Abstract
Summary
Vertebral fractures (VFs) are independent risk factors for new fractures. However, spine radiographs cannot be used as a screening method. EOS® has a good diagnostic value for the diagnosis of VF with a better legibility of upper thoracic spine and a higher concordance between readers compared to vertebral fracture assessment (VFA).
Introduction
Vertebral fractures (VFs) are risk factors for new fractures. However, spine radiographs cannot be used as a screening method for both cost and radiation concerns. EOS® X-ray imaging system which allows the acquisition of biplane images in an upright weight-bearing position with low radiation dose was used. The objective of this study was to compare EOS® to VFA for the diagnosis of VF.
Methods
We conducted a cross-sectional study in subjects aged above 50 years with indication for spine imaging. EOS® and VFA of the spine were performed the same day. Sensitivity (Se), specificity (Sp), negative predictive value (NPV), and the interobserver precision of EOS® were compared to VFA for the diagnosis of VF.
Results
Two hundred patients (mean age 66.2 years) were included. At the vertebral level, 2.4 and 3.6 % of vertebrae were not legible using EOS® and VFA, respectively (p = 0.0007). The legibility of spine was significantly affected by scoliosis (odds ratio (OR) = 2.8, p < 0.0001, for EOS®, and OR = 1.8, p = 0.0041, for VFA). Sixty-six patients (33.0 %) and 69 (34.5 %) had at least one VF using VFA and EOS®, respectively. At patient level, Se, Sp, and NPV for the diagnosis of VF of EOS® were 79.7, 91.6, and 99 %, respectively. Concordance between both observers was very good for EOS® (kappa-score = 0.89), higher than for VFA (κ = 0.67).
Conclusions
This study shows that EOS® has a good diagnostic value for the diagnosis of VF with a better legibility of upper thoracic spine and a higher concordance between readers compared to VFA.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Vertebral fractures (VFs) are the hallmark manifestation of osteoporosis, associated with increased morbidity, chronic pain, and functional limitations [1]. The increase in mortality related to clinical vertebral fractures in the elderly is similar to the one observed after hip fractures [1]. Prevalent vertebral fractures and age are the strongest risk factors for sustaining a vertebral and non-vertebral fracture [2–4]. Moreover, the number of vertebral fractures is also a determinant of the risk of sustaining a new fracture. The more is the number of VFs and the more severe are the fractures, the higher is the risk [5–7]. Thus, a thorough assessment of the whole spine is relevant to improve the fracture risk evaluation in postmenopausal osteoporosis [8]. In postmenopausal women referred for dual-energy X-ray absorptiometry (DXA) measurements because of risk factors for osteoporosis, 20 % have so far unknown vertebral fractures [9, 10]. However, identification of patients who require spine radiographs is difficult [11–13]. Performing systematic spine radiographs in asymptomatic subjects increases the cost of VFs diagnosis and exposes patients to unnecessary radiation. The detection of vertebral fractures using DXA, also known as vertebral fracture assessment (VFA), is a convenient method to assess vertebral fractures because VFA offers point-of-service convenience for the patient when it is done at the same visit as bone mineral density (BMD) measurement by DXA, with far less radiation than standard radiography [14]. The X-ray source is orthogonal to the vertebral bodies, not a cone-beam as for standard X-rays, avoiding geometric distortion. Previous studies showed a good to excellent agreement between the two imaging modalities [15, 16]. The main limitation of this technique has long been the difficulty of visualization of the upper thoracic spine [15–18], but new technological advancements further improve performance of the technique with the improvement of readability [19, 20]. VFA is recommended by the International Society of Clinical Densitometry (ISCD) when the results may influence clinical management of osteoporosis [21]. However one of the drawbacks of the assessment of VF by VFA is the lying position that prevents correct assessment of spine curvatures, although hyperkyphosis is an independent risk factor of incident vertebral and non-vertebral fractures and should be assessed in the management of fracture risk [22, 23]. Moreover, additional radiographs are necessary after VFA in some situations: two or more mild deformities without any moderate or severe (grade 2 or 3) fractures, lesions in vertebrae that cannot be attributed to benign causes, patient with a history of malignancy, unreadable vertebrae between T7-L4, sclerotic or lytic changes, or findings suggestive of conditions other than osteoporosis [21].
