Abstract
Introduction and hypothesis
Urinary incontinence (UI) is prevalent among women, including young women (18–30 years old). This article aims to explore the prevalence of UI, as well as toileting behaviors and other factors that are associated with UI, in female college students in central China.
Methods
We used convenience sampling to recruit 1000 students from five institutions of higher education. We distributed pencil-and-paper questionnaires to obtain demographic, environmental, and general health information, including whether UI was present or not, and information regarding toileting behaviors used by the respondents.
Results
Most students, n = 929, responded to the questionnaire. Their ages ranged from 18 to 26 years old (average: 20.5 ± 1.6); 23.6% of these respondents reported UI, 52.7% often/always worried about public toilet cleanliness, and 25.3% often/always delayed emptying their bladder when they were busy. Respondents who were between 21 and 26 years old had a lower probability of UI (odds ratio [OR] = 0.867 and 95% confidence interval [CI] = 0.771–0.975) than younger respondents (18–21 years old). Respondents who reported constipation (OR = 2.395, 95% CI = 1.494–3.839), drank alcohol (OR = 1.763, 95% CI = 1.114–2.792), often/always delayed urination (OR = 1.738, 95% CI = 1.306–2.313), and/or often/always strained to urinate (OR = 1.433, 95% CI = 1.111–1.849) had greater odds of having UI than respondents who did not have constipation or engage in these behaviors.
Conclusions
UI is prevalent in young Chinese women who are attending college. These women should be asked and given culturally appropriate information about UI and associated factors that include toileting behaviors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urinary incontinence (UI) is the complaint of involuntary loss of urine [1], which is one of several lower urinary tract symptoms that affect millions of women and their quality of life. Although considered a condition of older woman, UI also affects young women. For example a recent study reports that young women (mean age 23.5 years) have 10.3% prevalence of UI [2]. Of the 193 female full-time college students in the USA (mean age 21.2 ± 0.46 years) who responded to a survey on bladder health and toileting behaviors, 17.9% reported UI episodes [3]; of those, 83.9% said that UI bothered them at least “a little bit.” Aoki et al. described the association of female UI with age, noting that UI prevalence increases with age [4]. Bladder pathology in adulthood may begin early in life and left under- or untreated may persist into later life [5]. Thus, the identification of protective factors and risk factors of UI during early life stages is important.
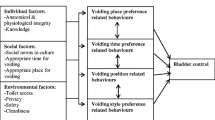
Toileting behaviors, which are related to urination and used by women across their life course, have received increased attention from researchers in recent years [6, 7]. For example, researchers have categorized toileting behaviors in terms of place/location, timing, and positions for voiding [8]. A recent study of employed women found an association between UI and toileting behaviors, specifically in regard to premature, delayed, or incomplete urination and straining to urinate [7]. Further research is needed to identify factors, especially modifiable ones, that are associated with UI in young women to facilitate the development of interventions that can prevent or mitigate UI while women are still young. Reducing UI incidence or delaying its onset in girls and young women may also help to reduce associated poor health conditions, costs, and negative impacts on quality of life [5].
A better understanding of the prevalence and associated factors of UI in young Chinese women is needed, especially given the large population of young women in China. For example, in 2010, 143 million women 18 to 30 years old were living in China [9]. The aim of this study is to explore the prevalence of UI in college-aged Chinese women and to identify toileting behaviors and other factors associated with UI in this population.
Methods
Study design and participants
From October to December 2017, the authors recruited a convenience sample of 1000 female students from five institutions of higher education in Xuzhou, Jiangsu Province, in east-central China. Trained research assistants went to classrooms, libraries, and dormitories and approached students to tell them about the study and to explain its aims and methods. Interested students were guaranteed confidentiality of their individual responses. Those students who verbally agreed to participate in our study were provided pencil-and-paper questionnaires and given space to complete them in a relaxed, quiet environment in a classroom, library, or dormitory.
