Abstract
Introduction and hypothesis
Weakness of the pelvic floor is quite common among women, and may occur following childbirth. The aim of this study was to compare pelvic floor muscle strength in women of reproductive age who were nulliparous or who had a cesarean section or normal vaginal delivery.
Methods
In this cross-sectional study, 341 women including 96 nulliparous women, 73 women with a history of normal vaginal delivery with and without episiotomy, and 172 women with a history of elective or emergency cesarean section were recruited randomly from public health centers in Ahvaz, Iran. Data were collected using a sociodemographic questionnaire and a checklist was used to record weight, height, body mass index, and pelvic floor muscle strength. Pelvic floor muscle strength was measured with the woman in the lithotomy position using a Peritron 9300 V perineometer. Data were analyzed using one-way analysis of variance, the least significant difference test and the chi-squared test.
Results
The nulliparous women had the highest mean pelvic muscle strength (55.62 ± 15.86 cm H2O). Women who had vaginal delivery with episiotomy had the lowest pelvic muscle strength (32.71 ± 14 cm H2O). In nulliparous women pelvic floor muscle strength was higher than in women who had normal vaginal delivery with episiotomy (p < 0.001), but was not significantly different from that in women with normal vaginal delivery without episiotomy or in women with cesarean section (elective or emergency, p = 0.245).
Conclusions
Nulliparous women had the highest pelvic floor muscle strength and there was no significant difference in pelvic floor muscle strength between women with normal vaginal delivery and those with cesarean section.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pelvic floor disorders (PFDs) may occur following childbirth. It is estimated that the prevalence of PFDs in the United States is 24% [1]. A study of 240 Iranian women aged 35–54 years showed that 89% had at least one PFD [2]. Predisposing factors for PFDs are age, vaginal delivery and obesity [1, 3, 4]. PFDs have physical, emotional and financial consequences for patients. It was estimated that more than 225,000 American women with PFDs underwent reconstructive surgery in 1997 [5]. The scores on the Pelvic Floor Distress Inventory [6] and Body Image Scale [7] are significantly lower in women with PFDs than in women with a normal pelvic floor.
Diez-Itza et al. [8] assessed pelvic organ support in 382 primigravida women 6 months after childbirth. Women with instrumental vaginal delivery were five times more likely to undergo an examination for pelvic organ prolapse (OR 5.52, 95% CI 1.79–17.30) than those who had a cesarean section, while women with spontaneous vaginal birth were three times more likely (OR 3.19, 95% CI 1.07–9.49). In another study, in 469 women with obstructed defecation syndrome, posterior pelvic floor dysfunction was assessed using dynamic 3D ultrasonography [9]. Older women experienced more posterior pelvic floor dysfunction, while there were no significant relationships between mode of delivery and parity and posterior pelvic floor dysfunction. Chen et al. studied 110 nulliparous women who planned to undergo normal vaginal delivery or elective cesarean section. Pelvic organ support was assessed at 36–38 weeks of gestation and 6 and 12 months after childbirth using the POP-Q system. Women with normal vaginal delivery were more likely to have pelvic organ prolapse 1 year after delivery than those who had a cesarean section (OR 0.04, 95% CI 0.01–0.18) [10].
A study in 365 Iranian women assessed the risk factors of pelvic organ prolapse using the POP-Q system and demonstrated that age, normal vaginal delivery and episiotomy were the most relevant risk factors for pelvic organ prolapse [11]. The rate of cesarean section in the Iranian population is as high as 50% in some hospitals [12]. One of the reasons that women undergo elective cesarean section is concerns about pelvic organ relaxation. A qualitative study by Faisal et al. showed that Iranian women choose cesarean section because of fear of childbirth, and complications after vaginal delivery such as pelvic organ prolapse and dyspareunia [13]. The primary aim of this study was to compare pelvic floor muscle strength in nulliparous women and women with normal vaginal delivery or cesarean section among Iranian women of reproductive-age.
