Abstract
Summary
Heart failure is associated with increased risk of osteoporosis. We evaluated the prevalence and predictors of osteoporosis in hospitalized patients with ADHF using quantitative computed tomography. Osteoporosis and vertebral fracture are prevalent in patients with ADHF and exercise capacity independently predicts bone mass and femoral bone geometry.
Introduction
Heart failure is associated with reduced bone mass and increased risk of osteoporotic fractures. However, the prevalence and predictors of osteoporosis in hospitalized patients with acute decompensated heart failure (ADHF) are not well understood.
Methods
Sixty-five patients (15 postmenopausal females and 50 males) with ADHF were prospectively and consecutively enrolled. After stabilization of heart failure symptoms, quantitative computed tomography for bone mineral density (BMD) and femoral geometry as well as biochemical, echocardiographic, and cardiopulmonary exercise tests were performed.
Results
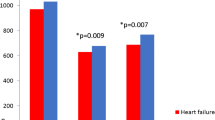
Fifteen postmenopausal female showed a high prevalence of osteoporosis (40 %) and vertebral fracture (53 %). Among 50 male patients, 12 % had osteoporosis and 32 % had osteopenia, while vertebral fracture was found in 12 %. Lumbar volumetric BMD (vBMD) was significantly lower in ischemic patients than non-ischemic patients (107.9 ± 47.5 vs. 145.4 ± 40.9 mg/cm3, p = 0.005) in male. Exercise capacity, indicated by peak oxygen consumption (VO2), was significantly associated with lumbar vBMD (r = 0.576, p < 0.001) and total hip areal BMD (aBMD) (r = 0.512, p = 0.001) and cortical thickness of the femur neck (r = 0.544, p = 0.001). When controlled for age, body mass index, N-terminal proBrain natriuretic protein (NT-proBNP), etiology of heart failure, hemoglobin, and thigh circumference, multivariate regression analysis revealed peak VO2 independently predicted lumbar vBMD (β = 0.448, p = 0.031), total hip aBMD (β = 0.547, p = 0.021), and cortical thickness of the femur neck (β = 0.590, p = 0.011).
Conclusion
In male patients with ADHF, osteoporosis and vertebral fracture are prevalent, and exercise capacity independently predicts bone mass and geometry. Given that heart failure patients with reduced exercise capacity carry a substantial increased risk of fracture, proper osteoporosis evaluation is important in these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Heart failure is associated with reduced bone mineral density (BMD) and increased risk of osteoporotic fractures, especially of the hip [1–3]. A population-based analysis of more than 16,000 patients revealed that heart failure is associated with an increased risk of subsequent fractures [1]. Another long term follow-up cohort study over 11 years revealed that patients with newly diagnosed heart failure are at a high risk for hip fractures [2]. A recent population-based cohort study of more than 45,500 adults showed that heart failure is associated with a 30 % increase in major fractures that is independent of traditional risk factors [3]. Moreover, mortality following hip fractures was markedly increased (~twofold) in both men and women with heart failure and a hip fracture, compared with those with heart failure who did not sustain a hip fracture [2]. However, the exact prevalence or predictors of osteoporosis in heart failure is not known. Furthermore, there has never been a detailed analysis of bone health in patients with heart failure evaluating parameters of bone quality and strength including bone turnover markers and geometric analysis besides BMD.
Previous studies of BMD measurements were done mainly in patients with chronic stable heart failure rather than in patients with acute decompensated heart failure (ADHF) [2–6]. Regarding ADHF patients, after proper decongestion and clinical stabilization, it is necessary to evaluate and manage co-morbidities before discharge. However, major heart failure guidelines do not cover the screening method or patient education in terms of osteoporosis or osteoporotic fracture, even though heart failure portends a substantial increased risk of fracture [7, 8]. Therefore, we evaluated the prevalence and predictors of osteoporosis in prospectively and consecutively enrolled ADHF patients. Dual-energy X-ray absorptiometry (DXA) is a widely accepted method to measure BMD to diagnose the osteoporosis. However, DXA has the limitation in that trabecular and cortical bone compartments are analyzed without distinction. Because the anatomic composition ratio of trabecular to cortical bone may be important for determining the resistance to fractures, we used quantitative computed tomography (QCT), which can measure BMD of the trabecular and cortical bone compartments separately. In addition, the use of QCT to calculate bone geometry parameters such as cortical thickness and buckling ratio (BR) may reveal the explanation for increased hip fractures in ADHF patients.
