Abstract
Introduction and hypothesis
The use of validated Quality of Life (QoL) questionnaires is useful in the standardization and interpretation process of pelvic floor patient symptoms, due to their functional nature and high prevalence. The Pelvic Floor Distress Inventory QoL questionnaire (PFDI-20) serves both as a symptom inventory and a measure of the degree of bother and distress caused by pelvic floor symptoms. It includes items related to pelvic organ prolapse and lower gastrointestinal and bladder dysfunction.
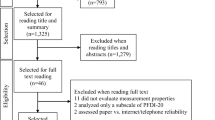
Methods
After consensus translation and a comprehension test, the Italian version of the questionnaire was submitted to patients reporting bowel, bladder, or pelvic disorders (cases) and to asymptomatic women (controls). Cases received the questionnaire once again 2 weeks later by email.
Results
A total of 254 patients answered the questionnaire. Construct validity was demonstrated by discriminating between cases and controls. Convergent validity was demonstrated for each domain (F < 0.001). In-ernal consistency reliability showed a satisfactory range (0.816–0.860).
Conclusions
The PFDI-20 allows a comprehensive assessment of the effect of pelvic floor disorders on the quality of life of women. Moreover, the PFDI-20 represents a very solid QoL tool, since it has been extensively used in literature, and its use is highly recommended by the International Consultation on Incontinence. The present study demonstrated good features for the Italian version of the PFDI-20 questionnaire.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pelvic floor disorders (PFDs) represent a series of conditions — including prolapse, bowel, and bladder dysfunction — related to pelvic floor weakening and/or tears, usually related to obstetric trauma [1, 2]. Pelvic floor disorders share the same factors and may frequently coexist or recur [3, 4]. These may involve age, menopausal status, and obesity [1, 5]. Also, changes in the composition of connective tissue and metalloproteinases can be observed in patients with pelvic floor disorders [6]. Moreover, pelvic floor disorders can occur and/ or persist as a consequence of pelvic floor surgery [7, 8]. Symptoms can be multiple, including urinary incontinence, fecal incontinence, pelvic organ prolapse symptoms, voiding dysfunction, and defecatory dysfunction [9]. These conditions may negatively affect social, occupational, domestic, and psychophysical well-being [10]. Conservative management includes lifestyle modification, pelvic floor muscle training, biofeedback/electrical stimulation, vaginal laser, magnetic stimulation, pessaries, and pharmacological treatments [11,12,13]. Surgical treatment is indicated when conservative management fails and may involve native tissue repair, mesh surgery, and injection of various agents including stem cells [14,15,16,17,18]. Due to the functional nature of PFDs, the use of validated outcome measures, involving the impact on quality of life, is of the utmost importance in evaluating the efficacy of the treatments. Quality of life (QoL) assessment is a milestone of clinical practice in gynecology. In particular, the use of validated QoL questionnaires is of the utmost importance for the evaluation of pelvic floor disorders, due to their functional nature and high prevalence [19]. Validated QoL questionnaires allow the assessment of pelvic floor symptoms' frequency and severity, their impact on quality of life, and trends over time. Moreover, self-completed questionnaires are preferable to clinical interviews since they minimize bias related to caregiver interpretation. Lastly, a structured questionnaire that covers most aspects of pelvic floor disorders would be a useful tool to screen the population. Although several sexual life QoL questionnaires are available for the general population, there are very few questionnaires specifically designed for the simultaneous evaluation of bladder, prolapse, and bowel dysfunction domains [20]. One of them is represented by the PFDI-20, a 5-point Likert scale self-reported questionnaire with 20 items covering three domains of pelvic floor function [21]. In brief, the PFDI-20 serves the role of both a symptom inventory and a measure of the degree of bother and distress caused by the broad array of pelvic floor symptoms. It includes items related to pelvic organ prolapse, lower gastrointestinal, and bladder dysfunction. Unfortunately, this questionnaire has not been validated in the Italian language yet.
Consequently, the aim of this study was to translate and validate the Italian language version of the Pelvic Floor Distress Inventory (PFDI-20) questionnaire evaluating the validity, internal consistency, and test–retest reliability. That ensures that the questionnaire will make sense to patients, that it is able to differentiate between symptomatic patients and controls, that it is able to measure what it was intended to measure, and that the answer to each question will not change substantially if the questionnaire is administered twice over a short period.
