Abstract
Introduction and hypothesis
Recurrent urinary tract infections (rUTIs) are commonly encountered in postmenopausal women. Optimal non-antimicrobial prophylaxis for rUTIs is an important health issue. The aim of this study was to evaluate the use of estrogen in the prevention of rUTIs versus placebo.
Methods
Eligible studies published up to December 2019 were retrieved through searches of MEDLINE, Embase, and Cochrane Central Register of Controlled Trials and Database of Systematic Reviews. We included randomized controlled trials of estrogen therapies versus placebo regarding the outcomes of preventing rUTIs. Changes in vaginal pH and estrogen-associated adverse events were also analyzed.
Results
Eight studies including 4702 patients (2367 who received estrogen and 2335 who received placebo) were identified. Five studies including 1936 patients evaluated the use of vaginal estrogen, which resulted in a significant reduction in rUTIs (relative risk, 0.42; 95% CI, 0.30–0.59). Three studies including 2766 patients evaluated the outcomes of oral estrogen in the prevention of UTIs and showed no significant difference in the number of rUTIs compared to treatment with placebo (relative risk, 1.11; 95% CI, 0.92–1.35). Two studies reviewed changes in vaginal pH and showed a lower pH (mean difference, −1.81; 95% CI, −3.10−−0.52) after vaginal estrogen therapy. Adverse events associated with vaginal estrogen were reported, including vaginal discomfort, irritation, burning, and itching. There was no significance increase in the vaginal estrogen group (relative risk, 3.06; 95% CI, 0.79–11.90).
Conclusions
Compared with placebo, vaginal estrogen treatment could reduce the number of rUTIs and lower the vaginal pH in postmenopausal women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urinary tract infections (UTIs) are common in women, and appropriate antibiotics are the mainstay of treatment of acute infections. Recurrent UTIs (rUTIs) are defined as at least two episodes of UTIs within 6 months or three episodes within 1 year [1]. It is an important health issue for women after menopause. Continuous long-term low-dose antibiotic treatment has been reported to be an effective management strategy to prevent rUTIs; however, it can lead to an increase in drug-resistance rates to the causative microorganisms, thereby leading to another health problem [2]. As a result, the use of optimal non-antimicrobial prophylaxis for rUTIs has become increasingly important. The proposed non-antimicrobial treatments include estrogen, probiotics, and vitamins. However, evidence-based data on the use of these prophylaxis treatments are still required.
The prevalence of UTIs increases with age in women [3,4,5], and 10–15% of women > 60 years old have been reported to have rUTIs [3, 4] compared to > 20% of those > 65 years and 25–50% of those > 80 years old [5]. An important pathogenesis of rUTIs in these women is hormonal deficiency [2,3,4,5,6]. Estrogen deficiency inhibits the growth of vaginal Lactobacillus flora, which can maintain vaginal pH and prevent colonization by uropathogens such as Escherichia coli [7]. The presence of such uropathogens increases the risk of infection. A few randomized controlled trials have evaluated the efficacy of using estrogen to prevent rUTIs, and they have reported the significant efficacy of local estrogen applications compared to systemic estrogen [2,3,4,5,6,7]. A Cochrane systematic review by Perrotta in 2008 reported that vaginal estrogen treatment could reduce the number of rUTIs in postmenopausal women [7]. However, this finding was based on only two randomized controlled studies [3, 4], and their study was published > 10 years ago. In addition, the methods of estrogen application in the two studies were different, using either vaginal cream or ring. Therefore, the aim of this review was to evaluate current data and evidence to elucidate the efficacy of estrogen treatment as non-antimicrobial prophylaxis for rUTIs in postmenopausal women. Vaginal pH and hormone-associated adverse events were also analyzed to evaluate the safety of the treatment.