It is well known that physical fitness and exercise capacity are important in maintaining bone mass in the general population. In addition, exercise capacity already is associated with bone mass in various disease states such as cystic fibrosis [9], chronic obstructive pulmonary disease [10], rheumatoid arthritis [11], and in survivors of childhood leukemia [12]. To evaluate the relationship between exercise capacity and bone mass in ADHF patients more precisely, we performed the cardiopulmonary exercise test (CPET) in all subjects after clinical stabilization with guideline-directed medical treatment.
In this study, we evaluated the prevalence and predictors of osteoporosis in patients with ADHF using QCT which can measure bone mass and geometry exquisitely. We hypothesized that exercise capacity measured by CPET would correlate with various bone parameters and proximal femoral geometry in these patients.
Materials and methods
Study population
Patients diagnosed with ADHF at Severance Cardiovascular Hospital were prospectively and consecutively enrolled between May 2012 and February 2013. Stabilized, ambulatory ADHF patients who had signs or symptoms of heart failure and one of the following criteria were eligible for the study: (i) lung congestion or (ii) objective findings of left ventricular systolic dysfunction or structural heart disease. Lung congestion was defined as “congestion” on a chest X-ray or as rales on physical examination. Patients with a history of pre-existing osteoporosis or osteoporotic fracture and a history of disorder that could possibly influence bone and mineral metabolism, such as hyperparathyroidism and overt thyroid functional disorder, were excluded from this study. In addition, patients were excluded if they had previously used drugs, such as glucocorticoids, estrogen, selective estrogen receptor modulators, and bisphosphonates that are known to impact bone and mineral metabolism. Informed consent was obtained from each patient, and the study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in a priori approval by the institutional review board of Severance Hospital (4-2012-0027).
Anthropometric, biochemical, and echocardiographic analysis
Height and weight were measured by standardized techniques and equipment. Waist circumference was measured at the midpoint between the lower margin of the least palpable rib and the top of the iliac crest. Hip circumference was measured around the widest portion of the buttocks. Thigh circumference was measured directly below the gluteal fold of the right thigh.
Blood samples were obtained after an 8-h overnight fast by venipuncture into plain and EDTA tubes. Complete blood count, serum sodium, serum calcium, uric acid, total cholesterol, and serum creatinine were measured using standard automated laboratory techniques. We estimated glomerular filtration rate (eGFR) using the Modification of Diet in Renal Disease formula. Plasma N-terminal probrain natriuretic peptide (NT-proBNP) was measured by electrochemiluminescence immunoassay (Elecsys proBNP; Roche Diagnostics, Basel, Switzerland); intra- and inter-assay coefficients of variations (CVs) were <1.3 and <1.7 %, respectively. NT-proBNP was drawn on the day of admission or the day after admission, at about the same time as echocardiographic measurements. Plasma high sensitivity C-reactive protein (hsCRP) levels were measured using an immunonephelometric method on a BNII analyzer (Dade-Behring, Germany) with the manufacturer’s reagents. The detection limit for hsCRP was 0.2 mg/L; intra- and inter-assay CVs were <5 %, respectively. Serum levels of osteocalcin (CIS Bio International, Gif-sur-Yvette, France; intra- and inter-assay CVs were <2.0 and <5.0 %, respectively) and serum carboxy-terminal cross-linking telopeptide of type 1 collagen (CTx) (Osteomark, Ostex International, Seattle, WA, USA; intra- and inter-assay CVs were <5.8 and <5.9 %, respectively) were measured by ELISA. Intact parathyroid hormone (PTH, IRMA; Biosource, Nivelles, Belgium; intra- and inter-assay CVs were <2.7 and <3.5 %, respectively) and 25-OH-VitD (D3-RIA-CT, Biosource, Nivelles, Belgium; intra- and inter-assay CVs were <11.0 and <12.5 %, respectively) were analyzed by radioimmunoassay.
