Abstract
Introduction and hypothesis
Pelvic organ prolapse (POP) is often diagnosed during an in-office examination, which looks for motion of the vaginal wall while performing a strain maneuver. It is believed that the pelvic organs in adequately supported women are relatively stationary. This study was aimed at investigating the physiological displacements of pelvic organs using MR defecography.
Methods
This prospective cohort study included 19 volunteers. Midsagittal slices representing rest and the maximum movement of the posterior vaginal fornix during three maneuvers were identified. Normalized axes for analysis were defined as the x’ (line connecting the inferior–posterior-most point on the pubic symphysis to the anterior edge of the sacrococcygeal joint) and the y’ (line orthogonal to the x axis that passed through the sacral promontory). The positions of the posterior vaginal fornix, mid-vagina, bladder neck, anorectal junction, and hymen were recorded. These subjects were then analyzed using the current radiological grading system of POP to determine any overlap between asymptomatic subjects and diagnostic ranges of POP.
Results
Evacuation caused the most motion in the landmarks. The majority of the motion of the landmarks was along the y axis. The posterior vaginal fornix experienced significant descent (125% of the initial distance) without much anterior–posterior translation (7% of the initial distance) during defecation. All landmarks experienced similar trends.
Conclusions
We have shown that there is significant rotational motion of the pelvic organs around the pubic bone in adequately supported women. This motion when described using radiological grading is likely to be considered mild or moderate prolapse, which may contribute to overdiagnosis of POP.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pelvic organ prolapse (POP) is a common clinical condition affecting millions of women worldwide [1, 2]. POP is associated with excessive motion of pelvic organs (toward the vaginal hymen and through the vaginal opening) with increases in intra-abdominal pressure. As such, symptomatic vaginal support has been defined as motion of the vaginal wall relative to the vaginal hymen while preforming a strain maneuver [3,4,5]. This belief has led to the overdiagnosis of POP when using some imaging modalities because pelvic organs actually have a larger range of motion during normal physiological events than was previously reported [6]. This motion may be missed during office vaginal examinations for two reasons:
-
1.
Complete levator relaxation typically happens during evacuation
-
2.
The hymen moves along with other pelvic organs/vaginal walls, which obscures the extent of mobility relative to static landmarks such as bones [6]
Our team previously used MRI of 12 women with adequate support of the vaginal apex (as defined by POP-Q) to describe the motion of the vaginal apex relative to three clinically relevant landmarks (hymen, sacral promontory, and S4–S5 intervertebral disc) during strain and defecation [6]. This study showed that the vaginal apex is a highly mobile structure with significantly more movement being demonstrated during defecation compared with strain. These data were significant because they contradict the general perception that the vaginal apex is relatively fixed within the pelvis of adequately supported women. In addition, these data showed that a strain maneuver underestimates the significant amount of motion that this structure can undergo during everyday physiological activities, such as defecation. This prospective cohort study was aimed at building on our previous work by:
-
1.
Investigating the physiological displacements of pelvic organs
-
2.
Establishing ranges of values for typical, asymptomatic motion of the pelvic organs in nulligravid women using MR defecography
Assuming that there is a continuous transition from an asymptomatic to a symptomatic state that is reflected by the mobility of the pelvic organs, defining ranges of asymptomatic pelvic motion will form an important baseline for early detection or prediction of POP. Additionally, comparing our findings of asymptomatic pelvic organ motion with the current radiological grading system for POP could determine to what extent the current grading methods over- or under-diagnose POP.
Materials and methods
We performed a prospective observational study including asymptomatic, nulliparous volunteers at our institution during September to December 2020 with International Review Board approval (EH20-133). Subjects were recruited from within the NorthShore Health System and were all health care workers. All subjects underwent a comprehensive interview by completing the Pelvic Floor Disability Index (PFDI-20) questionnaire, a pelvic examination including the Pelvic Organ Prolapse Quantification (POP-Q) examination, and dynamic MR defecography. Women who had a score of zero on the PFDI-20 questionnaire and had a POP-Q stage of zero on examination were included in this study.