EOS® is a low dose biplane X-ray imaging system (EOS imaging, Paris, France), available in more than 10 countries worldwide. The technology uses two perpendicular X-ray beams collimated in two very thin, horizontal, fan-shaped beams and two specific detectors based on the Nobel prize winning work of physicist Georges Charpak. Fan-beam X-rays and detectors are mounted on a C-arm and scan all or part of the patient’s body. This allows for frontal and lateral X-rays of a patient to be carried out simultaneously (in 4–6 s to scan the spine; Fig. 1a) and full body imaging without digital stitching [24]. EOS® is performed in an upright, weight-bearing position offering the opportunity to assess the spine and pelvic curvatures. The EOS® system provides digital images of the skeleton without geometric distortion, with lower radiation than conventional radiography: the mean entrance surface radiation dose for the postero-anterior spine and lateral spine is 0.23 and 0.37 milligrays (mGy), respectively, with EOS®, compared to 1.2 and 2.3 mGy, respectively, for conventional radiography [24]. Radiation dose must be “as low as reasonably achievable”; however, optimal legibility of bony details is necessary for the diagnosis of VF.
Our hypothesis is that EOS® is superior to VFA in the legibility of vertebral fractures and avoids performing additional radiographs. The aim of our study was to evaluate the performance of EOS® compared to VFA for the diagnosis of VF in subjects over 50 years.
Methods
Study design
This was an observational cross-sectional single-center study. Inclusion of cases was conducted from September 2013 to Mars 2014.
Patients
Postmenopausal women and men aged above 50 years with indication for spine radiographs (risk factors for osteoporosis, height loss, etc.) were included in this study. VFA is a routine procedure in our Rheumatology Department in these indications. The patient’s informed consent was obtained for the use of their EOS® data from all patients.
For each patient, age, height, weight, and body mass index (BMI) (kg/m2) were collected. Patients were classified as normal if their BMI was <27 kg/m2, overweight if BMI ≥27 kg/m2 and ≤30 kg/m2, and obese if BMI >30 kg/m2.
DXA measurements (BMD and VFA)
All patients had measurements of lumbar spine and hip BMD using a DXA device (QDR 4500, Hologic, Bedford, MA). The quality control protocol for the DXA device includes daily scanning of a phantom. A single device was used for the whole study. The World Health Organization (WHO) classification was used to define osteoporosis as T-score ≤−2.5 at lumbar spine, total hip, or femoral neck. VFA scan (software version 12.6) was done using the same DXA device at the same time from T4 to L4.
EOS® biplanar radiographs
All patients underwent a full spine 2-D EOS imaging, in an upright weight-bearing position. (Fig. 1a, b). Postero-anterior (PA) and lateral images were obtained simultaneously. Both imaging techniques were performed the same day.
Diagnosis of vertebral fracture
Two independent readers (both rheumatologists) performed a blinded reading of both imaging modalities. A training session was done on VFA and EOS® before the beginning of the study. Each reader was blinded to the diagnosis and medical files as well as to the other reader’s results and any previous imaging. Each investigator read the EOS® and VFA scans of the same patient with at least 1-month interval. Both EOS® and VFA scans were evaluated for legibility and presence of vertebral fracture. The software options (zooms, image processing) enhancing view option on EOS® and VFA was used to improve the legibility of the vertebrae, when necessary.
For each legible vertebra, the diagnosis of VF was performed according to Genant’s semi-quantitative grading from 0 to 3 [25]. Scoliosis was absent (grade 0), or classified in three grades according to the rotation of the vertebral body judged on the distance between the spinous process and the lateral border of the vertebral body. This distance was divided in two. If the spinous process was projected in the first half of the vertebral body, scoliosis was considered as minor; if it was in the second half, it was considered as moderate; and if it was lateral to vertebral body, it was considered as severe (grades 1, 2, and 3, respectively). For this study, scoliosis was defined by the presence of a grade ≥1.
Statistical analysis
We assessed performance of EOS® in the diagnosis of VF, as compared to VFA. The number of unreadable vertebrae was compared between the two methods using a McNemar test. Factors affecting legibility (age, BMI, BMD, presence of scoliosis) were tested using Fischer’s tests for categorical factors and Wilcoxon rank sum tests for continuous variables. Evaluation of the diagnostic value was performed using the results of the two readers both at vertebral and patient levels. At the vertebrae level, sensitivity and specificity of EOS® with 95 % exact confidence intervals were calculated. Positive and negative likelihood ratios (LRs) were also calculated, taking into account the grade of fracture. Values above 10 were considered to indicate a useful diagnostic test. The number of patients who require additional X-rays based on ISCD recommendations [21] was calculated. At the patient level, patients were classified as fractured (at least one fracture visible), normal (all vertebrae from T4 to L4 were readable and no vertebral fracture visible), or without possible diagnosis (no vertebral fracture visible but some vertebrae were unreadable). We calculated sensitivity and specificity with exact 95 % confidence interval (CI) of EOS®. Interobserver agreement for the diagnosis of fracture was evaluated for VFA and EOS® at the vertebral and at the patient level using κ statistics.
