Abstract
Introduction and hypothesis
To evaluate the efficacy of vaginal CO2 laser in women with stress predominant urinary incontinence (SUI) compared with the sham treatment.
Methods
A randomized controlled trial with sham treatment was conducted between January 2019 and April 2021. Women with predominant SUI were recruited and randomized into two groups: the CO2 laser group (n = 29) and the sham group (n = 30). The International Consultation on Continence Questionnaire—Urinary Incontinence Short Form (ICIQ-UI SF) was used to evaluate the efficacy at 3 months postoperatively. All participants in both groups were advised to perform pelvic floor muscle training (PFMT) after the intervention.
Results
A total of 59 women were studied. A total of 29 women were included in the CO2 laser group and 30 women were included in the sham group. The baseline scores of the ICIQ-UI SF were similar in both groups. A significant improvement in urinary incontinence scores was found in both groups 3 months after treatment (p < 0.001). However, there were no statistically significant differences between the two groups at 3 months (p = 0.8281). There were no changes in bladder neck descent or levator hiatal area immediately after intervention or 3 months after completion of treatment in either group. Most participants who received the active intervention reported mild vaginal pain during the procedure that resolved spontaneously at the end of treatment.
Conclusions
Fractional CO2 laser treatment does not provide any benefit over the sham technique in alleviating SUI symptoms. The improvement in SUI symptoms in both groups might be related to PFMT.
This study was registered with the Thai Clinical Trial Register (TCTR20190131004).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The use of vaginal lasers is increasingly popular in urogynecology. It is a minimally invasive procedure that is considered a treatment for the relief of mild to moderate symptoms of pelvic floor disorders such as stress urinary incontinence (SUI), pelvic organ prolapse (POP) and genitourinary symptoms of menopause. However, there is no strong scientific evidence to confirm the potential benefit of vaginal lasers [1,2,3] compared to placebo.
Microablative fractional CO2 lasers and non-ablative Er: YAG lasers are the two types of lasers that are commonly used in the vagina. The changes in the morphology of vaginal tissue due to its thermal effect lead to new collagen synthesis [4]. The pulsed laser photothermal effect stimulates collagen neogenesis and morphological changes in the upper dermis [5, 6] and adjacent pelvic floor tissue [7]. The collagen fibers in the vaginal epithelium are contracted when the temperature increases up to 63 ºC. This temperature also induces the processes of neocollagenesis, elastogenesis, neoangiogenesis, and increased fibroblast activity in the applied area [8]. Moreover, such a promising effect also promotes the density of capillaries and the thickness of the vaginal epithelium [9]. This is more theoretical than scientifically proven.
It is estimated that 25–45% of women experience urinary incontinence [10]. The most common type is stress urinary incontinence, which is the involuntary loss of urine resulting in a sudden increase in abdominal pressure, for example, from physical exertion, sneezing, or coughing [11]. The loss of anatomical support causing pelvic floor weakness or bladder neck hypermobility and/or urethral sphincter deficiency are the causes of SUI in the majority of patients [12, 13]. The effect of SUI on quality of life depends on the severity of symptoms. There are many modalities to improve such symptoms. Pelvic floor muscle training, avoiding activities that increase intraabdominal pressure suddenly, can alleviate SUI symptoms. If the symptoms do not improve satisfactorily, surgery is often the next step. While surgery is often considered the most effective method to relieve the SUI symptoms, adverse events, while uncommon, are still reported. Vaginal CO2 lasers are considered to be a minimally invasive therapy and are often considered a step to relieve symptoms before surgery [12, 13].
The data from Han et al. [14] established the association of collagen and SUI. Women with SUI had significantly lower expression levels of type I and type III collagen than women without SUI (p < 0.01); therefore, any interventions (i.e., vaginal laser application) that stimulate collagen production might improve SUI symptoms.
The aim of our study was to compare the efficacy of vaginal CO2 lasers to sham therapy in women with SUI immediately following therapy and at 3 months posttreatment.
