Abstract
Introduction and hypothesis
Stress urinary incontinence (SUI) is treated using intravaginal laser therapy. We wanted to find out how incontinence severity at baseline and the number of laser interventions affect success rate, and whether the effect of laser therapy was obvious 6 months and 2 years after the last laser intervention.
Methods
Fifty-nine women, 32 with SUI I, 16 with SUI II, and 11 with SUI III were treated using an erbium-doped yttrium aluminium garnet (Er:YAG) laser following the IncontiLase® protocol. Therapy included five laser sessions with a 1-month interval between sessions. Objective (1-h pad test) and subjective data (International Consultation on Incontinence Questionnaire-Urinary Incontinence Short Form [ICIQ-UI SF], Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire [PISQ-12]) were assessed at baseline, after two and four laser sessions and 6 months and 2 years after the fifth laser session.
Results
Objective cure/improve rates for mild SUI I were 69%, 78%, 91%, and 78% after two, four, and five laser sessions at the 6-month and 2-year follow-ups. Subjective cure rates (ICIQ-UI SF) were 53%, 69%, 72%, and 66%, and sexual function (PISQ-12) also improved. For SUI II, objective cure/improve rates were 31%, 63%, 69%, and 50%. Subjective cure rate was 13% at the 2-year follow-up. For SUI III, only one patient had an objective improvement after two and four laser sessions.
Conclusions
Intravaginal laser therapy led to cure/improvement for SUI I and SUI II, but not for severe SUI III. Outcome was better after four to five laser sessions than after two laser sessions. Follow-up data 6 months and 2 years after laser intervention showed sustainability of the treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anatomical causes of stress urinary incontinence (SUI) are insufficient support of urethra and bladder or impairment of the urethral sphincter and a reduction of the urethral closure pressure [1]. Causes of insufficient urethral support may be a loss of pelvic muscle strength due to damage of pelvic floor innervation after vaginal delivery, alteration of the mucosa due to the menopausal decrease of estrogen, or altered composition of the connective tissue and supporting ligaments due to decreased and insufficient collagen production [2].
Stress urinary incontinence should initially be treated by nonsurgical management, such as weight reduction, hormonal substitution, physiotherapy, pelvic floor exercise or the use of pessaries [3]. If these treatments do not lead to an improvement within 3–6 months, an operative intervention is indicated. For the past two decades, tension-free suburethral slings (TVT) were the gold standard for the operative treatment of SUI [3]. Tape insertion is recommended for moderate to severe cases of SUI, preferentially for women after the childbearing age. The trans- or periurethral injection of bulking agents can be an alternative, less invasive treatment option, especially suited to elderly, multi-morbid patients [4], or for recurrent SUI after midurethral sling failure [5].
So far, however, there are limited treatment alternatives for younger, active women between pregnancies with disturbing incontinence, for example, during physical exercise. Can the new, minimally invasive intravaginal laser therapy be an option for this patient group?
Currently, three different laser modalities have been published for treating SUI: the microablative fractional carbon dioxide (CO2) laser therapy (10,600 nm) [6]; dual-phase erbium-doped yttrium aluminium garnet (Er:YAG) laser therapy (2,940 nm) combining fractional cold ablation and thermal ablation [7]; and non-ablative Er:YAG laser therapy (2,940 nm) with SMOOTH mode technology [8, 9]. In all three cases, laser therapy induces neocollagenesis, thickens and strengthens the anterior vaginal wall, which leads to improved support of the bladder and urethra, and consequently, to continence [6, 10].
Randomized controlled trials directly comparing the three laser treatments for SUI have not been published. The fractional CO2 laser penetrates the vaginal epithelium to a depth of approximately 600 μm. Ablation leads to coagulation and tissue necrosis and a wound healing response with fibroblast stimulation and neocollagenesis [6, 11]. This process is accompanied by pain and a recovery phase of up to 20 days [11]. Dual-phase Er:YAG laser therapy is more gentle and less invasive. The cold fractional ablative mode creates small canals in the superficial layer of the vaginal epithelium, leaving intact tissue capable of regeneration in between, while the subsequent thermal mode reaches the lamina propria of the vaginal epithelium, irritates collagen fibers, and stimulates neocollagenesis. This thermal tissue effect leads to a controlled layer-by-layer ablation with rapid wound healing, without coagulation and tissue necrosis [7].
