Abstract
Introduction and hypothesis
We aimed to determine the prevalence of urinary incontinence (UI) in nulliparous female university students and to provide an overview of risk factors associated with urinary continence.
Methods
A total of 1,397 female university students aged 18–28 years were enrolled into this cross-sectional questionnaire study. The self-administered questionnaires, the International Consultation on Incontinence Questionnaire Short Form (ICIQ-SF), Overactive Bladder V8 (OAB-V8), demographics, and general characteristics were recorded. The frequency, type, and severity of urinary incontinence and related factors were evaluated.
Results
The mean age of the students was 20.27 ± 1.69 years. The prevalence of UI in female university students was 18.4% (n = 258). ICIQ-SF total score was 0.85 ± 2.11 (0–14). OAB–V8 total score was 5.97 ± 5.35 (0–40) and 27.0% of participants had scores of ≥8. Elevated BMI, childhood enuresis, constipation, exercising, positive family history for UI, accommodation in a dormitory, and holding urine at school are risk factors associated with UI in female university students.
Conclusion
We demonstrated that UI is a common condition among female university students. The identification of the associated risk factors will help to further raise the knowledge and awareness of the problem, and preventive strategies may be proposed to young women to improve the quality of life and psychological well-being.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urinary incontinence (UI) is involuntary urine leakage that leads to social and hygienic problems. It constitutes a common public health issue and negatively affects women of all ages and it causes the quality of life to deteriorate remarkably [1]. There are three common types of UI: stress UI refers to urine leakage provoked by effort, exercise, sneezing or coughing, urge UI refers to a constant sense of urgency to urinate and mixed UI refers to urine leakage resulting from the coexistence of stress and urge UI [2].
Age and obesity are well-established risk factors for UI [3]. The other risk factors are parity, smoking, chronic diseases, constipation, pelvic surgery, high-impact physical activities, menopause, caffeine use, difficult labor, giving birth to a newborn weighing more than 4 kg, and use of medications such as psychotropic drugs, angiotensin-converting enzyme inhibitors, and diuretics [4].
The prevalence of female UI varies widely in relevant publications. Most of these studies focus on perimenopausal and postmenopausal women. Urinary incontinence particularly affects the elderly and women who have given birth [3]. However, epidemiological studies demonstrated that young nulliparous women may also suffer from UI [5,6,7].
Urinary incontinence is an often underdiagnosed and undertreated condition in young women and only a few women with UI seek medical help in this age group [8]. The prevalence of complaints linked with UI may vary with age, and the UI prevalence in female university students has not yet been studied extensively. The determination of frequency and related factors for UI is important for the establishment of preventive measures. It is possible to treat or reduce the symptoms of UI by lifestyle modifications and other conservative treatment methods. Thus, we aimed to investigate the prevalence and potential risk factors of UI in female university students with no risk factors.
Materials and methods
This cross-sectional questionnaire study was performed in the obstetrics and gynecology and family medicine departments of our tertiary care center between January 2018 and June 2018. The study population consisted of female university students regardless of their departments. The questionnaires were distributed to the volunteers who were willing to participate in the study. All data collection was anonymous and the self-administered questionnaires were filled out with the aid of an assistant. The assistant who performed the data collection immediately checked whether the questionnaires were properly filled in. Missing and incomplete answers were highlighted and corrected by the participants on site. The questionnaire included a demographic session (age, height and weight, employment, marital status, and place of accommodation), and the International Consultation on Incontinence Questionnaire Short Form (ICIQ-SF) and Overactive Bladder V8 (OAB-V8) questionnaires to determine the frequency, type, severity, and related factors of the urinary incontinence. Ethics committee approval was received from the local institutional review board (decision No:2017/183).
