Abstract
Introduction and hypothesis
We aimed to demonstrate that laparoscopic sacrocolpopexy/cervicopexy (LSC-Cx) versus anterior vaginal mesh (AVM) results in a longer vaginal length without impacting sexual activity or function.
Methods
We performed a secondary analysis of sexual outcomes of a previous randomized control trial comparing LSC-Cx and AVM in 120 women (60/group) with symptomatic POP stage ≥ 3. We evaluated sexually active (SA) and non-sexually active women (NSA) using the Pelvic Organ Prolapse/Incontinence Sexual Questionnaire-IUGA-Revised (PISQ-IR) preoperatively and 1 year postoperatively. Multivariate logistic and linear regression models were built to assess the impact of different variables on sexual activity and function, respectively.
Results
Among 120 women included, no statistically significant differences were found between vaginal length and preoperative dyspareunia (20.7% AVM vs. 22,8% LSC-Cx) comparing SA to NSA women and LSC-Cx to AVM. Vaginal length was significantly longer after LSC-Cx versus AVM (p < 0.001). The postoperative dyspareunia rate was 17.2% AVM versus 10.5% LSC-Cx. Partnered women were significantly more likely to be SA than unpartnered women before (OR = 19.04; p = 0.006) and after surgery (OR = 36.28; p = 0.002). Only dyspareunia was independently associated with sexual function pre- (B = −0.431; p = 0.017) and postoperatively (B = −0.3 96; p = 0.007).
Conclusions
Vaginal length was greater following LSC-Cx compared to AVM. While vaginal length has no impact on female sexuality pre- and postoperatively, the most important factors were “having a partner” for sexual activity and dyspareunia for sexual function. Persistence of dyspareunia was higher after AVM. LSC-Cx should be considered in women with POP undergoing mesh surgery with future sexual expectations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mesh surgery may be indicated in women with symptomatic pelvic organ prolapse (POP) with a high risk of postoperative recurrence [1, 2], such as advanced POP (stage ≥ 3). The anatomical changes of the vagina following vaginal surgery with anterior vaginal mesh (AVM) or laparoscopic sacrocolpopexy/cervicopexy (LSC-Cx) differ [3,4,5], with the abdominal approach resulting in a longer vaginal length.
However, the impact of a longer vaginal length on female sexuality is still unclear. Gutman et al. [5] reported that sexual function scores improved after vaginal mesh hysteropexy and laparoscopic sacral hysteropexy regardless of the increase in vaginal length after the abdominal approach. On the other hand, Lucot et al. [4] concluded that sexual function was better preserved following laparoscopic mesh sacropexy compared to transvaginal mesh repair, based on longer vaginal length and less dyspareunia with the abdominal approach. Moreover, a meta-analysis comparing sacrocolpopexy to transvaginal mesh surgery [6] showed that the total vaginal length (TVL) was significantly greater in women undergoing the abdominal than the vaginal mesh approach, with a pooled mean difference of 0.77 (95% CI 0.31–1.23; p = 0.001). In addition, women who were sexually active before surgery more frequently developed new onset dyspareunia after transvaginal mesh than after sacrocolpopexy, with a pooled odds ratio of 0.44 (95% CI 0.23–0.88; p = 0.02). Therefore, the authors concluded that abdominal mesh might be more beneficial than transvaginal mesh but highlighted that the results should be validated because of the very-low-quality evidence.
In this context, it is important to investigate the association between TVL and dyspareunia after POP surgery with mesh, and its real impact on female sexual activity and function. Taking this into account, we decided to further analyse data from two previous studies from a randomized controlled trial (RCT) [3, 7] by our group including women undergoing POP mesh surgery. The results of the first study (main study) showed a statistically significant difference in TVL between LSC-Cx and AVM, being longer with the abdominal approach [3]. The second study (a secondary analysis) showed that the resolution of preoperative dyspareunia was statistically significant after the LSC-Cx approach but not after AVM [7]. The present study evaluated the correlation of these findings with the sexual activity and function of these patients longitudinally over a 1-year follow-up period.