Most studies on laser treatment of SUI applied the non-ablative SMOOTH mode technology of the Er:YAG laser [8, 12,13,14,15]. Special software settings make this treatment even less invasive. By absorption in the tissue, the laser beam is transformed to heat, but leaves the vaginal epithelium intact. Seven long consecutive SMOOTH mode pulses of 250 ms, each consisting of six micropulses with a non-ablative fluence, “pump” this heat away from the skin surface to a depth of 500 μm [9]. Temperatures of 60 °C in the tissue supporting the urethra [8] lead to heat-induced denaturation of dermal collagen, and consequently, to collagen remodeling and new collagen formation [16]. Histologically, an increase in the epithelial thickness, a higher number of capillaries, and increased volume density of the capillaries were also observed [10].
Studies on laser therapy for SUI mostly reported successful outcomes. However, individual study results, even when applying the SMOOTH mode technology, cannot be compared owing to different laser settings, different numbers of treatment sessions, different patient inclusion and exclusion criteria, and different definition of success [17]. Only one randomized controlled trial is available showing subjective superiority of the non-ablative laser over sham treatment at the 3-month follow-up [15]. Published data were often limited by a statistical bias, methodological flaws, and lack of a control group or comparison with other clinically proven treatment modalities [17]. Further limitations are small patient numbers, the absence of dose finding by empirically using one or two successive laser sessions, only a subjective therapy outcome, short follow-up observation periods between 1 month and a maximum of 12 months, or no consideration of initial incontinence severity grades. Therefore, international experts unanimously agree that more trials are necessary [17,18,19,20].
In this study, we focused on dose finding and a longer follow-up period of Er:YAG therapy with SMOOTH mode technology by comparing outcomes after two, four, and five laser sessions and by following therapy outcome for up to 2 years. We wanted to evaluate both subjective and objective outcomes and to find out how incontinence severity at baseline affects success rate. Stringent criteria, similar to those of previous studies on sling insertions, were used to rate therapy success [21].
Materials and methods
Fifty-nine women were included at a tertiary urogynecological center. The study was approved by the local ethics committee and patients gave written informed consent. Women needed to be 18 years or older, with a clinical and urodynamic diagnosis of SUI or mixed urinary incontinence (MUI) with predominant SUI. Diagnosis was based on a standardized stress provocation test (cough test) supine and in a standing position with a full bladder (300 ml) [5] and a pad weight of ≥5 g in a 1-h test under standardized conditions [22]. Urodynamic assessment was done using a Duet Logic (Medtronic, Düsseldorf, Germany) with a microtip catheter [23]. Physiotherapy was recommended prior to laser intervention and was not allowed during the study. Women with vaginal atrophy received local estrogens for ≥ 3 months before study initiation. Starting with local or systemic estrogen treatment < 3 months before or during the study was not allowed. Exclusion criteria were a pre-existing bladder condition, including radiation treatment, pregnancy or delivery < 6 months before study initiation, a body mass index (BMI) > 35, radical pelvic surgery, urinary tract infection or other active infections of the urinary tract or bladder, pelvic organ prolapse stage > II, diagnosis of predominant urge incontinence, diagnosis of collagen disorders, and incomplete bladder emptying. Patient characteristics, parity and delivery mode, previous operations, grade of prolapse, and presence of intrinsic sphincter deficiency (ISD), defined as the urodynamic maximal urethral closure pressure of ≤ 20 cm H2O [23], were evaluated at baseline. Severity of SUI was graded by Stamey’s incontinence scoring system, i.e., SUI 0 = no incontinence, SUI I = incontinence with coughing or straining, SUI II = incontinence with change in position or walking, SUI III = total incontinence at all times [24].