Materials and methods
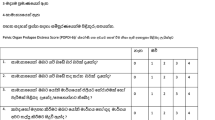
This was a multicenter study conducted in Italy. Ethical committee approval was obtained before starting the study (name of the protocol “ITA PFDI-20”). Investigators were experienced in the translation and validation of QoL tools [22, 23]. The questionnaire was based on the Pelvic Floor Distress Inventory (PFDI-20) questionnaire. This represents a validated questionnaire for bladder, bowel, and pelvic symptoms severity assessment in patients with pelvic floor disorders, which was developed in 2005 as the short form of the Pelvic Floor Distress Inventory (PFDI). The PFDI consists of 46 questions separated into three scales; the UDI, Pelvic Organ Prolapse Distress Inventory (POPDI), and the ColoRectal Anal Distress Inventory (CRADI) [21]. The PFDI-20 was then developed, since the relative length of the original version made the former somehow inefficient or impractical for most clinical and/or research situations. For the UDI scale, six items already existing as a separate tool (UDI-6) were incorporated in the PFDI short form. For the POPDI scale, six items were identified for the short form development due to the correlation between the combined score of these six questions (POPDI-6) and the total score deriving from the POPDI long form. For the CRADI scale, eight items (CRADI-8) that significantly correlated with the long-form version of the scale were identified [21]. To obtain the PFDI-20 score, the mean value of all of the answered items within the corresponding scale (possible value 0 to 4) should be obtained and then multiplied by 25 to obtain the scale score (range 0 to 100). Missing items are dealt with by using the mean from answered items only. Consequently, each of the three scales of the PFDI-20 is scored from 0 (least distress) to 100 (greatest distress) [21]. The sum of the scores of these three scales serves as the overall summary score of the PFDI-20 and ranges from 0 to 300.
Translation
The validation process of a linguistic translation must maintain conceptual and technical equivalence between the source and the target language [24]. The questionnaire was translated into Italian by the following procedural steps [25]. A preliminary translation from English into Italian was performed in parallel by two native Italian-speaking translators, with English as their first foreign language. Then, a consensus meeting among translators and the research group was held to compare the two Italian versions, which yielded the first consensus Italian version of the questionnaire. After that, a native English-speaking translator with Italian as his first foreign language back-translated the Italian consensus version. A second consensus meeting was held between the English mother-tongue translator and clinical investigators, during which the back-translated and the original questionnaires were compared and differences discussed. The process led to a revised version of the first consensus questionnaire. The comprehension of the obtained Italian consensus version was therefore tested in a real-life population to assess questionnaire comprehension. The questionnaire was submitted to women during a gynecological medical interview, and they were asked to evaluate their perceived degree of difficulty in understanding each question item. After that, the final Italian version of the questionnaire was obtained.
Study participants
Recruitment was obtained by the pelvic floor unit outpatients in the recruitment centers. Women referred for genital prolapse or incontinence, aged 18 years and over were included. Exclusion criteria included: insufficient Italian language proficiency and psychiatric or neurological disorders. Study participants filled out the questionnaire during clinical interviews. The questionnaire was submitted to women reporting bowel, bladder, or pelvic disorders (cases) and to asymptomatic patients (controls). For the test–retest evaluation, cases received the questionnaire 2 weeks later by email. Questionnaire distribution and all interviews were undertaken by the authors.
Questionnaire validation
Construct validity was tested to guarantee that the questionnaire is able to discriminate between women with pelvic floor symptoms and controls [26]. In order to test validity, the questionnaire was administered to women with and without pelvic floor disorders (respectively defined as ‘cases' and ‘controls'). Cases and controls were defined, as done previously, with respect to bowel, bladder, or prolapse symptoms using the question: “How much do your symptoms bother you?” and the following choice of answers: “Not applicable – I do not have symptoms”, “not at all”, “a little”, “quite a lot” and “very much” [22]. Controls were identified as women answering “Not applicable — I do not have symptoms” or “not at all”; otherwise, patients were defined as cases. Total scores for women with and without significant symptoms were compared and tested for statistical differences in order to assess validity. Given the heterogeneity of variances, the Wilcoxon test (non-parametric) was used to assess differences between cases and controls. Convergent validity for each domain was tested using specific items (#17, #18, and #19) of the Italian Version of the Prolapse Quality of Life Questionnaire (PQOL) [27].