Results
Patient characteristics
Two hundred consecutive patients (95 % women, mean age 66.2 years) were included in this study: 62.5 % were osteoporotic, 15.0 % had a mean T-score between −1 and −2.5, and 22.5 % had normal BMD (Table 1). One hundred twenty-five patients (62.5 %) of the patients did not have scoliosis, 38 (19.0 %) had a minor scoliosis (grade 1), 19 (9.5 %) a moderate scoliosis (grade 2), and 18 (9.0 %) a severe scoliosis (grade 3). One hundred sixty-one patients (80.5 %) had normal BMI, 28 (14.0 %) overweight, and 11 (5.5 %) were obese.
Legibility of the spine
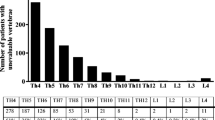
At the vertebral level (n = 5200, total reading of two readers), on EOS®, 5075 vertebrae (97.6 %) were considered readable and 125 (2.4 %) were unreadable. Unreadable vertebrae were located in T4 (n = 17 (0.32 %)), T5 (n = 13 (0.25 %), and T6 (n = 10 (0.19 %)), meaning that 4.25 % of T4 vertebrae, 3.25 % of T5 vertebrae, and 2.5 % of T6 were unreadable (Fig. 2). On the VFA radiographs, 5015 vertebrae (96.4 %) were considered readable and 185 (3.6 %) were unreadable. Unreadable vertebrae were located in T4 (n = 43 (0.82 %)), T5 (n = 43 (0.82 %)), and T6 (n = 25 (0.48 %)) meaning that 10.75 % of T4 vertebrae, 10.75 % of T5 vertebrae, and 6.25 % of T6 vertebrae were unreadable (Fig. 2).
At the patient level, thoraco-lumbar spine from T4 to L4 was readable without difficulty in 179 patients (89.5 %) on VFA scans and in 185 patients (92.5 %) on EOS®. Scoliosis (defined by a grade ≥1) affected the legibility of the vertebrae on EOS® (odds ratio (OR) = 2.85 [95 % CI 1.9; 4.28], p ≤ 0.005) and on VFA (OR = 1.85 [95 % CI 1.22; 2.82], p = 0.005). BMI, height, and low BMD did not significantly affect legibility of EOS® and VFA.
EOS® as a diagnostic tool
At the vertebral level, there were 4925 vertebrae assessable using both EOS and VFA methods. On EOS®, 4650 vertebrae (94.42 %) were normal, 94 (1.91 %) had grade 1, 96 (1.95 %) grade 2, and 85 (1.73 %) grade 3 fractures. Using VFA scans, 4693 vertebrae (95.29 %) were considered as normal, 84 (1.71 %) had grade 1, 86 (1.75 %) grade 2, and 62 (1.26 %) grade 3 fractures. Distribution of VF is represented in Fig. 3. Sensitivity of the diagnosis of fractures using EOS® versus VFA was 66 % (95 % CI 58–73), specificity was 99 % (95 % CI 98.0–99.0), and negative predictive value was 98.7 (95 % CI 98.0–99.0].
At the patient level, 69 (34.5 %) and 66 (33.0 %) patients had at least one vertebral fracture using EOS® and VFA, respectively. Sensitivity of the diagnosis of VF using EOS® compared with VFA scans was 80 % (95 % CI 68.0–88.0), specificity was 92.0 (95 % CI 85.0–95.0), and negative predictive value was 89.5 % (95 % CI 83.0–94.0], with a LR+ of 107.5 and LR− of 0.34.
Using VFA results, 21 (10.5 %) patients had indications for additional spine radiographs. Six patients had at least two grade 1 without any grade 2 or 3 and 15 patients had at least one unreadable vertebra between T7-L4. No patient had sclerotic or lytic changes or findings suggestive of conditions other than osteoporosis
Comparison of readers
At the vertebral level, only vertebrae that could be analyzed by both readers were included in this analysis (n = 2516 for EOS® and 2452 for VFA) (Fig. 2). For EOS®, there was a good interobserver agreement for the diagnosis of VF (κ-score = 0.889). For VFA, concordance between both readers was 0.647. At the patient level, interobserver concordance was 0.887 and 0.668 for EOS® and VFA, respectively.