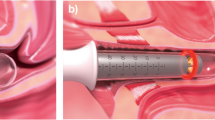
Patients were treated using an Er:YAG laser (FotonaSmooth XS®; 2,940 nm; Fotona, Ljubljana, Slovenia) in the SMOOTH mode following the IncontiLase protocol [25]. If requested, a lidocaine/prilocaine combination cream (Emla®) was applied. The IncontiLase protocol included three steps:
-
1.
Intravaginal laser pulses with a directed angular, patterned laser beam (PS03-GAc, 7 mm, 6 J/cm2, 1.6 Hz, seven pulses, six passes)
-
2.
Intravaginal laser pulses with a circular full laser beam (R11-GCc, 7 mm, 3 J/cm2, 1.6 Hz, seven pulses, two passes)
-
3.
Laser pulses of vestibule and introitus with a straight, patterned laser (PS03, 7 mm, 10 J/cm2, 1.6 Hz, two to three pulses, two to three passes)
All patients received five laser sessions, one at baseline, and one after 1, 2, 3, and 4 months.
Objective (1-h pad test) [22] and subjective International Consultation on Incontinence Questionnaire-Urinary Incontinence Short Form (ICIQ-UI SF) [26] and Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12) [27, 28] data and complications were assessed at baseline, 1 month after the second and the fourth laser session, and 6 months and 2 years after the fifth laser session, i.e., at 0, 2, 4, 10, and 28 months after baseline (Fig. 1). ICIQ-UI SF evaluates subjective incontinence symptoms and quality of life (sum scores: 0 = no problems to 21 = severe problems) and PISQ-12 assesses 12 subjective symptoms of pelvic organ prolapse, urinary incontinence, and sexual function (score: 0 = severe problems to 48 = no problems or maximum satisfaction). Patients were classed as “cured” based on ≤ 2 g of urine on the 1-h pad test [21] or an ICIQ-UI SF score ≤ 5 [26]. Patients were classed as “improved” when having a 1-h pad weight reduction > 50%, and classed as “not cured” when having a pad weight reduction ≤ 50% [13] or an ICIQ-UI SF score > 5 [26].
Descriptive statistics were used for baseline characteristics, outcome variables and complication rates. Differences among SUI grades were tested using the F-test for normally distributed continuous variables, with the Kruskal–Wallis test for non-normally distributed continuous variables, with Poisson regression for count data and with Fisher’s test for categorical variables. Results were considered to be significant at a level of α < 0.05. Statistical analysis and graphic representations of the data were generated using R 3.2.2 for Windows 7.
Results
At the time of inclusion, 32 patients had SUI I (54%), 16 had SUI II (27%), and 11 had SUI III (19%). Patient characteristics shown in Table 1. At baseline, significant differences between groups were only found for BMI and ISD, both being highest in SUI III (Table 1). A BMI ≥ 30 was found for 5 out of 11 SUI III, 2 out of 16 SUI II, and 1 out of 32 SUI I patients. Patients only had prolapse stages I and II and presence of prolapse was not significantly different between incontinence groups. One-hour pad weights and ICIQ-UI SF and PISQ-12 scores were significantly different between SUI groups. Only 1 patient with SUI III had undergone previous incontinence surgery with a sling (Table 1).