Materials and methods
We performed a detailed computerized data search in December 2019 of MEDLINE (1950–2019), EMBASE (1980–2019), and the Cochrane Central Register of Controlled Trials and Database of Systematic Reviews (1991–2019). The search strategy was to use combinations of search terms related to population, intervention, comparison, and outcome as follows: “postmenopausal or menopausal,” “recurrent urinary tract infection,” “urinary tract infection,” “dysuria,” “lower urinary tract symptoms,” “vaginal or systemic,” “estrogen or hormonal therapy,” “side effects,” and “prophylaxis”. The search was limited to human studies. We selected randomized controlled studies that reported on the effectiveness of preventing rUTIs after estrogen treatment versus placebo in postmenopausal women with a minimum of 12 weeks of follow-up. Studies including patients who received different estrogen applications (e.g., vaginal estrogen ring, pessary, tablets, cream, or oral estrogen) compared with placebo were included. Studies which were not in English, those that did not meet the criteria for rUTIs, and those in which the patients received antimicrobial treatments or other non-antimicrobial agents were excluded from the review. Data related to vaginal condition including vaginal pH and hormone-associated adverse events were also retrieved and analyzed.
Data were extracted from each study by two reviewers and confirmed by another reviewer. We assessed the risk of bias of studies using domain-based evaluations, which were produced by The Cochrane Collaboration in 2011 [8]. The risk of bias included generation of the allocation sequence, concealment of the allocation sequence, blinding, incomplete outcome data, selective outcome reporting, and other biases. The risk of bias was rated as “low,” “high,” or “unclear.” In addition, the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) methodology was used to rate the quality of evidence [9]. Meta-analysis was used to estimate the risk ratio (RR) (for binary outcomes) or net change (for continuous outcomes) using RevMan Review Manager Version 5.0 [RevMan Review Manager (RevMan) computer program, version 5.0. 2008. Copenhagen, The Nordic Cochrane Centre, The Cochrane Collaboration].
Results
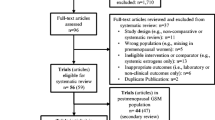
We identified 571 publications that evaluated the effect of estrogen preparations versus placebo for the prevention of rUTIs in postmenopausal women. The cited references in the primary articles or specialist reviews and publications were also searched. After removing duplicates, 227 publications were reviewed with regard to the inclusion and exclusion criteria. The flow diagram of the literature search and inclusion and exclusion criteria is shown in Fig. 1. A total of 188 articles were excluded, and 9 randomized controlled trials were eligible for initial assessment. Of these, one compared vaginal estrogen rings with antimicrobial agents and one included postmenopausal females who had already received oral hormone therapy before being randomized into the trial, and they were thus excluded from this review. The remaining eight articles were analyzed to assess the efficacy of estrogen as non-antimicrobial prophylaxis for rUTIs compared with placebo. Table 1 shows the characteristics of the studies included in the review. We reviewed the outcomes of different hormonal applications and compared vaginal and oral estrogen preparations versus placebo.
Vaginal estrogen
The use of vaginal estrogen was evaluated in five trials involving 324 patients. Two studies used vaginal estradiol silicone rings and conjugated estrogen cream [4, 5], and three used estriol in vaginal inserts (cream, ovules) [3, 10, 11]. Four studies evaluated the reduction or recurrence of new episodes of UTIs as the treatment outcome, whereas one trial assessed the occurrence of bacteriuria. All preparations of vaginal estrogen decreased the number of UTIs compared with placebo or compared to baseline conditions (number of UTIs before starting the trial or baseline bacteriuria) (relative risk, 0.42; 95% confidence interval, 0.30–0.59) (Fig. 2).
Oral estrogen
Three studies evaluated the outcomes of oral estrogen in the prevention of UTIs, including a total of 2766 patients [6, 12, 13]. Two studies used the same type of estriol but in different doses (3 mg daily for the duration of the study or 3 mg daily for 4 weeks and then 1 mg daily for the duration of the study), and another used oral tablets containing both conjugated estrogens (0.625 mg) and medroxyprogesterone acetate [12]. None of the studies showed a significant reduction in the episodes of UTIs compared with placebo (relative risk, 1.11; 95% confidence interval, 0.92–1.35) (Fig. 3). One study reported no improvements in UTI rate in the first 4 weeks but significant improvements at 12 weeks [13], and two studies reported no improvements after systemic estrogen therapy [6, 12].