MR defecography technique
All subjects underwent MR imaging in the supine position using a closed-configuration 1.5 T magnet and a Synergy body phased-array coil. As with routine dynamic pelvic floor MRI examinations performed at our institution, intravenous contrast medium was not used. No bowel preparation or intraluminal contrast material was administered. Subjects were instructed to empty their bladder 3 h before the examination to result in a moderately full urinary bladder during MRI. Static multiplanar images of the pelvis were acquired for anatomical evaluation using a 4-mm slice thickness with a 0-mm gap, for sagittal and axial T2-weighted sequences (echo time, 105 ms: repetition time, 3,000 ms). The rectum was then filled with 60 ml of ultrasound gel (1% Gd-DTPA-GEL-Mixture). Images were collected (1.5 Tesla MRI, Magnetom Symphony; Siemens, Erlangen, Germany) with subjects in the supine position, with hips and knees bent at 45°. The pelvic floor was visualized in three planes (axial, coronal, sagittal, T1 and T2) to find the appropriate sagittal plane in which all relevant pelvic floor organs could be acquired during defecation. The sequence lasted 36 s at a frequency of one shot per 1.1 s (True Fast Imaging with Steady State Precession; TR: 1.8 ms, TE: 1.01 ms). Slice thickness was 6 mm (field of view: 300 mm x 270 mm, image matrix: 256 x 256). During imaging, subjects were instructed via headphones to first relax and then to perform a squeeze maneuver as if they were trying to close the vaginal opening or to stop their urine stream. Next, subjects were instructed to perform a strain maneuver. They were asked to bear down and relax the pelvic floor without emptying their rectum. Finally, they were asked to evacuate with the goal of emptying their rectum as completely as possible. The sequences were acquired digitally and analyzed.
MR defecography image analysis
All measurements, in both analyses, were conducted twice by the same researcher and the average of the two measurements was used in calculations.
Measurements relative to bony landmarks
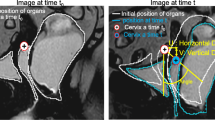
As a preprocessing step, all image series were stabilized in Blender (v. 2.8.0) to remove the effects of subject movement using the sacral promontory and the inferior–posterior-most point of the pubic symphysis as reference points. After stabilization, measurements were conducted using HOROS (v. 3.3.6). Midsagittal slices at rest (rest MRI) and showing the most movement of the posterior vaginal fornix (PVF) during evacuation (max evacuation), strain (max strain), and squeeze (max squeeze) were identified. In each instance, the coordinate system axes were defined using bony landmarks. The x axis was defined as the line connecting the inferior–posterior-most point on the pubic symphysis to the anterior edge of the sacrococcygeal joint, and the y axis was defined as the line orthogonal to the x axis that passed through the sacral promontory. These points (pubic bone, sacrococcygeal joint, and sacral promontory) were chosen as landmarks for defining these axes because they are easily identifiable and do not translate or deform in response to increases in intra-abdominal pressure. Then, an x’ axis and the y’ axis were determined by scaling each individual subject’s x and y axes based on the distance between the inferior–posterior point on the pubic symphysis, the anterior edge of the sacrococcygeal joint, and the perpendicular distance between the x axis and the sacral promontory. This was done to reduce variation in the description of organ position related to subject size. Finally, the y axis was translated to the pubic bone along the x axis, making the pubic bone the origin of this coordinate system (Fig. 1). The positions of the PVF (level 1 support), mid-vagina (level 2 support), bladder neck (level 2 support), the levator plate at the level of the anorectal junction (which will be referred to as the anorectal junction henceforth), and the hymen (level 3 support) were found and described with respect to the x’ and y’ axes (Fig. 1). Lines connecting the posterior vaginal fornix to the S4–S5 intravertebral disk–an approximation of the attachment of the uterosacral and sacrospinous ligament–and the sacral promontory–a common attachment point for sacral colpopexy–were also collected (Fig. 1). Each positional measure was broken into its x’ and y’ components. The average and standard deviation for each normalized measure was calculated for rest, evacuation, strain, and squeeze.