The ICIQ-SF scale has been developed by the International Continence Society (ICS) for the assessment of UI and its impact on the quality of life. It yields satisfactory degrees of sensitivity, validity, and reliability. The questionnaire possesses a good test–retest reliability, with the lowest kappa value of 0.54 in one of the categorical variables, whereas the other kappa values ranged between 0.61 and 1.0 [9]. This scale has been validated for Turkish language [10]. The Cronbach’s alpha reliability of ICIQ-SF was 0.95 [11]. The ICIQ-SF scale has four items other than age and gender. The ICIQ-SF monitors the frequency of UI and the amount of leaked urine in the first and second items respectively. The third item investigates the degree of deterioration of quality of daily life due to the leakage of urine. The total score of ICIQ-SF is calculated by the sum of the scores of these three items. The ICIQ-SF total score represents the severity and bother score, which ranges from 0 to 21. The total score can be graded for the severity of UI(0: no leak; 1–5: slight; 6–12: moderate; 13–18: severe; 21: very serious urine leakage) [9]. The fourth item of the ICIQ-SF questions the possible causes of UI and helps to identify the type of UI. Depending on the answers to the fourth question, urinary incontinence is categorized as having stress incontinence (leakage during coughing, sneezing or physical activity), urge incontinence (leakage before getting to the toilet), or mixed incontinence (a combination of stress and urge incontinence).
The OAB-V8 is a short questionnaire that focuses on the symptoms of urge UI. It contains eight questions for symptom scores. The total score is obtained from the sum of the answers given to all questions and it ranges between 0 and 40. Patients with total OAB-V8 score ≥8 were considered to have an OAB [12]. The Cronbach’s alpha reliability of OAB was 0.90 [13]. OAB-V8 questionnaire has been validated in the Turkish language [14].
Beverages such as tea, fruit tea, herbal tea, coffee, acidic beverages, fruit juices, and alcoholic drinks are liquids with a diuretic effect, whereas water, milk, buttermilk, soup, ice cream do not have a diuretic effect [15].
Two or more micturitions per night was defined as nocturia [16]. The body mass index (BMI) was classified as: <18.5 underweight; 18.5–24.9 normal weight; >25 overweight [17].
Female students aged between 18 and 28 years were included in our study. Students with any urological or gynecological disease, a history of surgery for urogynecological problems, neurological and respiratory diseases, urinary tract infection symptoms, and current or previous pregnancies were excluded from the study.
The Statistical Package for Social Sciences program (SPSS, Chicago, IL, USA) version 21 was used for the analysis of our data. In descriptive statistics, mean, standard deviation, and minimum and maximum values in numerical variables were given, whereas in categorical variables, on the other hand, number and percentage values were given. To test the presence of a significant difference between groups, a t test was performed. On the other hand, the differences between three or more groups were examined by one-way analysis of variance (ANOVA). In the case of the presence of a difference, the group(s) that showed the difference were examined using the paired comparisons test. The Pearson or Spearman coefficient of correlation was used to determine whether there was a significant relationship between numerical variables. When evaluating the effect of significant variables on the response variable together, multi-linear regression analysis was used. A p value less than 0.05 was considered statistically significant.
Results
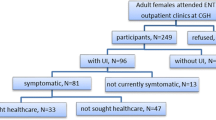
A total of 1,397 female university students participated in this study. The mean age of the students was 20.27 ± 1.69 years (minimum to maximum: 18–28). The mean height of the participants was 1.64 ± 0.06 m (64.56 ± 2.36 in; minimum to maximum: 1.45–1.87 m; 57.09–73.62 in), whereas their mean body weight 58.38 ± 9.59 kg (128.70 ± 21.14 lb; minimum to maximum: 40–125 kg; 88.18–275.58 lb). Table 1 demonstrates an overview of the sociodemographic characteristics of this population.
The mean total fluid intake with daily diuretic effect was 759.12 ± 499.52 ml, whereas it was 1,343 ± 639.39 ml for the mean fluid amount without diuretic effect. Four hundred and eighty-six participants (34.8%) had consumed less than 1,500 ml fluid daily, whereas 770 cases (55.1%) had a daily fluid consumption of between 1,500 and 3,000 ml, and 141 (10.1%) participants reported a daily fluid intake >3,000 ml.