Vaginal pH
Two studies were reviewed for the change in vaginal pH [3, 11], one of which used vaginal ovules and the other used vaginal cream. Estrogen showed significant efficacy in decreasing vaginal pH (mean difference, −1.81; 95% confidence interval, −3.10––0.52) (Fig. 4).
Adverse events
The adverse events associated with vaginal estrogen therapy included vaginal discomfort, irritation, burning, and itching. Compared with placebo, there was no significance increase in adverse events (relative risk, 3.06; 95% confidence interval, 0.79–11.90) (Fig. 5). The adverse effects in the oral systemic estrogen group varied widely, so they were difficult to evaluate [6, 12, 13]. One study reported no adverse events related to hormone therapy [13], and one study reported that oral estrogen increased the risks of diabetes, vaginal symptoms, and urge incontinence [12]. Another study reported that three (8.3%) patients had vaginal bleeding and seven (19.4%) had breast pain in the oral estrogen group compared to one (2.8%) with vaginal bleeding and one (2.8%) with breast pain in the placebo group [6].
Risk of bias and GRADE quality of evidence evaluation
The risks of bias assessments for each study are summarized and presented graphically in Figs. 6 and 7. There was a high risk of bias in 50% (4/8) of the trials due to incomplete outcome data. Other biases included blinding of outcome assessment (2/8, 25%), and blinding of the participants (1/8, 12.5%). The GRADE quality of evidence evaluation is summarized in Table 2.
Discussion
The results showed that vaginal estrogen could reduce the number of rUTIs in postmenopausal women compared with placebo (five studies, 1936 women: RR 0.42; 95% CI, 0.30–0.59), but that oral estrogen did not (three studies, 2766 women: RR 1.11; 95% CI, 0.92–1.35). Vaginal estrogen treatment significantly lowered vaginal pH (two studies, 211 women: mean difference, −1.81; 95% CI, −3.10––0.52) and was not associated with adverse events, including vaginal discomfort, irritation, burning, or itching (four studies, 324 women: RR 3.06; 95% CI, 0.79–11.90).
Several physiologic changes increase the risk of rUTIs in postmenopausal women, one of which is urogenital atrophy. Thinning of the vaginal or urethral mucosa and relaxation of pelvic floor muscles may cause the development of urinary or fecal incontinence and pelvic organ prolapse. These pelvic floor disorders can then cause an increase in post-voiding residual urine volume and incontinence causing poor hygiene, which are predisposing factors for UTIs. Another physiologic change is the change in vaginal microflora. Estrogen deficiency is not beneficial to lactobacilli-dominated vaginal microflora, which can maintain vaginal pH and prevent colonization by uropathogens [14]. In a prospective study, Meister et al. enrolled 70 postmenopausal women to evaluate changes in the urine inflammatory profile after vaginal estrogen therapy, and they proposed that hormone treatment could help to prevent rUTIs and reduce the symptoms of infection [15]. They also reported that vaginal estrogen could reduce levels of urine interleukin 6 and reduce urine inflammatory scores, indicating the genitourinary inflammatory response and suppression of associated symptoms with local estrogen treatment [15].