We hypothesised that surgical treatment of POP with abdominal mesh results in a longer vaginal length than with a vaginal approach, without impacting sexual activity or function.
Materials and methods
We designed a prospective, non-inferiority RCT performed from January 2011 to March 2017. Women with symptomatic POP who were candidates for primary or POP recurrence surgery with anterior vaginal wall descent (stage ≥ 3) and apical descent (stage ≥ 2) were included. Written informed consent was obtained from all the participants, who were randomly allocated to the AVM (Elevate® Anterior and Apical; AMS, Minnetonka, MN, USA) or LSC-Cx group.
Exclusion criteria included women under the age of 21, having had previous colposacropexy or a vaginal mesh procedure, a history of pelvic radiotherapy, the presence of comorbidity or having high anaesthetic risk requiring a particular approach or the inability to comprehend questionnaires or attend follow-up visits.
The trial was registered at ClinicalTrials.gov (Identifier: NCT01097200) and was approved by the Ethics Committee (reference number 2010/5989) of Hospital Clínic de Barcelona.
The methods of anatomical and sexual assessment in this RCT have been described elsewhere [3, 7]. The most relevant methods used in the present study are summarized below.
To analyse the impact of vaginal length on sexual activity and function, we compared data from the baseline visit with that at 1 year of follow-up, obtained by two urogynaecologists unrelated to the surgical interventions. The interventions were performed by two expert surgeons (one for each study arm). At both visits, the patients completed the same self-administered questionnaires. Sexual activity and function were evaluated with the Spanish version of the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire IUGA-Revised (PISQ-IR) [8]. The PISQ-IR is a condition-specific questionnaire for assessing sexuality in both sexually active (SA) and non-sexually active (NSA) patients according to Q1. To assess sexual life satisfaction, Q4a was used for NSA and Q19a for SA women, both with an inverse score, meaning that the higher the score the greater the impairment in sexual life. In addition, in SA women, satisfaction during sexual activity was evaluated with Q8a. For SA women, a global score can be obtained with the PISQ-IR summary score (mean calculation method), with higher scores (range 1.545–3.909) indicating better sexual function [9]. To date, no clear cut-off for a clinically meaningful PISQ-IR summary score has been established. Dyspareunia was assessed in both SA and NSA women. In NSA women, dyspareunia was considered when the patient reported pain as a cause of inactivity (Q2e of the PISQ-IR = strongly agree or somewhat agree), while in SA women, dyspareunia was considered when the patient reported “sometimes”, “usually” or “always” to Q11: “How often do you feel pain during sexual intercourse?” or avoidance of coital activity due to pain. De novo dyspareunia was considered in women who did not report dyspareunia prior to surgery (Q11: never, rarely or Q2e: somewhat disagree, strongly disagree), but who described dyspareunia (Q11: always, often, sometimes) or who answered sexual inactivity due to pain (Q2e: strongly agree, somewhat agree) at 1 year of follow-up.
Urinary, anal and POP symptoms were evaluated with the validated Spanish version of the Pelvic Floor Distress Inventory-20 (PFDI-20) [10], with a score ranging from 0 to 300. In addition to the questionnaires, a targeted medical history and physical examination were performed in all the patients according to the POP-Q classification.
Statistical analysis
The results are presented as absolute and relative frequencies for categorical variables and as mean and standard deviations (SD) for continuous variables. Fisher’s exact test was used for the comparative analysis of groups for categorical variables. Continuous variables were analysed with the Student’s t-test if the variables followed a normal distribution or the Mann-Whitney U test if the variables did not follow a normal distribution. The normality of the distribution of the variables was evaluated with the Kolmogorov-Smirnov test. The correlations were evaluated with Spearman’s rank correlation coefficient (rho). A multivariate logistic regression model was built to assess the impact of the different variables [age, time of menopause, having a partner, body mass index (BMI), vaginal length, dyspareunia, surgical approach] on sexual activity (SA vs. NSA according to Q1 of the PISQ-IR). In addition, multiple linear regression analysis was undertaken with the same variables to assess their impact on sexual function (according to the summary score of the PISQ-IR).