Discussion
This study shows that EOS® has a good diagnostic value for the diagnosis of vertebral fractures with a best legibility of upper thoracic spine as compared to VFA, and a higher concordance between readers. Moreover, EOS® avoids additional spine radiographs which are sometimes necessary after VFA exam.
Although conventional radiography remains the standard method for the detection of vertebral fractures, VFA is a densitometric technique, validated for reproducibility, sensitivity, and specificity as compared with spine radiographs, with the advantage of potentially reducing the parallax effects on fracture diagnosis, a low radiation exposure, and the applicability during BMD measurement by DXA. The main limiting factor in utilizing VFA is the legibility of the vertebrae, but with recent technology, recent generation of densitometers, and reader experience, the vertebral body visualization is improved with 92–95 % of all vertebral bodies which are readable [19, 20]. VFA results influence patient management, for both radiographs and treatment prescriptions. VFA could help avoiding unnecessary X-rays and modifies therapeutic decisions in a third of patients in a study conducted in experienced rheumatologists [26]. However, degenerative vertebrae may be confounded to vertebral fractures when seen at VFA; therefore, additional radiographs are sometimes necessary to exclude these degenerative vertebrae. Based on these arguments, we considered VFA as the reference technique, in the context of this clinical study.
In both EOS® and VFA technologies, the source of X-rays is always perpendicular to the target, avoiding any image distortion. But, EOS® is performed in standing position; thus, it is expected that scoliosis could have a greater impact on legibility of the vertebrae on EOS, than on VFA which is performed in a lying position. However, our study shows that the legibility is similar for the two techniques, and even better on EOS® at the upper thoracic spine: At the T4-T6 level, 2.5 to 4.25 % and 6.25 to 10.75 % of vertebrae were unreadable on EOS® and VFA, respectively. This has a consequence on clinical practice and the necessity of additional standard radiographs: Following ISCD guidelines, 10.5 % of our patients should have standard spine radiographs after VFA, with thus subsequent radiation and costs. Our patients were referred for osteoporosis assessment, and none of them had symptoms suggesting malignancy.
In this study, we used VFA as a gold standard, recognizing that recent VFA technology approaches the capability of radiographs [19], and taking into account that EOS® uses the same technology for radiographs source, without cone-beam geometry related problems. The two readers were experienced, and this study does not explore the potential impact of reader experience on VF identification on EOS®. However, EOS® offers enhanced image quality, and the images produced by EOS® are closer to the images obtained with standard radiographs than with VFA [24, 27]. The added utility of EOS® is the image quality of the antero-posterior spine, higher than VFA but also higher than standard radiographs [27]. The better results obtained on EOS® may be in part related to the AP view. The concordance between readers on EOS® was optimal in our study, and better than on VFA, a result that could be the consequence of the quality of the image. We are not aware of any study with direct comparison of EOS® and standard radiographs for the diagnosis of VF. There are few studies on the comparison between EOS® and standard radiographs for the diagnostic imaging of spine lesions. In the diagnosis of structural damage in spondyloarthritis, performance of the technique was good for spine involvement, with a similar sensitivity between EOS® and standard radiographs, low for sacroiliitis diagnosis, but similar to standard radiographs [28]. Radiation dose is a concern for patients who require repeated imaging. A large cohort study of patients with scoliosis and other spinal deformities exposed to repeated radiographs (at a time when radiation doses were higher than those currently used for standard radiographs) found an increased risk of breast cancer mortality among spinal deformity patients compared with the general female population [29]. There is a benefit of EOS® over standard radiographs technology, resulting in a fivefold to sixfold reduction of the radiation doses [24, 27]. The dose-area product for whole-spine (antero-posterior, lateral) radiographs has been reported to be 392 ± 232 and 158 ± 104 cGy/cm2 for standard radiographs and EOS®, respectively [30]. Over their lifetime, patients with osteoporosis and VF are repeatedly exposed to conventional radiographs, for follow-up. Indeed, a proportion of incident VFs can occur in these patients [31] and are an indication to change of treatment. On the other hand, back pain from other causes has a high prevalence in this population. Thus, the balance between the importance of imaging the spine for making an appropriate decision on treatment (if there is a VF), and the concern over unnecessary radiation (if pain is related to degenerative changes) is a remaining question [11]. EOS® imaging is a convenient technique in this matter.