Almost all echocardiographic measurements were performed at a relatively consistent time point for all of the cohort, that is, on the day of admission or the day after admission (median time was 1 day). Left ventricular ejection fraction (LVEF) was measured using the modified Quinones method [13]. In patients with regional wall motion abnormalities, the LVEF was calculated using Simpson’s biplane method with apical four- and two-chamber views [14].
Analysis of bone density and geometry
Densitometry measurements were performed using QCT in all subjects. BMD of the spine, femoral neck, and total hip were calculated from single-energy CT scans at the lumbar spine and proximal femur with a multidetector Light Speed QX-I scanner (GE Medical Systems, Waukesha, WI, USA). Three-dimensional CT images were analyzed by QCT PRO CTXA software (Mindways Software, Austin, TX, USA) to measure lumbar volumetric BMD (vBMD), areal BMD (aBMD) of the total hip, and femoral geometry. For the spine scan, the subject was placed in supine position on the scanner table and the L1 and L2 vertebrae were imaged after identifying their locations on a lateral scout view. The average of the two vBMD values was taken. After the spinal measurement, the calibration phantom was centered between the subject’s left hip and the region from just superior to the acetabulum to 3–5 mm inferior to the lesser trochanter was imaged. Quality-control measures, including weekly scanning of the calibration phantom and use of scan protocols for all participants, were performed at Severance Hospital. For the classification of osteoporosis and osteopenia, we used lumbar vBMD (osteoporosis: lumbar vBMD <80 mg/cm3; osteopenia: lumbar vBMD of 80–120 mg/cm3).
The aBMD, cortical thickness, and BR of the femoral neck and total hip also were analyzed. The total hip measurement included all of the femoral neck, trochanter, and intertrochanter region. The cortical thickness was calculated as the cortical average depth, which was derived from the following equations:
where A = area, BMC = bone mineral content, and V = volume.
The ratio of aBMD to vBMD is the average depth of the region of interest (ROI), that is, Average depth = aBMD/vBMD = (BMC/A)/(BMC/V) = V/ABR, known as the ratio of radius over cortical thickness, was calculated by taking the ratio of the volume of the femoral ROI over the volume of cortical bone (Vc) in the femoral ROI:
A clinically significant vertebral compression fracture was defined as grade 2 (moderate) or grade 3 (severe) [5, 15].
Assessment of exercise capacity
The CPET was performed after “clinical stabilization” according to current medical guidelines. Clinical stabilization was defined as readiness for discharge from hospital. Congestion was absent, and a stable, oral diuretic regimen was established for at least 48 h. The median time from admission was 9 days (3–42 days), and the CPET was performed at a relatively consistent time point, that is, on the day of discharge or on the day before discharge. Symptom-limited CPET utilized a treadmill according to the modified Bruce ramp protocol. Patients were strongly encouraged to achieve a peak respiratory exchange ratio (RER) > 1.10. Expired gasses were collected continuously throughout exercise and analyzed for ventilator volume, oxygen (O2) content, and carbon dioxide (CO2) content using a calibrated metabolic cart (Quark CPET, COSMED, Chicago, IL, USA). Expired gasses were reported every 15 s. During the exercise test, monitoring consisted of continuous 12-lead electrocardiography, manual blood pressure measurements at every stage, and heart rate recordings at every stage via electrocardiogram. CPET was terminated according to the following criteria; patient request, ventricular tachycardia, ng to cago, IL, USA). Expired gasses were reported every 1, or a drop in systolic blood pressure entricular tachycardia, ng to cagofied exercise physiologist under the supervision of a physician conducted each test. The following variables were derived from the CPET results: peak oxygen consumption (peak VO2); peak RER, defined by the ratio of CO2 production to O2 consumption at peak effort; and VE/VCO2 slope, defined as the slope of the increase in peak ventilation/increase in CO2 production throughout exercise. Peak RER was the highest 30 s averaged value during the last stage of the test.