The level of significance was set at p < 0.05. All the analyses were performed with the SPSS software package (19.0 version, SPSS Inc., Chicago, IL).
Results
Preoperative assessment
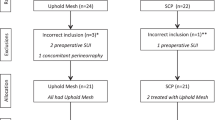
A CONSORT flow diagram of the study is shown in Fig. 1. The baseline characteristics of the participants according to the surgical approach [3] or to sexual activity/inactivity [7] have been published elsewhere. No statistically significant differences were observed between the surgical groups at baseline. However, NSA women were older (p = 0.047), had had more vaginal deliveries p = 0.015) and did not have a partner (p = 0.01) compared to SA women. There were no differences between the two approaches or between SA and NSA women on analysing concomitant comorbidities (diabetes, hypertension, neurological disorders or mental health disorders) and the time of menopause.
Among the 120 women included, the mean (SD) TVL was 8.10 (1.21) cm, ranging from 5 to 11. Patients with a previous hysterectomy had a lower baseline TVL [previous hysterectomy 7.5 (1.3) cm vs. no previous hysterectomy 8.2 (1.1) cm; p = 0.03]. Table 1 shows the baseline TVL and the prevalence of dyspareunia comparing SA to NSA women and the LSC-Cx to the AVM approach. Dyspareunia was reported by 21.7% of the women before surgery.
Preoperatively, in SA patients, a negative correlation is observed between TVL and dyspareunia (Q11), that is, the shorter the TVL, the greater the degree of dyspareunia (ρ = −0.350; p = 0.008). However, there was no correlation between TVL and satisfaction during sexual activity or sexual life satisfaction. On the other hand, no correlation was found between TVL and NSA due to pain or sexual life satisfaction in NSA patients.
Regression and linear models were used to further investigate the relationship of TVL and dyspareunia with other factors to determine possible variables which could impact sexual activity (according to Q1 of the PISQ-IR) and sexual function (according to the PISQ-IR summary score) in the preoperative assessment (Table 2). In relation to sexual activity, partnered women had a higher and statistically significant probability of being SA than unpartnered women. In relation to sexual function, it was found that the mean PISQ-IR summary score decreased significantly by 0.431 points in SA women who reported pain during sexual activity; “having a partner” was excluded from the model since all but one SA woman were partnered at baseline.
Postoperative assessment
Up to 95.8% of the women studied attended the 1 year follow-up visit and answered the questionnaires. Dyspareunia was reported by 13.9%. Of note was de novo dyspareunia rate of 10.11% at 1 year after surgery (10.87% AVM vs. 9.3% LSC-Cx). Analyses of the different parameters of TVL in NSA versus SA women and according to surgical approach are shown in Tables 3 and 4, respectively. Other variables which could impact female sexuality after POP surgery with mesh in SA versus NSA women and according to surgical approach are shown in Tables 5 and 6, respectively. There were no statistically significant differences in POPQ stage between SA and NSA or according to the type of surgery.
In relation to postoperative sexual activity, the logistic regression model is shown in Table 7. “Having a partner” was the only variable significantly associated with sexual activity. A multivariate linear regression model was again used to evaluate factors independently associated with the PISQ-IR summary score in all SA women after surgery (Table 7). Dyspareunia was found to be statistically associated with sexual function; “having a partner” was excluded because only one SA woman had no partner at 1 year of follow-up.
Discussion
The present study showed vaginal length does not influence sexual activity or function either pre- or postoperatively. Partnered women were more SA before and after surgery than unpartnered women, and dyspareunia was the main factor influencing sexual function both pre- and postoperatively.