Table 2 demonstrates the ICIQ-SF total scores and grades of participants. ICIQ-SF total score was 0.85 ± 2.11 (minimum to maximum: 0–14). Regarding the diagnostic fourth item, the ICIQ-SF question “Under which conditions does urinary incontinence occur?”, 81.6% of students (n = 1,139) reported that they never experienced UI. Of the remaining participants 18.4% (n = 258) stated that they had urinary incontinence in different situations. UI occurred before getting to the toilet (8.6%), on sneezing and coughing (1.2%), during sleeping (2.9%), with physical exertion (1.9%), after the cessation of micturition (3.3%), without any reason (0.4%), and all the time (0.0%). The responses to this question indicate the prevalence and type of UI and are displayed in Table 3.
The association between the severity of UI and risk factors is demonstrated in Table 4. The UI was found to be more frequent in students with a BMI > 25 (p = 0.011), a history of constipation (p = 0.002), family history of UI (p < 0.001), childhood enuresis (p < 0.001), who exercise every day (p < 0.001), who hold urine at school almost every day (p = 0.006) and who live in the dormitories (p = 0.005).
The sum of responses to eight questions in the OAB-V8 questionnaire yields the total score and it was 5.97 ± 5.35 (minimum to maximum: 0–40). 73.0% of participants had scores of <8, whereas 27.0% of participants had scores of ≥8. The association between OAB-V8 total score and risk factors is shown in Table 5. Accordingly, urge incontinence was found to be statistically highly significant in students with obesity (p < 0.001), constipation (p < 0.001), chronic diseases (p < 0.001), history of childhood enuresis (p < 0.001), and family history of UI (p < 0.001).
Discussion
Urinary incontinence is a frequent disorder that affects women of all ages. Although it is not a life-threatening condition, it adversely affects physical and mental health and causes the quality of life of women to deteriorate [8]. The prevalence of urinary incontinence increases with age, from 7% in non-pregnant women aged 20–39 years to 17% in in the age group 40–59, 23% in the age group 60–79 and 32% in women over 80 years old [18]. Most of the studies on this subject were performed on women in middle and advanced ages. In the relevant literature, we could find only one previous study, which focused on UI prevalence among female nulliparous women in a large series [6]. We aimed to determine the prevalence of UI in female university students and our results indicated that the prevalence of UI was 18.4% in this population. We demonstrated that UI was a common condition in women in this young age group with no additional risk factors.
Previous publications show a marked variation in the prevalence of UI in young women (ranging between 6.2% and 32%) and this variability may be attributed to the differences in methodology and definitions [6,7,19,20].
In our study, we found that BMI, childhood enuresis, constipation, exercising, a family history of UI and place of accommodation are the associated risk factors for UI in female university students, according to the ICIQ-SF questionnaire. Childhood enuresis and a family history of urinary incontinence and constipation were also supposed to be risk factors for UI in other studies [6,21]. Moreover, chronic diseases may constitute risk factors for UI in university students according to the OAB-V8 questionnaire.
Elevated BMI, exercising, and constipation may cause chronic increases in intra-abdominal pressure and causes an increase in intravesical pressure that exceeds the urethral closure pressure. Chronic elevated intra-abdominal pressure weakens the pelvic floor and leads to incontinence [22]. These factors are associated with stress UI. Obesity is closely related to the occurrence of UI. The association between BMI and UI had been studied previously and every five-unit increase in BMI augmented the risk of UI by 20–70% [23]. Hence, achieving a healthy BMI is important for reducing UI and improving women’s psychological and social well-being [24].
