Abstract
Summary
We determined the prevalence of osteosarcopenic obesity (loss of bone and muscle coexistent with increased adiposity) in overweight/obese postmenopausal women and compared their functionality to obese-only women. Results showed that osteosarcopenic obese women were outperformed by obese-only women in handgrip strength and walking/balance abilities indicating their higher risk for mobility impairments.
Introduction
Osteosarcopenic obesity (OSO) is a recently defined triad of osteopenia/osteoporosis, sarcopenia, and adiposity. We identified women with OSO in overweight/obese postmenopausal women and evaluated their functionality comparing them with obese-only (OB) women. Additionally, women with osteopenic/osteoporotic obesity (OO), but no sarcopenia, and those with sarcopenic obesity (SO), but no osteopenia/osteoporosis, were identified and compared. We hypothesized that OSO women will have the lowest scores for each of the functionality measures.
Methods
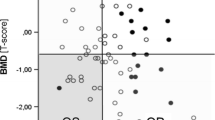
Participants (n = 258; % body fat ≥35) were assessed using a Lunar iDXA instrument for bone and body composition. Sarcopenia was determined from negative residuals of linear regression modeled on appendicular lean mass, height, and body fat, using 20th percentile as a cutoff. Participants with T-scores of L1–L4 vertebrae and/or total femur <−1, but without sarcopenia, were identified as OO (n = 99) and those with normal T-scores, but with sarcopenia, as SO (n = 28). OSO (n = 32) included women with both osteopenia/osteoporosis and sarcopenia, while those with normal bone and no sarcopenia were classified as OB (n = 99). Functionality measures such as handgrip strength, normal/brisk walking speed, and right/left leg stance were evaluated and compared among groups.
Results
Women with OSO presented with the lowest handgrip scores, slowest normal and brisk walking speed, and shortest time for each leg stance, but these results were statistically significantly different only from the OB group.
Conclusion
These findings indicate a poorer functionality in women presenting with OSO, particularly compared to OB women, increasing the risk for bone fractures and immobility from the combined decline in bone and muscle mass, and increased fat mass.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recently, a condition termed osteosarcopenic obesity (OSO) was identified in postmenopausal women and characterized by the simultaneous presence of osteopenia/osteoporosis (low bone mineral density), sarcopenia/dynapenia (decreased muscle mass and strength), and increased adiposity [1, 2]. The individuals with this condition experience both reduced bone and muscle mass and a high percentage of body fat, the latter either presented as infiltrated fat in bone and muscle tissue or overt clinical obesity (e.g., body mass index higher that 30 kg/m2 or body fat higher than 30 %). This indicates that increased adiposity does not necessarily protect against osteopenia/osteoporosis and subsequent fracture risk. In addition, reduced strength and mobility due to sarcopenia increases the risk of falls and fractures [3].
Currently, one in three American women over the age of 50 experiences a bone fracture [4], a major cause of morbidity and mortality, leading to loss of independence [5]. Osteoporosis, or low bone mineral density (BMD), is not adequate to fully explain the exponential increase in bone fractures that occur with aging. With this in mind, tools such as FRAX and Garvan have been developed to evaluate clinical markers beyond BMD and have improved fracture risk prediction. However, these methods also have their limitations and, in some cases, they are no better than older models based on age and BMD [6, 7]. The FRAX risk calculator contains more variables, including body weight and height and known risk factors for fracture (e.g., smoking) as well as family history, whereas the Garvan calculator utilizes only age, gender, previous fracture, femoral neck BMD, and falls in the last 12 months. Neither risk calculator considers other tissues involved in locomotion and postural stability and particularly not the amount of body fat or fat infiltration. Furthermore, individuals experiencing obesity and low BMD concurrently, in a condition termed osteopenic obesity (OO), are often overlooked in clinical settings based on the belief that obesity is protective against fractures [1]. Obese individuals also often lack adequate muscle mass and strength [8], presenting with sarcopenic obesity (SO), which increases the risk for immobility and falls, a relevant issue when assessing fracture risk [9]. Therefore, including the health status of bone and muscle and the level of fat mass could be important in future risk assessment. This makes the triad of deteriorated bone, reduced muscle mass, and increased adipose tissue, collectively termed as OSO, relevant when assessing patients for fracture risk and other morbidity conditions [1].