Statistical analysis
Continuous variables are presented as mean ± standard deviation. Categorical variables are presented as a percentage of the total group. Discrete variables were compared using the chi-squared method. ANOVA or independent t tests were used for the continuous variables. Post-hoc Bonferroni analysis was used after the ANOVA test for multiple comparisons. Pearson’s correlation analysis was used for the simple correlation between continuous variables. Univariate and multivariate regression analyses were performed to identify independent predictors for the bone mass and geometry in patients with ADHF. All statistical analyses were performed with SPSS version 20.0 (IBM Corporation, Armonk, NY, USA).
Results
High prevalence of osteoporosis in ADHF patients
Clinical characteristics, CPET, laboratory findings, and QCT data of 65 ADHF patients according to gender are summarized in Table 1. Fifteen postmenopausal females and 50 males were analyzed; the average age of the patients was 62 ± 16 years, and the mean ejection fraction of the group was 29.8 ± 13.1 %. The 15 postmenopausal females (69 ± 13 years) with ADHF showed a high prevalence of osteoporosis (40.0 %) and osteopenia (33.3 %) according to lumbar vBMD. In addition, more than half of these patients (53.3 %) had evidence of clinically significant vertebral compression fracture. Male ADHF patients showed relatively high incidence of osteoporosis (12.0 %) and osteopenia (32.0 %). When the male cohort was restricted to those over the age of 50, the prevalence of osteoporosis and osteopenia were even higher (osteoporosis: 15.8 %; osteopenia: 36.8 %). Six male ADHF patients (12.0 %) had incidental vertebral compression fractures as well. Because of the limited numbers of women, we analyzed the prevalence and predictors of osteoporosis only in the male patients.
Factors affecting bone mass and geometry in male ADHF patients
Bone mass showed significant differences according to the etiology of heart failure and exercise capacity in male ADHF patients. Lumbar vBMD was significantly lower in ischemic patients than non-ischemic patients (107.9 ± 47.5 mg/cm3 vs. 145.4 ± 40.9 mg/cm3, p = 0.005). However, there were no significant differences in lumbar vBMD between the patients with newly diagnosed ADHF and acute exacerbation of chronic heart failure (142.0 ± 40.3 mg/cm3 vs. 124.0 ± 50.6 mg/cm3, p = 0.174). In terms of CPET parameters, not only peak VO2, (r = 0.576, p < 0.001) but exercise duration (r = 0.627, p < 0.001) and VE/VCO2 slope (r = −0.423, p = 0.010) were all correlated with lumbar vBMD in these patients. Peak VO2 also was significantly correlated with total hip aBMD (r = 0.512, p = 0.001), femoral neck aBMD (r = 0.537, p = 0.001), cortical thickness of the femoral neck (r = 0.544, p = 0.001), total hip BR (r = −0.343, p = 0.04), and femoral neck BR (r = −0.343, p = 0.05). LVEF was not correlated with bone mass, while log transformed NT-proBNP showed an increased tendency to be observed in patients with reduced bone mass.
Clinical characteristics, CPET, laboratory findings, and QCT data according to lumbar vBMD for male ADHF patients are summarized in Table 2. Representative QCT data in two male patients are shown in Fig. 1. Male ADHF patients with reduced bone mass were older, had a higher proportion of ischemic etiology, and thinner thigh circumference. Markers of bone turnover including osteocalcin and CTx showed no significant differences among the three groups. Regarding other laboratory findings, there were no significant differences in other parameters except for hemoglobin. Not only lumbar vBMD, but aBMD and cortical thickness of the femoral neck and total hip were significantly lower, and BR was significantly higher in the osteoporosis group. The prevalence of vertebral compression fracture was 67 % in patients with osteoporosis.