The other risk factors, such as childhood enuresis, a family history of urinary incontinence, smoking habits and place of accommodation, may indicate psychological stress [25]. These conditions could share similar etiological factors. Childhood enuresis and family history of UI may be linked to a lack of learning how to achieve normal urinary bladder control during toilet training. These factors have been commonly reported with urge UI in other studies [26,27,28]. Recognition of UI at an early age may facilitate treatment, thereby avoiding the occurrence of UI in adulthood.
Many women experience emotional difficulties, such as shame and embarrassment about seeking medical aid for UI and related complaints. The hope for a spontaneous resolution of UI, embarrassment at being examined by a clinician, reluctance to discuss one’s complaint, the belief that urine leakage is a normal occurrence and lack of awareness regarding the availability of treatment were their reasons for not seeking UI treatment [8]. Women may experience fear and shame about UI and these feelings may lead to discouragement and ignorance of their complaints, resulting in a lack of resolution of UI. Younger women were more likely to be under stress and to be ashamed of their UI [19]. Previous publications reported that embarrassment was of central concern for women affected by UI and only about 25% of women seek medical help for this complaint [29].
Urinary incontinence was usually diagnosed only when its signs and symptoms persisted and became stronger [30]. It is difficult for women to identify UI as a medical condition. Health professionals should be aware of the fact that only a few women with UI seek medical help. The health professionals should give counseling to women by increasing their awareness about UI-related risk factors, by facilitating the expression of their urinary system complaints comfortably and by informing them about when to seek medical care for their urinary symptoms.
The prevention and timely diagnosis of UI is important, particularly at a young age. Based on the patients’ needs, UI can be managed in different preventive strategies, such as continence advisory services addressing lifestyle changes, behavioral therapy, and fluid intake management; physiotherapy for strengthening pelvic floor muscles, bladder retraining programs, and medication [31]. Health professionals have an important function in the identification of the components of an effective management plan, evaluation of risk factors for UI, establishment of interventions to diagnose the treatable underlying causes as per women’s needs, and the monitoring of women’s treatment outcomes.
Necessary measures should be taken in university students, including creating policies to improve women’s health by developing an early diagnosis, management and support programs, health policies, and prevention and management of the condition. Prevention of obesity, constipation, and urinary tract infections, regulation of the amount and content of the liquid consumed can reduce urinary incontinence episodes. Improvement in UI episodes has been noted after weight loss, treatment of constipation, and modification of lifestyle; thus, administration of a prevention program in young women at risk can be an effective and useful approach [32].
The main strengths of this study are the large sample size and the use of a validated questionnaire to diagnose UI. The potential limitations of this study involve data confined to the experience of a single-center, selection bias, and the lack of sophisticated diagnostic methods for UI. These limitations should be kept in mind when interpreting the results.
Urinary incontinence may lead to discomfort, loss of confidence, and self-esteem, and may have adverse effects, not only on physical and mental health but also on the quality of life of women. A multi-disciplinary assessment of women’s health and a preventive protocol can be developed for women at a young age to improve knowledge and awareness.
To conclude, UI is a hidden health problem in female university students. In our series involving a group of otherwise healthy young women, the UI prevalence was high. The estimation of UI prevalence in female university students and recognition of the risk factors may help to increase awareness of this problem. Our data may encourage young women to seek medical care for this complaint. Their quality of life will be improved owing to the effect of early diagnosis and appropriate treatment on their participation in daily activities such as sports, sexual life, and social communication. Further efforts should be made to implement preventive strategies and to provide counseling on the prevention of UI in young women.
References
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology. 2003;61:37–49. https://doi.org/10.1016/s0090-4295(02)02243-4.
Haylen BT, De Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29:4–20. https://doi.org/10.1002/nau.20798.
Minassian VA, Stewart WF, Wood GC. Urinary incontinence in women: variation in prevalence estimates and risk factors. Obstet Gynecol. 2008;111:324–31. https://doi.org/10.1097/01.AOG.0000267220.48987.17.