For SUI I, objective cured/improved rates were 69% (22 out of 32), 78% (25 out of 32), 91% (29 out of 32) or 78% (25 out of 32) 1 month after the second, 1 month after the fourth, or 6 months and 2 years after the fifth laser session respectively (Fig. 2). For SUI II, cured/improved rates were 31% (5 out of 16), 63% (10 out of 16), 69% (11 out of 16), and 50% (8 out of 16), and for SUI III, cured/improved rates were 9% (1 out of 11), 9% (1 out of 11), 0% (0 out of 11), and 0% (0 out of 7) at the same time points (Fig. 2). For SUI I, median urine loss decreased from 7 g to 3 g after two laser sessions, and remained at 2 g after four or five laser sessions (Table 2). Similarly, for SUI II, the strongest decrease was found after two laser sessions, but four or five laser sessions led to further improvement (Table 2). Outcome was equally positive 6 months or 2 years after laser intervention. The laser therapy only had a minor effect on SUI III (Table 2). The 4 SUI III patients with a pad weight ≥ 50 g, 3 of them with a BMI ≥ 30 and among them the patient with recurrent incontinence, dropped out after the 6-month follow-up visit, possibly because they opted for another incontinence therapy.
One-hour pad test. Objective cure rates (%) are shown for patients with initial stress urinary incontinence (SUI) I, SUI II or SUI III at the following time points: 1 month after two laser sessions (2 M), 1 month after four laser sessions (4 M), and 6 months and 2 years after the fifth laser session (10 M and 28 M). M month, green cured (pad weight ≤ 2 g), orange improved (pad weight reduction of > 50% compared with baseline), red not cured (pad weight reduction of ≤ 50% compared with baseline)
Objective outcome was not different in pre- and postmenopausal women for all SUI grades after the second or the fourth laser session, and 6 months after the fifth laser session. Only at the 2-year follow-up were results significantly better for premenopausal (89%, 17 out of 19 cured; 5%, 1 out of 19 improved; 5%, 1 out of 19 failed) versus postmenopausal (38%, 5 out of 13 cured; 15%, 2 out of 13 improved; 46%, 6 out of 13 failed) SUI I patients (p = 0.0053).
For SUI I, subjective cure rates (ICIQ-UI SF) were 53% (17 out of 32), 69% (22 out of 32), 72% (23 out of 32) or 66% (21 out of 32) 1 month after the second, 1 month after the fourth, or 6 months and 2 years after the fifth laser session respectively (Fig. 3). Thirteen percent of SUI II patients (2 out of 16) were cured at the 2-year follow-up. Other than that, subjective cure was not found for any SUI II or SUI III patients at any visit (Fig. 3). The median ICIQ-UI SF score improved after two laser sessions, from 10 to 5 for SUI I and from 15 to 10 for SUI II, and remained at this level even after four or five laser sessions (Table 3). Laser treatment did not affect the ICIQ-UI SF score of SUI III (Table 3).
International Consultation on Incontinence Questionnaire-Urinary Incontinence Short Form (ICIQ-UI SF) score. Subjective cure rates [%] are shown for patients with initial SUI I, SUI II or SUI III at the following time points: 1 month after two laser sessions (2 M), 1 month after four laser sessions (4 M) and 6 months and 2 years after the fifth laser session (10 M and 28 M). M month, green cured (ICIQ-UI SF ≤ 5), red not cured (ICIQ-UI SF > 5)
The PISQ-12 score improved from 20 at baseline to 31 at the 6-month follow-up visit for SUI I, from 14 to 24 for SUI II, and from 12 to 15 for SUI III (Table 4).
There were only minor complications of laser therapy. For most cases, topical anesthetic cream was not even necessary. Only 6 patients reported weak pain (11%, 6 out of 57) during or after laser therapy. The pain was transient and restricted to the first few days after laser application. One patient (1 out of 57; 2%) had vaginal discharge. Data were not available for 2 patients.
Discussion
Laser therapy has become increasingly popular, primarily in dermatology, cosmetics, and dentistry, but also in esthetic gynecology and urogynecology. In 2018, the US Food and Drug Administration (FDA) issued a warning that energy-based medical devices had not been cleared or approved to perform vaginal “rejuvenation,” cosmetic vaginal procedures, or nonsurgical vaginal procedures. Consequently, leading researchers in the field of urogynecology stated that the strict training of gynecology professionals and robust clinical trials are necessary to demonstrate the long-term complication profile, safety, and efficacy of nonsurgical and surgical lasers [18, 29].