The inclusion criteria were self-reports of: (1) being a full-time female college student, (2) being between 18 and 30 years of age, (3) willingness to participate voluntarily in the study, (4) not having taken diuretic medications in the past 3 months, and (5) not being pregnant at the time of the study. The exclusion criteria were self-reports of: (1) having a urinary tract infection in the past 4 weeks, (2) having been pregnant or given birth within the past 3 months, (3) having a chronic disease of the urinary system, (4) having a history of previous urologic operations, or (5) having a mental disorder.
Measurements
The questionnaire requested sociodemographic data that included age, race/ethnicity, health status, parents’ education and income, and health-related items developed by the authors. Terms used in the questionnaire included ‘constipation,’ defined as defecation less than three times a week and difficult passage of dry and hard stools [10]; ‘normal menstruation,’ defined as a menstrual cycle of 24 to 35 days; and ‘menstrual period,’ defined as lasting 2 to 7 days [11].
For this study, we used the Chinese version of the International Consultation on Incontinence Questionnaire-Female Lower Urinary Tract Symptoms (ICIQ-FLUTS) and the Toileting Behavior-Women’s Elimination Behaviors (TB-WEB) instrument [12]. The Cronbach’s alpha coefficient of the Chinese version of the ICIQ-FLUTS was 0.95. The agreement rate in the test-retest exceeded 95%, and kappa values were over 0.72 (p < 0.001) [13]. Women were considered to have UI if they responded with an answer other than ‘none’ to the item that queried the frequency of urine leakage [14]. The bother associated with UI was evaluated using a scale ranging from 0 (not bothered at all) to 10 (seriously bothered). Bother was also defined by dividing the Likert responses into three groups: minor (rated 1–4), moderate (rated 5–7), and severe (rated 8–10) [15].
The modified TB-WEB is a 22-item scale that consists of six domains: place preference for urination (4 items), premature urination (5 items), delayed urination (3 items), straining to urinate (4 items), emptying bladder completely (2 items), and position preference for urination (4 items). Each item is measured on a 5-point scale to assess how often women experienced each behavior (1 = never, 2 = rarely, 3 = sometimes, 4 = often, 5 = always). An ‘often’ or ‘always’ response is considered a habitual behavior [16]. Prior to this study, nurse researchers tested the reliability and validity of the original TB-WEB Chinese version; the total Cronbach’s alpha was 0.80. The Cronbach’s alpha value for each domain was > 0.70, and the reliability of each domain was > 0.60 [17].
The Institutional Review Board of Xuzhou Medical University approved this study. For students who met the eligibility criteria and verbally agreed to participate in the study, trained research assistants administered the questionnaire and remained nearby while the students completed it. The respondents remained anonymous, and data have been kept confidential.
Analytic plan
We employed chi-square tests to detect differences between women with and without UI according to the demographic information provided, presence of health conditions, and toileting behaviors. We explored differences in the continuous variables using Student’s t-tests and differences in the ordinal variables using the Mann-Whitney U nonparametric test. Variables significant at the p < 0.05 level in bivariate analyses were entered into multivariate logistic regression models. Questionnaires that had > 20% items with missing data were excluded from the analyses.
Results
We distributed 1000 questionnaires and obtained 929 usable questionnaires for analyses; see Fig. 1. We excluded the remaining 71 questionnaires for the following reasons: 21 respondents refused to participate and said “ashamed” upon seeing the questionnaire because of the perceived embarrassing nature of the study; 41 respondents’ questionnaires had 20% or more items with missing data; after beginning the questionnaire, 9 respondents reported having a urinary tract infection in the last 4 weeks. The respondents were between 18 and 26 years old (average age: 20.5 ± 1.6). The prevalence of UI was 23.6%. Most respondents with UI (82.5%) reported no bother and some respondents with UI (15.8%) reported minor bother. Few respondents (1.7%) reported moderate bother, and no respondents reported severe bother.
Table 1 presents the demographic characteristics of the respondents, and Table 2 presents the prevalence of habitual toileting behaviors and the types of toilets used in China. The most prevalent habitual toileting behaviors were emptying one’s bladder before leaving home (72.2%) and worrying about public toilet cleanliness (52.7%).