Materials and methods
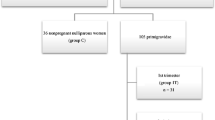
This was a cross-sectional study of 341 women including 172 with a history of cesarean section (86 elective and 86 emergency), 73 with a history of vaginal delivery with episiotomy (46) or without episiotomy (27) and 96 nulliparous women, who were recruited randomly from public health centers in Ahvaz, Iran. All women who had normal vaginal delivery with episiotomy had mediolateral episiotomy (the type of episiotomy was confirmed by inspection in each participant). The number of subjects in each group was calculated according to the procedure described by Baytur et al. [14], in which α was 0.05 and the power of study 0.8. The Ethics Committee of Ahvaz Jundishapur University of Medical Sciences approved the design of this study. Each participant gave written informed consent before data collection. Women who had given birth (normal vaginal delivery with episiotomy, normal vaginal delivery without episiotomy or cesarean section) in the previous 6 months and nulliparous women were included. Women less than 20 years old, multiparous women with a history of more than one delivery, women with a history of vaginal delivery before a cesarean section, women with a history of third and fourth degree vaginal tears, women with any spinal disorder, chronic cough or chronic constipation, smokers, and women engaged in heavy physical work were excluded from the study.
Eight public centers were randomly selected from among 22 in Ahvaz, four of which were located on the east bank and four on the west bank of the river in Ahvaz. Nulliparous women were also recruited randomly from eight public health centers. Eligible nulliparous women in each center were recruited when they came to the clinic for preconception counseling and care. Women who did not attend the clinic were contacted by one of the researchers and invited to attend. In total, 12 nulliparous women were recruited from each public health center.
Measures
A sociodemographic questionnaire was used to gather data regarding personal characteristics and factors related to pelvic relaxation. The content validity of the questionnaire was rated. A checklist was used to record data regarding pelvic floor muscle strength. The weight and height of each participant were measured using a Seca scale and a stadiometer with the subject wearing light clothing and barefooted. Body mass index (BMI) was calculated as kilograms per meter squared [15].
Procedure for measuring pelvic floor muscle strength
First, with the participant in the lithotomy position. the health provider placed her index and middle fingers in the vagina, and the participant was requested to press on the fingers with the pelvic muscles as hard as possible. This procedure was implemented to check the accuracy of the participant’s pressure on the pelvic floor muscles. A perineometer (Peritron 9300 V) was then placed in the vagina, and the participant was requested to press on the device as hard as possible with the pelvic muscles. The Peritron 9300 V is a hand-held microprocessor-controlled perineometer for assessing pelvic floor muscle strength. It is able to record muscle pressure in the range 0–300 cm H2O). This device is supplied with a vaginal sensor. The number displayed on the device was recorded as the pelvic floor muscle strength. This procedure was repeated three times and the average was recorded on the checklist. A condom was used to cover the device before inserting it into the vagina. The perineometer shows good reliability in measuring the strength and endurance of the pelvic floor muscles [16].
Statistics
All data were analyzed using SPSS version 18. The normality of continuous data was checked with the Kolmogorov-Smirnov test. One-way analysis of variance was used to compare groups regarding continuous data and the least significant difference (LSD) test was used as a post-hoc test. The chi-squared test was used for categorical data and p < 0.05 was considered significant.
Results
Most participants were under 30 years of age, and most of them in the five groups were overweight (BMI >25 kg/m2). Most of the women were housewives and had a secondary high school education. Table 1 shows other sociodemographic characteristics of the participants.Table 2 shows the mean pelvic muscle strengths in the five groups of participants. The nulliparous women had the highest mean pelvic muscle strength (55.62 ± 15.86 cm H2O). Women with vaginal delivery with mediolateral episiotomy had the lowest pelvic muscle strength (32.71 ± 14 cm H2O). There were significant differences in pelvic floor muscle strength among the five groups of participants (p = 0.02).