We propose that physical performance measurements, or functionality, in a clinical setting could potentially be utilized as a means to screen individuals with OSO, as all three tissues are involved in function. We previously employed some tests of physical performance that included handgrip strength, normal/brisk walking, and one leg stance time to evaluate their relationship with bone and body composition parameters in postmenopausal women [10–12]. Handgrip strength is a powerful predictor of functional abilities in older adults, and its decline is associated with increased risk of falls and disability [13, 14] as well as lower BMD [10, 12]. Handgrip strength is also positively correlated with total lean mass but negatively correlated with increased body fat [10]. In the epidemiological studies, walking (gait) speed and balance are considered “vital signs” in older adults. Their decrease is viewed as a compelling predictor of functional decline and risk for the development of frailty [15]. A higher amount of fat, particularly in the lower extremities, predicts slower walking speeds for both normal and brisk walking, whereas higher lean mass predicts faster walking speeds and balance [10]. Furthermore, BMD, particularly of the femoral neck, is positively correlated with normal and brisk gait speeds [12]. Taken together, these relatively simple tasks appear to identify older adults at risk for falls, frailty, and balance deficits and may indicate a decline in the entire locomotion system. These simple assessments could be an initial and relatively easy means to identify individuals who require further bone and body composition referrals and assessments.
Although there is a particular risk associated with each individual condition (osteopenia/osteoporosis, sarcopenia, and obesity), functional decline may be more aggravated in osteosarcopenic obesity, where there is the simultaneous presence of sarcopenia, osteopenia, and obesity.
The purpose of this study was to (a) identify cohorts of women with osteosarcopenic obesity, osteopenic/osteoporotic obesity, and sarcopenic obesity from a population of overweight and obese, white postmenopausal women and (b) evaluate measures of physical performance in all three groups and compare the results to obese-only (OB) women. We hypothesized that women with OSO will present with the lowest values for physical performance measures, including handgrip strength and measures of gait and balance, which might put them at increased risk for falls, fractures, and other morbidity conditions.
Methods
Participants
The participants were selected from over 300 Caucasian postmenopausal women recruited via newspaper and senior center advertisements and enrolled in two longitudinal clinical trials. Because of the enrollment criteria of the original two studies, all women had to be relatively healthy, free from chronic diseases such as hypertension, thyroid and/or kidney disease, cancer, diabetes, or severe osteoporosis (T-scores for spine and/or hip lower than −2.5 with the presence of previous/current fractures). In the original studies, women were excluded if they were on hormone replacement therapy or any other medications known to affect bone, body composition, or the endocrine system, 3 months prior to enrolling in the study, or were smoking more than one pack of cigarettes/day and consuming more than one alcoholic drink/day. For this study, baseline data from a total of n = 258 women who were overweight or obese (>35 % body fat) were evaluated. Each participant signed the informed consent, and the protocol was approved by the institutional review board.
Anthropometry and bone densitometry
Standing stature and body weight were measured using a wall stadiometer (Medart, St. Louis, MO, USA) and an electronic platform balance (Seca, Hanover, Maryland) by standard protocols. Body composition of soft (lean and fat) tissue and BMD were measured by dual energy X-ray absorptiometry (DXA) using a Lunar iDXA instrument (GE Medical Systems, Madison, WI, USA), as described previously [10, 12]. Briefly, participants were measured for areal BMD (g/cm2) of total body as well as for the anterior-posterior spine (L1–L4) and femur (neck and total), utilizing separate software for the latter regions of interest. For body composition analysis, the total fat (kg and %), total lean mass (kg), and arm and leg lean mass (kg) were derived from the total body scan. Each computer-derived scan analysis was checked immediately and manually corrected when the automated lines were not properly positioned. The quality analysis for the densitometer was conducted on a daily basis using a standard aluminum spine block (phantom) provided by the manufacturer. Measurements of the phantom were within the manufacturer’s tolerance, with a coefficient variation of less than 0.5 %.