The respondents who were aged 18 to 20 years had a higher prevalence of UI than the respondents aged 21 to 26 years: 26.8% (121/451) versus 20.4% (92/452), respectively; χ2 = 5.252, p = 0.022; see Table 3. The frequency of physical exercise in the group aged 21 to 26 years was lower than in the younger group aged 18 to 20 years (z = −5.570, p < 0.001). Respondents with UI also had a higher body mass index (BMI) than respondents who did not have UI: 19.90 ± 2.29 versus 20.34 ± 2.67, t = −2.377, p = 0.018. Other factors that were significantly associated with UI in this study were parents’ monthly income, respondents’ dietary fiber intake, frequency of underpants change, alcohol consumption of any quantity and frequency, and constipation. Table 3 also shows that nine items from the TB-WEB instrument are associated with UI; of these items, two are related to premature voiding, three items are related to delaying voiding, and four items are related to straining to void. Voiding positions were found to have no statistical correlation with UI (p > 0.05).
Table 4 presents the multivariate logistic regression analysis results that show that respondents aged 21 to 26 years (odds ratio [OR] = 0.867, 95% confidence interval [CI] = 0.771–0.975) were less likely to experience UI than the respondents who were between 18 and 20 years old. Respondents who reported constipation (OR = 2.395, 95% CI = 1.494–3.839) and alcohol consumption (OR = 1.763, 95% CI = 1.114–2.792) had greater odds of UI than those who did not report constipation and alcohol consumption. Respondents who habitually delayed urination (OR = 1.738, 95% CI = 1.306–2.313) and strained to urinate (OR = 1.433, 95% CI = 1.111–1.849) were more likely to have UI than those who did not delay urination or strain to urinate.
Discussion
Few studies have investigated UI in young women in China despite indications that UI is problematic for this population in other countries. This study found that 23.6% of full-time female Chinese college students with an average age of 20.5 ± 1.6 years reported UI in the 4 weeks prior to administration of this study’s questionnaire. The UI prevalence reported here is similar to that reported in other countries. For example, Da Roza conducted a survey in Portugal with female students (14 to 33 years old; 83.9% were college students, 16.1% were high school students) and found that 19.9% reported UI (i.e., any leakage or involuntary loss of urine) [18]. In The Netherlands, 20.1% of female nulliparous medical students reported involuntary urine loss of any amount and frequency [19]. Almost 13% (n = 1002, 12.6%) of women between the ages of 16 and 30 years in Australia who responded to O’Halloran et al.’s survey reported UI [20]. One reason that the UI prevalence rate is higher in our study than in that of O’Halloran et al. is the difference in UI definitions used. Our UI definition included any frequency of UI, whereas O’Halloran et al. required a response of UI frequency as at least “sometimes.” Reported prevalence rates also may vary among studies because of differences in study designs and data collection methods [21]. For our study, we used the International Continence Society’s definition of UI and a validated instrument to measure it.
In our study, female respondents who were between 18 and 20 years old (19.23 ± 0.86 years) had higher UI prevalence rates than respondents who were between 21 and 26 years old (21.82 ± 1.00). This finding is similar to the results of a survey of 1936 non-pregnant women (15 to 25 years old) in Italy that found that being younger than 19 years old is a risk factor for UI (OR = 1.0, 95% CI = 0.6–1.8) [22]. We also found that the frequency of physical exercise in the 18- to 20-year-old age group was higher than in the 21- to 26-year-old group. Although the female pelvic floor muscles can tolerate certain repetitive efforts and impact, active and frequent engagement in physical exercise may fatigue the pelvic floor muscles with no evidence of muscle damage, which may be associated with urine leakage [14]. Furthermore, another study showed that women aged 25 to 30 years have more awareness and understanding of pelvic floor disorders and are more likely to have received education regarding UI compared with women aged 19 to 24 years [2]. Knowledge and perceptions about healthy behavior are important to optimize bladder health [2, 16]. However, we did not collect data to differentiate among types of UI (such as stress UI, urgency UI, mixed UI, etc.), and the underlying mechanisms of UI in the two age groups (18 to 20 years old versus 21 to 26 years old) are not clear.