Measurement axes and landmarks of interest. The y axis has been shifted to the pubic bone, making point PB = (0, 0) for all measures. The x components are normalized to the length of the x axis, and the y’ components are normalized to the length of the orthogonal line from the sacral promontory to the x axis. Thus, the value of x’ and y’ at the sacrococcygeal joint and sacral promontory are both 1. a Measurements at rest with selected projections shown. b) Measurements at maximum evacuation with selected projections shown. Anatomy of interest is highlighted in the following colors: gray pubic bone, yellow urethra, cyan vagina, red rectum, purple sacrum, pink coccyx. BN bladder neck, HY hymen, MV mid-vagina, PVF posterior vaginal fornix (vaginal apex), AR anorectal, SP sacral promontory, SB S4–S5 intravertebral disk
Current radiological grading system
The next step included implementing criteria used by radiologists to diagnose pelvic organ prolapse on the same images [7]. These criteria are used to classify pelvic organ prolapse into three categories of POP: small, moderate, and large (some measures were categorized by mild/moderate/severe prolapse, for clarity we translated all measures to small/moderate/large). We analyzed the radiological scales to grade of cystocele, vaginal apex prolapse, anterior pouching of the rectum (anterior rectocele), hi–posterior-most point of the pubic symphysis to the last coccygeal joint. Cystocele and vaginal prolapse were measured as the distance between the PCL and the inferior–posterior-most point of the bladder and cervix respectively. Anterior pouching of the rectum was measured as the amount of anterior outpouching from the expected anorectal wall, i.e., anterior outpouching relative to a line drawn through the anal canal [7]. Finally, the H-line (the line connecting the pubic symphysis to the posterior wall of the rectum at the level of the anorectal junction) and the M-line (the line orthogonal to the PCL that passes through the posterior end of the H-line) were measured and described hiatal enlargement and pelvic floor descent respectively. Figure 2 visualizes all of these measurements on one participant’s midsagittal MRI. All measures were checked for normality using the Shapiro–Wilk test for normality in SPSS (released 2021, IBM SPSS Statistics for Macintosh, Version 28.0; IBM, Armonk, NY, USA). Using these data, an upper and lower bound of the asymptomatic cohort was calculated by adding and subtracting 1.96 standard deviations from the mean, which encompasses 95% of the population assuming a representative sample population and a normal distribution. The bound that trended toward increased POP severity, increased descent for cystocele and vaginal prolapse, and increased length for anterior pouching, H- and M-lines, were reported. Any measure found outside of these bounds would be expected to be tending toward symptomatic POP.
Figure showing the measures used in the current radiological grading scale, based on images that appear in del Salto et al. [7]. Some organs, bones, and reference landmarks are identified: blue bladder, gray pubic bone, purple sacrum, pink coccyx. PCL pubococcygeal line, PIB posterior–inferior bladder border, PIC posterior–inferior cervix, ATP rectal anterior pouching, AR levator plate at the level of the anorectal junction. a A white dotted line that passes through the anal canal was used as a reference for the expected margin of the anterior anorectal wall as defined in del Salto et al. [7]. In light blue are the measures of anterior—length of descent of the PIB—and middle compartment—the PIC-most—descent. Additionally, the length of anterior pouching—ATP—was also shown (orange). b The length of the M- and H-lines (representative of pelvic organ descent and hiatal enlargement respectively) are drawn in gold, connecting the PCL and pubic bone to the AR
Results
Measurements relative to bony landmarks
Twenty women were recruited for the study. One of the subjects became pregnant during the study and thus was excluded. Of the 19 (age: 29.7 ± 8.2 years, Body Mass Index (BMI): 24.3 ± 4.5 kg/m2) remaining subjects, 14 (age: 30.5 ± 9.0 years, BMI: 23.7 ± 3.9 kg/m2) were able to complete evacuation, 18 (age: 29.9 ± 8.4 years, BMI: 24.5 ± 4.5 kg/m2) were able to strain, and 17 (30.1 ± 8.6 years, BMI: 24.7 ± 4.5 kg/m2) were able to squeeze during the exam. Age and BMI were not statistically different between groups. Each of these 19 subjects were included in at least one group besides rest.