Botlero R, Davis SR, Urquhart DM, Shortreed S, Bell RJ. Age-specific prevalence of, and factors associated with, different types of urinary incontinence in community-dwelling Australian women assessed with a validated questionnaire. Maturitas. 2009;62:134–9. https://doi.org/10.1016/j.maturitas.2008.12.017.
O'Halloran T, Bell RJ, Robinson PJ, Davis SR. Urinary incontinence in young nulligravid women: a cross-sectional analysis. Ann Intern Med. 2012;157:87–93. https://doi.org/10.7326/0003-4819-157-2-201207170-00005.
Bardino M, Di Martino M, Ricci E, Parazzini F. Frequency and determinants of urinary incontinence in adolescent and young nulliparous women. J Pediatr Adolesc Gynecol. 2015;28:462–70. https://doi.org/10.1016/j.jpag.2015.01.003.
Da Roza T, Brandão S, Mascarenhas T, Jorge RN, Duarte JA. Urinary incontinence and levels of regular physical exercise in young women. Int J Sports Med. 2015;36:776–80. https://doi.org/10.1055/s-0034-1398625.
Van Breda HM, Bosch JL, de Kort LM. Hidden prevalence of lower urinary tract symptoms in healthy nulligravid young women. Int Urogynecol J. 2015;26:1637–1643. https://doi.org/10.1007/s00192-015-2754-1.
Avery K, Donovan J, Peters TJ, Shaw C, Gotoh M, Abrams P. ICIQ: a brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol Urodyn. 2004;23:322–30. https://doi.org/10.1002/nau.20041.
Çetinel B, Özkan B, Can G. The validation study of ICIQ-SF Turkish version. Turk Uroloji Dergisi. 2004;30:332–8.
Klovning A, Avery K, Sandvik H, Hunskaar S. Comparison of two questionnaires for assessing the severity of urinary incontinence: the ICIQ-UI SF versus the incontinence severity index. Neurourol Urodyn. 2009;28:411–5. https://doi.org/10.1002/nau.20674.
Acquadro C, Kopp Z, Coyne KS, Corcos J, Tubaro A, Choo MS, et al. Translating overactive bladder questionnaires in 14 languages. Urology. 2006;67:536–40. https://doi.org/10.1016/j.urology.2005.09.035.
Matza LS, Thompson CL, Krasnow J, Brewster-Jordan J, Zyczynski T, Coyne KS. Test–retest reliability of four questionnaires for patients with overactive bladder: the overactive bladder questionnaire (OAB-q), patient perception of bladder condition (PPBC), urgency questionnaire (UQ), and the primary OAB symptom questionnaire (POSQ). Neurourol Urodyn. 2005;24:215–25. https://doi.org/10.1002/nau.20110.
Tarcan T, Mangır N, Özgür MÖ, Akbal C. OAB-V8 Overactive Bladder Questionnaire Validation Study. Uroloji Bülteni. 2012;2:113–6.
Maughan RJ, Watson P, Cordery PA, Walsh NP, Oliver SJ, Dolci A, et al. A randomized trial to assess the potential of different beverages to affect hydration status: development of a beverage hydration index. Am J Clin Nutr. 2016;103:717–23. https://doi.org/10.3945/ajcn.115.114769.
Biyik I, Kucuk B, Arpaci HF, Demirci H. Factors affecting doctor visits of postmenopausal women with urinary incontinence. Low Urin Tract Symptoms. 2019;11:200–5. https://doi.org/10.1111/luts.12261.30916894.
Mondul AM, Giovannucci E, Platz EA. A prospective study of obesity, and the incidence and progression of lower urinary tract symptoms. J Urol. 2014;191:715–21. https://doi.org/10.1016/j.juro.2013.08.110.
Nygaard I, Barber MD, Burgio KL, Kenton K, Meikle S, Schaffer J, et al. Prevalence of symptomatic pelvic floor disorders in US women. JAMA. 2008;300:1311–6. https://doi.org/10.1001/jama.300.11.1311.