Association between TVL and sexual function and sexual activity
To our knowledge, this is the first study on vaginal length after LSC-Cx and AVM and its association with female sexuality in both SA and NSA women. In relation to TVL, we found that the TVL was associated with the surgical approach, being statistically significantly longer after LSC-Cx than after AVM, and after adjustment for different factors, no association was found between TVL and sexual function or sexual activity/inactivity.
A multicentre, prospective parallel cohort study [5] comparing laparoscopic sacral hysteropexy to vaginal mesh hysteropexy reported increased vaginal length after the abdominal approach (p < 0.001). In that study, a linear regression model showed no difference between groups in sexual function [Female Sexual Function Index (FSFI) total score] after adjusting for age, parity, POP-Q C and Bp, menopausal status and the baseline score. However, sexual satisfaction was significantly greater after abdominal surgery (p = 0.02). These results should be interpreted with caution since there may be several reasons for the differences in sexual outcomes: (1) baseline differences between groups (greater number of postmenopausal and older women in the vaginal group); (2) fewer SA women at 1 year with the vaginal approach (44% vs. 72%); (3) the lack of patient randomisation, that is, surgeons/patients may have been more likely to recommend/accept vaginal mesh for women less likely to be SA in the future. Other studies on different POP surgeries [11,12,13] also did not find an association between vaginal length and sexual function. Moreover, a retrospective study in symptomatic women with pelvic floor dysfunction [14] concluded that vaginal topography did not correlate with sexual function based on PISQ-12. However, these authors found that sexual activity was associated with longer vaginal length (+1 cm), even when controlling for potential confounding factors (BMI, age, educational status, menopausal status, advanced prolapse and prior hysterectomy). Thus, the study concluded, choosing a surgical approach known to better provide adequate vaginal length should be considered for women with POP undergoing surgery who want to maintain or begin sexual activity. However, the authors stated that the clinical significance of this slightly longer vaginal length was uncertain, since a difference of 1 cm may be more significant for women with overall shorter vaginal lengths.
In an attempt to answer this question, we analysed other vaginal length parameters in addition to the TVL. The first parameter was the change in TVL, that is, the difference between pre- and postoperative TVL, to verify whether women who postoperatively lose length have worse sexual function and/or are more NSA than those who gain length. Second, we evaluated the difference in pre- versus postoperative TVL related to preoperative TVL (relative change of TVL) to determine whether a greater proportional loss of TVL is associated with sexual inactivity and/or worse sexual function.
We observed a statistically significant greater loss of vaginal length in absolute and relative terms after the vaginal approach. Nevertheless, the change in TVL and the relative change of TVL were not factors independently related to sexual activity or function in the multivariate analysis. Therefore, we concluded that all the vaginal length parameters have no impact on the quality of sexual function or on the decision to be SA or NSA. The results of a recent study [15] on women after native tissue apical POP repair with antiincontinence surgery were consistent with our findings. In their analysis, the authors confirmed that TVL, genital hiatus and perineal body measured immediately postoperatively had no relationship with 2-year postoperative sexual function (PISQ-12) or treatment for painful sexual intercourse.
Another study [13] found a slight reduction of vaginal dimensions after urogynaecological surgery [mean decrease in vaginal length: 1 (1.8) cm; p < 0.001] which was not correlated with any change in sexual function. Unfortunately, this study did not use validated questionnaires and did not report on NSA women. It is of note that the authors tried to further investigate the relationship between objectives measures of vaginal dimensions and patient perception. Women were asked whether they thought there was any problem with the length of the vagina related to sexual activity, and 87% reported that there was no problem with vaginal length after surgery (change −1 cm). Of note, 11.5% of the women who considered that the vagina was too short after surgery had a change of −1.25 cm, only 25 mm less than women with a normal perception. Women who described the vaginal length as too short were more likely to experience dyspareunia. Therefore, the link between vaginal dimensions and women’s perceptions warrants further studies with validated questionnaires to assess sexuality in both SA and NSA women.