The range of motion for pelvic viscera with respect to the normalized coordinate system was quantified and is summarized in Table 1. Evacuation caused the most motion in the landmarks, followed by strain, then by squeeze. On average, the majority of the motion of the landmarks was along the y’ axis. During evacuation and strain, most landmarks that started above the x’ axis (PVF, mid-vagina, and bladder neck) and descended below the x’ axis by the end of the maneuver. The only exception to this was the PVF during strain (Table 2, Fig. 3).
Results of the measurements based on bony landmarks. The black dotted line in each frame is the x’ axis. Each landmark is placed at the angle with respect to the x’ plus/minus one standard deviation. The larger image shows measures with respect to level 3 support of the posterior vaginal fornix, and the anorectal junction. The smaller image in each frame shows the measures for level 1 (hymen), and level 2 support (bladder neck and mid-vagina). Frame a shows rest, frame b shows evacuation, frame c shows strain, and frame d shows squeeze. The shapes of each of the organs are not indicative of each of the in vivo organ shapes. PCL pubococcygeal line, PVF posterior vaginal fornix, PIB posterior–inferior bladder border, PIC posterior–inferior cervix, ATP rectal anterior pouching, AR levator plate at the level of the anorectal junction, SP sacral promontory, SB S4S5 intravertebral disk, BN bladder neck, MV mid-vagina, HY hymen
With respect to the evacuation maneuver, the PVF descended on average of 125% of its initial height along the y’ axis (toward the levator plate) while only shifting 7% along the x’ axis (toward the pubic bone). The midvaginal and bladder neck landmarks descended 213% and 192% along the y’ axis while only shifting 12% (towards the sacrococcygeal joint) and 6% (towards the pubic bone) along the x’ axis respectively. The anorectal junction and hymen both started below the x’ axis and displayed less motion than the other landmarks. Descent along the y’ axis was limited to 90% and 55% of their initial height and x’ translation was limited to 11% (toward the sacrococcygeal joint) and 27% (toward the pubic bone) respectively.
Relative to the pubic symphysis, all pelvic viscera landmarks rotated caudally, staying at approximately the same distance from the pubic symphysis while the angle with respect to the x’ axis decreased in value, becoming more negative for landmarks that started below the x’ axis (Fig. 3). Rotational motion was greatest in landmarks associated with level 1 and 2 support relative to level 3 support.
Measures of current radiological grading scale
The current radiological grading scales for POP were applied to 14 subjects (age: 30.5 ± 9.0 years, BMI: 23.7 ± 3.9 kg/m2) who successfully evacuated during the examination [7]. All measurements passed the Shapiro–Wilk test for normality, with p values > 0.05. Table 3 reports the ranges of each of these grades from the literature and those same measurements conducted on our asymptomatic cohort of women. The table also reports the bound that is most likely to overlap with the current grading scale. All five of the measurements observed overlap between our asymptomatic range and POP measures (Fig. 4), indicating that these women would have small to moderate prolapse for most measures. Interestingly, the 95% range of this asymptomatic cohort overlapped with the radiological grading scale for a large anterior rectocele, indicating that most of these women would be graded to have a moderate to large prolapse based on this measure.