Classification of the participants
A total of n = 258 participants having ≥35 % body fat as assessed using an iDXA instrument were included for further classification into each of four groups. The criterion previously used by Baumgartner et al. [16] compares appendicular lean mass (ALM) with height squared. However, this definition often underestimates sarcopenia in the overweight/obese [8, 17, 18]. Therefore, we used the method developed by Newman et al. which adjusts ALM for both height (m) and fat mass (kg) using a linear regression model [8]. Residuals from the linear regression were then used to identify those individuals whose ALM (obtained from iDXA) was higher or lower than the predicted values for their height and fat mass. Thus, negative residuals (values below the predicted value) indicate a sarcopenic state and positive residuals a more muscular state. The 20th percentile of the residual distribution was used as the cutoff point for sarcopenic obesity, with the following equation: ALM = − 17.4 + 18.3 × height (m) + 0.16 × body fat (kg), and a residual cutoff value of −1.43. This analysis revealed a significant relationship (p < 0.0001) between sarcopenia and fat mass, based on which 60 women (n = 60) were identified as having sarcopenic obesity. Low BMD was defined as having T-scores lower than −1 SD from the reference population mean. Of the 60 sarcopenic obese women, 32 (n = 32) were identified as having L1–L4 and/or total femur T-scores below −1, classifying them into the OSO group. The remaining 28 (n = 28) with normal T-scores were classified into the SO group. The women without SO, but with lower than −1 T-scores for L1–L4 and/or total femur, were classified into the OO group (n = 99). Finally, the obese women with normal T-scores and without sarcopenia were classified in the OB group (n = 99). Figure 1 presents the flowchart for the classification of subjects into each of the groups.
Physical performance measures
The measures of physical performance that participants completed for this study included handgrip strength, normal and brisk walking speeds and the number of steps for each, and left and right leg stance, as described previously [10, 12]. Briefly, handgrip strength was measured using a Lafayette instrument hand dynamometer (Lafayette, Indiana). With the arm extended at a 45° angle, the participant squeezed the handgrip with full force while exhaling. This test was repeated three times on each side. The highest strength was selected for each hand, and the values of both hands were added together and are presented. Normal and brisk walking speeds and the number of steps for each were tested in an 8-m-long hallway and were repeated twice with the average time and number of steps recorded and presented. Briefly, each woman started from a standing position behind the line and continued walking for several steps beyond the 8-m end line. For normal gait speed, women were told to walk from a marked starting line to an 8-m ending mark as if they were walking down a hallway in their own home. For brisk gait speed, women were asked to walk as quickly as possible without actually running. Time was measured in seconds with a stopwatch and rounded to the nearest hundredth of a second. Step numbering started with first heel strike counted and ended when footfall touched or crossed over the 8-m line. The left and right leg stance time was measured by asking each participant to stand on one leg for up to 30 s with the other limb elevated. The time was measured with a stopwatch starting when a participant was in the correct position and ending when any body part touched a supporting surface [10, 12].
Dietary and physical activity assessment
The participants’ dietary intake was assessed by 3-day dietary records (two weekdays and one weekend day) as well as by recording multivitamin/mineral supplement consumption. Dietary records were analyzed using Food Processor, software version 10.1.0 (ESHA Research, Salem, OR, USA). All nutrient and energy intakes were estimated using the software, but only energy, protein, calcium, and vitamin D intakes were used in this study. The amounts from supplements (namely those for calcium and vitamin D) were added to the amount from food and reported as the total intake. Physical activity was assessed using the Allied Dunbar National Fitness Survey for older adults that assesses activities such as heavy housework, gardening, step climbing, and recreational/sport activities, as described previously [19]. Data collected included frequency and duration of each activity and were reported as hours per week on the basis of the previous 4 weeks. Activity scores were created by summing hours per week engaged in each of the activities as well as the sum of all activities. The total activity score was used in the analyses.
Serum 25-hydroxy vitamin D
Serum 25-hydroxy vitamin D (25(OH)D) concentration was measured from the fasting blood sample by a competitive enzyme-linked immunosorbent assay (ELISA; Alpco Diagnostics, Salem, NH, USA). The intra-assay precision (% coefficient variation) was 5.3–6.7 % based on 10 runs, and the inter-assay precision was 4.6–8.7 % based on 11 runs.