The internal consistency — the strength of association among items — was tested using Cronbachʼs Alpha [28, 29]. Cases were given the questionnaire at baseline and 2 weeks later to evaluate the test–retest reliability. The test–retest reliability analysis was aimed to determine the questionnaire's reproducibility over time [26]. The degree of agreement of test–retest results of different individuals was tested with the intraclass correlation coefficient (ICC) [30, 31].
Statistical analysis
The statistical analysis was performed with JMP 7.0 (SAS, Cary, NC, USA). Where ratings were missing, items were excluded from the analysis pool. Patients who did not complete the questionnaire both at baseline and at the test–retest visit were excluded from the analyses. Continuous data are presented as mean ± standard deviation, and non-continuous data as absolute (relative) frequency. Wilcoxon non-parametric test, Cronbach’s Alpha, and the intraclass correlation coefficient were evaluated to assess the characteristics of the tool. A P < 0.05 was considered significant.
Results
The comprehension test was used to evaluate the ease of use of the questionnaire in a real population. Ten patients were given a preliminary interview after completing the questionnaire. All women correctly understood questions and pre-coded answers; no item was therefore changed. Consequently, the final Italian version of the questionnaire was obtained. In total, 254 women answered the final version of the questionnaire. The population characteristics are shown in Table 1. Most of the patients (80.3%) were in menopausal status. There was no dropout, since all of them answered at least part of the questionnaire. The rate of missing items was 0.4%. Table 2 summarizes the prevalence of considered pelvic floor disorders in the population of the study. The prevalence of prolapse, bowel, and bladder bothersome symptoms was respectively 63.4%, 49.2%, and 84.3%. Construct validity was demonstrated, as the questionnaire discriminated between patients with and without symptoms. Convergent validity was tested with PQOL-specific items, and was demonstrated for each domain (F < 0.001; Table 3). Internal consistency reliability evaluated with Cronbach's Alpha showed a satisfactory range (0.816–0.860; Table 4). Test–retest reliability evaluation is reported in Table 5. Intraclass correlation coefficients ranged between 0.792 and 0.933, indicating a very satisfactory overall agreement for each item. Specific ICC for each item is reported in Table 6.
Discussion
Pelvic floor disorders involve a wide variety of interrelated conditions, including urinary incontinence, fecal incontinence, pelvic organ prolapse symptoms, voiding dysfunction, and defecatory dysfunction, that can negatively impact the quality of life. Therefore, measuring quality of life is essential when evaluating symptoms at baseline and efficacy of treatments on the lives of women. According to a very recent systematic census of Italian-validated questionnaires on pelvic floor disorders, several questionnaires are available for evaluating different areas of pelvic floor disorders [20]. However, none of them completely evaluate pelvic floor disorders in three domains — namely prolapse, bowel, and bladder — like the PFDI-20. In the present study, we translated and tested the validity of the Italian version of this questionnaire. Translation and linguistic validation of a QOL tool are of the utmost importance, and should be implemented before the questionnaire is used in clinical practice [32]. A questionnaire that is valid and reliable for a particular language may not be valid and reliable when used in a different population and scenario [33]. In our study, no issues arose from the translation process, which was carried out following the method proposed by Guillemin, consisting of forward and backward translations with researchers–translators consensus meetings [25]. The obtained version of the questionnaire was tested for comprehension — according to the widely accepted process for linguistic validation — and no difficulties in understanding each question item and related precoded answers in a real-life population were found. Construct validity was confirmed, as the questionnaire was able to discriminate between patients with and without symptoms for all the domains of the questionnaire. Convergent validity was tested and demonstrated with specific items from the Italian version of the Prolapse Quality of Life Questionnaire (PQOL). A strong association of individual items in each domain was shown with the internal consistency reliability analysis using Cronbach's Alpha. Lastly, the longitudinal stability of the questionnaire was evaluated and confirmed with test–retest reliability through the intraclass correlation coefficients analysis.