Hägglund D, Olsson H, Leppert J. Urinary incontinence: an unexpected large problem among young females. Results from a population-based study. Fam Pract. 1999;16:506–9. https://doi.org/10.1093/fampra/16.5.506.
Stones RW, Padmadas SS, Guo S, Brown JJ, Zhao F, Li B. Dyspareunia, urinary sensory symptoms, and incontinence among young Chinese women. Arch Sex Behav. 2006;35:561–7. https://doi.org/10.1007/s10508-006-9070-2.
Brown SJ, Donath S, MacArthur C, McDonald EA, Krastev AH. Urinary incontinence in nulliparous women before and during pregnancy: prevalence, incidence, and associated risk factors. Int Urogynecol J. 2010;21:193–202. https://doi.org/10.1007/s00192-009-1011-x.
Ramalingam K, Monga A. Obesity and pelvic floor dysfunction. Best Pract Res Clin Obstet Gynaecol. 2015;29:541–7. https://doi.org/10.1016/j.bpobgyn.2015.02.002.
Subak LL, Richter HE, Hunskaar S. Obesity and urinary incontinence: epidemiology and clinical research update. J Urol. 2009;182:2–7. https://doi.org/10.1016/j.juro.2009.08.071.
Subak LL, Whitcomb E, Shen H, Saxton J, Vittinghoff E, Brown JS. Weight loss: a novel and effective treatment for urinary incontinence. J Urol. 2005;174:190–5. https://doi.org/10.1097/01.ju.0000162056.30326.83.
Perry S, McGrother CW, Turner K, Leicestershire MRC. An investigation of the relationship between anxiety and depression and urge incontinence in women: development of a psychological model. Br J Health Psychol. 2006;11:463–82. https://doi.org/10.1348/135910705X60742.
D'Ancona CA, Lopes MH, Faleiros-Martins AC, Lúcio AC, Campos RM, Costa JV. Childhood enuresis is a risk factor for bladder dysfunction in adult life? Neurourol Urodyn. 2012;31:634–6. https://doi.org/10.1002/nau.21195.
Fitzgerald MP, Thom DH, Wassel-Fyr C, Subak L, Brubaker L, Van Den Eeden SK, et al. Reproductive risks for incontinence study at Kaiser research group, childhood urinary symptoms predict adult overactive bladder symptoms. J Urol. 2006;175:989–93. https://doi.org/10.1016/S0022-5347(05)00416-7.
Salvatore S, Serati M, Origoni M, Candiani M. Is overactive bladder in children and adults the same condition? ICI-RS 2011. Neurourol Urodyn. 2012;31:349–51. https://doi.org/10.1002/nau.22223.
Kinchen KS, Burgio K, Diokno AC, Fultz NH, Bump R, Obenchain R. Factors associated with women's decisions to seek treatment for urinary incontinence. J Women's Health. 2003;12:687–98. https://doi.org/10.1089/154099903322404339.
Mendes A, Hoga L, Gonçalves B, Silva P, Pereira P. Adult women's experiences of urinary incontinence: a systematic review of qualitative evidence. JBI Database System Rev Implement Rep. 2017;15:1350–408. https://doi.org/10.11124/JBISRIR-2017-003389.
Lukacz ES, Santiago-Lastra Y, Albo ME, Brubaker L. Urinary incontinence in women: a review. JAMA. 2017;318:1592–604. https://doi.org/10.1001/jama.2017.12137.
Nambiar AK, Bosch R, Cruz F, Lemack GE, Thiruchelvam N, Tubaro A, et al. EAU guidelines on assessment and nonsurgical management of urinary incontinence. Eur Urol. 2018;73:596–609. https://doi.org/10.1016/j.eururo.2017.12.031.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ural, Ü.M., Gücük, S., Ekici, A. et al. Urinary incontinence in female university students. Int Urogynecol J 32, 367–373 (2021). https://doi.org/10.1007/s00192-020-04360-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04360-y