Although vaginal estrogen treatment appears to be a promising choice for postmenopausal women, there are concerns over the efficacy and safety of its long-term use. Because estradiol absorption is dose dependent and may be influenced by the delivery system, various formulations and positioning in the vagina have been suggested [16]. A Cochrane systematic review reported that vaginal estrogen cream may be associated with an increase in endometrial thickness compared to estrogen rings because of the higher doses of cream used [7]. Besides endometrial thickness, other estrogen-associated adverse events included breast tenderness, vaginal bleeding or spotting, non-physiologic discharge, vaginal irritation, burning, and itching [7]. Currently, the recommendations for local estrogen dosage and administration for vulvovaginal atrophy are to avoid a significant increase in serum estradiol [17]. The preparations of vaginal estrogen therapy can be classified as low-, intermediate-, and high-dosage preparations [18]. Low-dose vaginal estrogen is defined as around 7.5 μg for vaginal rings and 10 μg for tablets. Long-term low-dose vaginal estrogen administration has been reported to possibly increase plasma estradiol levels, but not above the normal range of ≤ 20 pg/ml [18], suggesting that low-dose estrogen therapy does not increase the rate of adverse events associated with systemic hormone therapy. An intermediate dose is defined as 25 μg estradiol or 0.3 mg conjugated equine estrogen, and a high dose is defined as 50–2000 μg estradiol or 0.625–2.5 mg conjugated equine estrogen. These doses may result in plasma estradiol levels approaching or exceeding 20 pg/ml [18]. In our review, all vaginal estrogen preparations used higher doses; however, no serious adverse events were reported. Although the meta-analysis revealed non-significant side effects, the longest use of vaginal estrogen therapy was only 36 weeks [4]. Therefore, further studies regarding the safety of long-term vaginal estrogen preparations are warranted. In addition, further studies to evaluate the efficacy of low-dose vaginal estrogen for preventing rUTIs are also warranted, because low-dose regimens may be preferred clinically to high-dose regimens in women, particularly for those who are concerned about the side effects of chronic estrogen therapy.
Although none of the studies reported direct outcomes with regard to the growth of lactobacilli flora, the meta-analysis showed that vaginal estrogen could lower vaginal pH in postmenopausal women. It is worth noting that vaginal estradiol absorption is acute with peaks at about 8 h that return to baseline at 12 h [19], indicating that the absorption of estradiol decreases shortly after the start of treatment. This means that vaginal mucosa and acidity may recover from an atrophic state if treatment with estrogen preparations is not continued. In this review, we included one study that used oral conjugated estrogens and medroxyprogesterone acetate; however, there were still insufficient data to compare their use with progestins for rUTIs in postmenopausal women. In addition to estrogen receptors, progesterone receptors are expressed in the bladder, trigone, and vagina, but their role is still not clear [18].
There are several limitations to this review. We limited the searches to English language, which may have missed potentially relevant studies. In addition, the number of patients, vaginal estrogen applications, and follow-up periods varied between the studies. Most of the studies had a limited follow-up period of ≤ 6 months, so the long-term outcomes were unclear. One study involved the use of oral conjugated estrogens and medroxyprogesterone acetate. Although there were insufficient data to evaluate the relationship between progestin and rUTIs, this combination of hormone therapy may have caused bias. We also acknowledge that some bias was unavoidable when performing the meta-analysis, especially with regard to the variations in intra-vaginal estrogen methods and formulations. There were too many inherent variables related to individual characteristics, patients’ compliance, application skill, and different delivery systems. For example, an estrogen-containing vaginal pessary inside the vagina can provide a steady and continuous delivery of estrogen, unlike vaginal estrogen cream which requires regular use to achieve an optimal functional estrogenization effect. Therefore, the results should be interpreted with caution because of potential bias.
There are also several strengths to this review. All of the recruited studies had similar characteristics, and all of the patients were postmenopausal and were diagnosed with rUTIs. To the best of our knowledge, this is the most complete, up-to-date, and relevant review regarding the efficacy of using systemic or local estrogen versus placebo in the prevention of rUTIs. Vaginal estrogen therapy may be an effective prophylaxis for rUTIs in postmenopausal women. Nevertheless, further studies are needed to survey the long-term effectiveness and safety of vaginal estrogen preparations and the lowest efficacious dosage as prophylaxis for rUTIs.
Abbreviations
- UTI:
-
urinary tract infection
- rUTI:
-
recurrent UTI
References
Raz R, Colodner R, Rohana Y, et al. Effectiveness of estriol-containing vaginal pessaries and nitrofurantoin macrocrystal therapy in the prevention of recurrent urinary tract infection in postmenopausal women. Clin Infect Dis. 2003;36:1362–8.