The LSD post hoc test showed a significant difference in pelvic muscle strength between nulliparous women and women with normal vaginal delivery and mediolateral episiotomy (p < 0.001). There was also a significant difference between nulliparous women and women with emergency cesarean section (p = 0.01). The mean pelvic muscle strength in women with normal vaginal delivery and mediolateral episiotomy was the lowest and was significantly different from the scores in nulliparous women, women with normal vaginal delivery without episiotomy, and women with elective or emergency cesarean section (p < 0.001 for all groups). Nulliparous women had greater pelvic muscle strength than women with normal vaginal delivery and mediolateral episiotomy (55.62 ± 15.86 vs. 32.71 ± 14 cm H2O, p < 0.001). Pelvic muscle strength in nulliparous women was not significantly different from that in women with normal vaginal delivery without episiotomy and women with either elective or emergency cesarean section (p = 0.245).
Discussion
This study was designed to compare the strength of the pelvic muscles in nulliparous women and women with normal vaginal delivery or cesarean section. Five groups of women were enrolled (women with either elective or emergency cesarean section, women with normal vaginal delivery with or without mediolateral episiotomy, and nulliparous women). Women with normal vaginal delivery and mediolateral episiotomy had the weakest pelvic muscles and nulliparous women had the strongest pelvic muscles. In a retrospective cohort study, Signorello et al. found that women who had a midline episiotomy had a greater risk of fecal incontinence 3 and 6 months after childbirth than women with an intact perineum or spontaneous laceration [17]. These results are similar to those found in the present study with the exception that all women in our study had mediolateral episiotomy. It has been shown that mediolateral episiotomy is not associated with an increased risk of prolapse and urinary and fecal incontinence compared with midline episiotomy. However, the role of episiotomy as a protective factor for pelvic organ relaxation remains unknown [18].
In a study evaluating abnormalities in levator ani muscles using magnetic resonance imaging in 80 nulliparous and 160 primiparous women who gave birth vaginally, none of the nulliparous women had levator ani defects, while 20% of the primiparous women had apparent levator ani defects and most of them had stress urinary incontinence [19]. These results are in line with our findings. In this study, women with elective cesarean section and normal vaginal delivery without episiotomy or perineal tears had almost the same pelvic floor muscle strength.
Rortveit et al. investigated the prevalence of incontinence of any type in 3,068 women aged 20 years or older who were nulliparous or had given birth by cesarean section or normal vaginal delivery. The mean ages of the women in the three groups were 31 ± 12, 36 ± 8.3 and 39.8 ± 8.4 years, respectively. Women with cesarean section were 1.5 times more likely to have incontinence of any type than nulliparous women (OR 1.5, 95% CI 1.2–1.9), and women with vaginal delivery were at higher risk of incontinence of any type than women with cesarean section (OR 1.7, 95% CI 1.3–2.1) [20]. These results are not in line with our findings. The reason for this discrepancy may be that Rortveit et al. only asked women about incontinence of any type and did not measure the strength of the pelvic muscles. Rørtveit and Hannestad found that cesarean section can protect women against urinary incontinence, but this effect decreases with age [21]. Considering the risks of cesarean section (heavy blood loss, risk of thrombosis events after surgery and overall increased risk of maternal morbidity and mortality), it is not recommended that women undergo cesarean section for prevention of pelvic relaxation.
In a study by Batista et al. in 31 women with normal vaginal delivery, 30 women after cesarean section and 30 nulliparous women, women with normal vaginal delivery had lower pelvic floor strength than women with cesarean section (25.6 ± 14.5 vs. 39.6 ± 22 cm H2O, p < 0.01) [22]. In our study, the strength of the pelvic muscles in women with normal vaginal delivery and those with elective cesarean section was almost the same (53.88 ± 20.9 vs. 52.9 ± 21.29 cm H2O, respectively). This indicates that normal vaginal delivery without perineal damage does not affect pelvic floor muscle strength.
In a study by Gameiro et al. [23] in 100 nulliparous and primiparous women comparing pelvic floor muscle strength during pregnancy (20 and 36 weeks of gestation) and 45 days after delivery, primiparous women had significantly lower muscle strength 45 days after delivery. These results are not in line with our results, as we found that pelvic floor muscle strength in nulliparous and primigravida women was almost the same. The reason for this discrepancy may be that we evaluated women 6 months after childbirth and Gameiro et al. assessed women 45 days after childbirth.