Finally, an interesting prospective cohort study [16] including 208 healthy premenopausal women found no significant differences between sexual function or orgasm (FSFI) and genital measurements. The breadth of the distribution of the measurements highlights the fact that ‘normal’ female genital measurements can vary and may explain why vaginal dimensions play only a minor role after surgery. On the other hand, this study observed a positive correlation between the FSFI and the Female Genital Self-image Scale Questionnaire, associating high genital perception with high sexual function. This finding is consistent with other studies reporting an association between genital/body image and sexual function in women with POP [17, 18] and an improvement after surgery [19, 20]. Thus, genital perception should be included as an outcome as valuable as vaginal dimensions in the population with POP.
Other factors associated with sexual activity
Changes in sexual activity and function after POP surgery were analysed in a recent systematic review [21], observing that a lack of partner or partner-related problems were common reasons for sexual inactivity, and pain was the primary reason for sexual inactivity in approximately 7.7%. However, these findings should be interpreted with caution since very few of the studies included reported both pre- and postoperative rates of sexual activity, in contrast with our study which included pre- and postoperative assessment. In accordance with this systematic review [21], our results demonstrated partnered women have a higher and statistically significant probability to be SA than unpartnered women both before and after surgery. Similarly, a multicentre, cross-sectional study of women with POP stage ≥ 2 [17] reported that marital status was also independently associated with sexual activity. Moreover, in that study, age, hypertension and body image score were also independently associated with sexual activity, whereas prior urogynaecological surgery, menopause, the POPDI score and POP-Q stage were not. In our sample, sexual inactivity seemed to be related to age and time of menopause, but the association disappeared when adjusted for other factors. Symptoms (PFDI), stage (POPQ) and type (compartment) of POP were not included in the preoperative multivariate analysis because of the homogeneity of these variables in our sample.
Other factors associated with sexual function
Our findings demonstrate that SA women with dyspareunia have worse sexual function than SA women without dyspareunia pre- and postoperatively.
Before surgery, one out of five women reported dyspareunia. In a prospective cohort study [22] of patients undergoing vaginal (66% with mesh) or abdominal repair (97% with mesh), Gupta et al. assessed baseline dyspareunia among SA women (PISQ-12), with 14.3% of patients with abdominal and 14.5% of patients with vaginal surgery reporting dyspareunia. Our slightly highest baseline dyspareunia rate may be due the inclusion of NSA women in our analysis.
In our study, after adjusting for age, time of menopause and TVL, a statistically significant decrease of 18% was observed in the global sexual function score in SA women who reported dyspareunia. Again, because of the homogeneity of these variables in our sample, symptoms (PFDI), stage (POP-Q) and type (compartment) of POP were not included in the preoperative multivariate analysis. The previously mentioned multicentre, cross-sectional study [17] evaluated factors independently associated with sexual function and found that the BMI, POPDI, and the Modified Body Image Score were independently associated with the total PISQ-12 score (B = −0.23, p < 0.005; B = −0.48, p < 0.04; B = −0.37, p < 0.0001; respectively). In that study, POP symptoms resulted in the highest reduction (−0.480) in the global sexual function score (PISQ-12, range 0–48), that is, only 1% of the total score. Therefore, preoperative assessment of sexual function in women with POP including all these factors should be performed, especially the presence of dyspareunia, which, according to our results, is one of the most important determinants of sexual dysfunction.
After adjusting for age, time of menopause, BMI, TVL, change of TVL, relative change of TVL, type of surgery and POP-Q in our sample, a statistically significant decrease of 16.7% was observed in the global sexual function score in SA women who reported dyspareunia following surgery. Thus, despite good anatomical correction and improvement of POP symptoms [10], pain during sexual activity (persistence of dyspareunia or de novo dyspareunia) still impairs sexual function after surgery.