Statistical analysis
Descriptive statistics and independent t tests were conducted to provide population characteristics and compare means. Data were expressed as mean ± SD, unless otherwise stated. All variables were tested using the Kolmogorov-Smirnov test for normality and log transformed when the distribution was not normal. Unequal variance t tests were utilized when Levene’s test of homogeneity of variance was considered significant; these tests have been shown to contribute the least to type I and II errors. Variables from physical performance measurements were compared between OSO, OO, SO, and OB women using analysis of covariance (ANCOVA) controlled for age and BMI, followed by Bonferroni corrections. All statistical tests were conducted using SPSS version 21.0 for Windows, SAS (version 9.3, 2013; SAS Institute Inc., Cary, NC, USA) and JMP (version 10, 2012; SAS Institute Inc., Cary, NC, USA). For all analyses, a p < 0.05 was considered statistically significant.
Results
The study included a total of n = 258 obese (% body fat ≥35), white postmenopausal women with age of 61.6 ± 7.4 years and BMI of 29.1 ± 4.5 kg/m2. Table 1 shows the descriptive characteristics of subjects, including anthropometrics, bone and body composition values, dietary and physical activity parameters, and serum vitamin D. Weight and BMI were significantly lower in the OSO and OO groups, so the subsequent analyses of physical performance measures were controlled for BMI and age.
Total and appendicular lean mass was significantly lower in both the OSO and SO groups, compared to OO and OB groups, confirming our classification of women with and without sarcopenia. Although only the women with ≥35 % of body fat were evaluated in this study, the OO group had the lowest % body fat (42.7 %), which was significantly lower than either the OSO or SO group, but not the OB group. However, total body fat (kg) was significantly higher in the SO and OB groups. The BMD of the total body, femur, and spine and the T-scores of both the femur and spine differed significantly between OSO and OO groups compared to SO and OB groups, with the OSO and OO women having lower values for all, again confirming the correct classification of participants. Regarding dietary intake, protein and calcium intake was not statistically significant among groups; however, in the SO group, daily protein intake (per kg/body weight) had the lowest value and was significantly different from other groups. The habitual activity level was not significantly different among the groups and neither was serum 25(OH)D, although dietary vitamin D was significantly lower in the SO group compared to other groups. Mean serum 25(OH)D values were in an adequate range with respect to bone and overall health requirements in all groups, as per the Institute of Medicine classification [20] (Table 1).
Among the physical performance measures (controlled for BMI and age), the handgrip strength, normal and brisk walking speed, and each leg stance were the lowest in the OSO group (Figs. 2, 3, and 4). For handgrip strength, the lowest value in the OSO group was followed by the SO group, with both OSO and SO groups significantly different from the OB group. There was no significant difference between the OSO, SO, and OO groups, and neither the OO group was significantly different from the OB group (Fig. 2). The OSO group also presented with the slowest normal and brisk walking speed, followed by the SO and OO groups, and all the three groups were significantly different from the OB group for normal speed, while only the OSO and SO groups were statistically significant from the OB group for the brisk speed. There was no statistical difference in normal or brisk walking speed between the OSO, SO, and OO groups (Fig. 3). Lastly, the OSO group had the shortest time for both left and right leg stance tests, followed by the SO and OO groups. However, only the OSO group was statistically different from the OB group (Fig. 4).
Discussion
The objective of this study was to identify women with osteosarcopenic obesity, osteopenic obesity, sarcopenic obesity, and obesity alone, in a population of generally healthy overweight and obese postmenopausal women, and to then compare measures of physical performance among the groups. For this study, obesity was not defined using BMI, rather it was determined using a percent body fat cutoff of ≥35 %. Some authors suggested the cutoff for obesity to be >30 and >40 % of total body fat for men and women, respectively [21]. However, we used a lower cutoff value (≥35 %) based on the latest findings in overweight/obese women, indicating a threshold of 33 and 38 % of total body fat at which BMD of femoral neck and lumbar spine, respectively, starts to decline [22]. Furthermore, the most recent American Society of Bariatric Physicians board recommends cutoffs of 25 and 30 % of body fat for men and women, respectively, to classify those with obesity [23]. Additionally, OSO does refer not only to the clinically obese people who fit into the category of having a BMI of >30 kg/m2 but also to those in whom adipose tissue infiltrates into both muscle and bone, impairing each tissue’s physiology and functioning. Therefore, the cutoff ≥35 % of total body fat, by iDXA, seems to be more appropriate for detecting fat infiltration, rather than extending the cutoff to 40 % to correspond to the BMI obesity classification, the latter also being rather arbitrary and widely criticized as a universal criterion for overweight/obesity classification [24, 25]. An interesting finding was that the OSO and SO groups had the highest % body fat, even though total body fat (kg) was significantly higher in the SO and OB groups, suggesting that fat infiltration of muscle and bone is occurring.