Distributions of the current radiological grading scale for cystocele, vaginal prolapse, anterior rectocele, hiatal enlargement, and pelvic floor descent conducted on an asymptomatic cohort. The colors along the distribution represent the different levels of the current grading scale (light blue small, blue moderate, dark blue large). The teal rectangles above each distribution show the mean (black vertical line) ± 1.96 standard deviations of the measures conducted on the asymptomatic cohort. All measurements are to scale. In some cases, the lower bound fell outside the range of the current grading scale and thus the full range was not shown. In cases where the range was cut off, the line is dashed. The mean of the range for hiatal enlargement fell outside the radiological grading scale; therefore, the range was extended to show the mean
Discussion
In this study, we described the physiological range and direction of motion of the pelvic organs in nulligravid, asymptomatic women, at rest and during three maneuvers that increase intra-abdominal pressure. Dynamic movements of these structures were observed, especially for the evacuation maneuver. The large amount of movement contradicts the perception that the pelvic viscera undergoes only relatively small motions in adequately supported women, as shown in previous studies based on a strain maneuver. The movement that was seen in this cohort substantially overlapped with diagnostic ranges of POP based on radiological grading, supporting the notion that POP is likely overdiagnosed by the existing radiological grading system. Potential sources of this overdiagnosis are that the current diagnostic methods disregard the motion of the vaginal hymen, which should not be treated as a static reference point, and the misunderstanding that only pathological organs experience large degrees of mobility.
The concept of pelvic organ mobility and its extent in a physiological setting has been a point of debate during the past decade. More recent studies have found that pelvic organs move a great deal during physiological events [8,9,10]. In one of these studies, Schreyer et al. showed substantial apical motion below the PCL during MR defecography [8]. Similarly, in our previous study focusing on the vaginal apex in women with adequate support, we found extensive motion, especially during defecation [6]. Schawkat et al. showed a similar trend to that we observed, where asymptomatic patients showed excessive posterior compartment descent [10]. Our current findings support this idea of displaying prominent motion of all pelvic organs (bladder, rectum, and vaginal apex), in asymptomatic women with no known pathological condition. This motion seems to be a crucial function of pelvic organ support enabling ample adaptation to change in intra-abdominal pressure.
Even in studies investigating the mobility of pelvic organs, there have been limited attempts at defining the asymptomatic range of motion of the pelvic viscera [6, 11, 12]. In these studies, few used bony landmarks as a reference (which removes the effect of vaginal hymen motion) [6, 11], whereas others only focused on symptomatic patients [13,14,15]. There has been some study of the dynamic motion of the bladder and rectum in asymptotic and symptomatic women [14, 15]. These studies were aimed at determining how motion correlated with POP symptom severity; however, they both used retrospective cohorts of women who had undergone a urogynecology examination for lower urinary tract dysfunction and/or prolapse [14, 15]. The studies may have shown less motion than if they compared asymptomatic and symptomatic patients [14, 15]. In addition, the study was limited to one maneuver (Valsalva), reducing the ability to quantify the full physiological range [16].
Pelvic floor support relies on suspensory ligaments located in the pelvic region. These ligaments are split into three levels of support, as described by DeLancey [17]. It has been hypothesized that laxity in any of these connective tissues and weakness of the levator ani muscles may lead to POP. Supportive connective tissues are often perceived to be limiting the motion of the pelvic organs [18]. However, these tissues must, at the same time, allow a certain degree of motion imperative for normal physiological function [19]. It seems that there is a point of equilibrium, which, on the one hand, restricts excessive motion, but, on the other, allows for normal physiology to occur. Our study showed that all three levels of support allow for rotational motion of vaginal apex, bladder neck, mid-vagina and hymen around pubic bone with level III showing the least degree of rotation. However, this motion is not observed during a physical examination. Two possible explanations are that:
-
1.
Maximum mobility can be seen during evacuation, but not strain
-
2.
POP-Q uses the hymen as a point of reference, but the hymen moves along with the organs; thus, relative motion is undermeasured
Our measurement system removes the effect of this motion by conducting measurements based on fixed axes constructed using bony landmarks [20].