The PFDI-20 carries some theoretical advantages compared to other QoL tools. The main one is that it allows a comprehensive assessment of the effect of pelvic floor disorders on the quality of life of women, rather than assessing just one aspect of pelvic floor function such as constipation or urinary incontinence. This is particularly important, since disorders of the pelvic floor share the same factors and may frequently coexist [34, 35]. Moreover, the treatment of one of these disorders can improve, worsen, or even predispose to another [7, 36]. For example, prolapse repair has been shown to improve overactive bladder symptoms, but worsening has been demonstrated when a concomitant sling procedure is performed at the time of surgery [35]. Similarly, the anterior vaginal compartment prolapse repair may predispose to postoperative stress urinary incontinence in case of the presence of urodynamic risk factors [7]. Due to these complex relationships, tools that allow a comprehensive approach to the baseline evaluation and assessment of treatment efficacy should be preferred. Moreover, the PFDI-20 total score has been recently stratified into three classes of distress severity, which can be used to facilitate the understanding of the patient’s health status [37]. Using a partial credit model, the authors proposed the following classification of distress: absence of symptoms (score zero), symptoms with mild distress (1 to 15 points), symptoms with moderate distress (16 to 34 points), and symptoms with severe distress (35 to 40 points). Lastly, PFDI-20 represents a very solid QoL tool, since it has been extensively used in literature, and its use is highly recommended by the International Consultation on Incontinence. A systematic review of 25 studies evaluating the measurement properties confirmed the high quality of evidence for criterion validity, construct validity-hypothesis testing and responsiveness, moderate quality for test–retest reliability, and measurement errors for PFDI-20 [38].
Strengths of the study include standardized procedural steps for translation/validation, its originality — being that the questionnaire in question is the first one able to evaluate three domains of pelvic floor disorders in the general population in the Italian language — and the evaluation of test–retest reliability.
Conclusions
The present study demonstrated good features for the Italian version of the PFDI-20 questionnaire. A validated Italian questionnaire is now available for clinical use to investigate the incidence, severity, and impact on the quality of life of prolapse, bowel, and bladder symptoms in women with pelvic floor disorders.
Data Availability
The datasets generated and/or analyzed during the current research are not publicly available as individual privacy could be compromised, but are available from the corresponding author on reasonable request.
References
Manodoro S, Frigerio M, Cola A, Spelzini F, Milani R. Risk factors for recurrence after hysterectomy plus native-tissue repair as primary treatment for genital prolapse. Int Urogynecol J. 2018;29(1):145–51. https://doi.org/10.1007/s00192-017-3448-7.
Frigerio M, Mastrolia SA, Spelzini F, Manodoro S, Yohay D, Weintraub AY. Long-term effects of episiotomy on urinary incontinence and pelvic organ prolapse: a systematic review. Arch Gynecol Obstet. 2019;299(2):317–25. https://doi.org/10.1007/s00404-018-5009-9.
Milani R, Frigerio M, Vellucci FL, Palmieri S, Spelzini F, Manodoro S. Transvaginal native-tissue repair of vaginal vault prolapse. Minerva Ginecol. 2018;70(4):371–7. https://doi.org/10.23736/S0026-4784.18.04191-6.
Milani R, Frigerio M, Spelzini F, Manodoro S. Transvaginal uterosacral ligament suspension for posthysterectomy vaginal vault prolapse repair. Int Urogynecol J. 2017;28(9):1421–3. https://doi.org/10.1007/s00192-017-3277-8.
Frigerio M, Regini C, Manodoro S, Spelzini F, Milani R. Mini-sling efficacy in obese versus non-obese patients for treatment of stress urinary incontinence. Minerva Ginecol. 2017;69(6):533–7. https://doi.org/10.23736/S0026-4784.17.04081-3.
Manodoro S, Spelzini F, Cesana MC, Frigerio M, Maggioni D, Ceresa C, Penati C, Sicuri M, Fruscio R, Nicolini G, Milani R. Histologic and metabolic assessment in a cohort of patients with genital prolapse: preoperative stage and recurrence investigations. Minerva Ginecol. 2017;69(3):233–8. https://doi.org/10.23736/S0026-4784.16.03977-0.
Frigerio M, Manodoro S, Palmieri S, Spelzini F, Milani R. Risk factors for stress urinary incontinence after native-tissue vaginal repair of pelvic organ prolapse. Int J Gynaecol Obstet. 2018;141(3):349–53. https://doi.org/10.1002/ijgo.12443.
Palmieri S, Frigerio M, Spelzini F, Manodoro S, Milani R. Risk factors for stress urinary incontinence recurrence after single-incision sling. Neurourol Urodyn. 2018;37(5):1711–6. https://doi.org/10.1002/nau.23487.
