Abstract
Introduction and hypothesis
Symptoms of obstructed defecation (OD) and anatomical abnormalities of the posterior compartment are prevalent in urogynecological patients. The aim of this study was to determine whether perineal hypermobility is an independent predictor of OD, as is the case for rectocele, enterocele and rectal intussusception.
Methods
This is a retrospective study of 2447 women attending a tertiary urodynamic center between September 2011 and December 2016. The assessment included a structured interview, urodynamic testing, a clinical examination and 4D transperineal ultrasound. After exclusion of previous pelvic floor surgery and defined anatomical abnormalities of the anorectum, 796 patients were left for analysis. Perineal hypermobility was defined as rectal descent ≥ 15 mm below the symphysis pubis, determined in stored ultrasound volume datasets offline, using proprietary software, blinded to all other data. Any association between perineal hypermobility and symptoms of obstructed defecation was tested for by chi-square (X2) test.
Results
For the 796 patients analyzed, median age was 52 (range, 16–88) years with a mean BMI of 27 (range, 15–64) kg/m2. Average vaginal parity was two (range, 0–8). Reported OD symptoms in this group included sensation of incomplete emptying in 335 (42%), straining at stool in 300 (37%) and digitation in 83 (10%). At least one of those symptoms was reported by 424 (53%) women; 153 showed perineal hypermobility. There was no significant association between perineal hypermobility and OD symptoms on univariate testing.
Conclusions
We found no evidence of an independent association between perineal hypermobility and obstructed defecation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Symptoms of obstructed defecation and anatomical abnormalities of the posterior compartment are prevalent in urogynecological patients and convey a significant burden in terms of quality of life [1]. The known anatomical causes of OD include rectocoele, enterocoele, rectal intussusception and rectal prolapse [2], which on gynecological examination may be evident as descent of the posterior vaginal compartment, or ‘rectocele.’ However, any such clinically detected ‘rectocele’ may be due to perineal hypermobility, a true defect of the rectovaginal septum or radiological rectocele, recto-enterocele, rectal intussusception or occasionally an isolated enterocele [2]. The etiology, pathophysiology and symptoms of those different conditions overlap widely and are not commonly diagnosed conclusively by imaging because of a lack of expertise and/or equipment.
It has long been suspected that perineal hypermobility, the ‘descending perineum syndrome’ of the colorectal literature first described by Parks [3], can result in pelvic floor dysfunction because of excessive elongation and stretching of the pudendal nerve [4]. It may be difficult however to determine causality as hypermobility of the perineum is likely a manifestation or epiphenomenon of levator hiatal ballooning [5], which is commonly a result of hiatal overdistension in vaginal childbirth. Such overdistension is a risk factor for prolapse and prolapse recurrence and associated with some conditions known to cause obstructed defecation, such as rectal intussusception [6]. It is not surprising that perineal hypermobility is associated with prolapse and that procedures aimed at prolapse reconstruction can alleviate perineal hypermobility [7].
It has been claimed that perineal hypermobility is a cause of obstructed defecation [8]. This view appears questionable, as it may be more plausible to regard excessive straining as the cause, rather than the effect, of abnormal hiatal distension and perineal descent. A large proportion of women with obstructed defecation will have abnormalities of not just one but several pelvic floor structures such as the levator ani and/or the rectovaginal septum, making it difficult to ascertain not just causality, but even association.
The aim of this study was to determine whether hypermobility of the perineum or anorectal junction detected on imaging is an independent predictor of OD in a large population of urogynecological patients who had undergone pelvic floor ultrasound.
Materials and methods
This is a retrospective study of women attending a tertiary urogynecological clinic for the investigation of symptoms of pelvic floor dysfunction between September 2011 and December 2016. The assessment included a structured physician-directed interview, multichannel urodynamic testing, a clinical (POP-Q) examination [9] and 4D transperineal ultrasound [10]. The interview specifically queried the following symptoms of obstructed defecation: straining at stool, the sensation of incomplete bowel emptying and perineal, vaginal or anal digitation. Translabial ultrasound imaging was performed supine following bladder emptying as previously described, including imaging at rest, on pelvic floor contraction and on Valsalva maneuver lasting at least 6 s [10].