In the present analysis, we failed to demonstrate statistically significant differences in dyspareunia when both surgical approaches were compared, probably because of an unpowered sample for that purpose. However, in a previous study by our group [7], we found that the resolution of dyspareunia after surgery was significantly reduced after LSC-Cx but not after AVM at the mid-term follow-up, indicating that the persistence of dyspareunia was higher after the vaginal approach. Similar to our study, Gupta et al. described a decrease in dyspareunia rates at each time point in the abdominal group, while remaining stable in the vaginal group. Nevertheless, this trend did not reach statistical significance at either 6 or 12 months. On the other hand, in a multicentre RCT [4], including 129 LSC-Cx and 128 vaginal mesh interventions, the rate of postoperative dyspareunia among SA women at 1 year of follow-up was significantly higher after the vaginal mesh approach, with the authors concluding that sexual function was better preserved after LSC-Cx compared to AVM. These authors suggest that the abdominal approach should be performed whenever possible as the first-line surgical treatment, especially in SA women.
De novo dyspareunia could be an important cause of worse sexual function. The previously mentioned systematic review [21] stated a rate of de novo dyspareunia of 9% after transvaginal mesh procedures and 5.9% after sacrocolpopexy, based on moderate-quality studies. Likewise, in a recent meta-analysis comparing sacrocolpopexy to transvaginal mesh surgery, Zhang et al. [6] concluded that very-low-quality evidence suggests that sacrocolpopexy might be more beneficial than transvaginal mesh surgery in terms of de novo dyspareunia. The overall de novo dyspareunia rate of our study was in line with these previous studies, albeit without achieving statistically significant differences between approaches, probably due to the need for a larger sample size.
Strengths and limitations
The main strength of our study lies in the use of the condition-specific PISQ-IR questionnaire to assess not only SA but also NSA women. Moreover, this tool allowed the description of validated definitions of sexual activity, function and dyspareunia. This analysis also benefits from the pre- and postoperative widespread sexual assessment. Lastly, we achieved a high follow-up rate, and postoperative examinations were performed by two urogynecologists unrelated with the surgery.
Nonetheless, there are inherent limitations to the secondary analysis. While this study may be insufficiently powered to identify differences in sexual data between groups, we wanted to explore secondary outcomes related to the pre- and postoperative sexuality of our patients following the current recommendation [21, 23] and to highlight that vaginal length may not be as significant as previously thought in relation to sexual function. Another limitation is that we did not include an instrument to evaluate body image perception. Finally, the single-centre design of the study was also a limitation. Nonetheless, while our results are less generalizable because only two expert surgeons (one for each arm) performed all the procedures, this fact also minimizes the influence of the surgeon’s experience and the technique used.
The implications of these new data
An important caveat is that the quality of future studies would be improved with the use of validated definitions of sexual activity, function and dyspareunia and reporting of these measures both pre- and postoperatively [21].
Our study included a sample of both NSA and SA women with advanced POP who underwent thorough sexual assessment before and 1 year after surgery. For the purpose of our study, we used the PISQ-IR, which also allows recording factors playing a major role in sexual function such as pain during sexual activity in both NSA and SA patients. Moreover, our data highlight the importance of evaluating not only anatomical outcomes such as vaginal length but also other relevant factors such as “having a partner” to adequately assess female sexuality in women with POP before and after surgery.
Conclusions
In summary, LSC-Cx results in a longer vaginal length compared to AVM, although this increase in length does not influence female sexual activity/inactivity and/or sexual function. Conversely, “having a partner” played an important role in women’s decisions about being SA or NSA pre- and postoperatively. In women with advanced POP, dyspareunia is the most relevant factor, related to worse sexual function before and after surgery. Postoperative pain during sexual activity is caused by de novo dyspareunia or by the persistence of dyspareunia, which is higher after the vaginal approach. Accordingly, an abdominal surgical approach should be considered in women with POP undergoing mesh surgery who wish to maintain or recover their sexuality. Further prospective RCTs with larger sample sizes and including sexual outcomes as a main variable using the PISQ-IR pre- and postsurgery are needed to confirm our findings.