The bivariate analysis results show significant differences in BMI between women with UI (20.34 ± 2.67 kg/m2) and without UI (19.90 ± 2.29 kg/m2); however, these values are within the normal BMI range (18.5–23.9 kg/m2) [15], and therefore they were not entered in the final logistic regression. In another study [22] with young women (aged 15 to 25 years), a BMI of ≥ 30 kg/m2 was associated with an increased risk of UI.
Our study also found that respondents who reported any alcohol consumption were more likely to have UI than those who never drank alcohol. Although the respondents did not report the amounts of alcohol consumed, most respondents (99.8%) reported that they did not drink alcohol excessively. Traditional Chinese culture does not encourage women to drink alcohol, and even though women are freer to drink than in the past, they tend to display little interest in doing so. Only two respondents (0.2%) reported that they drank large amounts of alcohol, whereas 124 respondents (13.4%) reported that they drank an appropriate amount of alcohol. In contrast, over half (51.3/%; n = 97/189) of the female undergraduate college students at a private university in the northeast US reported drinking alcohol two to five times per week [3]. Another study of adult Chinese women found that alcohol consumption (amount not specified) is a risk factor (OR = 1.51, 95% CI = 1.35–1.63) for UI (n = 18,992) [15].
Sexual activity has been associated with UI in nulliparous Australian women (22.5 ± 3.2 years) [20]. In our study, 94.4% of the respondents reported not engaging in sexual activity. We found no difference in UI prevalence between respondents who reported not being sexually active and those who reported being sexually active. In traditional Chinese culture, women feel ashamed to engage in sexual activity before marriage and are embarrassed to talk about sex. Sexual life is usually perceived as a symbol of uncleanliness rather than as a basic physiologic need for women. Chinese women rarely talk about sex with others, including parents, friends, and even healthcare providers [23]. Some respondents expressed embarrassment about responding to questionnaire items concerning UI and other conditions of the urogenital system. During our data collection process, 21 respondents refused to participate after seeing the questionnaire because of the personal nature of the questions. Sensitivity to these perceptions is needed as more education and research about sexual and bladder health are developed and conducted in China.
When we designed this study, we postulated that the cleanliness of the perineal area is associated with bladder health. To this end, we developed a questionnaire item to ask about the frequency of underpants change. The bivariate analysis results show that respondents who changed their underpants every day were less likely to have UI than those who did not. This variable did not remain significant in the multivariate analysis.
Our study also found that constipation increased the risk of UI. Women who ingested more fiber in their diets (χ2 = 12.333, p < 0.001) and fluid (χ2 = 22.875, p < 0.001) reported less constipation than those who did not. Ninomiya et al. also found that constipation is a risk factor for stress UI in 4804 Japanese women (average age = 40.4 years) [24]. These authors noted that, although the mechanism is not well defined, damage to the pelvic floor might be caused by repeated high abdominal pressure during defecation and dilation of the rectum caused by accumulated stool. Because constipation plays an important role in the development and worsening of UI [22], young women need to be aware of the importance of fiber and fluid intake to help prevent constipation and to be aware also of changes in urination and frequency of UI episodes when they note changes in the frequency of bowel movements.
Palmer et al.’s study found that the risk of having UI is greater for women (median age = 43 years, ranging from 26 to 68 years) who habitually delayed urination than for those who did not [25]; this finding is consistent with the results of our study. This finding may also have implications for the mechanisms that concern lower urinary tract control. When the bladder remains full with a large volume of urine due to delayed urination, intravesical pressure could exceed intraurethral pressure, leading to urine leakage [4]. Kowalik reported that adult women who delayed urination at work were more likely to experience bladder problems [26]. Over time, delayed urination may affect bladder function by leading to chronic excessive tension of the bladder’s smooth muscle (detrusor), which gradually results in the dysfunction (i.e., detrusor overactivity, detrusor under-activity, or detrusor hyperactivity impaired contractility) and low compliance of the bladder [4, 24] and impaired innervation [6]. Conversely, Xu et al. found that avoiding delayed urination (i.e., urinating when needing to do so) significantly relieved bladder symptoms (average marginal effect = −2.207, p < 0.001) and lowered the risk of having urgency UI (average marginal effect = −0.344, p < 0.001) among middle-aged and older patients with overactive bladder diagnoses [27]. A better understanding of the effects of these behaviors on underlying bladder storage and emptying mechanisms is important to designing interventions to prevent or delay lower urinary tract symptoms.