The major finding of our study was reporting a range of values for the POP radiological grading system and comparing the diagnostic ranges with an asymptomatic cohort. We believe lack of standardization in what constitutes asymptomatic pelvic motion contributes to misdiagnosis of POP, which may lead to unnecessary anxiety for patients, office visits, or even surgeries to treat pelvic organ prolapse [21]. The measures reported in this study are with respect to normalized coordinate axes (x’ and y’). This normalization accounts, to some degree, for the size of patients, something that is not accounted for with current radiological scales. It can be assumed that a larger pelvis may allow for greater asymptomatic pelvic organ descent; therefore, without normalization, a patient with a large pelvis who is adequately supported could be diagnosed with POP. Another potential issue with the current method of diagnosis is the use of deformable landmarks to make standardized measurements. The PCL, as defined by the current radiological grading scale, uses points between the coccygeal vertebrae as a landmark. However, the coccyx is a highly mobile structure that moves in response to intra-abdominal pressure. Thus, its use as a landmark may contribute to inaccurate measurements and grading; previous studies have shown the reliability of using the PCL as a measurement [22].
This study was limited by the number of subjects that were able to successfully evacuate (n=14) during dynamic MRI and the overall number of subjects that were recruited (n=19). Future work will have to confirm these findings in a larger sample of women and researchers may wish to expand the upper age range to include the most common ages for POP diagnosis (60–69 years) [7]. Including a wider range of ages will allow for a larger understanding of the physiological range of motion of the pelvic viscera throughout the lifespan. Another limitation was subject position, as all subjects underwent imaging while supine. However, data collected via dynamic MRI in the supine position are accepted as clinically relevant [10]. Although we hypothesize that women with POP would display more motion along the x’ axis (toward the genital hiatus); without the introduction of a symptomatic cohort, we are unable to confirm this theory. In future analyses, these groups will need to be accounted for and then, assuming a continuous transition from adequate support to inadequate support (asymptomatic to symptomatic), future studies on symptomatic cohorts would be able to fully define a continuum of measurements that may be more predictive of POP.
In conclusion, we have shown that there were large amounts of rotational motion of the pelvic organs around the pubic bone in adequately supported women. This includes all three levels of pelvic organ support. This motion, when described using radiological grading, is likely to be considered mild (cystocele, uterine prolapse, levator descent) or moderate (anterior rectocele) prolapse, which may contribute to patient anxiety, unnecessary urogynecology visits, and reconstructive surgeries.
Abbreviations
- BMI:
-
Body mass index
- POP:
-
Pelvic organ prolapse
- PVF:
-
Posterior vaginal fornix
- POP-Q:
-
Pelvic Organ Prolapse Quantification
- PFDI-20:
-
Pelvic Floor Disability Index
- PCL:
-
Pubococcygeal line
References
Cheon C, Maher C. Economics of pelvic organ prolapse surgery. Int Urogynecol J. 2013;24:1873–6.
Subak LL, Waetjen LE, Van Den Eeden S, Thom DH, Vittinghoff E, Brown JS. Cost of pelvic organ prolapse surgery in the United States. Obstet Gynecol. 2001;98(4):646–51.
Wagner A, Pahernik S, Pandey A. Pelvic organ prolapse. J Urol Urogynäkol. 2019;26(3):87–91.
Haylen BT, Maher CF, Barber MD, Camargo S, Dandolu V, Digesu A, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic organ prolapse (POP). Int Urogynecol J. 2016;27(2):165–94.
Bump RC, Mattiasson A, Brubaker LP, DeLancey JO, Klarskov P, Shull BL, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175(1):10–7.
Rostaminia G, Routzong M, Chang C, Goldberg RP, Abramowitch S. Motion of the vaginal apex during strain and defecation. Int Urogynecol J. 2020;31(2):391–400.
Del Salto LG, de Criado JM, del Hoyo LFA, Velasco LG, Rivas PF, Paradela MM, et al. MR imaging-based assessment of the female pelvic floor. Radiographics. 2014;34(5):1417–39.
Schreyer AG, Paetzel C, Fürst A, Dendl LM, Hutzel E, Müller-Wille R, et al. Dynamic magnetic resonance defecography in 10 asymptomatic volunteers. World J Gastroenterol. 2012;18(46):6836–42.
Swenson CW, Luo J, Chen L, Ashton-Miller JA, Delancey JOL. Traction force needed to reproduce physiologically observed uterine movement: technique development, feasibility assessment, and preliminary findings. Int Urogynecol J 2016;27(8):1227–34.