Wawrysiuk S, Naber K, Rechberger T, Miotla P. Prevention and treatment of uncomplicated lower urinary tract infections in the era of increasing antimicrobial resistance-non-antibiotic approaches: a systemic review. Arch Gynecol Obstet. 2019;300:821–8.
Raz R, Stamm WE. A controlled trial of intravaginal estriol in postmenopausal women with recurrent urinary tract infections. N Engl J Med. 1993;329:753–7.
Eriksen B. A randomized, open, parallel-group study on the preventive effect of an estradiol-releasing vaginal ring (Estring) on recurrent urinary tract infections in postmenopausal women. Am J Obstet Gynecol. 1999;180:1072–9.
Ferrante KL, Wasenda EJ, Jung CE et al (2019) Vaginal estrogen for the prevention of recurrent urinary tract infection in postmenopausal women: a randomized clinical trial. Female Pelvic Med Reconstr Surg.
Cardozo L, Benness C, Abbott D. Low dose oestrogen prophylaxis for recurrent urinary tract infections in elderly women. Br J Obstet Gynaecol. 1998;105:403–7.
Perrotta C, Aznar M, Mejia R, Albert X, Ng CW. Oestrogens for preventing recurrent urinary tract infection in postmenopausal women. Cochrane Database Syst Rev. 2008;2:CD005131.
Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. Br Med J. 2011;343:d5928.
Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64:383–94.
Simunić V, Banović I, Ciglar S, et al. Local Estrogen treatment in patients with urogenital symptoms. Int J Gynaecol Obstet. 2003;82:187–97.
Dessole S, Rubattu G, Ambrosini G, et al. Efficacy of low-dose intravaginal estriol on urogenital aging in postmenopausal women. Menopause. 2004;11:49–56.
Brown JS, Vittinghoff E, Kanaya AM. Urinary tract infections in postmenopausal women: effect of hormone therapy and risk factors. Obstet Gynecol. 2001;98:1045–52.
Kirkengen AL, Andersen P, Gjersøe E, Johannessen GR, Johnsen N, Bodd E. Oestriol in the prophylactic treatment of recurrent urinary tract infections in postmenopausal women. Scand J Prim Health Care. 1992;10:139–42.
Lüthje P, Hirschberg AL, Brauner A. Estrogenic action on innate defense mechanisms in the urinary tract. Maturitas. 2014;77:32–6.
Meister MR, Wang C, Lowder JL, Mysorekar IU (2019) Vaginal estrogen therapy is associated with decreased inflammatory response in postmenopausal women with recurrent urinary tract infections. Female Pelvic Med Reconstr Surg.
Santen RJ, Mirkin S, Bernick B, Constantine GD. Systemic estradiol levels with low-dose vaginal estrogens. Menopause. 2019;27:361–70.
Simon JA, Maamari RV. Ultra-low-dose vaginal estrogen tablets for the treatment of postmenopausal vaginal atrophy. Climacteric. 2013;16:37–43.
Dudley R, Philip TH, Linda C. The effect of hormones on the lower urinary tract. Menopause Int. 2013;19:155–62.
Santen RJ. Vaginal administration of estradiol: effects of dose, preparation and timing on plasma estradiol levels. Climacteric. 2015;18:121–34.
Author information
Authors and Affiliations
Contributions
Ying-Yu Chen: Protocol/project development, Data Collection and management, Data Analysis, Manuscript writing.
TH Su: Protocol/project development, Data collection and management.
HH Lau: Protocol/project development, Manuscript writing and editing.
Corresponding author
Ethics declarations
Financial disclaimer/conflict of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, YY., Su, TH. & Lau, HH. Estrogen for the prevention of recurrent urinary tract infections in postmenopausal women: a meta-analysis of randomized controlled trials. Int Urogynecol J 32, 17–25 (2021). https://doi.org/10.1007/s00192-020-04397-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04397-z