Our study has limitations. It was a cross-sectional analysis and our conclusions can apply only for the diagnosis of prevalent fractures. Our department is situated in a tertiary care setting, explaining the high prevalence of vertebral fractures; in our cohort; the results may be different in patients with different characteristics. We found a good interobserver agreement between readers for the diagnosis of VF using EOS® recognizing that we did not assess the intraobserver reproducibility. We did not use the most recent generation of DXA device and we cannot eliminate the hypothesis that the recent generation of densitometers might have compared more favorably to the EOS®. We assessed scoliosis based on rotation of the spinous process; we did not use methods based on quantification of angles (as Cobb’s), and thus we cannot anticipate how different methods of assessment could change our results.
In conclusion, this study shows that EOS® has a good diagnostic value for the diagnosis of VF. Other studies are necessary to assess the evidence that the use of EOS® can improve the osteoporotic patient’s management.
References
Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR (2009) Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA 301:513–21
Black DM, Arden NK, Palermo L, Pearson J, Cummings SR (1999) Prevalent vertebral deformities predict hip fractures and new vertebral deformities but not wrist fractures. Study of Osteoporotic Fractures Research Group. J Bone Miner Res 14:821–8
Lindsay R, Silverman SL, Cooper C, Hanley DA, Barton I, Broy SB, Licata A, Benhamou L, Geusens (2001) Risk of new vertebral fracture in the year following a fracture. JAMA 285:320–3
Ross PD, Davis JW, Epstein RS, Wasnich RD (1991) Pre-existing fractures and bone mass predict vertebral fracture incidence in women. Ann Intern Med 114:919–23
Roux C, Fechtenbaum J, Kolta S, Briot K, Girard M (2007) Mild prevalent and incident vertebral fractures are risk factors for new fractures. Osteoporos Int 18:1617–24
Kerkeni S, Kolta S, Fechtenbaum J, Roux C (2009) Spinal deformity index (SDI) is a good predictor of incident vertebral fractures. Osteoporos Int 20:1547–52
Nevitt MC, Ross PD, Palermo L, Musliner T, Genant HK, Thompson DE (1999) Association of prevalent vertebral fractures, bone density, and alendronate treatment with incident vertebral fractures: effect of number and spinal location of fractures. The Fracture Intervention Trial Research Group. Bone 25:613–9
Siris ES, Genant HK, Laster AJ, Chen P, Misurski DA, Krege JH (2007) Enhanced prediction of fracture risk combining vertebral fracture status and BMD. Osteoporos Int 18:761–70
Netelenbos JC, Lems WF, Geusens PP, Verhaar HJ, Boermans AJ, Boomsma MM, Mulder PG, Papapoulos SE (2009) Spine radiographs to improve the identification of women at high risk for fractures. Osteoporos Int 20:1347–52
Gallacher SJ, Gallagher AP, McQuillian C, Mitchell PJ, Dixon T (2007) The prevalence of vertebral fracture amongst patients presenting with non-vertebral fractures. Osteoporos Int 18:185–92
Roux C, Priol G, Fechtenbaum J, Cortet B, Liu-Léage S, Audran M (2007) A clinical tool to determine the necessity of spine radiography in postmenopausal women with osteoporosis presenting with back pain. Ann Rheum Dis 66:81–5
Kaptoge S, Armbrecht G, Felsenberg D, Lunt M, O’Neill TW, Silman AJ, Reeve J, EPOS Study Group (2004) When should the doctor order a spine X-ray? Identifying vertebral fractures for osteoporosis care: results from the European Prospective Osteoporosis Study (EPOS). J Bone Miner Res 19:1982–93
Schousboe JT, Ensrud KE, Nyman JA, Kane RL, Melton LJ 3rd (2005) Potential cost-effective use of spine radiographs to detect vertebral deformity and select osteopenic post-menopausal women for amino-bisphosphonate therapy. Osteoporos Int 16:1883–93
Lewis MK, Blake GM, Fogelman I (1994) Patient dose in dual x-ray absorptiometry. Osteoporos Int 4:11–5
Ferrar L, Jiang G, Barrington NA, Eastell R (2000) Identification of vertebral deformities in women: comparison of radiological assessment and quantitative morphometry using morphometric radiography and morphometric X-ray absorptiometry. J Bone Miner Res 15:575–585