In this study, we found very few and only minor and transient complications for treating SUI with the intravaginal Er:YAG laser therapy with SMOOTH mode technology. Objective therapy success depended on initial incontinence severity. At the 6-month post-laser visit, initial pad weights of 5–10 g had a cure rate of 67% (20 out of 30), an improvement rate of 27% (8 out of 30) and a failure rate of 7% (2 out of 30); 11–20 g urine loss resulted in 7% (1 out of 15) cure, 73% (11 out of 15) improvement and 20% (3 out of 15) failure; 21–86 g loss led to a failure rate of 100% (14 out of 14). Similarly, subjective success also depended on initial severity. An ICIQ-UI SF score of 6–10 at baseline resulted in 79% (19 out of 24) success and 21% (5 out of 24) failure; a score of 11–21 resulted in 11% (4/35) success and 89% (31/35) failure. Therefore, laser therapy should only be recommended for patients with a urine loss ≤ 20 g or an ICIQ-UI SF score ≤ 10. We could not confirm the results by Okui [14] that showed significant improvement for a mean 1-h pad weight of 34 g or a mean ICIQ-UI SF score of 12.
Laser treatment was sustainable for 2 years for premenopausal, but not for postmenopausal SUI I patients, possibly because of less vaginal atrophy in younger women. Similarly, Gambacciani et al. [30] showed that the laser effect lasted for 1, but not for 2 years in women with genitourinary syndrome of menopause. Laser treatment was also less successful for patients with a high BMI.
A strength of this trial is the evaluation of both objective and subjective outcomes. To investigate an association of objective and subjective improvement, we compared improvement in the pad test with the results of the ICIQ-UI SF question addressing the quality of life (“Overall, how much does leaking urine interfere with your everyday life?”). At the 6-month follow-up visit, only 10 of the 18 objectively improved patients (56%) also indicated subjective improvement (reduction of VAS score > 50% compared with baseline), whereas the therapy subjectively failed for the remaining 8 patients (reduction of VAS score ≤ 50% compared with baseline). The fact that objective outcome was better than subjective outcome may reflect that the laser therapy could not meet the patients’ very high expectations. Therefore, rational outcomes and expectations should be discussed before offering laser therapy for SUI.
Patients with mild to moderate SUI are good candidates for laser therapy. However, classification of SUI grades is defined by different criteria in the literature. According to the subjective criteria by Klovning et al. [26], none of our patients would fall into SUI category I, defined by an ICIQ-UI SF score of 1–5. Conversely, according to objective criteria by the International Continence Society [22], 8 of our SUI III patients (Stamey’s system [24]) would fall into SUI category II defined by a 1 h pad weight of 11–50 g. These discrepancies show the difficulty in choosing the right assessment criteria for successful laser therapy.
In this study, we made a dose finding and evaluated short- and midterm follow-up data (Figs. 2, 3). Two laser sessions showed a major cure/improvement, but success was even higher after four sessions, whereas outcome after five sessions was similar to that after four sessions. Therefore, three to four laser sessions at intervals of 1 month seem ideal for the most effective laser therapy. Outcomes at the 6-month and 2-year follow-up visits were similar, indicating that laser treatment is sustainable and does not need to be repeated within 2 years.
Limitations of this study are the relatively small case number, the lack of a placebo group, and no direct comparison with an alternative treatment group. However, two large European, randomized, single blinded, sham-controlled multicenter studies in which we are also participating are expected to overcome some of these limitations. A search on the ClinicalTrials.gov database revealed that even more data will be available in the future.
We recommend intravaginal laser therapy for younger women between childbirths with disturbing incontinence, for example, during sports activity. In addition, the therapy is minimally invasive, has few and only minor complications, and may be a valuable option for women who are afraid of incontinence surgery or who have had bad experience with a previous surgery. Further advantages of laser treatment are the absence of synthetic material and the ambulatory setting.