Milani R, Manodoro S, Cola A, Bellante N, Palmieri S, Frigerio M. Transvaginal uterosacral ligament hysteropexy versus hysterectomy plus uterosacral ligament suspension: a matched cohort study. Int Urogynecol J. 2020;31(9):1867–72. https://doi.org/10.1007/s00192-019-04206-2.
Frigerio M, Barba M, Cola A, et al. Quality of life, psychological wellbeing, and sexuality in women with urinary incontinence-where are we now: a narrative review. Medicina. 2022;58(4):525. https://doi.org/10.3390/medicina58040525. (Published 2022 Apr 9).
Palmieri S, Cola A, Milani R, Manodoro S, Frigerio M. Quality of life in women with advanced pelvic organ prolapse treated with Gellhorn pessary. Minerva Ginecol. 2018;70(4):490–2. https://doi.org/10.23736/S0026-4784.18.04199-0.
Ruffolo AF, Braga A, Torella M, Frigerio M, Cimmino C, De Rosa A, Sorice P, Castronovo F, Salvatore S, Serati M. Vaginal laser therapy for female stress urinary incontinence: new solutions for a well-known issue-a concise review. Medicina. 2022;58(4):512. https://doi.org/10.3390/medicina58040512.
Barba M, Lazar T, Cola A, Marino G, Manodoro S, Frigerio M. Learning curve of botulinum toxin bladder injection for the treatment of refractory overactive bladder. Int J Womens Health. 2022;14:1–7. https://doi.org/10.2147/IJWH.S345454.
Manodoro S, Frigerio M, Barba M, Bosio S, de Vitis LA, Marconi AM. Stem cells in clinical trials for pelvic floor disorders: a systematic literature review. Reprod Sci. 2022;29(6):1710–20. https://doi.org/10.1007/s43032-021-00745-6.
Serati M, Braga A, Salvatore S, et al. Up-to-date procedures in female stress urinary incontinence surgery: a concise review on bulking agents procedures. Medicina. 2022;58(6):775. https://doi.org/10.3390/medicina58060775. (Published 2022 Jun 8).
Braga A, Castronovo F, Ottone A, et al. Medium term outcomes of TVT-abbrevo for the treatment of stress urinary incontinence: efficacy and safety at 5-Year follow-up. Medicina. 2022;58(10):1412. https://doi.org/10.3390/medicina58101412. (Published 2022 Oct 8).
Spelzini F, Frigerio M, Regini C, Palmieri S, Manodoro S, Milani R. Learning curve for the single-incision suburethral sling procedure for female stress urinary incontinence. Int J Gynaecol Obstet. 2017;139(3):363–7. https://doi.org/10.1002/ijgo.12317.
Milani R, Frigerio M, Cola A, Beretta C, Spelzini F, Manodoro S. Outcomes of transvaginal high uterosacral ligaments suspension: over 500-patient single-center study. Female Pelvic Med Reconstr Surg. 2018;24(1):39–42. https://doi.org/10.1097/SPV.0000000000000403.
Palmieri S, De Bastiani SS, Degliuomini R, Ruffolo AF, Casiraghi A, Vergani P, Gallo P, Magoga G, Cicuti M, Parma M, Frigerio M, Urogynecology–Pelvic Floor Working Group (GLUP). Prevalence and severity of pelvic floor disorders in pregnant and postpartum women. Int J Gynaecol Obstet. 2022;158(2):346–51. https://doi.org/10.1002/ijgo.14019.
Braga A, Barba M, Serati M, Soligo M, Li Marzi V, FinazziAgrò E, Musco S, Caccia G, Castronovo F, Manodoro S, Frigerio M, Italian Society of Urodynamics. Update on Italian-validated questionnaires for pelvic floor disorders. Minerva Obstet Gynecol. 2021. https://doi.org/10.23736/S2724-606X.21.04901-0.
Barber MD, Walters MD, Bump RC. Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am J Obstet Gynecol. 2005;193(1):103–13. https://doi.org/10.1016/j.ajog.2004.12.025.
Palmieri S, Cola A, Ceccherelli A, Manodoro S, Frigerio M, Vergani P. Italian validation of the German Pelvic Floor Questionnaire for pregnant and postpartum women. Eur J Obstet Gynecol Reprod Biol. 2020;248:133–6. https://doi.org/10.1016/j.ejogrb.2020.03.032.