A somewhat surprising but important finding was the high percentage of osteopenia/osteoporosis (50.8 %) compared to sarcopenia (23.3 %) in this population of women, providing further evidence that overweight/obesity, or more specifically body fat, is not protective for bones. It could also be possible that the current method used to identify sarcopenic obesity [8, 17] underestimates its prevalence and some refinement and more investigation is warranted.
The OSO group had significantly lower scores for handgrip strength and slower normal and brisk walking speeds as well as smaller steps (thus a higher number) for both normal and brisk walk (not presented), compared to the OB group. Although the values for these measures were the lowest in the OSO group, they were not significantly different from OO and SO groups, suggesting that all three tissues are important when considering handgrip strength and walking speed. The SO group was also significantly lower than the OB group, but that was not the case with the OO group for any of the above variables (Figs. 2 and 3). Shin et al. [10] found both handgrip strength and walking speed to be positively associated with lean mass and negatively with fat mass in older women. Additionally, femoral neck BMD was lower in women with a slower walking speed, while those with lower grip strength had lower total BMD [10, 12]. Therefore, these findings indicate that sarcopenia, osteopenia, and increased fat mass, as seen in the OSO group, may explain some of the inferior physical performance measures, namely grip strength, slower gait speeds, and smaller steps in this cohort. In the case of the leg stance time, only the OSO group was significantly lower from the OB group, indicating that the combined condition of osteosarcopenic obesity has the greatest impact on balance.
There were also significant differences between groups in relation to their dietary intake of certain nutrients. Daily protein intake per kilogram of body weight (although adequate, as all mean group intakes were at or above the recommended daily intake) was significantly lower in the SO group (Table 1). This could have contributed to the lower performance outcomes in that group, although they were not significantly lower compared to the OSO group. A larger sample size may have helped understand what this result means. Vitamin D intake was significantly lower in the SO group compared to all the other groups; however, vitamin D status (serum 25(OH)D) was adequate, above 20 ng/mL, in all the groups (Table 1). Although dietary vitamin D intake was far below the recommendations [20], this discrepancy is probably due to the limitations of dietary records assessment. Recent studies show that vitamin D status (assessed as serum 25(OH)D), especially in older adults, influences physical performance, where the lower concentrations appear to contribute to poorer outcomes [26]. The energy intake of women in all groups was low which seems paradoxical with regard to their size and energy needs. These low-energy intake levels might be due to underreporting and/or inaccuracies in the assessment of food intake via dietary records. However, they might also present a true low-energy intake which does not result in weight loss, due to a very low metabolic rate characteristic for the overweight/obese postmenopausal women, as previously shown [10, 27].
These initial findings in osteosarcopenic obese women regarding the poorer physical performance are important, as they may be the first indicators of future frailty and risk for long-term disability in this population. Overweight and obese women, in general, are not being evaluated for frailty and fractures. With the new concept of osteosarcopenic obesity, and now considering its association with lower functional abilities compared to obesity alone, individuals from this group should be evaluated and subsequently informed regarding preventive measures. A recent review of hip fracture treatments identified the presence of pre-fracture frailty as a factor in suboptimal recovery and morbidity. Patients who were more limited in activities of daily living at the time of hip fracture had a significantly greater functional loss in the first year following the fracture [28]. Reduced grip strength has also been shown to lead to a greater propensity for fragility fractures and associated morbidity [29]. Similarly, walking performance/gait speed and balance were identified as the most reliable and accurate measures of frailty in older women, even better than chronological age [29, 30].