Mild to moderate SUI can successfully be treated using an Er:YAG laser with non-ablative SMOOTH mode technology. Three to four laser sessions at intervals of 1 month are ideal and the therapy is effective for up to 2 years post-treatment. Besides the incontinence severity grade, medical history, predisposition, and personal preferences also determine whether SUI should be treated using suburethral slings, bulking agents or laser therapy. According to this study, laser therapy is an ideal option for women between pregnancies who seek a fast, ambulatory, minimally invasive intervention free of synthetic material.
References
DeLancey JO, Trowbridge ER, Miller JM, Morgan DM, Guire K, Fenner DE, et al. Stress urinary incontinence: relative importance of urethral support and urethral closure pressure. J Urol. 2008;179:2286–90 discussion 90.
Fistonić I, Findri Guštek S, Fistonić N. Minimally invasive laser procedure for early stages of stress urinary incontinence (SUI). J Laser Health Academy. 2012;1:67–74.
Reisenauer C, Muche-Borowski C, Anthuber C, Finas D, Fink T, Gabriel B, et al. Interdisciplinary S2e guideline for the diagnosis and treatment of stress urinary incontinence in women: short version—AWMF registry no. 015-005, July 2013. Geburtshilfe Frauenheilkd. 2013;73:899–903.
Elmelund M, Sokol ER, Karram MM, Dmochowski R, Klarskov N. Patient characteristics that may influence the effect of urethral injection therapy for female stress urinary incontinence. J Urol. 2019;202:125–31.
Zivanovic I, Rautenberg O, Lobodasch K, von Bunau G, Walser C, Viereck V. Urethral bulking for recurrent stress urinary incontinence after midurethral sling failure. Neurourol Urodyn. 2017;36:722–6.
Gonzalez Isaza P, Jaguszewska K, Cardona JL, Lukaszuk M. Long-term effect of thermoablative fractional CO2 laser treatment as a novel approach to urinary incontinence management in women with genitourinary syndrome of menopause. Int Urogynecol J. 2018;29:211–5.
Mothes AR, Runnebaum M, Runnebaum IB. An innovative dual-phase protocol for pulsed ablative vaginal erbium:YAG laser treatment of urogynecological symptoms. Eur J Obstet Gynecol Reprod Biol. 2018;229:167–71.
Fistonić N, Fistonić I, Gustek SF, Turina IS, Marton I, Vizintin Z, et al. Minimally invasive, non-ablative Er:YAG laser treatment of stress urinary incontinence in women—a pilot study. Lasers Med Sci. 2016;31:635–43.
Lukac M, Gaspar A, Bajd F. Dual tissue regeneration: non-ablative resurfacing of soft tissues with FotonaSmooth® mode Er:YAG laser. J Laser Health Academy. 2018;1:1–15.
Lapii GA, Yakovleva AY, Neimark AI. Structural reorganization of the vaginal mucosa in stress urinary incontinence under conditions of Er:YAG laser treatment. Bull Exp Biol Med. 2017;162:510–4.
Gambacciani M, Torelli MG, Martella L, Bracco GL, Casagrande AG, Albertin E, et al. Rationale and design for the vaginal erbium laser academy study (VELAS): an international multicenter observational study on genitourinary syndrome of menopause and stress urinary incontinence. Climacteric. 2015;18(Suppl 1):43–8.
Ogrinc UB, Sencar S, Lenasi H. Novel minimally invasive laser treatment of urinary incontinence in women. Lasers Surg Med. 2015;47:689–97.
Tien YW, Hsiao SM, Lee CN, Lin HH. Effects of laser procedure for female urodynamic stress incontinence on pad weight, urodynamics, and sexual function. Int Urogynecol J. 2017;28:469–76.
Okui N. Comparison between erbium-doped yttrium aluminum garnet laser therapy and sling procedures in the treatment of stress and mixed urinary incontinence. World J Urol. 2019;37:885–9.