a 75-year-old ischemic heart failure patient with relatively preserved LVEF (45 %), but decreased exercise capacity (peak VO2 = 12.2 mL/kg/min) showed decreased lumbar vBMD (58.4 mg/cm3). b 56-year-old non-ischemic heart failure patient with severely depressed LVEF (20 %), but preserved exercise capacity (peak VO2 = 24.2 mL/kg/min) showed normal lumbar vBMD (122.5 mg/cm3). LVEF left ventricular ejection fraction, vBMD volumetric bone mineral density
To determine factors relevant to decreased bone mass in male ADHF patients, we performed univariate and multivariate analyses for lumbar vBMD, total hip aBMD, and cortical thickness of the femoral neck; these results are summarized in Table 3. When controlled for age, body mass index, NT-proBNP, etiology of heart failure, hemoglobin, and thigh circumference, multivariate regression analysis revealed peak VO2 independently predicted not only lumbar vBMD, but aBMD of the total hip, and cortical thickness of the femoral neck. Peak VO2, which is a well-known prognostic marker of ADHF, was the only factor that showed persistent statistical significance for various BMD and geometric parameters.
Discussion
The results from this study demonstrated that osteoporosis and vertebral fracture are prevalent in patients with ADHF, even in male ADHF patients. Furthermore, exercise capacity independently predicts lumbar vBMD, hip aBMD, and femoral cortical thickness even after the adjustment for age, BMI, types of heart failure, NT-proBNP, hemoglobin, and thigh circumference.
The pathophysiology of reduced bone mass in heart failure is not well understood. While shared risk factors, such as older age, smoking, diabetes, renal dysfunction, poor nutrition, low 25-OH-VitD levels, various cardiovascular medications, and physical inactivity might contribute to reduced bone mass in these patients, other factors, mainly those related to heart failure, might play a role. For example, reduced tissue perfusion in patients with heart failure might block the proliferation and differentiation of osteoblasts, while strongly stimulating osteoclasts. However, the resorptive function of osteoclasts is not impaired under hypoxic conditions [16]. The negative impact of heart failure on bone metabolism might be associated with the direct impact of reduced pO2 and pH [16]. In addition, neurohormonal activation, manifested by elevated aldosterone levels, has been demonstrated to play a crucial role in the risk of orthopedic fracture in animal models [17]. Furthermore, the use of spironolactone is inversely associated with fractures in men with heart failure [18], suggesting that aldosterone may be important in fracture risk. Recently, Leistner et al. showed a direct pathophysiological relationship between heart failure and catabolic bone remodeling that was associated with an increased osteoporotic fracture risk [19].
Beyond these mechanisms, poor exercise capacity might be another important aggravating factor of osteoporosis in patients with heart failure. To evaluate the relationship between exercise capacity and bone mass in ADHF patients more precisely, we performed CPET in all subjects after clinical stabilization. CPET is an important clinical tool used to determine the severity and prognosis of heart failure. Among the various CPET parameters, peak VO2, which reflects exercise capacity, is a composite index parameter for cardiopulmonary function, lower extremity muscle mass, and muscle strength. In this study, peak VO2 independently and consistently predicted not only lumbar vBMD but also aBMD of the total hip and cortical thickness of the femoral neck, indicating a significant relationship between exercise capacity and bone health in ADHF patients. Skeletal unloading due to prolonged bed rest or poor exercise capacity leads to bone loss via reductions in the mechanical forces applied to bones. The mechanism of this bone loss appears to be due to a decrease in the bone formation rate and a concurrent increase in the bone resorption rate [20]. Trebacz et al. used rat models to show that during even transient periods of immobilization, bone resorption and formation were unbalanced [21]. In contrast to inactivity, exercise appears to increase BMD. Greater physical activity is associated with a 9–17 % increase in BMD during adolescence and young adulthood [22]. Michalopoulou et al. also examined habitual physical activity, using peripheral QCT at the tibia, to gain a better understanding of the structural changes that may underlie the response of bone to exercise [23]. Habitual physical activity affects the geometry of both cortical and trabecular areas of the long bones of premenarchal girls in a dose-dependent manner. Specifically, physical activity increases not only the density of trabecular bone but also the density and size of cortical bone.