The increased pattern of frailty in women with osteosarcopenic obesity can also be examined on a cellular level, taking into consideration all three tissues: bone, muscle, and adipose. As pointed out previously [1, 22], adipose tissue can be detrimental to bone, contrary to conventional thought. Historically, obesity was thought to be protective against bone fracture and frailty. Although bone fractures are seen more in individuals with a low BMI (<20 kg/m2) and less as one approaches a normal weight (BMI 20–25 kg/m2), research has shown the relationship between BMI and hip fracture to be a U-shaped curve, where BMI showed limited protection at levels of obesity (BMI ≥ 30) [22] and even appeared to increase hip fracture risk [31]. Utilizing computed tomography, Lang et al. [32] found that fat infiltration, or myosteatosis of thigh muscles, led to an increase in hip fracture. Obese individuals and especially those with increased visceral fat, have higher circulating levels of inflammatory cytokines, TNF-α, IL-1 IL-6, and C-reactive protein [33, 34]. This is in effect of a state of a low-grade chronic inflammation that is perpetuated by further increases in fat accumulation as well as the deterioration of bone [34]. On the molecular level, osteoblasts and adipocytes share a common mesenchymal stem cell lineage which, when deregulated by inflammation, increases adipogenesis and suppresses osteoblastogenesis and myogenesis [1, 35].
This study has some limitations. Osteosarcopenic obesity is a newly defined condition, and the cutoff points are not well established [1, 2]. Although the cutoffs for osteopenia/osteoporosis have been established earlier, the same is not true for the osteopenic obesity and sarcopenic obesity, which are essentially in their infancy but are beginning to be refined by the scientific community [1, 14]. This is the first study estimating the prevalence of OSO in a cohort of overweight/obese postmenopausal women, and the cutoffs are based on the available literature and clinical practice. It is a necessary starting point for future refinement. Despite some insufficiencies in defining OSO, our analysis of the critical variables used to define the condition (lean and bone mass), in women, was confirmatory of the classifications for OSO, OO, SO, and OB, as described above. Another limitation is that the women in this study were all generally healthy and relatively young (∼62 years), resulting in a low prevalence (12.4 %) of OSO, thus limiting the generalizability of the results, although it did provide better homogeneity. Similarly, the number of SO cases was low at 10.8 %. These low numbers in the OSO and SO groups provided a limited power for the comparison with other groups. This required the use of unequal variance t tests to compare means between groups, the method noted to be within the nominal 5 % value of type I and II error rates [36, 37]. However, our results do highlight the need for screening. In our population of overweight and obese (initially by BMI) postmenopausal women who were perceived as being relatively healthy, only 38.4 % were actually diagnosed as obese only; the other 61.6 % of women had low bone mass and/or low muscle mass or both. Osteoporosis is already known as a silent disease, but it is possible that muscle loss (sarcopenia) may also be considered as a silent disease.
In conclusion, the osteosarcopenic obese women experiencing decreased BMD and muscle mass, in combination with increased adiposity, had the lowest scores for handgrip strength, walking speed, and balance compared to women who were only osteopenic obese, sarcopenic obese, or obese only (with normal bone and muscle mass). Although these findings are preliminary and the study has been conducted in generally healthy postmenopausal women, the results indicate that OSO carries with it a higher risk for frailty and fracture risk in women. The evaluation of even older individuals and those with some comorbidities (e.g., diabetes, cancer) and older males might be even more relevant to the clinicians. This study also provides the basis for new, either retrospective or prospective, studies to determine better diagnostic cutoffs for each separate condition that makes up OSO. Further research with larger sample size, perhaps investigating more diverse population and with various comorbidities in which adiposity is not clinically apparent (based on BMI classification), is warranted.