Blaganje M, Scepanovic D, Zgur L, Verdenik I, Pajk F, Lukanovic A. Non-ablative Er:YAG laser therapy effect on stress urinary incontinence related to quality of life and sexual function: a randomized controlled trial. Eur J Obstet Gynecol Reprod Biol. 2018;224:153–8.
Drnovsek-Olup B, Beltram M, Pizem J. Repetitive Er:YAG laser irradiation of human skin: a histological evaluation. Lasers Surg Med. 2004;35:146–51.
Pergialiotis V, Prodromidou A, Perrea DN, Doumouchtsis SK. A systematic review on vaginal laser therapy for treating stress urinary incontinence: do we have enough evidence? Int Urogynecol J. 2017;28:1445–51.
Shobeiri SA, Kerkhof MH, Minassian VA, Bazi T, Research I, Development C. IUGA committee opinion: laser-based vaginal devices for treatment of stress urinary incontinence, genitourinary syndrome of menopause, and vaginal laxity. Int Urogynecol J. 2019;30:371–6.
Bhide AA, Khullar V, Swift S, Digesu GA. The use of laser in urogynaecology. Int Urogynecol J. 2019;30:683–92.
Gambacciani M, Palacios S. Laser therapy for the restoration of vaginal function. Maturitas. 2017;99:10–5.
Kociszewski J, Rautenberg O, Kuszka A, Eberhard J, Hilgers R, Viereck V. Can we place tension-free vaginal tape where it should be? The one-third rule. Ultrasound Obstet Gynecol. 2012;39:210–4.
Krhut J, Zachoval R, Smith PP, Rosier PF, Valansky L, Martan A, et al. Pad weight testing in the evaluation of urinary incontinence. Neurourol Urodyn. 2014;33:507–10.
Wlazlak E, Viereck V, Kociszewski J, Kuszka A, Rautenberg O, Walser C, et al. Role of intrinsic sphincter deficiency with and without urethral hypomobility on the outcome of tape insertion. Neurourol Urodyn. 2017;36:1910–6.
Ghoniem G, Stanford E, Kenton K, Achtari C, Goldberg R, Mascarenhas T, et al. Evaluation and outcome measures in the treatment of female urinary stress incontinence: International Urogynecological Association (IUGA) guidelines for research and clinical practice. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:5–33.
Vizintin Z, Rivera M, Fistonić I, Saraçoğlu F, Guimares P, Gaviria J, et al. Novel minimally invasive VSP Er:YAG laser treatments in gynecology. J Laser Health Academy. 2012;1:46–58.
Klovning A, Avery K, Sandvik H, Hunskaar S. Comparison of two questionnaires for assessing the severity of urinary incontinence: the ICIQ-UI SF versus the incontinence severity index. Neurourol Urodyn. 2009;28:411–5.
Rogers RG, Coates KW, Kammerer-Doak D, Khalsa S, Qualls C. A short form of the pelvic organ prolapse/urinary incontinence sexual questionnaire (PISQ-12). Int Urogynecol J. 2003;14:164–8 discussion 8.
Rogers RG, Coates KW, Kammerer-Doak D, Khalsa S, Qualls C. A short form of the pelvic organ prolapse/urinary incontinence sexual questionnaire (PISQ-12). Int Urogynecol J. 2004;15:219.
Escribano JJ, Gonzalez-Isaza P, Tserotas K, Athanasiou S, Zerbinati N, Leibaschoff G, et al. In response to the FDA warning about the use of photomedicine in gynecology. Lasers Med Sci. 2019;34:1509–11.
Gambacciani M, Levancini M, Russo E, Vacca L, Simoncini T, Cervigni M. Long-term effects of vaginal erbium laser in the treatment of genitourinary syndrome of menopause. Climacteric. 2018;21:148–52.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kuszka, A., Gamper, M., Walser, C. et al. Erbium:YAG laser treatment of female stress urinary incontinence: midterm data. Int Urogynecol J 31, 1859–1866 (2020). https://doi.org/10.1007/s00192-019-04148-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-019-04148-9