncture point of unilateral was more lateral to the facet joint, and extraversion angle was larger. So, in the unilateral level, bone cement mainly distributed in the anterior and middle of the vertebra body (A, B, C, D, E, F), and in the bilateral level, bone cement mainly distributed in the lateral and posterior of the vertebra body (A, D, G, C, F, I). A significant improvement in the kyphotic angle could be shown. PKP, using both unilateral and bilateral techniques, have the ability to restore vertebral height and to improve alignment. For unilateral level, however, more postoperative kyphotic angle restorement can be achieved because of the bone cement distribution, which mainly distributed in the anterior and middle of the vertebra body.
Given the similar clinical efficacy, intraoperative factors, radiographic results, and complication may be important indicators of the more appropriate procedure. Unilateral PKP therefore seems to have advantages over bilateral for the treatment of OVCF, considering less volume of injected cement and radiation dose, shorter operation time, and less complications.
There were some limitations in this study. The number of patients included in this prospective study may be relatively small. In addition, the follow-up period was relatively shorter. Further long-term follow-up studies in a large patient population are warranted to generalize our results.
In conclusion, this study confirms that both bilateral and unilateral PKP are relatively safe and effective treatments for patients with painful OVCF. During the 12-month follow-up, both procedures demonstrated similar good clinical outcomes, but unilateral PKP received less radiation dose and operation time and resulted in less complication than bilateral. The benefits of these relative merits need to be ascertained in future long-term studies.
References
Klazen CA, Lohle PN, de Vries J, Jansen FH, Tielbeek AV, Blonk MC, Venmans A, van Rooij WJ, Schoemaker MC, Juttmann JR, Lo TH, Verhaar HJ, van der Graaf Y, van Everdingen KJ, Muller AF, Elgersma OE, Halkema DR, Fransen H, Janssens X, Buskens E, Mali WP (2010) Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (VERTOS II): an open-label randomised trial. Lancet 376:1085–1092
Rousing R, Hansen KL, Andersen MO, Jespersen SM, Thomsen K, Lauritsen JM (2010) Twelve-months’ follow-up in forty-nine patients with acute/semiacute osteoporotic vertebral fractures treated conservatively or with percutaneous vertebroplasty: a clinical randomized study. Spine 35:478–482
Kallmes DF, Comstock BA, Heagerty PJ, Turner JA, Wilson DJ, Diamond TH, Edwards R, Gray LA, Stout L, Owen S, Hollingworth W, Ghdoke B, Annesley-Williams DJ, Ralston SH, Jarvik JG (2009) A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med 361:569–579
Buchbinder R, Osborne RH, Ebeling PR, Wark JD, Mitchell P, Wriedt C, Graves S, Staples MP, Murphy B (2009) A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med 361:557–568
Rousing R, Andersen MO, Jespersen SM, Thomsen K, Lauritsen J (2009) Percutaneous vertebroplasty compared to conservative treatment in patients with painful acute or subacute osteoporotic vertebral fractures: three-months’ follow-up in a clinical randomized study. Spine 34:1349–1354
Chen YJ, Tan TS, Chen WH, Chen CC, Lee TS (2006) Intradural cement leakage: a devastatingly rare complication of vertebroplasty. Spine 31:379–382
Cosar M, Sasani M, Oktenoglu T, Kaner T, Ercelen O, Kose KC, Ozer AF (2009) The major complications of transpedicular vertebroplasty. J Neurosurg Spine 11:607–613
Fribourg D, Tang C, Sra P, Delamarter R, Bae H (2004) Incidence of subsequent vertebral fracture after kyphoplasty. Spine 29:2270–2277
Barr JD, Barr MS, Lemley TJ, McCann RM (2000) Percutaneous vertebroplasty for pain relief and spinal stabilization. Spine 25:923–928
Heini PF, Wa Ichli B, Berlemann U (2000) Percutaneous transpedicular vertebroplasty with PMMA: operative technique and early results. A prospective study for the treatment of osteoporotic compression fractures. Eur Spine J 9:445–450
Frankel BM, Monroe T, Wang C (2007) Percutaneous vertebral augmentation: an elevation in adjacent-level fracture risk in kyphoplasty as compared with vertebroplasty. Spine J 7:575–582
Mathis JM (2006) Percutaneous vertebroplasty or kyphoplasty: which one do I choose. Skeletal Radiol 35:629–631
Crandall D, Slaughter D, Hankins PJ, Moore C, Jerman J (2004) Acute versus chronic vertebral compression fractures treated with kyphoplasty: early results. Spine 4:418–424
Grohs JG, Matzner M, Trieb K, Krepler P (2005) Minimal invasive stabilization of osteoporotic vertebral fractures: a prospective nonrandomized comparison of vertebroplasty and balloon kyphoplasty. J Spinal Disord Tech 18:238–242
Shindle MK, Gardner JM, Koob J, Bukata S, Cabin JA, Lane JM (2006) Vertebral height restoration in osteoporotic compression fractures: kyphoplasty balloon tamp is superior to postural correction alone. Ostoporosis Int 17:1815–1819
Yang YM, Ren ZW, Ma W, Jha R (2013) Current status of percutaneous vertebroplasty and percutaneous kyphoplasty—a review. Med Sci Monit 19:826–836
Urrutia J, Bono CM, Mery P, Rojas C (2008) Early histologic changes following polymethylmethacrylate injection (vertebroplasty) in rabbit lumbar vertebrae. Spine 33:877–882
Acknowledgments
Dr Dingjun Hao and Dr Baorong He contributed equally to this work and should be considered as co-corresponding authors.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
The authors declare that they have no competing interests.
Ethical approval
The study protocol was approved by the Institutional Review Boards and the Ethics Committees of Hong Hui Hospital, Xi’an Jiaotong University.
Informed consent
Before surgery, informed consent was obtained from all patients after a full explanation of the therapeutic procedure.
Rights and permissions
About this article
Cite this article
Yan, L., He, B., Guo, H. et al. The prospective self-controlled study of unilateral transverse process-pedicle and bilateral puncture techniques in percutaneous kyphoplasty. Osteoporos Int 27, 1849–1855 (2016). https://doi.org/10.1007/s00198-015-3430-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-015-3430-5