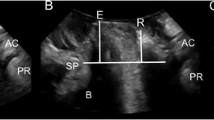
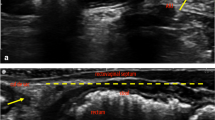
Definitions of the descending perineum syndrome vary substantially in the colorectal and radiological literature [8]. On translabial ultrasound, perineal hypermobility is defined as descent of the rectal ampulla to at least 15 mm below the symphysis pubis. Figure 1 illustrates the distinction between rectocele and perineal hypermobility. In both cases rectal contents descend to 15 mm below the symphyseal margin, but in rectocele this occurs in a diverticulum (the ‘true rectocele’), which is absent in isolated perineal hypermobility [1]. The presence of an intussusception was recorded at the time of the examination, while rectocele and enterocele were diagnosed offline at a later date by the second author on a desktop PC, using proprietary software, blinded to all other data. The criteria for these sonographic diagnoses have been validated repeatedly; for an overview see [11]. A true rectocele was diagnosed if there was an anterior diverticulum of the rectal ampulla of ≥ 10 mm in depth on maximal Valsalva. An enterocele was diagnosed if there was descent of the cul de sac to the level of the symphysis pubis, regardless of content, on maximal Valsalva. An intussusception was diagnosed if there was splaying of the anal canal with inversion of the anterior rectal muscularis into the anal canal on maximal Valsalva [11].
Abnormalities of the posterior compartment on tranbslabial ultrasound. (a) Perineal hypermobility; (b) rectocele. In both cases rectal descent of about 15 mm (vertical line) is measured against a horizontal reference line placed through the infero-posterior symphyseal margin. The dotted line in (b) outlines a true rectocele, i.e., a diverticulum of the rectal ampulla
This study was approved by the Nepean Blue Mountains Local Health District Human Research Ethics Committee (NBMLHD HREC 13–70). Statistical analysis was performed using SPSS v21. Chi-squared tests were performed for statistical analysis, and p < 0.05 was considered statistically significant. A post-hoc power calculation was performed assuming 80% power and an alpha of 0.05.
Results
Of the 2447 patients seen between 8 September 2011 and 8 December 2016, ultrasound data were missing in 114 patients, mostly because of lack of equipment availability. Seven hundred twenty patients were excluded for previous hysterectomy and 521 for previous pelvic floor surgery, leaving 1092 women. In 296 of those, we diagnosed defined anatomical abnormalities of the anorectum, i.e., true rectocele, enterocele and/or intussusception, leaving 796 patients for analysis as shown in the flow chart (Fig. 2).
In the 796 patients that were analyzed, median age was 52 (range, 16–88) years with a mean BMI of 27 (range, 15–64) kg/m2. The average vaginal parity was two (range, 0–8). 370 (46%) reported symptoms of prolapse (vaginal lump or bulge or a dragging sensation), 568 (71%) and 537 (67%) reported symptoms of stress and urge incontinence, respectively. Two hundred sixty-five (33%) had voiding dysfunction, 56 (8%) fecal incontinence and 163 (21%) constipation. Queried OD symptoms included a sensation of incomplete emptying in 335 (42%), straining at stool in 300 (37%) and digitation of any kind in 83 (10%). At least one of those symptoms was reported by 424 (53%) women.
In 153/796 women (19%), we found evidence of perineal hypermobility on imaging, with the rectal ampulla descending to at least 15 mm below a reference line placed through the infero-posterior symphyseal margin. Table 1 shows our results, with no significant association between perineal hypermobility and any individual OD symptoms or a composite of such symptoms. Apart from a trend towards an association between incomplete emptying and perineal hypermobility, all other components of OD remained non-significant.
Discussion
The results of this retrospective observational study in a large consecutively assessed cohort of urogynecological patients suggest that, in contrast to rectocele, enterocele and rectal intussusception, perineal hypermobility may not be an independent predictor for symptoms of obstructed defecation. Only the symptom of incomplete bowel emptying came close to being associated with perineal hypermobility (P = 0.08). A post-hoc power calculation suggests that a study recruiting 1282 women without any other anatomical explanation for obstructed defecation or previous pelvic surgery would be required to provide 80% power at an alpha of 0.05 to detect a significant association. This would require a population of about 4000 women to be examined. However, even if found to be statistically significant, the small effect size would suggest a lack of clinical relevance.