Volonte’ S, Barba M, Cola A, Marino G, Frigerio M. Italian validation of the short form of the pelvic organ prolapse/urinary incontinence sexual questionnaire (PISQ-12). Int Urogynecol J. 2022;33(11):3171–5. https://doi.org/10.1007/s00192-022-05235-0.
Hutchinson A, Bentzen N, Konig-Zahn C (1997) Cross cultural health outcome assessment: a user’s guide I. European Research Group on Health Outcomes, Groningen, Netherlands
Guillemin F, Bombardier C, Beaton D. Cross-cultural adaptation of health-related quality of life measures: literature review and proposed guidelines. J Clin Epidemiol. 1993;46:1417–32.
Revicki DA, Osoba D, Fairclough D, et al. Recommendations on health-related quality of life research to support labeling and promotional claims in the United States. Qual Life Res. 2000;9:887–900.
Digesu GA, Santamato S, Khullar V, et al. Validation of an Italian version of the prolapse quality of life questionnaire. Eur J Obstet Gynecol Reprod Biol. 2003;106(2):184–92. https://doi.org/10.1016/s0301-2115(02)00229-4.
H. Levene. Robust tests for equality of variances. In: I. Olkin, et al., Eds., Contributions to probability and statistics: essays in honor of Harold Hotelling. Palo Alto: Stanford University Press; 1960. p. 278–92
Bonferroni CE. Teoria statistica delle classi e calcolo delle probabilità. Pubblicazioni del R Istituto Superiore di Scienze Economiche e Commerciali di Firenze. 1936;8:3–62.
Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–8.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
Pasquali L. Psicometria. Rev Esc Enferm USP. 2009;43:992–9.
El-Azab AS, Abd-Elsayed AA, Imam HM. Patient reported and anatomical outcomes after surgery for pelvic organ prolapse. Neurourol Urodyn. 2009;28:219–24. https://doi.org/10.1002/nau.20626.
D’Alessandro G, Palmieri S, Cola A, Barba M, Manodoro S, Frigerio M. Detrusor underactivity prevalence and risk factors according to different definitions in women attending urogynecology clinic. Int Urogynecol J. 2022;33(4):835–40. https://doi.org/10.1007/s00192-021-04796-w.
Frigerio M, Manodoro S, Cola A, Palmieri S, Spelzini F, Milani R. Risk factors for persistent, de novo and overall overactive bladder syndrome after surgical prolapse repair. Eur J Obstet Gynecol Reprod Biol. 2019;233:141–5. https://doi.org/10.1016/j.ejogrb.2018.12.024.
Palmieri S, Manodoro S, Cola A, Spelzini F, Milani R, Frigerio M. Pelvic organ prolapse and voiding function before and after surgery. Minerva Ginecol. 2019;71(3):253–6. https://doi.org/10.23736/S0026-4784.19.04313-2.
de Arruda GT, de Andrade DF, Virtuoso JF. Internal structure and classification of pelvic floor dysfunction distress by PFDI-20 total score. J Patient Rep Outcomes. 2022;6(1):51. https://doi.org/10.1186/s41687-022-00459-6. (Published 2022 May 16).
de Arruda GT, Dos Santos HT, Virtuoso JF. Pelvic Floor Distress Inventory (PFDI)-systematic review of measurement properties. Int Urogynecol J. 2021;32(10):2657–69. https://doi.org/10.1007/s00192-021-04748-4.
Author information
Authors and Affiliations
Contributions
Marta Barba: data collection, manuscript writing.
Alice Cola: data collection, manuscript writing.
Tomaso Melocchi: data collection.
Andrea Braga: data collection.
Fabiana Castronovo: data collection.
Stefano Manodoro: data collection.
Marika Pennacchio: data collection.
Gaetano Maria Munno: data collection.
Alessandro Ferdinando Ruffolo: data collection.
Rebecca Susanna Degliuomini: data collection.
Stefano Salvatore: data collection.
Marco Torella: data collection.
Matteo Frigerio: project development, data collection, manuscript writing.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Barba, M., Cola, A., Melocchi, T. et al. Italian validation of the Pelvic Floor Distress Inventory (PFDI-20) questionnaire. Int Urogynecol J 34, 2459–2465 (2023). https://doi.org/10.1007/s00192-023-05572-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-023-05572-8