References
Glazener CM, Breeman S, Elders A, et al. Mesh, graft, or standard repair for women having primary transvaginal anterior or posterior compartment prolapse surgery: two parallel-group, multicentre, randomised, controlled trials (PROSPECT). Lancet. 2016;389(10067):381–92. https://doi.org/10.1016/S0140-6736(16)31596-3.
Maher C, Feiner B, Baessler K, Christmann-Schmid C, Haya N, Marjoribanks J. Transvaginal mesh or grafts compared with native tissue repair for vaginal prolapse. The Cochrane data base of systematic reviews. 2016;2:CD012079. https://doi.org/10.1002/14651858.CD012079.
Bataller E, Ros C, Anglès S, et al. Anatomical outcomes 1 year after pelvic organ prolapse surgery in patients with and without a uterus at a high risk of recurrence: a randomised controlled trial comparing laparoscopic sacrocolpopexy/cervicopexy and anterior vaginal mesh. Int Urogynecol J. 2019;30:545. https://doi.org/10.1007/s00192-018-3702-7.
Lucot JP, Cosson M, Bader G, et al. Safety of Vaginal vaginal mesh surgery versus laparoscopic mesh sacropexy for cystocele repair: results of the Prosthetic Pelvic Floor Repair (PROSPERE) Randomized Controlled Trial. Eur Urol. 2018;74(2):167–76. https://doi.org/10.1016/j.eururo.2018.01.044.
Gutman RE, Rardin CR, Sokol E, et al. Vaginal and laparoscopic mesh hysteropexy for uterovaginal prolapse: a parallel cohort study. Am J Obstet Gynecol. 2017;216(1):38.e1–38.e11. https://doi.org/10.1016/j.ajog.2016.08.035.
Zhang CY, Sun ZJ, Yang J, Xu T, Zhu L, Lang JH. Sacrocolpopexy compared with transvaginal mesh surgery: a systematic review and meta-analysis. BJOG. 2020. https://doi.org/10.1111/1471-0528.16324.
Anglès-Acedo S, Ros-Cerro C, Escura-Sancho S, Palau-Pascual MJ, Bataller-Sánchez E, Espuña-Pons M, et al. Sexual activity and function in women with advanced stages of pelvic organ prolapse, before and after laparoscopic or vaginal mesh surgery. Int Urogynecol J. 2020. https://doi.org/10.1007/s00192-020-04406-1.
Mestre M, Lleberia J, Pubill J, Espuna-Pons M. Spanish version of the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire IUGA-Revised (PISQ-IR): Transcultural validation. Int Urogynecol J. 2017;28:1865–73. https://doi.org/10.1007/s00192-017-3312-9.
Constantine ML, Pauls RN, Rogers RR, Rockwood TH. Validation of a single summary score for the prolapse/Incontinence sexual questionnaire–IUGA revised (PISQ-IR). Int Urogynecol J. 2017;28(12):1901–7. https://doi.org/10.1007/s00192-017-3373-9.
Sanchez-Sanchez B, Torres-Lacomba M, Yuste-Sanchez MJ, et al. Cultural adaptation and validation of the Pelvic Floor Distress Inventory short form (PFDI-20) and Pelvic Floor Impact Questionnaire short form (PFIQ-7) Spanish versions. Eur J ObstetGynecolReprodBiol. 2013;170:281–5. https://doi.org/10.1016/j.ejogrb.2013.07.006.
De La Cruz JF, Myers EM, Geller EJ. Vaginal versus robotic hysterectomy and concomitant pelvic support surgery: a comparison of postoperative vaginal length and sexual function. J Minim Invasive Gynecol. 2014;21:1010–4.
Uçar MG, et al. Sexual functioning before and after vaginal hysterectomy to treat pelvic organ prolapse and the effects of vaginal cuff closure techniques: a prospective randomised study. Eur J Obstetrics Gynecol Reprod Biol. 206:1–5.