References
Ilich JZ, Kelly OJ, Inglis JI, Panton LB, Duque G, Ormsbee MJ (2014) Interrelationship among muscle, fat, and bone: connecting the dots on cellular, hormonal, and whole body levels. Ageing Res Rev 15:51–60
Ormsbee MJ, Prado CM, Ilich JZ, Purcel S, Siervo M, Folsom A, Panton L (2014) Osteosarcopenic obesity: the role of bone, muscle and fat in health. J Cachexia Sarcopenia Mus 5:183–192
Walsh MC, Hunter GR, Livingstone MC (2006) Sarcopenia in premenopausal and postmenopausal women with osteopenia, osteoporosis and normal bone mineral density. Osteoporos Int 17:61–67
International Osteoporosis Foundation. www.iofbonehealth.org/facts-statistics. Accessed August 2014
Kanis JA, McCloskey EV, Johansson H, Oden A, Strom O, Borgstrom F (2010) Development and use of FRAX in osteoporosis. Osteoporos Int 21(Suppl 2):S407–S441
Roux S, Cabana F, Carrier N, Beaulieu M, April PM, Beaulieu MC, Boire G (2014) The World Health Organization fracture risk assessment tool (FRAX) underestimates incident and recurrent fractures in consecutive patients with fragility fractures. Clin Endocrinol Metab 7:2400–2408
Bolland MJ, Siu AT, Mason BH, Horne AM, Ames RW, Grey AB, Gamble GD, Reid IR (2011) Evaluation of the FRAX and Garvan fracture risk calculators in older women. J Bone Miner Res 26:420–427
Newman AB, Kupelian V, Visser M, Simonsick E, Goodpaster B, Nevitt M, Kritchevsky SB, Tylavsky FA, Rubin SM, Harris TB (2003) Sarcopenia: alternative definitions and associations with lower extremity function. J Amer Geriatric Soc 51:1602–1609
Binkley N, Krueger D, Buehrin B (2013) What’s in a name revisited: should osteoporosis and sarcopenia be considered components of “dysmobility syndrome?”. Osteoporos Int 24:2955–2959
Shin H, Liu PY, Panton LB, Ilich JZ (2014) Physical performance in relation to body composition and bone mineral density in healthy, overweight and obese postmenopausal women. J Ger Phys Therapy 37:7–16
Shin H, Panton LB, Dutton GR, Ilich JZ (2011) Relationship of physical performance with body composition and bone mineral density in individuals over 60 years of age: a systematic review. J Aging Res. doi:10.4061/2011/191896
Lindsey C, Brownbill RA, Bohannon RA, Ilich JZ (2005) Association of physical performance measures with bone mineral density in postmenopausal women. Arch Phys Med Rehab 86:1102–1107
Savino E, Martini E, Lauretani F, Pioli G, Zagatti AM, Frondini C, Pellicciotti F, Giordano A, Ferrari A, Nardelli A, Davoli ML, Zurlo A, Lunardelli ML, Volpato S (2013) Handgrip strength predicts persistent walking recovery after hip fracture surgery. Am J Med 126:1068–1075
Cruz-Jentoft AJ, Landi F, Schneider SM, et al. (2014) Prevalence of and interventions for sarcopenia in ageing adults: a systematic review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS). Age Ageing. 2014; pii: afu115
Lusardi MM (2012) Is walking speed a vital sign? Absolutely! Top Ger Rehab 28:67–76
Baumgartner RN, Koehler KM, Gallagher D, Romero L, Heymsfield SB, Ross RR, Garry PJ, Lindeman RD (1998) Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol 147:755–763
Domiciano D, Figueiredo C, Lopes J, Caparbo V, Takayama L, Menezes P, Bonfak E, Pereirak R (2012) Discriminating sarcopenia in community-dwelling older women with high frequency of overweight/obesity: the Sao Paulo Ageing & Health Study (SPAH). Osteoporos Int 24:595–603
Lourenco R, Perez-Zepeda M, Gutierrez-Robledo L, Rodriguez-Manas L, Garcia-Garcia F (2015) Performance of the European Working Group on Sarcopenia in Older People algorithm in screening older adults for muscle mass assessment. Age Ageing 44:334–8. doi:10.1093/ageing/afu192
Ilich JZ, Brownbill RA (2008) Habitual and low-impact activities are associated with better bone outcomes and lower body fat in older women. Calcif Tissue Int 83:260–271
Institute of Medicine of the National Academies (2012) Dietary reference intakes for calcium and vitamin D. Report. National Academy of Sciences, USA