Materials and Methods
A randomized controlled trial with the sham technique was conducted in the female pelvic medicine and reconstructive surgery unit, Department of Obstetrics and Gynaecology, Faculty of Medicine, Srinagarind Hospital, Khon Kaen University, Thailand, from January 2019 to April 2021. This study was approved by the Khon Kaen University Ethics Committee for Human Research (HE611135).
Women with SUI and mixed urinary incontinence, stress predominant, were recruited for this study. Patients with pelvic organ prolapse stage II or more, those with a history of recurrent UTI, previous anti-incontinence surgery, body mass index (BMI) > 30 kg/m2, use of hormonal treatments in postmenopausal women, current use of drug treatment for urinary incontinence, pain in the vagina with or without sexual intercourse, pregnancy, current active vaginal infections, abnormal uterine bleeding with unknown causes, and a history of vaginal laser treatment were excluded. This trial was performed and reported following the CONSORT statement and was registered with the Thai Clinical Trial Register (TCTR20190131004).
The participants who met the inclusion criteria were randomly allocated using computer generated randomization into two groups. All randomization sequences were kept in sequentially numbered opaque seal envelopes. The participants and assessor were blinded.
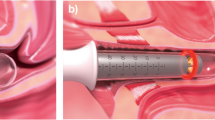
The intervention group was treated with transvaginal fractional microablative CO2 lasers (MonaLisa TouchTM®; Deka, Florence, Italy). Applicators of 360° and 90° were used. The rotational and withdrawal technique was performed after insertion of the 360° applicator using the entire length of the vagina. The CO2 energy was administered according to the product instructions. The 90° applicator was subsequently applied to the suburethral area of the anterior vaginal wall with a power setting of 40 W, 1000 µs of pulse duration, and 1000 µm spacing. The administration of CO2 was applied four times, 28–35 days apart on an outpatient basis. All participants were advised to avoid sexual intercourse for a week following treatment. Women in the sham group were treated in the same manner as the intervention group but with no energy administered. There was noise from the machine without power. The same urogynecologist performed both interventions. All participants in both groups were advised to perform pelvic floor muscle training regularly after the intervention and were provided handouts.
The validated Thai version of the International Consultation on Incontinence Questionnaire—Urinary Incontinence Short Form (ICIQ-UI SF) questionnaire [15] was used to evaluate symptoms. All women were studied using 4D trans-perineal pelvic floor ultrasonography before and immediately after four courses of CO2 energy administration and at 3 months after treatment.
The sample size was calculated using a 90% power and 0.05% level of significance to detect a difference in the ICIQ-UI SF score of 3 points, which was considered to be clinically significant. A 20% dropout rate was also considered [16].
Statistical analyses were performed using Stata 10 (Stata Corporation, College Station, Texas). Baseline characteristics are presented as descriptive information. Student’s t test was used to compare continuous variables. The chi-square or Fisher’s exact test was employed to compare categorical variables. Differences between the comparison groups were evaluated as the mean difference (MD) or relative risk (RR) with a 95% confidence interval (CI). Statistical analysis was conducted using mixed analysis of variance. A p value < 0.05 was considered to be statistically significant. All analyses were carried out based on the intention-to-treat analysis.
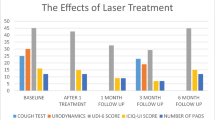
Results
A total of 64 participants were assessed for eligibility. Four participants did not meet the inclusion criteria, and one refused to participate in the study. Therefore, 59 participants were randomized into two groups; 29 women in the CO2 laser group and 30 in the sham group, as shown in the CONSORT flow diagram (Fig. 1). During the follow-up time, three participants withdrew from the study for personal reasons. Twenty-eight patients in the CO2 group and 28 patients in the sham group were studied using an intention-to-treat basis.
Patient characteristics are shown in Table 1. The percentages of SUI and MUI were not different between the two groups. The baseline scores of the ICIQ-UI SF were similar in both groups. There was no statistical significance in bladder neck descent or levator hiatal area between the two groups.
The urinary incontinence symptom scores improved significantly in both groups (p < 0.001 and p < 0.001, respectively). However, there were no statistically significant differences between the two groups immediately after four laser treatments (p = 0.9129) or 3 months after the last application of CO2 energy (p = 0.8281) (Table 2).