Weber AM, Walters MD, Piedmonte MR. Sexual function and vaginal anatomy in women before and after surgery for pelvic organ prolapse and urinary incontinence. Am J Obstet Gynecol. 2000;182:1610–5.
Edenfield AL, Levin PJ, Dieter AA, Amundsen CL, Siddiqui NY. Sexual activity and vaginal topography in women with symptomatic pelvic floor disorders. J Sex Med. 2015;12:416–23.
Siff LN, Barber MD, Zyczynski HM, Rardin CR, Jakus-Waldman S, Rahn DD, et al. NICHD pelvic floor disorders network immediate postoperative pelvic organ prolapse quantification measures and 2-year risk of prolapse recurrence. Obstet Gynecol. 2020;136(4):792–801. https://doi.org/10.1097/AOG.0000000000004043.
Ellibeş Kaya A, Doğan O, Yassa M, Başbuğ A, Özcan C, Çalışkan E. Do external female genital measurements affect genital perception and sexual function and orgasm? Turk J Obstet Gynecol. 2020;17(3):175–81. https://doi.org/10.4274/tjod.galenos.2020.89896.
Lowenstein L, Gamble T, Sanses TV, van Raalte H, Carberry C, Jakus S, et al. Sexual function is related to body image perception in women with pelvic organ prolapse. J Sex Med. 2009;6:2286–91.
Sung VW, Rogers RG, Barber MD, Clark MA. Conceptual framework for patient-important treatment outcomes for pelvic organ prolapse. Neurourol Urodyn. 2014;33(4):414–9. https://doi.org/10.1002/nau.22397.
Lowenstein L, Gamble T, Sanses TV, van Raalte H, Carberry C, Jakus S, Pham T, Nguyen A, Hoskey K, Kenton K; Fellow’s pelvic research network. Changes in sexual function after treatment for prolapse are related to the improvement in body image perception. J Sex Med 2010;7(2 Pt 2):1023-1028. https://doi.org/10.1111/j.1743-6109.2009.01586.x
Lowder JL, Ghetti C, Moalli P, Zyczynski H, Cash TF. Body image in women before and after reconstructive surgery for pelvic organ prolapse. Int Urogynecol J. 2010;21(8):919–25. https://doi.org/10.1007/s00192-010-1141-1.
Antosh DD, Kim-Fine S, Meriwether KV, Kanter G, Dieter AA, Mamik MM, et al. Changes in sexual activity and function after pelvic organ prolapse surgery: a systematic review. Obstet Gynecol. 2020;136(5):922–31. https://doi.org/10.1097/AOG.0000000000004125.
Gupta P, Payne J, Killinger KA, et al. Analysis of changes in sexual function in women undergoing pelvic organ prolapse repair with abdominal or vaginal approaches. Int Urogynecol J. 2016;27:1919. https://doi.org/10.1007/s00192-016-3066-9.
Maher C, Baessler K, Barber M, Cheon C, Consten E, Cooper K, et al (2016) Pelvic organ prolapse surgery. In: Incontinence Abrams P, Cardozo L, Wagg A, Wein A, editors. International consultation on Incontinence, 6th edition, Tokyo; pp. 1855-1991. ISBN: 978-0-9569607-3-3.
Acknowledgements
We thank Dr. Emilia Sánchez for her contribution to the statistical analyses.
Funding
The Elevate® Anterior and Apical kits were donated by AMS as a grant for the study without any other support or supervision.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Bataller was a consultant for AMS (Astora Women’s Health). The remaining authors claim no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Anglès-Acedo, S., Ros-Cerro, C., Escura-Sancho, S. et al. Female sexuality before and after sacrocolpopexy or vaginal mesh: is vaginal length one of the key factors?. Int Urogynecol J 33, 143–152 (2022). https://doi.org/10.1007/s00192-021-04697-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-04697-y