Another important finding of this study is that emptying the bladder by ‘pushing down’ is associated with UI (OR = 1.433, 95% CI = 1.111–1.849). Habitually straining to urinate may lead to movement of the bladder neck and urethra that weakens contraction of the detrusor, thus playing a role in UI. Lacima et al. found that straining is closely associated with combined fecal and urinary incontinence [28]. The ‘hammock hypothesis’ is widely accepted as a pathophysiologic explanation of stress UI that is associated with urethral hypermobility [4]. The endopelvic fascia creates a ‘hammock’ against the urethra that compresses the urethra during both rest and activity. This compression is combined with intrinsic urethral sphincter pressure and mucosal coaptation. Mucosal coaptation effectively closes the urethral lumen and prevents the involuntary loss of urine even when intravesical pressure increases [4]. When damage to the arcus tendineus fasciae pelvis or paravaginal tissue results from excess loading caused by obesity, chronic coughing, constipation, or straining [6], anatomical support for the bladder neck and urethra is decreased. Some researchers recommend that women should learn to relax the pelvic floor and avoid straining as the optimal way to empty their bladder [29].
Environmental and cultural factors also could impact the toileting behaviors of Chinese female college students. Due to China’s large population, shopping centers, hospitals, schools, and public places often are crowded; as a result, toilet facilities often are insufficient to accommodate the number of people who require them. Furthermore, the break time for students between classes is short (about 10 min); due to the lack of adequate toileting facilities, many students must wait in line until the next class begins. Rather than risk being late to class, they abandon the line and hold their urine until the next opportunity arises to go to the toilet. Patience is a virtue in Chinese traditional culture; thus, students accept that they must wait (and are accustomed to waiting) until toilet facilities are available. They also know that arriving late to class or leaving during class is considered by both their teachers and peers to be disrespectful. Therefore, female students adapt to environmental and cultural norms by delaying urination, straining to urinate, or urinating when they have no need to urinate. This topic is an important area of study because little is known about the short- and long-term effects of these behaviors on bladder function.
The squatting posture is the most common urination position in China because of the widespread use of squatting pans. Even though more Chinese families are using western-style toilets, such toilets are still rare in public places. Squatting has been associated with a significantly higher maximum flow rate and less postvoid residue in healthy adult women [30]. However, in this study, we did not find differences in UI prevalence between students who habitually used toilets to urinate and those who habitually used squatting pans. The long-term use, over several decades of life, of certain types of toilets may affect the development of UI.
Notably, China’s population exceeds 1.3 billion people, and women constitute almost half of this number [9]. Therefore, research into factors associated with UI and other lower urinary tract symptoms in young women is urgently needed for this enormous population. According to this study, some initiatives may facilitate bladder health in young Chinese women. First, health education about UI is important to increase awareness that attending to the physiologic need to urinate is important to women’s bladder health. This information could be disseminated in schools during lectures related to health and wellness and during club activities. Also, school administrators should consider policies that include assurance of students’ timely access to toilets. Changes in the environment, such as the provision of public toilets that are clean and well-maintained, may also promote bladder health. Providing adequate access to clean toilets should be normative at universities and other public places.
Longitudinal studies with young women are needed to shed light on the role toileting behaviors throughout their lives and in different environments may play in UI incidence. In addition, more research is needed to understand reasons why some young women use certain toileting behaviors when they are at school, but use other behaviors when they are at home. This information will aid in identifying roles these behaviors may play in the development and trajectory of UI or other lower urinary tract symptoms. Other behaviors, such as those related to perineal hygiene, should also be explored in relation to the bladder health of young women.