There were no changes in bladder neck descent immediately after intervention (p = 0.5414) or 3 months after completion of treatment (p = 0.4803) in either group, and the area of the levator hiatus at rest as well as the levator hiatal area on the maximal Valsava did not change significantly in the CO2 laser or the sham group immediately after treatment or 3 months after completion of treatment. However, the area of levator hiatus on maximal Valsalva was significantly reduced in the CO2 laser group immediately after treatment (p = 0.041), as shown in Table 2.
The majority of women treated with CO2 energy reported that minimal vaginal pain during the procedure resolved spontaneously after finishing the procedure. No one reported vaginal infection or dyspareunia after the procedures.
Discussion
Many prospective observational studies [17,18,19,20] have evaluated the effectiveness of CO2 lasers for treating SUI and many have found that SUI symptoms were improved significantly after CO2 application (in both subjective and objective outcomes). One study [21] included patients with both SUI and MUI symptoms and reported significant improvement in symptoms after three sessions of fractional microablative CO2 laser treatment. However, there is little data comparing laser therapy to placebo or sham therapy to establish its contribution to symptom improvement. Therefore, the current randomized sham controlled trial was conducted to evaluate the effectiveness of a CO2 laser for SUI treatment. This study found that there were significantly improved urinary incontinence symptoms from ICIQ-UI SF scores in both treatment and sham groups, but there were no significant differences in ICIQ-UI SF scores between the groups immediately or 3 months after treatment. This means that the reduction in symptom scores might be due to the recommended pelvic floor muscle exercises or placebo effect.
The data of another prospective randomized trial published in 2022 [22] revealed that both CO2 lasers and Er: YAG improved SUI symptoms significantly over the sham procedure. These results contradict the findings in the present study. That study and the present study had a similar number of participants, so it is difficult to reconcile the differences. However, the most significant difference between the two studies is that the present study participants were recommended to undergo pelvic floor muscle training. For the present study the authors felt that due to the ethical concerns of not providing any therapy for the sham group, the protocol should include a recommendation for pelvic floor muscle training and a handout on this therapy was provided to both groups. Participants in the present study did not undergo any specific training sessions for pelvic floor exercises. Therefore, the improvement in UI symptom scores in both groups might be due to the additional pelvic floor muscle training recommended in this setting or it might simply be a placebo effect.
In the context of pelvic floor ultrasonography, the thermal effect from the CO2 application did not show any significant changes to the bladder neck descent when compared to the sham technique. The area of the levator hiatus on maximal Valsalva was significantly reduced in the CO2 laser group immediately after treatment. It might be the effect of thermal energy that causes collagen tightening around the vaginal hiatus, but the effect did not last long. The differences were no longer detected at the 3-months follow-up exam.
There were few reported adverse events after CO2 application, with only minimal pain during the procedure that resolved spontaneously, which is similar to other studies [22]. Moreover, there was no report of serious adverse events from vaginal laser [23,24,25,26]. This suggests that CO2 vaginal application is safe with no serious adverse events in the short term. There are no data on long-term adverse events from laser use.
This study set out to explore a randomized placebo/sham controlled trial to investigate the efficacy of CO2 lasers for treating stress-predominant urinary incontinence. This study did not demonstrate the benefit of CO2 lasers over the sham technique in terms of SUI treatment. This study enrolled patients with both SUI and MUI, stress predominant, and the sample size, while appropriate, was small. Therefore, RCTs with larger sample sizes should be conducted.
Conclusions
Fractional CO2 laser treatment did not provide a benefit over the sham technique in alleviating SUI symptoms. The improvement in SUI symptoms might be due to pelvic floor muscle training that was recommended during the study period. There were no changes in bladder neck descent or levator hiatal area immediately after intervention or 3 months after completion of treatment in either group.
Data Availability
The data will be available on request.
References
Bhide AA, Khullar V, Swift S, Digesu GA. The use of laser in urogynaecology. Int Urogynecology J. 2019;30(5):683–92. https://doi.org/10.1007/s00192-018-3844-7.