In a study by Petricelli et al. in 60 pregnant women (30 nulliparous and 30 multiparous) at 35–40 weeks of gestation, muscle strength and electrical activity in nulliparous women was significantly higher than in multiparous women (p < 0.05) [24]. These results are not in line with our results, as we found that pelvic muscle strength was not different between nulliparous and primiparous women with vaginal delivery and without episiotomy. The reason for this discrepancy may be that in the study by Petricelli et al. multiparous women were significantly older and had higher BMI than the nulliparous women.
Strengths and limitations of the study
To the best of our knowledge this is the first study of pelvic floor muscle strength measured using an objective method (perineometer) in women of reproductive age in Iran. The rate of cesarean section [12] and also episiotomy [25] in Iran is quite high especially among primigravida women. Most women request cesarean section because of fear of childbirth and pelvic relaxation after normal vaginal delivery.
We only enrolled gravida 1 women for comparison with nulliparous women; perhaps the inclusion of multigravida women would have revealed differences with greater significance in the comparison between parous and nulliparous women. The use of a pressure measuring instrument particularly in localizing the muscle contributing to changes in pelvic floor strength is also a limitation of this study. Race is a very important factor in differences between the findings of our study and those of others. Finally, we did not check the baseline muscle strength of the pelvic floor before pregnancy, during pregnancy and immediately after childbirth. By 6 months after childbirth, when pelvic floor muscle strength was measured, the nervous system and pelvic muscle strength may have recovered; however this measurement time was the same for all groups of women recruited.
Conclusions
This study showed that there are no differences in pelvic floor muscle strength between nulliparous women and women with normal vaginal delivery or elective cesarean section. Women with normal vaginal delivery plus mediolateral episiotomy had the lowest muscle strength followed by those with emergency cesarean section. Women should be informed that elective cesarean section cannot prevent PFDs.
References
Nygaard I, Barber MD, Burgio KL, Kenton K, Meikle S, Schaffer J, et al. Prevalence of symptomatic pelvic floor disorders in US women. JAMA. 2008;300:1311–1316.
Akhlaghi F. The prevalence of pelvic floor disorders in women that referred to the clinic of gynecology in Zeinab hospital, Mashhad, Iran, 2003. Iran J Obstet Gynecol Infertil. 2004;7(1):25–31.
Handa VL, Blomquist JL, Knoepp LR, Hoskey KA, McDermott KC, Muñoz A. Pelvic floor disorders 5–10 years after vaginal or cesarean childbirth. Obstet Gynecol. 2011;118:777–784.
Uustal FE, Wingren G, Kjolhede P. Factors associated with pelvic floor dysfunction with emphasis on urinary and fecal incontinence and genital prolapse: an epidemiological study. Acta Obstet Gynecol Scand. 2004;83:383–389.
Sung VW, Washington B, Raker CA. Costs of ambulatory care related to female pelvic floor disorders in the United States. Am J Obstet Gynecol. 2010;202(5):483.e1–483.e4.
Segedi LM, Ilić KP, Curcić A, Visnjevac N. Quality of life in women with pelvic floor dysfunction. Vojnosanit Pregl. 2011;68(11):940–947.
Jelovsek JE, Barber MD. Women seeking treatment for advanced pelvic organ prolapse have decreased body image and quality of life. Am J Obstet Gynecol. 2006;194(5):1455–1461.
Diez-Itza I, Arrue M, Ibañez L, Paredes J, Murgiondo A, Sarasqueta C. Influence of mode of delivery on pelvic organ support 6 months postpartum. Gynecol Obstet Invest. 2011;72(2):123–129.
Murad-Regadas SM, Regadas FS, Rodrigues LV, Furtado DC, Gondim AC, Dealcanfreitas ID. Influence of age, mode of delivery and parity on the prevalence of posterior pelvic floor dysfunctions. Arq Gastroenterol. 2011;48(4):265–9.