To understand why hip fractures are relatively frequent in patients with heart failure, knowledge about femoral geometrical parameters, such as cortical thickness and BR in addition to bone mass, might be helpful to further understand the pathogenesis of hip fractures [24]. Assuming that bone size is similar, cortical thinning increases cortical instability under compressive loads, and bending may lead to increased risk of fractures. As expected, in male ADHF patients with osteoporosis, we found not only lower BMD in general, but also lower femoral neck cortical aBMD and thinner cortical bone as compared to the other groups.
Previous observational studies clearly and consistently showed that heart failure is associated with reduced BMD and increased risk of osteoporotic fractures [1–6]. However, current major heart failure guidelines do not cover the proper screening methods or patient education in terms of osteoporosis or osteoporotic fracture [7, 8]. Therefore, our study as well as other studies may serve as a springboard to discuss the necessities of bone health evaluation in patients with heart failure.
The present study has several potential limitations. First, due to the cross-sectional design of this study, we cannot define, but only suggest, a causal relationship between exercise capacity and bone mass. While exercise capacity certainly could be part of the causal pathway in the relationship between heart failure and osteoporosis, it could also be a marker of disease severity or a confounding variable with sarcopenia and impaired muscle-bone signaling. Second, our study population cannot represent chronic stable heart failure patients. In particular, the effects of heart failure medication on bone mass were not fully assessed because of the characteristics of the study population. The study subjects were hospitalized patients with ADHF, including newly diagnosed heart failure patients. Third, further detailed assessment of biochemical or inflammatory markers could have identified a possible link between exercise intolerance and decreased bone mass. In this study, we only measured markers of bone turnover, NT-proBNP and hsCRP, which were not significantly associated with osteoporosis. Lastly, our QCT data could not show intra-cortical remodeling and porosity because of limited resolution.
In conclusion, we evaluated the prevalence and predictors of osteoporosis in hospitalized patients with ADHF using QCT. Osteoporosis and vertebral fracture are prevalent in patients with ADHF, and exercise capacity independently predicts bone mass and femoral bone geometry. Given that heart failure diagnosis foreshadows a substantially increased risk of fracture, patient education and proper osteoporosis evaluation and treatment are necessary for the prevention of osteoporotic fractures in this population with decreased exercise capacity. Larger prospective studies with a longer follow-up period are necessary to determine the actual risk of osteoporotic fracture and its impact on clinical outcome in these patients.
References
van Diepen S, Majumdar SR, Bakal JA, McAlister FA, Ezekowitz JA (2008) Heart failure is a risk factor for orthopedic fracture: a population-based analysis of 16,294 patients. Circulation 118:1946–1952
Carbone L, Buzkova P, Fink HA, Lee JS, Chen Z, Ahmed A et al (2010) Hip fractures and heart failure: findings from the Cardiovascular Health Study. Eur Heart J 31:77–84
Majumdar SR, Ezekowitz JA, Lix LM, Leslie WD (2012) Heart failure is a clinically and densitometrically independent risk factor for osteoporotic fractures: population-based cohort study of 45,509 subjects. J Clin Endocrinol Metab 97:1179–1186
Jankowska EA, Jakubaszko J, Cwynar A, Majda J, Ponikowska B, Kustrzycka-Kratochwil D et al (2009) Bone mineral status and bone loss over time in men with chronic systolic heart failure and their clinical and hormonal determinants. Eur J Heart Fail 11:28–38