Ferrar L, Jiang G, Eastell R, Peel NFA (2003) Visual evaluation of vertebral fractures in osteoporosis using morphometric X-ray absorptiometry. J Bone Miner Res 18:933–938
Damiano J, Kolta S, Porcher R, Tournoux C, Dougados M, Roux C (2006) Diagnosis of vertebral fractures by vertebral fracture assessment. J Clin Densitom 9:66–71
Chapurlat RD, Duboeuf F, Marion-Audibert HO, Kalpakçioglu B, Mitlak BH, Delmas P (2006) Effectiveness of instant vertebral assessment to detect prevalent vertebral fracture. Osteoporos Int 1:1189–95
Buehring B, Krueger D, Checovich M, Gemar D, Vallarta-Ast N, Genant HK, Binkley N (2010) Vertebral fracture assessment: impact of instrument and reader. Osteoporos Int 21:487–94
Hospers IC, van der Laan JG, Zeebregts CJ, Nieboer P, Wolffenbuttel BH, Dierckx RA, Kreeftenberg HG, Jager PL, Slart RH (2009) Vertebral fracture assessment in supine position: comparison by using conventional semiquantitative radiography and visual radiography. Radiology 251:822–8
Schousboe JT, Shepherd JA, Bilezikian JP, Baim S (2013) Executive Summary of the 2013 ISCD Position Development Conference on Bone Densitometry. J Clin Densitom 16:455–467
Roux C, Fechtenbaum J, Kolta S, Said-Nahal R, Briot K, Benhamou CL (2010) Prospective assessment of thoracic kyphosis in postmenopausal women with osteoporosis. J Bone Miner Res 25:362–8
Kado DM, Miller-Martinez D, Lui LY, Cawthon P, Katzman WB, Hillier TA, Fink HA, Ensrud KE (2014) Hyperkyphosis, kyphosis progression, and risk of non-spine fractures in older community dwelling women: the study of osteoporotic fractures (SOF). J Bone Miner Res 29:2210–6
Wade R, Yang H, McKenna C, Faria R, Gummerson N, Woolacott N (2013) A systematic review of the clinical effectiveness of EOS 2D/3D X-ray imaging system. Eur Spine J 22:296–304
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8:1137–48
Roux C, Baron G, Audran M, Breuil V, Chapurlat R, Cortet B, Fardellone P, Trémollières F, Ravaud P (2011) Influence of vertebral fracture assessment by dual-energy X-ray absorptiometry on decision-making in osteoporosis: a structured vignette survey. Rheumatology (Oxford) 50:2264–9
Deschênes S, Charron G, Beaudoin G, Labelle H, Dubois J, Miron MC, Parent S (2010) Diagnostic imaging of spinal deformities: reducing patients radiation dose with a new slot-scanning X-ray imager. Spine (Phila Pa 1976) 35:989–94
Moltó A, Freire V, Feydy A, Paternotte S, Maksymowych WP, Benhamou M, Rannou F, Dougados M, Gossec L (2014) Assessing structural changes in axial spondyloarthritis using a low-dose biplanar imaging system. Rheumatology (Oxford) 53:1669–75
Ronckers CM, Land CE, Miller JS, Stovall M, Lonstein JE, Doody MM (2010) Cancer mortality among women frequently exposed to radiographic examinations for spinal disorders. Radiat Res 174:83–90
Dietrich TJ, Pfirrmann SA, Pankalla K, Buck FM (2013) Comparison of radiation dose, workflow, patient comfort and financial break-even of standard digital radiography and a novel biplanar low-dose X-ray system for upright full-length lower limb and whole spine radiography. Skeletal Radiol 42:959–67
Fink HA, Milavetz DL, Palermo L, Nevitt MC, Cauley JA, Genant HK, Black DM, Ensrud KE, Fracture Intervention Trial Research Group (2005) What proportion of incident radiographic vertebral deformities is clinically diagnosed and vice versa? J Bone Miner Res 20:1216–22
Conflicts of interest
K. Briot: Research grants and/or honoraria from Amgen, MSD, Lilly, Pfizer. J. Fechtenbaum: no disclosures. A. Etcheto: no disclosures. S. Kolta: no disclosures. A. Feydy: no disclosures. C. Roux: Research grants and/or honoraria and/for travel reimbursements from Amgen, MSD, Lilly, Pfizer, UCB.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Briot, K., Fechtenbaum, J., Etcheto, A. et al. Diagnosis of vertebral fractures using a low-dose biplanar imaging system. Osteoporos Int 26, 2649–2655 (2015). https://doi.org/10.1007/s00198-015-3190-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-015-3190-2