Digesu GA, Tailor V, Preti M, Vieira-Baptista P, Tarcan T, Stockdale C, et al. The energy based devices for vaginal “rejuvenation”, urinary incontinence, vaginal cosmetic procedures, and other vulvo-vaginal disorders: an international multidisciplinary expert panel opinion. Neurourol Urodyn. 2019;38(3):1005–8. https://doi.org/10.1002/nau.23927.
Preti M, Vieira-Baptista P, Digesu GA, Bretschneider CE, Damaser M, Demirkesen O, et al. The clinical role of LASER for vulvar and vaginal treatments in gynecology and female urology: an ICS/ISSVD best practice consensus document. J Low Genit Tract Dis. 2019;23(2):151–60. https://doi.org/10.1097/LGT.0000000000000462.
Gambacciani M, Palacios S. Laser therapy for the restoration of vaginal function. Maturitas. 2017;99:10–5. https://doi.org/10.1016/j.maturitas.2017.01.012.
Kunzi-Rapp K, Dierickx CC, Cambier B, Drosner M. Minimally invasive skin rejuvenation with Erbium: YAG laser used in thermal mode. Lasers Surg Med. 2006;38(10):899–907. https://doi.org/10.1002/lsm.20380.
El-Domyati M, Abd-El-Raheem T, Medhat W, Abdel-Wahab H, Al AM. Multiple fractional erbium: yttrium-aluminum-garnet laser sessions for upper facial rejuvenation: clinical and histological implications and expectations. J Cosmet Dermatol. 2014;13(1):30–7. https://doi.org/10.1111/jocd.12079.
Tadir Y, Gaspar A, Lev-Sagie A, Alexiades M, Alinsod R, Bader A, et al. Light and energy based therapeutics for genitourinary syndrome of menopause: consensus and controversies. Lasers Surg Med. 2017;49(2):137–59. https://doi.org/10.1002/lsm.22637.
Lapii GA, Yakovleva AY, Neimark AI. Structural reorganization of the vaginal mucosa in stress urinary incontinence under conditions of Er:YAG laser treatment. Bull Exp Biol Med. 2017;162(4):510–4. https://doi.org/10.1007/s10517-017-3650-0.
Franić D, Fistonić I. Laser therapy in the treatment of female urinary incontinence and genitourinary syndrome of menopause: an update. BioMed Res Int. 2019;2019:1576359. https://doi.org/10.1155/2019/1576359.
Buckley BS, Lapitan MCM, Epidemiology Committee of the Fourth International Consultation on Incontinence, Paris, 2008. Prevalence of urinary incontinence in men, women, and children--current evidence: findings of the Fourth International Consultation on Incontinence. Urology. 2010;76(2):265–70. https://doi.org/10.1016/j.urology.2009.11.078.
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21(1):5–26. https://doi.org/10.1007/s00192-009-0976-9.
Carr LK, Robert M, Kultgen PL, Herschorn S, Birch C, Murphy M, et al. Autologous muscle derived cell therapy for stress urinary incontinence: a prospective, dose ranging study. J Urol. 2013;189(2):595–601. https://doi.org/10.1016/j.juro.2012.09.028.
Wu JM. Stress incontinence in women. N Engl J Med. 2021;384(25):2428–36. https://doi.org/10.1056/NEJMcp1914037.
Han L, Wang L, Wang Q, Li H, Zang H. Association between pelvic organ prolapse and stress urinary incontinence with collagen. Exp Ther Med. 2014;7(5):1337–41. https://doi.org/10.3892/etm.2014.1563.
Apichatwong K, Asdornwised U, Pinyopasakul W, Tantiwong A, Leerasiri P. Factors associated with sexual functions in women with urinary incontinence. Nurs Sci J. 2016;34(4):47–56.
González Isaza P, Jaguszewska K, Cardona JL, Lukaszuk M. Long-term effect of thermoablative fractional CO2 laser treatment as a novel approach to urinary incontinence management in women with genitourinary syndrome of menopause. Int Urogynecol J. 2018;29(2):211–5. https://doi.org/10.1007/s00192-017-3352-1.