Lyons KJ, Majumdar SR, Ezekowitz JA (2011) The unrecognized burden of osteoporosis-related vertebral fractures in patients with heart failure. Circ Heart Fail 4:419–424
Terrovitis J, Zotos P, Kaldara E, Diakos N, Tseliou E, Vakrou S et al (2012) Bone mass loss in chronic heart failure is associated with secondary hyperparathyroidism and has prognostic significance. Eur J Heart Fail 14:326–332
McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Bohm M, Dickstein K et al (2012) ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the task force for the diagnosis and treatment of acute and chronic heart failure 2012 of the European society of cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J 33:1787–1847
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH et al (2013) 2013 ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation 128:1810–1852
Tejero Garcia S, Giraldez Sanchez MA, Cejudo P, Quintana Gallego E, Dapena J, Garcia Jimenez R et al (2011) Bone health, daily physical activity, and exercise tolerance in patients with cystic fibrosis. Chest 140:475–481
Vaquero-Barrios JM, Arenas-de Larriva MS, Redel-Montero J, Bujalance-Cabrera C, Santos-Luna F, Moreno-Casado P et al (2010) Bone mineral density in patients with chronic obstructive pulmonary disease who are candidates for lung transplant. Transplant Proc 42:3020–3022
Vosse D, de Vlam K (2009) Osteoporosis in rheumatoid arthritis and ankylosing spondylitis. Clin Exp Rheumatol 27:S62–S67
Jarfelt M, Fors H, Lannering B, Bjarnason R (2006) Bone mineral density and bone turnover in young adult survivors of childhood acute lymphoblastic leukaemia. Eur J Endocrinol 154:303–309
Quinones MA, Waggoner AD, Reduto L, Nelson J, Young J, Winters W et al (1981) A new, simplified and accurate method for determining ejection fraction with two-dimensional echocardiography. Circulation 64:744–753
Folland E, Parisi A, Moynihan P, Jones DR, Feldman CL, Tow D (1979) Assessment of left ventricular ejection fraction and volumes by real-time, two-dimensional echocardiography. A comparison of cineangiographic and radionuclide techniques. Circulation 60:760–766
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8:1137–1148
Arnett TR (2010) Acidosis, hypoxia and bone. Arch Biochem Biophys 503:103–109
Chhokar VS, Sun Y, Bhattacharya SK, Ahokas RA, Myers LK, Xing Z et al (2004) Loss of bone minerals and strength in rats with aldosteronism. Am J Physiol Heart Circ Physiol 287:H2023–H2026
Carbone LD, Cross JD, Raza SH, Bush AJ, Sepanski RJ, Dhawan S et al (2008) Fracture risk in men with congestive heart failure risk reduction with spironolactone. J Am Coll Cardiol 52:135–138
Leistner DM, Seeger FH, Fischer A, Roxe T, Klotsche J, Iekushi K et al (2012) Elevated levels of the mediator of catabolic bone remodeling RANKL in the bone marrow environment link chronic heart failure with osteoporosis. Circ Heart Fail 5:769–777
Bikle DD, Halloran BP (1999) The response of bone to unloading. J Bone Miner Metab 17:233–244
Trebacz H (2001) Disuse-induced deterioration of bone strength is not stopped after free remobilization in young adult rats. J Biomech 34:1631–1636
Baxter-Jones AD, Kontulainen SA, Faulkner RA, Bailey DA (2008) A longitudinal study of the relationship of physical activity to bone mineral accrual from adolescence to young adulthood. Bone 43:1101–1107
Michalopoulou M, Kambas A, Leontsini D, Chatzinikolaou A, Draganidis D, Avloniti A et al (2013) Physical activity is associated with bone geometry of premenarcheal girls in a dose-dependent manner. Metabolism 62:1811–1818
Gregory JS, Aspden RM (2008) Femoral geometry as a risk factor for osteoporotic hip fracture in men and women. Med Eng Phys 30:1275–1286
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Youn, JC., Lee, S.J., Lee, H.S. et al. Exercise capacity independently predicts bone mineral density and proximal femoral geometry in patients with acute decompensated heart failure. Osteoporos Int 26, 2121–2129 (2015). https://doi.org/10.1007/s00198-015-3112-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-015-3112-3