Schawkat K, Heinrich H, Parker H, Barth B, Mathew R, Weishaupt D, et al. How to define pathologic pelvic floor descent in MR defecography during defecation. Abdom Radiol (NY). 2018;1(43):3233–40.
Goh V, Halligan S, Kaplan G, Healy JC, Bartram CI. Dynamic MR imaging of the pelvic floor in asymptomatic subjects. Am J Roentgenol. 2000;174(3):661–6.
Colaiacomo MC, Masselli G, Polettini E, Lanciotti S, Casciani E, Bertini L, et al. Dynamic MR imaging of the pelvic floor: a pictorial review. Radiographics. 2009;29(3):1–42.
Singh K, Reid WMN, Berger LA. Assessment and grading of pelvic organ prolapse by use of dynamic magnetic resonance imaging. Am J Obstet Gynecol. 2001;185(1):71–7.
Dietz HP, Lekskulchai O. Ultrasound assessment of pelvic organ prolapse: the relationship between prolapse severity and symptoms. Ultrasound Obstet Gynecol. 2007;29:688–91.
Wen X, Tian H, Yan X, Sun Q, Du Y, Wen D, et al. The combined measurement of pelvic organ mobility and hiatus area improves the sensitivity of transperineal ultrasound when detecting pelvic organ prolapse. Front Med. 2021;8:1–11.
Dietz HP, Eldridge A, Grace M, Clarke B. Pelvic organ descent in young nulligravid women. Am J Obstet Gynecol. 2004;191(1):95–9.
DeLancey JOL. Anatomic aspects of vaginal eversion after hysterectomy. Am J Obstet Gynecol. 1992;166(6 Pt 1):1717–24; discussion 1724–8.
Kaniewska M, Gołofit P, Heubner M, Maake C, Kubik-Huch RA. Suspensory ligaments of the female genital organs: MRI evaluation with intraoperative correlation. Radiographics. 2018;38(7):2195–211.
Addington R, Stephens RE, Phelipa MM, Widdicombe JG, Ockey RR. Intra-abdominal pressures during voluntary and reflex cough. Cough. 2008;4:2.
Betschart C, Chen L, Ashton-Miller JA, DeLancey JOL. On pelvic reference lines and the MR evaluation of genital prolapse: a proposal for standardization using the pelvic inclination correction system. Int Urogynecol J. 2013:24:1421–8.
Weintraub AY, Glinter H, Marcus-Braun N. Narrative review of the epidemiology, diagnosis and pathophysiology of pelvic organ prolapse. Int Braz J Urol. 2020;46(1):5–14.
Madill S, Tang A, Pontbriand-Drolet S, Dumoulin C. Comparison of two methods for measuring the pubococcygeal line from sagittal plane magnetic resonance imaging. Neurourol Urodyn. 2011;30:1613–9.
Author information
Authors and Affiliations
Contributions
L.C. Martin: protocol/project development, data analysis, manuscript writing/editing; H.H. Chill: data collection, data analysis; M.R. Routzong: protocol/project development, data analysis, manuscript writing/editing; S.D. Abramowitch: protocol/project development, data analysis, manuscript editing; G. Rostaminia: protocol/project development, data collection, data analysis, manuscript editing
Corresponding author
Ethics declarations
Conflicts of interest
L.C. Martin reports Renovia Inc. regarding investigator-initiated funding for a project unrelated to this work; H.H. Chill has nothing to report; M.R. Routzong has nothing to report; S.D. Abramowitch reports Renovia Inc. regarding investigator-initiated funding for a project unrelated to this work; G. Rostaminia has nothing to report.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Martin, L.C., Chill, H.H., Routzong, M.R. et al. Quantifying the physiologic motions of the pelvic viscera during evacuation in nulligravid asymptomatic women. Int Urogynecol J 34, 535–543 (2023). https://doi.org/10.1007/s00192-022-05282-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-022-05282-7