Dabaja H, Lauterbach R, Matanes E, Gruenwald I, Lowenstein L. The safety and efficacy of CO2 laser in the treatment of stress urinary incontinence. Int Urogynecol J. 2020;31(8):1691–6. https://doi.org/10.1007/s00192-019-04204-4.
Alcalay M, Ben Ami M, Greenshpun A, Hagay Z, Schiff E. Fractional-pixel CO2 laser treatment in patients with urodynamic stress urinary incontinence: 1-year follow-up. Lasers Surg Med. 2021;53(7):960–7. https://doi.org/10.1002/lsm.23329.
Franić D, Fistonić I, Franić-Ivanišević M, Perdija Ž, Križmarić M. Pixel CO2 laser for the treatment of stress urinary incontinence: a prospective observational multicenter study. Lasers Surg Med. 2021;53(4):514–20. https://doi.org/10.1002/lsm.23319.
Nalewczynska AA, Barwijuk M, Kolczewski P, Dmoch-Gajzlerska E. Pixel-CO2 laser for the treatment of stress urinary incontinence. Lasers Med Sci. 2022;37(2):1061–7. https://doi.org/10.1007/s10103-021-03353-7.
Palacios S, Ramirez M. Efficacy of the use of fractional CO2RE intima laser treatment in stress and mixed urinary incontinence. Eur J Obstet Gynecol Reprod Biol. 2020;244:95–100. https://doi.org/10.1016/j.ejogrb.2019.10.048.
Ranjbar A, Mehrnoush V, Darsareh F, Kotb A, Zakaria A, Shekari M, et al. Vaginal laser therapy for stress urinary incontinence: a systematic review of prospective randomized clinical trials. J Menopausal Med. 2022;28(3):103–11. https://doi.org/10.6118/jmm.22017.
Aguiar LB, Politano CA, Costa-Paiva L, Juliato CRT. Efficacy of fractional CO2 laser, promestriene, and vaginal lubricant in the treatment of urinary symptoms in postmenopausal women: a randomized clinical trial. Lasers Surg Med. 2020;52(8):713–20. https://doi.org/10.1002/lsm.23220.
Seki AS, Bianchi-Ferraro AMHM, Fonseca ESM, Sartori MGF, Girão MJBC, Jarmy-Di Bella ZIK. CO2 Laser and radiofrequency compared to a sham control group in treatment of stress urinary incontinence (LARF study arm 3). A randomized controlled trial. Int Urogynecol J. 2022;33(12):3535–42. https://doi.org/10.1007/s00192-022-05091-y.
Blaganje M, Šćepanović D, Žgur L, Verdenik I, Pajk F, Lukanović A. Non-ablative Er:YAG laser therapy effect on stress urinary incontinence related to quality of life and sexual function: a randomized controlled trial. Eur J Obstet Gynecol Reprod Biol. 2018;224:153–8. https://doi.org/10.1016/j.ejogrb.2018.03.038.
Lauterbach R, Aharoni S, Justman N, Farago N, Gruenwald I, Lowenstein L. The efficacy and safety of a single maintenance laser treatment for stress urinary incontinence: a double-blinded randomized controlled trial. Int Urogynecol J. 2022;33(12):3499–504. https://doi.org/10.1007/s00192-022-05103-x.
Funding
Faculty of Medicine, Khon Kaen university, Khon Kaen, Thailand.
Author information
Authors and Affiliations
Contributions
Teerayut Temtanakitpaisan: Protocol development, Data collection or management, Data analysis and Manuscript writing.
Chompilas Chongsomchai: Protocol development and Manuscript editing.
Pranom Buppasiri: Protocol development and Manuscript editing.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Temtanakitpaisan, T., Chongsomchai, C. & Buppasiri, P. Fractional CO2 laser treatment for women with stress predominant urinary incontinence: a randomized controlled trial. Int Urogynecol J 34, 2827–2832 (2023). https://doi.org/10.1007/s00192-023-05655-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-023-05655-6