Chen Y, Li F-Y, Lin X, Chen J, Chen C, Guess MK. The recovery of pelvic organ support during the first year postpartum. BJOG. 2013;120:1430–1437.
Direkvand-Moghadam A, Ghazanfari Z, Montazeri A, Delpisheh A, Direkvand-Moghadam A. Risk factors of pelvic organ prolapse in Iranian women: a cross-sectional study. Int J Epidemiol Res. 2014;1(1):29–34.
Azami-Aghdash S, Ghojazadeh M, Dehdilani N, Mohammadi M, Asl Amin Abad R. Prevalence and causes of cesarean section in Iran: systematic review and meta-analysis. Iran J Public Health. 2014;43(5):545–555.
Faisal I, Matinnia N, Hejar AR, Khodakarami Z. Why do primigravidae request caesarean section in a normal pregnancy? A qualitative study in Iran. Midwifery. 2014;30(2):227–233. doi:10.1016/j.midw.2013.08.011.
Baytur YB, Deveci A, Uyar Y, Ozcakir HT, Kizilkaya S, Caglar H. Mode of delivery and pelvic floor muscle strength and sexual function after childbirth. Int J Gynaecol Obstet. 2005;88:276–280.
World Health Organization. Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. WHO Technical Report Series 854. Geneva: World Health Organization; 1995.
Rahmani N, Mohseni-Bandpei MA. Application of perineometer in the assessment of pelvic floor muscle strength and endurance: a reliability study. J Bodyw Mov Ther. 2011;15(2):209–214.
Signorello LB, Harlow BL, Chekos AK, Repke JT. Midline episiotomy and anal incontinence: retrospective cohort study. BMJ. 2000;320(7227):86–90.
Sartore A, De Seta F, Maso G, Pregazzi R, Grimaldi E, Guaschino S. The effects of mediolateral episiotomy on pelvic floor function after vaginal delivery. Obstet Gynecol. 2004;103(4):669–673.
DeLancey JO, Kearney R, Chou Q, Speights S, Binno S. The appearance of levator ani muscle abnormalities in magnetic resonance images after vaginal delivery. Obstet Gynecol. 2003;101(1):46–53.
Rortveit G, Daltveit AK, Hannestad YS. Urinary incontinence after vaginal delivery or cesarean section. N Engl J Med. 2003;348:900–907.
Rørtveit G, Hannestad YS. Association between mode of delivery and pelvic floor dysfunction. Tidsskr Nor Legeforen. 2014;134:1848–1852.
Batista EM, Conde DM, Do Amaral WN, Martinez EZ. Comparison of pelvic floor muscle strength between women undergoing vaginal delivery, cesarean section, and nulliparae using a perineometer and digital palpation. Gynecol Endocrinol. 2011;27(11):910–914.
Gameiro MO, Sousa VO, Gameiro LF, Muchailh RC, Padovani CR, Amaro JL. Comparison of pelvic floor muscle strength evaluations in nulliparous and primiparous women: a prospective study. Clinics (Sao Paulo). 2011;66(8):1389–1393.
Petricelli CD, Resende AP, Elito Júnior J, Araujo Júnior E, Alexandre SM, Zanetti MR, et al. Distensibility and strength of the pelvic floor muscles of women in the third trimester of pregnancy. Biomed Res Int. 2014;2014, 437867.
Rasouli M, Keramat A, Khosravi A, Mohabatpour Z. Prevalence and factors associated with episiotomy in Shahroud City, northeast of Iran. Int J Womens Health Reprod Sci. 2016;4(3):125–129.
Acknowledgements
This study formed part of the Master’s thesis of F.D. All funding for this research were provided by Ahvaz Jundishapur University of Medical Sciences. We thank all the women who participated in the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Afshari, P., Dabagh, F., Iravani, M. et al. Comparison of pelvic floor muscle strength in nulliparous women and those with normal vaginal delivery and cesarean section. Int Urogynecol J 28, 1171–1175 (2017). https://doi.org/10.1007/s00192-016-3239-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-016-3239-6