Dufour AB, Hannan MT, Murabito JM, Kielk DP, McLean RR (2013) Sarcopenia definitions considering body size and fat mass are associated with mobility limitations: the Framingham Study. J Gerontol A Biol Sci Med Sci 68:168–174
Liu P-Y, Ilich JZ, Brummel-Smith K, Ghosh S (2014) New insight into fat, muscle and bone relationship in women: determining the threshold at which body fat assumes negative relationship with bone mineral density. Inter J Prev Med 5:1452–1463
American Society of Bariatric Physicians (ASBP) (2015) Obesity algorithm. http://www.asbp.org/obesityalgorithm.html
Shah NR, Braverman ER (2012) Measuring adiposity in patients: the utility of body mass index (BMI), percent body fat, and leptin. PLoS ONE 7(4):e33308. doi:10.1371/journal.pone.0033308
Peterson MD, Al Snih S, Stoddard J, Shekar A, Hurvitz E (2014) Obesity misclassification and the metabolic syndrome in adults with functional mobility impairments: Nutrition Examination Survey 2003-2006. Prev Med 60:71–76
Lagari VS, Gómez-Marín O, Levis S (2014) Study design and baseline characteristics of participants in the vitamin D in vulnerable adults at the VA (the VIVA Study). Contemp Clin Trial 39:66–73
Shin H, Shin J, Liu P-Y, Dutton GR, Abood DA, Ilich JZ (2011) Self efficacy improves weight loss in overweight/obese postmenopausal women during a 6-month weight loss intervention. Nutr Res 31:822–828
Beaupre LA, Binder EF, Cameron ID, Jones AC, Orwig D, Sherrington C, Magaziner J (2013) Maximizing functional recovery following hip fracture in frail seniors. Best Pract Res Clin Rheumatol 27:771–788
Theou O, Jones GR, Jakobi JM, Mitnitski A, Vandervoort AA (2011) A comparison of the relationship of 14 performance-based measures with frailty in older women. Appl Physiol Nutr Metab 36:928–938
Viana JU, Silva SLA, Torres JL, Dias JMD, Pereira LSM, Dias RC (2013) Influence of sarcopenia and functionality indicators on the frailty profile of community-dwelling elderly subjects: a cross-sectional study. Braz J Phys Ther 17:373–381
De Laet C, Kanis J, Odén A, Johanson H, Johnell O, Delmas P, Eisman JA, Kroger H, Fujiwara S, Garnero P, McCloskey EV, Mellstrom D, Melton LJ, Meunier PJ, Pols HA, Reeve J, Silman A, Tenenhouse A (2005) Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos Int 16:1330–1338
Lang T, Cauley J, Tylavsky F, Bauer D, Cummings S, Harris T (2010) Computed tomographic measurements of thigh muscle cross-sectional area and attenuation coefficient predict hip fracture: the health, aging, and body composition study. J Bone Miner Res 25:513–519
Pradhan AD, Manson JE, Rifai N, Buring JE, Ridker PM (2001) C-reactive protein, interleukin 6, and risk of developing type 2 diabetes mellitus. JAMA 286:327–334
Liu P, Hornbuckle L, Panton L, Kim J, Ilich J (2012) Evidence for the association between abdominal fat and cardiovascular risk factors in overweight and obese African American women. J Am Coll Nutr 31:126–132
Ilich JZ, Kelly OJ, Kim Y, Spicer MT (2014) Low-grade chronic inflammation perpetuated by modern diet as a promoter of obesity and osteoporosis. Arch Indust Hygiene Toxicol 65:139–148
Coombs WT, Algina J, Oltman D (1996) Univariate and multivariate omnibus hypothesis tests selected to control type I error rates when population variances are not necessarily equal. Rev Educ Res 66:137–179
Zimmerman DW, Zumbo BN (1993) Rank transformations and the power of the Student t test and Welch t’ test for non-normal populations. Can J Exp Psychol 47:523
Acknowledgments
This work was funded in part by the USDA grant (2004-05287) and the Hazel K. Stiebeling Fellowship award.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ilich, J.Z., Inglis, J.E., Kelly, O.J. et al. Osteosarcopenic obesity is associated with reduced handgrip strength, walking abilities, and balance in postmenopausal women. Osteoporos Int 26, 2587–2595 (2015). https://doi.org/10.1007/s00198-015-3186-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-015-3186-y