Some features of this study may limit the generalizability of the findings. This study was conducted in one region in China and included only female college students. The students who participated in this study attended institutions of higher education in Xuzhou, located in the middle of China, which is the cradle of Han Dynasty culture and influenced by Confucian traditional culture, which is associated with quiet or demure behavior and being tolerant of others and the environment. The various ways that cultural influences may affect women’s habits related to urination needs and toileting behaviors still require study. Women from other regions in China with other customs, educational backgrounds, and occupations also should be recruited for studies to enrich scientific and clinical knowledge about bladder health in young Chinese women.
Conclusion
Age, alcohol consumption, constipation, delaying bladder emptying until it is difficult to continue holding urine, and emptying the bladder by pushing down or straining are factors associated with UI when controlling for other variables. This study provides important information for clinicians, researchers, and other healthcare professionals about toileting behaviors and how such habitual behaviors may relate to UI in this sample and potentially the general female college-aged population. Educational interventions that target toileting behaviors while taking into account environmental and cultural factors should be developed and tested to improve young women’s self-care with the aim to prevent or delay UI in middle and later life.
References
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21(1):5–26.
Parden AM, Griffin RL, Hoover K, Ellington DR, Gleason JL, Burgio KL, et al. Prevalence, awareness, and understanding of pelvic floor disorders in adolescent and young women. Female Pelvic Med Reconstr Surg. 2016;22(5):346–54.
Angelini KJ, Newman DK, Palmer MH. Psychometric evaluation of the toileting behaviors: women's elimination behaviors scale in a sample of college women. Female Pelvic Med Reconstr Surg. 2019. https://doi.org/10.1097/SPV.0000000000000711.
Aoki Y, Brown HW, Brubaker L, Cornu JN, Daly JO, Cartwright R. Urinary incontinence in women. Nat Rev Dis Primers. 2017;3:17042.
Harlow BL, Bavendam TG, Palmer MH, Brubaker L, Burgio KL, Lukacz ES, et al. The prevention of lower urinary tract symptoms (PLUS) research consortium: a transdisciplinary approach toward promoting bladder health and preventing lower urinary tract symptoms in women across the life course. J Women's Health (Larchmt). 2018;27(3):283–9.
Wan X, Wu C, Xu D, Huang L, Wang K. Toileting behaviours and lower urinary tract symptoms among female nurses: a cross-sectional questionnaire survey. Int J Nurs Stud. 2016;65:1–7.
Palmer MH, Willis-Gray MG, Zhou F, Newman DK, Wu JM. Self-reported toileting behaviors in employed women: are they associated with lower urinary tract symptoms? Neurourol Urodyn. 2018;37(2):735–43.
Wang K, Palmer MH. Women's toileting behaviour related to urinary elimination: concept analysis. J Adv Nurs. 2010;66(8):1874–84.
The State Council of Office of Population Censuses and Surveys. Data of the 2010 Census in China. China Statistics Press. 2012. http://www.stats.gov.cn/tjsj/pcsj/rkpc/6rp/indexch.htm.
Chinese Medical Association. Guidelines for diagnosis and treatment of chronic constipation in China. Chin J Dig. 2013;33(5):291–7.
Chinese Medical Association. Guidelines for clinical diagnosis and treatment of dysfunctional uterine bleeding. Chin J Obstet Gynecol. 2009;44(3):234–6.
Liu y WC, Sun T, Guan XM, Wang KF. Reliability and validity of the Chinese version of Women's toileting behavior scale: testing in community urinary incontinence. J Nurs Sci. 2012;27(16):78–80.
Huang L, Zhang SW, Wu SL, Ma L, Deng XH. The Chinese version of ICIQ: a useful tool in clinical practice and research on urinary incontinence. Neurourol Urodyn. 2008;27(6):522–4.
Alves JO, Luz STD, Brandao S, Da Luz CM, Jorge RN, Da Roza T. Urinary incontinence in physically active young women: prevalence and related factors. Int J Sports Med. 2017;38(12):937–41.