It has been argued that the ‘descending perineum syndrome’ is the consequence of anismus, i.e., pelvic floor dyssynergia at defecation, and that it may lead to nerve damage and all its attendant consequences [12]. It is plausible that excessive perineal descent, through whatever mechanism, would lead to pudendal neuropathy and secondary functional impairment. In some women the pudendal nerve may be stretched by 20% or more, a degree of elongation that is considered sufficient to induce neuropathy [13]. In theory, this may lead to symptoms of obstructed defecation due to both sensory and motor impairment and to anal incontinence [14].
Unfortunately, the literature on descending perineum syndrome does not contain a single study controlling for associated anatomical abnormalities such as rectocele, enterocele and rectal intussusception, let alone levator avulsion and hiatal ballooning. These conditions are all common, and some are clearly associated with symptoms of obstructed defecation. As these conditions tend to follow pathophysiological pathways that have little or nothing to do with dyssynergic defecation, they have to be controlled for when trying to determine any association between perineal hypermobility and obstructed defecation. The simplest way of controlling for such confounders is to exclude them from the analysis, which was possible in this study because of the large population investigated.
Perineal hypermobility is clearly associated with hiatal distensibility in urogynecological patients [5], and surgical colleagues acknowledge that the ‘descending perineum syndrome’ involves the entire pelvic diaphragm [12]. However, following Parks, surgeons usually see any abnormality of the pelvic floor as the result of excessive straining, not the other way around [3]. However, regardless of whether perineal hypermobility is the cause or effect of obstructed defecation, one would expect an independent association between symptoms of OD and perineal or anorectal descent. It is sometimes claimed that levator overdistension is due to excessive straining [12], when it is plainly obvious from the literature that, first, there is enormous inter-individual variation regarding hiatal distensibility, even in young, nulligravid women [15]; and second, childbirth seems to be the primary factor in acquired hiatal overdistension due to either avulsion of the puborectalis muscle or ‘microtrauma’ [16].
Strengths and weaknesses
The greatest strength of this study is the large population size, which allowed investigation of any association between perineal hypermobility and symptoms of obstructed defecation in over 750 women in whom there was no evidence of other anatomical causes of obstructed defecation. Another strength is the imaging methodology, which has been standardized internationally [17], an achievement that is absent regarding the radiological investigation of anorectal conditions associated with obstructed defecation.
There are however several weaknesses of this study that need to be acknowledged. First, this was a retrospective study without power calculations, the latter because pilot data to inform such calculations could not be obtained. In addition, we only utilized data obtained in routine clinical practice, which does not include perineal calipers [12] or obstructed defecation questionnaires, and neurophysiological tests were equally unavailable. Regarding the imaging method used, we were unable to exclude anismus as a confounder as we have not been able to validate the sonographic diagnosis of anismus in our population [18]. In addition, our patients were largely Caucasian, limiting the applicability of these findings in other ethnic groups. This is particularly relevant in view of the emerging data on the interethnic variability of posterior compartment anatomy [19]. Finally, some may consider the lack of defecation proctography or MR defecography data a weakness of this study. However, it is difficult to see how such interventions could be justified in such a large number of women, many of them asymptomatic of colorectal disorders. Translabial ultrasound has the obvious advantages of low cost, minimal effort and high tolerability [20].
In conclusion, this large retrospective study found no evidence of an independent association between perineal hypermobility and obstructed defecation. We propose that the perceived causal link between OD symptoms and the ‘descending perineum’ is spurious because of multiple anatomical confounders, with perineal hypermobility an epiphenomenon or manifestation of underlying disorders rather than a true component of causative chains.
References
Guzman Rojas R, Kamisan Atan I, Shek K, Dietz H. The prevalence of abnormal posterior compartment anatomy and its association with obstructed defecation symptoms in urogynecological patients. Int Urogynecol J. 2016;27(6):939–44.
Dietz HP, Steensma AB. Posterior compartment prolapse on two-dimensional and three-dimensional pelvic floor ultrasound: the distinction between true rectocele, perineal hypermobility and enterocele. Ultrasound Obstet Gynecol. 2005;26:73–7.