Zhang L, Zhu L, Xu T, Lang J, Li Z, Gong J, et al. A population-based survey of the prevalence, potential risk factors, and symptom-specific bother of lower urinary tract symptoms in adult Chinese women. Eur Urol. 2015;68(1):97–112.
Xu D, Chen L, Wan X, Zhang Y, Liu N, Wang K. Toileting behaviour and related health beliefs among Chinese female nurses. Int J Clin Pract. 2016;70(5):416–23.
Wan XJ, Zhang Y, Liu Y, Wu C, Wang KF. Reliability and validity of the Chinese version of women’ s toileting behavior scale among female nurses. Chin J Nurs. 2014;49(7):782–5.
Da Roza T, Brandao S, Mascarenhas T, Jorge RN, Duarte JA. Urinary incontinence and levels of regular physical exercise in young women. Int J Sports Med. 2015;36(9):776–80.
van Breda HM, Bosch JL, de Kort LM. Hidden prevalence of lower urinary tract symptoms in healthy nulligravid young women. Int Urogynecol J. 2015;26(11):1637–43.
O'Halloran T, Bell RJ, Robinson PJ, Davis SR. Urinary incontinence in young nulligravid women: a cross-sectional analysis. Ann Intern Med. 2012;157(2):87–93.
Bedretdinova D, Fritel X, Panjo H, Ringa V. Prevalence of female urinary incontinence in the general population according to different definitions and study designs. Eur Urol. 2016;69(2):256–64.
Bardino M, Di Martino M, Ricci E, Parazzini F. Frequency and determinants of urinary incontinence in adolescent and young nulliparous women. J Pediatr Adolesc Gynecol. 2015;28(6):462–70.
Wu C, Wang K, Sun T, Xu D, Palmer MH. Predicting help-seeking intention of women with urinary incontinence in Jinan, China: a theory of planned behaviour model. J Clin Nurs. 2015;24(3–4):457–64.
Ninomiya S, Naito K, Nakanishi K, Okayama H. Prevalence and risk factors of urinary incontinence and overactive bladder in Japanese women. Low Urin Tract Symptoms. 2018;10(3):308–14.
Palmer MH, Newman DK. Women's toileting behaviours: an online survey of female advanced practice providers. Int J Clin Pract. 2015;69(4):429–35.
Kowalik CG, Daily A, Delpe S, Kaufman MR, Fowke J, Dmochowski RR, et al. Toileting behaviors of women—what is healthy? J Urol. 2019;201(1):129–34.
Xu D, Huang L, Gao J, Li J, Wang X, Wang K. Effects of an education program on toileting behaviors and bladder symptoms in overactive bladder patients with type 2 diabetes: a randomized clinical trial. Int J Nurs Stud. 2018;87:131–9.
Lacima G, Espuna M, Pera M, Puig-Clota M, Quinto L, Garcia-Valdecasas JC. Clinical, urodynamic, and manometric findings in women with combined fecal and urinary incontinence. Neurourol Urodyn. 2002;21(5):464–9.
Sjogren J, Malmberg L, Stenzelius K. Toileting behavior and urinary tract symptoms among younger women. Int Urogynecol J. 2017;28(11):1677–84.
Gupta NP, Kumar A, Kumar R. Does position affect uroflowmetry parameters in women? Urol Int. 2008;80(1):37–40.
Funding
The Qing Lan Project (no. 53041608) provided funding for this research to Dr. Zhou. The First Quality Bladder Health Initiative also provided funding for this study. The funding entities had no role in the study or publication of the findings.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
First co-authors: Fang Zhou, Kaikai Xue, and Yuping Liu
Rights and permissions
About this article
Cite this article
Zhou, F., Xue, K., Liu, Y. et al. Toileting behaviors and factors associated with urinary incontinence in college-aged female students in China. Int Urogynecol J 31, 961–971 (2020). https://doi.org/10.1007/s00192-019-04043-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-019-04043-3