Parks A, Porter N, Hardcastle J. The syndrome of the descending perineum. Proc Royal Soc Med. 1966;59:6.
Harewood G, Coulie B, Camilleri M, Rath-Harvey D, Pemberton J. Descending perineum syndrome: audit of clinical and laboratory features and outcome of pelvic floor retraining. Am J Gastroenterol. 1999;94(1):126–30.
Chantarasorn V, Shek K, Dietz HP. Mobility of the perineal body and anorectal junction before and after childbirth. Int Urogynecol J. 2012;23:729–33.
Rodrigo N, Shek K, Dietz H. Rectal intussusception is associated with abnormal levator structure and morphometry. Tech Coloproctol. 2011;15:39–43.
Nessi A, Kane A, Vincens E, Salet-Lizée D, Lepigeon K, Villet R. Descending perineum associated with pelvic organ prolapse treated by sacral colpoperineopexy and retrorectal mesh fixation: preliminary results. Front Surg. 2018;5:50.
Chaudhry Z, Tarnay C. Descending perineum syndrome: a review of the presentation, diagnosis, and management. Int Urogynecol J. 2016;27:1149–56.
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175(1):10–7.
Dietz HP. Pelvic floor ultrasound. In: Fleischer A, editor. Sonography in obstetrics and gynecology: principles and practice. 8th ed. Columbus: McGraw Hill; 2017.
Dietz H. Ultrasound in the assessment of pelvic organ prolapse. Best Pract Res Clin Obstet Gynecol. 2019;54:12–30.
Pucciani F. Descending perineum syndrome: new perspectives. Tech Coloproctol. 2015;19:443–8.
Kiff E, Barnes P, Swash M. Evidence of pudendal neuropathy in patients with perineal descent and chronic strain at stool. Gut. 1984;25:1279–82.
Lefaucher J. Neurophysiological testing in anorectal disorders. Muscle Nerve. 2006;33:324–33.
Dietz H, Shek K, Clarke B. Biometry of the pubovisceral muscle and levator hiatus by three-dimensional pelvic floor ultrasound. Ultrasound Obstet Gynecol. 2005;25:580–5.
Shek K, Dietz H. Intrapartum risk factors of levator trauma. Br J Obstet Gynaecol. 2010;117:1485–92.
AIUM/IUGA practice parameter for the performance of Urogynecological ultrasound examinations. Int Urogynecol J. 2019;30:1389–400. https://doi.org/10.1007/s00192-019-03954-5.
Melon J, Gillor M, Neels H, Dietz H. Persistent levator co-activation is not associated with symptoms or bother of obstructed defecation. Int Urogynecol J. 2020, online ahead of print.
Cheung R, Chan S, Shek K, Chung T, Dietz H. Pelvic organ prolapse in Caucasian and East Asian women: a comparative study. Ultrasound Obstet Gynecol. 2019;53:541–5.
Dietz HP, Cartmill J. Imaging in patients with obstructed defecation. Tech Coloproctol. 2013;17:473–4.
Author information
Authors and Affiliations
Contributions
Hans Peter Dietz: Project conception, design and development; data acquisition; analysis and interpretation; drafting the manuscript, revising it critically for important intellectual content and final approval of the version to be published.
Maria Emilia Alcoba: Data acquisition; analysis and interpretation; drafting the manuscript, revising it critically for important intellectual content and final approval of the version to be published.
Talia Friedman: Data acquisition; analysis and interpretation; drafting the manuscript, revising it critically for important intellectual content and final approval of the version to be published.
Nishamini Subramaniam: Data acquisition; analysis and interpretation; drafting the manuscript, revising it critically for important intellectual content and final approval of the version to be published.
Corresponding author
Ethics declarations
Conflicts of interest
HP Dietz has received lecture honoraria and travel assistance from GE Medical and Mindray.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dietz, H.P., Alcoba, M.E., Friedman, T. et al. Is perineal hypermobility an independent predictor of obstructive defecation?. Int Urogynecol J 32, 2377–2381 (2021). https://doi.org/10.1007/s00192-021-04734-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-04734-w